Students
Nada Abdelrahim

Bioe extrodinaire: A student with an increasing interest in surgical procedures.This blog will cover my experiences shadowing the transplant surgery and orthopedics departments at UI Hospital in Chicago Illinois.
Nada Abdelrahim Blog
Nada Abdelrahim Blog
Nada Abdelrahim Blog

Image
Nada Abdelrahim Blog
Nada Abdelrahim Blog

Though the most exciting days are in my opinion the OR days, patients cannot enter surgery without going through the clinic first. A waiting room, seven patient rooms, and a very tight hallway houses multiple “clinics” at the same time. These clinics include pre-surgery and post-surgery patients. Inside where an MD, nurse, nutritionist, pharmD, financial adviser and social worker all work together, is where patients for potential transplants, organ donations, and dialysis port consultations come to see the transplant staff. Most of the patients are older and come to the clinic to become listed for a new kidney or kidney/pancreas combination. Also because this means their kidneys are approaching failure, they also need to receive a surgery to start dialysis until a kidney becomes available. Usually these patients are not only suffering from kidney failure but have had many operations in the past or currently have a number of ailments.
The fact is the people coming to this clinic are not healthy. I feel guilty at times that I am witnessing their private news alongside them. The doctor reveals the truth in a manner that is both direct and kind. I wonder how that can be done. The specific doctor I have been shadowing has a very amusing approach to dealing with her patients. She has a tendency to raise her eyebrows and joke with her patients. More importantly she never takes her actions to an inappropriate level and it is easy to tell she does not sugarcoat the issues of her patients to make sure they understand their options and what they are fighting against. This is an appreciative quality and I haven’t seen a patient become angry with the doctor as of yet.
Nada Abdelrahim Blog

Patient reactions/interactions are not all created equal however. One older gentlemen who came along with his wife would lightly banter with the doctor about his various surgeries and illnesses; he did not seem upset but more so used to his declining health. While the doctor was going about her procedure there was conversation and a more relaxed atmosphere. Another patient, a middle aged woman, came alone, and for every question the doctor asked she would give a stoic response. She did seem uncomfortable but not with answering the questions; it just seemed like the clinic was the last place she wanted to be. All the patients I followed the doctor to see gave off different body language and looks to us being there, but I believe that their desire to be healthy glossed over the fact that there were students to tag along for the ride.
July 17, 2014
Nada Abdelrahim Blog

Image
Nada Abdelrahim Blog

Nada Abdelrahim Blog

Nada Abdelrahim Blog

July 18, 2014
Nada Abdelrahim Blog

Image
Nada Abdelrahim Blog

Nada Abdelrahim Blog

Image
Nada Abdelrahim Blog

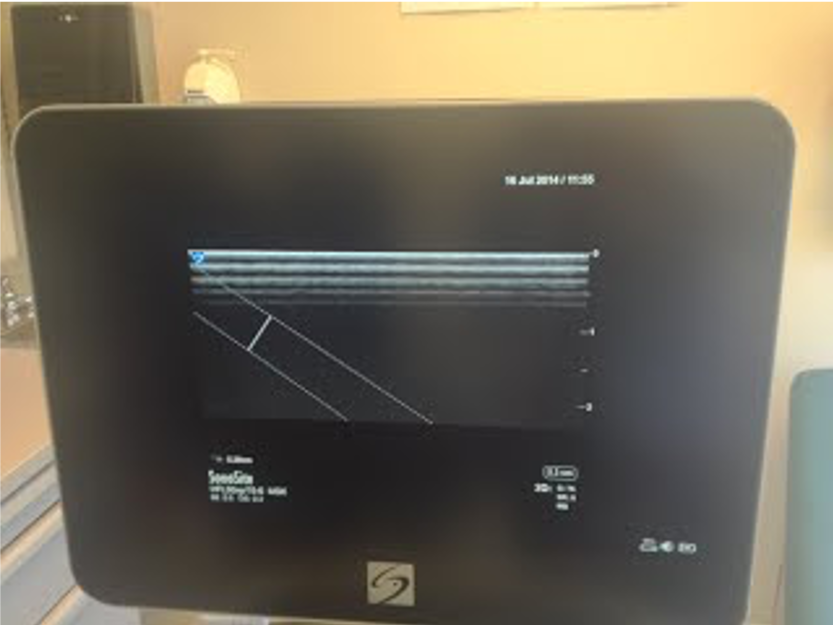
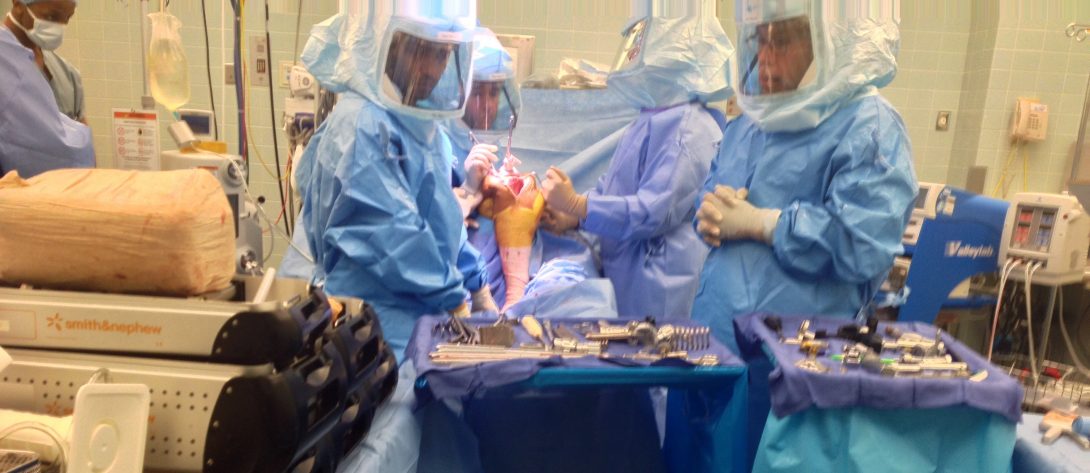
Indications for an arthoplasty include cartilage loss on the knee, severe arthritis, and generally includes severe pain associated with the entire knee. Pain is the root of the problem and this pain makes moblilty limited or even impossible. Some patients who came in for post operative examinations for the total knee were overall satisfied with some patients saying their prosthetic knee was being slowed down by their other knee. The total knee is pretty routine but it is a major surgery that requires involvement of the patient to ensure the healing process is complete to an optimal level. The actual surgery requires drills and buzzsaws to shave the femur and tibia bones to fit the prosthetic. Surgeons must be aggresive when conducting this operation to make holes in the bone and insert the knee prosthetic successfully. Also important is the angles they are the cutting the bones. A healthy knee should have a five to seven degree valgus of the knee. This means that the load bearing axis in the knee is not putting too much much pressure on the outside of the knee. If alignement is done correctly the surgeon will have successfuly replaced the bad knee and allow the patient to regain their comfort. If not done correctly the pressure from the forces on this joint will eventually lead to the prosthetic cracking. Needless to say, despite the routine nature of this operation, risks are high and infection is too prevalent. Understanding and designing prosthetics in a way to withstand infection would greatly reduce the risk associated with this operation.
Nada Abdelrahim Blog

Haroon Papa

The Bioengineering Clinical Immersion internship aims to produce engineering students with a greater understanding of the clinical domain . This is accomplished by placing students next to the physicians and patients in order to understand what they go through on a daily basis.
Haroon Papa Blog
Haroon Papa Blog
Entry 1: Week of 7/07/2014
posted Jul 9, 2014, 8:38 PM by Unknown user
The first day of the Bioengineering Clinical Internship begins! As customary, the first day began with a meeting to discuss the intern’s role in the clinical environment and what sort of thoughts should be running through our heads. We received nifty notebooks, and were told to go forth and document what we see, hear, and feel.
So, I trekked uncertainly to the G.I. lab for my first rotation and met the attending physician Dr. Robert Carrol, quoted by one nurse to be the resident genius. There may have been a little miscommunication as my contact, a Medical Fellow by the name of Dr. Vineel Kankanala, was not in the G.I. lab for my first day. Nevertheless, the nurses and another fellow, Dr. Sugir, in the lab graciously showed me around and got me acquainted with the lab. Without further ado, I was plunged into a procedure room in the middle of a routine colonoscopy.
Before setting my sights on the procedure I made sure to take a good look all around the room. What I noticed was a plethora of notes posted on walls, and little labels all over cabinets and drawers. Yet, most nurses and doctors hardly paid any attention to this information, and almost never used the drawers. Most of the equipment/gear that they used was already out and easily within reach. I came to the conclusion that the majority of unused medical equipment was for emergencies, which I came to realize were uncommon in G.I. procedures.
Finally I set my eyes on the operation itself, the climactic act of excising polyps from the colon. I almost passed out. Lead by a nurse I stumbled into the bathroom with a bag of ice around my neck, my eyes like plates. My body weighed an extra 100 lbs, and I wasn’t all too sure what had happened. Additionally, I had an ominous feeling about undertaking a medical career. When I came around, I found the nurse who helped me and profusely apologized for what happened. She warmly told me that it was not a big deal, and its not an infrequent occurrence. My response was something called a vasovagal response. After my experience, the attending physician and tech assistant laughed and told me they’ve seen responses such as mine commonly and it’s something many people deal with and overcome.
My experience with this phenomenon called the vasovagal response showed me the empathy the nurses and doctors have. I was blown away by how quickly and kindly the helped me, and I now have tremendous respect for the G.I. lab department.
Entry 2: Week of 7/07/2014
posted Jul 9, 2014, 8:41 PM by Unknown user [ updated Jul 12, 2014, 9:24 AM ]
AS A FOREWARD:
posted Jul 16, 2014, 8:40 PM by Unknown user
posted Jul 18, 2014, 7:50 PM by Unknown user
posted Jul 23, 2014, 4:26 PM by Unknown user
Entry 6: Week of 7/21/2014
posted Jul 23, 2014, 4:28 PM by Unknown user [ updated Jul 26, 2014, 2:44 PM ]
posted Aug 3, 2014, 7:58 AM by Unknown user
This week Justin and I rotated into Transplant Surgery under Dr. Ivo Tsvetnov. We found ourselves on the 7th Floor of the Hospital where many patients in the Transplant unit are in critical care.
posted Aug 3, 2014, 8:42 AM by Unknown user
At the instruction of residents and the medical students Justin and I spent time in the OR and the Transplant clinic in the Eye and Ear infirmary for the remainder of the week.
posted Aug 7, 2014, 10:36 PM by Unknown user
posted Aug 11, 2014, 12:57 AM by Unknown user [ updated Aug 15, 2014, 7:32 PM ]
My final week in transplant was bittersweet, but packed with unforgettable experiences. The second half of my week encompassed a few major operations and in-depth rounds. Furthermore, I got the experience to talk with Jurgis, a medical student, and a resident, Dr. Arun, about what I saw, heard, and felt.
A sobering and humbling experience in medicine is the inevitability of death. Despite the best efforts of the transplant physicians on staff and nurses, patients can die. The patient mentioned in blog post 9 passed away. His passing was chosen by his family, because he had reached a critical state where he would only survive with the constant infusion of blood, IV fluids, and oxygen. When I had last seen this patient he was gasping for air, hooked up to 6 infusion pumps, and had a heart rate above 120 consistently. In all honesty, I feel slightly relieved that the patient’s suffering did not continue. At the same time, I was dissatisfied with the technology that the man relied on, as it did not heal him but only just kept him alive. I was also musing that the patient’s family’s perception of the number of infusion pumps, IVs and monitoring equipment hooked up to the patient could have influenced their decision in removing the aforementioned systems. Although I have my own fascination with medicine, life, and healing the enormity of death will always oppose the efforts of physicians.
The major operation that I was privy to see was a nephrectomy; the surgical removal of the kidneys. This operation is only done when the kidneys become non-functional and are a detriment to a patient’s well-being. The patient in question had kidneys that had become non-functional and filled with cysts. The left kidney had broken through the peritoneum and had deformed the small bowel. The procedure required the kidneys to be tied off and removed surgically. The major tools used were scissors, a clamp to open up the cavity, and a cauterizer. Though these were relatively simple tools to conduct the surgery, it was done successfully. Prior to the surgical procedure, the patient was undergoing constant pain, and did not have a high quality of life. The surgery was a step towards restoring this patient back to health, and presumably a life with less pain. Ultimately, the patient will undergo dialysis 2 times per week until they can receive a transplanted organ.
These two experiences showed me vastly different sides of medicine. The human aspects as well as the technological aspects that we were meant to focus on. From this I now place more importance in human perception of healthcare along side the efficacy of the involved technologies. Between these two ideas design can emerge and create a common point of intersection that understands the issues of both a physicians and a patient with an engineering edge.
Final Blog — Friday, August 15th, 2014
posted Aug 15, 2014, 8:02 PM by Unknown user [ updated Aug 18, 2014, 12:45 AM ]
Whirlwind, experiential, unbelievable, beautiful, and downright fun. Those adjectives barely begin to describe the Clinical Immersion Internship under the guidance of Professor Sterling, and Dr. Kotche. The purpose of this internship was to guide students toward empathizing, and understanding the feelings of both patients, and clinicians in a healthcare setting. This experience was truly eye-opening.
I began my first day at the internship by nearly passing out in the middle of a routine colonoscopy in the UIC Hospital G.I. Lab. I remember the tunnel vision forming around my eyes, the sounds of the G.I. lab becoming more and more distant, and the sudden shock of an ice pack hitting the back my neck and bringing me back to reality. Thankfully, a nurse had been paying attention to me and made sure to sit me down in a bathroom and talk me through the frightening experience I was undergoing. This experience showed me the kind of care that nurses and doctors provide in the hospital; despite the enormous amount of bureaucratic shuffling they do, and filing of papers, at the end of the day they are there to take care of people.
Past the human standpoint, I went to analyze the tools/layout/procedures of the physicians in order to identify some sort of need. Now that leads one to question, what exactly is a need? A need is something that must be had, or something that is essential. The essentials that I witnessed were: extra training for colonoscopies, a more intuitive colonoscope, and a colonoscope with a larger visual field. My general experience in the G.I. Lab was that of EGDs (esophagogastroduodenoscopy) and colonoscopies. Though these procedures were typically outpatient, and not difficult in a skilled hand, new fellows and medical students would have difficulties in maneuvering and obtaining the correct positioning without causing some ramming of the intestinal wall. This observation founded my interest in extra training for G.I. fellows/students. Furthermore, the colonoscope has an incredible number of functions which range from taking HD pictures, clamping polyps for biopsies, deploying a net, spraying air or water, suction of air/water, and even cauterizing biopsied areas. It’s no wonder that 2 people, the attending physician and nurse, are required to operate the numerous different functions of the colonoscope by using a footpedal, a controller, and by literally pushing and pulling the colonoscope in and out of the colon. A more intuitive colonoscope would hopefully give all the control to 1 person, as well as be easily manageable in control by centralizing controls. In addition to this, I noticed that the colonoscope had to take several different camera angle shots, many of which required tricky maneuvering and extensive pushing and pulling of the scope for proper bending. Perhaps additional cameras with a wider scope/visual field would reduce the necessity of all these movements. In essence, these solutions seek to streamline the colonoscopy/EDG procedures because ultimately they are embarrassing, sometimes painful, and somewhat of a hassle (though they are HIGHLY necessary).
Next, I found myself in the Transplant Surgery rotation in the hospital. The main areas I frequented were the transplant ICU, the transplant clinic, and the OR. Between these three areas, the OR happened to have much of the advanced technology and techniques for surgical operations. For example, the da vinci robot for minimally invasive transplant surgeries is a tool that empowers surgeons to make incisions and cuts with higher precision and maneuverability than a human can normally do. While the transplant ICU featured ventilators, ultrasound equipment, infusion pumps, and ECG machines. Much of the equipment used in the ICU was typical in most ICUs in the hospital. The clinic on the other hand had little to no technology, for the most part it was meeting space for patients and physicians. Furthermore, the clinic was rather cramped and little adornment; the walls were largely blank and dull. Ultimately, many of the proposed improvements in technology for Transplant would be involved with the ICU. This is because the largest problems are not exactly health related, rather they are centered on the ergonomics of patient comfort. For example, infusion pumps are sometimes stack upon each other, up to 5, in case a patient needs multiple different intravenous medicines at once. This can lead to very heavy IV poles, and decreased patient mobility. Another issue noted was that the beds and infusion pump had no point of attachment. Some solutions for these issues would revolve around having 1 infusion pump do multiple medicines at once, rather than separate infusion pumps for each medicine. Also, the infusion pump device could be incorporated into the bed for increased mobility, or even a backpack apparatus for increased portability among younger patients/older patients.
What was most surprising about the Transplant surgical rotation was the human aspect. I learned that Transplant surgery was much more stressful than I anticipated. The rotation had medical students and residents working around the clock for 10 hours for multiple days, and many of them were running on minimal sleep. Between deciding medications and conducting surgeries that would determine the difference between life and death, the sleep deprived surgeons seem to have adapted to this high stress environment. In response to that conjecture, I feel that it would be highly appropriate to design tools that are easy to use at all times, and require little forethought before putting them into operation. I have reconsidered my interest in being a surgeon, as it calls for a greater sacrifice of personal time and life than I might want to give. I believe in living a balanced life, and in some ways the lives that are lived by the people I saw were undoubtedly one-sided (though I believe their work is necessary and incredibly important).
Once again, I would like to thank Dr. Kotche and Professor Sterling for allowing me to foray into these once alien subspecialties in medicine. I have learned incalculably important information, and I feel like I have developed a new design engineering mindset that will allow me to approach bioengineering problems in a new light.
Haroon Papa Blog

Image 1: A typical bedside for patients awaiting their procedure, or recuperating post-op.
Haroon Papa Blog
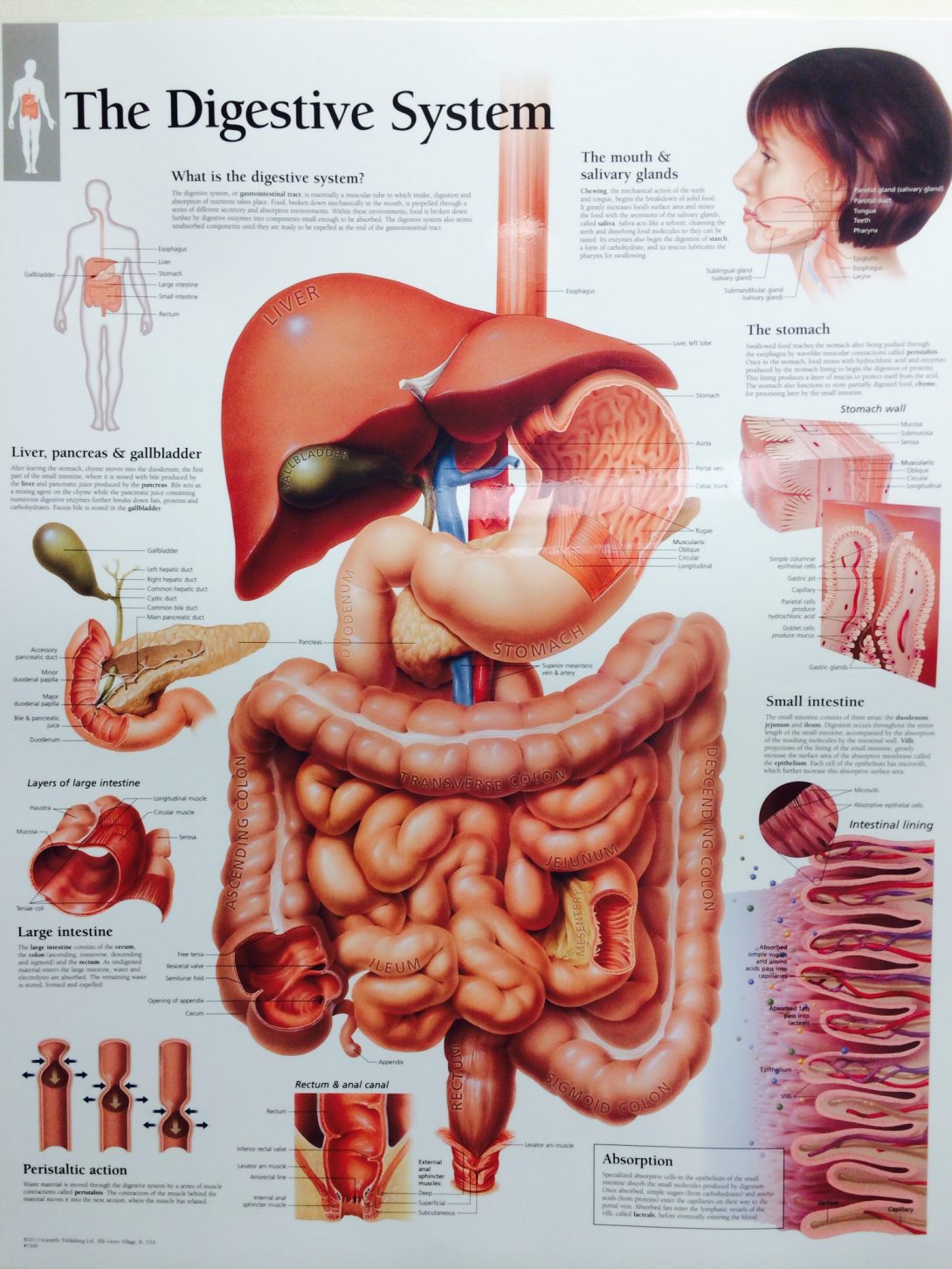
Image 2: Pictorial representation of the digestive system.
Haroon Papa Blog

Image 3: Fluoroscopy Room, where high contrast dyes are used for imaging.
Haroon Papa Blog

Haroon Papa Blog
Haroon Papa Blog

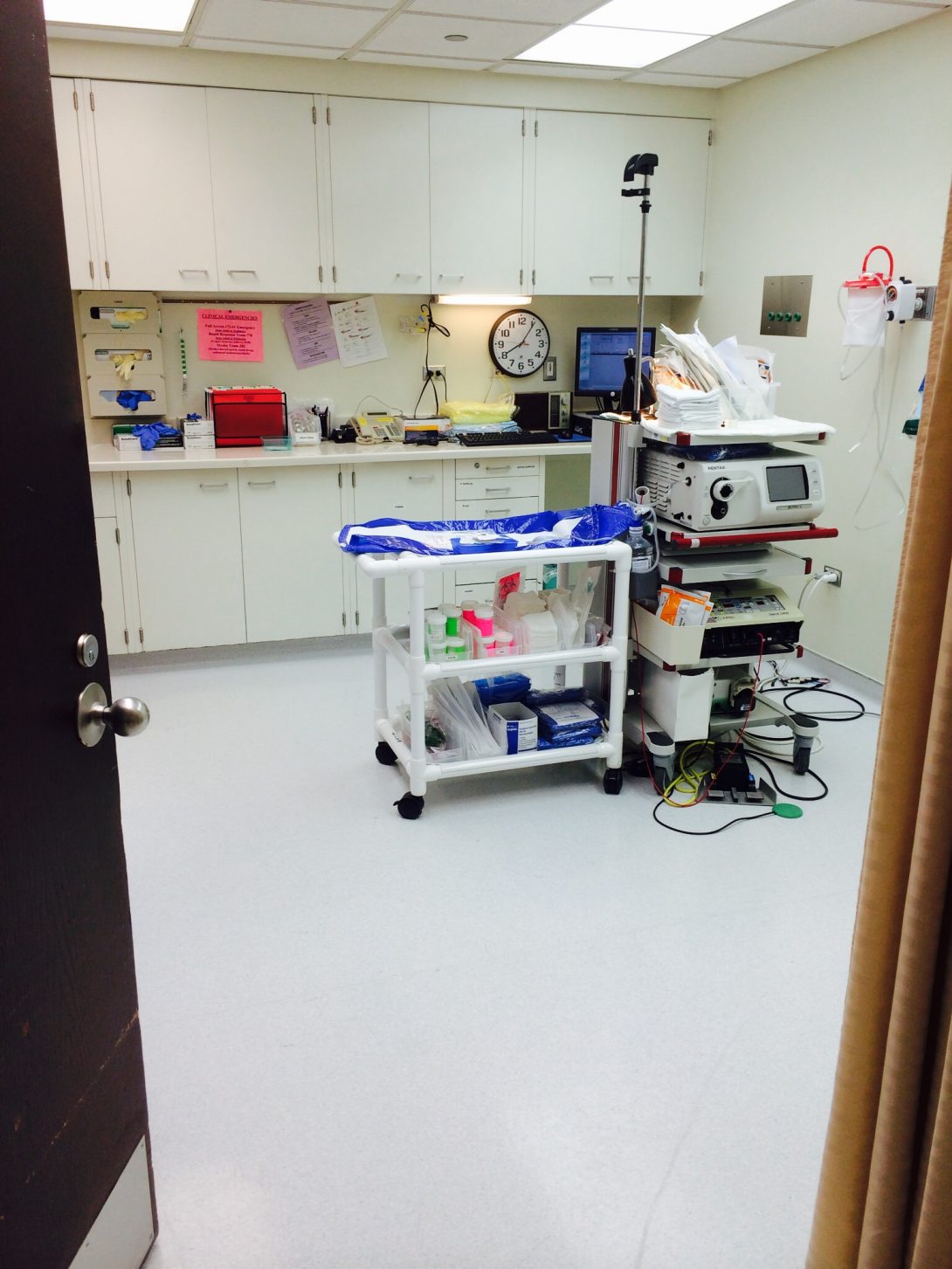
Image 6: Procedure room 2.
Haroon Papa Blog

Image 7: Procedure room 3.
Haroon Papa Blog

Image 8: Procedure room 4.
Haroon Papa Blog

Image 9: A colonoscope!!
Martin Gannon

Martin Gannon Blog
Martin Gannon Blog
Week 1 Ophthalmology
Week 1 Ophthalmology
Week 2 Ophthalmology
Saturday July 19th
Week 2 Ophthalmology
Sunday July 20th
Week 3 Ophthalmology
Monday July 21st
Week 3 Ophthalmology
Tuesday July 22nd
Week 3 Ophthalmology
Wednesday July 23rd
Week 4 Anesthesiology
Monday July 28th
Week 4 Anesthesiology
Tuesday July 29th
Week 5 Anesthesiology
Tuesday August 5th
Week 5 Anesthesiology
Wendsday August 6th
Oximetry
Week 5 Anesthesiology
Wednesday August 6th
Week 5 Anesthesiology
Martin Gannon Blog

