Students
Ossama Anis Heading link

A bioengineering student who is excited about this opportunity in the Clinical Immersion Program in order to further my knowledge in a clinical setting. I look forward to determining the needs in which us bioengineers can enhance the technology and equipment utilized in the medical field in the most innovative ways. Keep up with my blog to witness my adventures in Interventional Radiology (IR) and Orthopedics!
Ossama Anis Blog Heading link
-
Ossama Anis Blog
Interventional Radiology: First Blog Entry
Ossama Anis Blog
Monday, July 6, was the first day of our participation in the Clinical Immersion Program. My partner Wali and I were given the opportunity to observe the Interventional Radiology (IR) department of the University of Illinois Hospital. The first few days of the program definitely lived up to my expectations. Dr. Bui and the rest of the radiology staff were all nice and extremely welcoming. The staff members introduced themselves and explained things to us in between surgical procedures. The doctor himself was very calm when conducting his daily rounds. He also communicated and explained the procedures while he was performing them.
On the first day of the program, my partner and I were able to observe Dr. Bui performing a biopsy on a patient. An ultrasound was utilized to locate the tumor using sound pressure waves to create an image. Dr. Bui used a biopsy gun to extract a tissue sample from the given location. This biopsy gun is shown below followed by the extraction process.
The gun is inserted into the determined location. Once it is placed into the tissue, the trigger is pulled and the tip is released, the space between is sliced, clutching onto the desired sample.
Following the biopsy, we went to observe another case. Here, we were instructed to stand outside the room due to the fact that we were not wearing lead around our chest and waist while the x-ray machine was in use. Dr. Gaba, another physician that works in IR, revealed to us how chemotherapy is performed. He had two syringes containing two different substances. A syringe containing a concentrated chemotherapy medication is mixed with the contents of another syringe that contains a lipid-based solution using a simple connector (shown below).
After the two solutions were properly mixed to create an emulsifier, the doctor injected the mixed solution into the hepatic artery of the patient by way of a catheter. The patient showed signs of some pain and discomfort after the time of injection.
I made quite a number of observations while shadowing in the OR. We went into the OR where a number of physicians and nurses were stationed. The machinery is covered in disposable plastic sheets so that it does not get contaminated. I noticed there was a table that was prepped and sanitized. On it, we could see surgical tools, petri dishes, and a number of syringes. In the OR, the doctor observes a monitor that displays the most ideal version of the designated area in order for comparison. The doctor seems to have multiple monitors at his disposal. These monitors often times display the x-ray images of the area being treated. The nurses are ready to assist the doctor instantly and a few medical students are also watching the procedure. I noticed the tangled mess of electrical cords on the OR floor as this could be very hazardous.
My initial experience in the Clinical Immersion Program proved to be highly enlightening. Not only do these doctors handle the most delicate of procedures with complete ease, but they are eager to teach us bioengineers everything we need to know about the technology and equipment used along with the procedures being conducted. After day one, I’ve become very comfortable with Dr. Bui and asking questions at the appropriate times. I am extremely excited to learn more and looking forward to all the different experiences this program will bring.
Week One continued…
Ossama Anis Blog

The first week, my partner and I observed Dr. Bui performing a radiofrequency ablation procedure. This medical procedure ablates the tumor or other abnormal tissue using heat produced from high frequency alternating current. Dr. Bui used a Starburst Talon Device in order to destroy the tumor located in the patient. An ultrasound was utilized to locate the tumor in the liver. The Talon device was driven into the liver and the distal end of the device was placed directly in the middle of the tumor. After that, the four talons sprung out and each of them were heated to a temperature of 105° C. The device was held in place for nine minutes in order to destroy the tumor cells along with the surrounding tissue. The device shown below displays the temperature readings situated in a circle that represents each prong on the Talon.
My partner and I noticed that the Talon device did not look secure when the physician took his hands off of it. We thought that an improvement to this device would be to further secure it when it is heating and destroying the tumor. However, when addressing this to the doctor, we were told that the four prongs secure the device completely. The pictures below demonstrate the Talon device in both positions, prongs closed and prongs opened.
Another case that my partner and I observed was a patient with pancreatic cancer. Dr. Bui went over this patient’s CT scan while telling us about the biopsy procedure. He explained how he had to have the perfect placement of the needle in order to get a sample and study its’ pathology. The CT scan is performed first to find the correct needle placement. Then, this needle is used as guidance in order to obtain a biopsy sample. This case brought to light the importance of precision and how some cases come down to a matter of millimeters.
An interesting case we saw was a patient that was suffering from deep vein thrombosis. This is a condition in which blood clots reside in the deep veins of the leg or pelvis. Earlier in the day, Dr. Ray, another physician, had briefly spoken to us about filters that they place in a patient’s abdomen to assist with this condition. Filters are placed in the inferior vena cava (IVC) in order to break down blood clots that travel up from the veins of the leg or pelvis. These filters are vital in preventing blood clots from traveling to the lung or heart as this could result in pulmonary embolisms or even death. An example of this filter is pictured below. These cases brought to light the extreme amount of precision that is required in the clinical setting.
Week Two: Bone Biopsy and Embolization
Ossama Anis Blog

Week two is off to a great start. Observing the daily routines of these physicians is enlightening. One procedure my partner and I observed was a biopsy of the sacrum. The physician began by inserting a needle used for guidance into the back near the iliac crest. He then observed the patient’s CT scan in the axial view in order to assure it had been properly inserted into the sacrum. A drill, pictured below, was then utilized to cut through the tissue and into the bone in order to retrieve a sample. Observations made suggest an improvement in the way data is viewed, as a biopsy may be easier if the CT scan was observed in the sagittal and the axial view simultaneously.
Also observed was a patient with cancer in the kidney. The treatment for this patient consisted of microspheres being injected into the renal artery. This is a minimally invasive procedure in which microspheres block the flow of blood to the kidney. Once the microspheres are injected, they travel with the blood to the network of vessels that lead to the kidney. These microspheres block the blood flow leading to the tumor. This procedure is done in order to prevent growth and encourage shrinking of the tumor. Embospheres are microspheres that are heavily used in interventional radiology.
Embospheres are seen again in uterine fibroid-embolization (UFE). This process, pictured below, takes place when there is a benign tumor in the uterus. In this process, the catheter and stylet are placed into the uterus. Once in the desired location, a contrast, usually organically-bound iodine, is injected to assure the correct placement of the catheter. The embospheres are then injected and used to block the uterine artery in order to stop blood flow to the tumor. Uterine fibroid-embolization is the most common procedure that makes use of these embospheres.
Week Two: TIPS
Ossama Anis Blog
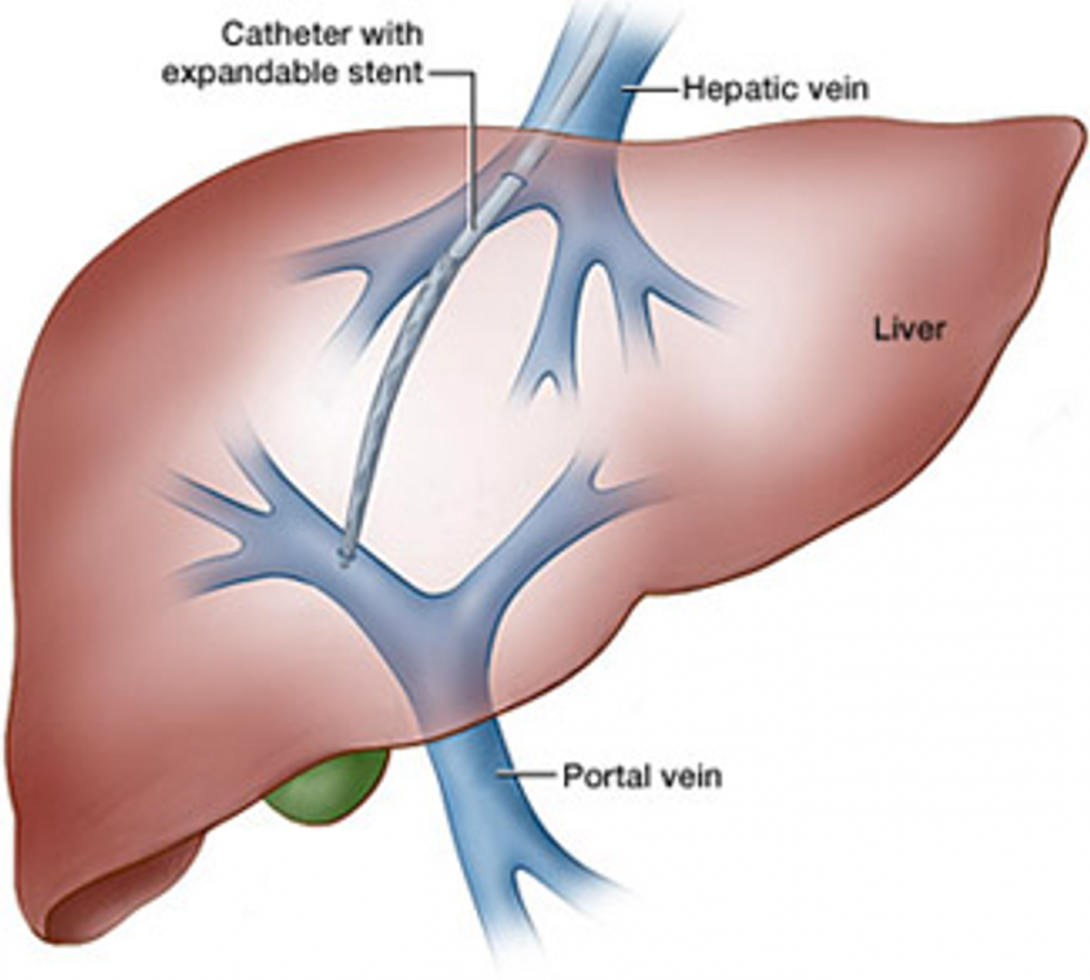
An interesting procedure we observed this week dealt with portal hypertension. Blood flows from the esophagus, stomach, and intestines through the liver. Damaged livers disrupt this flow and cause portal hypertension, which is the elevated pressure of the portal vein. Transjugular intrahepatic portosystemic shunt (TIPS) is a procedure that is used to create a connection between two blood vessels in your liver. The connection of these blood vessels, the hepatic vein and the portal vein, allow for relief of portal hypertension.
The physician conducts this procedure by observing the patient’s fluoroscopy. The patient was on his back and hooked up to heart and blood pressure monitors. This non-surgical procedure consisted of a catheter being inserted into the jugular vein in the neck. Using fluoroscopic visualization, this tube was guided into the portal vein. Once in proper position, the balloon was inflated to a specific pressure in order to dilate the path between the hepatic and portal veins. The physician then connected the portal vein to one of the hepatic veins. This connection relieves the portal hypertension. The pressure of the portal vein is observed using a pressure wedge in order to confirm the declination of pressure in the portal vein, thus declaring the procedure a success. The new pathway allows for blood flow to be regulated while easing the pressure on the organs involved.
This week has been a blast and I am looking forward to my final week in IR!
Week Three: PCN and Ureteral Stent
Ossama Anis Blog
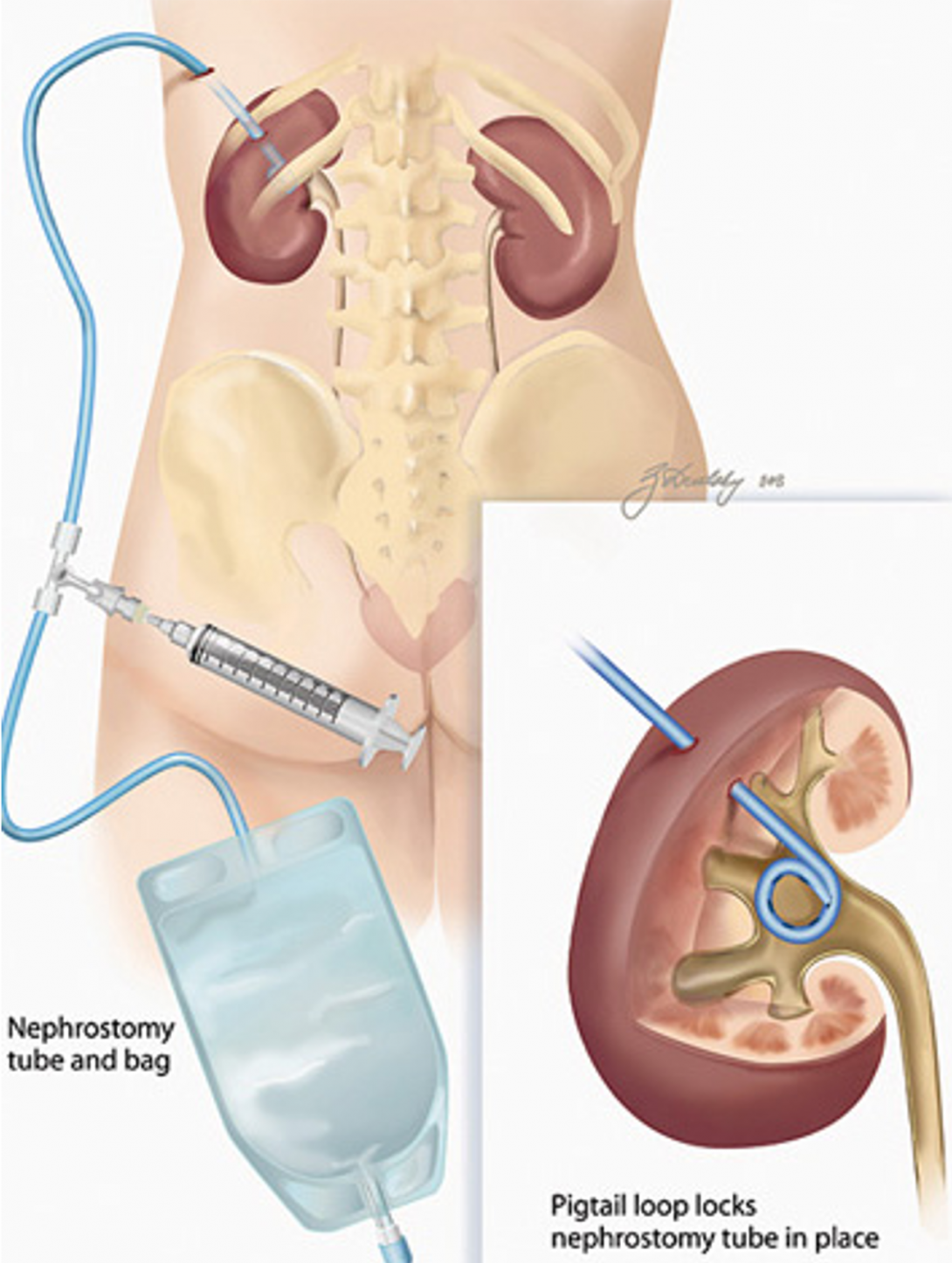
In the third week, Wali and I witnessed a physician perform a percutaneous nephrostomy (PCN). This procedure consists of gaining access to the kidney by placing a tube through the skin of the patient for drainage purposes. The doctor informed us that this procedure is often used to relieve the kidney of urine overload. In this procedure, access to the kidney for a catheter is granted percutaneously by using fluoroscopic guidance. After reviewing the patient’s medical condition, antibiotics were administered prior to the start of the procedure. The patient was sedated during the placement of the catheter.
To begin the process, Lidocaine was injected in the patient’s back near the kidney using an ultrasound as visual guidance. This needle is used as a guide for the placement of a nephrostomy tube, a specific catheter that travels from the incision to the kidney. After insertion, the stylet was removed, allowing for free flow of the renal tract. A drainage bag attached to the catheter was utilized to collect the urine.
Another interesting case that we witnessed was a ureteral stent placement. This was performed on the first pediatric patient we have seen thus far. Due to a blockage in the ureter, there was an accumulation of urine in the kidney. A ureteral stent is a thin tube that allows urine to flow from the kidney and into the bladder. This stent is placed temporarily to prevent damage from occurring to the kidney. After the procedure was complete, we sat down with Dr. Ray and discussed the complications with this case. He explained how the ureteral stent was difficult to see under fluoroscopic guidance. For that reason, excess radiation was emitted to the patient in order for the physician to determine the location of the stent. We then discussed how coating methods may improve the visualization of the stent when using a fluoroscope.
Week Three: End of IR
Ossama Anis Blog

This week, we observed a chest port removal, a procedure which calls for anesthesia. This device is installed in the upper chest underneath the skin. A catheter is used to connect the device to a vein in order to administer medication. The modern ports, pictured below, are easier to remove and have two septems so they can be used twice as long. One of the physicians informed us that each septum can take about 2000 injections. Under the guidance of fluoroscopy, the interventional radiologist makes a small incision and removes the device. These ports are used for chemotherapy and hemodialysis as well as a variety of other uses.
We also witnessed a transjugular liver biopsy. The physician uses ultrasound as guidance and makes a small incision in order to insert a catheter into the jugular vein and into the liver. A biopsy needle is inserted in order to retrieve a tissue sample.
Interventional Radiology has been enlightening as to how important technology and imaging can be in the medical world. Thank you to Dr. Bui and the entire IR department for teaching us so much and making us feel welcomed! This experience is unforgettable and invaluable as it has opened my eyes to much of what is done in hospitals and things that could use some improvement.
Week Four: Orthopaedics!
Ossama Anis Blog
My next clinical rotation is in orthopaedics which has been very interesting thus far. I originally thought the department would be bombarded with surgeries, but Tiana and I haven’t seen any surgeries so far. Instead we shadowed Dr. Gonzalez, Dr. Shmell, and a couple residents in the clinic.
I definitely had more exposure to physician and patient interaction in these past two days than I did throughout my entire rotation in interventional radiology. It is a pleasure to see how Dr. Gonzalez diagnoses the patient and develops different treatment plans according to the patient’s lifestyle. I noticed him asking patients personal questions like where they work, if they lift heavy objects, etc.
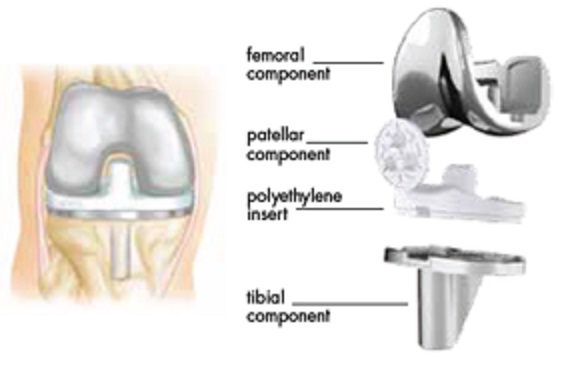
In between appointments, Dr. Gonzalez showed us an x-ray of a patient with a knee replacement. It consisted of two metal pieces, one attached to the femur and one to the tibia, and a wedge to diminish issues in between the two. He informed us on the issues with the wedge wearing away due to the excessive shear stress between wedge and the knee replacement. I noticed that the wedge is a darker shade of grey compared to the rest of the knee replacement obviously telling us that the material of the wedge is less dense than the counterparts.
One interesting case was a patient who came in regarding pain in his hand. The doctor said his hand looked like he had broken it a while ago because the bones in his hand were deformed. The patient then remembered that he may have originally broken it 10 years ago.The doctor informed the patient of the details about the procedure necessary to gain back the flexibility in his hand. It consisted of making an incision, breaking the deformed bones, taking some bone from the ilium, and screwing it all together. The doctor also said the hip may hurt more than the hand right after surgery. Another possible treatment is to take out the bad bone and bring the rest of the bones together. The fallback with this route is that it will take away 50% of the wrist’s mobility. The doctor said he has already lost about 50% for waiting a decade and causing a deformity.
On Tuesdays, we are to report to the 14th floor of the Crain Communications building, which is a skyscraper with a beautiful view of Millennium Park and the lake. On the first day, we met with Dr. Gonzalez and he took us out for lunch at The Gage. That was really nice of him, plus they had delicious food! Afterwards, we continued the day by going back to the clinic to attend to the rest of the patients. I am really enjoying orthopaedics so far and excited to observe surgery later this week.
Week Four: Joint Implants
Ossama Anis Blog

By the end of this week, we have seen a few surgeries in orthopaedics. The first procedure we observed was a total knee arthroplasty which consists of installing an artificial knee replacement. Many of the tools used, along with the knee replacement, were from Smith & Nephew.
The knee alignment device was positioned onto the lower leg to assure correct alignment before the cutting took place. A saw was used to shave off part of the proximal end of the tibia along with the distal end of the femur. A temporary knee replacement was used to help further assist the doctor with guidance for cutting, pinning, and drilling. Once the bones were carved to the correct shape for the knee replacement, cement manufactured by Stryker was applied. This acts as a glue between the bone and the knee replacement. Finally, the knee replacement was carefully inserted into the path created. Saline and Betadine were poured into the exposed knee and the opening was then sewed shut.
Rheumatoid arthritis is a chronic inflammatory disorder that causes pain and problems in the joints of the hand, sometimes requiring reconstructive hand surgery. Another case we saw dealt with a metacarpal phalangeal (MCP) joint prosthesis. The physician informed us on a scholarly resource that we can use to further explain details about this procedure and the equipment it requires. During this procedure, the physician removed the damaged joint and implanted an artificial joint made of silicone rubber. The implants have a stem that gets inserted into the bone on each end and a spacer in between the two components.
An incision was made on the proximal side of the knuckles. Then, part of the metacarpal and phalangeal bones were cut down using a saw. Afterwards, the joint was aligned and prepared for the installation of the implant. Trial implants were tested for size. Once the correct size was established, the stems on each part of the implants were inserted into the specified bones. The wound was treated with saline and antiseptic solutions and then sewn up. This procedure helps many rheumatoid arthritis patients who have deformities to their conditions.
People weren’t joking when they described orthopaedics as human carpentry. I noticed bone particles flying in the air when the saw was being utilized. I had a great first week in orthopaedics and can’t wait to see what else is in store for the final two weeks!
Week Five: At the Clinic
Ossama Anis Blog
During week five, a patient came in complaining about knee pain and how it got worse as the day went on. The doctor wanted to do a knee replacement but had concerns about her being overweight. Dr. Gonzalez then informed the patient of her BMI and the correlated data that has been accumulated, illustrating complications. These occur during total knee arthroplasty when the BMI is over 40. Blood clotting and infection are a couple of those complications. Since her BMI was right below 40, the surgery was scheduled to be in the first week of September.
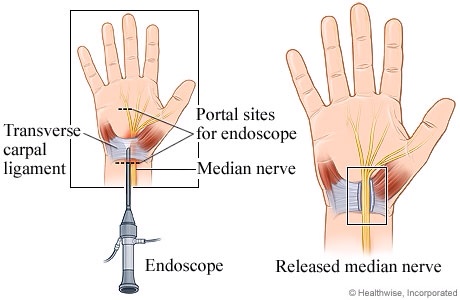
I noticed quite a few patients coming in regarding carpal tunnel syndrome. One, in particular, had a carpal tunnel reoccurrance due to the scar tissue that formed after the first surgery. This patient’s immune system produced more scar tissue than usual, thus resulting in the compression of the median nerve.
This syndrome occurs when the transverse carpal ligament presses down on the median nerve. The transverse carpal ligament holds the tendons and nerves in the hand together. However, after the surgery, the scar tissue replaces that function. A resident explained to us how Dr. Gonzalez performs surgery in order to relieve symptoms of carpal tunnel syndrome. First, an incision is made and using endoscopic guidance, the transverse carpal ligament is cut with a small knife that is attached to the endoscope.
I’ve become really comfortable in the clinic atmosphere and having a great time learning something new every day.
Week Five: Knee and Hip Replacements
Ossama Anis Blog
By the end of this week, we observed three knee replacements and one hip replacement. The procedure for all of the knee replacements were done very routinely. First, an incision about 5 inches long is made and the patella is placed along the lateral side percutaneously. After aligning the tibia with a device called Knee Align, they screwed and pinned a slotted cutting guide. This guide contains a small slit where the saw is placed to create smooth, leveled surfaces. Once the tibia and femur were properly trimmed, trial components of various sizes were inserted to determine the correct size for the patient at hand. Dr. Gonzalez has experienced complications with the patellar component of the prosthesis, therefore he keeps the real human patella in the patient. Cement is used to adhere the prosthesis onto the bone, and the wound is then cleaned up and either stapled or stitched.
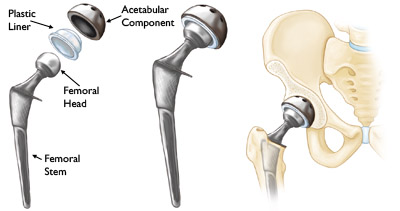
I was excited to watch the total hip arthroplasty since we haven’t watched it yet. Initially, an incision was made, about 4 to 5 inches long, and the femoral head was removed. Similarly to the knee replacement, trial components, from Depuy (a Johnson & Johnson company), were inserted to determine the correct size prosthesis. A plastic liner is used to separate the acetabular component from the femoral head in order to avoid contact between the two metals. Afterwards, the cut is sanitized and sealed.
The one day we had in the OR this week consisted of repetitive procedures. I wish we had at least two days observing surgery rather than one to allow for more exposure to the vast amount of cases and equipment this department has to offer. Although the clinic allows for much observation on physician patient interaction, the OR holds more of the knowledge bioengineers need to identify possible improvements.
Week Six: Last Week in Orthopaedics
Ossama Anis Blog

During my last week in orthopaedics, we followed up on a patient that came in two weeks ago concerning a fracture in her intermediate phalangeal. After taking a look at the x-ray, Dr. Gonzalez knew that the patient was going to have to undergo surgery. Since the patient did not come to the doctor immediately, the bone began to heal out of place. The surgery for this condition consists of making an incision, breaking the incorrectly healed phalangeal, aligning and placing the bones in correct form, securing the bones with a couple of screws, and finally sanitizing and stitching it all together. Surgery is necessary in order to prohibit the bone from healing incorrectly. Such conditions can interrupt the tendons and wear away the cartilage near the bone.
The patient in this case came in today for a follow up. Her surgery was last week. She is due to get her stitches removed about 2 weeks after the surgery. She is scheduled to keep a cast on for 6-8 weeks. The doctor instructed her not to lift weights because she will not have a good grip and may fall.
After shadowing physicians in this department, it is clear that they act conservatively. When a patient comes in regarding pain in their joints, the doctor tells them to attend therapy for 6-8 weeks. If they come back with pain, a steroid injection is administered. However, this only relieves pain temporarily. Injecting a steroid also has bad side effects such as wearing of the cartilage. Surgery is the final option physicians take when evidence and complaints indicate the patient is still in pain.
The last day in the operating room was exciting because we finally had a chance to observe a carpal tunnel release. After an incision was made near the wrist, an endoscope was utilized to tunnel under the skin in order to cut the transverse carpal ligament. The endoscope was one of the most technologically advanced components of this department. Usually, we see a lot more mechanic tools so it was nice to see some advanced equipment finally being utilized.Our time in orthopaedics is almost over so I’m glad we have been able to witness a variety of common procedures such as carpal tunnel release.Final Blog EntryOssama Anis Blog

My rotation in Orthopaedics came to a close along with the Clinical Immersion Program. I am extremely pleased with the vast amount of knowledge I have acquired in just six weeks!
On Thursday, our last day in orthopaedics, we were scheduled to watch a few surgeries, with a majority of them being hand procedures. The last case we observed in the orthopaedics OR consisted of a patient dealing with an infection in the hip. Dr. Gonzalez and the residents had to remove the original implant and insert an antibiotic spacer that releases a high dose of antibiotics into the joint and the surrounding tissue. A new prosthesis can be placed into the patient once the infection has cleared up. This individual may be more prone to a reoccurrence of an infection.
During the Orthopaedics rotation, we had a great deal of exposure to patient physician interaction. It was interesting to see how people had different pain tolerances. The doctor always wanted to start with therapy, followed by cortical steroid, and surgery if needed. Shadowing the doctor at the clinic was both interesting and enlightening. Each day he tended to about 20-80 patients, all with a wide range of symptoms and conditions. The other aspect of this rotation was in the OR and dealt with mostly invasive procedures. Here we observed all the different tools used, implants, and a wide range of procedures on various parts of the body. Orthopaedics was a great opportunity to get exposure to both clinic and OR aspects.
My time in Interventional Radiology was spent almost entirely in the OR. The ORs of the my rotations were very different. The orthopaedic OR consisted of highly invasive procedures while interventional radiology made procedures less invasive by using imaging modalities. Both departments have their pros and cons while their appeal depends on what an individual prefers to observe. Both rotations gave me invaluable knowledge in the clinical setting. There are many problems in the medical world and this program helps identify which problems need to be addressed and the severity of the need to find the solutions to those problems. Being in the OR gives more opportunities for engineers to observe the equipment, tools, and devices used. This kind of exposure and thought process allows to help further identify complications and possible solutions.
Thank you to Dr. Kotche and everyone involved for providing us with this amazing opportunity and unforgettable experience.
Jagan Jimmy Heading link

I am an bioengineering undergraduate student at UIC. Luckily enough, I was able to be part of the Bioengineering Clinical Immersion Program this summer. Through this blog, I will be able to share my experiences as I rotate through the Urology and the Hematology/Oncology departments over the course of the next six weeks.
Jagan Jimmy Blog Heading link
-
Jagan Jimmy Blog
Scrubs!
Jagan Jimmy Blog

Upon going up to the third floor of the main hospital building, we were asked to change into scrubs and to put on a head and shoe cap just like everyone else there. After having done as we were told, with a pen, a clinical immersion notebook, and our cell phones we stepped out in to the hallway. Stepping out of the locker room immediately left us in the middle of the intersection of two main hallways where the OR information desk was located. The young lady at the desk, with the deep and serious expression, seemed tired and stressed. It wouldn’t be a surprise for anyone sitting in her position to be tired and stressed because she had two large monitors on her crowded desk, and numerous people approaching her for information. One of the screens was evidently reporting the status of all the operating rooms. The information about the department occupying the OR, the attending in there, and the procedure, among other color-coded information seemed to be displayed on it. On that single floor based on the screen alone, there seemed to be about 19 operating rooms. The second screen in front of the lady seemed to be where she is making appointments and such.
Nonetheless, upon asking in which ORs where the urology department operating, she quickly gave us two OR room numbers and resumed her work while answering about at least 2 people at the same time. Through the relatively crowded hallway we stumbled upon the first OR. An extremely small packed room. We knew it was the right place because peeking through the rectangular glass window of the door we could see a room half filled with machines and the other half filled up with people. The doctor seemed to be working on a female patient while various curious faces of medical students hoovered around observing the procedure. Since there were practically no room in there, we decided to check out the second OR the lady at the information desk told us. While finding the second OR, I couldn’t help but notice the amount of people passing through the hallways, some rushing through, some pushing huge medical devices I have never seen before, some with large carts full of OR instruments, and some just hanging on the sides for a small chit chat.
When we reached the second OR, there were no patient or doctor to be found in there, but instead only a few surgical nurses and a nurse anesthetist were present there. Upon chatting with them a bit we learned that a surgery had just finished and that they were prepping for the next patient that would be brought in within an hour or so. The patient would have been in the OR sooner, however they seem to have ingested some food thus had to wait for complete digestion of the food. Nevertheless, one of the nurses was kind enough to show us various machines in the room and their uses, she was willing to do so because the sterilized tools for the next surgery had been put out already thus by standard protocol a nurse has to be in the room to ensure that the sterilized wouldn’t be contaminated. An interesting term I heard from her as she was pointing out the various equipment was “energy devices”, which turned out to be surgical tools and machines that make use of some degree of current. A picture of the OR in which the nurse introduced my partner and I to the various equipment is shown here.
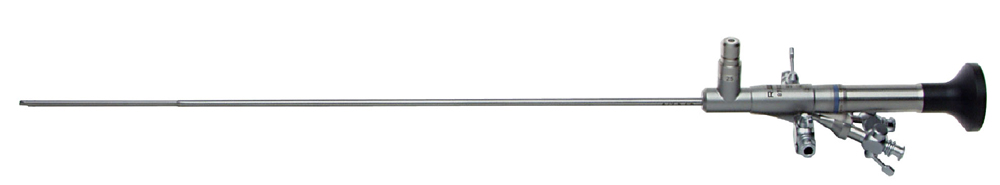
After our conversation with the surgical nurse, we returned to the OR we visited first. Thankfully, enough the surgeons and the medical student were standing outside because the x-ray technician had just brought in the x-ray machine and was setting it up. Meanwhile, we seized the opportunity to introduce ourselves to the medical students, residents, and the attending physician. The resident conducting the operation told us to come in to the OR, which would be about half of the size of the OR pictured above yet with almost all of the same equipment. However, in order to enter we were required to wear a leaded vest in order to protect ourselves from the radiation. Since the procedure being carried out at that point was a stent placement in the ureter to remove a kidney stone, which is a common procedure, some of the medical students didn’t bother to re-enter the OR, thus leaving my partner and I sufficient room in the OR to observe the procedure. The operating resident was using a resectoscope for the procedure, therefore the entire process was completed by looking at the visual provided by the camera on the resectoscope.
Following the procedure, most people in the OR moved to the larger OR that we had explored. This time an elderly gentlemen was brought in for a procedure known as Transurethral resection of the prostate (TURP). Given that it was a larger OR, it allowed a better view of the procedure and space for general observation. The case being operated was simply that there was a significant amount of scar tissue formation of the prostate gland around by the portion of the urethra that is close to the bladder. The scar tissue lead to obstruction of urine flow, which results in the buildup of the urine in the bladder; the buildup of urine could lead to further sever complications if not dealt with soon. The operating resident used a resectoscope to find the point of obstruction by inserting the resectoscope through the urinary meatus and sliding it through the urethra. The resident used the resectoscope to cauterize and remove the excess tissue gently and cleared the urethral pathway. The scarring was said to be due to the previous urological surgical procedure that the patient underwent. Nevertheless, while clearing the obstruction a few staples were found to be loosely hanging on the urethral wall – I found this to be interesting yet strange as I didn’t understand why they were placed in that part of the body in the first place. With that the, the resident finished up the work and was able to schedule the patient to leave home in the evening.
With the TURP procedure our first day in the OR came to an end. I was shocked to find that the surgical atmosphere was quite crowded in terms of the tools being used and the number of people involved in the procedure or simply observing. Nevertheless, it was an eye-opening experience to not only know the kind of task surgeons do on a daily basis but to also learn about the vast amount of surgical tools that have been engineered to make the surgical procedures minimally invasive and the safest.
I will be sharing with you more experiences from the OR and the urology clinic in my next post that will be posted within a day or two.
The remainder of the week
Jagan Jimmy Blog
The remainder of the week held even more exciting events than the first day. So far the schedule for the urology department is such that on Mondays, Thursdays, and Fridays are OR days when surgeries are performed. Tuesdays and Thursdays are clinic days during which the surgeons, residents, and medical students are all in the clinic and see patients while doing some minor procedures. The weekends are off days for the surgeon, and only emergency cases are attended to. Currently, the urology department is experiencing some technical difficulty seeing patient properly at the moment since they are relocating their clinic to a bigger building. Since the examination tools and other procedural tools haven’t been transferred to the new location the physicians simply sees patients on Tuesdays at the new location, and meet patients scheduled for simple procedure at the old location, where the tools are at. So Wednesday was more engaging and eventful that Tuesday. The old location that currently houses much of the department’s equipment is adjacent to the hematology/oncology clinic. An observer can easily see that because the two departments shares the clinic, the waiting area and the surroundings of the clinic are quite crowded.
While at the clinic we primarily just observed two procedures: cystoscopy, and transurethral biopsy. However, before I share an account of witnessing those procedures, I would like to share the insight we gained from the nurse working there. One of the male nurses at the clinic was generous enough to give us brief overview of the working of the clinic. He said that typically once a patient comes in they have to wait quite a while in the waiting area before bringing them in so that the nurse may prepare the procedure room. Note that these patients are the ones that are at the old locations where the department’s procedure tools still are at; therefore, the patients who came there already had an appointment. Once the nurse bring the patient to the procedure room, usually they give a brief overview of the procedure that is about to be done and addresses any concerns of the patient. Soon enough the patient is left to change in to a patient gown that’s more appropriate for the procedure. Then typically the patient waits there for anywhere from 30 minutes to an hour and sometimes more because they may be only one attending at the clinic. Since all patient seeing must be overseen by an attending, the resident cannot see the patient alone. Thus, during the long wait time the patient is usually left alone in the room, while the nurse checks in on them.
Another interesting observation that we made while we were there was that given the diversity of the area in which the hospital is located at, often the patients who comes in are not fluent in or doesn’t entirely speak English. In such cases, an interpreter is requested for the appropriate language. Having an interpreter present is an excellent choice since the patient wouldn’t feel so isolated and alone in the room among stranger; however, the drawback of it is that it can be time consuming because the interpreter needs to translate the doctor’s words and those of the patient. Nevertheless, the communication between the physician and the patient without the interpreter would be even more time consuming.
As mentioned above, the main procedures we observed were cystoscopy and transurethral biopsy. The resident (Dr. Tony) who carried out some of the procedures was helpful in explaining the procedure and the tools being used. Cystoscopy is simply an examination of the bladder. The procedure is done using a cystoscope. The biopsy was performed to obtain samples of the prostate to check whether the enlargement of the prostate was cancerous or not. In order to do so, an ultrasound probe was inserted into the anus of the patient to locate the spot. The ultrasound probe had an accessory that allowed the biopsy needle to be inserted and the ultrasound image shows where the needle is in relation to the prostate and from what angles to get the samples. An unfortunate need the nurse expressed is that the ultrasound probes are only available in the clinic in one size. Thus, for some patient the size of the probe can be a bit uncomfortable and painful.
Then during the last two surgical observation days we were able to observe some mind-blowing surgeries. One of the surgery was an explorative laparotomy. The patient was an elderly woman. The patient renal condition was critical because the right kidney was non-functional, and the left ureter being obstructed. Therefore, the previous surgery had connected the right ureter to the left kidney. However, due to the distance between the two parts the right ureter had two sharp turn to make before passing the urine into the bladder. Thus, the surgeons decided it is best to remove a portion of the bowel and create a ureter using that portion, and so they did. While doing so a tool that they used frequently is a sealer/divider. Basically a scissors that staples the edges of the two sides it cuts through to prevent bleeding. Nevertheless, the surgery took up almost the whole day because the surgeons took about 2 hours to simply cut into the peritoneal region due to many adhesions formed from previous surgery. Then it took them about an hour to properly reach the left kidney and locate it – the difficulty was primarily due to lack of visual. Once having done so they proceeded with the plane mentioned above. The surgeons were on their feet for about 7 hours until the urology surgeons could transfer the patient over to the general surgeons who dealt with the patient’s abdominal hernia.
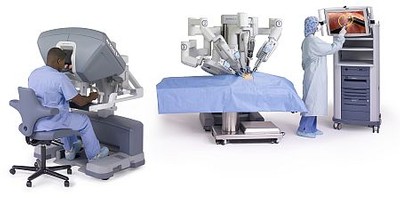
The following day we were able to see an adrenalectomy and partial nephrectomy carried out on a patient, and a prostatectomy on a second patient. What made these two cases quite exciting was the fact that they were both carried out by robotic laparoscopy. The Da Vinci robot is truly a magnificent device. In either case the surgeon made incisions on the patients and simply inserted the robotic arm with the tools that he would need while conducting the surgery. Often a resident would also be holding a tool laparoscopically so that they may practice the procedure while the robot (controlled by the attending) do the main portion of the surgery. The two main issues I have encountered are that because the attending sits at the control console of the robot that’s in the corner of the OR, while the resident with the manual probe/tool stays by the patient it is often a bit difficult to communicate between them due to the noise in the environment. Another flaw is that the da Vinci robot while being cutting edge technology fails to provide haptic feedback to the user. Inclusion of haptic feedback could in essence replicate the sense of touch the surgeon would have during open surgery.
With that, I’m going to stop the blog because to provide the fullest detail of the surgeries and the clinical procedures we observed would be a much longer post.
Note* the picture attached to this post is that of the Da Vinci robot. The picture I took which I wanted to upload seems to be too large such that I am unable to upload it.
Picture source: http://middlesexhospital.org/images/dmImage/StandardImage/450-da-vinci-system.jpg
Week 2 – First Half
Jagan Jimmy Blog
Week two of the clinical immersion in the urology department started out with even more surgeries for us to watch. I was able to observe placement of a suprapubic catheter, two lithotripsy procedures, and a circumcision. The suprapubic catheter was placed because the elderly patient was unable to have a catheter placed in her urethra. An odd act I noticed was that the attending physician was checking the placement of the catheter manually and ensuring it was in place without having a sterile gown or gloves on. This may be due to the fact that the procedure overall is a simply one, where the catheter is directly inserted into the bladder through an incision in the abdomen. The main downfall of having the procedure done is that the catheter is required to be replaced once every month and the abdominal incision remains open so long as the suprapubic catheter is in place.
The lithotripsy is a procedure by which kidney stones are broken into smaller pieces using sound waves and then removed from the urinary system. In either case of lithotripsy it is standard to use a holmium laser – a laser that emits sound waves at a specific wavelength. One of the procedure had to use laser in order to crush the stones, however the other one didn’t require the use of the laser. The second lithotripsy didn’t require the use of the laser because the kidney stone descended down the ureter quite easily since the patient had a stent placement. The medical student informed us that usually in cases where the patient already have a stent placed in the ureter it is most likely that the stone will descend and not require the laser. Which made me wonder whether if such an occurrence is quite common then isn’t it a lot more efficient to hold back from opening the sterile container containing components of the laser once it use has been ensured. Additionally, the attending mentioned that with the various scopes that they use, whether it be cystoscope or a ureteroscope, the ones that have good flexibility are the thin ones however the weaker the irrigation capabilities and vice versa for the thicker probes. Nevertheless, the adult circumcision procedure that followed was quite straight forward. The procedure is primarily done using the traditional tools with the exception of using a cauterizing tool to remove the foreskin and stop the bleeding.
Then during our time at the clinic, which unfortunately isn’t as exciting as the OR, we were able to observe some patient-physician interaction. However note that the new location of the clinic, which was supposed to be fully equipped and functional by the first of this month, still lack the equipment to do the procedures. Nevertheless, the prior to the physician seeing the patient the medical students and/or the residents goes in and collect information from the patient and reports it back to the attending. Patients who have been with the UIH system has all their information available readily and structured in the Cernet system. However, patients with documents, scan results, etc. from clinical environments outside the UIH system has to bring it in with them and isn’t automatically transferred. For example one of the case we observed was that of an individual in their mid-forty. They had to carry around their CT scans throughout on a CD. I didn’t understand why the resident who collected the patient information didn’t simply upload the CT scan images under their name. Moreover, an interesting thing I noticed is that it took a while for the computers to load the CT scan results because there were hundreds of pictures. Had the clinic had computers with the latest high-speed processors I am sure the time to load imaging results (which are usually large files) can be decreased a lot. Lastly, one thing I noticed is that the doctors doesn’t seem to be the best at providing emotional care for the patients. It may be because that the doctors I observe are surgeons specialized in urology and they usually simply deal with surgery. But there does seem to be a lack of empathic connection between them.
Tune in for my experience with seeing two robotic surgery back to back and more in the next blog post. I have attached below a figure of the rigid cystoscope and ureteroscope so that you may see how the potential capabilities of either tool differs based on its physical structure – the thinner one is the ureteroscope.
More robotic surgeries..!
Jagan Jimmy Blog