This is a neuro-radiology room. In the foreground you can see the patients brain vascular on the screen in the monitoring room. In the other room you can see the anesthesiology monitoring equipment and in the background is the radiology machines. They are able to obtain a 3D view of a patient’s vascular system.
Week 6 Immersion Review
Three Weeks:
I think rotations lasting three weeks can seem long. However I found that I was not really able to appreciate the nuance of a medical specialty until I had adjusted to everything. On the first day of ophthalmology I showed up cold at the glaucoma department. I didn’t know the first thing about how to examine someone’s eyes, how to looking into a teaching side scope, or how to interact with patients and staff. By the end of the ophthalmology rotation I was able to diagnose people with cataracts in 2 seconds. And felt comfortable in my role as a suede medical student when interacting with staff and patients. Similarly in anesthesiology, I spent the first few days going: “that’s really cool”, “that’s really sad”, ‘that’s really disgusting”, and “those are a lot of words I don’t understand”. But after I got used to all of that stuff I was able to understand the typical workflow that an anesthesiologist goes through for each patient. Towards the end of both rotations I felt like I knew how to ask more relevant questions concerning what doctors would like from engineers and also what are their top worries were during a procedure.
Week 6 Anesthesiology
By complete serendipity we had an opportunity to observe a meeting of OR nurses. They happened to be reviewing a spreadsheet of which products they want to buy. The following is a lightly edited version of my notes I took down on Evernote:
Senior nurses sit together deciding what equipment they need. They are mid career people, experienced but also young enough to not be counting the days till retirement.
Packaged deals get you a discount from Strykr. The hospital did not go with that option, unclear why.
Have to consider marginal costs (battery replacement, how cheap is to fix, how quickly do we need a replacement)
“How many times does this break…Has that effected patient care.”
Doctor XYZ is complaining about ABC. The squeaky wheel got greased.
At conferences world renown doctor lies to other doctors about having 3D vision microscope. 3D is not for patient care; it’s for educational and research reasons. (Nurses discuss whose budget this device falls under.)
They use combined experience of how the office works, how devices get used. The third floor ORs will be remodeling in a few months.
Excel spread sheet:
Service, ranking preferences for each category, Manufacture, Notes (links to brochures and pricing).
Brochure links are ignored
Renting rectal probe for $1,000 per operation was considered a good deal. No need to buy.
Synframe in spine curette tray removed from list while laughing.
$3k for spine fusion is cheap. But they are not needed; enough are lying around. There is a department at the hospital that figures out how much inventory waste vs the cheap cost.
Parts are out of date on some equipment in the OR. Once the device breaks “SOL”
Old device makes noise. “Is it supposed to do that?”
Device Blank is good for 5 years. We keep Device Blank for 7 years.
The goal of the meeting was too rank preferences for each medical device requested by group LMNO in each category. And then send that out to QRS.
Matt de la Cruz

Join me on this crazy awesome clinical journey!
Matt de la Cruz Blog
Matt de la Cruz Blog
First Clinical Post (Week 1 – First Post)
It’s only the first few days of this internship, but I’m already having a blast! The clinical environment is honestly quite new to me and it gets really hectic at times. The first few days I got to observe some physicians and nurse practitioners in the clinic. One of the nurses introduced me to the works of JJ Collins and gave me a little bit more background info about the Gastroenterology and Hepatology Clinic. I was informed of some of the procedures that patients have to undergo to see the problems in the GI Tract. I’ve noticed that patients are really hesitant to receive a liver biopsy, or really anything invasive. In my opinion, I don’t blame them. You can’t be on any blood thinners like Aspirin and it takes up the whole day. A few patients have had bad experiences with it. That is why I am excited for the clinic to receive a machine called FibroScan. Basically, it is able to non-invasively test for fibrosis in the kidney! I still have a lot to learn and I learn more every day that I spend in the clinic! Tomorrow, I plan to talk about the types of people that I’ve seen and the interactions I’ve observed.
First Week Recap (Week 1 – Second Post)
After we had given our introduction to the experience, I went to the GI Clinic with my heart racing and my mind ready for observation. I walked into the clinic and was received with friendly greetings from the receptionists. I then met my point person and we went into the infusion room. The infusion room was dark, mostly to the preference of the patients. My point person gave me a little background information about what goes on GI Clinic. I learned a little about Esophagogastroduodenoscopy (EGD), Diverticulitis, and Helicobacter Pylori. After a while, a practitioner arrived and I began to shadow him while he saw patients. The first patient was an older fellow, healthy too, discussing his condition of Primary Biliary Cirrhosis with the practitioner. When a biopsy was mentioned, he cringed because the last biopsy apparently did not go well. He and his wife seemed resigned, stating that his “clock’s ticking down.” The third patient had neurofibromatosis. She was remarkably insistent on some sort of pill to get her bowels moving, but the practitioner was stalwart that Miralax would be sufficient. A lot of people seem to want the “latest and greatest” in medicine, but the desire seems to blind them to methods that work just as well. Another patient came in for a check up on her carceroma, and contrary to that patient earlier, she just decided to not do anything because she is 77 years old. Not even a biopsy. She told us that she’s tired and that her kids already know her decision. I’ve never seen anything like that. In general, the practitioners try to be as personable as possible and make sure the patients know exactly what is going on. Practitioners answer only what they know is certain so that there is no room for confusion or misunderstanding. The clinical environment does not seek to leave people in the dark, it seeks to educate the people that come in. There were a few patients that required a Spanish translator and unfortunately I was not able to help with that.
Endoscopy-ception! (Week 2 – First Post)
This week I had the pleasure of being in the GI Lab. After a week talking about the procedures that happen, I would finally see it for myself. I meandered in to begin my second week of immersion.
Rise and Shine for a Radiology Conference! (Week 2 – Second Post)
The fourth day of the second week was observing more procedures. I started to understand just how difficult it is to move the endoscope through the GI tract. My colleague Haroon has a good a idea with creating a simulation of sorts so that not only fellows could get additional training, but maybe patients can understand more of the body. When procedures begin, a time out is done. That is simply name, date of birth, and the procedure. Prior to that, the attending physician comes in and informs the patient about the procedure whether it is a colonoscopy, EGD, or anything else. The standard of medicine has truly changed because now it is more of a let me help you understand what’s wrong and let me fix that. A technology that I was informed about was a pill camera. It is swallowed and then takes pictures of the entire GI tract! Amazing!
Provation 5.0? More Provation 5 point NO (Week 3 – First Post)
So starts the third week of my rotation in GI. The program said “inpatient consults,” so I was very interested to see what was going to happen. As soon as Haroon and I arrive at the lab to begin, we notice something different about the computers, specifically the records. Over the weekend, the lab changed to Provation 5.0. We were informed that it was in phase 2. Basically, all lab staff must log in with each new patient and out after every patient. This was not the case before as the records allowed doctors to freely examine the notes. Overall this is a change that should be implemented, but it is a bit of a hindrance in regards to acquiring information to reflect on. Before we started inpatient consult, we got to witness an Ileoscopy. The colostomy bag (a bag of waste) was removed and the endoscope was placed inside the Ileum. The patient had a small bowel transplant and was following up. After that we had went back to clinic to start the consults. Unfortunately, we were not able to keep up with the students that had the information. The consult is medical students and a fellow presenting cases to an attending physician and the physician talks through what’s happening and what’s going to happen with the patient. Once those had concluded, we took our leave.
GI Wrap Up (Week 3 – Second Post)
It’s been a little slow with inpatient consults for GI. It isn’t as involved and without prior information, it is very easy to get lost. However, we decided to make the most of observing procedures in the lab. We got to witness another Bronchoscopy, this time with X rays! The reason for the X rays is to be able to biopsy tissue from the lungs without collapsing it. Obviously, it is a very delicate procedure. A prior observation of the Bronchoscope was that it only moves in one plane. Perhaps that is because navigation through the bronchial tubes is easier in one plane so it might be to ease navigation. The bronchial tubes are indeed different from the colon or the esophagus, so a different design may be considered for it. One final interesting thing is the pill camera often gets stuck in the GI Tract. I wonder if there is a good way to get around that?
Onto Orthopedic Clinic! (Week 4 – First Post)
The time has come for the second rotation. This time, I am in Orthopedics. I will be recounting the events from Monday through Wednesday.
These Scrubs Are Awesome! (Week 4 – Second Post)
Thursday
Casting With Frank (Week 5 – First Post)
Frank in the casting room of the Orthopedic Clinic was kind enough to take Nada and me under his wing for the majority of the day. There, we got to witness cast removal and cast applications. Casts are either made up of Plaster of Paris or Fiberglass. Plaster of Paris takes longer to dry, is heavier, is more moldable and is also stronger. Fiberglass, in contrast, is lighter and it dries faster. Fiberglass is the material that is typically used, but Plaster of Paris is used occasionally for the instances where molding is necessary. Both materials must be dipped in water to start the hardening by removing the polyurethane resin. The cast is then applied over bandages and wraps. After the cast has been fully wrapped, it is rubbed down to facilitate drying and hardening. The cast removal is an oscillating blade hooked up to a vacuum to suck up the fiberglass shards. I had thought that maybe we could invent a way to make the cast removal mobile, but maybe it’s not such a good idea.
Here, We Observe a Hand Procedure – Oh, It’s Done Already. (Week 5 – Second Post)
We were fortunate to spend another day in the OR shadowing Dr. Mejia. Every doctor has their own specific way of doing things, seems obvious but there is quite a contrast between the three doctors we’ve followed. Mejia has shown in both surgery and clinic that he is very technical. He knows exactly what he wants, though I shouldn’t expect any less from the Director of the Residency Program. The most noteworthy thing we witnessed was a fracture surgery. The procedure was putting wires through the area of fracture to support the area while the bones heal. The wires were administered using a drill of sorts and were guided by X Ray so naturally we had to wear lead. The X Ray technician had to be ready to take an X Ray at the surgeon’s request. Most likely this was done to reduce the amount of radiation administered.
Wrap It Up (Week 6 – Last Post)
The last week of Orthopaedics just seemed to fly by. We followed the same schedule as the first week of the Ortho rotation, with the exception of Friday presentations of course. One remarkable thing about the week happened in the OR of course. Dr. Gonzalez performed a knee replacement on a patient, but the method seemed completely different from Dr. Chmell. Gonzalez uses cement to secure the joint, but Chmell does not use cement. It shouldn’t come as a surprise, but it’s kind of refreshing to see that even within the department, there is a great amount of diversity. Frank explained to us that even for a simple stabilization of the finger, the physicians do completely different things. One more thing, Frank Radja is an amazing human being that really made Ortho a wonderful, fantastic experience. He even invited us to a wrapping class! Thanks to Frank, Dr. Gonzalez, Dr. Chmell, Dr. Mejia, and all of the residents, we ended up having a wonderful time in Ortho! I learned to re-evaluate my knowledge and put forth a greater effort to develop my expertise. I leave the department with higher spirits and a determination to do the best I can do!
Image 1

Image 1
Image 2

Image 2
Image 3
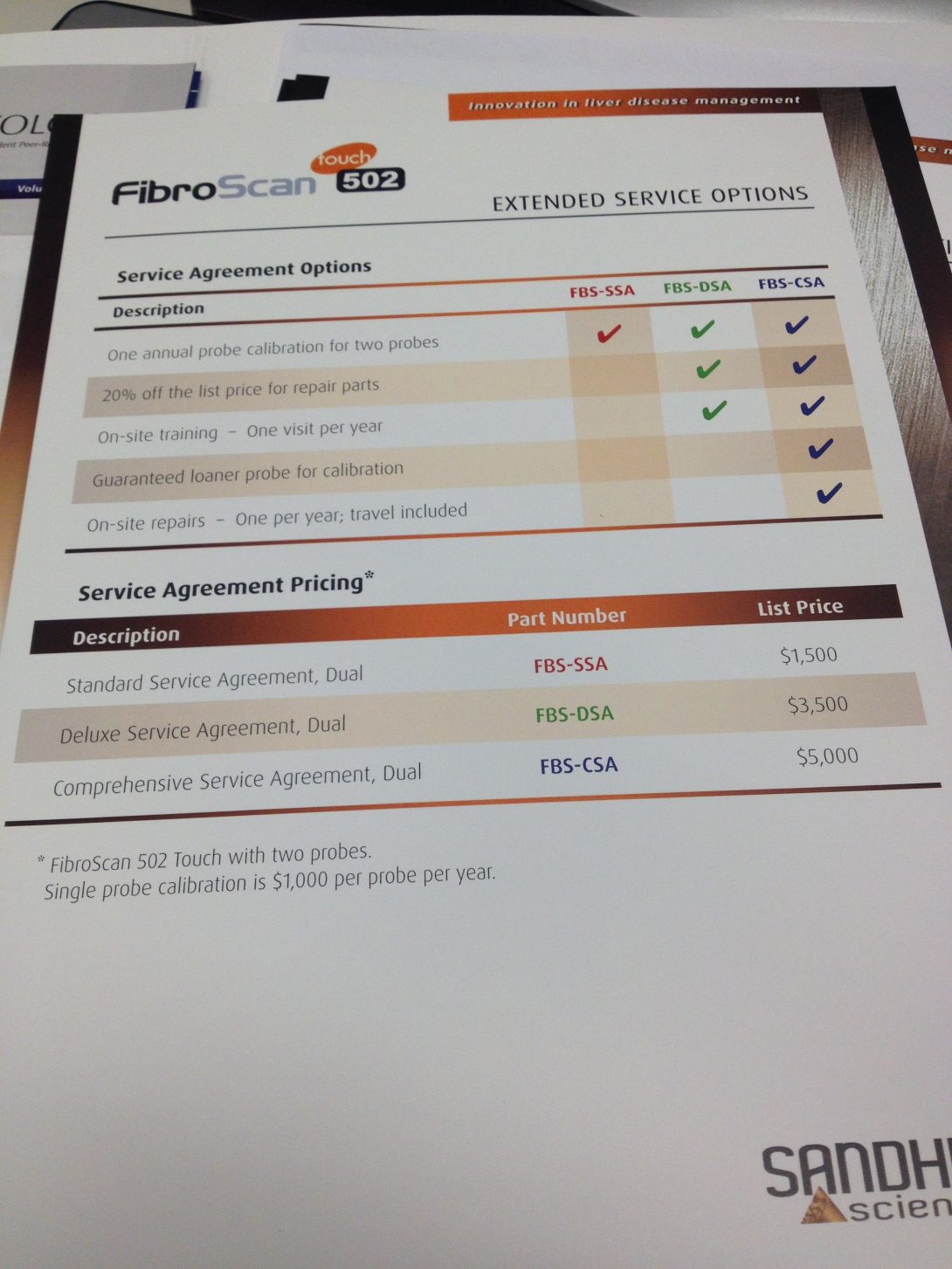
Image 3
Image 4

Image 4
Image 5

Image 5
Image 6

Image 6
Image 7
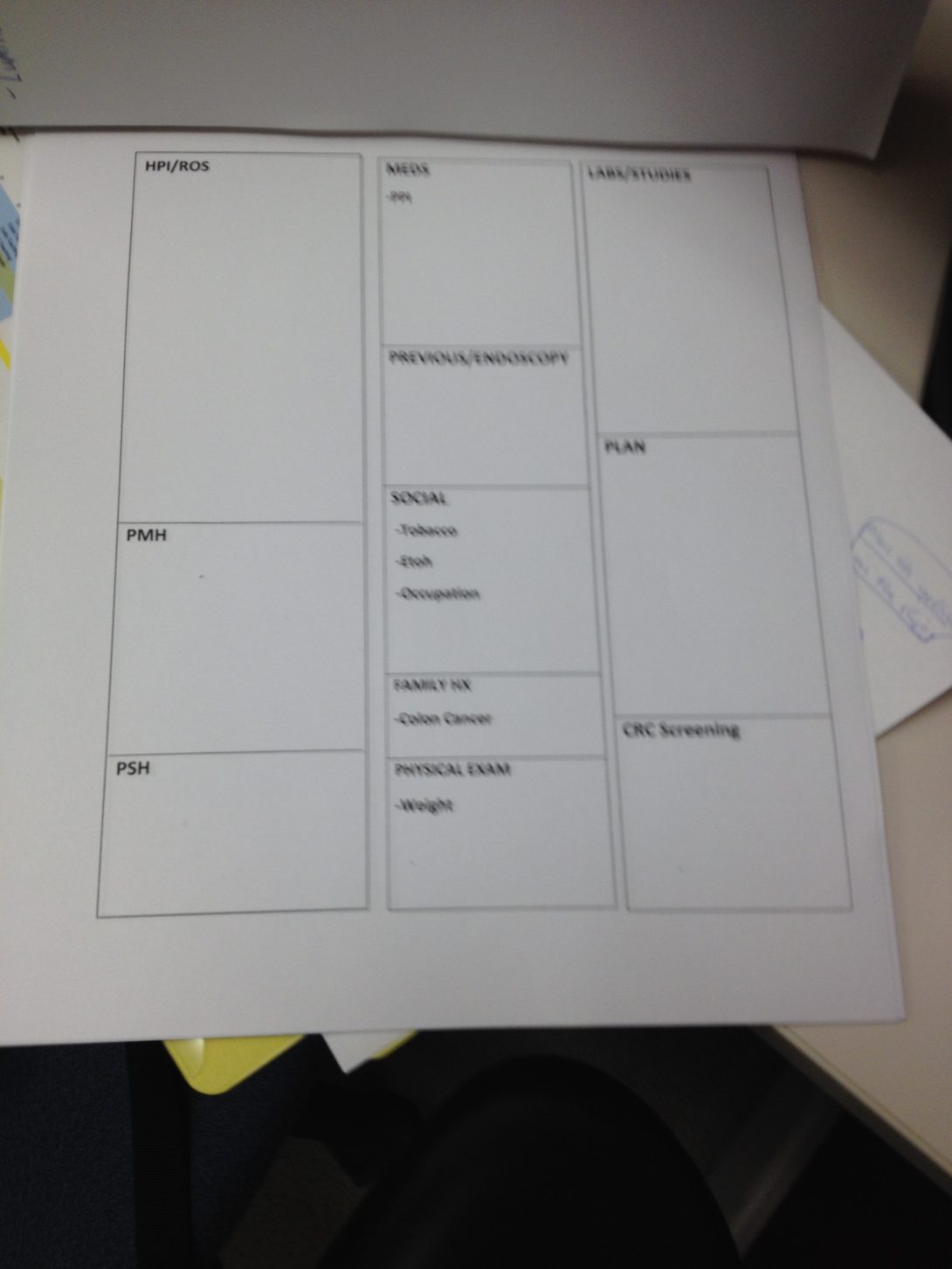
Image 7
Image 8
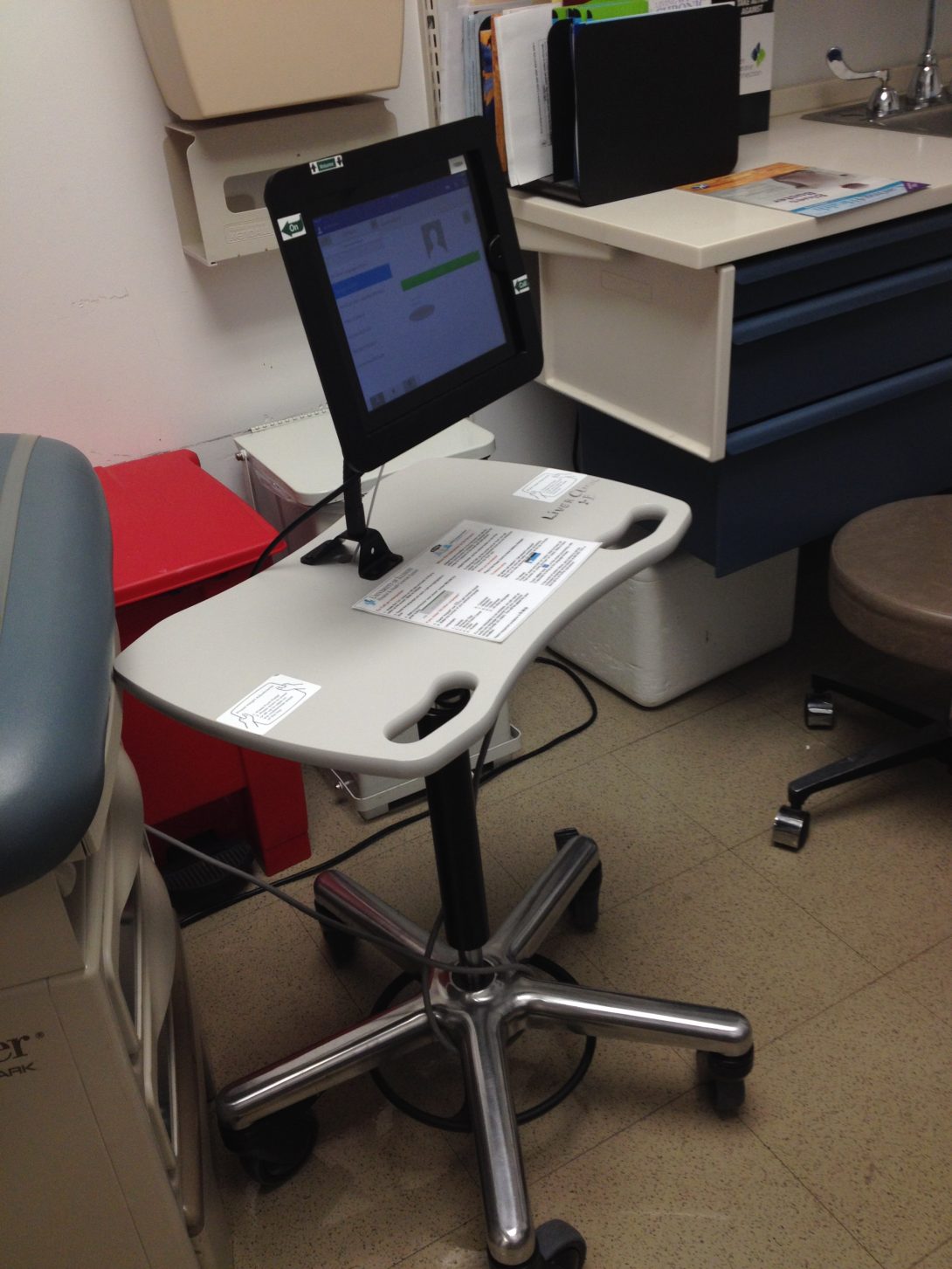
Image 8
Image 9
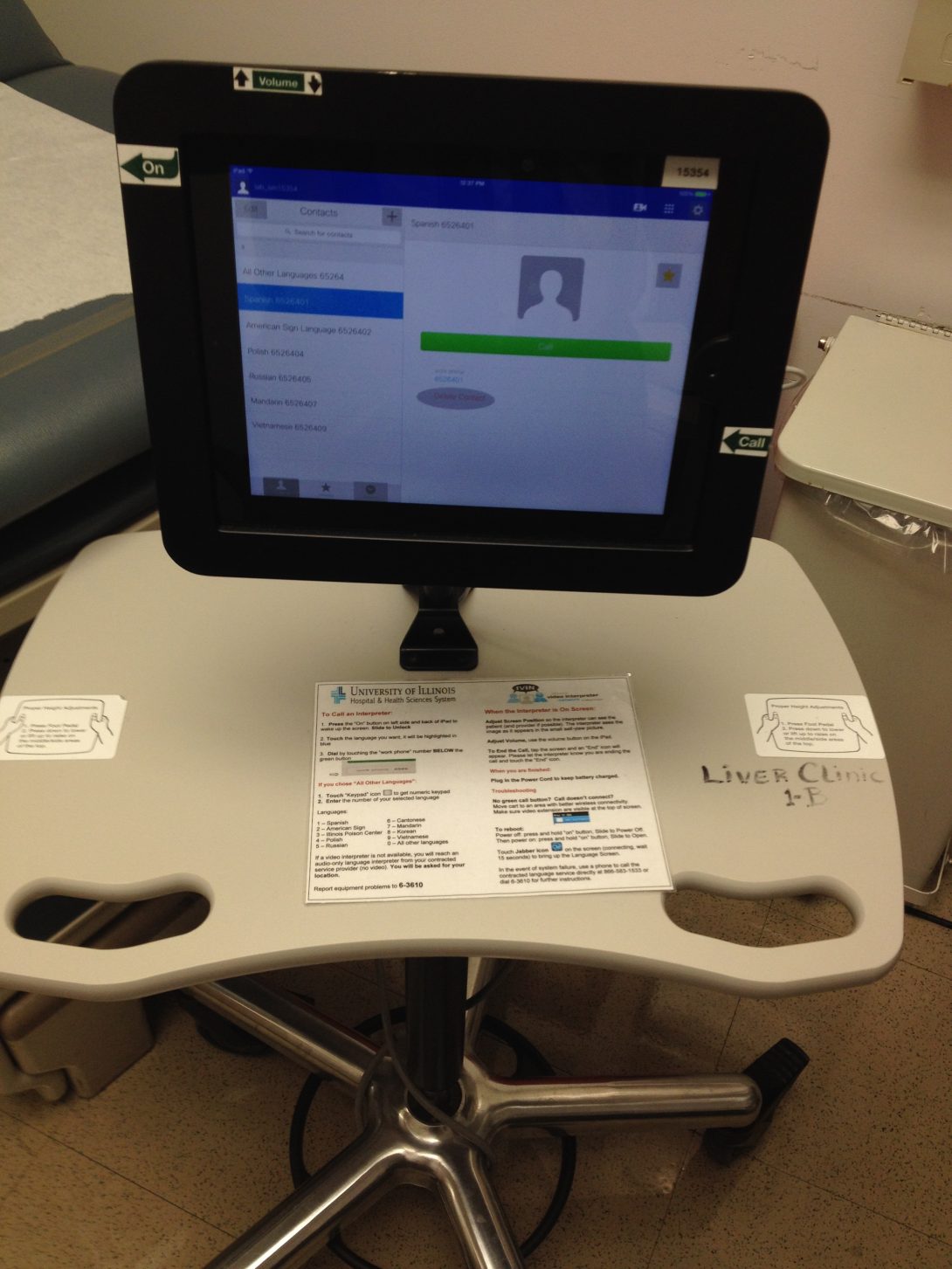
Image 9
Image 10
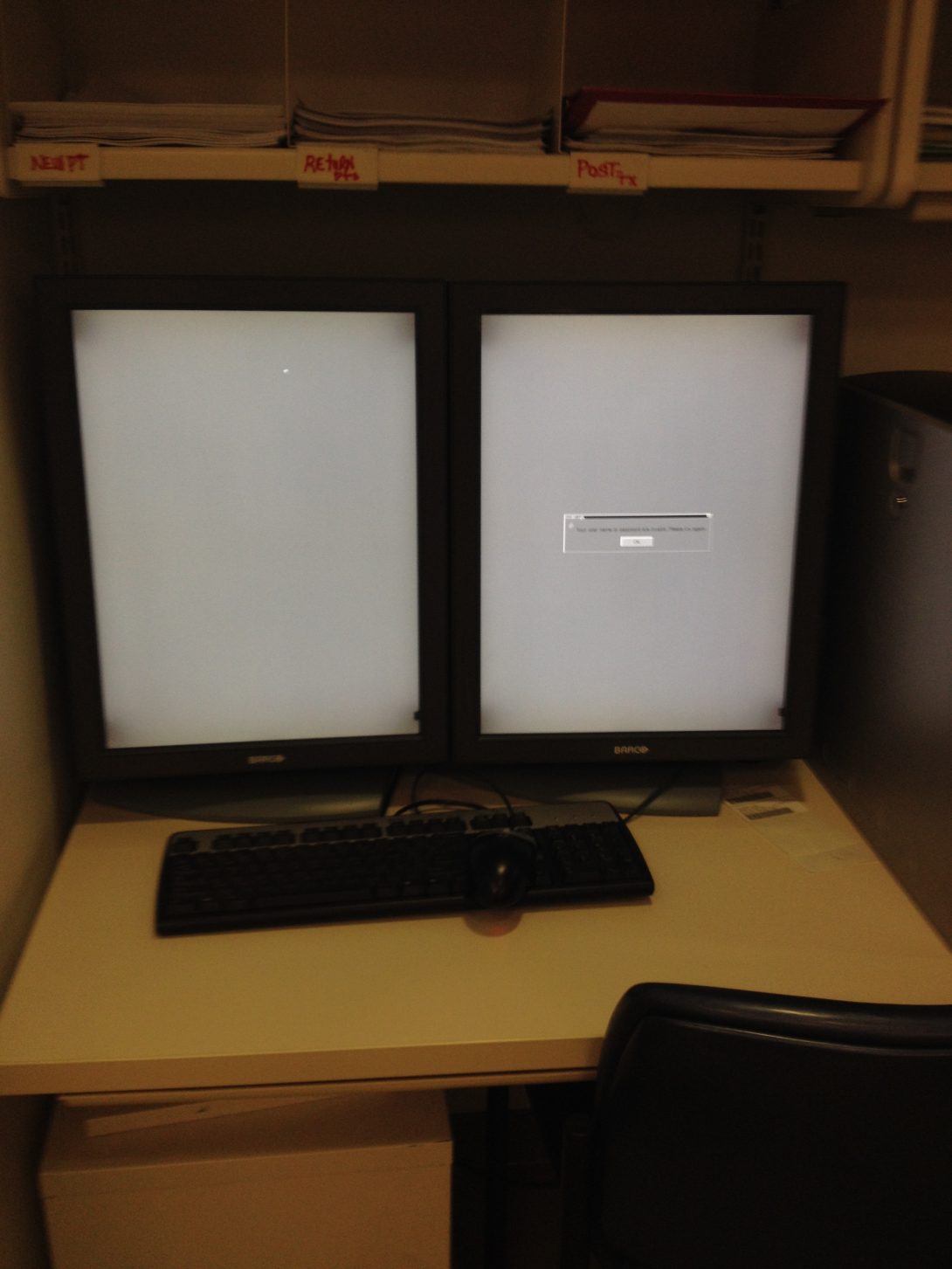
Image 10
Image 11