The second half of the week is always more exciting than the first half because we get to spend more time observing surgeries. One of the interesting procedures we observed was varicochelectomy. The procedure is about simply the removal of the varicose veins around the testes. Given that it was a microsurgery, only two surgeons (residents) were operating on the patient at a time by using a microscope. The attending present at the surgery was generous enough to narrate the whole procedure. Once an incision of necessary size was made the tissue of interest was brought forward for better visual under the microscope. Under the microscope the operating surgeons examined the tissue to determine which of it were the arteries, veins, lymphatic vessels, and just fascia. This task seemed to be a bit difficult since they often look very much alike. Interestingly, enough they also used a Doppler ultrasound to distinguish between the artery and the other vessels. However, there seemed to be considerable ambient noises that results in the ultrasound being active. Upon further inquiry with medical students, they informed us that the microsurgeries cannot typically be done by robot assisted. Another interesting observation I made during the surgery was that when the sealer/divider ran out of staples, rather than reloading with the staple the entire tool was disposed and a new one was used. I found such discarding to be quite unnecessary and inefficient.
On the same day we were able to observe two more robotic surgeries. The procedures were robotic assisted laparoscopic prostatectomy, and a partial nephrectomy. The unfortunate truth is that having seen these same procedures more than one does start to make the observation less exciting. At this point having already mentioned what the procedures through the earlier blogs I am not going to define the procedures here. However, a few observations I made was that the camera used for internal view often gets smudge on them from the cauterizing, blood, etc. In such cases the camera has to be taken out and removed from the robotic arm and replaced with a different one. In such cases I think it would significantly more important if the camera was self-cleaning or could be cleaned and used again. I have attached here a picture of the resident in action during the robotic laparoscopic prostatectomy, along with the wide array of tools used.
The following day we got to see three more surgeries. The first of which was a cyst urethra extraction – an extraction of a cyst in the urethra. It may be because the patient was a female that the surgeon didn’t have to do the procedure laparoscopically, since anatomically the female urethra is much shorter than that of the male and may be operated on easily. The second one was a transurethral removal of bladder tumor. The procedure was laparoscopic and the tumor was simply removed using a resectoscope. I noted that it would be a bit better if they could adjust the pressure of the irrigation on the scope. Also the bag into which the water that was flowing out of the urethra was collected could have been bigger since there were many instances during which the residual fluid spilled on the floor.
Following that we were able to observer a vesicovaginal fistula repair. The procedure is simply in that the surgeon simply closes the fistula that formed between the bladder and the vaginal tract. It was a bit odd that the surgery had to be delayed by a few hours so that one of the staff could go obtain a special kind of retractor known as the lone star retractor. I have attached a picture of the retractor below. The retractors use is simple such that the tissue may be hooked to a string or cord and latched on the retractor to hold back the tissue.
You really only need one kidney!
Jagan Jimmy Blog
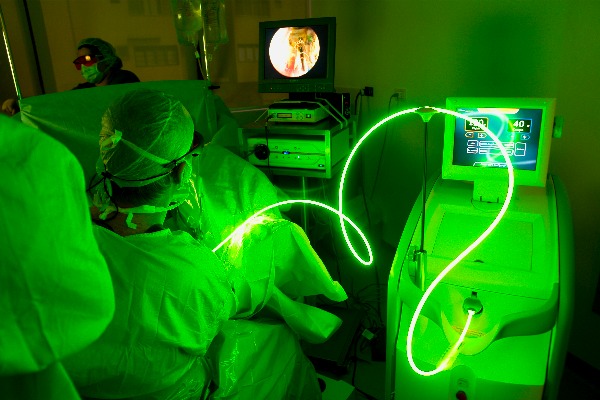
During the first half of the week we were fortunate enough to see a few interesting procedures. The procedures we saw were the vaporization of a prostate tumor, artificial urinary sphincter placement, and a full radical nephrectomy. The vaporization of the prostate tumor was a surprisingly simple procedure. A scope with a laser attached was simply inserted through the urethra and the laser therapy provided by the AMS green light XPS system was focused on the tumorous area. I may include the picture of the procedure if it isn’t too big for the blog to upload (If I can’t upload I will upload an image from online of the laser being used)
After that we were fortunate enough to see a major portion of the artificial urinary sphincter placement procedure. The urinary sphincter placement was for a patient whom we saw in the clinic last week. It was interesting to understand how simple the functioning of the artificial sphincter was. The artificial sphincter has three components to it: a balloon with a fluid, a pump, and a cleft (see image). The balloon is the pressure regulator and a fluid reservoir. The pump acts to move the liquid back from the cleft to the balloon; and the cleft is what encases the urethra near by the bladder neck. The balloon is placed in the lower abdominal region. The balloon will be adjusted so that the regular pressure abdomen (with an empty bladder) will be sufficient enough to cause the balloon to push the fluid it holds into the cleft. As the fluid moves into the cleft, the cleft inflates and pinches on the urethra thus preventing incontinence. In order to void when the bladder is full, one needs to squeeze the pump repeatedly so that the fluid that inflated the cleft may be pushed back to the balloon, which then loosens the urethra and allows for voiding. Due to a delayed resistor system placed in the pump, the cleft is then automatically re-inflated as the fluid moves from the balloon to the cleft. The procedure is a bit complicated due to the importance of the placement of the components of the artificial sphincter. One of the major downside of the sphincter is the liquid that inflates the cuff or the one that is moved between the balloon and the cleft disappears over time. Which means that they diffuse out of the tube, leading the sphincter to artificial sphincter to fail.
Another procedure that we able to observe was a robot assisted radical nephrectomy. The procedure was different from the other nephrectomies that we previously saw because this was the first full nephrectomy we saw. Once again the patient was one who we saw last week in the clinic. Overall, the set up and such is not any different from the other nephrectomies. Once the patient is brought into the OR they are put under anesthesia, then under the guidance of the attending surgeon the patient is positioned to allow for optimal use of the Da Vince robot. First an incision in the region of operation is made and using a scope the internal position of the organs and such are examined and the surgeon makes the decision as to where to make the additional incisions for the robotic arms. There are certain rules about how far the incisions for the robotic arms should be made for the robotic arm to be able to move around once inside. Once the robotic arms were in place the surgery was started out by the resident surgeon by cauterizing and cutting one tissue at a time. The complicated portion of the surgery was having to clip the major vessels such as the renal artery and the renal veins. During the procedure a thick branch of the renal vein began bleeding, and the surgeon had to quickly cut off the blood supply and clip the ends. However, the surgeon couldn’t do this fast enough because the clip applier could only hold one clip at a time and had to be detached from the arm for the nurse to reload it. Nonetheless, after clipping all the major vessels carrying the various fluids in and out of the left kidney were clipped and cut off, and after all the fascia (connective tissue) around the kidney was detached the kidney was bagged. I personally found the surgeons’ attempt at removing the bagged kidney from abdominal cavity through one of the incision to be quite weird. They literally tried to pull out entire bag through a small incision while stretching out the skin. However, after being unsuccessful they had no other choice but to make the incision larger to get the kidney out. To my surprise the kidney they pulled out was quite large. It was about 7 inches in length and its central portion was as big, if not bigger than, my fist. Also, during the procedure one thing I noticed was that the distance between the console and the patient is far enough that sometimes the surgeon at the console cannot communicate properly to the resident by the patient.
So that pretty much sums up the most exciting things we saw during the first half of the week. Look for the next blog to know more about our visit to urology department’s clinic for private patients, and about my overall thoughts on the first rotation.
Voiding from Urology 🙁
Jagan Jimmy Blog

During the second half of the week my rotation partner (Mark) and I were able to visit the University Center for Urology and get a glance at the OR one last time. The University Center for Urology is on the fourteenth floor of the building located at 60 E Delaware Avenue. The clinic is still part of the UI Health system, however it is dedicated exclusively to seeing/serving private patients. From what we saw when we were there, there were only three nurses present at the clinic, and we were told that the clinic only has one attending at a time. While we were there, the attending present was Dr. Ross. As how it was at the other clinic, we were able to observe the two common clinical procedures of performed by urologist: a cystoscopy, and a transrectal prostate biopsy.
The clinic being dedicated to private patients, I had expected the instruments and such of the clinic to be up-to-date with what’s available in the market. However, I couldn’t be any more wrong about making such an assumption. The clinic in fact had instruments that were older and outdated than the ones the outpatient clinic open to the public at the main hospital had. Dr. Ross explained that the clinic doesn’t need the costly newer equipment because the clinic isn’t big enough nor have lot of patients requiring newer equipment. Whereas, the outpatient clinic at the main hospital need newer equipment since more patient is being seen there and the newer models makes procedures a bit easier and faster.
Note that here when I refer to old and new equipment, I am primarily referring to the cystoscope and the prostate biopsy needle gun. The cystoscope at the University Center for Urology is a flexible one however it isn’t high-tech enough to allow to be connected to a monitor and such to display the visual. The user has to look in through the eye-piece at the external end of the cystoscope. Whereas, at the outpatient clinic at the new hospital has cystoscopes by which the user may see the visual enlarged on a monitor. Similarly, the prostate needle biopsy gun used at the former location is a reusable one whereas at the other clinic it is disposable one.
Overall, the environment at the University Center for Urology was quite calming and organized. The patients barely had any waiting time as there weren’t many of them and was never overbooked. Moreover, I think it would do injustice to accounting for our experience at the University Center if I didn’t mention a few words about Dr. Ross. Given the vast experience he has had in the field, he is able to explain thoroughly even the most complicated concepts humbly in simple terms to the patients and students. He is greatly passionate about education and patient care, so that while ensuring the patient’s comfort he also acts as a great teacher by narrating every procedure and encouraging active participation.
Following the clinic we were able to be visit the OR one last time as part of our Urology rotation. During our rotation we say a robot assisted laparoscopic prostatectomy. At this point my partner and I have seen more than five prostatectomies by different surgeons over the past three weeks, and it is safe to say that we know the procedure well enough to provide a general narration. Nevertheless, each time we see the surgery there are different specifics we notice and identify. For example this time around we were noticed that for laparoscopic procedure having suction that is flexible at the tip so that it may be angled to reach certain corners. Whether such suction tool exists for as a Da Vinci robot addition is unknown, however such a tool doesn’t exist for manual laparoscopic uses and could be highly useful.
The past three weeks have shown me how wonderful the realms of medicine and engineering are when they coincide. The rotation has provided me with an in-depth exposure to the hospital areas and settings that I wouldn’t have been able to see, otherwise. I have come to realize the importance of innovative and efficient engineering as the needs for the new instruments and concepts are far great in the general discipline of surgery. Hopefully, one day advanced robots or medicine or an even other convenient forms of treatment may be engineered that’s highly effective, yet minimally invasive to improve health of the people. Nonetheless, it is extremely important to acknowledge the great effort put in by the medical students in the rotation, residents, and the attending surgeons who helped us explore the department and shared their thoughts to make the experience a memorable one. Two individuals I would like to thank specifically would be Dr. Tony Nimeh, M.D and Dr Niedenberger. The former for put up with us and making sure that we are getting a wide variety of exposure and helping us out whenever we were lost, and the latter mentioned for taking the initiative to have urology department in the Clinical Immersion program. Thank you Urology for the wonderful three weeks.
Next up, it’s time to explore Hematology/Oncology and Radiation Oncology. I am excited and looking forward to that rotation.
*Note: To the handful of individuals who take the time out of their day to look over at my blog, I am thankful for your time and attention, and am genuinely sorry for not updating some of these posts sooner.
**I have included here a picture of the cart containing the cystoscope that is pushed around from room to room as needed at the University Center for Urology as needed.
Hello Hematology/Oncology
Jagan Jimmy Blog

As we start the fourth week of this wonderful internship, everyone is starting their second rotation in a new department. I had to wrap up my stay at the Urology department and start exploring the Hematology/Oncology department with a new partner. Unfortunately enough, I was unable to come in on Monday and therefore didn’t get to meet the handful of members at the new department along with my partner. Nevertheless over the next two days I was able to meet most of the staff there and attend a few events such as the research lab meeting, see the stem cell lab, and even do inpatient rounds with an attending and the residents.
I found the research lab meeting to be interesting, however it wasn’t anything out of the ordinary. The meeting had only eight individuals involved (excluding us two interns). The lab meeting reminded me very much that I am used to having with the members of UIC LPPD. Dr. Rondelli talked to each one of them about their research or about the tasks they ought to complete. He spent the most time discussing with Dr. Patel about edits to the figures for a paper they are writing. I found it interesting that even doctors with years of experience as researchers still have to spend a great deal of time making figures for researchers papers a great deal appealing. Moreover, another major portion of the meeting was a discussion with another member there (whose name I did not catch nor could find on the department’s website). Interestingly enough, the discussion between the researcher and Dr. Rondelli was about which of the research, carried out by the former, to prioritize and pursue. Inevitably, despite how cool a topic maybe what would be appealing the most to the investors and the people who fund the research was heavily considered when determining when deciding which area to further purse.
An interesting characteristic I observed about Dr. Rondelli was that from the way he communicates to his peers he seems to be able to get them to do what he sees fit without having to order or demand them to do so. I suppose it is because he possesses such profound leadership skills, along with other skills, that he was able to reach the position of the department director. Asides from that, nothing out of the ordinary took place during that hour. The meeting took place in an extremely small conference room equipped with a large TV with smartboard tools equipped to it.
After that, my partner and I were able to visit the Stem Cell Lab. The manager of the Lab gave us a brief overview of the various tasks they carried out in the lab. While doing so, she also mentioned that the lab is a clinical lab and not a research lab – meaning that they don’t store or in general deal with stem cells of anything aside from humans. Overall, the lab employs three very friendly technicians. While giving us a tour of the lab, we were also able to get a glimpse at the costly aspect of healthcare. She said the usage of various machines in the lab, and even some of the lab equipment are simply too expensive to be affordable by the patients who the UI health system serves.
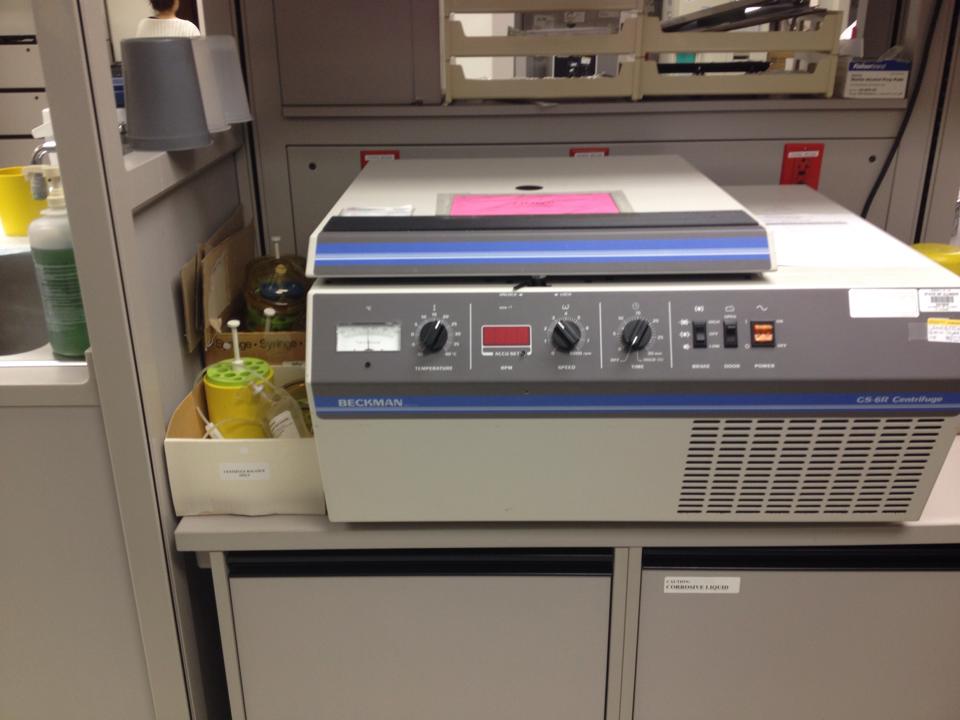
Nevertheless, during our visit we were able to observe the cryopreservation process of a patients stem cells. The sample blood collected was centrifuged altogether in a huge centrifuge machine. In order to prevent the bag with the blood from being thrown out of the machine another bag of equal weight with water needed to be placed opposite to the machine. Once the centrifuge process is complete the bag with the blood is taken out, which at this point has various levels of blood content separated. Based on the total amount of sample collected the lab tech has a way of calculating how much of the platelet should be taken out and how much freezing mixture should be added to the sample. Meanwhile, another lab technician also took a sample of the blood and viewed it under the microscope with a blue dye applied on it in order to calculate what percent of the cells are viable. If the cell is dead its membrane becomes weak and allows the dye to perfuse into it, which then shows up as a blue circle under the microscope. The live cells then would appear as non-blue circles under the microscope. Nevertheless, the technician carries out a counting procedure and determines the viability of the sample. The sample is not stored if the viability is not above the standard set in place. Note that at this point some of the steps are time restricted and are carried out by the lab technician very efficiently. Nevertheless, the sample from which the plateles have been removed and freezing mixture added is then place in a container that lowers its temperature to -90oC in a series of steps. This process alone takes about an hour. Then the sample is placed in a large storage “tank” that is kept cool using liquid nitrogen. Note that the boiling temperature of nitrogen in -196oC, thus one can imagine how cold those storage units must be.
I think the lab can greatly benefit from a large timer to monitor their time restricted procedures and a software that could determine the amounts of freezing mixture components for a specific sample could make their technicians work easier and more efficient.
A picture of lab technicians checking for cell viability and adding freezing mixture to the sample is being shown here.
Getting well-rounded with rounds
Jagan Jimmy Blog

The remainder of the first week with the Hematology/Oncology department was even more exciting than the first half. During the second half of the week we primarily went on rounds with the attending and residents, as well shadowed/observed a few physicians at the clinic.
My partner and I were able to do inpatient rounds with Dr. Venepalli in the Oncology section of the department. It honestly was one of the coolest experiences ever. At a fixed time the attending and the residents meet to do rounds; however, prior to meeting up, the residents and the attending seem to have read up quite a bit on the patient status and history, the former seems to have done a more extensive review of the patients. Each resident seemed to be only responsible for a portion of all the patients on the list. Whether the residents split up the patients among themselves or whether they are assigned to them, I do not know. Nevertheless, upon meeting up, the attending, the residents, and us (interns) collectively walked towards the room of the first patient on the list to see. They stop at the entrance of each of the room and the resident who is responsible for the patient begins to debrief. The review the patient demographics, the diagnosis, complications, current state of being, the state of being for the past few days, any new symptoms, their vitals, and even their alertness. Without flaw, they review every health aspect of the patient. Obviously, to memorize such large amount of information can be tricky thus they all seemed to have small pieces of paper, each being dedicated to jotting down notes on one patient so that recalling information while reporting is easier. The attending also takes notes as the residents are reporting patient info, and she often asks the resident what they think about the patients’ current status, what a diagnosis might be for a set of symptoms, etc. Such practice of requiring the patients to do some critical thinking definitely helps them learn more and makes them more competent doctors.
One of the interesting things I noticed was how calm and caring the attending was when interacting with the residents and patients. I suppose this is why medical school look for candidates that are socially well-rounded and able to keep cool.
During the second half of the week we were also able to spend some time in the clinic with Dr. Rondelli and Dr. Patel. We followed Dr. Rondelli almost through every one of his patient. I was shocked by how different the physician-patient interaction was in the department when compared with Urology. The physicians and patients here seemed to know each other well enough given that they have been working together for a long period of time. The interesting part was that as we walk into the room it is evident to tell how the patients are. The ones who are improving their conditions seems are excited and thrilled, whereas the ones who are not feeling as great or is undergoing the chemotherapy seem to be quite saddened and in pain. Nevertheless, the diverse amount of emotions the patients’ exhibit does require the physician to be quite emotionally competent. While in the clinic two specific cases caught my attention. One was that of a young woman undergoing chemotherapy. Dr. Rondelli informed us of the therapy is difficult on her not only physically, but also emotionally as she is not getting the sufficient social and emotional care she needs outside the hospital. Her situation was quite sad such that her siblings aren’t on good terms with her thus the motive for the siblings to even pay any attention to her are monetary reasons. Such a relation was evident in the clinic, as the sister wasn’t actively engaged in talking about the patient’s care and such.
The second case that caught my attention was that of an elderly man who is terminal, however currently feeling quite healthy. The doctor suggested that he can enjoy the good quality of life that he is experiencing currently or that he may enroll in drug trials that may or may not work and that could have side effects. When compared to the other patients he was actively involved in his care such that he didn’t leave the doctor to making all the decisions. Thus, elderly man was excited enough to enroll in the trial with the reasoning that it may do well to more people. I was quite touched by his decision because he was willing to sacrifice the good quality of life so that medicine research and technology may be advanced.
Furthermore, while spending time in the clinic with Dr. Patel one of the biggest thing that caught my attention was the use of the translation device with a patient. I had previously seen the device however never seen it in use. It is almost like a telephone in that the translator who is virtually connected from a different location listens to the physician and translates to the patient. The major downfall of the system is that since the translator is not physically present in the room they aren’t seeing the physician speak and the non-verbal communication taking place. Lacking such physical cues could lead to not translating the physician’s words with the current tone and pitch. Furthermore, another major drawback was that the translator often couldn’t tell the difference when the physician was talking to the patient versus the resident in the room. Thus, in such cases the translator often interrupts by translating the physician-resident conversation. Overall, one can’t say the system is useless, however it definitely is a slow system that could be improved. The system is placed on a wheeling stand and works through an iPad, however given the actual use of the system one may conclude that having such extensive support system is unnecessary. Further inquire revealed the system is set up in such fancy manner because it was originally meant to be used as a video call system.
Too many people are rounding…!
Jagan Jimmy Blog
The second week of rotation in the department was quite exciting, if not more exciting than the first week. This week we got to spend more time in the Hematology unit of the department. Just like last week one of the main thing we were able to do was go on rounds with Dr. Sharaf. This rounding experience was far different from the rounding experience we had in terms of the number of people going on rounds. Aside from us, there were the physician, fellows, residents, medical students, pharmacist, pharmacy resident, pharmacy students, and the dietician. Overall, there was about thirteen people in the group as we went on rounds. One thing I noticed was that the use of hand sanitizer was more prominent in this department than it is in the other ones. Upon further inquiry, the dietician was able to inform us that this is the case because recently they had an incident where the patient in that one entire wing of the hospital all acquired a specific disease – even the patient who weren’t prone to the disease. Thus, in that case the only explanation was that it was a problem on behalf of the staff. The thought that the medical staff giving the patients disease is quite frightening especially in this department. The patients who are in the department already has a severely weak immune system and thus even slightest exposure to something foreign could make them sick. Obviously, such instances of infection spreading isn’t necessarily because people deliberately do not follow direction, but instead its due to instances where someone sticking their head into the patient room to ask a quick question etc. These tiny instance may not seem to be doing much harm, but evidently enough the consequences of these small slipups can be devastating. This made me wonder why they didn’t have a communication system (like a direct intercom to the patient room form the outside) that nurses or doctors could use to communicate with the patient briefly without having to go inside. The dietician also informed us that to ensure infection control protocols were being followed there would often be people (often designated students, or staff) that would lurk around checking if hand hygiene and other procedures were being followed.
While doing rounds I came to appreciate the dietician’s actions about patient privacy. She was generous enough to not go into some rooms collectively with the group. She wanted to give the patient more privacy, thus visited the patient privately after the group left. Also, she was more economically conservative about not going into rooms where the visitors are required to wear a yellow gown. She didn’t want to waste a gown and go in because prior to rounding she had visited them. My partner and I also decided best not to go into room that required yellow gowns in order to minimize the usage of the gowns. Nevertheless, she informed us that the main reason why everyone goes into the room together is because it is inevitably a learning experience. By having everyone be present in the room, problems won’t be overlooked, and problems may be solved on the spot rather than requiring additional consulting.
The usage of the gowns while visiting a lot of the patients was required because many of them were bone marrow transplant candidate and were on immunosuppressant. Given that they are on immunosuppressant, it is important to not expose them to many foreign substances. Thus, it would be a lot better if the ones who were wearing the gown did put it on properly rather than be lazy about it. Also, an interesting thing I noticed was that there was a stethoscope designated to most patients, so that it stays in the room and only comes into contact with the patient. Lastly, one of the things I noticed while on rounds was that often the care given is hindered or delayed by insurance since the doctors are limited to offering the patients care that they are able to afford – having to make such decisions in such a field is quite saddening because I don’t think anyone should have to think twice about saving someone’s life and saving it using the most efficient method available.
Moreover, we were also able to talk with the director of patient care services. Talking to him was quite interesting. He shared his past work experiences with us and told us about how he got to doing what he does today and such. In terms of his role in the department there wasn’t a well-defined/restricted set of activities or responsibilities that he carry out because he is involved in so many things such as addressing patient concerns directly and indirectly and working with the administration about management issues and such.
We were then also able to get another glimpse into the bone marrow transplant meeting. During the meeting the team involved in the unit comes together and discusses each patient they have seen and talks about their status and asks for suggestions about future decisions if needed. We unfortunately had to leave the meeting early to see the processing of an HPC-A collection. This time around I noticed how the collection had to be transferred into a narrower bag from the bag in which it was originally collected because that bag isn’t ideal for centrifuging. In order to avoid wasting time transferring the collection, it would be highly beneficial if the bag in which the collection was collected was the narrow bag. Since the collection bag is part of a kit the manufacturer would have to produce bags in such shape.
Nevertheless, since it was a larger sample a bigger centrifuge system had to be used, and even that system required placement of a bag of equal weight to that of the collected sample for it to centrifuge properly.
A picture of the centrifuge system is shown here.
The Time I “Malfunctioned”!
Jagan Jimmy Blog

The second half of the second week of the rotation is probably going to be one of those moments I will best remember whenever I recall this internship. Nevertheless, prior to spilling the interesting story here is a brief overview of the other events that my partner and I participated in.
One of the mornings we attended the Lung Tumor board meeting. The meeting had medical students, nurses, physician assistants, and attending and residents from the oncology, and the pulmonary and cardiology departments present there. The meeting took place in a well spacious room. As with the bone marrow meeting, the list of patients dealing with lung tumors that are being treated was by those doctors were discussed and reviewed. Interestingly enough, some of the patients were from the VA. Thus, they had to remotely access the VA server to pull up the images of the patient. The computer was quite slow at the accessing the VA server remotely. The discussion about the patients may have gone by quicker if the computer worked faster.
Moreover, during the meeting something that caught my attention was the concerns and problems one of the physician assistants brought up. She was talking about one of the patient’s primary physician noted a serious tumor however did not directly send the patient to Oncology by getting the patient an appointment that week, but instead the patient only got an appointment a month later. Which brought up the topic of leaving time slots in the physician’s schedule for immediate and emergency cases that need an appointment. They physicians nonetheless become overbooked and are often not able to fit in the new patient into their schedule. Which then raises the question about if they were to prioritize seeing a patient over another one, what standards would be used to determine which patients’ case is more pressing than the other.
Following that, we got the chance to spend some time with the palliative care residents, and got to know about what Palliative care is. They told us how it is a new field and that it wasn’t till recently that UIC got a palliative care department. Nevertheless, the residents shared their reasons to want to go into Palliative care and informed us that because the field itself is only about a decade or so old there aren’t that many programs that offer it and that it is quite a non-competitive field.
Then later on, we were able to go watch an HPC-A collection. HPC-A collection means hematopoietic progenitor cells apheresis collection. The collection was done by Septia Optia Apheresis system, which was linked directly to the central line. The machine system is able to separate the HPC cells along with some other components of blood from the plasma. The plasma is returned into the patient whereas the remaining is collected.
Now comes the eventful part of the week. My partner and I were lucky enough to be allowed to observe a bone marrow biopsy. The procedure is very medieval, yet straightforward. The physician sterilized the area being injected and numbed it. The biopsy needle is then inserted into the bone, and the center of the needle is removed through which then the hollow needle is inserted to get the biopsy sample. Something interesting the physician did was that she coated the inside tubing of the syringes with heparin so that when collecting blood it wouldn’t clog in the syringe. Lastly, once the necessary samples were obtained the biopsy needle was removed. And that’s when things started going downhill for me. Prior to the procedure the attending did warn my partner and I to sit down while watching the procedure, especially since it was our first time. Initially we were seated, however since our view of the procedure was obstructed we stood up to get a better view; and we had thought the physician suggested us to sit because we may be squeamish about blood and needles, which neither of us are we didn’t see the problem with standing up.
Anyways, once the biopsy needle was removed my I started to sweat rapidly, I felt like a heat wave was passing over me, especially back and forth on my scalp. My field of vision began narrowing. I could still hear what other people were saying but I started to lose comprehension of what I hear. Then I felt like I was unstable and had immediately sat down. For a few seconds I couldn’t process anything going around, I recall hearing my partner asking if I was okay however I was unable to respond. One of the brilliant residents realized what was going on from afar and kindly offered me a fruit punch, lemonade, and orange juice. After which the medical student insisted I sit down for a while, just to ensure that I won’t faint again. Meanwhile, she described the episode as a vasovagal syncope. I later on looked in to the condition, and found that it is a “malfunction” of the nervous system upon exposure to a trigger. Interestingly enough, it does happened during or post biopsy procedures. Even though, I felt like my body system failed me because I was totally comfortable seeing the biopsy procedure, given that I have seen even more gruesome stuff in urology, this incident reminded me about how there is so much more to the human body that I don’t know and has yet to be discovered.
Learning about a lot of new professions in the medical field
Jagan Jimmy Blog

This was unfortunately the last week of the internship. I was actually looking forward to meeting with the members of the radiation oncology department. Upon entering the department we were able to meet with few of the residents and the attending, and then we got to meet with the medical physicists. We were able to talk with a few of the medical physicists there. I was absolutely intrigued by getting to know that particular profession, as I have never heard of them before (as I write this blog, I am about 55% sure I want to be a medical physicist, and about 45% sure about going into medical school). Talking to the medical physicist I learned about what they do and the potential for the profession.
Talking to the radiation physicist he told us about future of imaging and radiation. Ideally in the future, imaging should be able provide the same information as a biopsy. The physicist and researchers work on developing new techniques for administering radiation while minimizing unnecessary exposure. Efforts are also being made to make the most imaging techniques and analysis computerized. Overall, the medical physicists and other workers there do a lot of different tasks some more clinical, whereas some do more theoretical work.
One of the days we were able to come in early to see the radiation machines being turned on. One of the medical physicist was responsible for starting things up and running the quality assessment. The medical physicist was an intelligent fellow who was able to successfully automate many of the machine check tests that they do. Interestingly enough, the fellow said often the machines are turned on by the therapists rather than the physicist however when there are monthly assessments that need to be done the physicists has to do it.
Moreover, the patients usually come in during their assigned time for the therapy session. One thing I noticed was that they have a tight schedule for the radiation therapy especially with many of the patients are scheduled for therapy every day for a couple of weeks. Nevertheless, ideally they shouldn’t be starting any procedure prior to the arrival of at least one attending. However, one of the days the attending that was supposed to come in early slept in and they had to wait till they start the first therapy session.
Moreover, we were able to talk with the engineer in the department about his role and how he fits into the environment. He told us how he is mainly called upon if any problems rises and that most of his work is afterhours. He runs some diagnostic testing at the end of the day. He said he isn’t experienced with the newer machine, however a relatively good expert on the older machine’s functioning. I found his job to be quite interesting as it required a lot of on-the-job learning. Furthermore, he shared with us the story of how a problem with the machine where the radiation beam wasn’t being positioned correctly killed a few patients. It was a bit scary to hear that more than one patient died on the table because the flaw of the machine went unnoticed. Nevertheless, this is why it is even more important for someone like him to check the machine and run some diagnostic testing every day the machine is used. Also, he shared that a common problem with working with the machines is that, since the machine is so big often it is quite difficult to identify the actual problem is because they have to check the machine all around to identify the problem.
And….That’s a wrap! :'(
Jagan Jimmy Blog
The second half of the week my partner and I were able to see a few more interesting things, while being in a hustle to put together the final report and presentation. The rounding experience in the department was quite different from all of them I have seen so far. The physicians, physicist, nurse, and dosimetrist all meet in the conference room and go through the case of each patient. Given that most of their patients comes in and leave after each of their session, this is the most reasonable way in which they may do patient rounds. I was really impressed with the computers and the additional tech they have down in their department. Obviously, this is expected since the nature of the department requires extensive use of imaging results that need computers with fast processors and quality display.
Moreover, we were able to seek out and learn more about what the dosimetrist and the medical physicist does as part of the team. We were able to see the medical physicist carry out the process of ordering the necessary radioactive components for someone with a tumor around or near the eye. The order is sent via email to the medical physicist who does some numerical calculation by hand to determine how many radioactive components are needed to administer the prescribed dosage. Once he determines that amount and creates a report of it, he then has to place the order by phone. Interestingly enough, he also said that it is him who make the customized eye patch for the patient using lead material so that they may wear it when going out, etc. as to keep those around them safe. Another cool thing was that the way they position the radioactive components in the plaque of the appropriate size is standardized based on research findings; the best part is that there is a program available that models how the radiation is distributed and its intensity from the sources for various position combinations.
Moreover, my partner and I were able to see a stem cell infusion. Interestingly enough the infusion was that of the same patient who we saw they collection of earlier. As the frozen cells are transported in the portable cooler a few inconveniences were noticed. For example, it would be a lot more helpful if the portable cooler had an accurate built in temperature read, and also a handle that can either be folded out to or is at the level of the technician so that the cooler may be pushed around more easily. The thawing procedure was simple enough such that the frozen sample was placed in a larger bag which acts as a buffer to the treatment of sudden heat and it is placed in to a hot water bay at 37 degree Celsius.
While thawing the frozen sample, the technician informed us about how at some infusion centers they take additional steps in order to remove the DMSO that was added to the sample as part of the freezing mix. This step is helpful since it reduces or eliminates the possibility of the patient experiencing some side effects to it. Upon infusion anyone in the room can smell the DMSO since it has a garlic-like smell to it. Moreover, the nurse practitioner present there did inform us about how it would be much convenient if there was an easier way to attach the infusion line to the sample.
Once we were done seeing the infusion we heard the nurses talking about the network being down. The then had to record their measurements and other values on paper and later transfer it when the network was active again. In the ten additional minutes that we were there the problem wasn’t fixed and didn’t see any software tech working nearby.
Another interesting, yet a very rigorous treatment that we were able to witness was brachytherapy. The medical physicist informed us that the this treatment is usually used as either the last resort in the fight with cancer, or as the way to ensure cancer has been entirely wiped out from the region of interest. The patient we say receiving the treatment was unfortunately using it as a last resort to treat her aggressive cervical cancer. The treatment requires high team work and great precision from the medical physicist and the physician since the tissue is being directly placed in contact with heavy radiation. The treatment was also a bit scary for the patient since while being exposed to radiation, everyone else vacates the room. Nevertheless, the three most important factors of radiation to consider at all times when formulating a treatment plan are distance, time, and shielding.
Lastly, the wonderful engineer in the department was so kind enough to show my partner and I the interior of the machine radiation machines. He took apart the external covering of the older machine for us alone and went out of his way to explain the theory and concepts behind it. Although I wasn’t able to understand or absorb some of the information he shared his brief tour gave us a general idea of how the machine works. Moreover, it was interesting to see that many of the flaws he mentioned with the older machine was either solved or improved in the newer machine. As an engineer he shared that a lot of the things that he does requires learning on the spot. Over the years he has become accustomed to the workings of the older machine and is able to fix the problems that arise with it. However, he himself is still only learning the newer and more sophisticated machine piece by piece. If the newer machine shows any problem, it is usually reported to manufacturer who then sends their own specialized tech/engineer to solve the issue. The department is looking forward to getting a newer machine in early 2016. The process of replacing the old machine takes about 9 months since the entire room needs to be re-built to fit the new machine and its specifications.
With such wonderful experience the internship finally came to an end.
I must say this internship is by far one of the most enriching experience I had as a bioengineer and a prospective medical student. The wide variety of people I met over the past six weeks were simply amazing and impressed me with their contributions to helping people and advancing medicine. The up-close view I got of the hospital motivated me to be a physician and an engineer simultaneously, because there are simply too many medical problems to be resolved, questions to be answered, and lives to be saved.
P.s. The picture indicates a favorite phrase of an inspiring individual I met during the latter half of the internship. Although the quote maybe simple, the message is definitely something that is overlooked often and needs to be valued more.
Marianne Palczewski Heading link

A bioengineering student’s exploration of the worlds of Hematology/Oncology, Radiation Oncology, Gastroenterology, and Hepatology at the University of Illinois at Chicago Hospital.
Marianne Palczewski Blog Heading link
-
Marianne Palczewski Blog
Week 1, Part 1: The Beginning
Marianne Palczewski Blog

I began my week in a meeting with Dr. Kotche and Dr. Stirling, who explained to us what to look for as we observe medical procedures in our respective rotations. Later that afternoon, I went down to the oncology clinic and met with Dr. Pritesh Patel, who is our mentor. We sat in the nurse’s station in the bustling clinic until he came by. As he took us around the clinic, I noticed that there were three hallways, containing both infusion rooms (where patients would receive chemotherapy) and examination rooms (where patients would meet with physicians and discuss the medication they were to receive or the status of their cancer treatment). Dr. Patel also explained that bone marrow transplants are often used to treat aggressive lymphomas and myelomas, and are generally very effective for certain types of cancers.
We also spoke with a perfusion nurse, Lupe, who explained how the clinic operates. When receiving chemotherapy, patients first come in for their appointment and have their blood drawn. They then wait anywhere from 30 minutes to 2 hours for their blood results and vitals to be analyzed, which is something that particularly surprised me. This information is used to calculate the optimal chemotherapy rate of injection and quantity of injection for the patient. Lupe also mentioned that a very important part of chemotherapy is ensuring that patients have a nutritious diet complementary to their treatment. She suggested that they might be better off with a nutritionist on staff. As we walked around the clinic, I also noticed that there was a pharmacy and lab where patients could easily access their drugs.
We then attended a board meeting with all of the hematology /oncology staff, including physicians, pharmacists, nurses, and social workers. The patients were discussed one by one, and all the physicians and nurses were invited to contribute any information about the patient or any suggestions for a change in treatment. Each person was given a spreadsheet with the patients and their status. It was difficult to follow the discussion because of the jargon and acronyms the physicians used.
The next day we went on rounds on the eighth floor of the hospital, in the stem cell transplant wing. We followed Dr. Khan as she and a team of 3 or 4 fellows discussed each patient on a portable desktop computer stand, and then went into the room to ask the patient how he/she was feeling, check his/her heart and lung function using a stethoscope, and ask if he/she had any questions or problems with the treatment. I was surprised by the amount of waste used in this process. The patients’ rooms were labeled with the level of protection necessary to enter the room. For our first patient we had to wear yellow gowns and face masks, and the physicians who touched the patients had to wear gloves. It took a long time to put on the gowns, and when one was pulled out of the container attached to the door, all of the gowns also fell out. Perhaps a dispenser system could be implemented which only gave one of each item. Almost all of the patients were neutropenic, which means that they had a low blood count. This meant that they were very susceptible to infection, and the main reason for our protective equipment was to protect the patient from our germs. Something I noticed about the portable computer the doctors used to review the medical history and test results from the patients was that there was a stack of pill cups that were taped to the top of it, since nurses also use the same stand to administer medications. Perhaps a cylindrical indent could be implemented into the stand for the pill cups, and it could even be operated on a spring.
Later that day, we observed a lumbar puncture, which lasted for one hour and was very painful for the patient.
We were also able to observe the stem cell collection storage. When stem cells are harvested from a donor, the donor must sit for 4-8 hours with two IVs, which are connected to a machine. Blood is taken out of the patient’s vein, centrifuged and filtered so only the white blood cells are collected, and the red blood cells and plasma go back into the donor. The blood is then brought to the lab, where it is processed to filter out only the white blood cells, then to filter out only the stem cells, and finally to store them in a liquid nitrogen tank for later infusion into the appropriate patient. Something Youngmin (the main lab technician) mentioned was the the monitors on the Liquid Nitrogen tanks tend to malfunction, since they are so absurdly cold (-150 to -190 degrees).
The next day, we attended a lung tumor board meeting, where each patient was again discussed in turn. This time, however, we were able to see a PETCT or CT scan of the patient’s lungs and any tumors or lesions that might be observed therein. It was fascinating. Next, we sat in on a meeting where the main doctors discussed some financially beneficial strategies for the hospital. This surprised me because I thought that hospital administrators mainly discussed such things, rather than doctors. We went on rounds again and then went to the radiology department to look at the machines they used to make the scans analyzed in the meetings. Some machines we were able to observed were the PET scan machine, CT scanner, Xray, Fluorimetric X ray, and Ultrasound. We then met with Dr. Patel and discussed some of the things we learned.
Week 1, Part 2: Bone Marrow Biopsy!
Marianne Palczewski Blog
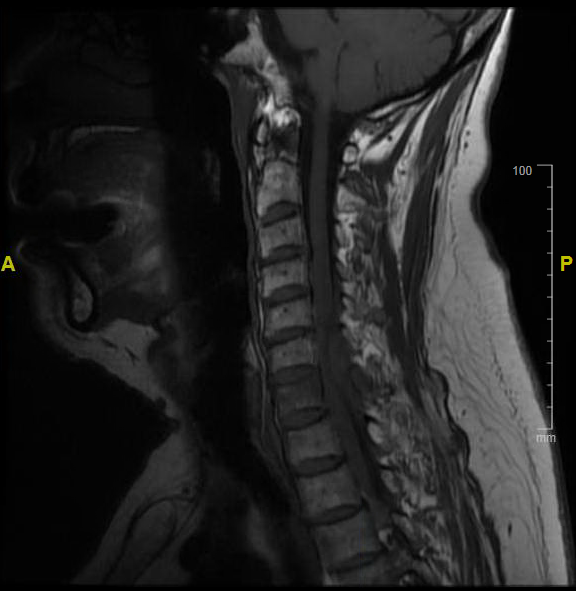
The next day was spent almost entirely in the clinic. In the morning, Dr. Patel had five or six patients. For one of these patient discussions, a polish translator was necessary. The translator’s first language was not polish, and she had a difficult time explaining some of the more technical medical procedures to the patient and her spouse. It was uncomfortable for everyone, since the patient was frustrated that she could not understand, on top of receiving the news that a bone marrow transplant would be the best route of action. A handheld translator may have been more useful here.
We were then able to observe a bone marrow biopsy, where a nurse placed the patient to lay on his stomach, and essentially drove a large needle into his hip bone in order to extract some bone and the liquid marrow inside. I was surprised with the ease with which she could dig into the bone. The patient was not in too much pain, as the nurse injected a local anesthetic into the skin, and into the periosteum, which covers the bone. I did hear him groan a few times, which was a little unsettling.
Later that afternoon, I was then able to look at the marrow sample under a 6-person microscope in the pathology department. When looking through the eyepiece, I saw a cursor in the middle of the field of view. As the pathologist analyzed the sample, he would point to different cells using this cursor and tell us what the cell indicated about the success of the patient’s bone marrow transplant. We did not see many blast cells, meaning that the cancerous nature of the leukemia was essentially eliminated. We looked at the peripheral blood sample and at the bone marrow sample. In the bone marrow sample, I saw fat, connective tissue, and a variety of blood cell types in varying stages of development.
The next day, we did rounds in the morning with Dr. Khan and then went to the clinic with Dr. Patel. We only saw one patient, who had a tumor in his spinal cord. The PET sagittal slice of his cervical spine is below.
Week 2, Part 1: Meetings & Discussions
Marianne Palczewski Blog
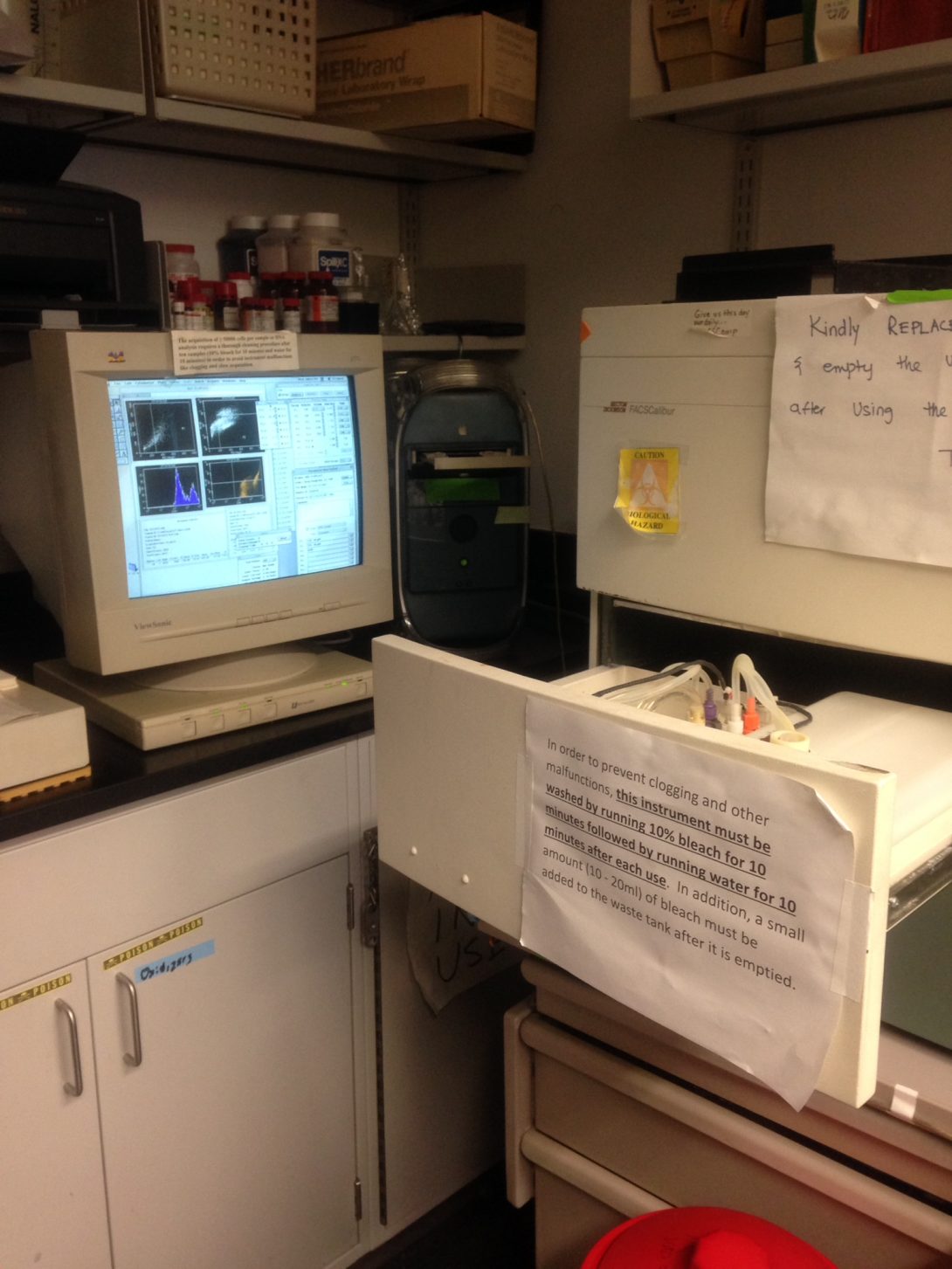
The beginning of this week was spent doing much of what we did last week. Monday afternoon was one of the more depressing days of the rotation so far. We were able to observe a chemotherapy infusion, which is done by a nurse. The patient was a multiple myeloma survivor in remission. Before injecting the actual drug (which in this case was a bone strengthener), he received an injection of saline because he was dehydrated and his blood volume was low. The saline flowed into his veins while the nurse checked on his insurance. There seemed to be no exact science to the length of time to use for the saline, it was just pumped through his veins until the nurse was done. I noticed that only about 10% of the saline in the bag was used before he was switched to the bone strengthener. The rest of the saline was then thrown away, which seemed like an incredible waste. Perhaps if smaller bags were used, much of that waste could be avoided.
We talked with him and his wife for close to an hour, and they explained exactly what he went through, starting with his diagnosis last year. His wife mentioned that they had also lost their daughter to myeloma a few years ago, and began crying as she was explaining it. This was the first time I had seen someone cry in the clinic, and because I didn’t want to cross any boundaries, I was not sure how to console her or continue the conversation. Something interesting they mentioned was that when he was staying in the hospital for about 3 weeks after his bone marrow transplant, he had to take 15 pills, three times a day, which was exhausting. This surprised me because I had assumed that hospital patients receive most of their medications intravenously rather than in pill form. He also showed us some purple discs that appeared on his skin, and said that he was waiting on a pulse skin biopsy that would indicate what those lesions were.
Hearing about how long everything took, the patient’s feelings, and aspects of his care he wished were different led me to think differently while observing all other physician-patient interactions.
As we left to go to the hematology/oncology board meeting, Dr. Patel came in the room to talk to the patients. He later told us that he had to break the news that the patient’s myeloma was back and he stood little chance of living much longer. It was incredibly sad to hear this after spending so much time getting to know the patient and seeing how much hardship he and his family had already been through.
Later that afternoon, we had a chance to speak to a fellow, who explained that attending doctors have to write notes after every time they go on rounds, which actually takes up a good part of their day. Often times the fellows will write this to save time for the attending physicians.
On Tuesday, we attended a 7 AM gynecological tumor meeting in the pathology department. It was much different than both the leukemia meeting and the lung tumor meeting because it took place around a 16-person microscope. The image was reflected around the room by a series of mirrors. One doctor led the meeting and went through each patient individually, showing the accompanying slides (differentially stained tissue slices) and describing the cells and what they mean for the prognosis of the patient. This meeting was much more understandable than the other meetings because of its slower pace. Something I found interesting here was that the doctors are able to determine the size of the tumor by looking at these stained slides, and estimating the length in relation to the diameter of the field of view. For example, for a 4x magnification, the circular field of view represents a diameter of 5mm, while the 20x magnification boasted a diameter of 1 mm. If using the 4x objective and the tumor took up half the screen, one could say it was about 2.5 mm. I also learned about different types of tumors (cul-de-sac, serous, mesothelial) as well as different types of diagnostic tools. Something else mentioned was that, if mesothelioma is suspected and traditional microscopy proves inconclusive, electron microscopy can sometimes be used to examine the fresh tissue. I had previously though that electron microscopy was reserved for research labs, so this was a pleasant surprise.
One hour later in the same room, we attended a genitourinary tumor meeting. The doctors sat around the same microscope, but strangely did not use it. Instead, we looked at PETCT scans on a small monitor in the corner of the room. Before I attended these board meetings, I had thought that one doctor would present the patient to the group, and then each physician would in turn say what they thought would be the best next course of action. Conversely, for almost all of these tumor board meetings, it seemed like it was only a conversation between the presenter and 1-3 top physicians in the group, with 10 residents, students, and even senior physicians just listening in.
After the meetings, we went up to the 8thfloor of the hospital to see if we could catch the tail end of rounds, but were surprised to find the attending physician, Dr. Khan, and the 5-6 fellows/residents talking about the patients around a table instead of at the portable computer in front of each respective door. I later learned that this was because it was Dr. Khan’s last day as attending physician in the clinic, and on Wednesday she was replaced by Dr. Quigley. Attending physicians rotate every 2 weeks, which I think has both positive and negative aspects. On one hand, patients who are used to one doctor are confused by the new doctor and feel uncomfortable with them. However, on the positive side, two doctors can have completely different diagnostic styles, which can lead to an overall better treatment. Another benefit is that if a patient and doctor did not get along well or understand one another, the patient might feel more comfortable with another physician.
As they discussed each patient and his/her medical history, medications, and complications, I couldn’t help but notice the wide variety of ailments that befell these patients. One patient had end stage renal disease, while another had a catheter, and yet another had temporal wasting and dysphasia. I suspect that surgeons or other specialty physicians only need a deep understanding of the part of the body they work most intimately with. Because chemotherapy can affect almost every organ or part of the body, these hematology/oncology physicians must truly have a sophisticated understanding of every organ and disease.
That afternoon, we shadowed Dr. Oh in clinic, and were able to see two patients, both of which spoke Spanish with Dr. Oh. Nearly half of all of the patients I have seen in clinic have Spanish as their primary language. Luckily, Dr. Oh spoke Spanish and we did not need to use the tablet translator, which takes a long time to set up and can make for an uncomfortable situation, not to mention that these sessions take twice as long. I think that public hospitals such as UIC might consider providing a Spanish training program for their physicians, so they at least know the most important phrases and questions to ask their patients. I also speak Spanish, and more than once I heard a discrepancy between what the patient said and what the translator conveyed to the doctor. It did not affect the diagnosis, but in some cases it might.
Dr. Oh also took some time to discuss new immunotherapic cancer treatments with us and had us research three similar drugs, Rituximab, Ofatumumab, and Obinutuzumab, and then present to her what we found. What is interesting about these drugs is that they are all for CD20 positive CLL, chronic lymphoidal leukemia, (leukemia where B-cells contain the CD20 receptor on their cell surfaces), but induce cell death in different ways. They are all monoclonal antibody drugs, but Rituximab dimishes the NF-kappa-B pathway, leading to cellular toxicity. Obinutuzumab involves caspase-independent apoptosis (not including NF-kappa-B), while Ofatumumab involves complement dependent cell lysis. Dr. Oh also told us about two other emerging chemotherapy strategies that are not yet available at this hospital, Car T Cells, and biTE treatment. Both of these treatments take advantage of the body’s own immune system, using it to target and kill only cancer cells.
The next day we attended rounds with Dr. Quigley, which started once again sitting down around a table. The residents presented each patient to Dr. Quigley, and had to adhere to a strict format while presenting, which led to a much different atmosphere than with Dr. Khan. After a several-hour discussion, we went to each patient’s room, once again debriefing Dr. Quigley before each room. It seemed quite repetitive and perhaps it would have been better if the discussion happened just in the hallway, with the patient visit immediately after his presentation. I know that if I were the attending physician, I would have preferred it that way. Something I noticed on rounds is that on each IV stand are little strips of green caps. A resident explained that those were alcohol-filled caps that helped to minimize the spread of disease when transporting and administering the IV bags.
After rounds, we visited the lab of Dr. Oh, Dr. Patel, and Dr. Mahmud in COMRB. Not many experiments were going on, but it looked to be a similar set up to that which I have in my own lab in MBRB, including culture hoods, liquid nitrogen tanks, an incubator, a cold room, and lab desks and benches. A researcher in the lab showed us a flow cytometry machine, which I had never seen before. Cells in suspension are sucked into a thin metal tube, and are sorted by a variety of factors, such as fluorescent label, FSC (granule level), and SSC (cell size). Four distinct graphs were produced per sample. Water needed to be fed into the metal tube between samples, to avoid contamination and incorrect readings from residual cells and media. The two main receptors tested when looking for stem cells are CD33 and CD45. The computer was very old and worked very slowly, but I assume the flow cytometer software was only compatible to the old operating system, which is why they did not replace the computer.
Week 2, Part 2: An Infusion and a Humbling Conversation
Marianne Palczewski Blog

On Thursday we finally saw a stem cell infusion. We also were given lab coats to wear, because we would be entering the patients’ rooms. The order of events in a stem cell infusion is as follows. First, the appropriate cassettes (filled with donor stem cells) are removed from the storage liquid nitrogen tank and moved to the small, portable liquid nitrogen tank that will be transported to the patient room. A water bath was also moved to outside of the patient’s room a half hour before the procedure, so it would have time to heat up and be ready to thaw the frozen blood. Once ready, the blood is removed from the cassette and thawed by moving it back and forth in the water bath. Next, two samples of the blood are extracted into vials, one to check the viability (usually 75-80%, if less than 50% the infusion cannot proceed), and one to be sent to the microbiology lab to check for infection. If an infection is found in the blood, the patient receives antibiotics or antifungal medication to counteract this.
While the sample tests are being done outside, the patient is receiving a saline solution intravenously. As seen in the picture, once the stem cells are ready, they are connected to the line with the saline and then filtered, to minimize injection of debris or unnecessary red blood cells. After filtration, the cells travel down the IV tube into the patient’s arm. When looking at the IV tubing, I saw clumps of white traveling through and into the patient, which are actually the clumped stem cells.
Before the procedure, the patient will receive Benadryl to calm him/her down or hopefully fall asleep. If the patient was nervous or anxious during the procedure, this could cause a hypersensitivity reaction, leading to a rejection of the stem cell transplant. It surprised me how big of a factor mental stressors were to the procedure. To ensure there are no adverse effects and that the body is accepting the transplant, a nurse will monitor the patient’s vital signs every five minutes. A doctor is not present, but is told to remain in the wing in case of complications.
When one bag looks like it is reaching its end, the technician heads back outside into the hallway to thaw the next bag of blood. It is important not to thaw all the bags at one time because this will severely decrease cell viability, as cells start dying as soon as they are thawed. Thursday’s infusion involved only 4 bags (50 mL x 4 = 200 mL), but infusions can use up to 8 bags of 50 mL. After the infusion, we went to the clinical stem cell laboratory and saw the viability tests, done with Trypan blue on a hemocytometer. We also learned how to use the heat-powered IV tube sealer and cutter, which can actually combine two tubes into one continuous one. I was surprised by the strength and integrity of the IV tubing after sealing two distinct parts together.
After lab, we headed to the clinic and went on rounds with Dr. Khan. I noticed that all of the beds/examining chairs in the clinic had outlets on them, although I have never seen them used.
One patient in clinic had had a liver transplant some years before, and as Dr. Khan examined her abdomen I saw an interesting scar on her stomach. Dr. Khan explained that a common surgical technique for liver transplants is to cut a “Mercedes sign,” and it really did look that way, with little dots lining the incisions where the sutures had been.
The rest of the patients in the clinic only spoke Spanish, and Dr. Khan used the Interpretalk service both on a portable tablet and on a fellow’s iPhone. It seemed to work better on the tablet, since the interpreter from the iPhone really had trouble understanding anything, not to mention that there was a 5 second lag, which really added up when asking many questions.
After we saw a patient on a clinical trial medication, Dr. Khan explained to me that clinical trial patients need to be assessed on a standard scale in order to have the data accepted by the NIH. There are certain grades of disease; for example a grade 1 allergic reaction involves some redness and hives. The patients are assessed in this way in an effort to make the data more quantitative, as it is difficult to know what symptoms one doctor perceives as severe rather than moderate. Also, each patient on clinical trial medicine undergoes detailed testing after three months.
The last patient in clinic that day was an older gentleman with mylofibrosis who was there with his daughter. Dr. Khan told him and his daughter that he had leukemia, and they both took it surprisingly well. He was hard of hearing, so it is possible that he did not exactly hear the diagnosis, but his daughter was calm and collected, as if she had expected it. Dr. Khan discussed their options with them, which were either to have supportive care (antibiotics, transfusions, etc.) or to take a drug meant to cure the leukemia (which could extend his life by 8-12 months).
The next morning was spent on a patient discussion around a table, with the intent for actual rounds to begin at 2 PM. I did not realize that attending physicians could decide when to do rounds or how to do them, since there is a schedule to medication and food and blood draws.
After our class meeting from 1 – 3 PM, we met with Dr. Mahmud, the director of the stem cell laboratory. Our discussion was something I never would have expected. We talked about our future career goals, and about thinking about problems as a child would, without any limiting mental schemas or ideas. Dr. Mahmud also discussed the science and history of stem cell research and bone marrow transplant, as well as his own career history and how he came to UIC. As a group we even discussed some lines from a book of philosophy of the Indian poet Gitanjali, which were about a man who was building up a plaster wall to perfection, not realizing that he was standing in its shadow. Something else interesting he shared with us was that we have enough bone marrow to sustain us for 4 lifespans.
Week 3, Part 1: To Radiate or not to Radiate?
Marianne Palczewski Blog

At noon, I attended the general tumor board meeting. I was surprised to see that in some cases, in addition to analyzing the pathology and PETCT or MRI images of cancers, the doctors also looked at a macroscopic view of the removed tumor (which in one striking case had taken over an entire testicle).
And so begins radiation oncology! After we descended into the basement of the oncology clinic, we were introduced to Dr. Bhave, who explained the flow of radiation treatment. First, patients are referred to the department. Typically, once they are referred they have already gone through one or more other departments in the hospital, and have received PET/CT, MRI, or other images that help the physicians see exactly where the tumor is and what volume to radiate. Nonetheless, the patient is placed into the CT Simulator, also known as the “CT Sim,” where he is immobilized using custom-made devices that encase his legs and arms, as well as the part of the body he will be receiving radiation. A CT scan is taken, and the scan and immobilization devices will be used for every subsequent treatment to make sure radiation is delivered to the same spot.
Dr. Bhave also explained that there are two main types of radiation therapy done in the hospital. The first is fractionated treatment, which is where the patient comes in for 25-30 sessions of radiation, every day for 5-6 weeks. Another option is radiosurgery (1-3 sessions), which is typically done for lung cancer, or for patients with poor lungs. Often times, chemotherapy and/or steroids (to reduce inflammation) will be administered to the patient in tandem with either of these two procedures. I was surprised to learn that radiation can be given for a wide variety of other conditions, namely keloids, heterotopic ossification, gynecomastia, and excessive salivation, among others.
We were introduced to the radiation technicians who operate the linear accelerator (LINAC) that actually delivers the radiation. The machine delivers IMRT (intensity modulated radiation therapy), where there are several beams passing through dynamically opening and closing MLCs (multileaf collimators) that shape the beam to the target area. The beams rotate all the way around the patient, and can even deliver radiation through the bed.
When a patient comes to the clinic to receive radiation, a technician first brings the patient into the room and uses their immobilization devices and aligning lasers to align him/her onto the bed. The other technician then does a preliminary x-ray of the patient, and uses the computer to move the bed, aligning him/her with the initial CT scan done in the CT simulator. He then pushes a button and the radiation begins.
Interestingly, a pelvis cancer patient’s elbow was near the edge of the bed, and as the linear accelerator was rotating around her pelvis, the machine displayed an error and stopped treatment although it was nowhere near it. The technician had to press an override button while the rest of the radiation was conducted. It was strange to see that such a sophisticated machine could not match its motion sensor to the area of treatment.
We started the next day with 7 AM gynecological oncology and genitourinary oncology tumor board meetings in the pathology department. Afterwards, we were able to observe a brachytherapy procedure, which is actually another type of radiation therapy, done over 3-5 sessions. Here, a device (whose shape varies depending on the cancer) is inserted into the patient and a targeted dose of radiation is given, typically in the form of a radioactive iridium “seed”. We observed cervical cancer brachytherapy, and thus the device was a long cylinder inserted into the vagina.
We then spent more time with the radiation technicians, and discussed another type of alignment. In lung and torso cancers, a common issue is delivering radiation to the tumor while the patient is breathing, since the tumor is displaced with each breath. At the UIC hospital, the physician will just circle a larger radiation area that will cover the tumor at all stages of breathing. In other machines in different hospitals, the radiation will only turn on for a certain stage of the breathing cycle, resulting in a more targeted radiation effect and less damaged healthy tissue.
After some discussion, I asked the technicians if they had ever treated a pregnant patient. In fact, a past patient with pelvic cancer had been pregnant, and she had to decide between saving her life and the life of her unborn child, since there was no chance for the child to survive the high energy beams. In the end, she decided to save her own life, taking her four other children into consideration. This ethical dilemma opened my eyes to how truly devastating cancer can be, to not only a person, but to his/her entire family.
The two main tasks for radiation oncologists seem to be looking at MRI/PET/CT scans and drawing out tumor volumes, as well as seeing patients. I sat in on a few of these consults. Radiation oncology differs from other hospital departments in that none of the physicians use pagers (or cell phones, for that matter). For one, all the doctors are from the University of Chicago, and have not been issued UIC pagers. Also, since they are in the basement, the reception is terrible. Therefore, all communications are sent to the nurses’ station landline, and are then broadcasted via intercom. I thought this would result in some confusion, but everyone actually seems to prefer it.
On a related note, Drs. Kauffman and Bhave mentioned that one of the only problems they came across in the clinic was that it is difficult to communicate with other departments (medical oncology in particular). This can actually lead to ineffective radiation treatment if not correctly matched with a chemotherapy regimen.
Week 3, Part 2: “Cure sometimes, Treat often, Comfort always”
Marianne Palczewski Blog
We spent most of the end of the week talking to Drs. Bhave and Kauffman in the physician’s office, and a bit of time observing the CT simulator in action. On Thursday morning, we sat in on table rounds, where each new patient plan was discussed in turn, including a presentation of their scans and symptoms. I learned that anaplastic thyroid cancer is the worst cancer one could possibly have. It is incredibly fast growing and kills by constricting the trachea to the point where the patient can no longer breathe. The images of this patient were truly striking–the tumor looked to be almost twice the size of his neck.
A topic discussed at length with every case is whether the radiation will be palliative or curative. In metastatic cancers, most therapies are strictly palliative, to minimize symptoms and provide a better quality of life for the time the patient has left. Doctors also often refer to the National Cancer Center Network (NCCN), which provides documentation on staging cancers as well as treatment options to choose from. Everyone at the meeting was very welcoming and explained complicated cases to us.
We then watched the CT Sim technician arrange a patient on the bed and develop the molds, which took about 30 minutes to dry and harden. This was a patient with a tumor just under his skull, so he also had a face mask made for him. The technician first covered his face and head with saran wrap, and then made the mask out of strips of cloth-like covering dipped in a white paste. Another option was to make a more modern fiber “hockey mask” for him, but the technician said that in reality the two are almost identically effective. One difference is that in the hockey mask, the mouthpiece is built in, but for the paste/cloth a separate mouthpiece must be made. This mouthpiece is important in radiation because it keeps the teeth the same distance apart every time. As it turns out, nothing can be used to cover the patient’s healthy tissue, as I had thought. Placing lead over some part of the patient’s body only directs the photons to the surface of the body, leading to more skin burning, peeling, and complications. The patient also received contrast delivered by a robotic arm.
Later, Dr. Kauffman told us about a plaque brachytherapy he observed, where a patient had an operation to insert a gold/steel plaque behind his eye to treat his eye cancer. The plaque had radioactive seeds in it that would work over time to treat the tumor. The patient actually needs to keep a lead eye patch over their eye so they do not radiate other people they encounter. This seemed like something out of a superhero movie.
The doctors seemed to spend a good amount of time in their office. I noticed a large portion of the patients did not show up to their appointments, and after asking Dr. Kauffman about it he said that around 50% were no-shows. The department might consider a rescheduling fee or missed appointment fee to avoid this type of thing from happening—otherwise the doctors could have focused more closely on drawing the tumor volumes or discussing other patients.
On Friday we discussed emotions and comforting patients. The doctors explained that although their work can be depressing at times, radiation oncology is one of the most rewarding fields of medicine because without radiation treatment, some of these patients would pass away within the next few weeks. The patients are incredibly delicate, both mentally and physically, and sometimes can only find solace in the doctor who understands what exactly is happening in their body. Dr. Bhave mentioned that one physician in the radiation clinic actually cries with his patients, and that this helps them both to cope. Half of the time, palliative treatment is the only option, and the doctors just have to try and give the patient as pain-free a life as possible. As Hippocrates once said, doctors must “cure sometimes, treat often, comfort always.” This really holds true in the field of oncology.
In our last moments in oncology, we attended a breast tumor board meeting. The most surprising thing here was that the solution to everything seemed to be a mastectomy, regardless of the severity of the cancer. The reasoning behind this was that when a tumor is resected, the most likely place for cancer to come back is in the empty space left over. Perhaps the doctors might consider placing something in the empty space or applying necrotizing chemicals that will prevent the resurgence of cancer.
Overall, I really enjoyed my time in hemeonc/radonc. I have worked on cancer research for the last year now, but this experience allowed me to see the disease from both the patient’s and physician’s perspective.
Although it does not have to do with bioengineering or biomedical device design, the most surprising aspect of this rotation was the relatively positive attitudes of the patients. With how lighthearted some of the patients were, it was easy to forget that they are suffering through one of the worst diseases mankind can contract. After hearing that we were bioengineers, some patients even offered suggestions for procedures that could be improved.
Even so, when going on inpatient rounds, in some rooms I almost cried after seeing the patients in their weakened state. Although they try to remain humorous and positive, an inner sadness is unmistakable.
Week 4, Part 1: In the Gastroenterology/Hepatology clinic!
Marianne Palczewski Blog
This week marked the beginning of my next rotation – gastroenterology and hepatology! For this week, we are in the outpatient clinic on Taylor Street. The clinic is divided up into half days, with either GI or hepatology dominating the clinic at any given time. Mark and I spent time shadowing attending physicians, fellows, residents, a nurse practitioner, a pharmacist, a transplant nurse, a medical assistant, and patients. Much about this clinic was comparable to the hematology/oncology clinic: the awkward organization of the doctor’s office, the communal computers, discussions of patients between fellow and attending physician, and writing notes.
Medical staff in the GI/Hep clinic use Cerner, as well as a system called Provation that allows for easy analysis of endoscopic and colonoscopic images.
Something unique about the GI clinic is that each patient is visited by 3-4 people: the pharmacist, nurse, fellow, and attending physician. Each person is there for a different reason, but the patient still has to repeat their symptoms and concerns for each. I enjoyed observing differences and similarities in technique. As they are asking questions, everyone except for the attending physician sits at the computer the entire time and only looks up from their notes every once in a while. This is also different from the oncology clinic—there, the fellows wrote down the information by hand and transferred it to online notes after the appointment. It seems like typing the notes is actually very distracting and makes the patient feel awkward and ignored, even though the notes are all about them.
In one particular case, a patient could only speak Spanish, so they brought in Ivan, the infamous tablet translator to help. As the interpreter was speaking in Spanish to the patient, the fellow was typing very loudly on the computer so I could barely hear what was being said. There were actually many issues with setting up Ivan—in one case it took the nurse about 30 minutes to set up the Cantonese translator, resulting in a 3 hour appointment for the patient.
Imaging the upper digestive system is typically done with an endoscopy, where a tube with a camera and light at one end are inserted into a patient’s mouth and moved down the esophagus, through the stomach, and into the duodenum. The lower digestive system is imaged in a colonoscopy, where a tube is inserted into the anus to image the rectum and colon. We talked with one attending physician extensively about camera capsules that a patient swallows to image the small intestine. The capsule is not retrieved after it travels through the digestive system; rather, the images are transmitted to a device clipped onto the patient’s belt. Because of the small focal length of the camera, it is really only good for imaging the small intestine—it bounces around too much in the stomach and is too small to visualize the colon properly. These imaging techniques can find ulcers (stomach), polyps (colon), cancer, inflammation, and other diagnostic features that will steer the doctor towards a certain treatment regimen.
I also saw an ultrasound! A patient complained of some RUQ (right upper quadrant) abdominal pain, and a fellow (Rupa) did a quick ultrasound of that area just to rule out any gallbladder problems. She first had the patient lay back on the bed and rubbed some blue gel onto her stomach. Then, Rupa grabbed a probe from the portable ultrasound machine and rubbed it back and forth in the area until she located the liver. She then moved down a bit and found the gallbladder. The image below was found online, but it’s comparable to what I saw. The gallbladder looks black underneath the liver, and any white marks inside of it might indicate gallstones. I had never seen an ultrasound before and was surprised by how truly real-time it is. During the procedure, the patient actually felt uncomfortable with so many people watching her, so Mark and Dr. Carroll left the room. Both the patient and I were surprised with how quick the ultrasound lasted, as it was only about 1-2 minutes, since Rupa was only looking for one thing.
Below I am including some images of the physician’s office. The first image shows the station where doctors can look more closely at endoscopic/colonoscopic images with a larger monitor. The middle image shows the printer and table where doctors put food they bring to share. Everyone was incredibly friendly, and offered Mark and I grapes, turkish candy, and peaches. The last image shows one of the computer stations. On the wall are several papers that pertain to both GI and liver disease.
source for ultrasound image: BCF technology (http://www.uk-ireland.bcftechnology.com)
Week 4, Part 2: The Patient Experience
Marianne Palczewski Blog

On Thursday, Mark and I got the chance to really connect with a liver transplant patient—we spent about 1 hour just talking to him in his room. We came in with the nurse practitioner, and stayed in his room as the pharmacist, fellow, and doctor came in and out. He confirmed what we learned from the medical assistant about the flow of the clinic. First, the patients check in at the front desk. They wait in the waiting room until their names are called. Then, the medical assistant will show them to their room, taking their vital signs and conducting a physical assessment. The patient then waits in the room until the pharmacist, nurse, or fellow come in. There is no real order here; it just depends on how many patients there are and who is free first. The pharmacist asks about the medications they are taking and if they are experiencing any side effects. The nurse will also ask about side effects and general symptoms. If it is a new consult, the fellow will ask enough questions to establish a medical history, but if not he will conduct a physical examination and again listen to any symptoms the patient is having. The fellow then goes to the doctor’s office and tells the attending everything he/she learned and suggests a possible treatment. The attending will then comment and the two will come up with an appropriate plan of attack. The attending and fellow then come in at the end and give the patient his final recommendation and examination.
I asked the patient if he thought the procedure was too repetitive, and he stated that it was a little bit, but he didn’t really mind since everyone had to write a different report. He seemed glad that everyone was concerned about him and wanted to help him.
The patient also told us about the transplant process, including the waiting list, the operation itself, and the liver disease present in his family. After patients have their transplant, they must take a very high dose of prograph, an immunosuppression drug. After some time, the dose is lowered until an optimal dose is reached—the patient will then take that dose for the rest of their lives. In some cases, the body will reject the new liver. Typically, the only solution to this is to give the patient a higher dose of immunosuppressant drugs and wait for another liver transplant donor. I was very surprised by this. It’s hard to imagine that the rejection of a large organ like the liver wouldn’t have an incredible toxic effect on a patient.
Most patients in the liver clinic have actually had liver transplants or are planning to get one soon. Otherwise, they have hepatitis C or some type of liver cancer. We actually sat in on several consultations where the patient had sunglasses on. Dr. Boulay, the attending on Friday, said that this is very common—hepatitis C tends to make the white of the eyes yellow because of the high levels of bilirubin.
Hepatitis C medication have come a long way in recent years. In the past, a very painful shot was injected into the abdomen, and this drug actually did not cure the disease. Now, a simple pill is given to the patient for 12 months and he/she is cured. There were a few patients who were living with hepatitis C and did not want treatment for fear of the older medication. The nurse and attending physician tried to explain to one patient that the new medicine was about 97% effective and had close to no side effects, but he stated that “if it ain’t broke, don’t fix it” since he did not have very strong symptoms from it.
Mark and I later met a patient who had a transplant two weeks earlier, and still had staples in his stomach where it was opened for the operation. He also had a JP drain in place, which looked like a urine bag to me. A JP drain (Jackson-Pratt Drain) is a suction device that is used post-operatively to collect excess fluids from surgical sites (which in this case was right underneath the liver). The yellow fluids were collected in a clear container that the patient had strapped to his pants. About 6 inches of the drain was actually inside of the patient’s abdomen, since the drain exited the body near his pelvis. This was done so the surgical site would not be exposed to potential infection. The doctor took this out, along with his staples. He used what looked like a staple remover at the end of a small pair of metal scissors. This was really interesting to watch, and the patient looked like he didn’t feel it at all. The doctor then put sterile tape on the incision to make sure it wouldn’t open up.
After seeing a few more patients, I noticed that each of them was taking 5-15 pills each day. I asked the pharmacists if patients ever mix up their drugs, and she said that it actually happens all the time. I thought of an idea for a pill dispenser to be used by patients in their homes. The patient could input what they were supposed to be taking and how they should take it, and the machine would take the pills out of their bottles and distribute them each day, displaying instructions if prompted. Or, another option is for the doctor to control the dispensing of the drugs, even communicating with the patient through the device. For example, if a patient’s blood work comes back with a very high level of creatine, the doctor could tell the device to give the patient a lower dose of prograph instead of having to call the patient and tell him/her to take a lower dose.
On another note, I really enjoyed shadowing Dr. Boulay. He uses candid language when talking to the patient, which makes him seem more trustworthy. He also does not use the computer at all when in the examination room. He prints out the patient’s records and writes notes on them, which he then transfers to a computer that evening at home. He also showed us some youtube videos and interesting information.
We also talked about how one of the main medications for certain GI problems is to take an antidepressant. However, if a patient is already taking antidepressants, adding any more drugs of that class can lead to serotonin syndrome, which can be potentially deadly. I always knew the brain and gut were closely related, but I had no idea that antidepressants could make both your mind and stomach happier.
Finally, the last patient we were with on Friday was asking about allopathic medicines to cure ulcerative colitis, such as ginger root and herbal tea. The attending physician said that she doesn’t want to discredit them, but just doesn’t know enough about them to say whether or not they will help his condition. I was really surprised by this, since nutrition and diet seems like it should be key in the field of gastroenterology. Not a lot of actual diet advice was given to any of the patients I observed.
Below are a few more images of the doctor’s office and the clinic entrance.
Week 5, Part 1: At last!
Marianne Palczewski Blog