Image 11
Image 12

Image 12
Image 13
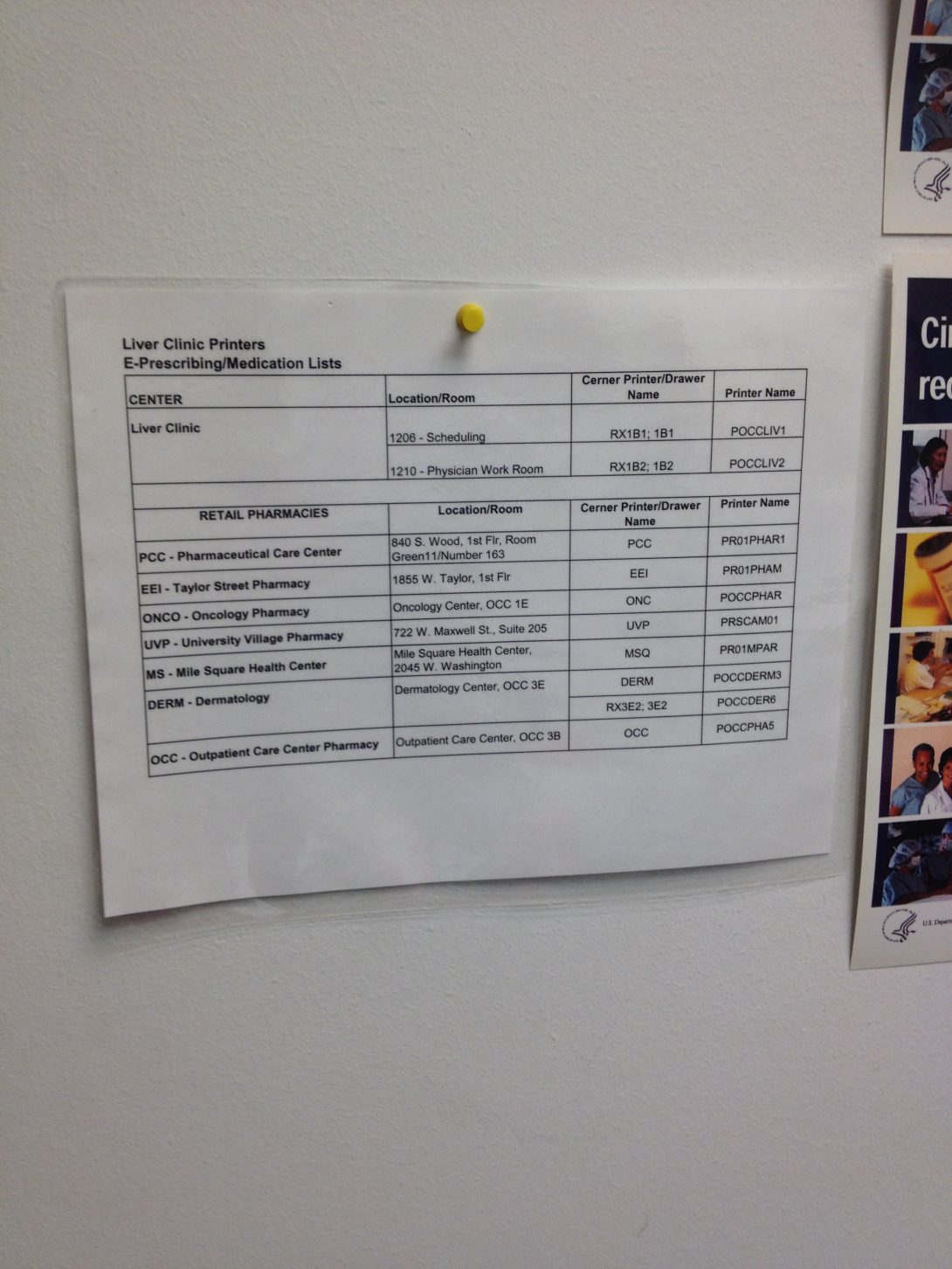
Image 13
Image 14
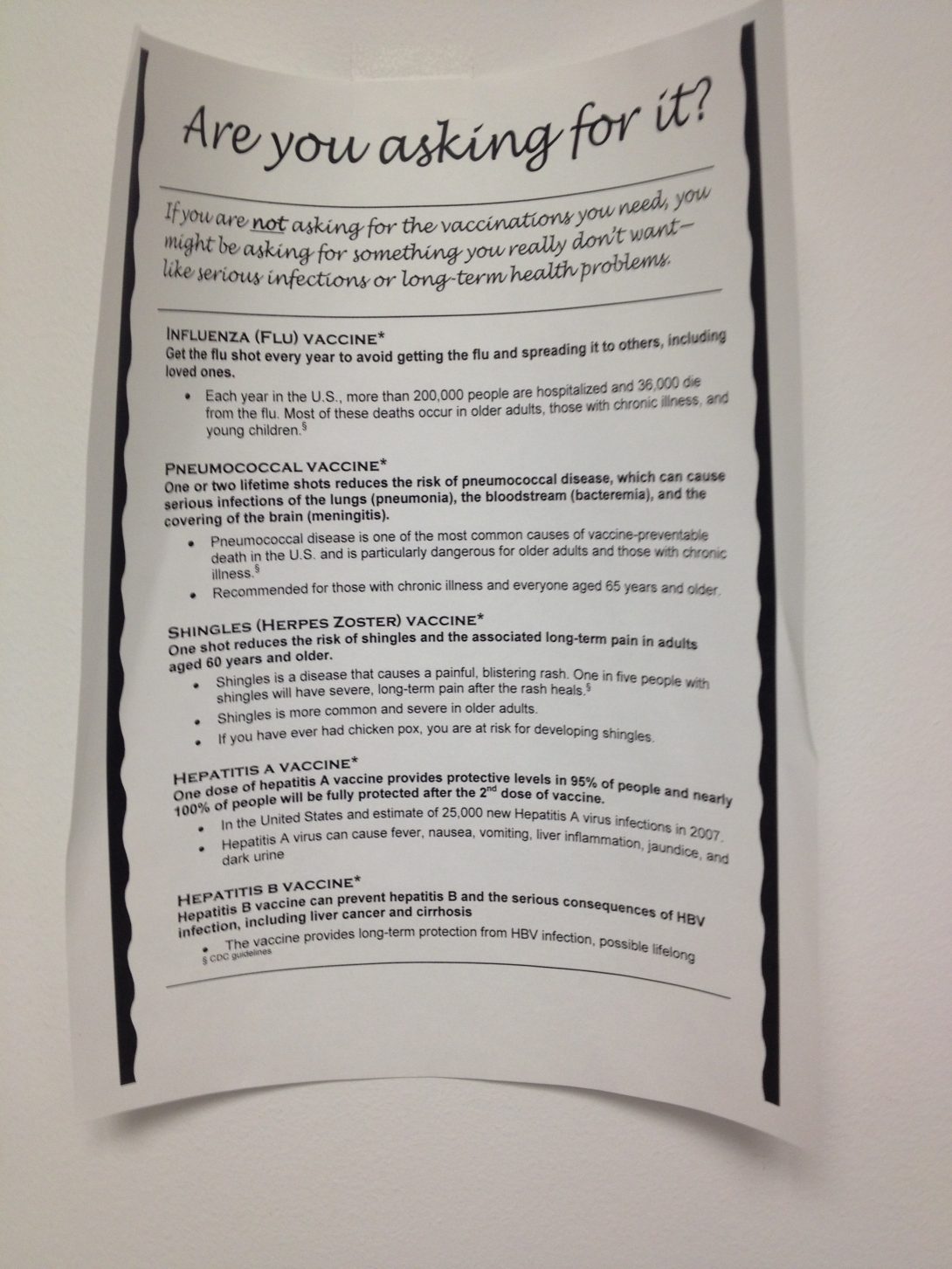
Image 14
Image 15
Image 15
Image 16

Image 16
Ryan Orda
Ryan Orda Blog
Ryan Orda Blog
First Day
posted Jul 10, 2014, 1:31 PM by Unknown user
To begin, my experience at the Orthopedic Clinic was a very brief but eventful first day. When we arrived at the clinic we were introduced to Dr. Chmell, who was constantly being bombarded with questions by med students. We proceeded to shadow Dr. Chmell as he saw patients and watch as new residents gave knee injections. We even had the opportunity in assisting in putting a knee brace on a patient (pictured below). The doctor’s office was always very busy and crowded, with doctors coming in and out to view X-rays and assess patients. In the hall, red and green flags hung outside each patient door. If a green flag was raised up, it meant the patient needed to be seen. If both green and red flags were raised, then the patient was in the process of being seen. Lastly, a raised red flag meant the patient had already been seen and was awaiting further assistance (such as putting on a knee brace). One important thing to take away from this experience is the importance of hand hygiene, as evident from the various signs hanging around the office reminding doctors to wash their hands and the hand sanitizer dispensers located in the halls.
Ryan Orda Blog

Surgery
posted Jul 10, 2014, 2:18 PM by Unknown user [ updated Aug 4, 2014, 4:15 PM ]
The first week of our clinical immersion has passed, and boy do I have a lot to share. I didn’t think I would have seen this much right away and in such a short period of time. On our second day, we were already changing into scrubs and observing surgery in the OR. One procedure that I found really interesting and also had a really good view of was the total knee replacement. I didn’t get any actual pictures in the OR, but this picture (below) from the company OrthAlign is pretty close to what I saw. The vendor from OrthAlign was actually in the OR as well, where he essentially walked the surgeons through which equipment to use. The surgeons wore body exhaust systems or “space suits” which include helmets with battery operated fans (also pictured below). After the operation, the vendor showed us how his device, KneeAlign, works. The device utilizes accelerometers for both tibal and femoral alignment.
Ryan Orda Blog

Surgery?
posted Jul 14, 2014, 2:59 PM by Unknown user [ updated Jul 17, 2014, 1:54 PM ]
“We operate on people, not X-Rays,” Dr. Chmell told a patient. He later elaborated to me, in some situations: X-Rays may not look bad, but the patient can be in extreme pain. In this case, surgery may be required. The situation may also be that the X-Ray looks bad, but the patient isn’t experiencing that much pain and is still manageable. The patient may then require a cast or more physical therapy. A shocking new statistic I found, was that one out of three knee replacement surgeries are completely unnecessary. In these cases, patients may be more susceptible to further complications that can occur during surgery.
Clinics
posted Jul 19, 2014, 2:53 PM by Unknown user [ updated Aug 4, 2014, 4:11 PM ]
Ryan Orda Blog

Image
Ryan Orda Blog

Image
Ryan Orda Blog

Ryan Orda Blog
Top Display (showing path of injection)
Ryan Orda Blog
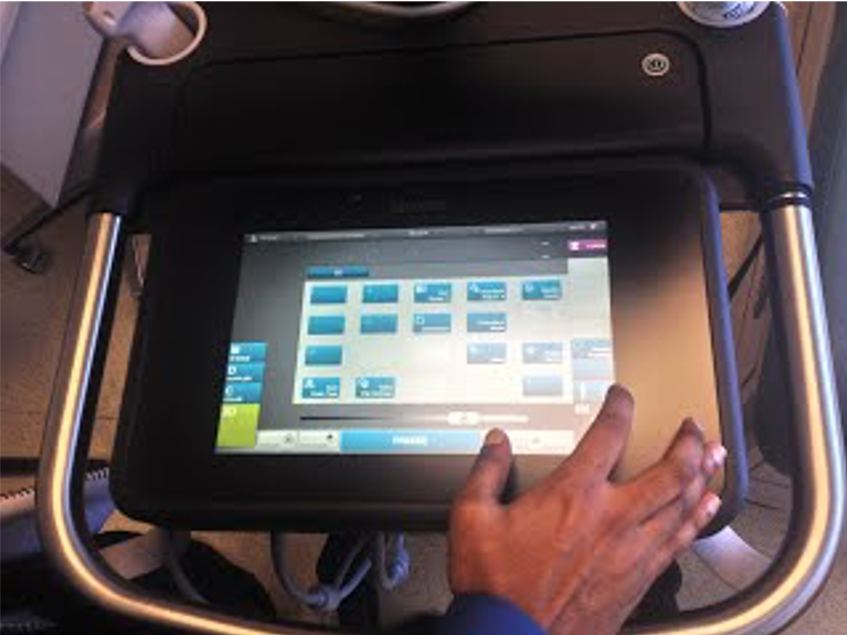
Bottom Display (user interface)
Ryan Orda Blog

Applied Medical Simsei Laparoscopic Training System with different size Trocars
Engineering
posted Jul 23, 2014, 7:42 PM by Unknown user
Yesterday we went back to Dr. Gonzalez’s clinic at the Illinois Bone & Joint Institute, where he gave us several presentations on his research and studies on hip and knee implants. A big concern when designing implants is wear. Cross linking decreases plastic deformations. A study determined large metal heads of hip implants caused corrosion. This led to research in switching from metal on metal joints to ceramic on metal. Another concern is sub-micron particles as a result of friction. Sub-micron particles, as opposed to micron particles, can be phagocytized by macrophages and cause osteolysis.
Today we returned to the U of I clinic. One problem I noticed was when the nurses would check which patient rooms were available. Nurses would get frustrated when the doctors forgot to either put the red/green flags back down or switch the “in use” sign to “available.” It seemed a little redundant to have the signs in addition to the flags, and this caused uncertainty to whether or not the rooms were available or not. Other times, a sling or documents would be left in the room and appeared the room was still in use.
Knee Revision
posted Jul 25, 2014, 12:13 PM by Unknown user
Ryan Orda Blog
On Thursday, we were back in the OR observing a knee revision surgery. The patient’s knee (pictured above) had gotten an infection and the implant needed to be replaced. This surgery is more complicated than a regular total knee replacement, since the implant that needs to be replaced has begun to grow into the bone. One complication to arise from this surgery was actually due to the vendor’s equipment. Smith & Nephew was the vendor and typically use the same trial spacers every time. These trial spacers are used in place of the actual spacer to test for sizing as necessary. The problem that occurred was that the trial spacers’ screw holes had been stripped due to prolonged use. Dr. Gonzalez got frustrated with this and made sure the vendor knew that by telling him that they need to have new ones next time and assure this does not happen again.
Ryan Orda Blog

Image
Ryan Orda Blog

Last Day
posted Jul 28, 2014, 5:17 PM by Unknown user
1) The University of Illinois Hospital is the only hospital in Chicago to accept public aid
2) Don’t give a patient a steroid injection if they have uncontrolled diabetes
3) The KneeAlign device works for tibial, but not femoral alignment (according to Dr. Gonzalez)
4) Orthopedic and Orthopaedic are both correct
First Day Again
posted Jul 31, 2014, 12:24 AM by Unknown user [ updated Jul 31, 2014, 12:29 AM ]
Ryan Orda Blog

Ryan Orda Blog

Ryan Orda Blog

Afraid to be Bored
posted Jul 31, 2014, 9:55 PM by Unknown user [ updated Jul 31, 2014, 10:16 PM ]
Ryan Orda Blog

Stem Cell Storage Tanks
Ryan Orda Blog
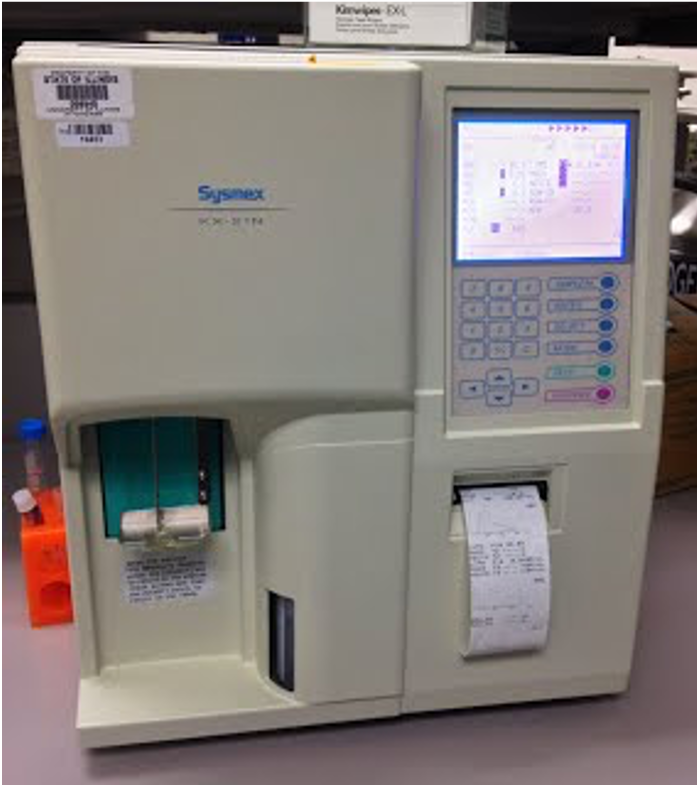
Automated Hematology Analyzer
Ryan Orda Blog

CD34 Reagent System
Ryan Orda Blog

Temperature Monitoring
After we visited the Stem Cell Lab, we returned to the clinic where we had the opportunity to observe a bone marrow aspiration and biopsy. I was surprised how quickly this procedure was and how it was all done in the patient room. The bone marrow kit used was from Hospital Service and is identical to the picture I included in my last post.
An alternative to the bone marrow kit used in the clinic is a “gun-shaped” device that takes care of the biopsy procedure in one shot. However, a few down sides to this device are its cost and noise, due to drilling. Dr. Rondelli brought up an interesting idea for a Bone Marrow Catheter. The device would need to be thin and flexible and could hypothetically transfer stem cells through the blood system.
Inpatient Center
posted Aug 6, 2014, 2:23 PM by Unknown user [ updated Aug 7, 2014, 6:44 PM ]
Ryan Orda Blog

Image
Ryan Orda Blog

Image
Ryan Orda Blog

Image
Ryan Orda Blog

Otoscopes hanging on wall
Ryan Orda Blog

Wall mounted vital machine & multiple outlets
Ryan Orda Blog

Transfusion machines
On Tuesday, we followed Dr. Rondelli as he held rounds at the Inpatient Center. The center is located on the eighth floor of the hospital. The entire floor was remodeled thanks to a $1.5 million donation. It is easily the nicest floor in the hospital with its hardwood floors and yellow painted walls. Dr. Rondelli hand picked pictures of various cities to be placed in each patient rooms. His favorite is the one pictured above, which features pictures from his home: Venice, Italy. Included in each patient room is a TV, computer, wireless keyboard, and webcam. Also, in each room is a fridge (the only hospital to include one). Dr. Rondelli believes patients should be as comfortable as possible in the hospital and still maintain connection with friends and family. There is even a bench that pulls out to be a bed for family members to stay overnight.
Several areas of possible improvement are the bathroom tubs could be changed to standing showers for easier patient access and X-Ray equipment could be mounted from the wall to take standing X-Rays.
Stem Cells
posted Aug 6, 2014, 11:03 PM by Unknown user [ updated Aug 7, 2014, 7:57 PM ]
Ryan Orda Blog

COBE Spectra Apheresis System
Ryan Orda Blog
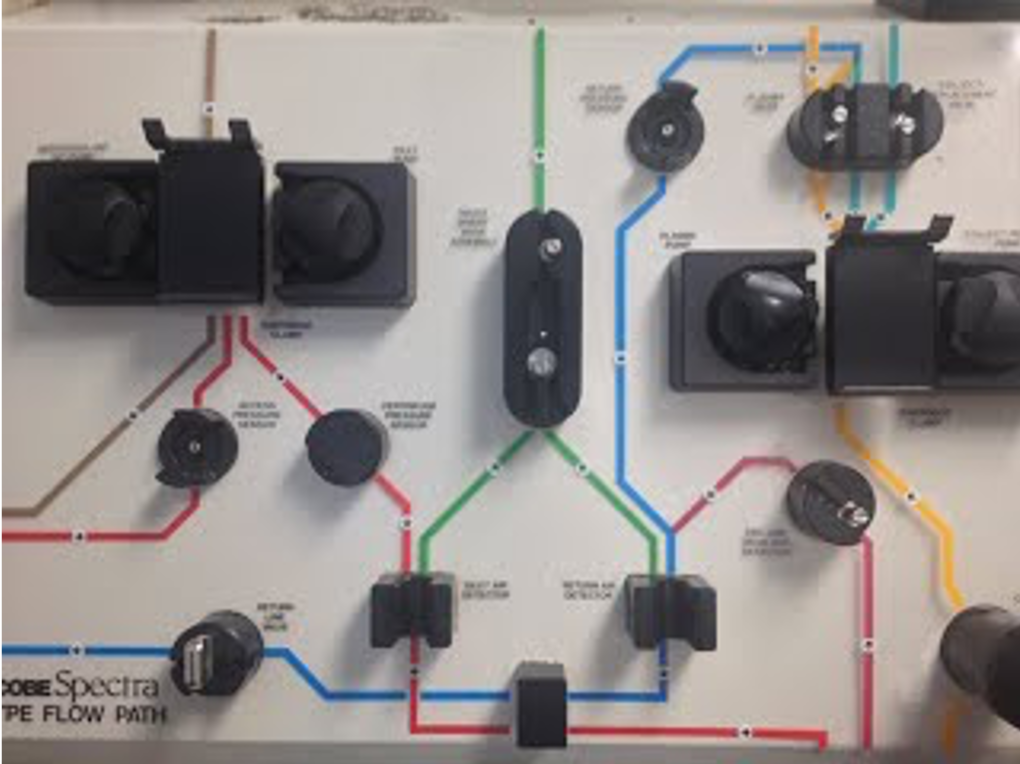
Flow path for COBE Spectra System
Ryan Orda Blog