Today we finally saw an upper endoscopy (EGD) and colonoscopy, and on the same patient! The procedure surpassed all expectations. I had never seen any type of surgery in Oncology, so this was a particularly fascinating experience.
Before a colonoscopy, patients have to drink 4 liters of a solution called “Go Lightly” which will clear out their intestines. Before endoscopies, they have to refrain from eating for several hours before the procedure. When the patient first enters the room, he/she is anesthetized using two drugs that are injected intravenously. The patient then enters a “twilight” stage, which is halfway between no anesthesia and complete anesthesia. The tolerance for these drugs widely varies from patient to patient, and different people can remember different aspects of the procedure. In some cases the patient is actually able to hold a full conversation with the doctor while he is performing the colonoscopy!
The sheer number of devices in the room was a bit overwhelming at first. Next to the patient’s bed is a large monitor that the doctor looks at while scoping. Near where the doctor stands is the processor for the scope as well as the cauterizing machine. Next to the processor is a cart which holds the water reservoir and specimen jars. The scopes for EGDs and colonoscopies are very similar, save for their diameters. At the end that goes into the patient, there is an LED light and a digital camera. Most of these scopes have three channels in addition to the fiber optic cable that transmits the video to the screen. These channels are for air, water, and tools, such as biopsy forceps or snares. In the middle of the scope is the control center, where doctors can direct where the scope will turn and how much water and air to use. The scope then plugs into a console, with separate plugs for the image processor and the light source. Different scope diameters are reserved for different procedures and patient sizes.
In colonoscopies, polyps are removed using snares. These tools come in many different shapes and sizes depending on the orientation and size of the polyp. The three we saw were the standard circular, lariat, and duck-billed. The removal of one of the polyps took three attempts with two different types of snares to get everything. The cauterizing machine has two settings: cut and coagulate. These two are used in varying amounts to remove the polyp. After the polyp was cut off of the GI wall, the doctor turned on the suction feature and just removed the endoscope with the suction on the whole time, which pulled the polyp out. Another option would be to insert the net tool, which can grab the polyp, allowing the nurse to remove it through the channel.
During endoscopies, an interesting green plastic device is used to restrict the patient’s tongue and allow the scope to enter the mouth easily. Also, before the scope is inserted, it is lubricated using a packet of sterile jelly that is poured onto a square of gauze and then rubbed onto the scope. The same is done during colonoscopies. To me, this seemed like a waste of the packaging since one full package was used per patient, and only one half got onto the scope. Perhaps it could be dispensed in a different way.
It was remarkable to see the insides of a patient lying right in front of me. In the first colonoscopy we saw, the intestines were lined with a yellow liquid that looked like bile (which was actually stool). In almost every procedure the doctor would take several tissue biopsies from different parts of the GI tract. These biopsies, or “bites,” were taken with a biopsy forceps that looks like a tiny clamp with a needle in the middle to hold onto the tissues. The biopsies are taken out through the channel and dumped into a very large jar filled with water.
image source: http://g.vatgia.vn/gallery_img/14/dbm1397362828.jpg
There was quite a bit of blood that seeped out of every “bite,” but Dr. Cemal said that it would not typically cause infection unless the bite went too deep.
During the procedure, a nurse monitored the patient’s heart rate, end tidal carbon dioxide level, respiration, and blood pressure. One of the most interesting things I noticed during the procedure was the interaction between the doctor and the nurse when using the forceps or snare. The doctor controls where the scope/tool is oriented, but the nurse controls the opening and closing of the tool. For example, while injecting methylene blue, a chemical that helps distinguish polyp tissue from regular mucosa, the doctor put the needle next to the tissue and said “Inject.” The nurse would inject and say “injecting…injecting…injecting” until the doctor told her to stop. There were 4-5 people in the room and they all watched the screen and discussed what they saw.
Week 5, Part 2: Scope Cleaning and a Stressful Bronchoscopy
Marianne Palczewski Blog

After a few days of seeing the scopes in action, Mark and I decided to check out the endoscope cleaning room. A technician, Shay, explained the process of cleaning the scopes as well as how the machines worked. The process actually begins in the procedure room, where the inside and outside of the scope are flushed with an enzyme cleaning solution. The scope and associated components are then sealed up in a drawstring bag and transported to the cleaning room.
Here, the technician will first remove all buttons, check that the motor is sealed in its air-tight container, and brush clean every button and opening two times. Every opening is then flushed with the enzyme detergent. The sink is then drained and fresh water is poured in and used to clean the detergent out of the scope. At this point, the scope is moved to the washing machine, which looks and sounds like a unique dishwasher. The scope is sprayed with alcohol, and the various IDs are scanned, namely the patient ID, scope ID, cleaner cassette ID, and the technician’s own ID.
When this is done, the scope is taken out, dried, capped with a green foam cylinder, and placed in a closet to hang. There are closets specific to the scope type. Everything must be handled with gloves to maintain sterility.
It was very interesting to observe the scope while it was in the washing machine. Each machine can handle two scopes at a time, and it uses a potent solution to clean everything properly. There is a metal bar that rotates and ejects water onto the scope at different intervals.
On Wednesday, Mark and I observed a bronchoscopy with Namrata. There were two fellows, an attending physician, a nurse, and two nursing students in the room with us. All bronchoscopies are done in a room that is next to but separate from the GI procedures. Bronchoscopies, like endoscopies and colonoscopies, begin with patient anesthesia. A vaporizer is first used by the patient to numb her airway. She then snorts a lidocaine gel (2%) to numb the area where the scope will enter (the nasal cavity). As the scope progresses down the airway, lidocaine is injected via syringe into the scope before hitting any new branch (primary bronchus, secondary bronchus, etc). In this procedure, we saw a few bumps on the bronchus which later turned out to be cancerous.
This particular bronchoscopy made me extremely uncomfortable and stressed. It was the fellow’s first time, and the attending was screaming at him whenever he did something incorrectly. This led to the fellow becoming more stressed, which led to more mistakes, which led to more pain and coughing for the patient, which caused the endoscope to hit the tracheal and bronchial wall, which resulted in a blood-filled airway that was impossible to navigate! The 15 minute procedure turned into 2 hours of pain for everyone in the room.
Before there was blood everywhere, I could see the scope travel down the trachea and into the left lobe. It was here that I was particularly thankful for my year in anatomy class as I knew exactly what I was seeing. Even though I knew what I was looking at, I still found it incredible to see the lungs from this perspective. The most interesting part was looking at the trachea when the patient coughed. The back of the trachea contracted in a unique way that I now think of every time I cough myself.
Week 6, Part 1: A Venture through Procedure Room 5
Marianne Palczewski Blog

In the beginning of our last week, Mark and I decided to divide our time between following around Dr. KumKum Patel and just jumping into any interesting procedures going on. We followed Dr. Patel up to the 7th floor of the main hospital to listen in on some inpatient rounds discussions. Here we listened to five doctors talk about the status of 5 patients in the GI inpatient wing. Much like in Hematology/Oncology, the doctors discussed the protein and electrolyte level of each patient as well as any side effects from medications. The main difference between rounds here and in oncology was that almost every patient was to have a colonoscopy or endoscopy at some time in the future.
The two most interesting and unique procedures we observed were endoscopic ultrasonography (EUS) and endoscopic retrograde cholangiopancreatography (ERCP). Most of these procedures are done in procedure room 5, which has arrangements for general anesthesia and x-ray imaging. Double balloon enteroscopies (DBE, to examine the small bowel) are also done here, although we did not see one.
The first procedure with ERCP was done to place stents to transport bile. Two stents were placed into the common bile duct and pancreatic duct through the hepatopancreatic ampulla in the duodenum. The ERCP scope has the camera on the side rather than in the front, so it is tricky to maneuver the scope down the GI tract. However, once it hits the duodenum, the side facing camera makes it easy to visualize anatomical features on the wall, such as the ampulla. One monitor displayed the camera on the scope, and two monitors displayed an x ray image that was being taken of the patient’s abdomen. After injecting contrast into the bile ducts, the doctors could see where they were aiming for and they could make sure they were placing the stents in the right spot. These plastic stents need to be replaced every 3 or so months, so this is a relatively common procedure for the doctors.
During each ERCP, everyone in the room had to wear a lead apron to protect their bodies from any stray radiation beams, including Mark and myself. The most interesting aspect of this first ERCP was that I saw the stents both outside of the body on the tray and inside of the body on the scope camera and on the X-ray. Comparing the old, brown stent to the new, blue stent was also very interesting. The stents turn brown because of how much bile they come into contact with.
Another interesting case was a patient that received an EGD, EUS, and ERCP one right after the other! The whole operation took 4-5 hours. The EGD was very quick and was just done diagnostically to see if there were any ulcers that might be missed with the more specialized scopes. Next, the EUS was done with a different scope. This scope had a camera but also had an ultrasound probe at the end. A balloon was filled with water and placed on the end of the scope to minimize interference from interaction with a different medium (air). The scope also had an attachment that was inserted into the portable ultrasound machine (pictured below). As the doctors used this probe, they looked at the ultrasound machine the entire time, and could see different organs such as the pancreas, liver, and gallbladder. In this case they were looking for a possible tumor mass that could explain the patient’s weight loss and painless jaundice.
The ultrasound was inconclusive save for some irregularity with the ampulla, so they decided to do an ERCP to see the ampulla more closely and take a few biopsies. The ampulla was extremely large and the bile ducts were blocked, so they used a needle knife tool to cut it open and release the bile. The needle knife was essentially a hot needle that was pressed against tissue and broke it apart. As it cut through the ampulla, I saw smoke on the screen, which was very odd to see inside the human body. They actually had to bring in a separate machine to use the needle knife. Attached to this machine were blue and yellow pedals that the doctor could press depending on which setting he desired. The settings were either cut, which resulted in more bleeding but a faster cut, or cauterize, which had less bleeding but a less precise incision. For this case, the doctor just cut right through the ampulla. I really enjoyed observing this procedure, and felt especially honored to see it since one of the fellows said he had never seen it before!
After this experience, I finally understood what my classmates felt when they complained about foot pain during long procedures.
Week 6, Part 2: A Look Inside GI
Marianne Palczewski Blog
In our last few days in gastroenterology, we observed a few colonoscopies and EGDs, and tried to really hone in on the clinical needs in our department.
Something interesting I noticed during a colonoscopy is that there were three different settings that the doctor could switch between to visualize the colon better. The Pentax endoscopy system has three iScan image enhancement settings to visualize different types of lesions. iScan1 is involved in surface enhancement, and enhances structures by edge recognition. iScan2 (which we saw used most frequently aside from the normal setting) is done to enhance contrast, and the doctors used it in patients suspected to have dysphagia. iScan3 is a tone enhancement, and modifies the “combination of RGB components for each pixel” to enhance individual organs.
Gastroenterology differs from other specialties in that the doctors don’t know what they will be treating until they get inside of the patient. For example, during routine colonoscopy screenings (which are recommended for all patients above age 50) doctors recognize and treat any polyps that they see. In most other fields, the doctors know what they will be doing and what tools they need to use. In GI, all tools need to be kept on hand and all nurses and doctors need to be prepared for any eventuality.
An emerging field of research in gastroenterology is the capsule endoscopy (see below), which I mentioned in an earlier blog. We decided to look into capsule cameras for the colon, which have only recently been made. An issue with these capsules is that they only identify 60-70% of true polyps and falsely identify 10-20% of polyps that don’t exist. The likely problem here is that in the colon has pouches called haustra. These pouches are difficult to visualize with only a front facing camera. We considered series of 2-4 cameras that could be placed along the length of the pill that would allow for visualization of all angles of the colon. Another possibility is to develop image analysis software that would ensure the doctors don’t miss any abnormalities in the gut.
Image source: http://mayoclinichealthsystem.org/locations/eau-claire/medical-services/gastroenterology-and-hepatology/capsule-endoscopy
Another problem with capsule endoscopies is that in patients with slow stomachs, the battery may die and not record crucial area of the digestive tract. To remedy this, we considered a wireless/inductive charger that would be attached to the electrodes that stem from the receiver (see image below). There would be tiny coils of wire in this charger that would generate flux and charge the pill. The electrodes themselves could also be charged wirelessly, or could be powered with a more powerful battery.
Image source: http://www.sgihealth.com/capsule-endoscopy/
After analyzing all of our data, we presented to Dr. Patel on Thursday. She suggested that the electromagnetic field created by the recharging feature could interfere with pacemakers and defibrillators, which many of these older patients have. The solution to this, then, could be to only use it for patients without pacemakers or to develop a short range magnetic field that would not radiate more than 1-2 inches from the electrode.
On Friday, we met as a class and presented and discussed our rotations and what we gained through this experience. Overall, I found this rotation to be amazing, from both a technical and a personal standpoint. I am glad I chose GI, and was happy with how much I learned from both patients and physicians!
Mark Hillstrom Heading link

Hello, I will be a senior bioengineering student concentrating in medical imaging starting this fall. The clinical immersion experience will surely provide myself and the other interns with invaluable knowledge of the relationship between machines designed by bioengineers and the end users themselves, namely physicians and nurses. I am super excited for the next six weeks. Let the blogging begin!
Mark Hillstrom Blog Heading link
-
Mark Hillstrom Blog
First Day
Monday July 6 2015
Mark Hillstrom Blog

Today was a very eventful first day of the clinical immersion experience. We began with a brief orientation at the innovation center (which I had never been to) which included bagels and some meet and greet. Dr. Kotche and Susan shared some great information and past stories with us. They also provided us a solid framework of the weeks to come including deadlines and a great deal of worthwhile advice. Overall a very productive morning. For the first three-week rotation I am paired with Jagan. We discussed some hopes and fears we have toward the next six weeks during the morning session and decided to walk to west campus just after being dismissed from the innovation center. It was a good walk. We caught up with Misia, Julie, and Tiana about half way to 1700 West Taylor and all five of us walked together for a bit before parting ways. Jagan and I went to SCW to sit and relax a little before our 1:00 pm start time.
We arrived at the hospital around 12:50 pm and proceeded to find the elevators. We had no problem gaining access because the security man saw our handy dandy badges. The next fifteen minutes were a bit hectic. We had to check out a scrubs-vending-machine-card which is just as it sounds. Jagan and I eventually found it after asking some nice people for directions, checked out scrubs from the machine, and proceeded to ask more nice people to direct us toward the changing room.
After changing we were told that Urology surgeries were taking place in rooms 4 and 17 today. So we decided to visit room 17 first. After we approached the room and peeked through the door it was obvious the room was very crowded. Room 17 was one of the smaller ORs on the floor. We didn’t feel comfortable entering a room full of people with masks who looked quite serious so we decided not to enter. Not sure where to go next, we walked to room 4. This room was being sterilized as a surgery had just ended. We met a very nice nurse and anesthesiologist nurse (not the proper title) who explained much of the room’s equipment to us. These included a ventilator, power supplies, and the cauterization tool. The room is pictured below (). Because the patient had eaten food earlier in the day, the next surgery had been postponed to 3:30 pm. The nurse said that usually patients must abstain from eating for at least 6 hours before surgery, 8 hours in some cases. So Jagan and I migrated back to the smaller operating room 17 to see what was happening there.
I guess when we peeked through the window before everyone was just setting up. When we arrived back there were medical students in the hallway picking out lead vests with supplemental lead neck coverings. The procedure was being done on a morbidly obese patient who had recently underwent gastric bypass surgery and was currently suffering from a subsequent kidney stone. The vests were needed because x-ray images were being taken throughout the procedure. I made the mistake of choosing a vest that covered my entire torso but fell just short of protecting my male parts from radiation. The nice nurse noticed this and told me halfway through and advised me to stand behind Jagan (who picked a vest of adequate length). I decided to just leave the room and find a longer vest to be better protected. Hopefully the short exposure did not cause any significant damage (fingers crossed). The situation caused me to remember my parents telling me that when they were kids they used to play with liquid mercury balls when a thermometer broke and see a live x-ray of their feet while at the shoe store. Back on topic. After this procedure Jagan and I talked with the medical students, residents, and the attending physician briefly. We told them a little about ourselves, the internship we were a part of, and what we hope to learn in the coming six weeks.
Jagan and I then walked back to the larger OR (room 4) as did most of the people from the procedure that just occurred in room 17. People are required to wear masks in the OR and someone needs to be in the room at all times to supervise and make sure none of the equipment and sterilized tools are tampered with. The man was eventually brought in for surgery. He complained of difficulty urinating. This surgery was absolutely fascinating to witness. The surgeons went right in through his urethra and eventually found a narrowing section just before the bladder. Many methods were used to penetrate a tough section of built-up scar tissue from a previous surgery. The tool the surgeons used has two functions: to cut tissue and to cauterize tissue if blood vessels are punctured. The whole process is monitored in real time from the monitor. The clump of tissue was stubborn and the surgeons were making little progress with the electric cutting tool, so they switched gears to what looked like an x-acto knife. After a few swipes and jabs, they broke into the bladder. There was a mild cheer from the audience and a subtle fist clench from the physician. Next the electric cutting tool was reinserted and the abnormal growth began to be trimmed. It was so neat to watch this on the monitor. We even had access to the two ureters (which connect both kidneys to the bladder). As the trimming continued we came across a few staples that must have been leftovers from a previous surgery. As the obstruction between bladder and urethra was slowly sheared away, a large amount of urine began flowing. The whole procedure was just incredible to observe. I guess I had this preconception that surgeries dealing with male/female reproductive organs would be more finessed and gentle. It was anything but. At times violent and thrusting to acquire the best angle. A giant rod needs to be inserted into the urethra. It is here that cuts are made and cauterized when made too deep and capillaries burst. The reproductive organs are dense with nerves so it’s a good thing patients are sedated during these procedures.
I assume the patient will be quite sore over the next few days.
Second Half Week One
Saturday July 11, 2015
Mark Hillstrom Blog

Since last entry was a little engineering-light, I’ll try to focus more on the devices this time around. Jagan and I have been exposed to a whole slew of new machines and procedures over the past few days. Urologic procedures in the OR take place on Mondays, Thursdays, and Fridays. Tuesdays and Wednesdays are spent in the clinic. Although procedures do take place in the clinic environment, they are much less invasive. There is a small “procedure room” among the less well-equipped rooms in the clinic where we observed an ultrasound guided prostate biopsy. All procedures performed in the clinic are done with the patient awake. Sometimes lidocaine is used to numb entry points and make the experience more bearable and comfortable for the patient. Some of the equipment we encountered in clinic are pictured below. One piece I found interesting was a translating machine. Turns out the hospital contracts this function to a separate company who provides either video or audio real-time calling. It seemed pretty simple to use and had eight languages listed with more available to search. These included Spanish, Chinese, Korean, polish, french, … you name it. Language barriers are sometimes very difficult to overcome so I was happy to see this machine in place to help people who may not be super familiar with the English language. :o)
Thursday and Friday were by far my favorite days of the internship thus far. Thursday Jagan and I witness an extremely rate 8 hour ureter resection. The patient had her right kidney removed previously (nephrectomy) with the left ureter exiting the left kidney in a zig-zag shape and connecting to the right ureter entry point into the bladder. I’ll never forget the rest of my life when the surgeon literally cut the patient’s small intestine in two because the procedure had to be modified which meant they had to feed urine from her kidney into the small intestine using a piece of the small intestine as tubing. It was a complete mess and I felt so sorry for her. She probably won’t live much longer. It was however a fantastic learning experience as Jagan and I and the medical students witness real-time peristalsis of her intestines. So incredible. The kidneys are located along the back wall abdominal cavity and the surgeons entered her body through the front. So they were forced to shove aside all sorts of organs just to reach the left kidney. Very cool to see. They used a gauze-like pad at one point called “Surgiskin” to absorb blood quickly. The pad is convenient in that it can be left inside the patient. One more interesting point. Just “opening up” the patient took 2 hours. This involves making the correct cuts and familiarizing yourself with the patient’s insides.
Friday included just two procedures, both involving the DaVinci robotic machine. The first was a partial kidney nephrectomy to remove a cyst attached to the right kidney and also to remove the right adrenal gland. I never realized how compartmentalized the body is. Each organ is anchored to structures which are encapsulated with various tissues that are then protected with even more attachments. The design also provides a nice cushion. The woman undergoing this procedure weighed around ~400 lbs so just finding the kidney and rummaging through the caverns of excess fat was a challenge. The doctors had to be extremely careful as the vena cava and ovarian vein were in super close proximity to the points of interest. I swear it was just like a scavenger hunt or video game. Except if you opened the wrong door (cut in the wrong area) someone would die. The doctors are equipped with an expert level of anatomical knowledge but still encounter challenges when determining what is what and where certain organs are and also the next steps to take. There were a few times when a staple or needed or some other instrument would be dropped inside the body. Recovering such small leftover pieces of equipment must be daunting and super stressful. What if you can’t find it? Gosh I don’t even want to imagine.
The second procedure Friday was a prostatectomy. Midway through one of the sixth year residents left the room to assist another doctor in a separate OR. This freed up one of the two control consoles of the DaVinci robot (other console was being controlled by Dr. Abern). I was privileged to watch the 3D action from the unoccupied console. It was amazing to witness. Watching the masterful technique of a skilled surgeon operate this machine is just beautiful. All the movements flow smoothly. So to prep the robot 4 entry points are made in the beginning of the surgery. Once inside the body, the operator is equipped with a few tools. One is called the bipolar dissecting forceps and is used to electrically cut, cauterize, and coagulate blood. It can also act as a non-electrical cutting tool. The second tool used was a forceps. I’ve been reading about all the attachments through the website, but basically it’s a gripping tool. It never slipped during the procedure and is so amazing to watch in action. It looks like two paper clips lines with serrated teeth that clamp together. One observation made was that all machines in the OR are situated on top of wheels. This is convenient but also sometimes cumbersome as the wires attaching each machine to an outlet can become tangled. I really love this internship so far.
One aspect of our medical system that I noticed and thought about excluding from this entry because it may not be deemed relevant or appropriate is the fact that a significant percentage of people undergoing these surgeries are grossly obese. Sure there are genetic causes but overwhelmingly a person’s (excess) weight is their decision. There have been such incredible advances in medicine in recent times that it just seems so wasteful for patients to undergo extraordinarily complex procedures when the most effective treatment could be the simple choice to eat more carrots, and less cake. As bioengineers I think we all have a deep-rooted desire to help people. But it’s difficult to have sympathy (at least for me) for people who have eaten their way into oblivion and don’t want to help themselves. People in less rich countries don’t even have access to simple antibiotics, yet alone a $2 million dollar DaVinci surgical robot machine. Sorry if the above sounded cruel, it’s just how I see it.
I also apologize for the one day late and less descriptive entry – somehow my notebook with tons of good information was misplaced on Friday after leaving the internship. I’ve been searching extra hard and trying to retrace my steps but so far no luck. It will show up eventually. I hope the descriptions in this entry were adequate – they were produced all from memory. I really want to share more because there are so many extraordinary things we are seeing and learning!!! That statement is genuine. Can’t wait for Monday.
Week Two Part One
Wednesday July 15, 2015
Mark Hillstrom Blog

It is now the third day of week two and Jagan and I are in full swing urology immersion. The week began in the OR where we witnessed a few interesting and notable procedures. One was a circumcision performed on a ~25 year old male. The procedure was more complex than one might think. This man had a sort of congenital permanently encapsulating foreskin that the physicians had to forcefully excise using a few snips of the scissors. They then had to peel back the excess skin and cauterize the trickling blood vessels. It was a little disturbing. But the procedure will change this man’s life forever. Which is amazing. All instruments used throughout this procedure were pretty basic. Somehow I became amazed by all the little kits used by physicians and nurse’s alike. There is a disposable kit for everything. Cleaning the area of interest with iodine, grab a kit. Need to insert a catheter? Grab a kit. Manufacturers must make a fortune. Everything is throw away. Nothing is reused except the mainstay machines such as those used for imaging, lighting, power, Davinci, etc. Anyway, on to some clinical experiences.
Tuesday we had the opportunity to witness some interesting/sad cases. One man complained of urine with a pink tinge and extreme pain along his left flank. In the ER in Indiana, he underwent an abdomen CT w/wo contrast. The result was not pretty. The young man, age 42 and a former smoker, had kidney cancer with potential seeding in the bladder. It was just awful, but entirely routine for the urology staff who see on average one patient every 15 minutes on clinical days. Jagan mentioned a complete disconnect between physician and patient on an emotional basis. I agree but cite desensitization as the main culprit, not a lack of empathy. The doctored carefully explained to the sobbing patient and his mother that seeding is actually better than spreading. Because for cancer to spread, it must travel through the blood. Seeding, however, contained the cancer within the same organ system. This makes is much easier to treat and provides a higher probability of treatment success. It was interesting because the same patient just mentioned underwent a ureter/bladder biopsy to determine if the cancer had spread around 2 pm this afternoon. The attending doctor was busy performing a partial nephrectomy on a different patient using Davinci when a resident entered the room and explained to the attending physician the positive results of the biopsy. The physician gave an “Oh that’s great news!” upon hearing.
The beginning of this week has allowed Jagan and I to meet two additional attending urologists. One has over 40 years of experience. The other is a bit younger but still very experienced and an expert with the Davinci system. We’ve spent more time with the younger of the two new doctor’s the past few days and have learned a great deal. /He’s very willing to explain techniques and machines to us. He likes answering why a procedure is necessary or what treatment options were available in the past. As described before, the Davinci surgical system has three elements. A console, power supply/software and the four arms. The model used in UIC ORs is around three years old, he told us. The new machine (we looked on the website) is sleeker and has an auto attach feature that quickly finds the joining parts from arm to patient’s body. Just incredible. There is still so much improvement potential for these machines. Jagan has mentioned a few times a resistance gauge of sorts. It would act as a tissue biopsy, testing only a few parameters, but producing an accurate model of what tissues lie where. Many times during these surgeries physicians have difficulty identifying between veins, arteries, lymph tissue, connective tissue/fascia, and others. The result is most of surgery time is spend differentiating between tissues and finding/reaching the point of interests instead of on the points of interest themselves. Below are some pictures of the sterile table with instruments used during a Davinci partial nephrectomy. As shown there are multiple replacement attachments for each instrument. The other picture is the software/power component of the Davinci. Jagan and I will spend an hour after work tomorrow to brainstorm and decide on a doable/worthwhile problem statement. More to come on that in next entry. Bye for now!
Week Two Second Half
Mark Hillstrom Blog

Hello again! This week was not as eventful or jaw-dropping as the last, but Jagan and I were given the opportunity to have some quality one-on-one time with a few of the senior-level residents. The urology specialty requires a six year residency and UIC department of urology has at the moment one sixth year and one fifth year resident. There is also a first or second year resident on the team. Most of the routine procedures are performed mostly by the residents however some rarer ones are almost entirely done by the attending physician. Jagan and I were able to witness a new procedure. It was called greenlight laser therapy to treat benign prostatic hyperplasia. BPH is also know as enlargement of the prostate. Symptoms include difficulty starting flow, frequent urination, and feeling like you just didn’t get it all out. So the laser is inserted into the urethra and literally vaporizes enlarged prostate tissue near the bladder. It was pretty neat to watch and reminded me of being in a haunted house with flashing green strobe lights. The company also spared no opportunity to add as many LEDs to the device as possible. The cord was green, there were green buttons decorating the housing unit which was about the size of 1 foot x 2 feet x 4 feet cuboid. Pretty neat device. Also, there were two techs from the company present during the entire operation. They oversaw the procedure and adjusted the instruments as needed and provided advice at times. The procedure was damn bloody. There was a steady flow exiting the catheter after the resident removed the laser apparatus. At one time I wasn’t sure the flow would stop. It eventually subsided. . . I felt bad for this guy. He will undoubtedly have a rough recovery. Jagan and I then excited the room and switched rooms in hope there would be another procedure either started or even better just starting. There was a circumcision but the resident prepping the patient told us to go and read about a device that would be used in an upcoming procedure. So we did. More to come in next blog! Stay tuned!
Week Three First Half
Mark Hillstrom Blog
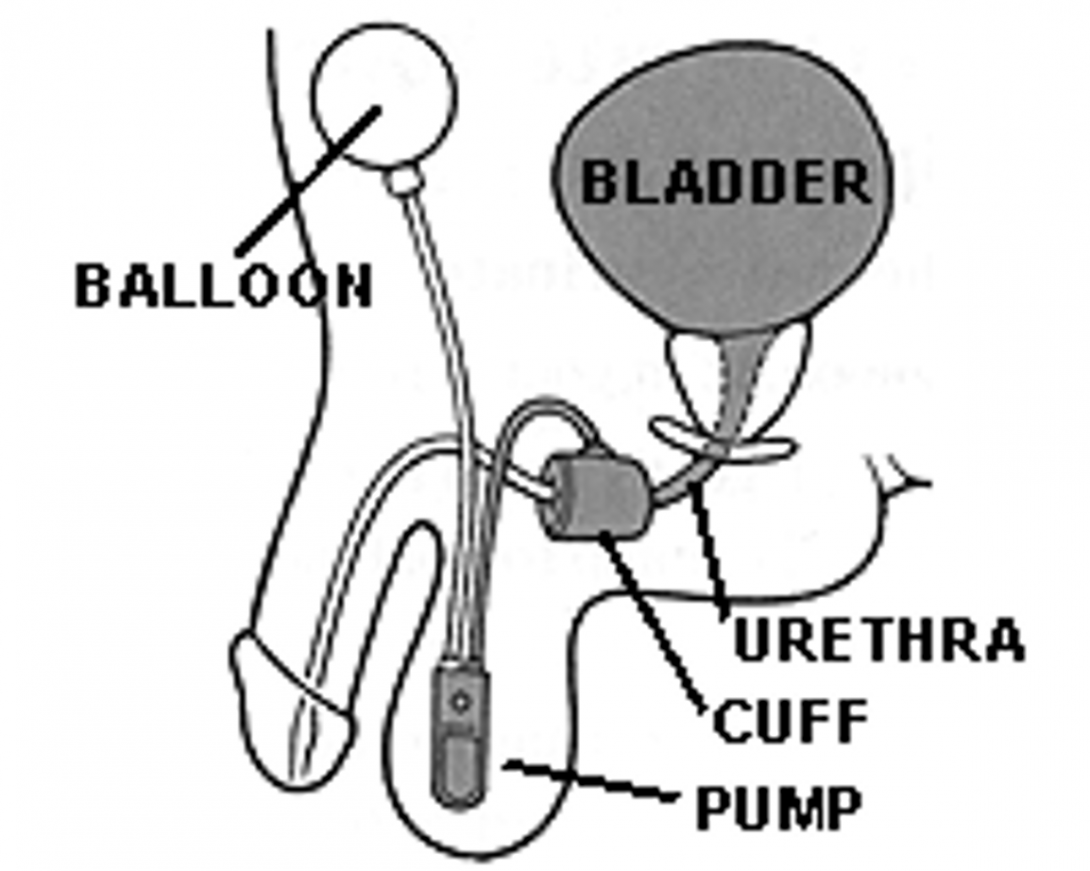
Jagan and I were lucky enough to witness the removal of an old and implantation of a new device previously unseen by us. The procedure was called artificial urinary sphincter placement. And the device is as the name suggests. We had some down time between procedures which provided ample time to learn about the device. We came across one thorough source with background and functional workings. It was actually pretty awesome because we both became immersed in the history, development of, and future implications of the device. The device is actually remarkable simple. Though the components may be difficult to see on the picture (actually, I’ll upload it as the main picture J), there are only three of them: occlusive cuff, pressure regulating balloon, control pump. This quote was found on a website but I found it very interesting, here you go: ”An artificial urinary sphincter is reserved for treatment of complex or severe stress urinary incontinence. Type III stress urinary incontinence, or intrinsic sphincteric dysfunction, is the inability of the urethra to maintain effective resting urethral closure pressure sufficient to keep the patient clinically dry at rest and during periods of reasonable physical activity.” Pretty much it’s not a common procedure and reserved only for individuals with severe incontinence but who also have the mental sufficiency and motivation to operate such a device. No Dementia permitted.
The balloon part is available in five differing pressures which are chosen based on the minimal pressure required to close the urethra entirely. The cuff also comes in varying sizes and wraps around the urethra near the bladder exit. The control pump is pretty amazing as it is placed inside the scrotum or labia and is multifunctional. It obviously deflates the cuff letting urine flow from the bladder through the urethra. But it can also be locked in the deflate position. This would be a useful feature during catheter placement. There is also a delay fill mechanism meaning after the cuff has been deflated and no additional urine remains in the bladder, the cuff re-inflates within 3-5 minutes. The fluid traveling between the balloon and cuff passes through the cuff and is unidirectional at any given time. When the patient wishes to urinate, the pump is squeeze which sends fluid from the cuff to the balloon reservoir. I would love to find the criteria for cuff size selection. And how the designers came up with proper tubing lengths between balloon and control and control and cuff. The device is so simple yet improves a select few people’s lives tremendously. When urinary incontinence becomes this severe, the patient must either choose between having permanent catheter inside their urethra at all times with accompanying urine drainage bag or undergoing the artificial sphincter placement procedure.
This is related to the last device and procedure. Many of the devices used throughout urologic surgeries seem entirely mechanical and dated in a way. I don’t mean this in a bad way. But I do see a huge opportunity to improve many of them. Many of the devices and machines (minus robot) were designed in decades past and remain little unchanged. There is this massive window of opportunity to improve basically every part of a surgery. The new DaVinci system proves this. One of the doctors recently explained to us how the new model (released this year) automatically “finds” the insertion holes in the patient and connects to them automatically. This makes moving the sometimes cumbersome machine across the room and lining up each and every hole obsolete. Step by step these little changes will continue taking place. The next decades are going to be exciting.
Last Half Week Three
Mark Hillstrom Blog
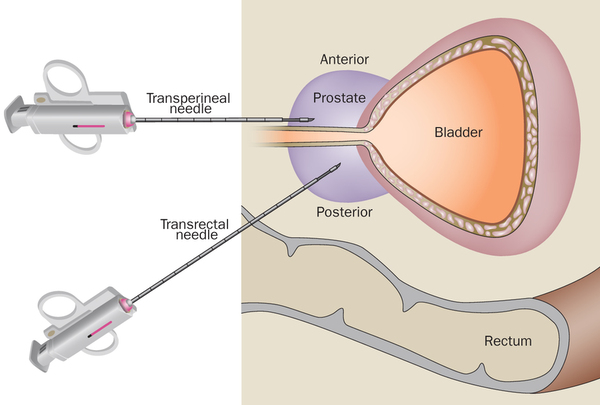
Today (7/23/15) is the second to last day of our Urology rotation. We decided to visit the University Center for Urology located at 60 East Delaware. This facility caters to patients with private insurance. Overall, the facility is very similar to the clinic located in the medical campus. Actually the medicaid facility had newer equipment, larger rooms, and more working space. Maybe because the volume of patients is that much greater. It would be interesting to see some numbers. Pretty much Jagan and I saw a prostate 12 core ultrasound guided prostate biopsy. It was fun to watch. Before this the physician looked through and eyepiece attached to a flexible cystoscope to examine the inside of the patient’s bladder wall. it was interesting because Jagan and I have seen this procedure done tens of times before in the OR while the patient was under general anesthesia. In the OR, sometimes patients would be awake and numbed if the cystoscopy was simply a visual examination. If the urethra had to be resected the patient would not be awake. Urology has been an incredible experience and I am going to miss it. The people we’ve had the opportunity to interact with have been amazing.
The last day of Urology rotation also allowed us the privilege of witnessing a semi-catastrophic event. During a routine nephrectomy a resident physician accidentally trimmed too much supporting tissue near the renal vein. This caused the blood vessel to tear and blood to openly flow through an unknown location. The attending physician quickly realized the gravity of the situation and told the resident to scrub in. They two men switched places and the physician began work locating and fixing the tear. Tributary vessels had to be clamped shut and cut. All in all, I think around 15 clamps were used. Some of the vessels were so large in diameter that the clamp barely fit. Even though the scale of Davinci camera is small, there was significant blood loss. I remember thinking to myself while watching the entire situation in 3D through the second console that this patient was going to die. The entire room remained calm throughout. Incidents like this must be commonplace. Attending surgeons with 20 year experience have seen mostly every situation imaginable, and then some. It was fascinating to watch and I feel extremely privileged.
Week One GI/Liver Clinic Part One
GI Week One
Mark Hillstrom Blog
Misia and I are super excited after hearing so much about the wonders of GI rotation. On the first day we were greeted by one attending, one fellow, and one hepatologist. We were quickly thrown into the mix and began seeing patients. I remember being super happy at this time after not being charged for a double chocolate cookie at Subway. The order was also inputted wrongly in that the sandwich listed on the receipt was a turkey when in fact I had chicken teriyaki. Muahaha, anyways, back to GI. The first patient we saw was an older woman in her late 70s who was falling apart. It was pretty sad. She had lung, heart, liver, bone, diabetes, and heartburn issues. She was also too frail to undergo an upper GI scope. This type of procedure is essential to determine esophageal, stomach, and beginnings of the small intestinal tract health. The doctor present was very thorough and nice. He slowly indicated what he was doing each and every step with comments like “Going to open a note here. . . “. The next patient we saw was a 44 yr old with acid reflux. Nothing too remarkable happened there. We next saw a patient with fatty liver. The doctor was slightly concerned about H Pylori infection. For this patient a translator service called “Ivan” was used. It worked nicely, although Namrata is right in saying a smartphone is just as capable. The language translator service must cost a pretty penny. For this patient the doctor recommended pancreatic enzyme and amylase tests. One physician was nice enough to explain the difference between sensitivity and specificity to us. So far Misia and I have absorbed information just like little sponges.
One realization even more pronounced this rotation is the omnipresent patient fatness. It’s pretty disgusting. I’m not sure why but not one physician/nurse/PA has remotely suggested to a patient that he/she change their dietary habits. This really bothers me. Many diseases of the gut are caused by inflammation. The main driver of inflammation is the immune system’s overresponse to a perceived threat. Feeding your body food with little nutrition, little fiber, and lots of sugar is a recipe for disaster. Instead we as an advanced society choose to load people up with countless medications. It would be neat to see doctors prescribe patients vegetables. Wow, that sounded so earth-loving. Anyways, the next patient had multiple complaints including HA and neck pain. It was interesting to learn that narcotics and marijuana slow gut motility.
The second day of GI/Liver rotation was all about livers. Many people we had the privilege of meeting were transplant patients who had just recently undergone surgery and were in the recovery stage. I learned that for the rest of their lives these people must take immunosuppressant drugs. The days, weeks, and months following a transplant surgery are forth telling to the patient’s future prognosis. We spoke to one good spirited man who had surgery the 6th of July, so around three weeks ago. We were in the room for one and half hours with him while various professionals entered/exited the room (pharmacist, attending, nurse…). He was so friendly and told us he was walking the second day after surgery. His older brother passed away three years ago after he refused to have a liver transplant. His family has a genetic propensity for liver disease. But this man explained to us the points system for liver donation/reception. It’s based on your severity level. You can receive points for good behavior and lose points for violating rules. He was very thorough and mentioned that above all his family was right by his side through the entire process supporting him. He said if you don’t have that and you’re all by yourself, he could not have made it this far. This man was awesome. He told us stories about him being a picky eater beginning in childhood and how he wouldn’t eat the chorizo his mother would cook when him and siblings were little tots. Some people like this man were so very thankful for the treatment he was able to receive. He was a true pleasure to be around. He also commented about how he had changed his entire diet to not include salts or other unhealthy food. Others, however, seem to just not “get it”. They don’t follow the rules or listen to what they are told. They expect to get better and live a normal life by continuing to not take care of themselves. The liver transplant is truly a marvel of medicine. Wow, I can’t wait to learn more.
Second Half Week Four (GI/Liver)
Mark Hillstrom Blog