Therakos CellEx Photopheresis System
Ryan Orda Blog

SCD 312 Sterile Tubing Welder
Radiation
posted Aug 7, 2014, 8:22 PM by Unknown user [ updated Aug 10, 2014, 5:54 PM ]
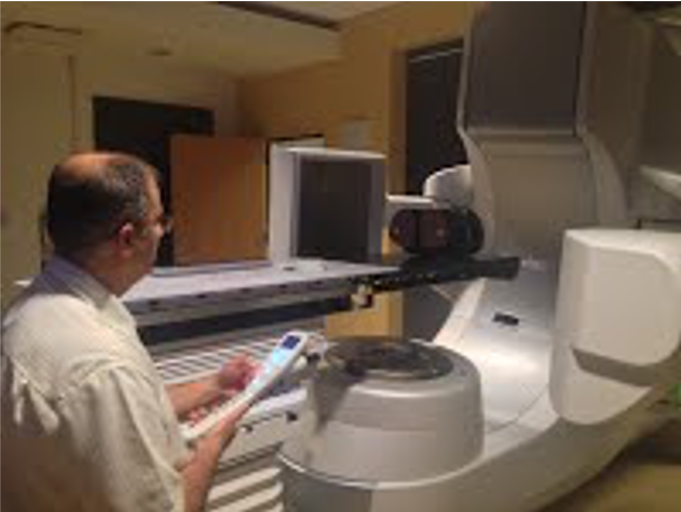
Ryan Orda Blog

Linear Accelerator
Ryan Orda Blog
Remote Control
Ryan Orda Blog

Console Control
Today we visited the Radiation Oncology department, where they use radiation therapy as a cancer treatment and to prevent tumor recurrence. The main device that is used is the linear accelerator. This machine uses electrons traveling nearly at the speed of light to kill cancer cells. The device is controlled from a console outside the room. The console includes camera control to see inside the X-Ray room. The machine moves precisely by entering in coordinate dimensions and automatically adjusting to the settings. A CT scan is initially taken by the device to acquire an image to determine a target setting. An individual plan is created for each patient, by studying their CT scan and movement of the tumor based on bodily movements. A margin is then created to account for that movement. Treatment can last from 5-6 weeks and 15-20 minutes a day. A mold is created to keep the patient in the same position each day and reduce error. When we talked to the radiologist about how he creates the patient’s plans he told us, “Words will confuse you, just look at the pictures.” It’s true that it is much easier to show someone how something needs to be done as opposed to telling them. The linear accelerator machine we saw was actually a new device (Varian TrueBeam STX costing approximately $4million) that was still being set up. Side effects of radiation therapy include nausea and complications that can arise from improper target alignment
End
posted Aug 15, 2014, 2:14 PM by Unknown user [ updated Aug 15, 2014, 11:06 PM ]
Ryan Orda Blog

Image
Ryan Orda Blog

The final week of our rotation saw the conclusion of the stem cell transplant procedure. We previously followed the technologists retrieve the bone marrow from the donor bank and then to the stem cell lab for the stem cells to be frozen. Which brings us to the final step of giving the new donor stem cells to the patient. The stem cells were brought up to the inpatient center from the lab, where they had to be defrosted to a “slushy” consistency before being given to the patient. The one side effect that patients experienced from the procedure was a sour taste left in their mouth. Some patients have worse experiences than others, and can cause nausea and vomiting in some cases. The nurses give the patients hard candy to help with this problem.
All in all, this clinical immersion experience has gone by incredibly fast and there is so much insight and knowledge I have gained from my time in both Orthopaedics and Hematology/Oncology. I want to thank Dr. Kotche and Prof. Sterling for giving me this opportunity; as well as Dr. Gonzalez, Dr. Rondelli, and all of the hospital staff for letting us observe them and teaching us all about medicine and how it incorporates engineering.
Nadia Crawley

Nadia Crawley
My name is Nadia Crawley. I am a senior Bioengineering student at the University of Illinois at Chicago, with a concentration in Cell & Tissue. I am an intern in the Bioengineering Clinical Immersion Program. I will use this blog to document my experiences while in the clinical environments: Transplant Surgery and Anesthesiology. This blog will help centralize my “raw data” and better help me analyze the dynamics of a clinical environment, and how the products and protocols of engineers impact the atmospheres in which they are implemented.
Nadia Crawley Blog
Nadia Crawley Blog
First Day July 7th, 2014
posted Jul 7, 2014, 4:33 PM by Unknown user [ updated Jul 7, 2014, 5:11 PM ]
Nadia Crawley Blog

Talk about immersion! No more than an hour into my first day, I found myself in scrubs and in the “middle of action” in the operating department of the University of Illinois Medical Center. The foot traffic was hectic, nurses were walking back and forth, the phone kept ringing off the hook, and the charge nurse seemed rather stressed. Soon I found myself walking into an operating room where two surgeons were reconstructing the arteries of a pancreas in preparation for surgery. I couldn’t believe what I was seeing! And to top it off, the lead surgeon seemed more than happy to explain what exactly he was doing, and even encouraged my partner and I to come behind and watch! Just when I thought my day couldn’t get any better my shadow doctor, Dr. Jeon, allowed my partner and I to come into his operating room where he was removing fluid from a patient. To witness the prep, incision, and operation of a patient in such close proximity was exciting, yet slightly nerve wracking as I was constantly moving to get out of the way. Nevertheless, I witnessed some pretty amazing things today.
Friday July 11th, 2014
posted Jul 13, 2014, 8:39 PM by Unknown user
At the end of the first week I was relieved and exhausted, but most importantly, I was excited for the coming week. I really didn’t know what to expect, but the experiences that I’ve had in just short days were incredible. I was able to see surgery, in which a HERO catheter was placed in a man’s arm. I also shadowed a doctor as she did her rounds in the Transplant Clinic. Most of my time last week was spent in the clinic, and while it was interesting to hear patient’s stories, it was also very sad. I wasn’t really prepared to hear of patient’s tumultuous health history, their struggles as they wait to be put on the “list”, a patient being notified he may have cancer, and the list goes on and on. Those type of encounters were pretty tough to hear, and it made me more aware of my own mortality. Many patients were diabetic and suffering from kidney failure. Many patients were on dialysis, and the toll it takes on the human body was exposed through each pair of enlarged veins I witnessed. It made me wonder, in what ways could the process be improved to not damage the human body in such a manner; or further more, in what ways can we develop practices in which we prevent the use of dialysis machines?
Week 2 Recap July 14th – July 18th, 2014
posted Jul 21, 2014, 6:48 AM by Unknown user
Some really great things happened this past week! First, I noticed that I felt more comfortable coming into this second week of Transplant Surgery. I knew my way around the hospital more, I had developed a nice relationship with the fellows, and I was really excited to see more surgery. On Monday, while there was no procedures going on to observe, I was able to play with the Da Vinci surgical robot! In a cold and sterile “large animal procedure room,” I experience, first hand, what it felt like to use a device as an extension of my own hands. It turned out that the device was quite easy to use. After speaking with Dr. Jeon, I grew to understand the benefits and disadvantages of the robot. While it is great to use on overweight patients, there are a few factors that could be improved. The arms could be a bit slimmer as to not bump in each other when multiple arms are being used. And the robot lacks tactile feedback. So there were times when I gripped the testing board too hard. Had that been human tissue or flesh, that could have been very painful. The only issue with designing improvements to the device, or any device for that matter, is patent laws. We learned, to the irritation of our doctor, that improvements or ideas are no longer based solely on the advancement of medicine and science, but business. And so the company that makes the Da Vinci robot and patented so much of the technology that they use, that it would almost impossible to design an improvement to the device without selling it to them. That was very interesting to hear.
Week 2 Concerns July 14th – July 18th, 2014
posted Jul 21, 2014, 6:54 AM by Unknown user
While some great things happened this past week, a few things concerned me. Our doctor was very much absent and non-responsive to us. When were attempting to locate him or figure out where to go next, we were pretty much left to our own devices. We took the initiative, at times, to speak with the residents and nurses. However, we were also aware that this is a busy running hospital with busy employees. So sometimes there wasn’t an opportunity to “bother” anyone at the moment. We did our best to quietly observe or shadow, but there was often downtime when were wondering what we should do or where we should go. We know it is not the responsibility of the nurses or residents to accommodate us, but we were shocked with the great distinction we discovered in our doctor from the first week to this one.
Pancreas Transplant July 22th – July 23rd
posted Jul 23, 2014, 10:58 AM by Unknown user [ updated Jul 23, 2014, 10:58 AM ]
Goodbye Transplant July 25th, 2014
posted Jul 27, 2014, 1:18 PM by Unknown user [ updated Jul 27, 2014, 1:19 PM ]
Nadia Crawley Blog

Nadia Crawley Blog

Image
Nadia Crawley Blog

Image
Nadia Crawley Blog

All in all, I really enjoyed my time in transplant. I feel I have obtained a better understanding of the clinical environment. I was able to identify common issues within the hospital, in terms of medical devices, that need further development. I gained a very strong sense of empathy for the patients that need these medical devices or procedures done. I also gained a sense of empathy for the users of the devices, such as the medical staff. I believe that I now have the first-hand knowledge and experience to explore better options, to explain was obstacles within a clinical environments, and the motivation to be apart of the advancement of medical practice. Although I will miss the Transplant unit deeply, I’m looking forward to see what lies ahead in Anesthesiology.
Anesthesiology!!! July 29th, 2014
posted Aug 3, 2014, 8:20 PM by Unknown user [ updated Aug 3, 2014, 8:37 PM ]
Can I just start off by saying that I love the anesthesiology department! Not only is this rotation much more organized; but our doctor is amazing and the number of engineering related applications in this department help me better conceptualize the true purpose of this program. On our second day, but first day in the OR, we saw two neuro cases: a brain tumor resection and deep brain stimulation for Parkinson’s disease.
Nadia Crawley Blog

fig. A
Nadia Crawley Blog

fig. B
Nadia Crawley Blog

fig. C
Nadia Crawley Blog

fig. A
The use of different medical devices in this single day proved to me to advantages of engineering concepts in the medical field. And it has already got the wheels in my brain turning of certain improvements. Little did I know the amount of work that went into an anesthesiologist’s job, nor how engineering intensive these operations are. But I’m excited for the rest of this rotation.
What do Anesthesiologists Want
posted Aug 3, 2014, 8:56 PM by Unknown user
My first week of Anesthesiology has been absolutely amazing. I’ve seen multiple neuro cases, lumbar back cases, robotic gastric bypass, laryngectomy cases, and the list goes on and on. I’ve gotten so used to the procedures that seeing blood and guts doesn’t even phase me anymore. I find myself asking soon afterwards, “So when’s lunch?” But although each case may be completely different, with different body parts and surgeons and complications; there are a few universal problems that I’ve found in all operating rooms.
Nadia Crawley Blog

Interventional Radiology (IR)
posted Aug 24, 2014, 5:22 PM by Unknown user
I really enjoyed going to the IR department. I must admit I was a bit biased, because my mother is an IR nurse. So I was very intrigued to finally the devices and procedures I heard her speak of so often. On this particular day I witnessed a biliary tube exchange. A man suffering from cancer of the bile duct had to come in every 6-8 weeks to have the tubes in the bile duct replaced. The tubes hung outside of his body, on the side of his abdomen. After so long, the tubes become obstructed due to the thickness of the bile, which causes build up. The procedure was very straight forward. Guide wires were placed inside the old tubes as place holders. The old tubes were removed and the new tubes were inserted where guide wires were. The procedure took all of thirty minutes. But I wondered if there was a way to prolong the life of the tubes a bit longer than just the 6-8 weeks. I thought of different tubing material or a better porting system to drain the bile, but keep the tubes intact. But there already seemed to be a plethora of devices in the IR department. In fact, it resembled a grocery store in the main hall. I noticed tons of catheter systems and tubing from Abbott, Boston Scientific, Kimberly-Clark, Cook Medical, etc. The number of different medical device manufactures in the department was astonishing. I did not have nearly enough time to try and distinguish between the multiple devices to determine their difference. Nonetheless, it seemed each tool had a purpose and was there for a reason.
Blog Posts and Saving Lives…
posted Aug 24, 2014, 4:46 PM by Unknown user
My immersion in the Anesthesiology department really made me think of how I budget my own time and priorities. I seemed to really struggle with updating my blog regularly. I always felt that by the time I got home from a long work day and an even longer commute, that I was way too tired to write a blog post. I would push the blog to the next day, then the next day, and then before I knew it…it was Sunday night. I must admit, initially I felt quite justified in my excuse for not completing my required posts. But I soon became rather disgusted with myself for two reasons.
Saying Goodbye to Anesthesiology
posted Aug 24, 2014, 5:50 PM by Unknown user
I loved this department. I truly enjoyed Dr. Edelman, the entire department, and the awesome people we got to meet along the way. What I took away from shadowing the anesthesiologists was sheer respect for what they do. Their job far exceeds what I ever thought. They hold one of the most important positions in the hospital. They allow for surgery to take place. They assess a patient’s status to determine what drugs are appropriate. They alleviate pain. They consult the patient before and after surgery. They serve as doctors, confidants, and therapists. And though they carry so much responsibility, their working situations are less than ideal. While their technology is advanced, they still lack many advancements, namely wireless connections, which could really alleviate the stress of their jobs. However, even with all of the stress, the staff still welcomed us with open arms and were happy to teach.
Martin Strama

Martin Strama
In my opinion, a bioengineer advances human health by producing medical breakthroughs that improve the quality of human life. Originally, I thought that bioengineers need only to balance their knowledge of engineering, human anatomy and the life sciences to produce and maintain systems and equipment used to assist health-care professionals. However, humans are complex, dynamic systems in themselves, and are often omitted from the center of the story when converting medical need into demand.
Being accepted into the UIC Bioengineering Clinical Immersion Program, I will be able to learn from the lives of patients by spending six weeks immersed in the clinical environments at the University of Illinois Medical Center. Therefore, this blog will serve as a detailed account of my experiences within the program in an attempt to document the actual experiences of people as they improvise through their daily lives in a clinical environment. I will begin my immersion at the Ophthalmology department. After three weeks, I will rotate into the Anesthesiology department for the remainder of the program.
Martin Strama Blog
Martin Strama Blog
Uncharted Territory
posted Jul 9, 2014, 9:11 PM by Unknown user [ updated Aug 1, 2014, 5:14 PM ]
Observations
To grow and prosper as a bioengineer, I decided to completely get outside of my natural engineering mindset and see the world through the eyes of the patients coming to the Illinois Eye and Ear Infirmary from the very beginning. What I soon came to realize was that solving differential equations seemed to be easier than watching what patients don’t do, and listening to what they don’t say.
After entering the building and taking the elevator to the third floor, I encountered rows of chairs inhabited by patients and medical technicians running about. As I stepped out of the elevator, I soon learned that I was in the wild. The air was stuffy, the lighting was bright, and there was no clear sign to direct patient flow. After turning my head left and right a couple of times to decide where I should go, I noticed that by the ceiling hung a dark sign with white letters that read “Reception.” Approaching the reception area, I noticed numerous documents taped on the sliding panels above the counter. The patients neglected the taped documents and instead went directly to the desk receptionist. I then spotted another sign attached to the far left wall that gave directions to the different services located on this floor. A typical patient with visual problems would not have been able to read such a sign from the elevator area. Above the sign, on the ceiling, hung another sign indicating the service that is provided in this area. Apparently, dark signs with white letters are the basic template in this building. Luckily, the sign read “Cornea,” the service I was looking for. The Cornea Service houses Dr. Joel Sugar, a renowned Cornea specialist who has received numerous of awards including “Best Doctors in America.” Dr. Sugar is to serve as my clinical mentor during my rotation in the Ophthalmology department. After brief introductions and a tour of the department, Dr. Sugar assigned me to the Oculoplastics & Reconstructive Surgery Service under Dr. Pete Setabutr for the morning, and to the Glaucoma Service in the afternoon under Dr. Ketki Soin.
Although I was fortunate enough to observe two completely different services, both have similar patient-centered approaches. Ocuplastics did not have a dedicated waiting room for the patients, and as a result, the patients would stand in the halls and block traffic. Patient check-in and check-out occurred over the same counter, so patients who are checking out have to wait until new patients are done checking in. Furthermore, the counter was dirty, cluttered and contained unnecessary medical equipment such as gloves. Similar observations were seen in Glaucoma with the exception that this service provided a waiting area, or at least chairs that formed rows to resemble a waiting area. In the waiting area hung a muted HDTV that caught the eye of none of the patients. Most of the patients were on their cellphones or tablet devices playing games. There were no accessible outlets for the patients to charge their devices after waiting 1-2 hours to see a doctor. Attached to some of the walls were magazine racks that were untouched by the patients. There was no vibrant colors to brighten the room either.
In the patient rooms, desks were cluttered with unnecessary diagrams/objects, leftover medication bottles/droplets, disorganized paperwork, and bulky equipment. The doctor barely had a place to do paperwork. Meanwhile, cables from the equipment were exposed and scattered all across the floor. Walls were chipped, scratched and dirty. In addition, meaningless screensavers about the new UIC Medical Logo were being displayed to the patient in the background. Furthermore, the windows always had their blinds down and made the patient feel like he/she was in prison. While sitting in the patient chair, the patient keeps to himself/herself as tightly as possible, and holds onto personal items because there is no place to put them besides on the floor next to the chair. The patient chair is relatively close to the doctor’s chair, but additional chairs for family and friends are located far off into the distance. In a sense, the patient was isolated from loved ones and was left to face the doctor by themselves. When explaining a condition to a patient, the doctor uses multiple hand gestures to convey their point across to the patient. The patient usually does not comprehend the doctor until the third iteration. After the patient understands what the doctor has said, the patient is left to wonder in silence with any questions he/she may have because the doctor is filling out paperwork. Non-English patients rely on relatives to adequately translate between the doctor and themselves. During initial measurements, the doctor loads the patient’s medical history over the internet and displays it on the monitor. The software utilized in not coherent and relies on additional programs to open up image files that take time to load. While the doctor is looking for the desired files, silence fills the room. Hence, the information flow and exchange between patient and doctor is insufficient, and varies from service to service.
Soon the clock struck 5 PM, and it was time to regroup with Dr. Sugar. This immersion experience is going to be harder than I thought. Suddenly I am missing equations. However, I did get to review ocular anatomy in vivo using a Slit Lamp! At the end of the day I realized that no matter what patient room I entered, two basic and critical medical instruments were always waiting to be utilized: the Phoropter and Slit Lamp / Biomicroscopy.
Equipment
- Phoropter – an instrument that contains various lenses to determine the refraction of the eye during vision testing and prescribe eyeglass lenses. Cons: easy to dislodge from place, manually set -> easy to forget to change lens settings, patient can’t recall previous options when lenses are switched, hard to record lens numbers in dark.
- Slit Lamp – a thin sheet of light is illuminated into the eye from a high-intensity light source. Cons: handheld lenses are utilized to examine the retina, huge learning curve, head and chin rest need to be constantly sterilized from patient to patient, pressure sensor stick out to the side.
Barriers
- Floor Layout – The layout of the patient rooms are tight and next to each other, the location and size of the waiting areas vary considerably from service to service, reception desks are detached from service of interest, and their is no clear signals to direct patients sufficiently.
- Communication / Information Flow / Patient History
- Interior design / décor
- Privacy
Connect the Dots
posted Jul 11, 2014, 8:46 PM by Unknown user [ updated Aug 1, 2014, 5:14 PM ]
Emotional Connections
On Wednesday, I had the privilege to observe Dr. Sugar in Cornea for my morning shift. I knew he was good, but I just didn’t expect him to be flawless. Dr. Sugar approached patients with respect and conversed with them before engaging into business. In essence, Dr. Sugar was inviting patients into his home. At the front door, Dr. Sugar personally greeted the patients, guided them down a narrow corridor, into his room, and seated the patient. The patients did not feel lost or misplaced, but comfortable, relaxed, and human. Then it hit me, Dr. Sugar never forgot that he, himself, is also human. He was modest and humble when patients complemented him and his abilities. He did not let his status define him. Instead, his hospitality and actions made him memorable to his patients. Such qualities create loyal patients coming back to see him, even one who had received a Castroviejo square corneal graft back in the 1950’s, a rare graft that I had got to see first-hand. Just as friends shake hands before saying good-bye, Dr. Sugar walks the patient out of his house after every visit. Not once did a patient leave him without a smile on their face. Dr. Sugar did not learn this behavior from any textbook, but from his personal experiences. Dr. Sugar treats patients, and in turn, the patients teach him. Such a connection is priceless. Initially, I thought I would just be observing Dr. Sugar as he evaluated his patients. I was dead wrong. Dr. Sugar immersed me into the process by allowing me to view patients through the teaching scope of the slit lamp. Furthermore, Dr. Sugar did not tell me what ailment was bestowed on a given patient. Instead, he gave me clues from the observations I saw through the teaching scope and made me put the pieces together. He genuinely wanted me to learn, and I couldn’t have been more grateful. I mean to be in the presence of Dr. Sugar is one thing, but to be personally taught by him is like meeting a celebrity and getting their autograph.
In the afternoon, I was taken in by Dr. Azar in Pediatric Ophthalmology & Adult Service. Dr. Azar exposed me to a world of muscles located around the eye. I learned about various cases that fall under strabismus such as esotropia and exotropia. Like Dr. Sugar, Dr. Azar engaged with the patients before proceeding with examinations and after, and that makes all the difference.
Overall, Wednesday was an amazing day. I got to observe the mental state of patients in a completely different perspective, a perspective based on personal care.
On Thursday, I also got to observe patients in a different perspective, a perspective based on extreme care.
(To be continued… Surgical Connections)
Surgical Connections
posted Jul 13, 2014, 7:23 PM by Unknown user [ updated Jul 13, 2014, 8:08 PM ]
The operating room, the OR, or the panic room is a daunting place for anyone who has never set foot in the place. As I entered the main OR entrance, I noticed that everyone had hair nets on, foot slippers, and scrubs. It was like being inside an ant hill, except the ants were trained OR personnel. Each person had their own job, was rushing about, and seemed overworked. Before entering the OR, I had to put a mouth mask on for sterilization purposes. I looked great! Entering the OR room, I encountered the main staff: a circulating nurse, an anesthesiologist, and a surgical technician. This trio was prepping the room for the upcoming operation to music played from an iHome docking station. Each person had their own corner workstation in a sense. The room seemed cluttered with equipment and loose, unlabeled cables/tubes. The surgical technician sterilizes the room by placing sterile, blue sheets onto medical equipment and instrument trays. These areas are considered sterile and cannot be touched by unauthorized personnel. The surgical technician told me that everything used in the operation is labeled with a pre-printed label prior to the operation. If a label is missing, the technician must hand-write a label with a marker that can smudge. Also, the technician and nurse must exchange verbal confirmations before exchanging fluids/medication between each other. The technician also mentioned that the chairs utilized by the doctors are uncomfortable. After sterilizing the room, the patient was wheeled in on a stretcher and placed in the center of the room. Upon entry, the patient was exposed to bright lights and a chaotic atmosphere. When positioned in the center of the room, everyone cluttered around the patient. I was beginning to feel claustrophobic for the patient. In addition, the patient was not put to sleep and was able to communicate with the doctors and personnel. The team performed a quick verbal debrief before starting the operation. The patient’s file was placed beneath the patient’s feet on the stretcher. There was no dedicated place for personal items or desk space for paperwork. I observed Dr. Tu, a cornea specialist, perform multiple cataract surgeries and corneal transplants. Observing the beginning, middle, and ending of these surgeries was a great experience. I saw how the donor corneas were packaged, extracted, and modified for the patients. While trying to find weak points in these surgeries, I could not. These surgeries were so elegantly performed and averaged half an hour. I asked Dr. Sugar if he knew of any weak points, or places that can be improved upon. Dr. Sugar told me that there is no standard protocol/procedure for these operations. It was up to the doctor to use whichever technique he pleased. Furthermore, Dr. Sugar told me that the standards for these operations would be changing soon to techniques that are currently used in Europe. Currently, an aspirator and image inverting microscope with two teaching scopes are the two main instruments used by the doctor to perform the surgical procedures. The aspirator contains several functions that sculpt and irrigate the eye during the operation. Dr. Sugar said that the current medical equipment utilized are outdated, but do not constrain the operations in any significant way. New instruments utilize a cloud-like service that allow the doctors to prep for the operation in their offices beforehand. The doctor must be comfortable using two feet pedals at the same time to operate these machines while performing the operation. I got to operate the foot pedal for the inverting microscope, and it was extremely difficult. Dr. Sugar pointed out that most doctors wear only socks to operate the foot pedal because they need the freedom of motion. The skill needed to be comfortable using these foot pedals while operating is unbelievable. Aside, I was astonished to see how steady the doctor’s hands were when performing these operations. In addition, there was no place for the doctor’s hands to rest. Furthermore, the patient’s chest was utilized to hold medical sponges and forceps. Also, folded sheets were used to comfort the patient’s neck. In addition, a holding sac was creating by the side of the patients head to hold the liquid oozing out of the patient’s eye. After the operation, the patient was comforted and taken away into the ant hill. The OR was then turned over for the next patient, and the process repeated. After four operations, I could only image how tired Dr. Tu’s arms were. I definitely enjoyed the thrill and rush of being in the OR.
Furthermore, on Friday I got to shadow Dr. Shorter in Contact Lenses and Dr. Chau in Retina. In Contact Lenses, I learned that the PROSE contact lenses are like a six month long surgery. The patients need to constantly make appointments to come back and refit/reshape their contact lenses for comfort or for more refractive power. In Retina, an indirect ophthalmoscope is used in conjunction with magnifying lens to view the retina. Another machine emits ultrasound wavelengths from a probe onto the patient’s eyelid. This instrument is non-invasive, provides high resolution pictures and videos of the retina. In addition, optical coherence tomography (OCT) is another method used to get the cross-section of the retina to view gross cell layers. Both of these services utilize drops to treat the patients. Patients primarily identify their medication using the cap color of the bottle if they do not recall the name of their medication. Patients are also asked the same questions by the nurse and doctor regarding their medical history. This redundancy allows the patient to extend his/her responses, but may not always be to the doctor. When interviewing the patients, the doctor asks the patient for personal contact information to update their records so that the patient can receive messages from the doctor’s office. The patient could be updating their personal information/medical history while waiting for the doctor in the waiting room instead of sitting idly by doing nothing productive. I underestimated how much a barrier information flow is in a clinical setting.
All in all, an awesome, eventful week. I am looking forward to learning more in the coming two weeks!
Fire the Laser!
posted Jul 16, 2014, 7:41 PM by Unknown user [ updated Aug 1, 2014, 5:13 PM ]
Towards the middle of the week I observed several retinal detachment and vitrectomy procedures performed by Dr. Lim. These procedures utilized a more complex aspirator/visual system that powered a laser to patch the retina. The system was color-coded in order to correctly attach various tubes to the machine. In addition, the machine verbally confirmed any modifications performed by the surgical technician. Furthermore, these operations came with their own tray that contained the necessary instruments for the procedure. The tray also included the labels for the instruments and provided the technician with an overview of the required instruments/medication for the operation. Dr. Sugar mentioned that some of the microscopes contain a light source defect that only supply 20% of the light from the source to a head. Ideally, all three of the microscope heads would have full illumination and stereopsis/depth perception in case the doctor required additional help during surgery. In addition, Dr. Dela Cruz demonstrated a laser surgery using a LenSx Laser System. The system was the first femtosecond laser cleared for cataract surgery. Essentially, the doctor creates a template on a monitor, follows a series of steps to modify settings and ensure safety, and clicks a button. The laser makes the desired incisions, and the doctor aspirates the left-overs. The technology is so advanced that the hospital actually loses money when using the machine on most patients (approx. $300 per use of the docking station and $50,000 per contract)! On the bright side, the surgery time is drastically shortened. I love to see bioengineering at work! I just wish it could be more affordable to the general public.
Second Week Down
posted Jul 18, 2014, 2:55 PM by Unknown user
A Balancing Act
posted Jul 23, 2014, 6:17 PM by Unknown user [ updated Aug 1, 2014, 5:12 PM ]
Patients are verbally summoned and guided from the waiting area to a patient room by a technician/resident. During the trip, the technician communicates with the patient on a personal level in order to provide a sense of comfort to the patient. The patient is then guided into an illuminated room. Upon entry, a patient always encounters a chair that is located towards the end of the room. Attached to the chair are the phoropter and slip lamp. These two instruments are relatively large and can be intimidating to children and adults alike. When not in use, these instruments hover to the side and often get in the doctor’s way during visual examinations. The chair also contains a foot pedal that repositions the patient to a comfortable level prior to using the phoropter or slit lamp. The foot pedal is often mistakenly utilized by the patients before sitting down. When the patient takes a seat, they look right and left for a place to put their personal belongings. Often the patients put their personal belongings on the floor, in their lap, on the phoropter arm, or on a chair located on the other side of the room. Furthermore, patients often have to get up and walk over to their personal belongings to get their glasses, medications, or documents. Rising from the patient chair and walking across the room may seem like a trivial task but it can be dangerous given the design of the patient chair. The patient chair contains a foot holder, which many patients forget about when standing up. As a result, many patients seem to “slip” off the foot rest.
The whole introductory process could be streamlined with technology to better manage traffic flow, but would such technology be necessary? For instance, at Panera Bread, a buzzer is given to a customer after placing an order. The patient then finds an available seat in the “waiting area.” Next, the buzzer goes off when the food is ready to be picked up. This type of system can be easily implemented into the hospital setting, but instead of the buzzer going off, the buzzer would indicate to the patient that they are ready to be seen and could direct the patient to their room by displaying a room number. If such a system were to be implemented, personal interaction between patient and technician/doctor would be delayed. As a result, the patient could feel isolated, nervous, or even scared. In contrast, the technician/doctor could utilize the additional time to better acquaint themselves with the patient file to better communicate with the patient.
After the patient is seated, the technician/doctor goes over their medical history. The patient file is either in electronic or paper format. Electronic medical records (EMR) are convenient for accessing a patient’s medical history, but lack flexibility in regards to data/figure entry. In contrast, paper records are convenient for data/figure entry, but lack the ability to view the patient’s entire medical history. Furthermore, both methods take time for the technician/doctor. Usually the technician/doctor asks a patient a question and writes/types the response. During this time, the technician/doctor has their back to the patient and silence fills the room. Instead of waiting until the technician/doctor sees the patient to ask basic questions regarding their medical history, patients should be proactive in the waiting room. Patients could be handed a tablet containing forms/documents that help gather necessary data regarding their personal and medical history. The data could then be instantly linked to the technician/doctor at their office to review before visiting the patient. This would give the technician/doctor an opportunity to personalize patient care beforehand. Furthermore, the technician/doctor could then directly communicate with the patient right off the bat. Patients prefer to see the technician’s/doctor’s eyes instead of their backs. Thus, technicians/doctors could be equipped with tablets to record examination results, etc. while keeping their faces visible to their patients. Since tablets allow the use of a pen, technicians/doctors do not need a keyboard and can “write” their notes directly into electronic format. Again, the question arises whether such technology is needed?
I feel as doctors try to maintain a balance between technology and personal contact with patients. Many of the instruments utilized by ophthalmologists call for patient cooperation and patient contact such as light torches and loose lenses. However, such instruments require manual operation. As a result, the doctor’s hands often get tired. Nevertheless, patients are engaged in their examinations and are not just visitors.
This post was mainly to address the balance between technology and personal care in regards to servicing a patient. My next post will try to be more geared towards observations relating to pathologies/conditions.
Variables
posted Jul 25, 2014, 2:36 PM by Unknown user [ updated Aug 1, 2014, 5:12 PM ]
In a sense, doctors function as MISO (multiple input, single output) control systems. For a given patient, the doctor must extract vital information and piece the inputs together in order to form a coherent diagnosis. The information can be obtained verbally from a patient, electronically via EMRs, or physically from several different examinations. Patients are not alike, and so, the inputs vary from patient to patient. As a result, the constraints differ from patient to patient too. Furthermore, a trial-and-error process in often taken to refine the diagnosis, similar to a negative feedback loop. The process a doctor undertakes is almost analogous to the process an engineer takes when solving a problem. However, doctors can’t change their inputs while engineers can’t change their constraints.
In addition, disturbances are dispersed throughout the system. One prominent disturbance is scheduling. Typically, the front desk schedules 50 consultations for a given day. However, the doctor can usually handle 35 consultations. Of the 50 scheduled consultations, approximately only 25 actually show up. Doctors have no control over such disturbances. If a patient does not show up, the doctor stands idle. Another prominent disturbance is language. A large portion of the patient clientele is Hispanic and speak Spanish. If the doctor doesn’t speak the patient’s native language, the doctor tries to overcome this disturbance by seeking the help of office employees who do. A translator hotline service is available, but doctors prefer in-person translations. The in-person translations allow the doctor to display hand and facial gestures to the patients while speaking to the translator. Thus, the patient observes the doctor’s gestures while listening to the translator.
Medical instruments/equipment pose another disturbance for doctors. Doctors operate the phoropter and slit lamp in the dark or very dim light. Doctors must read and interpret the data from these instruments in the dark. A majority of the equipment is loose and hand-held. While performing retinoscopy, doctors manually maneuver a light torch horizontally and vertically. In addition, doctors must be familiar with many different instruments that cross different specialties. Children pose another disturbance for doctors. When observing children in pediatrics, a majority of children are uncooperative. To overcome this disturbance, the doctor asks the child’s mom/dad to sit in the chair with them and constrain them. Children get bored easily and have short attention spans. As a result, performing thorough eye examinations is very difficult. In addition, checking a child’s eye pressure is nearly impossible. Children who receive drops become scared of the doctor and environment. In essence, the child becomes emotionally disturbed. In such cases, the disturbances disrupt the system entirely.
Today wraps up my rotation in the Ophthalmology department. I can’t believe it’s already the third week. Time is flying! I learned so much about eye care, anatomy, and the medical instruments currently utilized by the doctors to keep vision alive. This has been a rewarding experience. I am definitely looking forward to my next rotation in Anesthesiology!
Wires and the Concept of Breathing
posted Jul 30, 2014, 6:03 PM by Unknown user [ updated Aug 8, 2014, 3:59 PM ]
This week I began my exciting adventure in Anesthesiology under Dr. Edelman. When I first met Dr. Edelman, I could immediately tell that he was going to be a great mentor from his Squidward sticker ID badge. Dr. Edelman stated that no individual really knows what anesthesiology is because no one has completely identified the chemical pathways triggered by anesthetics. As a result, there is no standard protocol for anesthesiologists. Instead, there are suggestive studies that indicate ranges of anesthetics for given operations. Thus, each patient receives individualized care based on their medical background. In essence, anesthesiologists are the jack of all trades. There are neural anesthesiologists, cardio, ophtho, etc. Each area requires specialization and has their own constraints regarding anesthetics. Right off the bat I was immersed into two highly specialized neurosurgical procedures: a craniectomy involving the removal of a brain tumor in the pineal body (the center of the head) and a deep brain stimulation (DBS) operation to treat Parkinson’s. In the craniectomy operation, Dr. Edelman explained that the patient was put under local anesthesia as opposed to inhaled anesthesia so that the intraoperative neurophysiological monitoring technician could acquire meaningful invoked signals. These technicians monitor the neural integrity of sensory and motor functions. This is another example of how an anesthesiologist must consider all aspects of a given operation, from the staff to the actual procedure. It definitely feels like the weight of the world is on their shoulders at the beginning of any operation. To make matters worse, the patient was oriented in a sitting position. When under anesthetics, positioning of the patient is a critical consideration. Since the brainstem goes to sleep, a patient loses hemodynamic abilities resulting in lower blood pressure. Thus, a war wages on to keep blood pressure up to normal ranges. In addition, nerves need to be padded and tissues need to be relaxed. All the things sentient humans take for granted are what anesthesiologists need to monitor/regulate.
When a patient enters the OR room, the anesthesiology team springs into action. They attach a pulse oximeter to a finger to monitor oxygen concentration; a blood pressure cuff on the bicep to monitor blood pressure; electrodes on the chest to monitor heart rate (EKG), an endotracheal tube via CCD video endoscope to allow respiratory functions and monitor CO2, and a bispectral index (BIS) strip on the forehead to monitor neural activity (analyzes an EEG and EMG signal and returns a number). The electrodes are oriented across the chest and transversely across the body. The CCD cable serves as a guidewire for the endotracheal tube and is utilized for patients with stiff necks or for patients with spine injuries. The cable is equipped with an oxygen port to blast away barriers and a camera that produces colored video onto a monitor. The anesthesiologist slips the tube onto the cable and tapes the end of the tube onto the cable. The anesthesiologist then proceeds to navigate the cable into the trachea via handheld controller by looking at a monitor. The CCD allows the anesthesiologist to look around corners. Once the cable has reached the desired position, as indicated by the markings on the cable, the anesthesiologist detaches the tube and manually shoves the tube along the cable. The BIS strip is based on an imperfect science where a number between 40-60 is usually accepted as indicating that a patient is under general anesthesia. In more fragile cases, real-time blood pressure monitoring is utilized via IV catheter. Thus, the anesthesiologist does not have to wait for the blood pressure cuff. To insert the IV catheter, the anesthesiologist has to locate a radial artery by palpating the artery. In essence, the anesthesiologist is blindly poking around until blood leaks.
Each sensor is attached via cable to a machine with analyzers for the various physiological parameters. One popular machine located in many of the ORs is the Dragus-Fabius Tiro. In addition, the machine contains ventilators and vaporizers. The monitors on the machine are touch-sensitive. In addition, the machine can be programmed to emit audible alerts for a given physiological variable. Thus, during the operation the anesthesiologist does not have to look at the screen to know which parameter needs attention because the alerts can be customized to emit different sounds. Based on the sound heard, the anesthesiologist knows which parameter needs attention.
Given the amount of physiological parameters an anesthesiologist needs to monitor, one could guess that a lot of cables are involved. Indeed, a labyrinth of cables is formed on the floor. Everyone in the OR needs to watch their step at all times and navigate their way through this complex labyrinth. One would think that these connections would be wireless in this day of age given wi-fi, Bluetooth, or IR technology. I must say, the labyrinth is quite deadly.
Martin Strama Blog
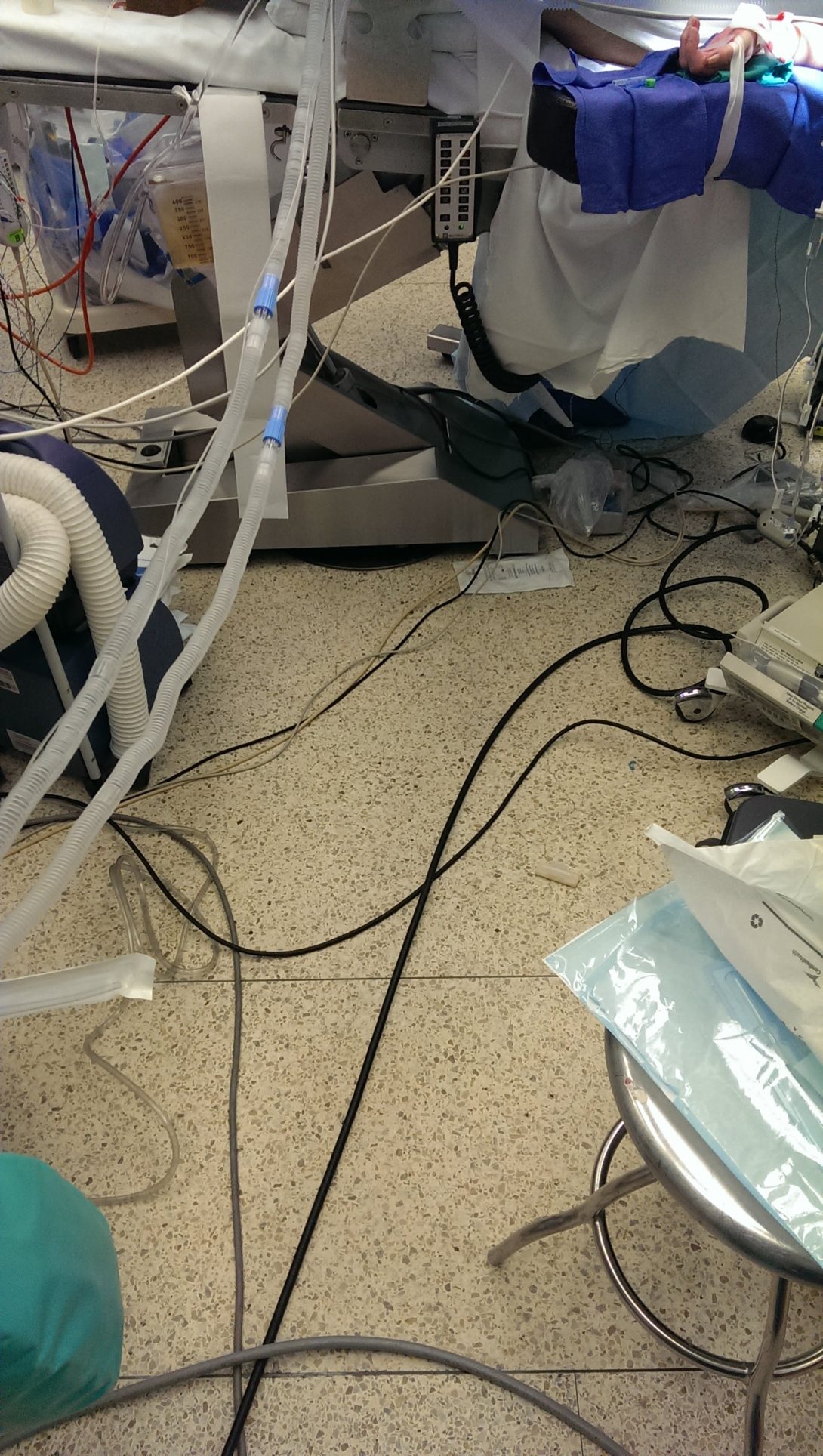
Image
Martin Strama Blog
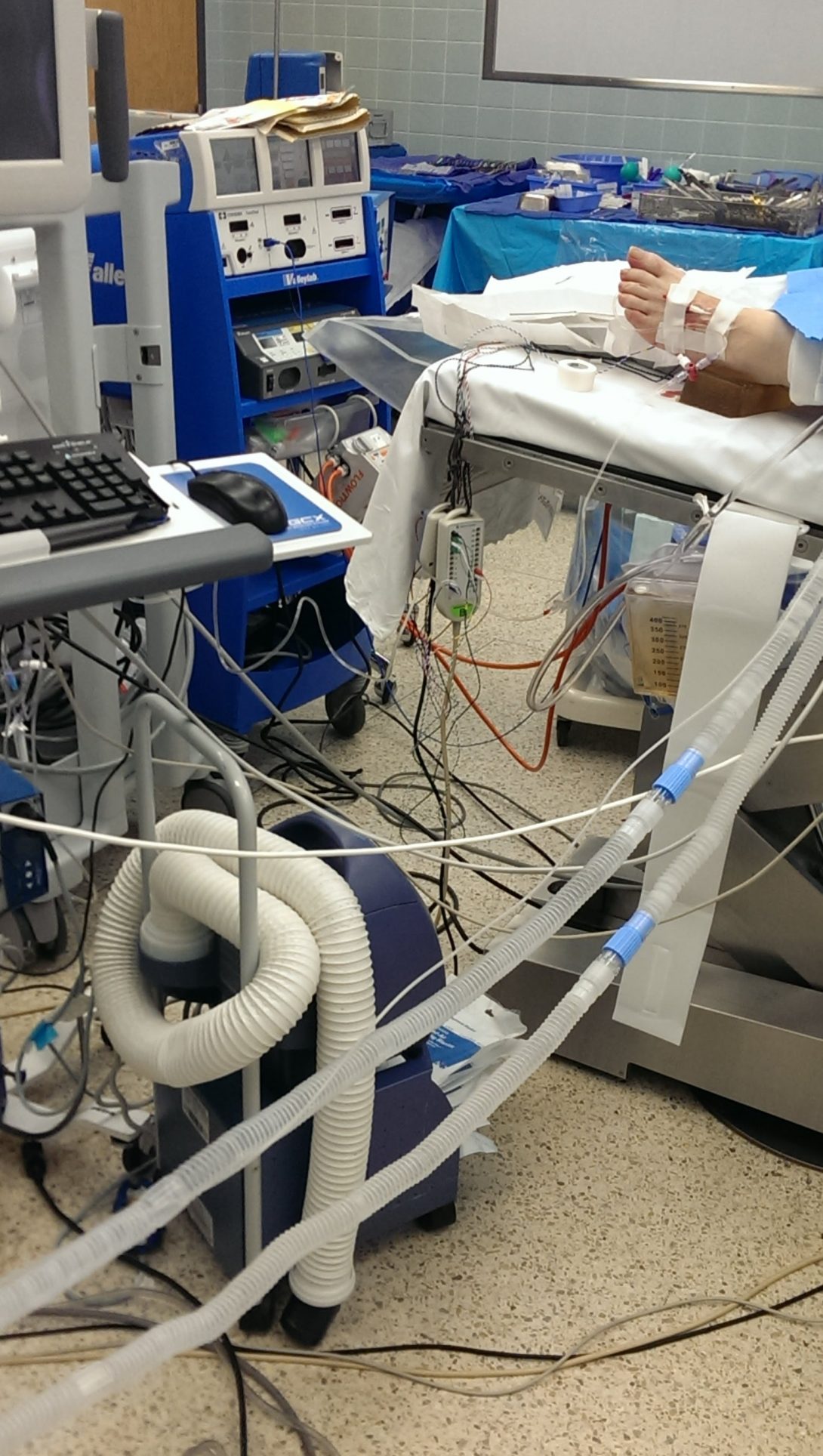
Image
Martin Strama Blog

Image
Martin Strama Blog

Image
Martin Strama Blog
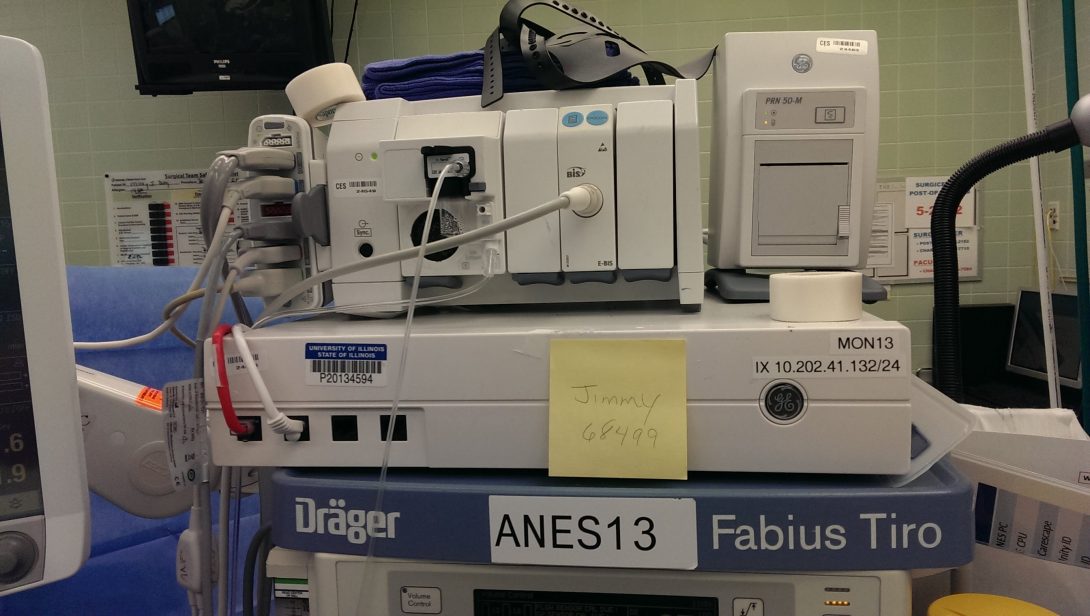
Jackpot (Case Studies: Pt. 1)
posted Aug 1, 2014, 7:08 PM by Unknown user
The best part of being in the anesthesiology rotation is that I am not confined to a single department in the OR. Anesthesiologist are everywhere. Thus, I am exposed to many different surgeries, and consequently, many different medical devices! How amazing. This is a jackpot for any bioengineer. As a result, I will be posting many different case studies along with significant medical devices utilized by both anesthesiologists and the surgeons.
Deep Brain Stimulation to treat Parkinson’s
In DBS, the patient was awake and under local anesthetics. The surgeon targeted the subthalamic nucleus with electrodes. These electrodes emit a radio frequency that correlate to the brain activity at their positioned location. Essentially, the radio frequency mimics brain responses and the brain waves are picked up on a monitor. The patient is awake in order for the neurologist to examine the patient during stimulation. The neurologist directs the patients with verbal and physical cues. For example, the neurologist would move the patient’s arm and listen for the electrode response. In addition, the surgeon would increase the current in the electrode to assess the maximum pain threshold the patient can perceive before muscle spasms occur.
Spine Lumbar Laminectomy
In this operation, the anesthesiologists were concerned about the patient’s blood pressure because the patient had a weak heart. The two main medical devices/instruments utilized were an echocardiogram and a pulmonary artery catheter. The echocardiogram is positioned in the esophagus and uses Doppler ultrasound to produce images of the back of the heart. The images allow the anesthesiologist to assess the heart muscle, valves, contractility, pumping capacity, and tissue damage. The pulmonary artery catheter is used to monitor pressures in the heart chambers. To insert the catheter, the anesthesiologist created a central line across the patient’s chest using ultrasound. The anesthesiologist then looks at the EKG to make sure there is no irregular heartbeat as a result of the central line. The central line is then sutured to the patient’s skin for stability. During the operation, anesthesiologists are also concerned with cardiac output and cardiac index parameters. To obtain these parameters, a separate machine performs calculations on the EKG trace to obtain the cardiac output, and another requires the patient’s height and weight in order to obtain the patient’s body surface area, which is required to calculate the cardiac index. Thus, machines do the math for the anesthesiologists, which makes sense since they should be more focused on the patient instead of calculations.
Right Ventriculoperitoneal Shunt
In this procedure, a small hole is drilled into the skull to allow a catheter to pass into a ventricle in the brain. The surgeon used an infrared pen to position and guide the catheter to the ventricle. Another catheter was guided in a similar manner down the neck, chest, and into the belly area. Excess cerebrospinal fluid drains down this catheter network in order to reduce intracranial pressure.
Anesthesiologists’ Complaints
During my lunch break in the anesthesiology break room, I engaged with some anesthesiologists to inquire if they experienced any problems with the medical devices. One anesthesiologist enthusiastically wanted all medical devices to be like a car in the sense that one would not have to read a user manual in order to operate the device. In essence, devices should be more intuitive with simple knobs and no icons. Make signals be straight to the point with words. Another anesthesiologist mentioned that placing the various EKG leads onto patients takes too much time. Additionally, the leads are attached to cables that clump together and create a mess.
Martin Strama Blog
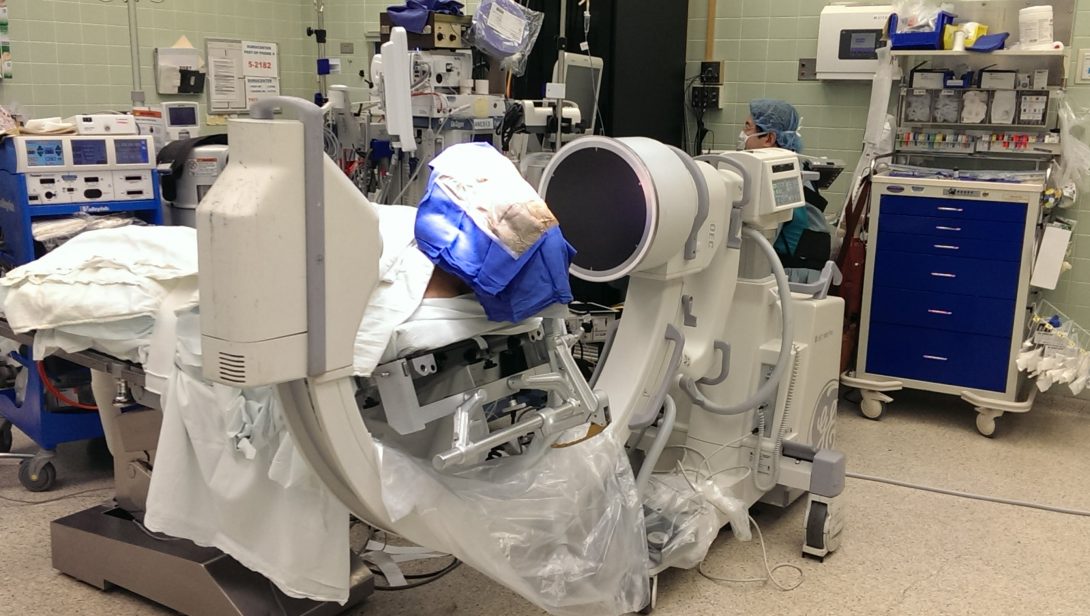
Image
Martin Strama Blog
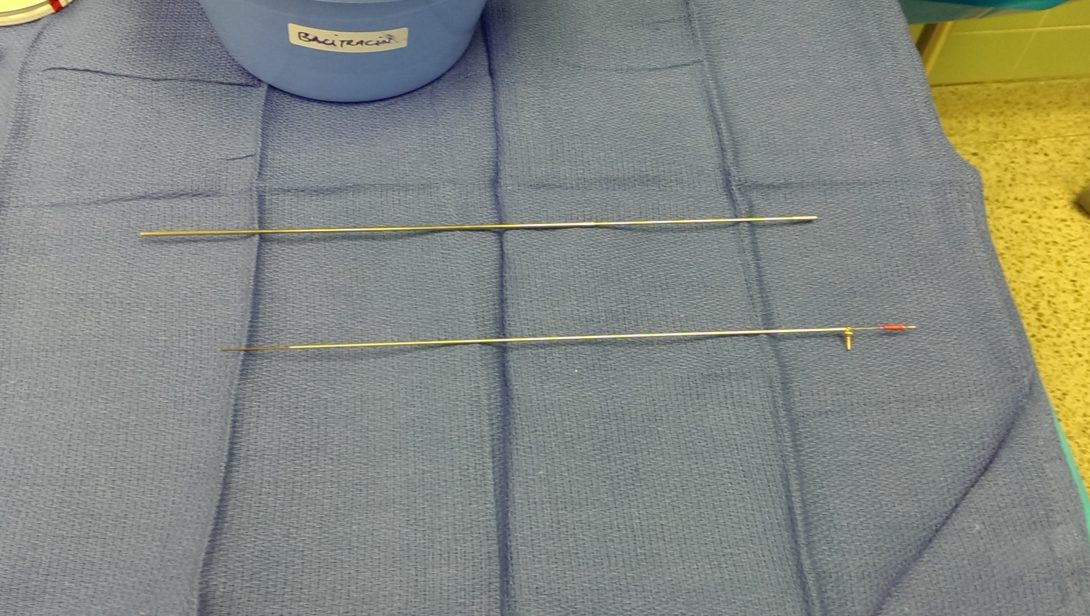
Image
Martin Strama Blog