Hello again. The last half of the week was mostly GI and Misia and I had the chance to meet even more friendly/enthusiastic physicians. The empathy aspect really hit home over the last few days. There was one patient who had an average of ten and sometimes forty bowel movements per day. He was rightfully very frustrated. His brother had a history of IBS. I had a feeling of willingness to help this man because his situation was so miserable. I sincerely hope his situation improves. He stopped taking all medications in 2011 after he was laid off from work. The fellow and attending devised a great plan to help push his life in a more bearable direction. During the 9-12am time period Misia and I have noticed an average of 2 patients. Sometimes the business flow is closer to 1 patient/hour. The majority of the time spent on a patient is writing their note. I’d estimate around ¾ of the time. This is a huge inconvenience. It converts the profession of doctor into more of a clerical position. Even time spent in the room with patients is time spent typing and looking at a computer and not patients. There is one physician who never uses the computer in the room and chooses to write all his notes while at home. He cites “it’s embarrassing to have to look into a note if you don’t know some of the patient’s history. I never want to be stumped by the patient.” A much valid point. Even a speech recognition software such as dragon would save tremendous amounts of time. I know exactly how doctor’s notes work because I wrote them for six months in an ER setting. It’s surprising that scribing has not been more widely accepted in clinical settings. Although, if it was, these physicians would not have much to do in terms of note writing. They could instead spend more time caring for and seeing additional patients. I know the scribing movement has caught on in clinical settings such as general family medicine. More about the company I’m familiar with can be seen here: https://www.scribeamerica.com/
Let the colonoscopies begin!! 😀
Mark Hillstrom Blog
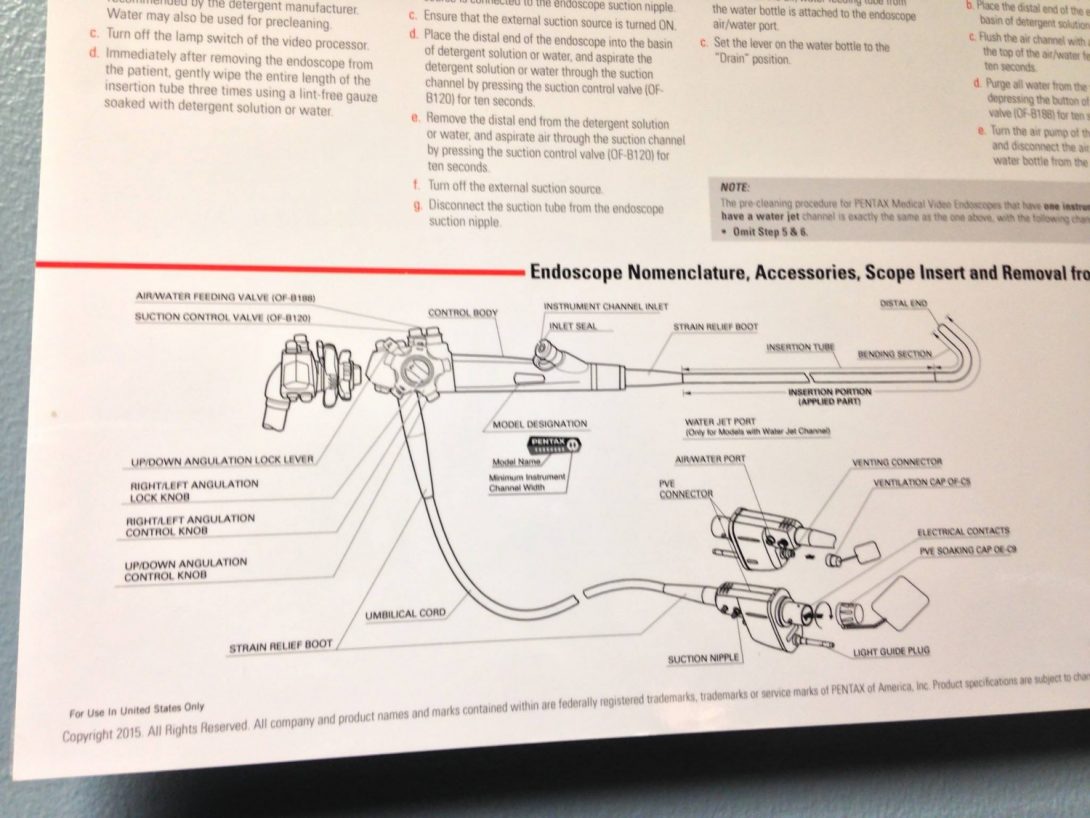
So, Misia and I are currently in the second week of GI/Liver rotation. Last week was entirely patient consults. Pretty much it entailed watching people have their doctor’s appointments. Not to downplay the importance of consults, but this week is more exciting and interesting for us. There are five procedures routinely done throughout GI lab. Being given the opportunity to watch and be exposed to these procedures is just incredible. The five are as follows: EGD which stands for esophagogastroduodenoscopy and visualizes the upper GI tract, colonoscopy which visualizes the lower GI tract, ERCP or endoscopic retrograde cholangiopancreatogram which checks the tubes that drain the liver, gallbladder, and pancreas, EUS or endoscopic ultrasound which aids in visualizing points of interest within the pancreas, gallbladder, liver, and lower lungs through the first section of the small bowel in order to take biopsies and examine potentially suspicious tissue, and double balloon enteroscopy which looks extensively at the small bowel. Capsule endoscopy is not really a procedure but I’ll expand on that later. There has been so much learning and great information accumulated since the beginning of this week that I want to include in this blog but find it difficult because there is just SO MUCH. Ok, well I guess we can start with….Ugh I’m having trouble making this decision. Let’s begin with a typical upper GI scope.
Typically if a patient is experiencing high volume diarrhea the likely source is within the upper GI tract (stomach, small intestine). However, if the diarrhea at patient experiences is low volume the likely culprit resides somewhere in the lower bowels. This helps physicians determine which tests to consider. Sometimes both an EGD and colonoscopy are performed in series. Because patients are injected with benzodiazepine and narcotic medications throughout their stay they are not allowed to drive home. One huge advantage of these procedures that I noticed in urology also is their noninvasive nature. Most patients go directly home later that day and experience little soreness/inflammation if any over the next few days. The two drugs used to sedate the patient and transform them into a “Happy Land” are fentanyl and versed. Both are administered throughout the procedure the make the patient more comfortable. When a procedure ends and the physician goes through assigning the captured pictures to their respective anatomical locations and finishing the procedure note, they always ask nurse “How much did we give?”. This refers to these two aforementioned drugs. Fentanyl is very potent and given in micrograms with versed given in milligrams. Typical number I’ve witness hover around 75 and 4, respectively. Some people require more, some less. After the patient is sedated the physician enters either their lower/upper GI opening. A lot can be determine by simple visual inspection throughout these procedures. Biopsies are taken when suspicious tissue is visualized or as part of routine maintenance for long-term diseased patients. This is done through a “bite”. I’m very surprised not one group reenacted the bite process three Mondays ago when we divided into groups and thought up a skit. The bite reminds me a little PacMan. Except it has teeth, and literally rips tissue from the point of interest. I also related it to the cookie cutter shark: https://www.google.com/search?q=cookie cutter fish&oq=cookie cutter fish&aqs=chrome..69i57.2831j0j7&sourceid=chrome&es_sm=93&ie=UTF-8. Taking a biopsy through a bite is a two person process. The nurse feeds a wire through an inlet in the tubed scope. The wire has the “jaw” at one end and the lock/unlock mechanism at the other. I think the mechanism is spring loaded. When a nurse squeezes the apparatus with two fingers the jaws open and are ready for impact. Then a physician rams the jaw toward the tissue of interest and finely maneuvers it to grip and recover the best sample possible. Then the doctor says “close” and the nurse releases. “Open” and “close” can be said many times before adequate samples are taken. The wire is then pulled from the tube and the jaw opened in a sample jar. Pretty neat. Bites are very small, usually half the size of a sharpened pencil tip. If a patient reacts negatively to the two sedative drugs or if their blood pressure/pulse lowers unreasonably, a pure antagonist GABA blocker called narcan can be administered to reverse the effects. The same drug is used to treat overdosed heroin users. Usually patients do not lie on their back during procedures due to the underlying asphyxiation risk.
The cost of a Pentax GI scope is around $35k and the EUS scope around $85k. The cleaning process is extensive and we were lucky enough to be shown step-by-step how it is done. I’ll include this and other stories in the next post. Stay tuned!
Cleaning Scopes Day
Mark Hillstrom Blog

The day before a colonoscopy patients are supposed to drink 4 liters of a not-so-delicious drink. For EGD patients drink only 2 liters. The purpose of the drink is to clear the GI tract until stool is clear and almost all water. Clearing the system not only make the cleaning job easier for physicians but vastly improves the overall exam accuracy. A colon spotted feces with makes it super difficult to identify potentially suspicious polyps. Overall if patients follow directions they can be certain of the thoroughness of their exam. The scopes are cleaned after each use. The process is extensive. We had the opportunity to watch step-by-step exactly how it’s done. 1. Remove all buttons. It’s important to scrub every single crevice to rid all bacteria. 2. Test for leaks. This is done by placing curling at the bottom of a sink and submerging it in water. Leaks are found when air bubbles rise to the surface. 3. Leaks are examined further by the bubble test. This entails pushing air into the tube and visually inspecting if any bubbles rise. 4. Let the air pumped into the tube disperse. 5. Next, a chemical agent is distributed to the sink at 4-5 ounces per gallon of water. The scope is then scrubbed to give it an initial cleaning. 6. The areas where the buttons were removed need to be brushed thoroughly. It is here that bacteria tends to build up. 7. Then a brush is fed all the way through the biopsy channel until zero debris is seen exiting. 8. The channel is suctioned with water/cleaning agent solution. 9. Now the tube is ready to be prepped for the cleaning machine. All holes in the machine are attached to a suction valve. It is now that the scope goes through a 40 minute deep clean cycle. 10. Before the cycle begins the biopsy channel is flushed one last time. 11. Then flush the scope with clean water (tap water). 12. The scope is encircled at the bottom of the washing machine and wrapped so it is as loose as possible. The chemical agent is Rapicide. Our friend told us it is extremely strong. She has to be careful when replacing the bottles as to not breath/sniff any. 13. All parts of the tube have a bar code which are scanned before the wash begins. This is part of the record keeping process. The employee also scans in when the chemicals are changed or when they begin/end a wash cycle. After the was the end of the scopes are fitted with a green protection sponge and hung in a closet to dry.
GI Last Week :'(
Mark Hillstrom Blog
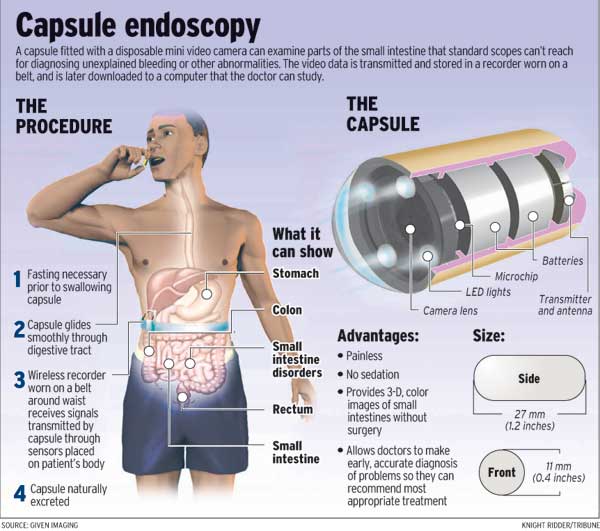
A procedure I failed to mention last entry is the capsule endoscopy. It’s more at test than a procedure actually and is used when physicians need to assess portions of the small bowel between those reachable by either EGD or colonoscopy. It involves the patient swallowing a larger-than-average (30 mm length) pill that contains a battery, camera, and four LEDs. Each manufacturer varies so all pill designs are not created equal. The capsule used at UIC boasts a 2 Hz image capture rate as well as 12 hours of battery life. To clear the digestive tract patients typically drink 2 liters (half what is required for a colonoscopy) of special concoction the night before. If a patient has diverticulitis, complications can arise. Sometimes the pill will remain stuck inside a coil of the small intestine where it stays. If left alone for a long period of time (weeks, months, years) the body will form a protective coating around the pill which fuses it to the intestine wall. Many times, however, pills that do not exit the patient’s system after a few days must be manually retrieved. This requires even more work that carries much higher risks. An attending physician told us that for every 10 colonoscopies/EGDs performed there is one capsule endoscopy. Common reasons for doing Capsule Endoscopy include unexplained bleeding, unexplained iron deficiency, unexplained abdominal pain, search for polyps, ulcers and tumors of small intestine and inflammatory bowel disease such as Crohn’s disease [wiki]. One major downside of this test is that pills are not reusable. Perhaps if the battery could be recharged wirelessly the exterior of the pill could be sterilized and the pill itself could be used more than once.. All images are transmitted to a receiver the patient wears around their waist. This also produces a map of the small intestine from the time the capsule is activated and enters the mouth to the time the battery dies. Very neat stuff.
We were also given the opportunity to witness a liver transplant meeting. This was exciting and we are grateful for being there. It involved about 12 people including four attending physicians, 3-4 residents, and a few administrative people. One-by-one the patients were talked about. The meeting discussed the patient’s current condition, how many “points” they had, and their viability as a potential transplant candidate. The points system, which I believe was talked about in a earlier blog, is extensive and only the most qualified are chosen. Patients with any current substance abuse issues not 100% controlled are dismissed immediately. It’s not worth the hard work necessary by the medical team to deal with noncompliant patients. Sometimes physicians have differing view on the same patient which leads to debate. It was really interesting to see the room dynamic learn about the process. We were lucky to be there.
Mike Oneill Heading link

My first rotation is Hematology Oncology/Radiation Oncology, where I have particular interest in the comfort of patients as well as the acquisition, storage, and treatment associated with stem cells.
My second rotation is Ophthalmology; I’m interested in degenerative diseases of the eye and the methods of operating on such a sensitive organ.
Mike Oneill Blog Heading link
-
Mike Oneill Blog
July 6th to July 8th — Immersed in the Immersion
Mike Oneill Blog

I feel the need to start by saying, wow. What an eye-opening three days it’s been! While the experience is still only beginning, I feel like I’ve learned so much in these three days.
7/6/15
My partner, Misia, and I met up at the Clinical Sciences Building where we were met by Cindy Bernabe. Cindy took us to the Bone Marrow Transplant unit of the Oncology clinic off of Taylor Street. Since our mentor was still finishing up some patient appointments, we were allowed to sit behind the front desk. It’s kind of sad to admit, but this was my first taste of celebrity status in the oncology department. Soon enough, Dr. Patel was ready to show us around the BMT unit. We saw patients sitting in rooms, having chemotherapy inductions done. These patients come routinely for chemotherapy through IV, and don’t need to be admitted for treatment. Most of the induction rooms consist of chairs and TVs, but there are two beds for patients who are unable to sit up comfortably.
We were scheduled to attend a transplant meeting later in the day, and resolved to meet with Dr. Patel closer to the meeting time. With this downtime, we took it upon ourselves to speak to Lupe, one of the induction nurses. Lupe explained some of the standard procedures, what the clinic does well, and what the clinic could improve on. Nutrition is very important for cancer patients, and the clinic is lacking a nutritionist. Lupe told us other hospitals have nutritionists to speak with patients and advise them on how to eat healthy to aid in their treatment. We were well educated on patient reactions to the chemotherapy, and the precautions in place to care for them in the case of such reactions. There are crash carts, oxygen tanks, a pharmacy on-site, and 911 is also an option for severe cases.
We met back up with Dr. Patel and attended the transplant meeting. During this time, physicians and other oncology staff discussed patient conditions, as well as what point in their treatment the patients were in. There is a lot of abbreviation in the department, which was kind of hard to follow, but I feel as if I’m becoming more accustomed to hearing things like “ALL” and “CML” which are types of leukemia. Also, the meeting gave some background information on the patients who I would be visiting the following day. We ended our first day by following Dr. Patel up to 8 West, where the admitted transplant patients are. Dr. Patel advised us to follow Dr. Khan on rounds the following morning, and we departed.
7/7/15
The next morning, Misia and I returned to 8 West and met with Dr. Khan at 9am. Dr. Khan was accompanied by hospital Fellows and Residents; altogether I think there were 6 of us. The patients in this area of the hospital have either completed stem cell/bone marrow transplant, or are awaiting transplant. In either case, their immune systems are compromised, so precaution must always be taken to eliminate contamination risk. The first patient we visited required us to don gowns, gloves and masks. It was pretty emotional for me to see her; she reminded me of a co-worker I lost due to breast cancer. Despite her condition she was seemed to have a lot of energy, and she was very personable toward the doctors, Misia and me. Other patients after her were not in such serious conditions, so masks were usually not necessary. Some required gowns, some simply required hand sanitizer upon entering and leaving the room. One thing I noticed was that the stethoscopes were never in the same place in every room, and sometimes were not in the room at all. It’s my understanding that these particular stethoscopes have to be disposable, so that could explain some of the non-uniformity.
Everything seemed to be going fine until one of the last patients. We walked into the room of a patient much younger than any of the previous ones we visited. Hearing how real her situation was and how matter-of-fact she spoke about her treatment really affected me. Imagining how the cancer is robbing her of her youth, as well as seeing her mom… it was at that moment I realized cancer really sucks. I never took the time to understand how much time is actually required to even treat these diseases. The treatments these patients undergo weaken their immune systems over the course of 10 days, and they don’t recover for another week after that. Everything must be very precise in terms of measuring white blood cells, hemoglobin, and platelet counts. After finishing rounds, we took some time to see the cafeteria and eat lunch.
After lunch, we returned to 8 West and were informed that the girl from earlier was undergoing a lumbar puncture procedure. Thankfully we were allowed to observe. I was surprised to see the numbing agent, Lidocaine was in a glass bottle that had to be broken to access. Sterility reasons seem to be a valid explanation, but perhaps there is another way of guaranteeing a sterile dose. I was able to get a picture of the lumbar puncture kit, which shows the Lidocaine bottles and needles, thermometers and sample containers.
The entire procedure took an hour, which is not that common. There is a very small area in the spine that the needle must find in order to collect CSF, and it is made even more difficult by basically being a “blind” procedure. There are options to use imagining to easily guide the needle in between the vertebrae, but that is expensive and difficult to schedule. After an hour, enough CSF was collected from the patient, and she was given an equal amount of chemo medication. This is important to alleviate headaches due to CSF removal. I feel like I still cannot express my gratitude to the patient for bearing through the procedure and allowing me to be there for all of it.
We were due to meet Youngmin in the stem cell lab on the third floor later in that day, so we took an early trip down to what we expected would be the lab–we were wrong. Youngmin instructed us to go to a particular room number on the third floor, but we didn’t know that there were two completelydifferent rooms with the same number. Misia and I ended up in the OR and were stopped in our tracks when we were the only people not wearing scrubs or hair nets. With a little guidance, we found our way to the stem cell lab. Youngmin explained the processes involved with obtaining stem cells from blood, centrifuging the sample to separate the plasma, white blood cells, and red blood cells. After separating these phases, the goal is to keep the plasma in a separate bag, namely “waste”.
Above is the apparatus used to separate the plasma and the other contents of the bag. The 60ml syringe is used to extract plasma from one bag, and also inject it into the waste bag. The device is quite interesting, but it seems really inefficient. When going from bag to bag, the valve in the middle must be turned to block flow to the bag not receiving or giving fluid. in addition to valve management, there are individual stops on the tubing coming from the bags. Thus, every time someone switches from extracting plasma to adding plasma, they have to undo the stopper on the tubing, turn the valve to block one bag, then operate the syringe. Going back and forth doing this is quite time consuming, and one of the bags’ tubing stopped up completely and inexplicably.
7/8/15
This morning began with a lung tumor board meeting at 7:30 am.Not the ideal start to a day in my opinion, but it was very informative. We were able to observe PET scans of patients, and got a little insight into the cost/benefit balance of patient care. I’m not sure how much I can say, but it’s frustrating that funding can rule out certain services to patients. Prior to the meeting we met Dr. Menchaca, who was interested in having us shadow her in radiology. We took down her information and decided we’d meet up with her later if there wasn’t anything else to do in oncology. As soon as the meeting was over, we shot back up to 8 West for more rounds.
Today was certainly more relaxed for me. We had already seen most of these patients the previous day, and we were more familiar with the protocol in preventing infection. I realized today moreso than yesterday that we have something in common with House, M.D. Doctors in that show gather in a glass room and discuss patient conditions, but during rounds the patients are discussed with mobile computer stations outside of their rooms. I also got to see the hospital’s iPad translator in action toward the end of rounds. It’s very cool to see how far technology has come; you can just Skype someone to translate conversation between doctor and patient. I made more observations about the layout of patient rooms and hallways, and how certain equipment might be cumbersome or annoying to patients and physicians. The medicine pumps beep occasionally (I’m not sure why), but it seemed like it was a nurse’s responsibility to tend to the machines. Because of this, if a pump begins beeping, it will do so until the end of a physician’s evaluation. Rounds finished around noon again, and it was lunch time.
After lunch, we met up with Dr. Menchaca in ultrasound and she showed us some of the imagining machines they use. I’ll try to make another blog post for these pictures; I think this post may be too long to include them. For writing lengthy reports, we saw Dr. Menchaca use a program that converted her spoken words to text on a screen. She spoke very fast, but it was still able to pick everything up accurately. Radiology was very interested and I saw a few scans that would do quite nicely as a computer background. We ended the day meeting with Dr. Patel in his office, eager to hear about our plans for the next day and clear up questions we developed during rounds. All in all, it has been a very tiresome few days for my feet and back, but also very fulfilling in so many ways.
July 9th & 10th – Unfitting Feng Shui
Mike Oneill Blog

July 9th
The rest of our week in heme/onc kicked off with Dr. Patel’s morning clinic. Misia and I met with him in the oncology department and we followed him into the office where the physician and resident computers are. In this area, doctors are able to view and update patient information, compile notes from the appointments, and discuss cases together. There were a few problems with the entire space. For one, it is a very compact area for the amount of people that we have seen in there. Especially when several people are gathered around one station to review patient information, it can be difficult to navigate the area. When nurses or other physicians are looking for someone, the first place to look is in the office area. Usually we have to shuffle behind people throughout the whole area to find the person we’re looking for and it’s disheartening when the person isn’t there. Misia can be seen in the featured photo expressing her delight to be in such a well-engineered area.
Following Dr. Patel to each patient’s room, we were able to experience the difficult task he faces most days: telling someone they have cancer. To be quite honest though, he was very matter-of-fact in telling them their situation. He said what the condition was, what the patient could expect, and possible side-effects from the treatment. The first room we went in was a Polish woman and her husband who didn’t really speak english. Suffice to say I was lost for much of this interaction but hey, there were no tears! Following the first room, I was able to observe a bone marrow biopsy. I would have assumed general anesthetic would be necessary for something as painful as penetrating bone, but a nice slathering of lidocaine on the periosteum seemed to do the trick. I’m willing to admit the biopsy was not for me and I started to feel a bit squeamish when the sample was suckedout of the patient.
The final bit of information I can recall from Thursday is that, in the event of a patient not having a family member able to donate stem cells, there are over 40 million donors worldwide. Unfortunately, due to paperwork and testing, arranging to have these donor samples brought to the hospital can take 6-8 weeks. If I was a patient awaiting transplant those would be a very nervous uncertain 6-8 weeks.
July 10th
Nothing terribly exciting happened Friday. We had rounds in the morning with Dr. Khan. I believe there was a new patient or two. We’d only seen transplant patients who had been there for multiple days or weeks, so we had no idea the amount of time that was needed to really catch everyone up on the condition of the patient. During this time, we actually found out that the packs of gowns outside each patient’s room are charged to the patient in the sum of $5 per pack. I feel like there can’t be more than six in a pack and Misia and I must have used three or four apiece now. With our new-found “financial burden” mindset, we headed down to the clinic to get more exposure to the outpatient procedures. We met a man whose legs and arms were greatly weakened due to a tumor that was compressing his spine for a very long time. In his room I noticed there was an additional door to a bathroom. This bathroom was also open to the hallway so we could hear it being used while speaking to the patient. Weird. Toward the end of the day Dr. Patel was trying to order a prescription for a patient, but there were complications and ultimately the system had to be restarted. Turns out the computers are somewhat dated and freezing problems are not uncommon.
Week 2 Part 1 – 7AM Board Meetings? Really?
Mike Oneill Blog

The beginning of the second week of the internship saw an abrupt shift from learning to collaborating. In the innovation center, Misia and I were able to compare our observations from the previous week and assemble them spatially on a board. We grouped our observations in terms of where we noticed them: Clinic, Rounds, Lab, or Meetings. In retrospect, these groups can and will be changed to better suit our problem statements. Upon the class adjourning, we zipped back to the hospital to try to make the general tumor board meeting (scheduled for noon).
We ended up not knowing where the board meeting was held (and we arrived considerably later than noon), so we agreed to head to the clinic to further process the layout and also interact with patients. Thankfully, Monday was swamped in the clinic. I think having two interns following you around is fine on relaxed days, but Dr. Patel was happy to allow us to interact with a chemotherapy infusion patient for a while. Due to the very busy nature of the clinic on Monday, there were multiple patients put into each room. Bear in mind, these people are expecting to have their own rooms, but when life hands you too many patients… you assign roommates! So we conversed with a man for close to an hour about the trials and tribulations he went through from the beginning of his transplant to the present, where his cancer is in remission. He told us in the hospital he had to take fifteen pills, three times a day. In addition to this, he said he barely got much sleep. Nurses come in every five hours or so to draw blood and change the bedding in the room. He was pleased to say he was never bored because of this, but sleep is definitely something recovering transplant patients need. I really enjoyed interacting with him and hearing his story. I also remembered to get a picture of the odd bathroom setup I detailed in my previous blog post.
As you can see, this door to a bathroom is connected to the clinic room. This is super convenient for patients who use this room, but as I said there is hallway access. You can hear random people come into the bathroom from the hallway, do their business, and then wash their hands. Also, it doesn’t seem like it’s really intended to be used by the patient (note the large scale seeming to block the door).
The next day is very cloudy to me. As someone who has been conditioned to wake up at 11:00AM all summer, getting to work at 9AM is a struggle, let alone 7AM for board meetings! Disclaimer: if anyone from another rotation (anesthesiology) is reading this, please forgive me. I know you have to be at the hospital earlier, but I am weak, and I must complain about this. So the first board meeting was at 7AM for gynecological oncology. There was a 12 person microscope that everyone was sitting around, and the presenter would put a slide under his lens, allowing everyone to observe. I thought this was a very novel way to review patient cases and discuss the courses of action. What I felt was not novel was that in one location of the microscope, two of the viewing stations were uncomfortably close together. If two people were to sit next to each other and use those stations, the proximity would lead to cheek touching (which is more than I could handle, especially at 7AM). This meeting was followed shortly after by a urologolical oncology board meeting. The microscopes were not used, but rather a computer display showed scans of the patients. Nothing too remarkable was gathered from this meeting. The rest of our day was spent with Dr. Oh in the clinic. Dr. Oh gave us a more engineering-centric (as engineering-centric as you can get with blood cancer) view on oncology. We talked about how certain cancer cells have markers to distinguish them from other cells. Using antigens, these markers can be honed in on to deliver targetted drug therapy to eliminate the cancer.
Wednesday was the day I learned that attending physicians rotate on rounds every two weeks. Gone were the days of Dr. Khan; this was the beginning of the Quigley Era. Immediately we could see a difference in the personality of the doctors and the way they preferred to conduct rounds. This difference seemed to throw some of the team off, especially when he insisted the patient information be described just-so. Each category had to be presented in a specific order; he would stop the resident if this rule was not followed. One more thing of note on this rounding day was that I officially located the gauze patch-up on one of the doors. I’m not sure what purpose it served, but I know gauze is definitely not designed for that.
Week 2 Part 2- Stem Cell Transplant!
Mike Oneill Blog

7/16
Thursday morning, we were scheduled to return to the stem cell lab prior to a transfusion. We met with Youngmin and waited in the office while students from Dr. Mahmud’s lab were shown around the facility. We had the pleasure of trying out the back-support attachment on Najma’s chair in the meantime. Eventually the tour came to a close and the transplant was ready to begin. Maintaining a temperature of -150 C is important until the samples are ready to be thawed. The lab uses a cryoshipper to keep the cassettes of blood frozen during transport to the eighth floor.
Once the team arrived outside the patient’s room, we could begin thawing the stem cells in preparation for the transplant. In our case, the patient received eight bags of 50ml each of stem cells. After thawing each bag, a sample must be analyzed for viability or contamination. If a bag has bacteria or some other contamination, the team will usually treat the patient rather than the sample being transplanted. The transfusion is done intravenously with the patient somewhat sedated. The sedation is to prevent an anxiety response; being pumped with someone else’s blood can be kind of weird.
7/17
Most of Friday was spent wrapping up the rotation and preparing to transition to Radiation Oncology. We sat in with Dr. Quigley for a decent portion of the morning. After that, we got to revisit the man we spoke to in the oncology clinic; this time he was staying in the inpatient unit and had to have a bone marrow biopsy. His great personality still shone through even though he was kind of being a baby about the whole process. It’s understandable if the patient groans or winces when being stuck with a needle, but he was yelling “OW!” when the doctor was locating his bone with her fingers. He turned to Misia when she walked in the room and said “Look away, Marianne. You’re too young to see this!” Turns out I was too young to see it because I started feeling faint again and had to leave the room.
After a presentation by Dr. Gonzalez, we were scheduled to meet Dr. Mahmud in his office at COMRB. The insight we received from him kind of shattered my world for the rest of that day. We were supposed to discuss the department and field of bone marrow transplants, but we ended up having a much more philosophical discussion than I expected. He kept stressing the importance of working for a goal and loving what you do. I told him I was planning to enter industry with a focus on medical device design, which he challenged. He asked me why I wanted to do device design and I didn’t have a very strong reason. I like the field and I don’t think I would mind developing devices. However, he made me remember why I switched to Bioengineering: my grandmother needed a lung transplant which caused me to look into synthesizing organs. Dr. Mahmud concluded that I had a reason to work in regenerative medicine thanks to my grandmother.
Week 3, Part 1 – It’s (Joe) Miller Time!
Mike Oneill Blog

This is the week we transitioned into radiation oncology! Upon descending to the concourse of the oncology clinic, we were immediately met by friendly receptionists at the front desk. They directed Misia and me to Dr. Kauffman, who we bumped into in the hallway. Dr. Kauffman is a radation oncology resident from University of Chicago. In fact, most of the doctors in radiation oncology are on rotation from UofC; because of this, they don’t have pagers but rather a floor-wide intercom system. I think the pager system works well for this area. It’s a relatively small floor with fewer physicians, and I’ll admit I enjoyed trying to identify the voices of the people behind the intercom.
There weren’t many patient consultations, so we were able to shadow the radiation therapists, mainly the man pictured above: Joe Miller. Joe did an awesome job of giving us a step-by-step explanation of how the Linear Accelerator works to administer radiation treatment to patients. He showed us the interface on the computer as well as the monitors that show different angles of the treatment room.
[INSERT MONITORS]
[INSERT CONTROL PANEL]
There were fish on the ceiling and Pandora radio playing softly in the treatment room.
We saw the linear accelerator up close! All it took was a journey down a hallway consisting of six-inch thick walls and doors, with two turns and a very foreboding warning sign.
Eventually we saw patients with Dr. Kauffman; these were very similar to the patient consults in HemOnc, just with different details. I couldn’t get a picture, but one of the examination rooms had a curtain that would catch in the door every time I tried to shut it. Not only did that make me feel like I looked super new, but I feel like it impeded the door’s closing ability. After a few more bright-and-early board meetings, it was more of the same in the RadOnc clinic: patient consults, radiation therapy, discussions with Dr. Kauffman and Dr. Bhave. One of the most unfortunate patterns I noticed throughout the week was that most patients were coming in for palliative treatment, with no cure in sight. There was a case of someone who had anaplastic thyroid cancer, which progresses very quickly. With treatment, these patients are expected to live half a year; without treatment–maybe a week. Eventually though, the tumor will grow to be so large that it constricts the airway completely, making breathing impossible. I’m beginning to wonder if all this exposure is numbing me emotionally..
Week 3, Part 2 – Intermission
Mike Oneill Blog
The final two days in Oncology! This week ended in a bittersweet way. With one final 8:00 am board meeting, the early mornings were behind me. In said meeting, the radiation team reviewed patient cases. Dr. Howard from UofC was unavailable to be on-site, so he was added to the conference via Skype. I didn’t think this would be as fruitful as it was; he could speak freely without the rest of us drowning him out. Misia and I saw volume maps for radiation treatment of these patients. After the meeting, we were able to walk around the floor more. Misia and I discovered the CT simulator, where patients are fitted for their immobilization devices and CT scanned for future treatment plans. We watched as Bill used fiberglass casting material (think broken arm) to mold the patients face. Using the mold, Bill was able to create a mask that would prevent the patient from moving his head during radiation treatment.
I was able to catch a glimpse (and a picture) of an MRI scan involving a bullet in a patient’s lung. Please keep in mind this bullet has been in the lung for several months. Also please keep in mind the bullet has nothing to do with cancer. It is the sparkly object on the left side of the scan; the cancer is on the right side, just as bright but less sparkly.
The last memory I will have of this rotation lies in the hands of Dr. Mahmud. We saw him on the previous Friday; our conversation was so meaningful to all of us that it seemed only natural to revisit him. He educated Misia and I on the concept of stem cells–what is stem-ness, and how does a bone marrow transplant intend to fight cancer? Overall I am very thankful for the time I was able to spend in hematology/oncology and radiation oncology. So much thinking goes in to the treatment of cancer and it really is a team-oriented science. It has been a truly unique experience that I would love to revisit, given the chance.
Week 4, Part 1 – SCRUBS!!!!
Mike Oneill Blog

Has it really been three weeks already? I feel like a parent whose children are growing up a bit too fast. Either way, ophthalmology is already a night and day transition from oncology! My new partner, Julie (Dr. Wagner), and I arrived at the eye and ear infirmary Monday afternoon quite unsure of what to expect. Nothing could have prepared us for the man we would soon face: Dr. Sugar. He has an interesting way of teaching in that he will give us mini-quizzes to make sure we’re paying attention and learning. I’m quite sad to say I don’t think my quiz average is very high. One thing that can be observed about the technology used in ophthalmology involves the most common tool for observing the cornea, the slit scope.
Mike Oneill Blog

You can see the patient rests their chin on part of the device, with their forehead pressed flush against a bar. A lot of times, the patient’s head does not stay completely flush with the bar and Dr. Sugar had to readjust them before continuing the examination. A head-strap sounds like an easy fix, but I don’t think the solution can be that simple. We sat in on a few outpatient visits in the cornea department before Dr. Sugar toured us around the ophthalmology department. There are 9 divisions in the ophthalmology department. I’m only going to list the divisions I’ve seen so far this week.
1. Cornea – involves the surface of the eye as well as cataracts and all things cornea.
2. Glaucoma – involves high eye pressure (note: marijuana is a very poor method of treating glaucoma. It only lowers intraocular pressure for 3-4 hours. This means patients would have to be under the influence pretty much all day every day).
3. Plastics – involves the eyelids, eye socket, and bones around the area.
4. Retina – involves, you guessed it, the retina.
I haven’t had much exposure to the retina department, so I’m not exactly well versed on what they cover. The technology seems fairly consistent throughout: the aforementioned slit scope, an indirect scope for viewing a bigger portion of the retina using lenses, and fluorescein dye, which is used to stain the surface of the eye. The staining of the eye allows physicians to asses any surface abnormalities that could indicate dryness or damage to the cornea.
Wednesday is a very important day because Julie and I were able to go to the OR! “Finally,” I thought, walking through the doors with Julie to get the scrub card “I get to see some action!” I didn’t know how to get scrubs, I didn’t know how to get changed, and I definitely didn’t know where to find the booties for my shoes. But it was incredible. With the help of Sam, Wali, Julie and Dr. Sugar, I was able to figure things out and get suited up for some carnage. We primarily hung around with Dr. Sugar; he doesn’t do surgeries anymore, but he oversees them closely. In the case of the cataract surgeries we watched, Dr. Sugar sat right next to the operating doctor and irrigated the eye. Dr. Sugar reassured the patient while also calling us in during important moments. The surgery uses two incisions on the surface of the eye to access the cataract inside. The physicians uses several intermediate methods before employing an ultrasonic hose device to break up and extract the cataract. After it is removed, an artificial lens is loaded into a syringe which is placed in the incisions and deployed into the eye. The lens unfolds and after a little positioning, the surgery is pretty much complete. It’s miraculous how quickly these procedures were: 17-30 minutes only. We became somewhat versed in the overhead microscope used during the procedure. By this I mean Julie was able to focus on her watch and I was incredibly clumsy while trying to find my arm in the microscope.
We heard of another surgery happening nearby: an enucleation. This patient had trauma to his eye which caused pain and blindness in the eye. The solution? Cut it out. This procedure is much longer than cataract surgery, so Julie and I bounced back and forth between the two rooms. In order to extract the eye, the doctors had to sever the four muscles that move the eye. These must be preserved to give a natural appearance to a prosthetic eye later.
There are many tools used throughout the procedure, I can detail the specific function of only a few of them. There are scissors for cutting sutures and different scissors for cutting flesh. They use packing with epinephrine to absorb blood and hinder bleeding. The most interesting devices to me are the ball-on-the-rod devices in the previous pictures.
While I do not know the exact name of these devices, I know they are used to measure the size of the orbit in the skull. After enucleation, the patient will have a gaping chasm that needs to be filled for several reasons. The physicians measures the orbit with these devices and chooses the appropriate size when he or she can observe only a small amount of space with the device in. A corresponding orbital implant is chosen and placed in the orbit. After the implant is in, the doctors begin sewing the muscles together to seal with cavity. A patient’s options after this surgery usually include eye prosthesis which can sometimes be fixed to the muscles to simulate natural movement.
Week 4, Part 2 — Shrek is Love, Shrek is Life
Mike Oneill Blog
Julie and I have not quite had the chance to be partners so far in this rotation. In lieu of Dr. Sugar’s orders, we split our day Thursday between contacts and pediatrics. We would split up and switch departments after lunch. My vicious paternal instinct lunged me down to the second floor for pediatrics, where I met Dr. Abbasian. She is so incredibly personable and knowledgeable! I felt completely comfortable asking her questions I had (which were numerous). For starters, I couldn’t understand why pediatric ophthalmology used the same chairs as all the adult departments. Many of the younger patients I saw had to sit on their knees to match their faces up with the slit scope. Additionally, children are very squirmy! Adults are usually more resilient when having lights shined in their eyes, but some of the kids I ran into were not having it. In some situations, Dr. Abbasian had to call in help to hold the children still. Things have to get done; it’s not like the patients can be sedated for vision exams either. It was tough to be around, but the talent in pediatrics is inspiring; and I had a blast seeing the different children’s movies in the rooms. I don’t think I was in the department for more than 5 minutes before I heard Frozen playing in the background.
Due to the previously discussed squirminess, it can be difficult to obtain eye pressure measurements too. To solve this, I saw a newer tool used, called the iCare tonometer.
Supposedly, this device is able to measure intraocular pressure without the patient feeling anything. This is a great concept for sensitive patients such as children, but if IOP is above normal (~20), it gives very unrealistic readings so the doctor has to measure manually anyway.
My time in contacts was somewhat reminiscent of oncology. Dr. Joslin was personable with patients and myself. She was always able to recall facts about patients’ lives, which I think is important especially in gaining patients’ trust. She explained to me that many of the patients she sees need hard contacts due to eye surface irregularities. Hard contacts create an artificial, uniform surface on the eye. If the eye has ridges on its surface, light can split off of them causing impaired vision; soft lenses would simply fall into the grooves and just create a raised, still irregular surface. I’ve yet to investigate deep into big technologies that the contacts specialization uses, however I’ve identified plungers that are used for inserting and removing tough-to-manage lenses. In some cases, patients need scleral lenses which cover much of the front of your eye. These lenses are usually filled with a solution prior to being placed in the eye, so the patient will have to face straight down and put the lens in vertically. I can see how it’d be uncomfortable and difficult, so the plunger below is designed to help with that.
Week 5, Part 1 – Souvenirs
Mike Oneill Blog