Image
Martin Strama Blog
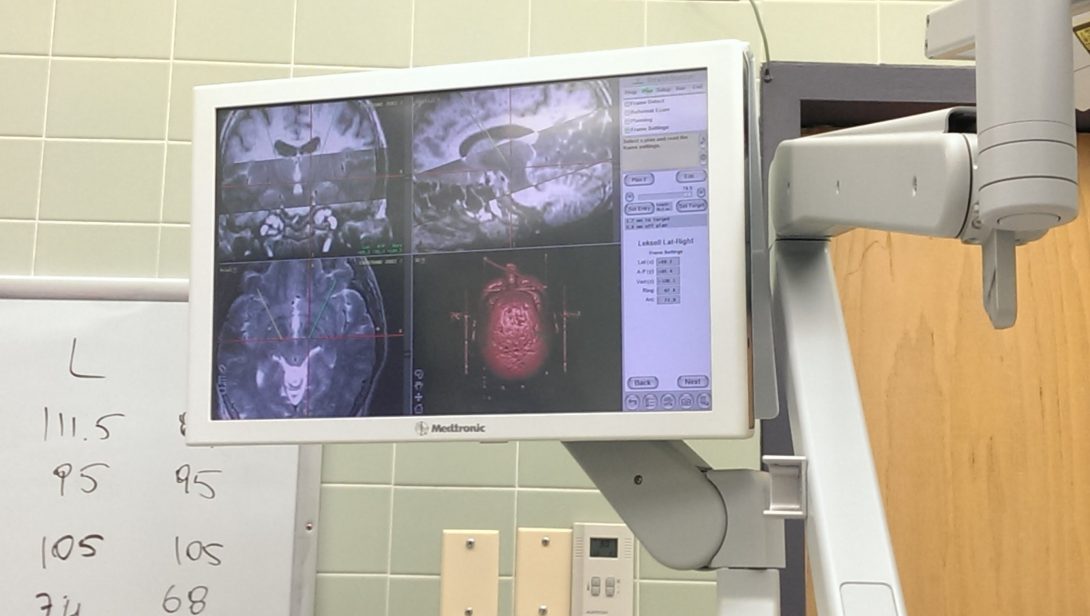
Image
Martin Strama Blog
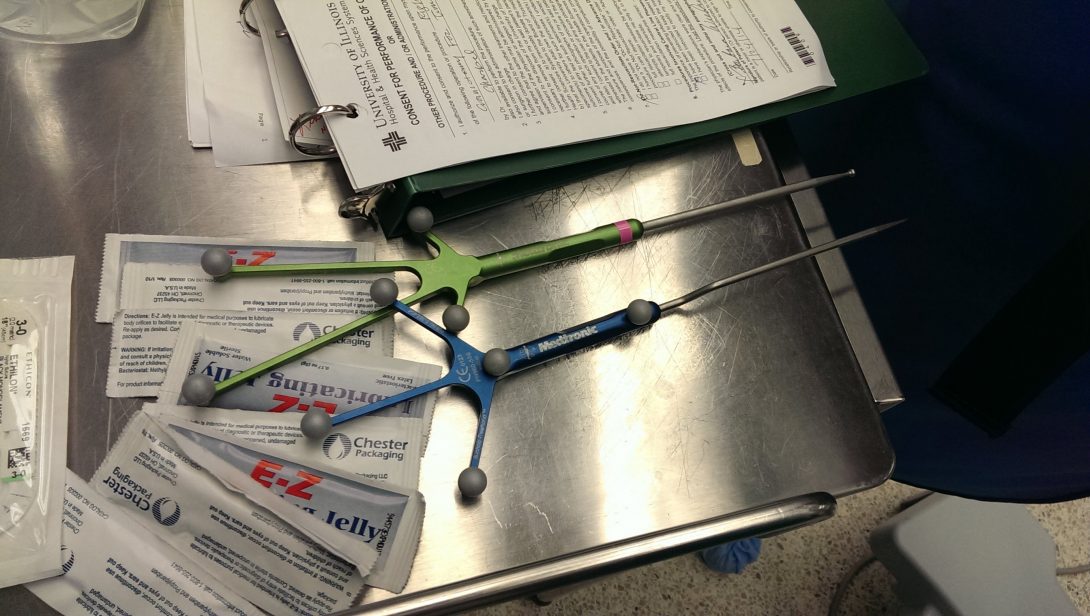
Image
Martin Strama Blog

Image
Martin Strama Blog
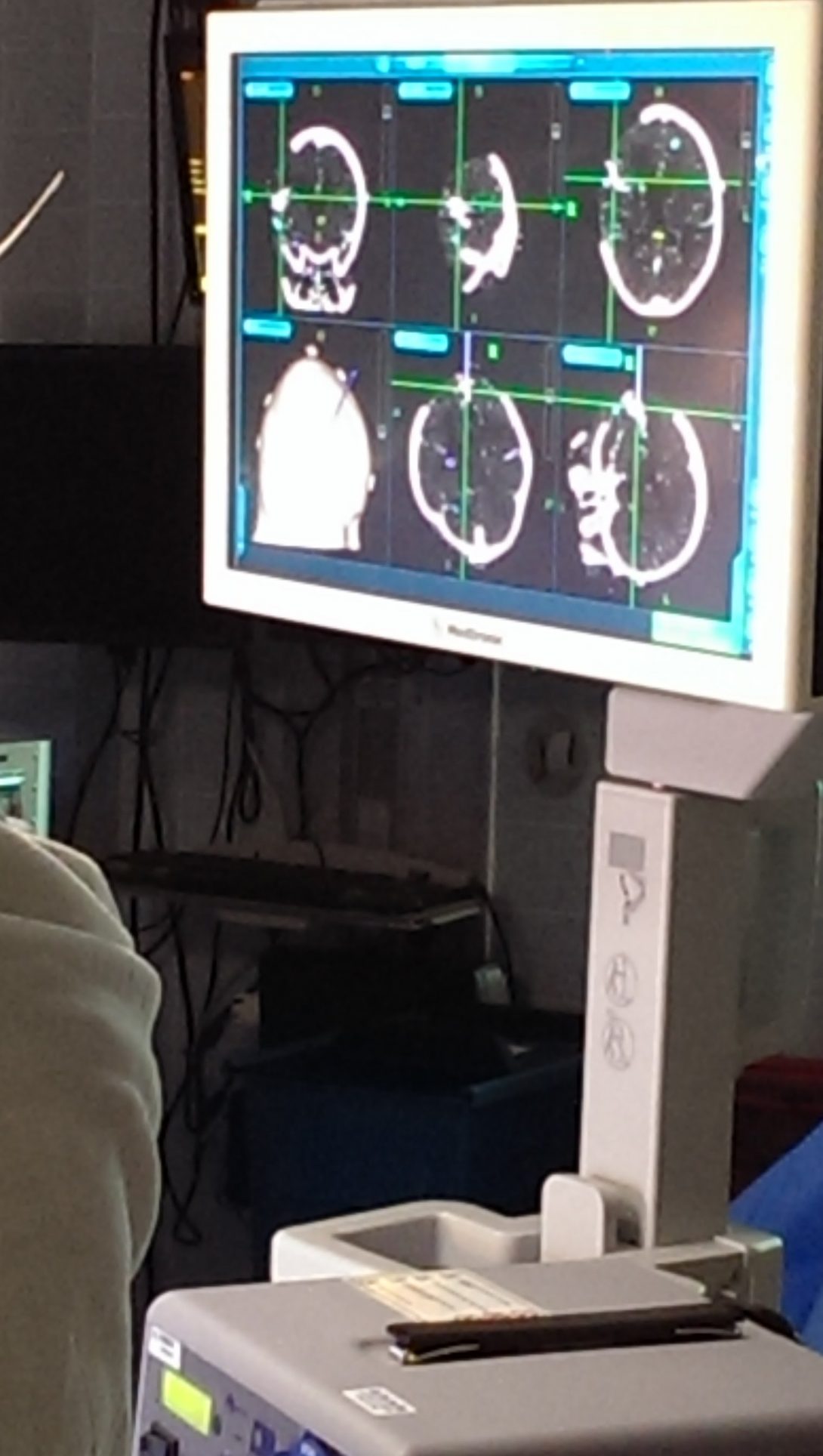
Image
Martin Strama Blog

Terminator: Rise of the Robots (Case Studies: Pt.2)
posted Aug 6, 2014, 3:44 PM by Martin Strama
Robotic devices are fully functional and operational in the OR. More specifically, the da Vinci robotic system is the dominant robotic platform. Such procedures that utilize the da Vinci Surgical System include laparoscopic cholecystectomies, gastric bypass surgeries and laryngectomies. Robotic platforms offer smaller incisions for major surgeries, more precision, and faster recovery times. In these operations, miniature wristed instruments along with a HD 3D camera are inserted and controlled externally by the surgeon at a console. The surgeon’s hand capabilities are expanded into micromovements of the wristed instruments. Although an incredible step forward, the wristed instruments of the da Vinci Surgical System lack tactile feedback. The incorporation of tactile feedback would allow surgeons to better assess their surroundings inside the patient, increase precision, and minimize errors in severing tissues. To address this issue, haptic technology should be implanted into robotic platforms. In addition, robotic platforms have no indication for which cables are which and where the cables are connected. For such a sophisticated system, there are no indications for malfunctioning equipment, which prolongs the troubleshooting procedures.
Anesthesiologists’ Complaints
Patient-controlled analgesia (PCA) infusion pumps allow a patient to self-administer opiates at the click of a button for pain relief. Patients feel empowered and experience immediate results. However, one main problem is monitoring and recording the injections. Most of the time, someone other than the patient administer the pain medication in a situation known as PCA by proxy. PCAs are programmed to reject additional injections requested by patients who are oversedated. However, such safety features are overridden in PCA by proxy. Thus, physicians need to be able to monitor when the injections are occurring as well as who is facilitating such injections. Such information needs to be recorded electronically to EMRs so physicians can have immediate access to such information from their office.
Currently used infusion pumps are bulky, brick-like, and not emergency-friendly. The pumps are stacked on top of each other on a pole and can be easily dislodged from position. The interface for the pumps are difficult to navigate and exhibit delayed response times. Many times, the IV pumps are unplugged and replugged for a quick restart. The drug library for each pump varies for each department. As such, the selection process becomes a hassle and causes delays. Infusions need to be seamlessly integrated into one system to drive IV standardization. Infusion pumps need to be compact, lightweight, and infuse a wide range of fluids. The pumps should include dose rate calculators, convenient drug libraries, and perform titrations of drugs. In addition, the exterior should feature a user-friendly interface with durable buttons. Furthermore, IV injections should be barcoded and scanned directly into EMRs with dosage.
Mission Aborted (Case Studies: Pt. 3)
posted Aug 8, 2014, 3:55 PM by Unknown user
During a robotic airway laryngeal tumor operation, the attending anesthesiologist expected the operation to last for several hours and so, front loaded the patient with large doses of anesthetics, which is a common tactic for long operations. The anesthesiologist then proceeded to attach all the various physiological monitoring sensors and then intubated the patient. In this procedure, the endotracheal tube was wrapped with a laser absorbent tape. The tape served to protect the tube from catching fire from a laser that was going to be used during the operation. As an additional safety precaution, a special dye was injected into the tube. If the dye was seen during the operation, the surgeon knows that the tube had been breached by the laser. During intubation, the anesthesiologist had difficulty inserting the tube into the trachea, a red flag. After 20 minutes or so, once everything was prepped and the sterile field was up, the surgeons approached the patient and proceeded to examine the patient’s throat. After examining the throat for less than a minute, they knew the operation was in peril for the tumor had progressed to the back of the throat. The case was cancelled, all the prep work and open instruments had gone to waste. However, a war was then raging between the anesthesiologist and the extubation process. The anesthesiologist had to extubate the patient hours ahead of time after a heavy preload. The anesthesiologist needed to reverse muscle paralysis, relax the muscles and reactivate the respiratory system. The whole crisis could have been adverted if the surgeons just glanced at the throat to begin with. Instead, the patient’s health was at risk, money went down the drain, and valuable time was wasted.
Pain is a highly subjective topic. On a scale of 1 to 10, how much pain are you in? Has your pain decreased or increased overnight? What more can we do for you? These questions are often asked by the pain clinic anesthesiologists who administer various narcotics to patients for pain management. When not administering narcotics from IV pumps, the anesthesiologists treat pain by burning nerves inside a patient. In a lumbar pineal shunt case, after applying anesthetics to the nerves, a needle that emits radiofrequency is guided via ultrasound to the area. Ultrasound is utilized instead of X-rays because X-rays can’t show depth. However, while ultrasound can show depth, it cannot show detailed anatomic structures. For example, a rib is a rib, but which rib is it? An experienced anesthesiologist who is familiar with the ultrasound can navigate such difficult paths. In addition, the anesthesiologist does not have binocular vision and can’t look at the ultrasound monitor while guiding the needle at the same time. Instead, the anesthesiologist relies on tactile feedback while looking at the monitor. Furthermore, the anesthesiologist cannot modify the ultrasound machine by himself/herself when inserting the needle. Once positioned properly, the needle emits radiofrequency to burn the sensory nerves. During this process, the patient experiences painful heating sensations. In addition, the pain relief generally lasts from 3 months to a year.
Carry On My Wayward Son
posted Aug 15, 2014, 6:26 PM by Unknown user
My experience in the anesthesiology department has been nothing less than spectacular. Everyday we were faced with new opportunities for advancement. Before my rotation in anesthesiology, I believed that anesthesiologists only had to view a monitor and inject medication into a patient at various stages during a procedure. How wrong I was to imagine such a simple and calm environment for anesthesiologists. These specialists are essentially engineers in the sense that they must analyze various inputs and constraints in order to determine the most optimal treatment for their patients in real-time. In addition, they must be proficient in comprehending and utilizing a wide array of sophisticated medical devices in chaotic and congested environments. Current technological advancements aim to reduce the risk an anesthesiologist experiences during surgery, but fail to integrate seamlessly into existing procedures and work areas. As a result, anesthesiologists require additional training, and are forced to love the addition of cables and tubes. This immersion helped me understand that physicians need to be able to do more with less. I envision to design medical devices that are multi-dimensional in terms of functionality and efficiency. Possible design projects include wireless telemetry systems that integrate various physiological sensors and communicate the data to external peripheral devices, as well as a syringe auto-injector for constant pressure IV injections.
Thank you Dr. Sugar, Dr. Edelman, the Ophthalmology department, the Anesthesiology department, and last but definitely not least, Dr. Kotche and Professor Sterling, all of which have made this immersion experience a once in a lifetime opportunity that I won’t soon forget!
Justin Thomas

Justin Thomas Blog
Justin Thomas Blog
July 7th, 2014
posted Jul 13, 2014, 9:50 PM by Unknown user [ updated Jul 26, 2014, 7:28 PM ]
It was the first day of the clinical immersion program, and I was a little nervous but mostly excited. I’ve never been to an orthopaedic department, so I had no idea what to expect. For our first day, Ryan and I were sent to the orthopaedic clinic at the outpatient care center. We walked in to the waiting room and saw a lot of people. Some were waiting in line at the front desk, and others were sitting down. We were told to meet Dr. Chmell, so the front desk clerk guided us to a room called the “Attending Office.” There we saw many people with white lab coats. They all looked busy. A few of them were on computers looking at X-ray images or filling out paperwork. There were others walking around while reading papers. Finally, we found Dr. Chmell with residents and medical students all around him presenting their patients to him. Dr. Chmell was happy to see us and greeted us. He seemed like a very kind person. He honestly didn’t know what he was supposed to do with us, but he did his best to keep us entertained. Since he knew we were engineering students, he thought it would be interesting for us to check out a new knee brace that a patient was receiving. The knee brace that the patient received was an Ossur Innovator DLX which was a post-operative knee brace to help rehabilitate the knee. The doctor sets an angle that the patient can bend his or her leg, so the knee can improve. Ryan and I helped put the knee brace on the patient. During our first day, we also observed a knee tap. This is basically removing fluid from the knee for testing. Ryan and I then walked around the clinic. We noticed a few hand sanitizer dispensers in the hallways right outside patient rooms. The attending office was in the center of the clinic with doors on both sides of the room. This allowed doctors to quickly move around the clinic to see patients in either hallway. The patient rooms were like ordinary patient rooms we see at any clinic. There is a bed, a few chairs for the patient, a computer for the physician, cabinets filled with medical supplies, a garbage bin for the paper used on the beds, a red bio-hazard bin, a regular garbage bin, and a bin for used injection needles located on the wall. Something that was interesting was that there were green and red flags outside of each patient room. A single green flag meant there is a new patient that needs to be seen. A green and red flag meant that the patient is currently being seen by a doctor. A single red flag meant that the patient needs further assistance such as having a knee brace put on. When the flags are crossed, it means that the patient needs paperwork filled out. When there are no flags, the room is being unused. Our first day at the clinic was a little scary because we were not familiar with the place and how things were done, but we definitely enjoyed our time there.
Justin Thomas Blog

Image
Justin Thomas Blog

Image
Justin Thomas Blog

Image
Justin Thomas Blog

Image
Justin Thomas Blog

July 8th, 2014
posted Jul 13, 2014, 9:54 PM by Unknown user [ updated Jul 20, 2014, 5:20 PM ]
Today was an exciting day for me because it was going to be my first time watching a live surgery. I’ve been to an operating room before, but I never seen the environment when a surgery or operation was going on. Ryan and I went to the Main OR on the third floor, and had to change into scrubs. We had to pick up the scrubs at a scrub vending machine. After changing into the scrubs, we put on hair nets and shoe covers. This was all needed to prevent the spread of germs. We then headed to OR 3 where we met a medical student who gave us instructions. Since an x-ray was being used during the operation, we had to wear a lead apron and collar. We also had to put on a surgical face mask. Now we were ready to enter the OR. As soon as we stepped into the room, we saw a lot of people in the room. The anesthesiologist was at her machine teaching a student how it works. There were people in red hats, and they were the specialists for the tools used. One of them was a vendor from Stryker, and he gave advice to the surgeon throughout the operation. There was a scrub nurse handing the surgical tools to the surgeon. There was also a circulating nurse who made sure the operation follows hospital policy and safety guidelines. There were also a few residents and medical students watching the surgeon’s every move. The patient that was being operated on was an elderly women who fractured her hip, so the plan was to put a rod down her leg and use screws to secure it. The surgeon used the Stryker Gamma3 IM Nailing System. The surgeon used a drill to put the rod down the patient’s leg. He had to be precise when placing the rod, so he took x-ray images of the leg every time he moved the rod. When he finally placed it at the location he wanted, he then used a tool that helped the surgeon guide the screws into the leg. When it was ready to close the patient, the surgeon used a technique what i believe is called the buried suture. This is a type of suture where the surgeon only sews inside the walls of the incision without ever sewing above the skin. It results with no suturing scars and no need to take out the suture because it would dissolve in the body with some time. After the operation, the patient is woken up and brought to the post-op room. Then, a few people come in to clean up the room. We then went to another OR to watch another operation. There were less people in this room because there wasn’t residents and medical students observing. The surgery that was being performed was an arthroscopic shoulder surgery. The surgeon made two holes on the shoulder and placed a trocar for each hole. The trocar is used to keep the hole open while the surgeon inserts tools inside the hole. The surgeon inserted an arthroscope into one hole and a shaver into the other. An arthroscope is a camera with a light source used to view the joints. There is also a lumen so salt water or saline solution can flow into the arm. The shaver is used to clear up tissue. The surgeon made several holes to place the tools at different locations on the arm. Then, the tools were removed and the holes were closed. Throughout the second surgery, Ryan and I were extremely tired of standing for so long. I don’t understand how the surgeons can do this when there are surgeries back to back. Also, the room was very cold.
July 10, 2014
posted Jul 20, 2014, 5:35 PM by Unknown user [ updated Jul 20, 2014, 7:19 PM ]
Today was another day at the OR. The first surgery we watched was a total knee replacement. The surgeons were wearing a big suit that covered there entire body. It looked like a space suit. The suits were needed to protect the surgeons from bone and tissue fragments. We arrived in the middle of the surgery, so it was a little confusing what was going on. I saw a metal cap on top of the knee, and the surgeons were using a sagittal saw to cut the bone. After cutting, they removed the metal cap. Then there was a plastic object that they kept inserting into the knee. I think they were trying to make sure the plastic object fits nicely in the knee. It seemed like the plastic piece wasn’t fitting nicely, so they continued to use the sagittal saw. Once the adjustments were made, the surgeon made a white cement by mixing a liquid and a powder together. The cement had a very strong smell. They then put the cement on the knee and hammered the prosthesis to the knee. There was a vendor from Orthalign named John. He took us outside to explain the device that was being used in the surgery before me and Ryan came. It was a device used to make sure the surgeons were correctly placing the prosthesis. The device works by using an accelerometer. There was also a LCD on the device that gave the surgeon simple instructions on what to do. The device was only used for the first part of the surgery because the surgeon wanted to use his way for the second part. Next, Ryan and I watched a total hip replacement. This time we couldn’t see anything except a huge hole, so the experience was not that great. We tried getting a better view, but we didn’t have any luck. The surgery was over two hours, so we were really tired of standing for so long.
Justin Thomas Blog