The second week of our rotation in ophthalmology resumed in much the same way the first week ended. Due to space restrictions, and the fact that we’d seen different departments individually, this was the time to “fill in the blanks” in our exposure, so to say. Julie needed to see what plastics was all about, and I had still barely scratched the surface in the retina building. However, I was offered several choices, one of which was to observe retina surgery! A pleasant chill went down my spine and I trotted off to the secret corridor that connects the eye and ear infirmary to the hospital.
I had a much easier experience with changing into scrubs and applying the mask and booties. As I entered OR room 18, the team was in the middle of a cataract/vitrectomy surgery. I should first begin by explaining why a vitrectomy is needed and why it is accompanied with cataract surgery. Firstly, the vitreous (humor) is a clear gel that fills the space in the eye between the lens and retina, giving the eye its spherical shape. A very high majority (98-99%) of this vitreous is water, and it can become detached from the optic nerve disc. In cases like this, the patient will see constant floaters which represent the vitreous shifting within the eye during movement. Surgery on this part of the eye cannot be done under the surface of the cornea, as there is no access. Therefore, the surgeon must establish access to the inner part of the eye, both physically and visually. The least invasive way to see inside the eye is to look through the cornea and the lens toward the back of the eye. Because of this, it becomes apparent why cataracts must be removed prior to the vitrectomy (otherwise there would be a cloudy wall for the surgeon to look through). I will be describing a more strenuous case of vitrectomy, PVR, which follows mostly the same methodology. PVR stands for Proliferative Vitrioretinopathy, where a previously reattached retina becomes re-detached and folded due to contraction of the vitreous shown below.
Mike Oneill Blog
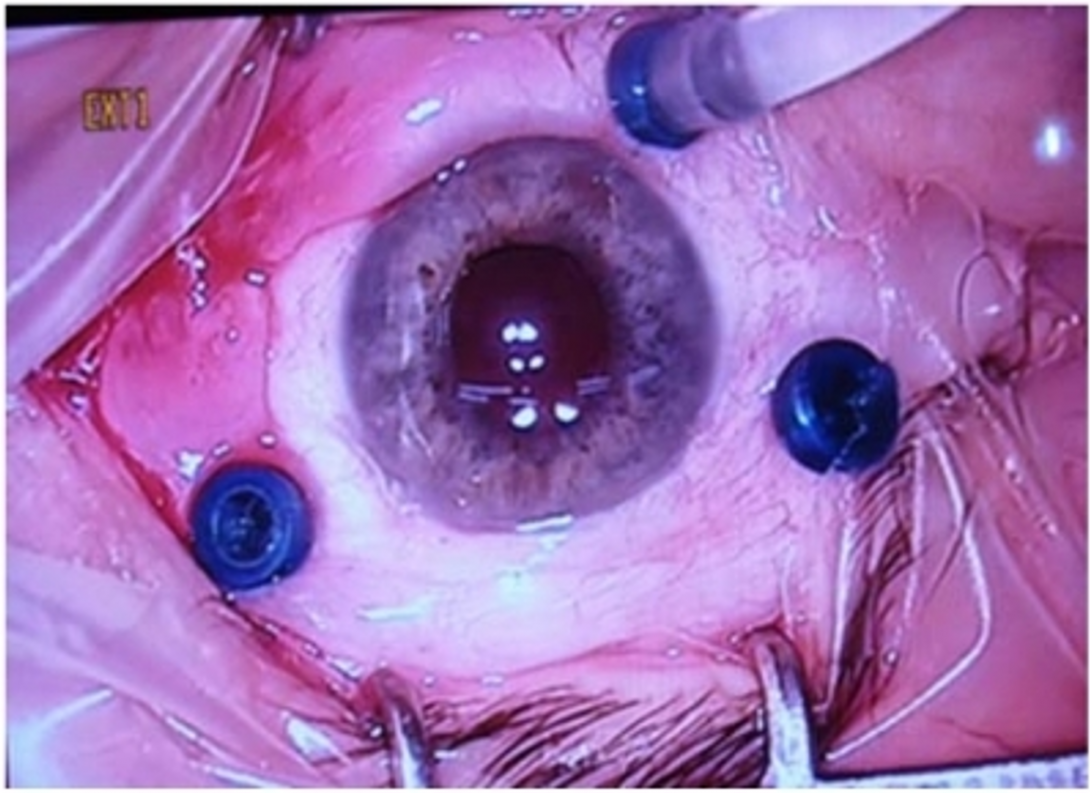
In order for the surgeon to access the back of the eye, three trocars are plunged through the sclera. One trocar is for irrigation, to maintain desired pressure in the eye, while the other two are for tools: a light, a snare, a blade, or forceps. These tools are usually less than a millimeter in diameter and can fit easily through the trocars. For much of the procedure, the surgeon will chip away vitreous, which is quite difficult due to the poor illumination within the eye. Dr. Lim suggested forceps with a light attached to better allow the surgeon to see exactly what he or she is gripping. We saw that the blade had a light on it, but obviously the forceps did not. Comparing the PVR vitrectomy to its more “standard” counterpart, I noticed a much longer operational period. The combination of cataract and vitrectomy for non PVR lasted 30-40 minutes, maximum. However, the painstaking chipping away of the vitreous lasted close to 3.5 hours. Bear in mind the patient is awake and expected to look up at a light during this entire process. Eventually, to re-affix the retina to the back of the eye, the surgeon fills the eye with air and lasers the retina to reattach it. After this, a long-lasting gas (C3F8) is recruited to replace the air. The C3F8 will last a few weeks and its purpose is to keep the retina pressed up against the back of the eye long enough for it to heal. The patient will experience blurred vision during this recovery time, but once the gas dissipates things should improve.
After the surgery, we asked one of the fellows if we could take pictures of the tools and he told us we could keep them! Sanitizing was imperative first because of the dangers of Hepatitis C, but after that was handled, we were free to take our trophies for future research and bragging.
Week 5, Part 2 – Controlled Strabismus
Mike Oneill Blog
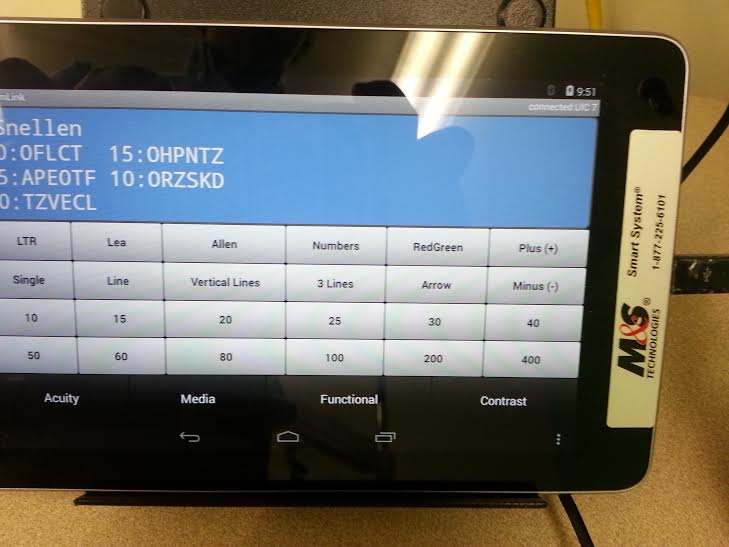
In order to further my expertise in the pediatrics/adult strabismus department, I decided to devote an entire day to shadowing an orthoptist. An orthoptist can be thought of as a “technician” of sorts: he or she sees the patients before the attending physician. In my case, the orthoptist tested patients for double vision, amblyopia (when the brain ignores the signal one particular eye receives), color blindness, and general vision. She also applied dilating drops, or in one unfortunate case, the dilation spray. On one hand, the dilation spray (which is an all-in-one for the various drops needed for pediatric patients) is efficient. You don’t have to constantly switch back and forth between three bottles. On the other hand, a brave high school boy looked very very affected by the sheer blasting power that little spray bottle held. An alternative to the inevitable resistance posed by children having liquid dropped into their eye is the papoose. For the past week and a half, I’d heard “I’m gonna papoose ya!” and I didn’t know it was a serious offer. Turns out wrapping children like burritos is pretty effective at immobilizing them from the neck down, leaving just a pair of resistant eyelids to overcome. Plus, just look how relaxed and comfortable this little boy looks.
In all seriousness, I didn’t have to see the papoose employed, but I was able to take the same vision-related tests as the patients. There is a book with 3D glasses included. The back cover has a giant fly on it whose wings jump out of the page in people with binocular vision. Inside, there are diamonds where one of four circles is supposed to become 3D. These increase in difficulty and I’m not ashamed to admit I failed 2 of 9. Another technique for measuring communication between the eyes is the Worth 4-dot test.
Mike Oneill Blog
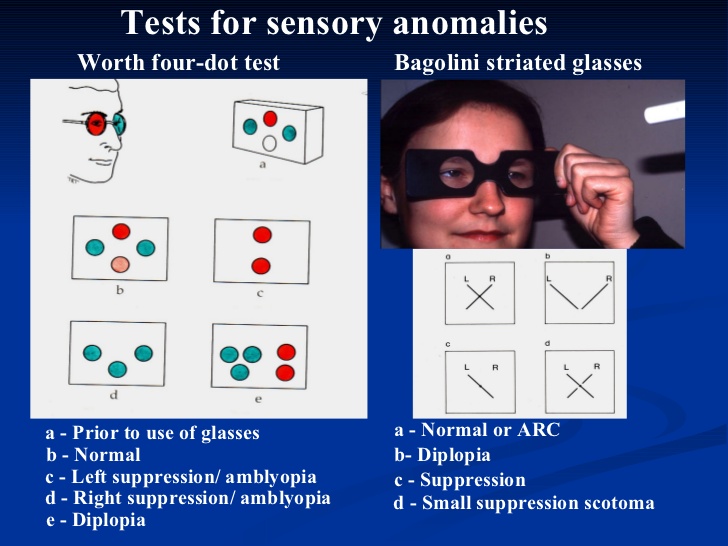
I put on the John Lennon glasses and was able to see the two green dots with a red dot on top and on the bottom. I didn’t realize until this moment that I’ve had controlled strabismus since middle school. My eyes naturally separate when I’m not focusing them, so I took this opportunity to see if I could manipulate my results. I didn’t see the diplopic results, but more of a vertical summation of the red lights and the green lights.
Mike Oneill Blog

In retina clinic, I followed Dr. Ulamski who was very efficient at seeing patients. We saw a woman who was seeing clouds. After inspecting her cornea, Dr. Ulamski realized she had some scratches on the surface of her eye. He needed to test her vision, but there wasn’t enough distance between the chair and the wall for the patient to read letters from the wall. To solve this, Dr. Ulamski ran across to another building to get the PAM visual acuity tester. It is added on to the slit lamp and the patient reads through the lines as they normally would with letters on the wall. I felt like it was a pretty dated piece of technology and the fact that he had to leave the building to get it was something that stood out to me.
Namrata Saha Heading link

Hi! Welcome to my blog about my experiences this year in the Bioengineering Clinical Immersion Program!
Namrata Saha Blog Heading link
-
Namrata Saha Blog
GI/Liver Outpatient Clinic WEEK 1 Entry 1
Namrata Saha Blog
I began my first day, not quite knowing exactly what to expect although I did expect a somewhat calm day since I knew I was in the outpatient clinic of the GI/Liver specialty. Our first attending physician was not scheduled till 4 so in the meantime, my partner and I observed the waiting room as well as the attending conference room which is where all the medical practitioners congregate to debrief themselves on their patients, fill out necessary paperwork, and discuss different treatment plans with fellows that are working with them.
Once Dr. Carroll arrived we were taken on his first consult which included the use of a portable ultrasound to check the gallbladder of a patient which was exciting because we were able to see a device used as necessary. He demonstrated some of the features to us such as a the sonar capability of the instrument which shows the heartbeat. I was able to take the pulse of the patient to match it to the sonar displayed by the ultrasound machine!
The procedure for seeing patients seemed routine to him as he asked a wide array of questions then determined a course of action, most of which included getting different tests. Over the last three days, it has become apparent that most outpatient consults result in the patient explaining their symptoms and the doctor recommending different tests to be ordered such as colonoscopies and full ultrasounds. There seem to be no actual procedures carried out other than a physical exam on the exam bed present in all exam rooms and the ultrasound.
I also noticed that a patient that had their own chart on which they recorded their medicines as well as key information about them such as side affects and approximate times to take the medicine. This seemed to really benefit them and they said they had received a similar chart from the office. Here is the comparison of the two charts with the homemade one on the left.
I had the opportunity to follow a single patient through their entire process of when they walked in the door to when they left and was able to create a timeline as follows
2:00 PM– Patient Appointment Time
2:10 PM– Patient Arrives
2:50 PM– Patient taken to back room for vitals check
2:55 PM– Patient returned to waiting room to wait till doctor is ready since there aren’t enough exam rooms
3:05 PM– Patient called back to room and the Fellow is with patient till… (at this time the patient askes how much longer the appointment will take since her 2 month old is at home with the nanny, patient is given an estimation of 30-45 minutes)
3:18 PM– Fellow leaves room
3:25 PM– Fellow returns with attending physician and is with the patient till…
3:37 PM– The attending physician leaves while the fellow finishes with online orders until…
3:42 PM– The fellow leaves and the patient is told to wait for a Hep A/B injection
3:45 PM– Patient is sent back to waiting room while the insurance is being consulted to determine whether it is covered.
3:55 PM– Patient leaves reason unknown
Total Time Patient Spent: 1 hour 45 minutes
Thinking back to this experiment, I am able to see that from a patients perspective thatsome of the processes may take a long time of waiting. But also viewing it from behind the scenes in on the doctors side, there are a variety of factors that cause the longer wait time.
Some doctors take time in the room to personally get to know the patient while others ask patients questions and immediately enter the information into the system. There are different pros and cons to each strategy that I observed. One of the benefits of solely speaking to the patient and jotting down a few notes allows for the doctor to judge from the behavior of the patient the accuracy of the information being told. For example, there are certain questions that patients are reluctant to divulge information usually regarding drug use and alcohol. However though, they seem more compliant when pressed by the doctor. A con to this method is that it may take much longer to get through patients since the doctor then needs to go back to the conference room and enter in notes as well as orders.
Another method I observed was that the doctor seeing the patient, took their notes directly while talking to the patient. All the questions that were asked were recorded immediately which may allow for a higher level of detail. This process allowed for a larger quantity of patients to be seen by one doctor which in turn made the wait times shorter.
Overall the first few days were very instructive and by today, I think I gained a good understanding of how the outpatient clinic works on a day- to -day basis. When asked if they could change one thing, the most common response was asking for more exam rooms. Everyone was very welcoming and by the third day I was seeing familiar faces around who asked how my partner and I were doing. I am excited to continue my journey for the rest of this rotation which so far has been very instructive!
GI/Liver Clinic Outpatient WEEK 1 Entry 2
Namrata Saha Blog
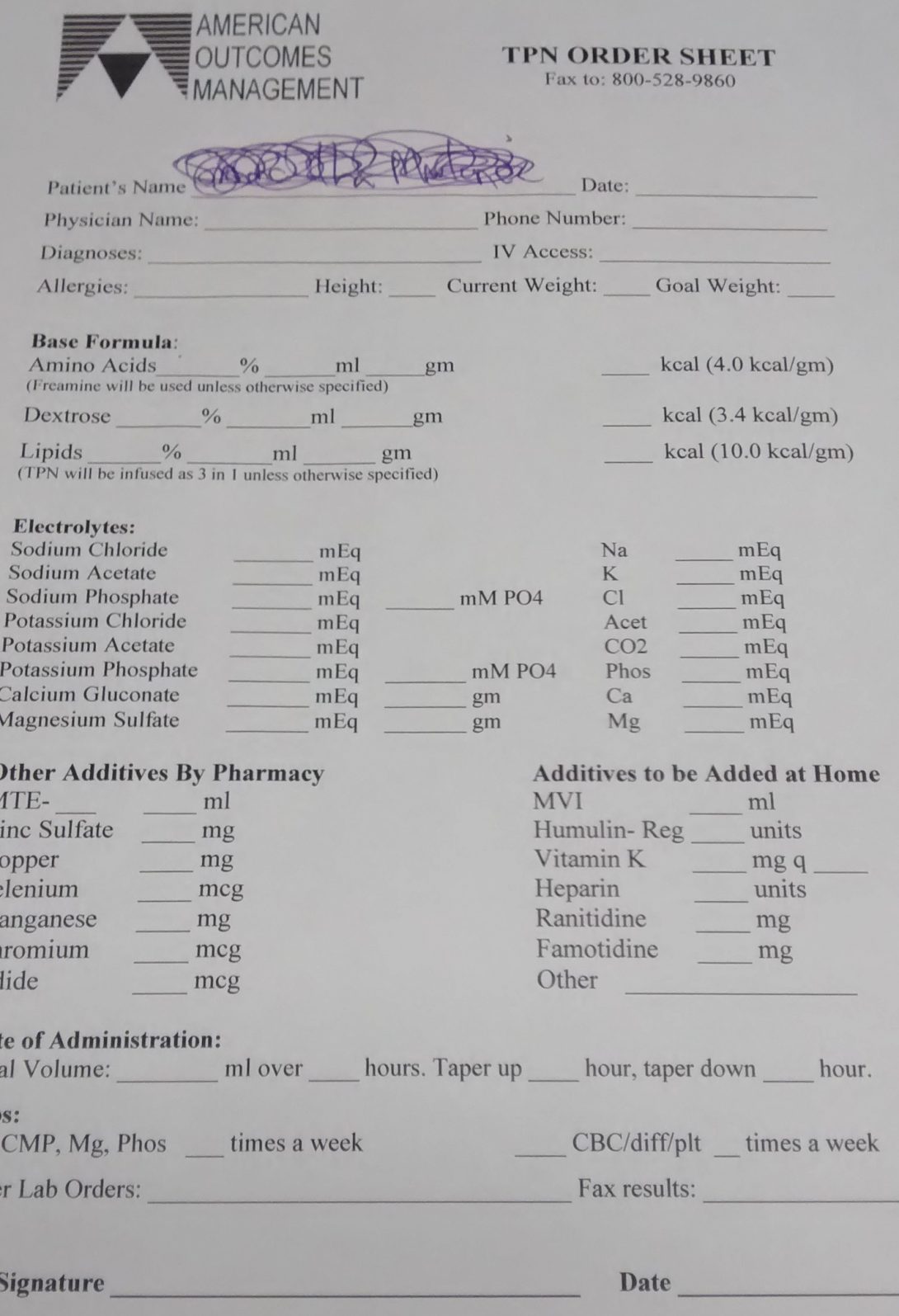
Just when I thought my week couldn’t get any more exciting… it did. After getting into the general flow of things I was expecting another day of consults with more patients but Dr. Carroll had a surprise for us. He explained the basics of Total Parenteral Nutrition calculation, printed us a power point, pulled up a patients chart, and told us to figure out what the patient should be receiving in the IV. Christine and I were surprised at this unexpected turn of events and the fact that we were actually able to do math! Diving headfirst in, I pulled up one of the sources cited in the vague powerpoint Dr. Carroll printed for us while Christine pulled the information on which calculations needed to be used from the powerpoint. After looking up the patient’s diagnosis and height and weight using the Cerner powerchart, we were able to use the online instructions to complete the calculations. I was also able to pull up an online TPN calculation in order for us to check our numbers which did match up! After we finished we went of our work with Dr. Carroll who seemed pleased with our progress!
Dr. Carroll also told us that the price for the TPN for a year averages around a hundred thousand dollars. Christine and I were both taken aback by the cost of the healthcare and we inquired as to why it was so expensive. It turns out that the ingredients are not all that expensive but the process of making the TPN is since it needs to be done in a sterile environment. Also since there is only a select demand for patients that need TPN i.e. patients that are not able to feed themselves, corporations that make it such as Walgreens and CVS are able to control the price.
After an exciting Thursday morning, we observed some more G.I consults. We observed a few appointments with patients that were Spanish speaking. It seemed most if not all of the attending physicians were not Spanish speaking and thus the use of Ian was needed. Ian is an Ipad mounted on a potable stand that connects to an outside service over the phone which translates for both the doctor and the patient. I noticed that each appointment that Ian was used at required about double the time of a regular English speaking patient, yet on the doctors schedule there was no extra time scheduled. My mind immediately jumped to the conclusion that if a patient is Spanish speaking, they should be scheduled for extra time so that the physician is not running behind, increasing the wait time. The one thing I noticed all throughout the week was that the doctors were always running late resulting in waits upwards of two hours. It seemed that this was caused by the combination of schedules being overbooked with the notion that 30% on the patients would be no-shows and the fact that there weren’t enough rooms to put all the patients in at a given time.
My first week seemed to be a little different than everyone else’s but I feel I got to observe a lot of interaction with patients and medical personal! I can’t wait for next week in the Endoscopy Lab where we will have the opportunity to observe some procedures!
Scoping out the GI Lab WEEK 2 Entry 1
Namrata Saha Blog

After a week in the outpatient clinic, we ventured to the GI Lab in order to scope out some of the procedures that had been recommended to patients. The lab, located on the second floor was and easy to navigate rectangular shape which allowed for two different paths which helped with traffic in the lab. Just as in the previous week, I kept track of a timeline of events for a patient receiving a colonoscopy which can show the general schematic for procedures.
10:45 AM– Patient Appointment Time
10:15 AM– Patient Arrives
10:15 AM– Patient taken to lab, changes into hospital gown and has an IV inserted
10:45 AM– Patient is wheeled into procedure room and identity of patient is verified.
10:53 AM– Patient is given anaesthetic medication.
10:57 AM– Scope is inserted
11:34 AM– Scope is removed
11:40 AM– Patient is wheeled into holding area for recovery/rest for 30 minutes after last anaesthetic medication is administered which is about 10 minutes after the patient is wheeled into the holding area.
11:50– Patient is allowed to leave with family member/driver
Total Time Patient Spent: 1 hour 35 minutes
Total Time Attending Physician spends: 55 minutes
After the procedure, I was curious about the processes used to sterilize and clean the scopes. Once the scope is done being used the scope is placed into a drawstring bag and transported into the scope room which has an attached cleaning room. The scope is placed in a rack that has labels dirty and pre-cleaned.
The scope is then tested with air for any damage from the procedure such as needle punctures since submerging it in water will ruin the device if there is any damage.
Once the scope is deemed in good condition, it is submerged in hot water and a brush is used to clean out the different pathways that include a biopsy channel, a power flush, and suction. Larger scopes include a power flush since they are large enough to accommodate it.
Once the scope is pre cleaned, it is moved to the “BMW of washing machines,” which are very high-tech washing machines. Each machine uses a block that attaches to all the different channels of a scope. Different blocks are present for different sizes of scope as well as different brands of scopes such as Pentax and Olympus.
In order to be used, the technician must scan, his ID, then the blocks id, then the patient’s bar-code, then the bar code of the scope in order to begin the washing process.
Once all the correct bar codes scan, then the machine turns on and begins the process of washing which takes about 36 minutes.
The machine is made by Medivators and utilizes peraceitic acid to disinfect the scope.
The machine also performs the air pressure test that was performed manually and will automatically stop if there is any damage detected. If the scope fails the air pressure test, it is placed in a suitcase and sent to the company for repair.
The scope cleaning process seems very efficient although one small problem that occurred was that the scopes were not bar-coded properly. To remedy the problem, a scope of the same size was scanned instead of the one being washed to start the process. An easy solution to the problem would be to make sure each scope is bar-coded correctly.
This week opened my eyes to the large disparities within the hospital system. When asked what the biggest problem he faced, a physician replied with an ominous “its a systems problem.” My time here has led me to believe that many of the problems in the system come down to money. Just as the world revolves around money, healthcare revolves around money. The cost of healthcare is large on all ends of the spectrum from insurance, to patients, to doctors, to hospitals. Many of the problems I’m seeing already have solutions, yet the reason they are not implemented lies in the cost. There is a delicate balance of machinery vs. human capital, and any changes to the system could upset that. We must remember to look at problems holistically, and I have realized that even if there is a simple fix to a problem, the effects must also be taken into consideration. For example, if a device or process is made to be more efficient, it may decrease the amount of time a patient needs to spend in the hospital. However, this may decrease the profit the hospital makes, and thus the hospital administration might not encourage the change since they will loose money. Unfortunately money seems to take precedence in the grand scheme of things.
This doesn’t affect the beginning process of thinking of problem statements, but thinking about costs and the business will be important when designing and implementing solutions.
**Photos to come once the internet gremlins decide they will let me connect for more than 5 minutes!
Foreign Objects and Tangled Cords WEEK 2 Entry 2
Namrata Saha Blog

Finishing up the week in the lab, I came away with a better understanding of the processes in the hospital. Many of the doctors had their own insights on how their processes could be made easier and more efficient. One doctor told us that it would be beneficial to have a signal sent to indicate that the end of the colon had been reached during a colonoscopy. Another asked if it would be possible to create a scope that would be able to enter the bile duct in an endoscopy.
One of the most interesting parts of the week was that there were two patients that had swallowed objects, one a pencil, and one a metal cable tie. The process for removing them required an endoscopy which then used forceps to remove the objects. The metal cable tie procedure took about 15 minutes total. These patients who had swallowed the objects were incarcerated. I was told that these patients usually swallow objects to be allowed a trip to the hospital for a day out of prison. This seems like a vast waste of resources that could be otherwise prevented. If the prisoners were discouraged from engaging in such behaviour, they may be fewer cases that could have been completely prevented.
Something I noticed about colonoscopies is the fact that they are not always 100% accurate in detecting cancer for a variety of reasons. A major part in the colonoscopy is how well the patient takes the prep which encompasses drinking a large volume of liquid and laxatives. Many patients are not able to tolerate such a rigorous prep, and thus their colon may not be completely flushed out for the colonoscopy. Without a proper prep, the accuracy of polyp detection decreases. It may be beneficial to look for a way to make the prep for colonoscopies easier for patients.
Speaking of performing colonoscopies, there were cords all over the room that all medical personal had to be careful to step over which made their overall jobs harder.
Next week we will be doing inpatient rounds with the GI department!
Inpatient Rounds around the Hospital WEEK 3 Entry 1
Namrata Saha Blog
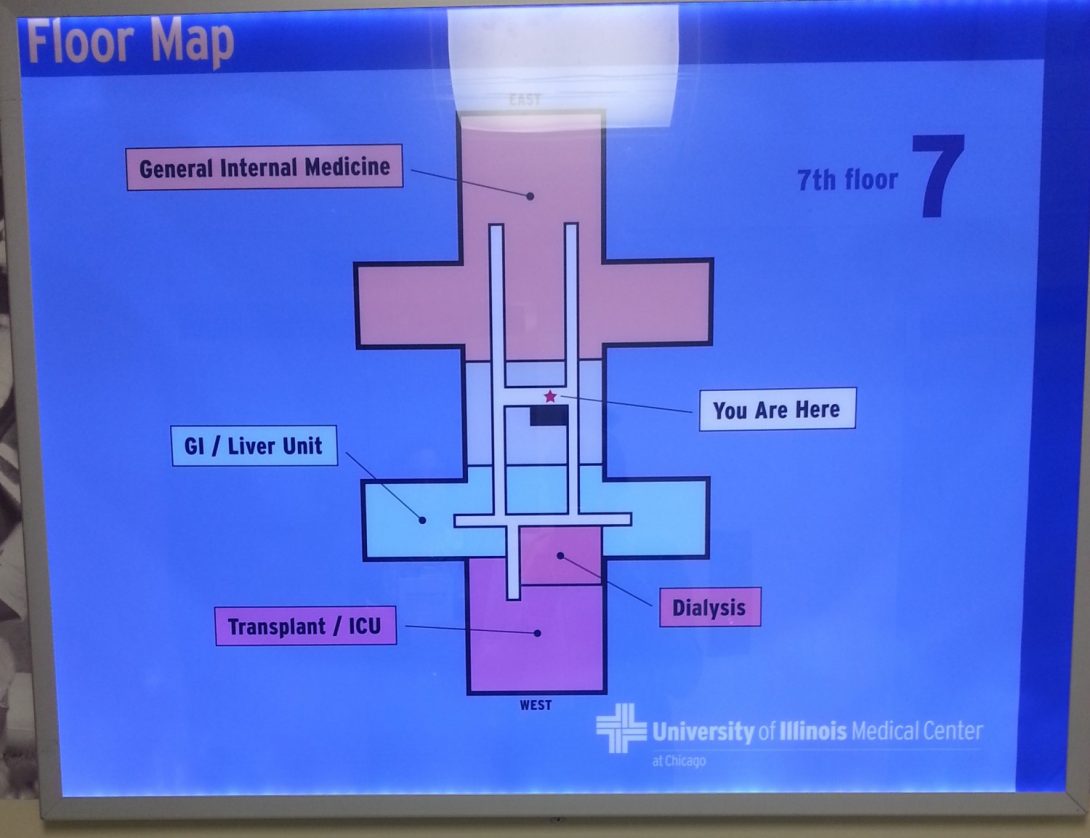
Beginning week 3 we moved to inpatient rounds guided by the wonderful Dr. Sleesman.
Most inpatients come to be admitted into the GI inpatient ward through the ER. They generally report to the ER and are assessed by the ER doctors, then transferred to the GI inpatient if their symptoms require treatment in the main hospital. Once admitted, they are assessed by GI residents. If immediate attention is required, the fellows and attending are contacted and the patient is examined by them and further action is taken if deemed necessary. If the resident does not see need for immediate attention, the GI fellow and attending physician examine the patient the following morning during their rounds.
Rounds take place at 7 am by the resident, fellow, and attending physician, some with a cup of coffee in their hand. Most inpatients are in on the 6thand 7thfloor of the hospital which includes the Medical Intensive Care Unit as well as the GI Ward although we did observe a patient with a GI problem in the maternity ward.
As with the previous weeks I documented the general schedule of rounds. The general schematic for rounds includes a discussion outside the patient’s room where the resident debriefs the attending and fellow. The attending and fellow ask any questions they have to the resident and then discuss a plan of actions which encompasses ordering different tests, medications, and treatment plans. Then, all three enter the patient’s room and the attending speaks with the patient, asks any additional questions, and gives the recommendation and plan of action. If the patient has already been in the hospital for more than one day, the attending is essentially following up on the symptoms and test results. They then determine whether the patient is able to be discharged or kept for further observation or treatment.
7 AM- Rounds Start
7:13 AM- 7:17 AM- 1stpatient – 5 Minutes
7:25 AM- 7:30 AM- 2ndpatient- 5 Minutes
7:40 AM-7:47 AM- 3rdpatient – 7 Minutes
7:55 AM- 4thpatient not present in room- receiving ultra sound – 0 Minutes
7:58 AM- 8 AM- 5thpatient- 2 minutes
8:14 AM- 8:21 AM- 6thpatient – 7 minutes
Total time for Rounds: 1 hour 21 minutes
Average time with patient: 4.3 minutes
Some of the devices I noticed in the ward was a monitor that displayed the vitals of all the patients in the hallway. The monitor had a spot for 12 patients and at the time I viewed it, 5 were being used corresponding to the 5 inpatients in the hallway.
There were also portable computers in the hallway available for use if a physician, fellow, or resident needed to look up any information on the Cerner or Provation systems.
Although the time with each patient may seem low, the resident does spend more time with the patient getting the essential information. It is also important to note that some cases include multiple specialty doctors and thus they are examined by each specialty doctor team separately.
hello world
Namrata Saha Blog
hello world
End of the GI Scope WEEK 3 Entry 2
Namrata Saha Blog

We had the opportunity to attend a lecture given by Dr. Brian Boulay, an attending physician in the GI department. The topic covered was cholangitis and was attended by most of the fellows. This way the doctors are able to stay up to date on medical information which may better their scope of treatment. The lecture took place in a conference room around a table which encouraged the asking of questions while maintaining a casual air. We also learned about a choledochoduodenostomy, or rather attempted to say it!
Unfortunately our trust Dr. Sleesman had clinic duty but he sent us on an exciting field trip with Dr. Kankanala and his infectious laughter. Dr. Kankanala was off for morning duty at the Jesse Brown VA Hospital which takes care of all the medical needs of the veterans. It was a quick 7 minute walk after the lecture and we arrived to find that the computer systems were down. The VA uses a different EMR system called CPRS rather than Cerner which the UIC hospital uses. It is currently in a transition to new technology which didn’t seem to be going too smoothly.
The VA is a collaboration with physicians from UIC as well as Northwestern. Since the VA pays for half of the fellows’ salaries, the fellows split their time equally with UIC and the VA even though the demand is much more in the UIC Hospital.
After speaking to Dr. Stacy Prenner, an attending physician from Northwestern, my eyes were opened to many of the day to day problems she faced. Some of the inconveniences include patients that don’t show up on time, cancelations, prep orders that not completed when they should, and room turnover time. The accumulation of all these problems leads to an inefficient clinic which can waste valuable time of medical personal.
Once we returned to the general hospital, we were just in time to watch a capsule endoscopy. Dr. Sugir Velpari showed us the video feed from a previous capsule endoscopy. We then had the opportunity to view the process of a patient swallowing the capsule. A capsule endoscopy involves a camera contained within a pill that records pictures every 3 seconds and sends it to a monitor worn around the waist of the patient. Once the procedure is finished, the monitor is then plugged into the computer and the pictures are viewed at leisure. The battery life of the capsule ranges from 8 to 12 hours.
The patient is prepared for the procedure by a nurse explaining the whole process as well as how the device works which takes about 10 minutes. Dr. Boulay also uses a lead system to help track the capsule within the patient. There are 8 leads attached to the patient. Once that is completed, the capsule is swallowed and the amber light turns to a blinking blue. The patient will know once the battery stops working and when the test is over when the light turns back to amber in about 8 hours. The patient is instructed not to eat anything for 4 hours and not to drink anything for 2. The capsule seemed pretty easy to swallow and the whole procedure went pretty smoothly.
Something I also felt that was effective was mail tube system in place that allowed messages and samples such as blood and urine vials to different parts of the hospital! This saves manpower when samples need to be sent but, now messages may just be sent through emails.
We’d like to give a special shout-out to the entire GI Team! Thank you for being so welcoming, patient and answering all our questions! We gained a lot of valuable experience and knowledge from our time with you.
Take deep breaths, its a new week
Namrata Saha Blog

Allergy Clinic
Our day in the allergy clinic started with the nurse administering an allergy test where the patient is tested with different pollens. The patient is given positive and negative controls as well as all the possible substances that they have suspicions that they are allergic to. A device which has eight pointers is used and it penetrates the skin a small amount as to not raise blood but to allow the substance to cause a reaction if the patient is allergic to it. This patient seemed to have very sensitive skin as there was very little difference between the positive and negative control.
Then we were able to observe the nurse administer a spirometry test to another patient which measures lunch function. The test measures the volume you are able to inhale and exhale and how quickly you are able to do that. This test may give light to different lung ailments such as asthma.
MICU
We saw how rounds were carried out in the medical intensive care unit. The team of physicians assembles at 8 am in order to relay information about the previous night to the attending physician of the day. The resident that was present overnight relays the information to the attending, fellows, as well the other residents that will be taken over for the day. The general process is seeing the sickest patients first, then moving on to the newer ones, and finally finishing with the patients that have been established for a few days. The resident relays the information as well as a plan for the day and the attending reviews and approves the plan. Then the attending goes in the room and checks on the patient and relays any new information to the patient or family. A total of eleven patients were seen and the rounds took about 2 hours and 25 minutes. We also saw a patient that required a code one. When a patient codes they have no heartbeat and need to be resuscitated. There are about 15 part of the code team. The MICU is the department that announces all the codes. When a code one is announces, it is announced with the room number and wing of the hospital. The code team drops whatever they are doing and rushes to the room to take care of the patient. There were 15 people in the room along with one family member. The patient survived but yet the experience was still jarring.
Fellow Clinic
We viewed the Fellows clinic where outpatients came in for consults. I was shown different CAT scans of patients torso’s and was told how radiologists and pulmonologists collaborate to identify different health risks. Speaking to one of the physicians, she informed me about the trouble patients have accessing medications. This happens because insurance companies frequently change the medications that they cover. When these changes are made, neither the physican’s office or patient is notified and when the patient goes to fill their prescription, they are charged the full amount, usually which medicare/medcaid patients aren’t able to afford. The pharmacist is very good about viewing the insurance company websites and keeping updated lists of medications, but sometime even the website aren’t updated.
I saw how compassionate Dr. Jacobson was in offering information to a patient with a possible patient diagnosis ensuring her, “We’re your team. We’re here to help you.” He made sure to tell her he would do whatever possible to help her gain information about her prognosis as well as understand and make informed decisions about her health care.
Pulmonary Function Testing Lab
I spent a morning in the testing lab, where the tech showed me the experience from the patient’s side. I was given the standard PTFs (pulmonary function tests) and was able to view my results. The equipment used was all very up to date and worked smoothly. The tech told me he had no complaints except for more space to move around in. The testing required a lot of cooperation from the patient which I was able to experience first-hand. The tests require a lot of voluntary breathing patterns that are different from normal breathing such as deep inhalation as well as exhalation. The tech was very good about urging me along throughout all the tests which I think was key to a good reading. I saw him use the same technique on a patient who was very compliant. I can foresee that if a patient is not very compliant these tests will be very hard to complete. I also was wondering what would happen if a patient spoke a different language since in a spirometry chamber, the patient hears the tech through a microphone and the translator service would not be able to translate quickly enough for the type of tests being done. The tech explained to me that he would resort to sign language and learn the words for inhale and exhale since there are not many words that need to be used. Next week I will talk more about the different quantities measured by these experiments as well as how they work as I am better acquainted with them.
Bronchoscopy Lab
THEY LET ME USE THE SCOPE!
I took a trip down memory lane back to the endoscopy suite where I had been the previous weeks for GI. The bronchoscopy procedures are done here as well although they use a smaller scope which passes through the nasal cavity to the trachea. This scope is different from the endoscopy and colonoscopy scopes as it is smaller and only includes a biopsy channel. The fellow and the pulmonary tech allowed me to practice using the scope on a rubber lung model which was absolutely exhilarating. I got the hang of it pretty soon and I was able to use the brush tool through the biopsy channel to brush out some material to study (it was just some rubber from the model).
This hand on experience allowed me to gain some real understanding about the mechanics scopes. Since this is a smaller scope the tip is only able to move up and down, in order to maneuver it left or right, one must twist the scope as well as their hand supporting the end of the scope in the direction they want to go. This wasn’t too much of a hindrance as I was able to get the hang of it in about 5 minutes and little instruction which led to the question whether or not I play too many video games. The one thing that was slightly hard about holding the scope was that it had to be elevated which can cause fatigue in the arm of the user during long procedures.
I was also shown along with a few other residents how to put in a central line for a dialysis catheter. The process was very methodical and I was able to show the fellow the process after one full run through. Although I was able to get the steps down, I know it would be very different when there is an actual patient and all the motions are going to involving real tissue and not just theory.
These first few days allowed me to gain an basic understanding of the workings of the pulmonary world and I am excited to delve deeper into the processes and devices used in the next few weeks!
The Politics of the MICU WEEK 4 Entry 2
Namrata Saha Blog

MICU
I had the opportunity to take a closer look at the respirators in the intensive care unit. There is a fulltime technician that works with all the patients that need respirators. He is generally present every time there a patient needs to be intubated or extubated. The respirators are complex machines that need to work 100% of the time since any flaws could be fatal. I learned about the different modes the respirator has. On manual which delivers a breath to the patient at the given interval, and one spontaneous which allows the patient to breathe on their own, but delivers extra oxygen when a breath is taken and/or if the patient fails to breathe on their own. The respirator has a double filter system that essentially removes all pollution and bacteria from the air being delivered since some patients may have greatly suppressed immune systems.
If a patient has been intubated for more than 2 weeks, the chance of infection increases exponentially. The long term solution is to insert a tube into the trachea in which the air may be delivered instead of a tube in the mouth. This procedure is called a tracheostomy or simply trach. I had the experience of seeing this procedure done which utilizes a bronch scope. Generally bronch scopes go through the nasal cavity, but since the patient already was intubated, the scope was passed through the same tube. The rest of the procedure consists of making an incision, dilating to the proper size of the final airway tube, and suturing it into place. The procedure that I saw was performed in the Neuro MICU using the mobile bronch station. This mobile station consisted of the monitor and all the equipment to project the scope to the monitor which was brought to the patient’s room. This procedure also consisted of a PEG, or insertion of a feeding tube in the stomach. I had seen this before in my previous GI rotation and it is performed with an endoscopy scope. The difference between the endoscopy scope and a bronch scope is that the bronch scope is much smaller and has only a biopsy channel. Because of this, the mobile bronch cart has no need for a water holder since there is no flush being used. I saw that the tech had added a water bottle onto the cart so the endoscopy PEG procedure could still be carried out using the bronch cart.
I also saw some of the different politics of the MICU involving a procedure. A patient was slotted to receive a central line which was going to be carried out by the residents on the MICU rotation. A nurse however stopped by, said she really liked the patient, and said she had called the PICK team (a team that inserts a catheter through the arm instead of the neck) since it would cause the patient less pain. After she left I was informed that there really is no difference and the only reason she had asked for the PICK team is because if a central line was put in, she would have to stand and take vitals every five minutes which would be more work for her. It seems like the personal preferences of personal come into play in a patient’s medical care as well as the general workflow.
This week gave me a great introduction to all the different aspects of pulmonary critical care. Stay tuned for next week as I delve deeper into the inner workings of everything I’ve seen thus far!
Tense Procedure WEEK 5 Entry 1
Namrata Saha Blog