Image
Justin Thomas Blog

July 16, 2014
posted Jul 20, 2014, 8:45 PM by Unknown user [ updated Jul 20, 2014, 9:39 PM ]
So far this week, we haven’t been to the OR. On Monday, we were at the clinic, and saw a lot of patients. When a doctor sees a green flag, they go to the patient’s door and pulls out the patient’s papers from the door. The papers tell the doctor the patient’s history and the reason for their visit. Before entering the room, the doctor puts the red flag up so that both green and red flags are up. When the doctor enters the room, they greet the patient and sit close to the patient. They try to get the patient comfortable before actually evaluating them. When a doctor sees a patient with hand pain, I noticed the doctors use the same tests to evaluate the hand. They tell the patient to squeeze their hand to test the patients strength. They also touch the tip of the patients fingers to see if the patient has any tingling sensation. They then tell the patient to spread their fingers and try to resist when the doctor tries to squeeze them together. They also tell the patient to bend their hand forward and backward to see the joints mobility. If the patients never had surgery before and their problem isn’t too bad, then the doctor would advise physical therapy. If the patient has severe pain, then they would give the patient an injection of steroids. The injection is performed first by applying iodine and alcohol pad. Then they inject the needle. Patients have a lot of pain when they get the injection, so the doctors sometimes apply a spray while giving the injection. The spray is supposed to ease the pain. If the injections and physical therapy don’t work then the doctor advises surgery. Another thing I noticed is that the doctors didn’t really use many tools. One tool they use is a goniometer, and it is used to measure angles such as the angle when someone bends their hands. Another device they use is an x-ray which is really important when evaluating a patient. We also saw patients who needed their cast removed. Normally people who work at the cast room would remove the cast, but when we were there the medical students wanted to remove the cast. They used a cast remover to remove the cast. The device has an oscillating blade that only cuts through hard material. It can’t cut through skin because the skin moves with the oscillating blade. A hard object like the cast doesn’t move with the blade, so the blade can cut through it. The clinic at the UIC medical center is usually busy, and the doctors don’t really have a break. The clinic downtown is totally different. It is more like an office environment with a great view of Millennium park. The layout of the clinic was different too. The doctor’s office was far away from the patient’s room. The center of the clinic was the x-ray machine and the cast room. I think the clinic was designed this way because there is not a lot of patients at the clinic at one time, so the doctors don;t really need to rush over to the patients. The downtown clinic also had flags, but they weren’t used often. I also think it’s because there is not a lot of patients to see at one time. I noticed there wasn’t any hand sanitizer dispensers anywhere. There was only one anti-septic container in the hallway. They were also in every patient room. One thing that was interesting was that there was a room that was latex free. I don’t think there was a room like this at the UIC medical center. The patients were also different. All of the patients downtown were all Caucasian and seemed pretty wealthy. They also took care of themselves, so there cases weren’t that serious. The UIC medical center had a lot of minorities and poorer people. They did not really take care of themselves and were normally overweight. I think it was great going to the clinic downtown because we can compare the two clinics.
Justin Thomas Blog
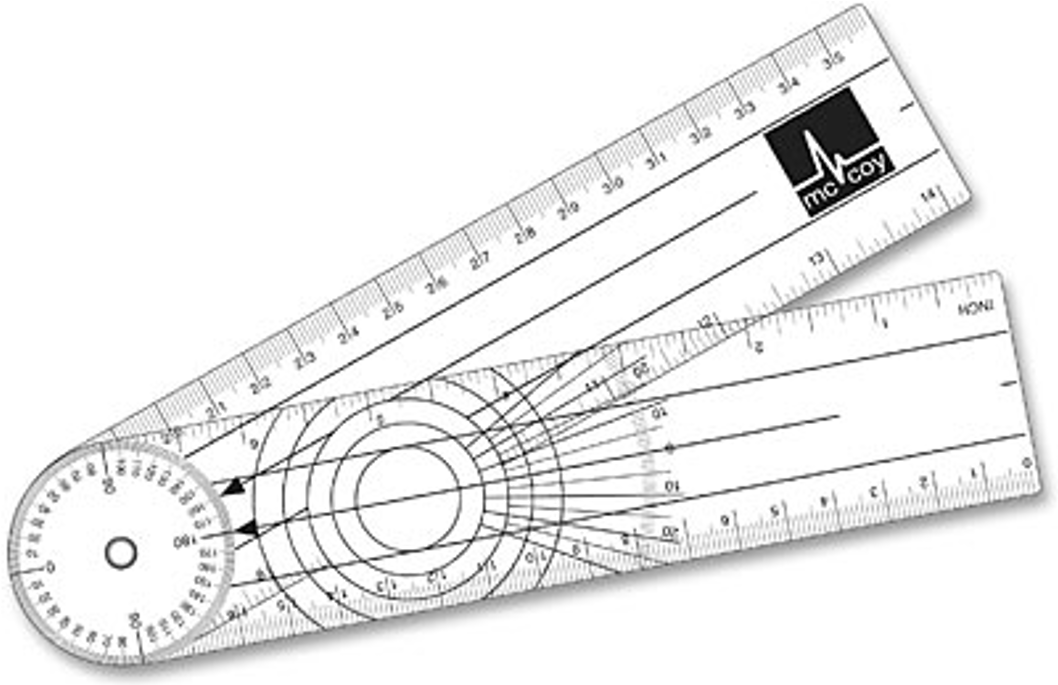
Image
Justin Thomas Blog

Image
Justin Thomas Blog

July 17, 2014
posted Jul 21, 2014, 5:21 AM by Unknown user [ updated Aug 10, 2014, 1:34 PM ]
Today was another day at the OR. This time we were able to watch a total knee replacement from start to end. This made it much easier to understand what was going on. The first thing that happened when the patient entered the OR was putting the patient to sleep. This job was done by the anesthesiologist. Then the patient had a urinary catheter inserted. The patient was also hooked up to a Zimmer automatic tourniquet machine. The tourniquet is important because it controls bleeding. Then, the surgeons applied iodine and alcohol pad all over the patients leg to get rid of any bacteria on the surface of the skin. Then, the patient’s whole body except one of his or her leg was covered by blue sterile drapes. This was done to prevent the spread of infection. If a surgeon touches skin that isn’t properly cleaned and then touches the surgical area, then bacteria can go inside the patient and cause infection. The drapes also prevents the patient from getting blood all over their body. Next, a bandage was tightly wounded around the leg and then removed to decrease blood flow. Then they put an orange film over to prevent bacteria to go into the body. I also noticed that a DVT pump was used. It was cool seeing the DVT pumps in surgery because I was familiar with them. I had to repair them a lot at Northwestern. The surgeons and scrub nurse go outside the OR and properly wash their hands. Then they return wearing a helmet called the Stryker T5. The helmet is light and has a fan at the back for airflow. Then they put on their “spacesuits” and layers of gloves with the assistance of the scrub nurse and the circulating nurse. Once it was time to make an incision, the circulating nurse called timeout and stated the patient’s name, age, operation, and any allergies. The first thing the surgeons did was cut through the skin until they reached the kneecap using a scalpel. They also used retractors to keep the surgical wound open, and they also used suction to get rid of any fluid. Then a tool was placed on the joint of the femur. It was secured on the joint by having pins hammered into it. There are slots in the tool, so a sagittal saw can be used to shave off bone. Next, the Orthalign system was being used. The system was placed over the shin, and pins were used again to keep the device in place. The surgeon followed the instructions on the screen of the device. This allowed precise tibial resection. The orthalign system was then removed and put aside. Another device was placed over the joint of the femur. It also had slots, so that a sagittal saw can be used to shave off bone. The joint was sculpted, so that the prosthesis would fit. There were test prosthesis, so that the surgeon can keep checking if the final prosthesis will fit nicely. Once the sculpting was done, the surgeon made cement and applied it to the joint. Then the prosthesis was hammered into the patient. Now the surgeon was ready to close up the knee.
Justin Thomas Blog

July 23 2014
posted Jul 27, 2014, 6:09 PM by Unknown user
The past few days, Ryan and I were at the UIC clinic and the downtown clinic. At the UIC clinic, I sparked a conversation with Dr. Schmell and the other residents about their opinion on Orthalign. They were saying that the system is very precise, but there wasn’t any proven fact that patients do better. They were talking about a study on Orthalign and that the patients who had the Orthalign system used on them actually had a worse recovery than patients who didn’t use Orthalign. The reason is because there isn’t a good ligament balance when using Orthalign. Another problem with the device is that it causes the operation to be longer. I noticed that orthopaedic surgeons like things quick and easy, so the device increasing the time of the operation is not great. However, Dr. Schmell said that the device does work in getting the correct angle or tibial resection. Dr. Schmell doesn’t use the device at all during surgery, but Dr. Gonzalez uses it for the tibial resection. I asked Dr. Gonzalez for his opinion on Orthalign, and he said the same thing. It is good for tibial resection and that is why he uses it. He said he would like to use the device for the second part of the surgery, but the device isn’t effective then. I found this orthalign issue interesting. At the UIC clinic, we saw patient and physician conflict for the first time. One issue was that a patient was behaving immaturely and made the doctors feel uncomfortable and think their lives were in danger. The patient’s behavior led her to be kicked out of the spine clinic. Dr. Gonzalez talked to the patient and told her that their are rules in the clinic and the patient’s behavior was unacceptable for the clinic and in general. Since he knew the patient for a while, he did not throw her out from the orthopaedic clinic. Later that day, there was another patient-physician conflict. A patient was very mad that she could not have surgery. Dr. Gonzalez kept telling her that there is an increase risk of infection and blood cots if the patient had the surgery done because she was overweight. The patient could not let this go and things escalated. The two kept yelling at each other until Dr. Gonzalez couldn’t take it anymore and called security to kick her out the clinic. I’ve never seen patients and doctors getting into serious conflicts to the point that a patient is banished from the clinic. I never knew a patient could even be banished. I noticed that all of the residents and medical students talked about what happened in a low voice when Dr. Gonzalez wasn’t around, but they didn’t mention the situation when he was around. This was a very strange experience for me.
July 24, 2014
posted Jul 27, 2014, 6:29 PM by Unknown user
Today was the last day going to the OR for the orthopaedic department. It was a great day because there were a lot of surgeries scheduled today. One surgery in particular was very interesting. It was a total knee revision. The patient’s knee replacement became infected, so she needed a new prosthesis. From the start, the surgery was a complicating surgery, but there were more complications during the surgery. One major complication was when the test for the femoral component wasn’t working properly. Dr. Gonzalez tried to attach a piece to the test device, but the device was so worn out from being used multiple times that he wasn’t able to properly attach the piece. This made him furious because he was spending a lot of time trying to fix the test device and also the implant may not fit correctly. Since he wasn’t able to properly screw the piece to the test device, he just put them together without screwing them together and placed it into the knee. He then continued the surgery. One thing that was interesting was that the surgeons and the scrub nurse had to wear special gloves since the patient had HIV and hepatitis C. The gloves were to protect the surgeons and scrub nurse from getting infected. I thought this was interesting because they are already wearing layers of gloves, so I wondered how also wearing this special glove can make such an impact. I then remembered my gloves breaking many times when I worked at Northwestern. I also looked up why layers of gloves are needed, and it is because there is a a lot of defects in gloves.
July 30, 2014
posted Aug 3, 2014, 10:48 PM by Unknown user [ updated Aug 8, 2014, 12:01 PM ]
The first few days with the transplant department were spent at the ICU. During the morning, the residents and medical students present the patients to Dr. Ivo Tsvetnov. The reason they do this is to make sure everyone is up to date with the patient, and so that everyone can discuss on what further actions can be done for the patient. One of the residents said they do this, so that they can figure out how to discharge the patients as fast as possible. The presentations or rounds take a few hours. I noticed most of the doctors talked in a low voice. I think they do this so that the patients can’t hear what the doctors are saying about them. Since the doctors are discussing and making speculations, they probably don’t want to scare the patients. However, it still seems uncomfortable for the patient because a group of residents, medical students, and pharmacists stand outside their room and talk about them. The patients look scared and curious of what the physicians are talking about. What I liked about the ICU was that there were a lot of medical devices. For example, there is a few Braun infusion pumps, a DVT pump, a GE patient monitor, urinary catheter, urine drainage bag, a glucose testing machine called the ACCU CHEK Inform II, an endotracheal tube, a ventilator, and many more. The ventilator was very interesting because the machine has many modes when assisting a patient. The ventilator can have full control and breathe for the patient. The machine basically pushes in air to the lungs. The volume and pressure can be adjusted by the physician. The person who sets up the ventilator is the respiratory therapist. We’ve also went to the Interventional Radiology (IR) room where minimally invasive procedures were done. The procedure that Haroon and I observed was the placement of a central line. The setting of the room where the procedure was performed was similar to an OR. Everything in the room was sterile. The patient was properly cleaned with iodine and had drapes over their bodies. The radiologist who performs the procedure also wears gloves and surgical aprons, but they also wear lead glasses, lead apron, and lead cuffs. The radiologist also used an ultrasound to see where to place the central line, and they also used an x-ray to see where the central line, which was coated with radiopaque, was when it was inside the patient. I’ve never heard of an IR so this was an interesting experience for me.
Justin Thomas Blog

Image
Justin Thomas Blog

Image
Justin Thomas Blog

Image
Justin Thomas Blog

Image
Justin Thomas Blog

Image
Justin Thomas Blog

August 1, 2014
posted Aug 3, 2014, 10:58 PM by Unknown user [ updated Aug 19, 2014, 9:33 AM ]
Haroon and I went to the OR on Thursday and Friday. I saw a vendor from Applied Medical that I met a couple weeks before, and he asked us if we wanted to see his new trocars in action. We agreed and watched a hysterectomy. The surgery was interesting because the surgeon used a minimally invasive method to remove a whole organ (the uterus). The surgeon made a few holes over the patients stomach and pushed the trocars through the skin. What was special about these trocars is that they have a camera at the tip, so the surgeon can safely insert the trocar through the patients body without damaging any organs. Also, the trocar has a balloon, so the trocar doesn’t move around. The trocar is important for minimally invasive surgery because it keeps the surgical hole open, and it allows surgeons to put tools inside the patient. The procedure took a while because the surgeon was carefully cutting away tissue with an Ethicon laproscopic tool. The tool was similar to a cauterizer but it’s end looked like scissors. I was thinking that laproscopic surgery is great because it’s minimally invasive and there is a less chance of developing infection, but it causes surgeries to take much longer.
In the transplant department, there are a lot of surgeries related to the fistula. When Haroon and I were at the Transplant clinic, we saw many patients that had a fistula. A fistula is a substitute for a catheter for dialysis patients. Catheters are not great because they increase the chance of infection, so fistula’s are recommended. The fistula is a pathway created by a surgeon. A fistula is needed because dialysis takes blood out of the body at a fast rate which causes veins to collapse. Thus, the fistula prevents the vein from collapsing. However, when the fistula does not work, then a graft is used. Haroon and I saw a procedure done in the OR, that inserted a HeRO graft into a patient. This was done by making an incision at the left shoulder and above the elbow. The graft is then tunneled through the skin using a device shaped like a hook.
Justin Thomas Blog
August 6, 2014
posted Aug 9, 2014, 9:39 PM by Unknown user
The past few days have been very slow. There were no procedures at the OR, so Haroon and I were at the ICU and transplant clinic. We attended rounds in the morning as usual. Then we walked around the ICU, and observed the staff. There wasn’t really anything interesting going on. The residents and medical students were taking notes and talking on the phone. They also just sat there and talked to each other about their days. Every now and then they would check up on their patients. Most of the cases there were also not interesting. They were mostly patients recovering from surgery. While walking around the ICU, I noticed a device that I wasn’t familiar with, so I asked Dr. Tzvetanov what it does. The device was an Edwards Lifesciences Vigileo monitor. He explained that the device gives hemodynamic information to doctors. There is a catheter placed into a patient’s artery, and then the device can display the volume of blood and oxygen saturation. Dr. Tzetanov was telling us that engineers build these deices, so that doctors can obtain more information about their patient and try to figure out what is wrong with their patient. He then told us that creating infusion pumps with pressure sensors have helped medicine. He said that doctors had to do calculations when using IV, so making a better infusion pump has made their lives easier. He then talked about how machines can be wrong, so a doctor needs to understand machines to verify if what is being displayed by the machine makes sense.
Justin Thomas Blog

The patient that was hooked up to the Vigileo monitor was having many health problems after his surgery. He was continuously bleeding, and the doctors could not stop the bleeding. The patient was in need of blood, so the nurses got blood for him. However, the patient’s name tag was not on the blood, so the nurse refused to give him blood until she was sure it was okay to give the patient the blood. The resident in charge was very calm about the situation, but the nurse was not calm. She did not want to give the patient blood because she was scared of losing her nursing license. Once the blood was verified, the nurse gave the blood to the patient.
August 7, 2014
posted Aug 10, 2014, 2:27 PM by Unknown user [ updated Aug 19, 2014, 9:31 AM ]
Today, Haroon and I were finally at the OR. The first procedure was the removal of both kidneys. The kidneys were very large and looked deformed. After removing the kidneys, they were placed on a table. It was a profound scene. We then watched a fistula creation. It was a simple surgery where the surgeon made an incision by the brachial artery. They then use a cauterizer to continue cutting through the skin and stop small bleeders. The surgeon then used a retractor to keep the surgical hole open. The surgeon then cuts the cephalic vein and attaches it to the brachial artery with sutures. I noticed the surgeon had trouble keeping the surgical hole open with just one retractor, so he added another retractor that crossed the first retractor. It seemed like the surgeon had difficulty placing the two retractors, but he eventually got it. After attaching the vein to the artery, the surgeon closed up the patient.
Justin Thomas Blog
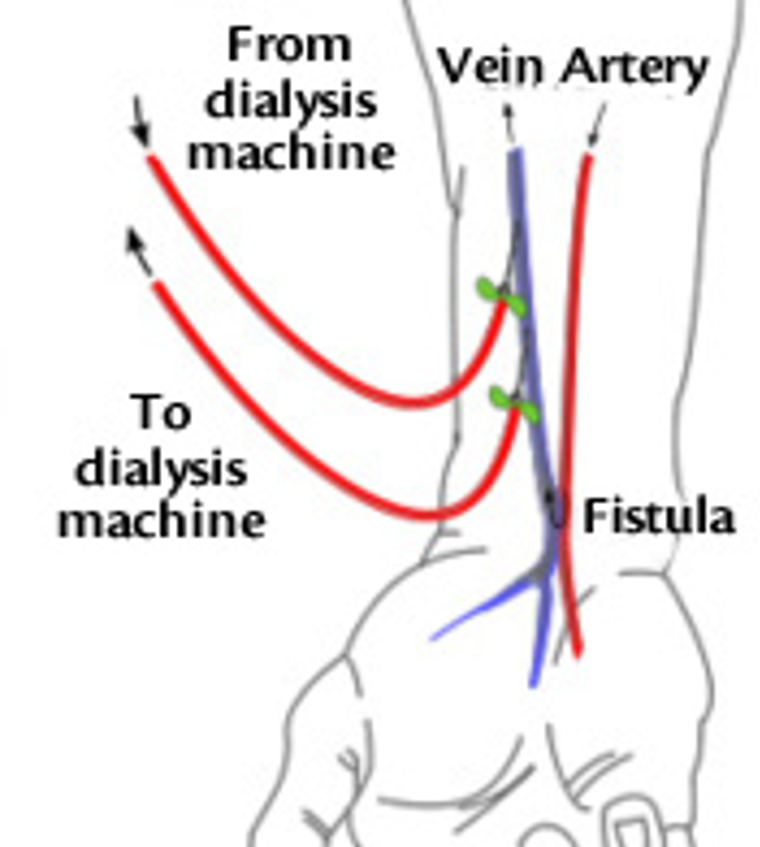
Image
Justin Thomas Blog

The next procedure I observed was a kidney transplant. The surgeon made an incision at the lower right side of the patient. She then used a big device called an omni retractor to keep the surgical hole open. The surgeon seemed like she was having difficulty setting up the omni retractor. She then made some incisions inside the patient, and then attached the new kidney to the patient.
Justin Thomas Blog
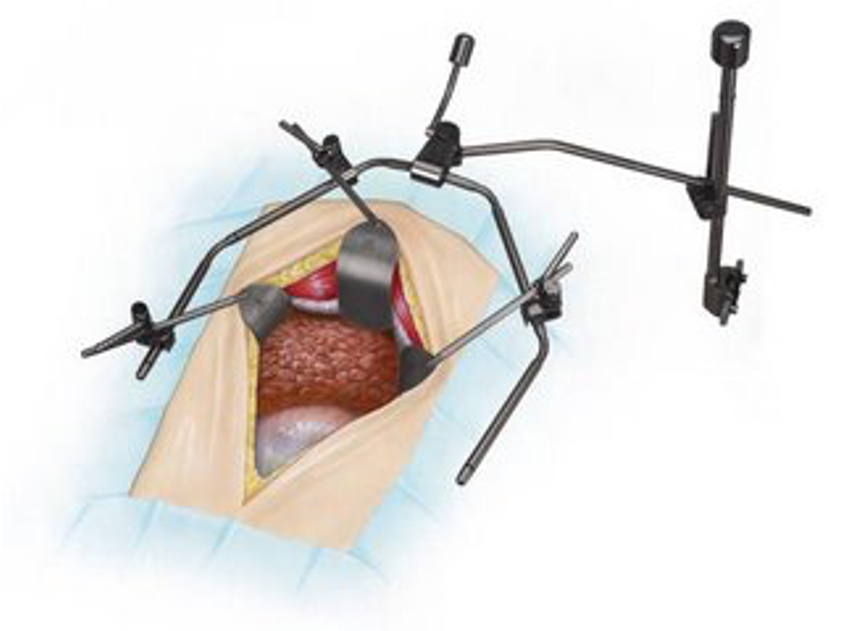
Image
Justin Thomas Blog

August 14, 2014
posted Aug 19, 2014, 10:02 AM by Unknown user
Justin Thomas Blog

Image
Justin Thomas Blog

I have really enjoyed the bioengineering clinical immersion. From my first day at the Orthopaedics department to the Transplant department, I have learned a lot about what kind of devices are needed in each environment. This experience also allowed me to learn about what current medical devices are being used and what flaws there are. I am glad that I was able to partake in this internship because now I have some future projects I want to work on.
Victoria Way