Just as I’ve been doing for the last few weeks, I took the total amount of time required for bronchoscopy procedure. This case was an in-patient case so the first step was to obtain a signed consent form from the patient. The fellow that was going to be performing the procedure when up to the inpatient room about 30 minutes before the procedure was scheduled to start (10:30). He had already discussed the risks with the patient previously when he was consulting with her, so the signing only took a couple minutes, on a single sheet of paper. Then, things started going downhill. Everyone was ready yet the patient hadn’t been brought in yet. Finally the patient arrives and the procedure goes as follows.
11:15 –Nebulizer started with a 1% lidocaine solution. The lidocaine solution has been made from 1 part water and 1 part 2% lidocaine since the 1% was not available in the room.
11:26- Lidocaine gel is snorted by the patient to further numb her airway
11:33- Patient gets up to go to the bathroom (patient did go to the bathroom beforehand)
11:44- Q-tips with lidocaine jelly are inserted into the nostril to numb the area as well as to check whether the scope will fit. The nasal cavity is deemed in good condition for the scope. At this point the fellows realize that the scope plugged in, is a pediatric scope and it is switched out for a regular one. I am also told that all the steps thus far are completed by the pulmonary tech who is on vacation.
11:51- Sedation is begun to put the patient into a moderate sedation which is the general protocol.
11:55- The scope is inserted into the nasal cavity. After about 10 minutes of trying, which includes attempting to switch to a pediatric scope, the nasal cavity is deemed too small and thus the scope will have to be used orally. This process is extremely tense as the attending is raising his voice as he guides the fellow. At one point he seems so frustrated that he grabs the scope (without putting any gloves on) and attempts to put the scope in.
12:05- The scope is inserted orally, and finally the process of screening all lobes of the lungs is begun. First the left lobe is inspected which goes pretty smoothly. Each of the two lobes is examined quickly, efficiently, and to the satisfaction of the attending. He is very adamant about injecting a lidocaine flush through the biopsy channel at the entrance site of each lobe. The attending raises voice to emphasize the lidocaine but he has to do it about 4 times before the fellow injecting the flush does it without any prompting. Then the right lobes are viewed and many nodules are visible. It seems that the scope is irritating the area since as time goes on viewing anything becomes very difficult.
12:22- A biopsy is taken so the cause of the inflammation and nodules may be determined.
12:28- Another biopsy is taken from the surround regions in the right lobe. At this point visibility is becoming lower and lower which makes it harder to take the biopsy. Meanwhile, the attending is becoming more and more agitated, even yelling at the fellows multiple times. The overall environment in the procedure room is very tense. The attending even exclaims that the nurse is not watching the vitals monitor while she is grabbing a tool for the fellow. The fellow quickly jumps in and says he has been watching the vitals screen for the 20 seconds she has been away from the screen.
12:40- Another biopsy is taken and this one is done completely blind since there is so much blood and liquid that it is impossible to see anything.
12:45- Scope is removed.
Total time: 1 hour 15 minutes
The description for the procedure speaks for itself. As far as device design goes. The bronch scopes are designed very similarly to the endoscopy and colonoscopy scopes. The visibility issue here doesn’t seem to be a general problem during bronchoscopies, but the nature of this case caused for a lot of trouble. It seemed almost as if the scope was causing much of the problem. This was probably because the lung was irritated with this particular infection already which made it susceptible to damage from the scope easier.
Patient Compliance WEEK 5 Entry 2
Namrata Saha Blog

Sleep Clinic
This week we observed the Sleep Clinic. Naz and I were not prepared for such a large change of scenery. Arriving at the clinic which is tucked away about a mile west of the hospital, we met the attending who explained the process of seeing patients to us. Expecting the regular routine of clinic visits, we were surprised to see how different the consult rooms looked like! They all had full beds all made up with pillows and their own bathroom. They pretty much looked like bedrooms with the exception of the chairs and desk that looked like ones in general consult rooms. Most of the patients we saw were coming in for problems with sleep apnea. Many sleep tests occur overnight at this clinic where patients are hooked up to electrodes.
We learned a little about the CPAP machines which help with sleep apnea. They all require some sort of face mask, and there are many available. Even though there are many different designs, in the end, there is still something on the face and it’s a human’s natural instinct to try and brush it away which in turn may make the machine less effective. The machines are able to monitor patient compliance on how much of the time they are being used. There are some insurance companies that require the machine to be used more than a certain percent of the time for insurance to cover the cost of the treatment. The attending mention a big problem of the machines and stated that it would be a lot easier if the machines were able to automatically upload the data to the system to view and analyze it instead of the patient bringing in the machine and physically downloading the data.
Overall sleep clinic was an interesting change and it would be nice if we are able to go back at around 8 pm to see how all the electrodes are attached to the overnight patients to see how the general process works.
MICU
While in the Intensive care unit, I noticed that many patients were hooked up to antibiotics on their IV’s. Recently, I had listened to a TED talk regarding antibiotics and some of the negative effects they may have. The gist of the talk is that as antibiotics are used more widespread, there are bacteria that are constantly evolving in order to stay alive, and thus antibiotic-resistant bacteria are born. As time goes on, the antibiotics need to be constantly evolving in order to keep up with the bacteria that are evolving on their own. For many drug companies, it is not lucrative to keep making new antibiotics and this humanity may be falling behind in treating bacterial infections. I brought this topic up with the pharmacist that was currently on rounds and he gave me an overview of how the hospital deals with antibiotics. There is a full time pharmacist whose sole job is to ensure that the correct antibiotics are used. The hospital generally tries to use narrow range antibiotics to solve specific problems. I deduced that patients can be treated with narrow range antibiotics only if their specific problem is known. This would have to be identified by tests or by a doctor’s discretion as they are admitted into the hospital. It seems that the faster the hospital is able to admit and perform the correct tests and diagnosis on the patient, the faster narrow-range antibiotics may be given instead of wide-range antibiotics that are given as precautionary measures. Patients are also instructed to finish their entire course of antibiotics in order for the infection to be wiped out completely even though they may feel better a few days after starting them. Here patient compliance plays a large role since patients may choose just to stop taking their pills just because they are feeling better.
While we were rounding, the rounds were interrupted by a doctor who informed us about the increase in cases of c.diff in the hospital which is an infection very easily transmitted through spores and causes bad diarrhea. She emphasized the importance of washing hands with antibacterial soap and warm water which is more effective than sanitizing hands. I noticed that in some of the older rooms (about half the ward has been renovated) that the sinks are in the back of the room. This is a problem since once the health practitioner has seen the patient, they must take off their gown and gloves at the door, but must venture all the way back into the room to wash their hands only to walk through the contaminated room to get outside.
I also asked the pharmacist about drug shortage since I noticed a sign on the drug dispenser that stated a shortage. He said that usually shortages occur when a certain manufacturing plant is either contaminated or short in supply. The manufacturing plant then sells the drug to a wholesaler which acts as the middleman to supply the UIC hospital. I was told that if there was a shortage, the drug wouldn’t be able to be bought from another wholesaler since UIC has a contract with its current wholesaler. In case of a shortage, usually the pharmacy has a stockpile of the drug so treatment will still be able to be delivered. If there is a dire shortage of a drug, all the pharmacists are notified to use certain drug in cases where the certain drug is the only option or in a life-saving situation. I think each shortage depends on what drug there is a shortage of, the number of patients in the hospital that may require it, and how much the shortage is. The pharmacists take all those factors, as well as probably a few more into consideration when dealing with drug shortages. This made me think about the overuse of drugs since the pharmacist implied that patients would get certain drugs only if they were absolutely necessary, but how would their care be negatively affected if they didn’t get a certain drug since it was in shortage?
It seems that patient compliance is a big theme in all aspects of pulmonary critical care whether it be in the pulmonary function testing, taking antibiotics, or taking different types of treatment such as asthma medication or using the CPAP machine.
Sleepers and Wires WEEK 6 Entry 1
Namrata Saha Blog
Sleep Clinic
This week we visited the sleep clinic as they prepared for their nighttime sleep studies on patients. These clinics usually occur from 8pm to around 6pm. There were two techs working that night for a total of four patients. I was told that the volume of patients was more during the weekends. Patients check in and are given a parking sticker for the lot outside. Once they are settled, they are taken to the consult room that has a bed. They finish some paperwork for a few minutes while the technician gets ready. Once the technicians are ready. They prepare the body of the patient by cleaning the areas the leads will be attached with a gel. The leads that are used are gold plated although in other institutions, there are regular plastic leads that are used. The reason gold leads are used are because they have the best level of transmission which is needed since the facility is located right next to a MRI facility. The MRI machines have high levels of signal interference.
It takes about 30-40 minutes to hook the patient up to about 20 leads which are all plugged into a box that the patient may sling on their shoulder if they need to go to the bathroom in the middle of the night. This is the part that is the most complained about since many patients ask weather they can just wear a helmet and body suit. This is currently not possible since the leads need to have good contact with the skin in order to transmit signals well. Also, there are wireless leads that have been invented but this facility doesn’t use them.
One the patient is all hooked up, they are instructed to lay in the bed. The tech then goes into the holding room and performs some tests to make sure the equipment is working properly. There is an intercom system set up in the room where the patient can just speak if they need any assistance and the tech will hear them. The tech may also speak to the patient by pushing a button on the intercom. The preliminary tests provide a baseline for the rest of the night. There is a breathing monitor that senses when a patient is breathing and depending on if a patients breathing, they are put on a CPAP machine in order to see if it helps with their breathing. The prelim tests also monitor what a REM sleep cycle may look like by mimicking rapid eye movement done voluntarily by the patient (here also patient compliance is a key factor in providing an accurate test). Once these tests are completed the patient is told to sleep as they would normally.
Each of the rooms is equipped with a private bathroom as well as a television. There is also a camera that monitors the patient for the whole night for security as well as monitoring purposes.
I think these sleep test would be better utilized if they were performed in the patients natural sleeping environment such as the bed they sleep in every night. Some people may have different patterns when they are somewhere other than their own bed. Another factor that should be taken into consideration is if the patient sleeps with a partner in their bed or not because that may affect results.
Normal
0false
false
falseEN-US
JA
X-NONE/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-parent:””;
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin:0in;
mso-para-margin-bottom:.0001pt;
mso-pagination:widow-orphan;
font-size:12.0pt;
font-family:Cambria;
mso-ascii-font-family:Cambria;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Cambria;
mso-hansi-theme-font:minor-latin;}I also received an update from the procedure mentioned last week. Unfortunately the patient the bronchoscopy was performed on has small cell lung cancer. This was determined from the biopsies taken during the procedure and stained for cancer agents. I could see that the cells had little cytoplasm, enlarged nucleuses, and chromatin that wasn’t as condensed as it usually should be.
One last blog… WEEK 6 Entry 2
Namrata Saha Blog

Wow, I can’t believe it’s my last blog post, it seems like just yesterday I was writing my first. The immense amount of knowledge and skills I have gained from this program has been incredible. I have really learned to look at processes and systems around me with a critical eye. I think what benefited me most from this program is the ability to think critically about all the problems around me, while empathizing with all parties involved while solving the problems that exist.
I realized that many problems I encountered were large scale problems with fixes that are not just as simple as designing a device to be more efficient or remodelling a hospital room. There are so many other factors that go into determining what improvements will be carried out such as funding, budgets, ethical barriers, politics. I have realized it is not possible to please everyone, but rather to acknowledge the different viewpoints of people and work towards solutions that are not so drastic. Humans are incredibly well adapted to adaptation even though they may not like it. I believe it is possible to change many problems for the better, not at a drastic rate, but step- by step.
Changes can be small. But 100 small changes can make a big change. I am very optimistic for the good changes that are coming to overall healthcare and I could not be more excited to partake in this revolution in my career. This Immersion program has felt like a giant leap into the ocean even though I now realize I have barely jumped into a pond. I hope to take everything I learned and work on making the ocean, and world a better place!
Special Thanks to my two partners, Rachel Joseph and Naz Hussain who were always there to help develop my ideas!
Nazir Hussain Blog Heading link
-
Nazir Hussain Blog
//one //blue //the other m(ixup)
//one
Nazir Hussain Blog

Post 1. Week 1. Day 1. Today was exactly what I expected out of a first day, until the last 2 hours. I expected this internship to leave me feeling like the residents following House, wide eyed and enamored following a doctor around halls and corners. The day started simply, an orientation with bagels and cream cheese. The room was quiet, whether it was shyness or sleepiness causing it depends on the intern. We talked about the purpose of the program, read the syllabus, and outlined our hopes and fears for the next 6 weeks. To be completely honest, my partner and I didn’t really have any fears. There wasn’t anything to fear, we were meeting new people and learning from them; essentially it was school. Side note, my partner’s name is Sam and we are in the Orthopedics rotation We met Susan King after the meeting. She showed us around the areas we would be working in for most of this 3-week rotation, the OR and the clinic. We then waited to meet with Dr. Mejia. A few hours pass and we get news that Dr. Mejia is still in the OR operating on a patient. Arrangements were made quickly and we were taken to the clinic We were then left in the hands of Dr. Chmell, who carries a very happy air about him. He was older but very upbeat and energetic, often asking residents, “Do you got anybody? Do you got anybody?” If a resident had a patient he would immediately introduce us and have us follow them into a procedure. Within 30 minutes I watched a patient have fluid removed from their knee, and another have collagen* added to their knees. For the next hour and a half we followed Dr. Chmell and the residents around the clinic, into, and out of office spaces.
//blue
Day 1 was basically the kiddie pool compared to the deep end that was Day 2. Waking up at 4:30 am to arrive at the hospital by 5:45 am to observe a 6:30 am total knee replacement surgery. Completely worth it. The day started quickly and moved quickly. With two total knee replacements completed before noon, the synergy and capabilities of the teams we were assigned to was more than present. I was introduced to some of the doctors who would be working with us during the procedure. Everyone was warm and friendly, especially for it being 6:30. I was shown equipment used in the OR, including an electric suture.
Prior to the patient arriving I was told the one thing I needed to remember: stay away from the blue. The “blue” referred to the blue cloths wrapped around sterile tools. Actually, everything that was to be treated as sterile was blue, from the surgeons gowns to the draping. Touch the blue and it’s over. The surgery has to be aborted,
The first patient presented with rheumatoid arthritis in the left knee, with the femur and tibia eroding and causing pain. After sedating and sterilizing the patient, the procedure began. Lasting about 2 hours from prepping to suturing, the procedure itself seemed both advanced and archaic using both crude tools such as mallets and saws to cutting edge technology including a flexible drill bit.
The third and final procedure lasted the longest. The patient was shot in the leg during the 4th of July weekend, with a bullet lodged well into the right femur. A steel plate was inserted tangent to the femur and drilled in using screws of various size. I don’t know if it was the fact that this surgery was muchlonger than the others or if it was the fact that it was the last surgery today, but my feet were killing me by the time I left. But, like I said it was completely worth it. There were some interesting circumstances about the last patient that make it stand out. The one thing I will not forger is when I heard one of the surgeons say “I can’t find the hole” while placing a catheter. Full team of doctors, not a single scrubbed doctor could figure this out. Some time later a urologist scrubbed in, I had to see what we was going to do. Big mistake of the day, weirdest looking genitalia I have ever seen.
//the other m(ixup)
coming soon//simple gifts //hustle and slow
//simple gifts
Nazir Hussain Blog

Conversation is the forefront of innovation. Simple ideas can be passed from one individual to another until they reach someone who can capitalize upon them. My partner, Sam Dreyer, is the President of BMES at UIC. One of his main personal goals within the program is to find a problem that could be addressed with a simple device design project for members of his chapter. Throughout this week doctors have been able to readily answer our questions but recently they have given us little gems of information that elude to a device design.
The first was during a carpal tunnel release. The procedure is completed with all of the surgeons seated in draped seats around the operating table, which is attached to the bed the patient is resting on. This particular table has a single leg which rests on the ground for support. Immediately we could see the work around doctors used on the table, the foot of the operating table had been wrapped in Coban. Coban is a self adhesive wrap that exhibits grip similar to a rubber end in this case it was used to replace a worn end. The primary question I had was why a simple piece like this needed a makeshift replacement as opposed to simply purchasing the required replacement piece. Considering the size of the hospital, it’s surprising that there isn’t a machine shop nearby to fabricate simple replacement pieces like this. Even more surprising is that since the U of I Hospital is in such close proximity to the UIC campus, it doesn’t have accessibility to the many machine shops on campus. It is my personal opinion that many of the makeshift parts could be replaced if a relationship between the hospital and a campus machine shop was formed.
When talking with another doctor during a later procedure he noted that the approximate cost of one minute of time in the OR was $80. This fact became more relevant when discussing the lengthy extension of a procedure due to the suturing and cast molding. The cast molding procedure requires that a scrubbed surgeon must physically hold the cast and limb in place in accordance to the angles for optimal recovery. This is arbitrary and done subjective to the surgeon, not to say they aren’t capable of doing that but human error does occur. For some surgical procedures, plaster casts are used as opposed to fiberglass. This is because plaster is much easier to mold, however, it take 20 minutes to hold. The approximate value of a device that could hold a plaster cast after it has been molded with similar or improved accuracy is at minimum $1600 per surgery. It also allows for a swifter surgery and potentially a faster turnover of OR. This problem statement could be resolved in a number of ways an will definitely be investigated further.
The last notable improvement we noticed is procedurally based. The turnover of a hospital room can run up to an hour and a half on average. This leads to less surgeries taking place which the room is being cleaned and then prepped for the next surgery. While options to address this problem have been introduced in modern hospitals, there are currently no well known options to retrofit an older hospital to these newer procedure. This will be looked into further over the next week.
//hustle and slow
coming soon//in the shell
Nazir Hussain Blog

Prosthetics and orthotics are why I decided to major in Bioengineering. The idea that you could replace and potentially augment a human limb eludes to a future defined by the limits of technology as opposed to physiology is mind blowing. However, until recently, I didn’t have an opportunity to work with prosthetics first hand. A recent research paper I wrote for a class at UIC, BioE 430, focused on the potential of myoelectric prostheses. These prostheses function in response to the electrical signals normally sent to muscles to cause motor function. The main benefit of these prostheses when compared to body powered prostheses is that myoelectric prostheses can fully replicate the intuitive function of a natural hand.
While in the clinic I had expressed an interest in the process for custom fitting a hip brace, as a patient from last week was scheduled to come in for the fitting process. According to our schedule I would not be present for the fitting process and as such I wanted to receive as much information about the procedure prior to. I was pointed to a Technical Representative from Scheck and Siress, a prosthetics and orthotics distribution company, who brought me to their facility at the hospital. The facility looked like a bike shop that sold prosthetics; the devices were strewn across work benches and parts hung from the walls and off of shelves. I was first introduced to the orthotic devices, namely the hip brace that would be used on the patient. The size range ran from infants to overweight adults with a vast set of parts reliant on the three main size measurements: the circumference of the waist, of the pelvis, and of the thigh. A single fitting for the thigh was connected to a waist band that surrounded the pelvic area in a similar fashion as the plate we saw attached to a femur last week. Limiting parameters such as maximum leg flexion and abduction were set by the orthotist who would be installing the brace. An important point was made differentiating the terms custom fit compared to custom made. Custom fit implies a device that is adjusted to fit the user, like a seat belt it can accommodate a large user population with a single design. Contrarily, custom made implies that a device is made specifically for the patient and is manufactured specifically for their body, like a tailored suit.
After the crash course in orthotics I was shown the golden egg of the facility, a $60,000 Ottobock myoelectric prosthetic hand named the Michelangelo. I had done a fair amount of research on this specific product and knew its capabilities but was ignorant as to where it fell short. The concept of a motor signal causing motion in the hand was straight forward and seemed almost foolproof. In addition, I asked the prosthetist if he found the Michelangelo to be more intuitive that other current market prostheses, especially considering its usage of pattern recognition to ‘learn’ the patient’s intended action and associate it with complex signals. To my surprise he disagreed pointing out a flaw within the concept of myoelectric prostheses. The electrical signal processed had the potential to misfire if it read a false positive or if the patient accidentally trigger the wrong mechanism, causing some patients to desire the simpler, body-powered, hook prosthesis. While the pattern recognition software offers the capability to prevent these misfires, modern myoelectric prostheses are still a developing technology. As such, it can be expected that in the foreseeable future problems such as misfiring will be addressed and eventually eliminated as signal processing and pattern recognition software improves.
Note: Image used taken fromOttobock.com
//horizon
Nazir Hussain Blog

The Illinois Bone and Joint Institute on North Michigan Avenue is a perfect example of the potential of a private practice. As an LLC, they enjoy the rights and privileges of the IBJI while retaining some level of independent function, thus operating similarly to that of a private practice. The clinic is nowhere near as hectic. The view is incredible, erected in close proximity to Millennium Park, with a full view of Soldier Field, the Field Museum, Shedd Aquarium, and Adler Planetarium. It’s more than evident that the attending physicians are leaders in their field. It is no surprise that one of these physicians is Dr. Gonzalez, the orthopedics department head. However it should be noted that with great power comes great responsibility.
Ensuring the patient is on the path to recovery is a doctor’s top priority whether in the clinic or the operating room. However it is important to note that this requires a patient to be present. One of our patients was an elderly woman with diabetes who presented with pain in her right knee. She was brought in by a caretaker who mentioned that she was new to the position and the previous caregiver neglected the patient. She was skinny, frail really, her face was sunk in a sorrowful gaze. Her right knee was very swollen, which the doctors assumed to be fluid. In an effort to reduce the swelling they asked her to change into a pair of paper shorts so they could drain the site. While we waited for her to be changed we viewed an x-ray of her right knee that showed damage caused by rheumatoid arthritis.
When we reentered the room my partner and I were visibly taken back. The patient’s legs were covered in what looked to be picked at scars or burns. As it turns out, it was caused by mismanaged diabetes developing ulcers on her legs. Not only did a significant amount of pain and scarring result from the neglect on behalf of her former caregiver, but future pain as the surgery could not commence with so many open wounds and her blood sugar levels.
It’s easy to get lost in the horizon from the 14thfloor of 150 North Michigan, but when you turn around the real world presents you with complex cases that you, as a clinician, are responsible for solving. Dr. Gonzalez stayed within the confines of his specialty, mentioning that the patient should see a wound specialist and lower her blood sugar levels before her next scheduled appointment. That is all he could have and should have done. Responsibility isn’t about being the one person who saves the day but being humble enough to let the best man do the job.
//jump
Nazir Hussain Blog

It’s not common to meet someone holding a current national record. It’s less common that this person used to have cancer. It’s even less common that this national record holding, former cancer patient, is an amputee who uses his foot as a knee. Sam Grewe is an incredible young man, whom I was able to meet this week during a stop by Scheck and Siress.
The focus of this visit was to become more familiar with the procedures the CTOs use to optimize a prosthesis for a patient. On the way to the office/machine shop, we passed up a father and his son sitting outside of the room. At first glance I noticed that the son has a prosthetic leg, but I pushed forward into the machine shop to find out that the young man outside was an athlete. I had heard of how many athletes Scheck and Siress work with, and the stories of amputees running quite quickly in the hallway. The limb he was going to receive that day was for athletic use and nor for daily use. With carbon fiber supports and an Ottobock blade, Sam would use this blade to compete in the high jump. The fitting procedure was quite lengthy, with CTOs referencing the extended hours needed to find the most comfortable fit, carefully cutting and removing small sections until 2 am. There were certain oddities about this prosthetic compared to other, primarily a section of carbon fiber near the knee joint. It appeared out of shape to fit a tibia and far too low to fit the femur. The CTO explained that the patient had undergone a procedure called a rotationplasty, where a section of a limb is removed and the remainder is rotated as needed then reconnected. After a few hours of laborious fine tuning, we took the prosthetic out to Sam where he put it on and laced it up.
Then, he ran.
His first run was his high jump form which differed significantly in lateral acceleration when compared to his more lateral form. He could easily outrun me, but his talent wasn’t amplified by the prosthetic, he was just thatgood. A few laps later, he gave his opinion on the fit and adjustments were made to prevent any irritation or uncomfortable friction. Without a doubt the impact of orthopedics is more than evident, not only can an amputee walk, but run, and even jump higher than any other man of his caliber.
//sophisticated savagery
Nazir Hussain Blog
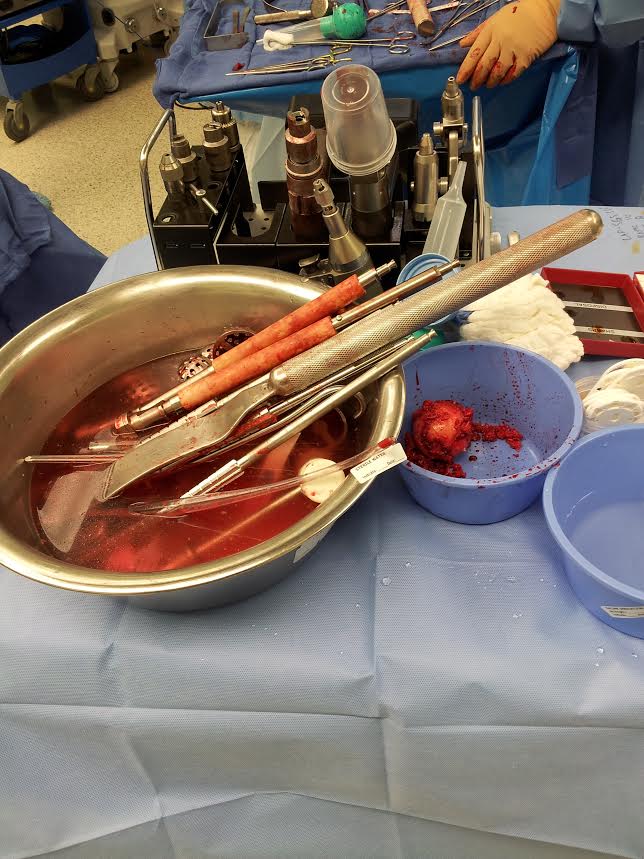
Surgery is often either gentle or completely medieval in the eyes of the media. Shows like House thrive off of the lack of synergy between the two, however the realism lies more with the human element of the proceedings. Surgery is difficult, which is no profound statement, however it is interesting to see how the surgeons react to stress. On TV you see the beads of sweat resting on the forehead of a frantic doctor, worried about the next complication. In the OR you find that doctors will step away from a patient, frustrated and at times impatient before calming down and returning to the procedure. The control over human emotion is incredible, even when a surgery is difficult or not going to plan the near nullification of frustration is only a moments notice away.
During a particular case in the last week of our rotation we were able to view a revision surgery. In the most basic sense it means that the prior surgery had a flaw major enough to require another corrective surgery. The patient was a large man whose hip replacement slipped and caused a hole in his femur. Initially I believed that the hole in the patient’s femur needed to be plugged prior to the insertion of the next hip replacement. The attending physician informed me that the reason for the slip and subsequent hole was because the hip that was inserted into the femur was too small.
Overall the surgery seemed similar to the total hip arthroscopy we had witnessed earlier that day. The removed hip rested next to a bowl filled with bloodied tools resting in saline in the previous procedure. This time there was an artificial hip as opposed to the ball of the organic hip, tissue from the bone still clinging to the rougher edges of the artificial hip. Looking at the blood stained surgeons you could almost assume the procedure was medieval. This was until you noticed what was happening with the blood. It was being suctioned and then filtered into a large basin, to then be placed into bags and circulated back into the patient. This prevented the need for withdrawals from the blood bank for a patient.
The procedure was going according to plan until suddenly the attending backed away from the table. There was a very still moment within the OR and then he spoke, “The femur cracked”. His frustration was more than apparent, but in the blink of an eye he was back, calm and ready to proceed. His calmness was much needed as the 3 hour procedure immediately doubled in length with that simple crack.
//breathe
Nazir Hussain Blog

My rotation with Orthopaedics has finished and now I am beginning my rotation with the Pulmonary Critical Care division. Walking in to the hospital to meet and greet a new set of doctors, nurses, and medical assistants reminded me of walking in 3 weeks ago to meet Dr. Chmell and the Ortho Team. This time I met with Dr. Dudek and later the two teams he directs.
It’s crazy how just 4 weeks ago I was picking up my hospital badge, excited to start the internship I had been waiting all summer for. After picking it up there was a second card behind the badge explaining the various codes that may be called over the intercom system. The most confusing for me was the Number 1 Emergency. I’m rather cynical so the next thing that I wondered was what constituted a Number 2 Emergency and the priority given to each one. For the next 3 weeks I wouldn’t ask for clarification as I had plenty to learn from in the Ortho Department; however within the first few days of being with PCC, I would experience a Number 1 Emergency first hand.
Dr. Dudek clarified that Number 1 Emergencies happen every other day within the Medical Intensive Care Unit (MICU), and are called when a team of doctors is needed to treat a patient in arrest. This may include respiratory arrest or cardiac arrest, in either case it requires a full team of doctors because as Dr. Dudek said, “The patient is actively dying”. I wasn’t prepared for this concept, seeing lots of blood in a surgery or the smell of bone dust didn’t bother me because often the patient would walk out of the facility. To think that someone I was going to pass in the halls often could eventually simply be gone left a very empty feeling within me.
Day 2 began with a tour of the MICU during the PCC Rounds. These took about 2 hours to complete and required anywhere from 9 – 16 doctors to occupy 150 square foot area in the hallway. A report was given on each patient’s current status and the doctor went in to see the patient and get a response if he could. This hit home hard as during the first week of the internship a close friend of mine was in the NSICU, across the hall. There was a very stark realization in the fact that this is where people fight what could be their last fight. This is where every breathe counts and all you have left is your life. The world outside seemed to no longer matter when I realized that this is where my friend had been admitted for a few weeks, fortunately she is presumed to make a full recovery in due time.
Lunch was a moments reprieve from the morbidness that is the MICU. Laughing with the other interns as rap battles commenced, hair advice was traded, and stories were told took my mind away from what I would inevitably have to return to. The final fleeting minutes of the break were approaching when on the intercom an announcement was made, “Number 1 Emergency in Room 6xx. Number 1 Emergency in Room 6xx.” My partner and I sprung up, we knew we had to go to truly immerse ourselves, but it wasn;t the most desirable pool of knowledge.
Walking into the room the air changed. There were 17 doctors scattered around the room, it seemed like madness. There was no way they could be any near as coordinated as the OR staff. The patients pO2 dropped quickly, at times flat lining to zero as the heart pumped at 150 bpm. Then his blood pressure skyrocketed. In the back of the room, amidst the rushing doctors and the chaos and tension there was a woman. She must have been the mans family member, rocking back and forth with tears streaming down her face. I found myself tense as well, hoping I would not have to see her watch a loved one die.
This is real.
This is all very real.
People live and die daily in the rotation I am in, changing the lives of those around them instantly.
This is the world I have to improve, to make safer, to make easier.
That is my responsibility as an engineer.
//for the love of
Nazir Hussain Blog

We talk about empathy a lot in this rotation. Considering the amount of time spent in the MICU we have to be careful with every action we make. Curiosity isn’t exactly welcome by families with admitted loved ones. Nevertheless we are there to learn and that can be accomplished with a bit of tact. Taking interest in the discontent of a patient’s family leads to conversations about the patient’s perceptions about hospital procedures. This opens a dialogue that can help enhance transparency in certain areas so that patients are more aware of why certain actions are taking as long as they are. Discussing difficulty completing a test or discomfort while a minor procedure was taking place allowed for insight as to shortcomings regarding the devices and procedures used by doctors. Essentially, we had to listen to the patient’s complaints. However, it’s interesting how I feel that we get more out of a patient within the brief conversations that take place as opposed to the results I assume they receive in the rarely completed surveys offered online. The difference being that now the person that is hearing your plight is also coming to you as opposed to waiting for you to go and fill out a form on your own time.
While exploring the odds and ends of the supply room, filled with various equipment used for everything ranging from testing procedures to IV equipment to basic hygiene. While certain items held interesting purposes, like the green dots sterilizers that allow doctors to sterilize the connector ports of IVs quickly and effectively, there was one item that stood out from the rest.
A teddy bear.
Surrounded by hygiene products like toothbrushes, deodorant, and combs, there was a basket filled with fluffy brown bears. Although it is easy to assume why they were there, I asked the nurse and received an answer slightly outside of my original thoughts. As opposed to being used to comfort as children, the teddy bear served multiple purposes. Some patients who may have been in the hospital as a child may find it comforting and reminiscent to the past the overcame and hold onto the bear. For others it serves as a new texture as opposed to the crisp sterility of hospital sheets. The most unique application involved a small overlooked feature of the bear, its flat back. Patients with may find hugging the bear with its back facing their chest may help alleviate various pains the patient may feel. Overall, this adorable stuffed animal shows how easily it is to integrate the empathy into the melancholy of the MICU. Simple actions followed by simpler objects can help create comfort during an incredibly difficult time.
//grey area
Nazir Hussain Blog
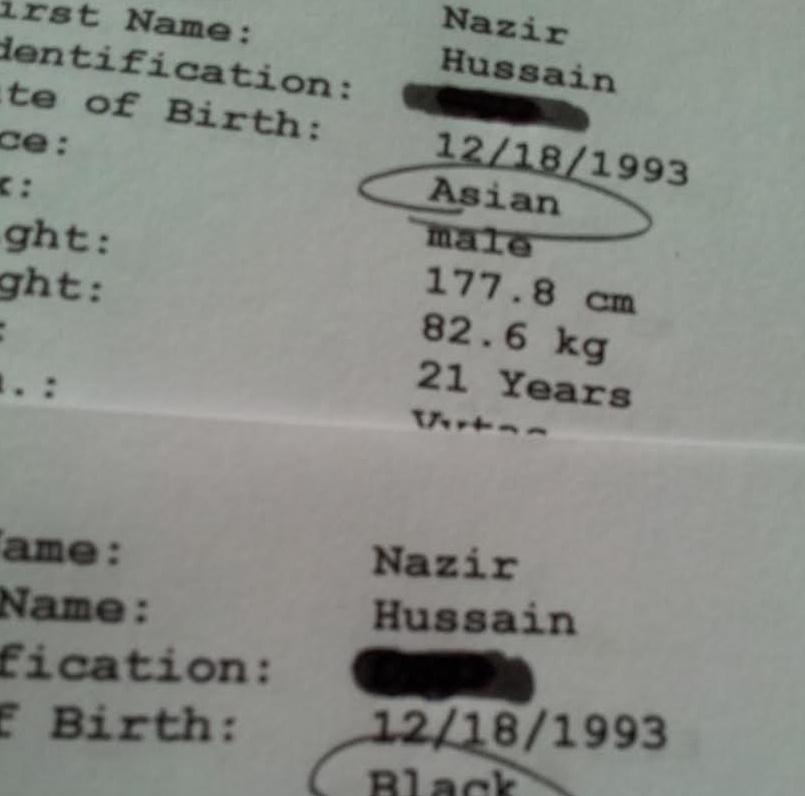
I’m biracial. A product of my Indian father and my African American mother, I’ve been exposed to both cultures at different stages of my life. A significant part of my childhood was spent surrounded with Indian food and culture, influencing my upbringing and understanding of race. this changed when I moved to the suburbs in my early teens and, for various reasons, I was able to more easily identify with the black part of my heritage. Being able to understand the differences between the two cultures while existing in the grey areas between them has allowed me to shift between the two depending on the circumstances I am in. For the most part the choices I have made and the perception of my race in the eyes of others has had no truly major difference in my life. Until Wednesday.
I took a PFT or pulmonary function test. In the simplest terms you blow into a pipe in different breathing patterns and intensities. Various metrics including volume and flow rate are then processed to provide information regarding the state of the patient’s overall pulmonary function. The test requires that each section is reproduced three times with relatively similar results. The technicians who perform the test are incredibly expressive and coach patients so that they can provide the proper waveform to the best of their abilities. The only profession even slightly similar to the expressiveness of these technicians would be a futbol commentator. After about half an hour the test was complete and my results were read to me. The first thing the technician mentioned was that I had about 70% of the lung capacity as compared to the predicted capacity based on my height and weight. I explained that I used to be a heavy smoker a few years ago and the technician stated that this wouldn’t explain such a large discrepancy at such a young age. He also noted a flattening of the bottom of my Flow vs Volume waveform, which signified restriction while inhaling. This could be a cause for my snoring if related to redundant tissue near my esophagus.
Another patient entered the room maybe 10 minutes after I had completed my test and we were prepared to observe the procedure. The technician asked the patient if she identified as Hispanic and she replied that she is Latina. I asked if race was a factor in the testing to which he replied that the only race with more than marginal changes in predicted values was African Americans. There is an overall 15% difference in some predicted values which alters the subsequent calculations quite a bit. This is dude to African physiology, comprised of smaller torsos and longer legs. I noticed the technician had set my race to Asian, which he based off of my last name, and asked if he could reprocess the results as Black. There was still restriction present, easily explained by the smoking, but the results improved dramatically. For the first time being lost in the grey area between races wouldn’t suffice.
//forty two //reminisce //the big G
//forty two
Nazir Hussain Blog

It has been forty two days since we first began this internship. The time flew by quickly and the perspective I had of the program transformed throughout the 6 weeks I spent shadowing clinicians and patients. To be completely honest I wasn’t entirely thrilled with the idea of my first and only undergraduate internship would come from the university I attend. However, looking at the intensity and true immersion the program has provided, I am more than exhilarated from my experience and the opportunities afforded to me. The understanding of how the University of Illinois Hospital functions not only as a hub for medical teaching, environment of healing, and as a profitable business puts quite a bit about the healthcare system into perspective.
//reminisce
I waited over a week to actually post this post so that I could revisit some of the thoughts I initially had about the internship. Also, I wanted to be able to describe the feeling of coming back to school after an internship. This semester I am taking 18 credit hours. The mere concept of that initially would make my stomach turn over in the past. However, after seeing the discipline and drive of physicians under pressure, I’m both inspired and motivated to take the task at hand on. Knowing that I want to pursue an M.D. in the future, it is more than possible for me to complete my degree with excellence.
//the big G
God. There are countless religions, conflicts, and controversy surrounding the topic/idea of an absolute power. For some, God is the final solution, to others a pure fallacy. However there are places when the views of one should not be forced upon another. The hospital is one of those places.
One thing I have not talked about was the fact that the a few days prior to the beginning of the internship, one of the most active and prolific friends I have suffered an incredibly debilitating injury. She is destined for greatness. Weeks after meeting with Chelsea Clinton, and months prior to what was supposed to be her presentation to the United Nations in New York, she had sever neck pain and was completely unable to move her left arm. The doctor she went to see ignored her symptoms, which pointed to a neurological issue, instead stating that “It could be a pinched nerve or something” and leaving without actually treating the patient. Within days she suffered an aneurysm near her medulla due to an undetected AVM (arteriovenous malformation) which could have been prevented by some level of competency by the doctor who saw her (please note this doctor was not from University of Illinois Hospital).
She could have died. Most people die. She is not most people.
As her body was shutting down, and while fighting through excruciating pain, she managed to call 911 and was taken to the hospital where she was stabilized and then cared for. Throughout the 6 week internship she was at University of Illinois Hospital, making visiting her more than convenient. I was there to see her unable to move or speak, when her sensory and motor function was severely impaired. I was there to see her cry due to nurses’ lapses of empathy. I was there to see her wiggle her toes again, when the doctors told her she could make a full recovery. I was there to see God become an issue.
Poop. It’s usually inconvenient, it’s usually smelly, and it usually causes pain if you can’t release it. Part of losing all of your motor function is the inability to open your sphincter. The buildup of bowels due to constipation was causing her intense pain. During a brief stay at RIC, she found that digitally impacting her bowels provided immediate relief. Now, this a gross procedure. A nurse would have to stick their finger up the patients rectum, and essentially poke around until the poop comes out. For those of you who have made it this far in the post, this is where things come together.
My friend’s nurse at UIH for the day was a woman named Carol. She is known for her Catholic beliefs. After suffering in pain due to days of constipation, my friend asked the nurse to digitally impact her. An abridged version of the conversation is below.
Patient: Hey I’ve been constipated for days. Can you do this procedure they did at RIC?
Nurse: Are you Catholic?
PT: Uh, sure.
NR: You should pray to this saint. She was a guardian for those in pain.
PT: Are you giving me spiritual advice as opposed to medical care?
NR: It’s almost 3 pm, you should really pray. Do you know why we pray at 3 pm? Jesus died at 3 pm.
PT: If you won’t do the procedure will you find someone who will?
NR (quoted because I will not forget the sheer gall of this statement in a hospital): “You should embrace your suffering. The pain you feel is saving countless souls”
This is not a joke. This nurse said this. There are moments where God can be someone’s hope and salvation, and there are times when God has given you a procedure to help alleviate the pain of a patient.
Sam Dreyer Heading link