Victoria Way Blog
Victoria Way Blog
Week 1-7/13
The later half of the week began with OR. I was able to observe several cornea transplants from donor tissue. What stood out to me as most interesting was donor cornea tissue is only viable for 2 weeks after it is retrieved. Even though this appears to be a restriction, donor corneas exceed the patient need for transplants. My first thoughts into entering the OR were more lighting could be installed, A Dr. complained about the chairs not always working properly while they are in the middle of a surgery and not staying in place. The microscope used during surgery had two teaching scopes attached for residents and fellows. Attached to the microscope is a foot pedal, where the Dr. often removes his shoe to control the movement of the microscope. During an operation the Dr. voiced that the microscope would “flinch” once in a while, minimally affecting vision, but affecting it none the less. In the OR, blue sterile papers are laid over any environment which is sterile and not to be touched by anyone who did not scrub in. Music is played in the room. My assumptions for this is for the patients, because they are awake during these procedures. Patients are calmed with a mild sedative. For each procedure performed they have designated sterile trays containing all the necessary instruments to perform the surgery. Once the patient is ready for the cornea tissue to be stitched in, the doctor or fellow will cut around the cornea with a device that has sizable tips to correlate with the size of the patients eye, it is used every time and is very effective. I also notice they have a “drainage bag” on the side of the patients head. Everything is labeled in the OR, from air to water. One of the nurses mentioned that often times it will smudge (They hand write it) my thought for this is to already have multiple labels printed for ease, or introduction a small printer into the OR where they can quickly obtain labels. In making the patient comfortable they roll a sheet and place it under the patients neck, my thoughts are that a long thin pillow would be useful and more comfortable, especially for longer procedures. a workaround- the Anesthesiologist cut the O2 tubing that was going into the patients nose because it didn’t fit properly, once she did that the patient was able consume more oxygen and the procedure could begin. The equipment used was very intimidating, I assumed it was the most advanced but then found out there is already a newer model out, but isn’t an urgent necessity. The most interesting tool is the machine they use to get the eye ready for a transplant, it sculpts, polishes, vacuums etc while providing irrigation to the eye. It was beneficial to observe the equipment being used in the OR and how everyone worked together as an organized team. The last day of the week involved observing doctors with patients. An interesting thing I enjoyed was the Dr.used a specific dye that turns green in the eye to show epithelial deformities. A doctor from another country was also observing, he explained that america is one of the only countries to use the 20/20 vision system, most everyone else uses the 6/6. In speaking with a Dr, I learned that cornea transplants have a low rejection rate when the patients continually uses steroids. This is often due to abrasions or infections occurring. I observed a patient who had an infection and waited a very long time to come see the doctor, they then proceeded to heat a metal rod under a small burner in the patient room and scrape along the eye to begin a culture. The patient appeared to be very unsure of their process. What I found interesting was they actually have a fridge filled with corneas for teaching. One patient found it to be awkward to have us there observing, which in turn made me feel a little uncomfortable. One of the machines i observed was an ultra sound for the eye, it was a small probe that could view the fluid (sub-retina fluid) in the eye at a high resolution. Some doctors will use the ophthalmic scope on their head vs. the one attached to the patient chair and will use handheld lenses that provide extra magnification because you need a certain length between the light and magnification which can be controlled by the doctor. Overall it was an intense week, but very incredible.
Week 1-7/9
At first arriving to the ophthalmology clinic, there were patients everywhere, long lines of them. Most were unsure of where to check in for their appointment, There were many signs up, but at first glance they appear very cluttered, some could have been enlarged for better visibility. There is a distinct room in the cornea department with several instruments for measuring and documenting various attributes of the eye. To continue with my time in the cornea department, the exam rooms were compact four rooms in a small hallway, it seems optimal for doctors to quickly move to new patients, however when there are multiple people assisting the doctor it can feel very cramped. In each exam room there is a large piece of equipment containing scopes for doctors to view the patients eyes using the slit lamp. In most rooms there was a ‘teaching scope’ attached, which was extremely helpful in observing what the doctor is looking at. It would be beneficial to have them implemented into all of the exam rooms. Some general observations – doctors were incredibly diligent with cleanliness, as expected. Residents, students, and fellows also did the same. Majority of patients I observed were very friendly and open to allowing me to observe the Dr. examine them and watch how he uses various tools. In the exam rooms, patients and optometrists seems to have limited leg room when the doctor closely examines them with the scope because of the device placements on the patients, no one seemed to be bothered but it could have been improved. One of the most interesting devices was the field of vision. As the technician physically marked where the patient could view the light (they buzzed when it appeared in their field), my first thought is, instead of the technician having to stop every time the patient buzzes, a device could be implemented onto the equipment to mark the sheet simultaneously while the patient indicates light in their vision. In taking in more basics about the office setting, each room contained a desk close to the patients chair for easy examining and additional chairs for family, etc. After many patients I observed a minor surgery where all that was required were tweezers and forced to remove a cyst on the eyelid. This may be considered a work around, a patient could not understand English so the doctor then learned the terms for “up” “down” “left” and “right” from a family member in Spanish so she could examine the patient with ease. One of my favorite things was observing the contact lenses department. In this department, I was most familiar with the terminology. Having taken cell and tissue engineering classes, we learned a lot about the “kpro” created by UIC. I observed many patients with this sutured onto their lens. following that, they would be fitted with either soft or hard lenses, or even hybrids which contained hard lenses in the center followed by different skirt lengths of soft lenses. In this department patients seemed most relaxed. One thing i would change about the equipment is that most rooms now have a tv screen where doctors can put various letter sizes up on the screen for patients to read, not all rooms possessed this however. some had boards, or projectors, it would be beneficial to upgrade them all. Also, patient files are scanned into the computer instead of directly entered. this could be upgraded, but in speaking to the department head this would cost around 500 million to update the entire hospital and health systems to an online system, such as Epic. Another great instrument I observed in action was an infra red laser which vaporized unwanted tissue. I also got to use it on a kleenex box. An interesting case I enjoyed was someone who had a stem cell transplant in his cornea, improving his vision to 20/15. Overall, the doctors were very informative and welcoming, they even provided me with a list of permeable membrane materials used for lenses which helped put the process into perspective, since proper oxygen flow is crucial.
Week 2-7/16
During the beginning of this week I shadowed a Dr. in the contact lenses department. I observed several patients with large gas permeable lenses – large, hard, and rigid. One thing that stood out to me was the cost of the prosthetic, $2,000 per eye! However, the Dr. always personalizes a letter to the insurance company to help pay for the cost so the patient can have the best lens possible to improve their vision. An interesting conversation I got to be a part of involved limbal stem cells. They are trying to be able to induce the natural production of them around the cornea to aid in vision repair. An apparatus I found intriguing was another way they check a patients prescription. They have a large draw filled with a huge amount of interchangeable lenses they can pop in and out of what appeared to be a set of large bulky glasses. With this, patients were able to walk around and become comfortable in what would be their new prescription. I found the rooms to be more spacious than the previous cornea department. The equipment was the same as described before in each room, although they did not have a teaching scope which would have been very beneficial. Following contact lenses, I spent the next day in the OR. I observed several vitrectomys which cleaned up scarring, and cleaned the aqueous and vitreous membranes. Through out this procedure I gained a better understanding of the anatomy of the eye. I saw the membrane of the eye being peeled to improve vision and the repair of a torn retina. What stood out the most was the advanced tools being implemented. A machine called “constellation vision system” supported majority of the tools required for the procedure. It had color coded tools for the cutter, laser, polisher, etc. Anytime the doctor asked for a setting to be changed on the machine, the system would verbally confirm the change, reducing room for error. Before each surgery the machine is checked for defects. Some nurses found the verbal confirmation to be annoying at times, I was mostly fascinated with it. Its almost hard not to look for problems in any situation presented to me, I feel as though the engineering side of me continually wants to solve problems. A fascinating device we got to observe was a laser that could do majority of the procedure for the doctors so less time was spent in the eye during the operation. However, there was one slight issue, the machine doesn’t make the hospital money so it is primarily used in self pay patients, because then it would be a price reduction for them. There is a lot of room for technological strides in this procedure but the reimbursement in health care prevents doctors from facilitating advancements. Continuing with the procedure it was intriguing to learn about the type of gas they use to keep the retina held back C3F8 or SF6. Patients are not allowed on airplanes for a few weeks after the procedure, one patient actually went against this and his eye ruptured. I never understood why some patients choose not to listen to their doctor. I noticed that through out the OR’s different music is played in each of them, must be doctor preference. Although the surgery techs only went to school for 2 years they are required to know all the names of the medications and how each machine operations. Training must be exhausting. Moving through the week, I sat in on an interesting lecture about using the eye for translational research, and studying graft vs host disease. despite some of the knowledge being beyond my scope it was interesting to see the results of them using in vivo to track T cells within the eye. They performed cornea transplants on mice and experienced high rejection rates, increased graft survival was found using chemokines and receptors to block anti-recruitment therapy. One thing I understood the most was using an anti-VEGF to prevent the build up of blood vessels within the eye in diabetic patients. Lastly, I spent some time in pediatric ophthalmology. Some observations I made were that the rooms were much larger, and had brighter colors. There was plenty of room for family and students to observe. The standard equipment was the same in pediatrics, also without the teaching scope. Movies are played for the kids in the rooms so they can focus on something while the doctor examines them. Or the dr would allow the child to sit on the parents lab as well during the examination. The overall appearance was very bright, it felt friendly like you wanted to be there. In pediatrics you observe a lot of children with crossed or drifting eyes. A tool I thought to be interesting was the prism blocks to see how much correction is needed to be done to the muscle to straighten the eye in surgery. One diaper equaled a 1/2 degree. With these they could bend the light to the fovia to document the correction needed. One thing I found to be challenging is that in the ophthalmology department there are larger numbers on the doors, for example 3143, then also on that door was “exam room 1” or a variation of that with more room numbers, it became a little confusing when directing patients or searching for a room. Overall, the first half of the week was very informative.
Week 2-7/18
The second half of the week began in the OR. I noticed the room was grounded for safety, I’ve learned about it briefly in class, but to actually see it was fascinating! I was able to observe strabismus surgery. With this I was able to get up close with the pediatric surgeon and see the muscles they were working with and how they measure the diameter length needed for correction so the eye could be straight. An interesting technique the Dr. talked about was how she leaves an exposed stitch so she can fine tune the adjustment of the eyes when the patients wake up and focus on a fixed object. I noticed that all of the rooms had red outlets, this indicates that even if the power were to go out they would be connected to the generator. I found that to be extremely beneficial, I hadn’t thought about how hospitals operated during a power outage. Moreover, during this procedure the doctor places a microscope on her head where the lenses can rest over her eyes, versus the large microscope in prior operating rooms, visibility was great for students to watch the operation. I observed them cauterizing parts of the eye to stop the bleeding, the room feels much more relaxed than the previous OR’s. Something I found most interesting while observing a resident do the surgery is that they practice on pig eyes before being able to operate. An interesting case I observed was twins who needed the same surgery for correction, they needed the same exact millimeter correction to straighten their eyes, it was fascinating. Moving back into patient cares, I noticed a machine called a pupilometer, it measures how much the pupil reacts to light and had a large “bioengineering” stamp engraved on it, it was neat to see that. I experienced a patient that did not allow students to observe her, patients are typically very welcoming to us observing, even though some appear overwhelmed to the amount of us there are (fellows, residents, med students, and engineers). I’ve been finding that through this shadowing process I am gaining a lot of knowledge applying to the eye and its anatomy, it makes each day more intriguing because I can understand more of the diagnosis and typical patient/doctor reactions. An interesting conversation I got to be a part of was how they are creating contact lenses that can monitor your blood pressure through out the day and even your eye pressure. This seems ideal for those with high pressures to minimize the risk of the condition worsening. In a few of the rooms I noticed domestic violence signs, I found that to be odd seeing as it is an ophthalmology clinic. One of the doctors actually let me use some of the instruments she uses to treat patients, that made the experience even more like a clinical immersion. Rotating in the neurological ophthalmology department allowed me to observe patients with underlying conditions that cause eye related problems, one of the most fascinating causes was a patient whose autoimmune system began to attack the healthy cells in the eye. The patient appeared to be calm and understanding, although you would think a different reaction would arise. Overall, the week was filled with new clinical experiences and interesting patient cases.
Week 3-7/23
During this week I listened to some of the doctor’s voice their opinions on issues within the clinic. One that arises often is patients in wheelchairs; it’s hard to examine them without inconveniencing the doctor. A solution we discussed would be to have the room chairs slide back; allowing the wheelchair to come in its place so the doctor can better evaluate the patient. An interesting conversation I took part in involved tissue glue, which acts as a clotting factor. As a future tissue engineer this grabbed my interest. It’s made up of proteins that cause clotting without the cells often used in glaucoma patients. It’s rewarding to hear them discuss a case that you fully understand, such as them referring to the material PMMA. In class we learned it to be an option in hybrid lenses, but in actuality it is only used in trials because it isn’t O2 permeable. Moreover, I have gotten different reactions to EMR when discussing it with the doctors, some really want it while others have to make sketches of the patient’s eye and find that it would be difficult and time consuming to perform that on an online system. In spending more time in pediatrics I’ve learned that children have a higher rejection rate of transplants because their eyes change more drastically. Parents often try to self-medicate their children, by googling, WebMD, etc. I noticed a doctor wishing the public was better educated about the risks of not treating a child’s problem correctly or avoiding an immediate doctor visit. Doctors are incredible at multitasking, nothing seems to slip by them, and it’s very admirable. The amount of patience they possess is incredible, especially in pediatrics where children are very timid to doctors and often screaming while receiving eye drops. Something I found interesting was a patient was taking a diuretic to reduce eye swelling; it never occurred to me how simple over the counter medicine can apply to more global problems. I observed a patient who had no sensation what so ever, it was very hard for the doctor to work with them; it’s very difficult to know if there is a problem within the eye because they don’t perceive an issue. There is no sensory system, so even an eye lash that may be in the eye wouldn’t be detected. An intriguing case I observed was a patient who got a chemical burn in their eye. The surgeon took tissue from this lip and reconstructed his eyelid. It looked absolutely perfect. That patient was extremely grateful. Seeing patients like this make me better understand why doctors find this so rewarding. In viewing a glaucoma patient, they compared their screenings to a “normal Caucasian” because that’s all they have for comparison. It would prove to be more beneficial to have multiple races included. Moreover, I spend majority of my time in the lenses department where they work with k-pro’s and prose. What I find most intriguing is the hybrid lenses. They are composed of a soft lens and a rigid lens within the center. The lens should not touch the cornea; therefore there is a base curve within the hard lens. I had a discussion with the doctor about room for improvement. I noticed in patients that have these are often uncomfortable at some point. The material they are constructed with could be made moister so less deposits form which cause irritation in the patient. A major issue is keeping them moist. As the patient wears them throughout the day they become tight on the eye, a moister surface would prevent this. The shape of the soft lens can often contour and suction to the eye, which is very unhealthy. This generated my interest as a possible project to look into new material options with optimal permeability for ultimate patient comfort. A lot of the constraint is that the material needs to be bio-compatible to the eye. I observed patients complain about the pain of removing a suctioned lens. As I continue more closely within one department it opens my eyes to more of how the patient feels and how the doctor adapts to each individual case putting their best knowledge forth for minimal error.
Week 3-7/25
The second half of the week was spent talking a lot about innovation and design, reflecting on the various departments we have visited. In the previous post, I discussed working with hybrid lenses, and how I would improve them. Going further into innovation, the Dr. and I discussed bio-integratable K-pros. It would be an excellent idea to use a porous material, so the tissue can grow into the pores and secure the implant. Another issue we discussed was cornea banks. There is not enough for the world; however there is plenty for the United States. We obtain about 60,000 corneas a year, and export around 15,000 of them to places around the world. If we could come up with a bio-engineered cornea, this would completely eliminate the need for donor tissue. Another interesting point was that there is always a demand for higher resolution imaging to see through cloudy media. Most of the instruments I observed used ultra sound to take imaging, which most doctors appeared to be content with. I spent majority of the rest of the week in pediatrics. They try to make most tasks a game with the children; they become engaged and seem to forget they are even being examined. The movies they play for the kids make them feel much more comfortable as well. The technician will often times let the child sit on the parents lap in the exam chair. One thing I noticed was they use a small device to check the patients eye pressure, it is described to the child as it just “tickles their eyelashes” which proved to be effective and true. The only issue with the device is that there is only one of them for the whole clinic; technicians are often going from room to room looking for it. It would become a faster process if they had more than one circulating. It takes such a great amount of patience to work with children every day. I experienced a few children that had quite the attitude! The parents didn’t really do anything about it, maybe they were used to it. I felt bad for the technicians trying to examine them. I observed an adult patient who had 4 compression’s done. That entails the bones being broken around their eye four times to make room for swelling of the eye. The patient had thyroid eye disease following breast cancer. Seeing patients every day really makes me fortunate for my good health. I noticed it takes much longer to dilate children, they need to wait about 40-45 min, while an adult only waits about 15 min. This is due to the doctors needing to completely paralyze the accommodation in children otherwise it can result in too high of a prescription and cause headaches. Parents often get irritated because they don’t understand why it takes so much longer for their kids to dilate when it hardly takes any time for them. I think a lot of the issues in the clinic arise from people being uneducated and having language barriers. One of the highlights of my week was the other interns and I got to give each other eye exams with the instruments! It was a great experience, I found out I see 20/15 which is really fascinating. We became familiar with some of the equipment without feeling the pressure of having patients around. Most importantly we had a lot of fun testing each other and understanding what we were looking for within the eye. Overall my last week in ophthalmology was filled with great doctors that really took the time to explain to me what was happening with each patient. I was approached with the question of “what surprised you the most about being here?” My answer was simply, the willingness of all the doctors, fellows, residents, and students wanting to help us. It made me feel much more welcome and less in the way especially when I got to participate in diagnosis discussions. At times it felt a little crowded to be there, but overall I had a great experience in ophthalmology and am looking forward to starting a new rotation where I can partake in a new environment and view a different setting.
Week 4-7/30
This week I began a rotation through the hematology/oncology department. All the staff was very open and friendly to having us there. The week began with a stem cell transplant meeting, in this they discussed upcoming stem cell transplants and identified donors as well. It was a very open discussion of what was appropriate for the patient. Each doctor knew their patients very well in heavy detail which astonished me. They discussed presenting risks and benefits before anything is taken from the donor to avoid any confusion. I became educated on the difference between autologous and allogeneic donors. What I found most interesting was that autologous means the cells are coming from the patient. The benefit of this is that, they take the patients cells before chemotherapy. Since chemotherapy kills majority of bone marrow, they can inject the cells into the patient once chemotherapy is complete to revive their immune system. On the other hand, those who use an allogeneic donor have a difference role. This does not replace the bone marrow; it serves as a genetic match where the new immune system is transplanted to the attack the cancer cells. At the same time, the current immune system needs to be suppressed for long periods of time. I found this information incredibly beneficial because seeing patients in the clinic I can better understand the type of transplant they went through. Some interesting facts I learned were that your family only has a 25% chance of being a donor match. There is actually a large donor bank where unrelated donors donate stem cells and patients can be matched to them on the DNA level. A discussion I found interesting was involving cord and placenta blood stem cells after birth. This was interesting to me because I have actually been asked my opinion on this topic before and was not able to give adequate advice. I learned that it can be extremely beneficial but there is a very microscopic chance it will need to be used, an alternative is to donate the stem cells after birth. In my opinion that would be very beneficial, even just for research purposes. I was hoping to get a look at a bone marrow harvest in the OR. Unfortunately they only do 4 or 5 a year. It usually takes about 1-2 hours and they take barrow from flat bones, like the back of pelvic bone they puncture 30 to 40 different areas so they don’t drain the same spot. I spoke to a physician about this and they mentioned a device that would be extremely beneficial – a device that takes bone marrow painlessly, they seemed to laugh it off however seeing the difficulty. Moving into the clinics, the facility was very nice, the hallways were bright and the rooms were well spaced out so that there was minimal traffic. Nurses seemed to wear their own scrubs as well, seemed to be anything they liked. In the chemotherapy section, rooms are typically shared by patients – two in a room. And there are a few private rooms. It arose that inmates often get the private rooms even though you would think a frequent patient would be first in line for it. A nurse commented it didn’t seem right prisoners got special treatment seeing as there are limited private rooms. The rooms all have TV’s bathrooms and recliners. This seems like a problem could arise if you are paired with a patient whom you share no interests with, nurses try to pre-place patients to accommodate for this. The lighting in the rooms could be a little brighter. The department uses Cerner for EMR. Most like it, however I have encountered complaints of having to click too many times to get somewhere and they cope and paste everything for each visit and just add a few new notes, you would think there would be a better way to update the patient records other than continual copy and pasting. Chemotherapy seems to be all about patient comfort, which is good! There isn’t a whole lot of activity besides making sure patients are feeling their best. Moving more into the clinical side, I observed patients coming in for check-ups. A lot of what is done is making sure patients remain in remission or they are either working to prolong their life. A lot of it is also trying to improve the quality of life for the patients, even though it may be ending soon. I feel very out of place at times, its such personal news for family that I think I shouldn’t be involved. If I was in their place I wouldn’t allow extra people in the room, but that is just how I feel. I am grateful to be there regardless I just hope I am not making anyone feel uncomfortable. The patient rooms are very tight; I think this adds to the fact of me being slightly uncomfortable. Patients are very open to us being there, which surprised me. I witnessed a patient emergency where one fainted, apparently it happens enough to where their approach of the system could be updated. There are so many cables and lines in these situations that it makes a situation where you need to act fast potentially difficult. Overall the patient experience was beneficial, I will be spending this week in clinical, the next in the stem cell lab, and the last week in inpatient.
Week 4-8/1
The second half of the week was also spent in clinical. I found it interesting that they specify each day of the week for a certain cancer, for instance, Wednesdays are for lung cancers and Fridays are for breast cancers and so on. I think that is most effective, especially for the doctors that specialize in a certain type of oncology to be on rotation with one another on the same day. When the patients medication is not working for them, or they don’t see improvement doctors try to enroll patients in clinical trials. They have trials in all types of cancers including brain, gastrointestinal, lung, head and neck, gynecologic, genitourinary, breast and hematologic. An issue I noticed is that nurses have a hard time finding veins on heavier set people, the doctors will flat out tell them they are fat or need to lose weight. That seems like it would almost be uncomfortable for the patient and the doctor, but physicians seem to have no problem saying it out right. The oncology department not only aims to cure cancers, but in patients that are terminally ill or have little chance of recovery physicians try to improve the quality of life. Patients are often faced with the decision of quality or quantity. Either to continue chemo and live longer, but not feel as great or stop chemo and enjoy what time you do have. Two people in my family have passed of cancer actually and they both chose quality or quantity, as much as families want them to live longer you also want them to be able to enjoy what time they do have. We got a chance to visit the stem cell laboratory. It made the BioE 456 lab look very low quality! The lab was incredible, the technologies astonished me. They have a cell count machine that takes seconds to count cells in a vial, it’s amazing. In the lab they harvest stem cells from donors that get called in. They store them in large tanks using cryopreservation, controlled by liquid nitrogen. They got through about 4 tanks of liquid nitrogen a week. I spoke to the doctor who controlled the lab; he had a great outlook on life. He emphasized the fact that it is in fact good to be bored. People often do not take enough time to reflect and be innovative. You need to find a learning style; teaching only goes so far, individually you need to develop your own way of thinking. The new generation these days relies very heavily on technology. Kids often have the best ideas, they are very simple minded. Things that adults often miss, kids easily pick up. Engineers often over think, myself included. His overall point is that, we don’t take enough time to reflect and question why things perform the way they do. His outlook was incredibly motivating and made me want to go be innovative! Following that, we observed a bone marrow biopsy. They aspirate the marrow and take a sample. When the physician is numbing the area, you can hear the needle continually hitting the bone and they try to numb the fibers on the bone as well. This process is not done in the OR which ultimately surprised me. They drape sterile clothes in the patient room and work from there. The patient did not feel the procedure until they began aspirating. The change in pressure causes excruciating pain and the patient often screams. It’s very quick though. The device they used to extract the sample is very simple. They penetrate the skin with the needle and remove it while keep the rest of the device in the body, they then turn the tool 360 degrees several times to obtain the sample. Another part is inserted to remove the section and the procedure is over within 10-15 minutes. The week ended in the breast cancer clinic, we almost felt uncomfortable because they cancer is much more intimate. The physician welcomed us to observe. They would pull a curtain around the patient when it came time for the examination, which we were thankful for. I don’t want to ever make the patient uncomfortable. For breast cancer, they actually have an online tool called “Adjuvant” it processes all the patient information and looks at all parameters to assist the doctor in deciding the best chemotherapy route. Those who have overcome breast cancer are then placed into categories: low, intermediate, and high. These assess their risk for the cancer returning based on clinical trials that are occurring. Patients in the intermediate and high category often receive chemo even though for now they are cancer free. Doctors try to do all they can to eliminate the return of the cancer. Overall the week went by very quickly and was filled with a lot of great experiences!
Week 5-8/6
This week started off with a bone marrow transplant meeting. They discuss on going cases and their status for transplant, as well as the possible donors. They discussed an interesting case were the patient would not accept cells from her sister because they were feuding. When it comes to something that could save your life you would think the feud would be put aside. In their instance they are going to look for an unrelated donor but that could take time. A lab technician expressed her concern of how hard it is to find an unrelated donor, especially with mixed races today. We then went to the stem cell laboratory where they used a two-way syringe to extract the plasma from the cell plus plasma collection. Additional plasma is added if a higher volume is needed for the transplant. For cryopreservation of the sample, they freeze it to -90 then to -150 C. This halts all the chemical reactions in the cell, and essentially put the process on “pause.” The following day was spent in inpatient. These are typically patients with cancer that cannot go home because their stage is too far along. This is the newest wing of the hospital, it looks incredible. The rooms are spacious, the hospital beds appear comfortable and large, and there are chairs and a couch that folds out into a bed for patients staying overnight. The hospital received a 1.5 million dollar donation to create this wing. The room also includes its own private patient bathroom, as well as a TV that doubles as a computer. The colors throughout the wing are bright yellow; they make you feel happy when you walk through. Patients appear to be very comfortable there. The nurse’s stand is very open; they have their own area with glass walls to view patient hallways. A group of doctors, residents, and pharmacologists discuss each patient before they enter the room to update the patient on their status. The doctor quizzes the resident, before entering their input. We saw a patient that developed another cancer from getting treatment for another cancer. I didn’t get a chance to ask the physician how rare that was, but I can imagine it’s a small percentage. In observing the infusion pumps we noticed how beneficial it would be to have an infusion pump that could handle multiple drugs. Similar to what we discussed in class Monday, having codes for each drug to control them. Shortly after the inpatient area, we visited the hemapheresis center. Here they perform collection of stem cells; they use a 17 gage needle in the patient’s vein. If that doesn’t fit they have to put a port into an artery. The apparatus they use entails four pumps – anticoagulant, blood outlet, replacement, and plasma pump. The nurses stressed the importance of collecting the thin band produced by the centrifuge. They try to collect between 3% and 2% HCT. The patient seems to struggle during the hours they remain there, and feel pain when the needle is pulled out. The nurses discussed that when the FDA approves something the products become more expensive; the reagents cost up to 5,000 and are typically one time use. This enlightens me, seeing as how much health care cost these days. The last part of the day was spent observing the stem cell lab and how they extract the plasma from the red blood cells. The machines they use are incredible and extremely exact when they perform cell counts. We are always astonished at the technology in the lab.
Week 5-8/8
The last half of the week was spent in radiation oncology and continuing clinic observations. Radiation oncology is incredible! Not only do the devices astonish, but the programs are very intimidating. 30-35 patients can come a day from treatments ranging from 15-30 minutes. The clinic is smaller, and a little outdated except for the equipment. The radiation clinic consists of physicists, doctors, an engineer, and many technicians. The flow of patients seems to be on time and is thoroughly planned out several times. The newest machine they are in the process of implementing is the linear accelerator. This device is huge, and takes up a large amount of space. It operates by accelerating photons and electrons to the speed of light to the desired tumor location. Radiation is often received for 5-6 weeks. Tumor location is determined very precisely. They have an individual plan for each patient; they start from scratch each time for a precise plan. This plan creates a target location where the tumor needs to be hit with radiation. With each area of the body they use different margins to spare surrounding tissue. For instance, tumors in the brain have a very small margin of the area around the desired spot. For these patients their skulls are held in place during the procedure because even the slightest move can create many problems and damage healthy tissues. In majority of tumor locations they can spare the surrounding tissues. For cancers like prostate in the pelvic area the surrounding tissues are compromised, such as the bladder, because there is no other way to fully reach the infected area without damage to a larger margin. They use different levels of energy depending on tumor depth and sensitivity of the area. The deeper the tumor is the higher level of energy required. They can manipulate the radiation as “sliding windows” to zero in on one spot and not harm anywhere else. Another interesting feature is that they can layer pet scans or CT scans over the 3D plan to compare and contrast. All measures of accuracy are taken before the process even begins. Before the patient comes in, an exact plan is made for the tumor location. When the patient is actually in the machine they can take real time images to compare with the plan and make precise adjustments if necessary. The program prompts you with each step ‘are you sure you want to do this?’ and login and password must be entered. The machine will also stop if a problem is detected or the patient moves out of place. The staff agreed the program was very easy to navigate through while I found myself to be very lost. When asked if they would change anything, they replied with nothing. The machine is truly amazing with its capabilities. It costs 4 million dollars! You can easily see that. The technology is mind blowing. This has been my favorite part of the oncology experience so far. They showed us majority of all these features on a fake patient. The clinic has become a very routine environment for me. I am starting to observe many of the same issues, too many patients with appointments running hours behind waiting to talk to the doctor for sometimes 10 minutes and sometimes 45 minutes. It appears to be hard to determine patient times for oncology because family members often come, and many questions arise. It can take a lot of time to make patients feel comfortable and assure them of their progress or decline in treatment. I prefer to spend my time in the lab, radiation, and the donor bank. The clinic is such an intimate, personal space for most of these patients and I feel like I’m invading their privacy at most times even though this is a teaching hospital. I find myself empathizing more with patients in this department. Their expressions lead me to believe they feel intimidated having multiple people in the exam room. It seems to give off the impression of extremely bad news, which is not what you want a patient facing a life threatening illness to feel like when they are already vulnerable fighting for their life.
Week 6
The final week of the rotation was spent in various departments from radiation, to clinic, to the stem cell laboratory. In previous weeks we have seen the harvesting of bone marrow stem cells; this week we got to observe a patient being given the transplant. The stem cell mixture gets warmed to body temperature and fed through an IV into the patient. The technicians informed us that the media mixed in with the stem cells causes nausea in the patients. Nurses have them eat hard candy during the process. It was interesting to observe the whole transplant process, from the donation to the cryopreservation, ending with the recipient. The week went by very fast! I am very appreciative to have experienced a clinical immersion with such a welcoming department. The staff alone has made me feel comfortable in the clinic and the lab, enlightening me with stories and techniques. It’s always hard to end an internship, helping the staff and feeling like you’re making a difference makes it all worth it. In both of my rotations I have experienced incredible doctors and compassionate nurses and technicians. They seem to have a great amount of patience and such a drive to help people. Surrounding myself with such an astonishing group of individuals, with a passion for patient care, motivated me to want to do the same with medical devices. In previous school assignments where we were instructed to create a device or solve a problem, I never thought of the impact it would have on patients, and how they would perceive it. I am most grateful to have a new outlook on the design process. I’ve always found myself to be a very empathetic person, and working with patients brought that out in me even more. Additionally, from this experience, I hope to bring the knowledge I’ve gained to IPD. I envision myself designing medical products not only from an engineering standpoint, but from an empathetic designers view as well. I would like to create medical devices that are comfortable to patients and easy to operate for doctors. I am very thankful for the opportunity to immerse myself in a clinical environment throughout one of the largest teaching hospitals. I’ve experience a lot of doctors and staff take interest in the path id like embark on after graduation. Many of them pushed me to try observing different specialties throughout the departments, which turned out to be another great learning experience. They were even interested in me as a person, and what I’d like to take away from this experience and where I’d like to apply it. It’s rewarding working with people who take the time to invest themselves in you, and make sure you gain the complete clinical and surgical experience. I think I would have preferred doing three, two week rotations and viewing another department, but I am thankful in general to have seen one, let alone two. Overall, I didn’t know what to expect when I walked into the clinical for the first day. Everything has surpassed my expectations, and I couldn’t be more excited to apply what I’ve learned to my future endeavors. Being immersed in the clinic has not only helped me to grow as an engineer but as an individual.