I am a Bioengineering student with a focus on Neural Engineering. As the President of the Biomedical Engineering Society on campus, I am passionate about enabling students to utilize their skills and change the world.
Sam Dreyer Blog Heading link
-
Sam Dreyer Blog
First Impressions (7/6/15-7/8/15)
Sam Dreyer Blog

After just the first two and a half days in the program, I am already impressed with the wide array of experiences I have had the pleasure of being exposed to. My first rotation is in the Orthopedics division and I spent the first afternoon observing outpatient procedures with Dr. Chmell.
The most engineering-focused case was when Dr. Chmell showed us some x-rays from a patient with a tibial fracture. This patient had a titanium rod inserted through the tibia to assist with healing. Until fairly recently, these rods were typically stainless steel but titanium has surged in popularity due to the fact that it’s modulus of elasticity is more similar to that of bone. However, the rod was now bearing the load instead of the bone. This greatly reduces the force of compression at the point of injury, which is actually what stimulates the natural calcification healing process.
The next day was spent in the operating room (OR). Here we began by observing two total knee replacement surgeries. These were fairly routine procedures for the team on staff and I was very impressed by their speed and efficiency. The distal portion of the tibia is actually sawed into a boxy shape and then the titanium replacement is fitted onto it, without the need of sealant to fill the gap between the bone and the implant.
Here are some of the most interesting observations from these surgeries:
- Before the procedure begins, blood samples are taken from the patient. The platelets are extracted from the samples and concentrated during surgery and then injected back into the patient at the site of injury to speed the healing process. Emphasizing as natural as possible solutions was something I hadn’t previously considered.
- Representatives from the company that designs and builds the implants were actually in the OR during the procedure and advising the doctors on which size implants to use. The doctors all spoke highly of the depth of knowledge of the reps with regards to their products and were glad they were present for the operations.
- At the interface between the bone and the implant, the implant was coated with a layer of hydroxyapatite. This encourages bone fixation and allows for the implant to be attached to the body without the use of cement.
The last surgery we observed on that day was a young male with a severe tibial fracture as a result of a gunshot wound. This involved screwing a titanium plate onto the tibia across the fracture. To constantly gauge the progress of the surgery and check the location of the screws, there was a constant stream of x-rays taken; requiring us to wear a lead jacket throughout the operation.
Due to the rarity of operations like this, the industry representative was even more instrumental in the success of the surgery. He continually talked the doctors through the correct implementation of the proprietary instruments. While extracting the bullet was ultimately not feasible, the plate was attached successfully.
Lastly, the first portion of our third day was spent in the audience of an Orthopedic conference. Doctors and medical students took turns presenting different case studies or specific injuries to the group. Occasionally, people would be called on to answer questions about the anatomy or treatment so you had to be on your toes!
Over the first couple of days in this program, I have had an incredible array of experiences. From the OR to the clinic to the classroom, there is always something new to learn.
The Rest of the First Week (7/8/15-7/10/15)
Sam Dreyer Blog
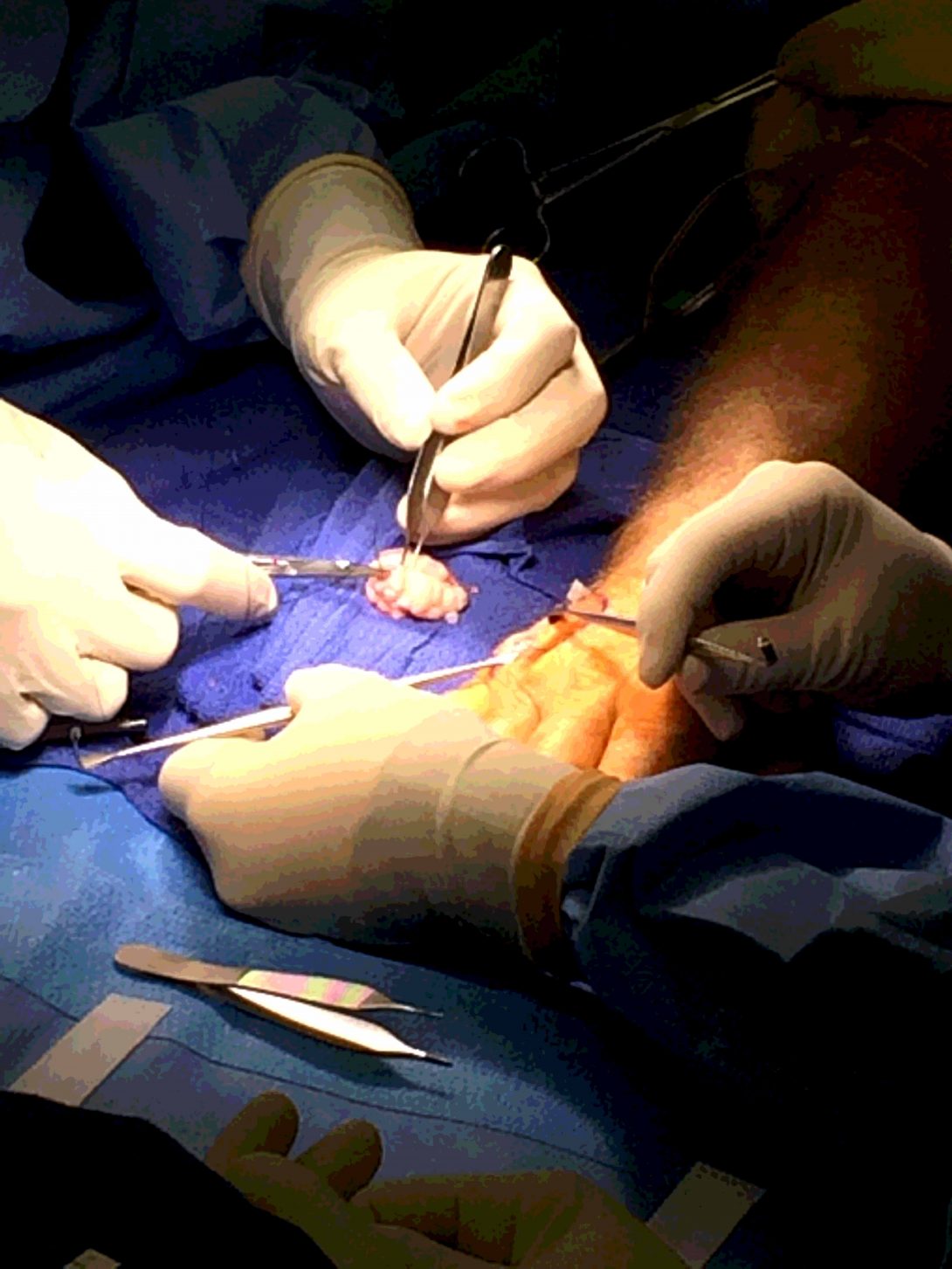
After wrapping up the Orthopedic Conference, we attended training for the first year residents led by Dr. Mejia. While the training videos about suturing and other skills were interesting, Dr. Mejia’s anecdotes about real-world benefits and drawbacks helped make the lessons more applicable. One comment from Dr. Mejia concerned the practice of “signing your site.” This is where the surgeon writes his initials on the body part to be operated on before the surgery starts. Apparently, before this was implemented, 24% of orthopedic surgeons would accidentally operate on the wrong side of the body at least once in their career. I, for one, am thankful for this change in policy.
Another surprise for me at my first look “behind the curtain” of healthcare was the physicians use of the internet. It’s very easy to assume that physicians are a walking encyclopedia of medical knowledge and let the title “Doctor” mask the fact that they are real people, with the same limitations as the rest of us. The medical field is so advanced and full of information that many caretakers will take a moment to refresh their knowledge of the specific issue the patient is presenting in order to provide the best possible care.
Dr. Mejia said something during our clinical time that really changed my (biased) view of how doctors treat patients. A patient arrived that was supposedly suffering from “trigger finger,” a condition in which a patient’s finger will sometimes lock in a fixed flexed position. However, while the patient had been recently asymptomatic, they were very insistent on receiving a shot to help with the ache. Here is my poor attempt of paraphrasing what he said, “Everything in medicine is a risk assessment. Even if the patient wants something, the shot could lead to an infection, a diabetic reaction, or other negative things. The odds are low but it is still a risk. There is no risk for wearing a splint.” As an engineer, I feel like I’ve had a bias to jump to the solution, any solution. Think a shot will help? Sure, let’s go for it? Reoccurring pain? How about surgery? This statement made me realize the emphasis in the medical field on starting with treatments that are as minimally invasive as possible and only once all options have been exhausted, moving up from there.
On Thursday, we spent the full day in the clinic working with patients. This was also my first time seeing one of the coolest pieces of technology I had seen so far; the “lidocaine popper,” also known as the J-Tip syringe. This syringe uses compressed carbon dioxide instead of a needle to deliver the drug through the skin.
Friday was spent entirely in the operating rooms with Dr. Mejia. The day began with two carpal tunnel release procedures. For these, I was most impressed with the efficiency of the tourniquet. With how highly vascularized the hand is, there was essentially no blood until the end of the operation when it was released just before suturing. We also had the opportunity to observe a mass excision which is pictured above.
The last patient required a finger amputation as a result of severe frostbite. Even after my short two days spent on the opposite side of the surgical knife, it became easy to dissociate with the patient in surgery. Until this final patient. While waiting for the anesthesia to set in, his teary gaze remained locked on his hand. It was one of those moments in where you feel like you know a stranger’s thoughts. The empathy came back quickly as I realized he was looking at his finger on his hand for the last time.
What a way to end my first week.
Clinic Time (7/13/15-7/14/15)
Sam Dreyer Blog
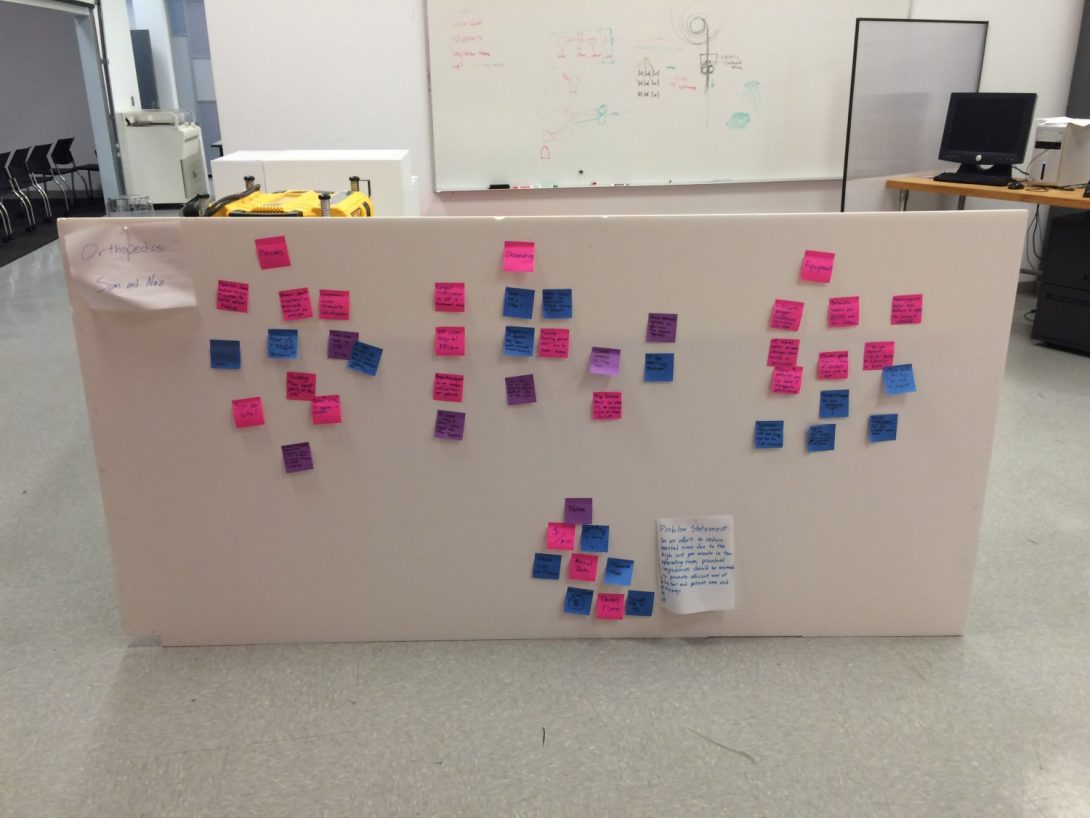
At the beginning of the second week of our program, we once again met as a group to discuss the specifics of our final reports and catch up on the progress of the other students. Hearing the differences in the daily routines within each specialty was very interesting. We also discussed different ways to extract information from the professionals we were observing without being too intrusive and interfering with their job. To help present our initial observations to the rest of the teams, we built a design board with post-it notes under three different categories: Equipment, Process, and Observations (pictured). Lastly, Naz and I talked about which “problem statement” we were going to identify in our final report. While I had reservations about this due to only having one week of experience to draw on, as we talked about our interactions with all of the medical staff it became clear that there was one thing on everyone’s mind: time inefficiency. With so many patients to see in a given day, any sort of delay in the process has massive effects on everyone involved. For example, a delay of one hour in the operating room makes every subsequent patient wait another hour (at least) before being seen, costs the hospital $4,800, and keeps the doctors and nurses at work and away from their family for an additional hour (again, at least). We agreed that any process or product that could assist more efficiently leveraging time in the operating room would be gratefully received.
That afternoon, we were back to clinical rotations. Right away we were introduced to a new medical procedure that heavily utilized engineering principles. It is called a “reverse shoulder replacement” and works by replacing the “ball” and “socket” portions of the shoulder with titanium implants and switching their natural orientation. This is due to the physics of the musculoskeletal system. To lift your arm, the deltoid takes on most of the load but also requires activation of the rotator cuff. In patients with a torn rotator cuff and a regular shoulder replacement, this is very difficult because the deltoid is only able to lift the arm partially. With the reverse shoulder replacement, the ball portion of the joint is attached to the scapula, allowing the deltoid to “roll” the joint up the ball and raise the arm on its own.
There was a patient at the end of the day that came in for a third opinion. He was a seventy seven year old man experiencing some shoulder pain. Two previous doctors had told him that they wanted to do a reverse shoulder replacement and he wanted to confirm with Dr. Goldberg that the surgery was his only option. After examining his range of motion, Dr. Goldberg told him that he could get the surgery if he wanted but if there wasn’t significant pain and his movement wasn’t inhibited, he didn’t need the surgery unless he wanted it. The patient was very happy to hear this and said, “I’ve been told twice that reverse shoulder replacement is [the only option] by doctors that never asked about my quality of life.”
The next day was spent with Dr. Gonzales at the Illinois Bone and Joint clinic on Michigan Avenue. We observed seventeen patients over the course of six hours which kept things at a steady pace without feeling too overwhelming. One thing on the mind of many of the doctors was the recent release of surgical complication rates by ProPublica. While doctors support transparency, there were some issues with how ProPublica decided to define complications. For example, readmissions are counted toward a doctor’s complication numbers. Additionally, there were concerns that this type of ranking would negatively impact patient care. Doctors concerned about their ranking may be inclined to not accept patients needing procedures with a high risk of complications, such as infections.
Processing (7/15/15-7/17/15)
Sam Dreyer Blog

Wednesday was spent back in the clinic and was mainly uneventful. Even after roughly a week of experience in the clinical setting, some of the symptoms that patients came in for were starting to feel routine for me. That’s not to say that I am anything close to resembling an orthopedist, but you can only see so many people with carpal tunnel or trigger finger before they all start to feel similar and predictable. In one regard, I find it incredible that we’ve identified such specific and universal physiological markers of underlying disease that can be easily measured. In another, especially as a passive observer, watching a doctor tap on a patient’s wrist is only novel for so long. A couple of patients were entertaining purely due to their unshakable belief that they knew more than the doctors. I don’t think I’ll ever understand the reasoning of a person that goes to a professional for a diagnosis and then argues with them if they don’t like what they are hearing.
Thankfully, the next day we were back in the Operating Room with Dr. Gonzalez. The first procedure was a total knee arthroplasty, something I observed the previous week with Dr. Chmell. Having already seen the procedure twice before, I was feeling pretty confident that this would be right in line with expectations. And, for the most part, it was. Until they began prepping the inner portion of the implant with a thick paste. My mind scrambled, “Where’s the hydroxyapatite?” It turns out that doctors are actually given a significant amount of freedom to choose the tools that deem best for each surgery. While one doctor may feel that the bone ingrowth onto a hydroxyapatite-plated implant is significant enough for use, another may feel that the cemented method is more reliable. If there is no significant consensus in the literature, both are allowed to perform the surgery in their own way. While I do have some reservations about this degree of personal choice, I’ve ultimately decided that it’s probably best for the doctors to be as comfortable during surgery as possible.
Next up were a couple of closed carpal tunnel release surgeries using an endoscope with a blade attachment. This was a very cool procedure to observe because the endoscope was attached to a large screen and the point of surgery was very easy to see, unlike some of the other operations we had seen in the past. The advantage of doing this surgery “closed” is that the doctors only need to make one small incision for the endoscope instead of cutting open the whole wrist. However, the correct ligament is sometimes more difficult to find. In one of these surgeries with a fairly obese patient, the ligament was lost in all of the fat tissue and the surgeons were having so much difficulty locating it that they almost switched to an open surgery.
We closed the day by sitting in on a ligament reconstruction. The patient had torn a ligament in their thumb and had lost significant functionality. The doctors solved this by removing a vestigial tendon in the wrist and reattaching it to the thumb. This degree of resourcefulness really impressed me. As we learned later, artificial tendons and ligaments still have yet to be developed and so doctors have discovered a non-functional tendon from the patient’s own body that they can simply remove and “reinstall” somewhere else entirely.
Friday morning was very slow due to abundant patient cancellations. The heat index at 105 degrees was very likely a contributing factor and I can’t say I blame them! In the afternoon, Dr. Gonzalez presented a very insightful overview of the engineering applications within orthopedics.
Clinic and Casting (7/20/15-7/22/15)
Sam Dreyer Blog

To start our final week of the first rotation, we met at the Innovation Center and participated in a workshop geared to get us thinking about empathy. As I’ve written about previously, the one thing that has surprised me about my experiences so far is how quickly and easily I detached myself emotionally from the patients. It’s very easy to be so concentrated on the procedure and the problem getting fixed that the fact this is a living person drifts to the back of your mind. We spent that afternoon in the clinic with Dr. Chmell. After seeing a total knee replacement done with using cemented implants, I wanted to know why he chose to use the cementless implants with hydroxyapatite. While he had a number of reasons for doing so, he emphasized one particular point. He said, “Academic institutions should be at the forefront and using the latest and best technology.” I was not expecting an answer like that and was very impressed. It makes a lot of sense to me that the medical students should learn the newest technology because that is what they will most likely be seeing a lot of early in their careers. Obviously the technology will continue to improve over their career, but by starting out their careers with experience at the bleeding edge, they are more capable and knowledgeable.
Next we got permission from the Scheck and Siress representative to go down to the basement and get a tour of their workshop. This was definitely one of the coolest experiences for me so far. My admiration for prosthetics was one of the driving factors for be choosing to get a bioengineering degree and seeing all of the different varieties up close and personal was awesome. One thing that stood out to me right off the bat was how realistic some of the prosthetics were. I’d seen pictures but what blew me away was the fact that even in person and up close, it would be almost impossible to notice any difference. While I think I would personally want something more robotic looking, some patients have psychosocial concerns and want to blend in more.
We also met a patient who lost their knee to cancer at thirteen years old. Instead of living with a complete above the knee amputation, he elected for a rotationplasty. This is where the tibia is fused to the femur and the foot is rotated completely, allowing the ankle to function as a knee. I certainly had my doubts about the viability of the ankle being able to support weight and bend to the degree that is done by the knee but these were quickly silenced. It turns out that the patient is a record holder in the high jump at the paralympics! He had come in because his new knee was having some slippage with the prosthetic when he was running. The machinists were able to quickly attach some velcro straps that held the heel of his foot (now in the location of the patella), more securely. After a couple of incredibly fast practice runs down the hall, the velcro was doing its job.
We spent Tuesday with Dr. Gonzalez at the Illinois Bone and Joint Institute and it ended up being a pretty slow day. In one of the lulls, Dr. Gonzalez took the time to give us a lecture on the biomechanics of the digits which covered that anchor points of the muscles, tendons, and ligaments and the physics of how these work together.
Finally, on Wednesday morning, we sat in on a class taught by Frank, the orthopedic technician. Frank’s class covered a lot of interesting differences between fiberglass and plaster casts including the whens and whys between the two. In his experience, the older clinicians prefer the plaster because they’ve used it throughout their careers but he hasn’t seen a preference in recent years graduates.
I can’t believe that I only have a couple days left in orthopedics! Even when consciously trying to take it all in and process everything (which is pretty much impossible in the medical environment), it has flown by so much more quickly than I expected.
Final Thoughts on Orthopedics (7/22/15-7/24/15)
Sam Dreyer Blog

After three blazingly fast weeks in the Orthopedics department, my rotation has come to an end. First, however, I’d like to focus on everything that happened in the last portion of this final week.
After Frank’s casting class, we attended another lecture to all of the residents led by Dr. Gonzalez. The topic concerned hip implants, something we had not seen yet in the operating room, but had been seeing in x-rays and hearing about since the beginning of the program. This was very convenient because we would be seeing two different hip procedures the very next day. That afternoon was spent in the clinic and was a very atypical experience due to the low number of patients. The only real moment of note was a patient that had torn their ACL and meniscus. While talking the patient through the procedure, Dr. Goldberg explained that it could be done using the patient’s own tissue, or taking the tissue from a cadaver. A patient electing to use their own tissue faces lower rates of infection or rejection, but also loses about 10% of their knee flexion strength (not enough to be noticeable to the patient). Most patients see this as a fairly easy decision to elect for their own tissue and this patient was no exception.
Thursday was our last day in the operating room with the orthopedics team and it did not disappoint! As I mentioned earlier, we had the opportunity to begin by observing our first total hip arthroplasty. While I could probably write a whole post just on this procedure alone, I’ll stick to the moments I found to be most interesting. For starters, the patient needs to be held on their side during the procedure. This is accomplished by rolling up edges of the bedroll and inserting posts into the bedframe which brace the patient on their side. I also noticed levels of sterilization within layers of sterilization. For example, the patient must be sterilized, draped, a “sock” applied to the body part of interest, and lastly, an Ioban surgical drape must be applied to the skin around the point of incision. There’s the whole overview. You may, as I previously did, consider these steps to be singular. The interesting part I noticed was during the sterilization of the limb with the betadine surgical swabs. Even then,you sterilize the dirtier portion last (in this case, the foot), without going back over the surgical site with the now “less sterile” sterilization swab. A little confusing, but also makes a good deal of sense.
We also had the opportunity to observe some more carpal tunnel release surgeries with the endoscope. One we missed completely by observing a different operation in another room. While we were walking back to check in on it, we caught Dr. Gonzalez leaving the room. He had taken just thirteen minutes from incision to suturing to complete the entire procedure. This was very impressive to me and I took it as a revealing glance inside just how effective and efficient modern medicine can be.
The next surgery was not quite as smooth. This patient was in for a hip arthroplasty revision, meaning that they were having issues with their current implant and need it removed and repaired. In this case, the implant hadn’t been sized properly for the patient and had wiggled in the bone, eventually breaking through the bone wall with the distal portion of the implant. While removing the implant and drilling a new hole for the new implant, the femur fractured. This required additional work where wires had to be wrapped around the femur to keep it in place. Six hours after incision, the procedure was finished.
We spent our final day in Orthopedics back with Dr. Gonzalez in the clinic. Where we gave a patient a steroid injection for trigger finger in his pinkie. He claimed to have had corrective surgery to each other digit, but only wanted the injection for now because the recovery time would prevent him from attending Burning Man. Whether it’s the patients, the residents, or the doctors themselves, you never know what to expect in the medical field.
Next week I’ll be starting a new rotation with a new partner. I hope to learn as much as I have these first few weeks and I’m sure I will. I can’t believe this program is at the halfway point!
First Impressions on Urology (7/27/15-7/29/15)
Sam Dreyer Blog

Well my first rotation is up and it’s on to the next one: Urology. My introductory reading on the subject informed me that this particular discipline focuses on the urinary tract system and male reproductive organs. The main reason that Urology was at the upper end of my preferred rotations is their extensive use of the da Vinci surgical robot, which is one of the coolest and most advanced pieces of medical technology around today.
Right off the bat, we observed a transurethral resection of the prostate using cystoscopy. The patient was having difficulty urinating due to an enlarged prostate, which had to be trimmed down. To accomplish this, they used a laser which is tuned to the specific wavelength of blood vessels. This allows the doctors to clear away the obstructive tissue without bleeding, very similar to the cauterization tools like the Bovie which I saw used extensively in Orthopedics.
The actual implementation of this involves pushing a scope through the urethra up to the location of the blockage, and then passing this laser through the scope to precisely target the tissue. Now, you may be thinking that this sounds like a lot of things to be passing through a urethra and you’d be right. I’m going to try and describe this as clinically as possible but seeing it in person was much more visceral. As we were told by one of the doctors, “The urethra must be dilated to fit all of the equipment.” This is done by inserting rods of increasing diameter into the urethra to stretch it out until it can handle having a relatively large scope pushed through it. After that initial trauma, the rest of the surgery went smoothly and was very fun to observe.
The next surgery we had the opportunity to see was a robotic partial nephrectomy. We finally got to see the da Vinci machine in action! This patient had a tumor on top of their kidney that had to be removed and seeing it happen had to be one of the coolest procedures I have seen to date. Here’s some awesome things I noticed while watching the da Vinci machine at work:
- Two camera feeds allows the operator to see the operation take place in three dimensions. At first, I was skeptical about how useful this would actually be (thanks 3D movies), but I was truly blown away after sitting at the operator’s station. It was like seeing it in front of you, it was incredible.
- There is a special screen in the operating room which can be written on by other doctors much like an NFL commentator. These annotations can be seen by the operator and used to target specific tissues.
- The da Vinci also allows the doctors to place a an ultrasound feed beneath the main screen of the operator. With this enabled, they can use an ultrasound probe and see what is beneath the tissue in front of their instruments.
The first half of the first week is mainly about getting used to the new rotation and taking it all in. I’m very impressed by everything that has happened already and can’t wait to see what will happen during my time in Urology.
End of Week One in Urology (7/30/15-7/31/15)
Sam Dreyer Blog
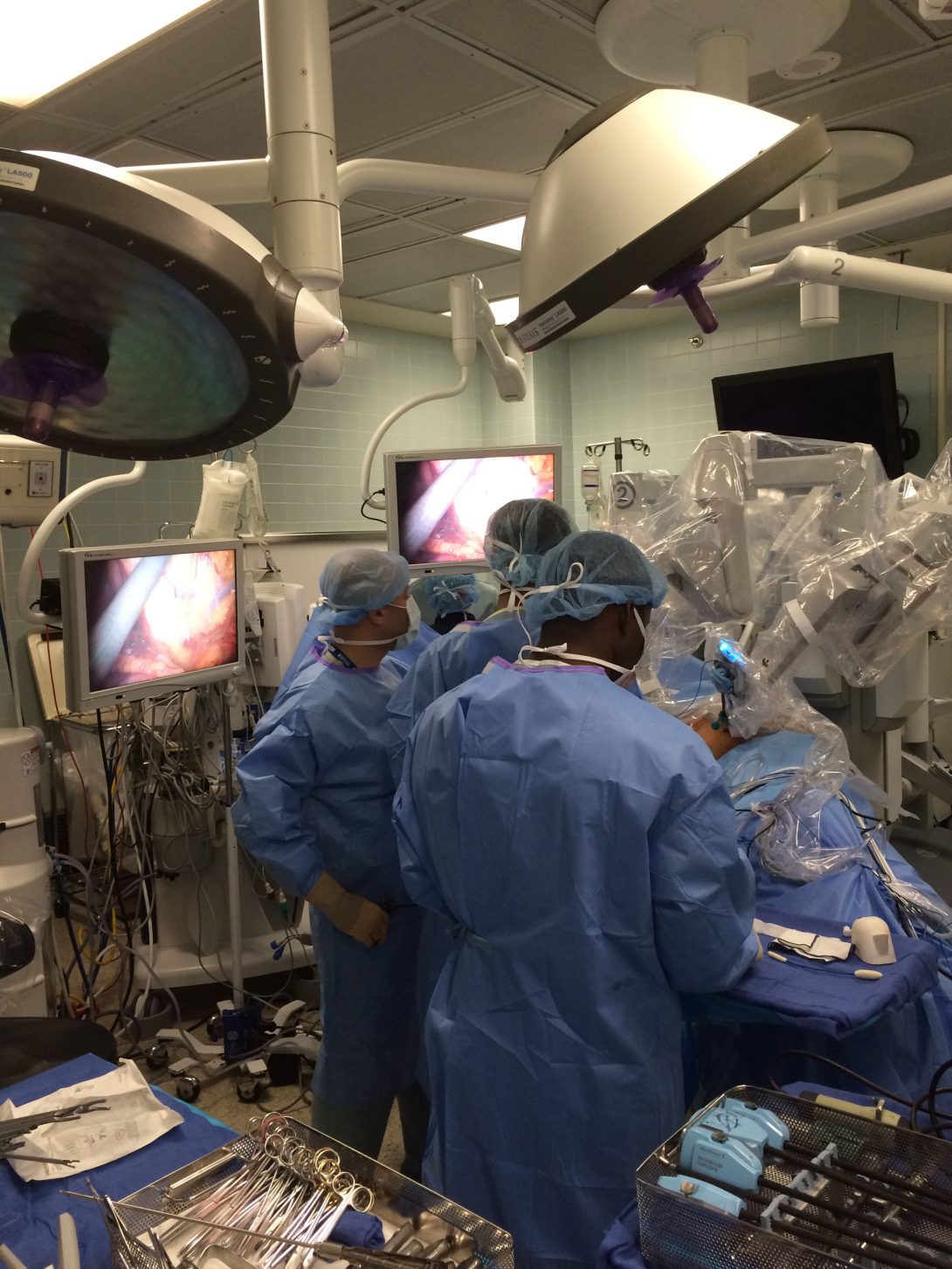
I spent the last couple days of the first week in the Urology rotation solely in the operating room. The sights were awesome and the smells were… less so. I had the opportunity to observe two prostatectomies, one robotic and one “old school.” It was really interesting contrasting the similarities and differences between the two. In both, samples of the lymph nodes surrounding the prostate were removed for future biopsy. This is done to determine if the cancer has spread to the nodes, which raises the severity of the diagnosis. Beyond the precision and less invasive nature of robotic surgery, it also has the advantage of containing the smell of burning flesh during the cauterizing process. Even so, you could still hear the clipping of the scissors through the skin and organs. That was not something I was prepared for.
During an abdominal mass excision, I saw a useful tool that I hadn’t seen utilized before. This was an endoscopic surgical stapler that is used to clamp a piece of tissue, and then it simultaneously staples the edges while cutting the tissue in the middle. It allows the surgeon to separate a piece of tissue while minimizing bleeding.
We also observed a cystoscopy on a patient with urinary incontinence. These are done to determine the specific cause of the patient’s problem. The cause of the problem was quickly determined. While interior organs are supposed to be smooth and supple, they can become muscular and striated. In this case, it is called trabeculation of the bladder lining. This is a result of long term bladder outlet obstruction and will require medication to treat.
Lastly, we were called to a patient’s bedside in the hospital. The patient had sustained an injury to his urethra seventeen years prior, and had been using a suprapubic catheter to collect waste from the bladder. These catheters need to be replaced monthly and should be done by a medical professional. In this case, the patient chose to replace these himself and had been up until a month ago, when he noticed blood during the exchange process and wanted professional help. It took him weeks to get an appointment and by the time he came in, the hole had begun to close. This made it impossible to get another catheter in and the hole had to be dilated, much like the urethra from my previous post. It was incredibly painful for the patient and he had to be given morphine for the pain. While this was a long shot to do at the bedside, it would save the patient a trip to the operating room. Luckily, they were able to get a catheter in and saved the patient an expensive trip.
Discovering Needs (8/3/15-8/5/15)
Sam Dreyer Blog
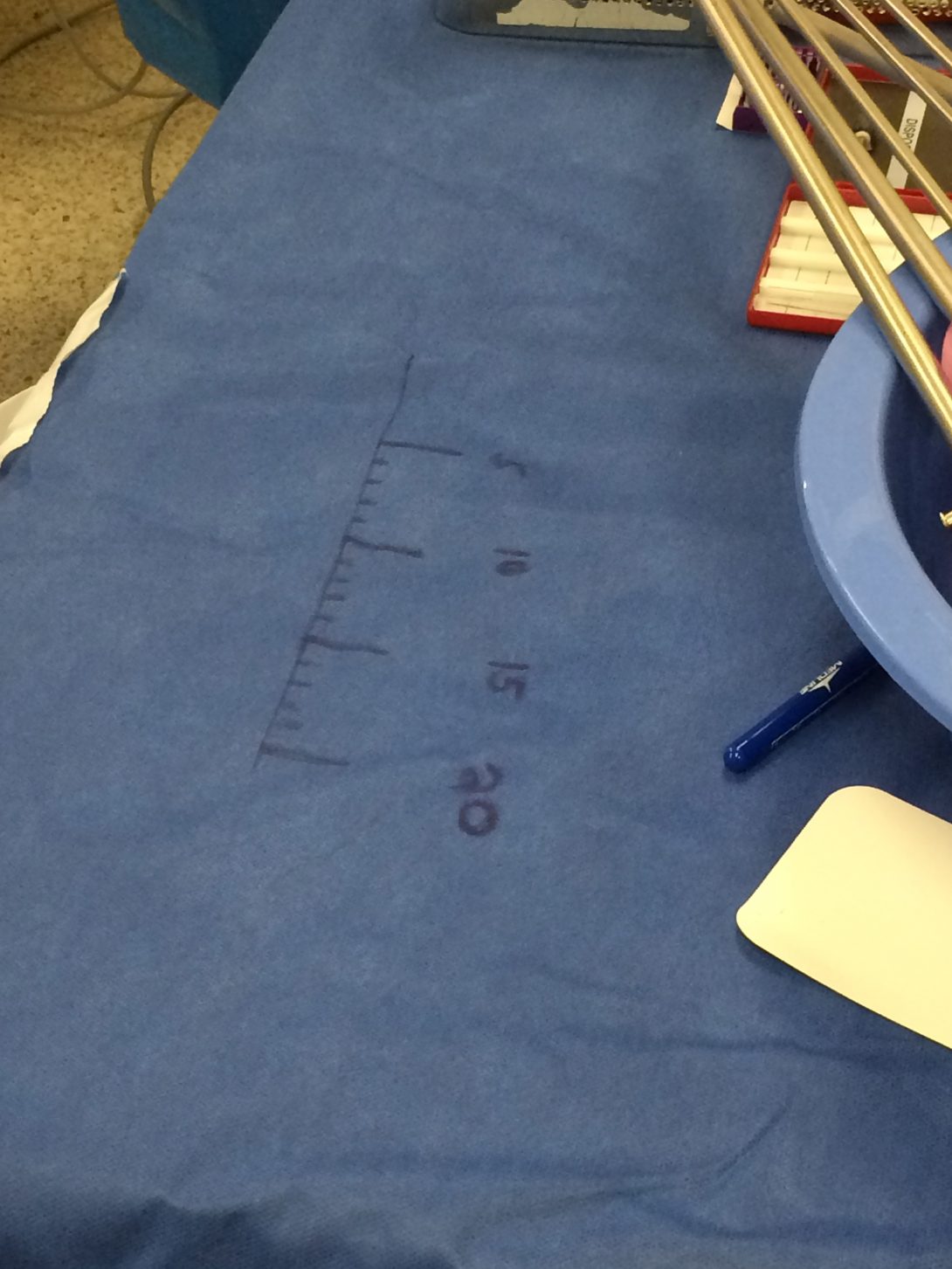
During the first week of a new rotation, it’s almost entirely spent trying to understand everything that is going on and this makes it impossible to look for improvements. After having already been through a rotation, I knew that at the beginning of this week I wanted to focus on looking for those potential improvements.
The first procedure I observed this week was one that I had already seen before, a Greenlight Cystoscopy Transurethral Resection of the Prostate. However, this procedure was slightly different because the patient had a large bladder stone that also needed to be destroyed. While tools exist that can mechanically crunch bladder stones into pieces that are small enough to flush out, these were not available. Instead, a holmium laser was used to break up the bladder stone and the green laser was used to remove the excessive prostate tissue.
The main issue with the addition of the bladder stone process is that the stone and the prostate are destroyed by different wavelengths of light, which requires two completely different lasers in the operating room. While the fiber optic that aims the laser at the tissue is about the size of a strand of pasta, the laser itself is similar to the size of a large bedside table. If both of the lasers could be generated from a single machine, it would cut down on the number of machines in the room and make this type of procedure much easier for the doctor.
Another procedure of note at the beginning of this week was a Robotic Ureteroneocystostomy. This is done because of a stricture of one of the patient’s ureters near the bladder. To fix this, the impeded portion of the ureter needed to be removed and the healthy remaining tissue reattached to the bladder. There were a number of very impressive technologies at work aiding this surgery. First, a dye that is visible with X-ray was injected into the patient at the site of the bladder and ureter. This allowed the doctors to determine the extent of the blockage and how to proceed with the surgery. Next, a cyanine dye called indocyanine green (ICG) is injected into the affected ureter. This allows the doctor controlling the da Vinci machine to select an alternate camera that filters all of the tissue to grayscale, except for the ureter with the dye which shines bright green.
Last week, I noticed almost all of the da Vinci attachments have the ability to cauterize tissue. However, some are labeled as monopolar and some as bipolar even though they might both be very similar tools physically. This is because monopolar tools use a ground on the patient’s skin (typically the leg), for their electrical discharges. Monopolar tools have a larger effect but are not very precise. Bipolar, on the other hand, passes electrical charges between the opposite ends of the instrument. This allows for much more precise cauterizing, but cannot be as powerful.
Lastly, during this surgery I saw a workaround that I almost couldn’t believe (pictured above). During robotic surgeries, precision is key and the doctor will often ask a technician for a suture of a specific length. While a technician’s kit does include a ruler, it is ridiculously small and typically only used as a reference for the technician to draw their own, larger ruler on the sterile cloth!
Last Week in Urology (8/6/15-8/7/15)
Sam Dreyer Blog

It’s the end of the second week in Urology and I can’t believe how fast the time has gone by. Mainly this is because they are in the process of moving the Urology clinic, so all of our time has been spent in the operating room (OR). Time in the OR flies by because even if you’re observing a surgery you’ve already seen, there is usually at least one wrinkle that makes this patient unique and changes something about the procedure.
The first surgery we observed this Thursday was a Urethral Stent Exchange. The plastic stent that had previously been implanted had degraded and needed to be replaced. Metal stents can be in place for up to a year, so the doctors chose to replace it with a metal one. These metal stents look like a tightly coiled spring and curl both at the kidney and bladder ends to keep it in place. This is a fairly straightforward procedure but there was one hiccup that may be easily addressed. The doctors used metal forceps to reposition the stent in the body but because the forceps and stent are both metal, they kept slipping and made it difficult for the doctors to control the stent as much as they would have liked.
Another surgery of note at the end of this week was a typical cystoscopy. The patient came into the clinic complaining of monthly recurring urinary tract infections that had been going on for the last ten months. A quick cystoscopy could narrow down the potential causes and normally would be done under local anesthesia in the clinic. However, with the clinic in the process of moving buildings, there isn’t an established space and this patient had to have the procedure done in the OR with general anesthesia. A urine sample was collected at the very beginning of the procedure to test for interstitial cystitis. Other than that, the procedure was done in a manner of minutes. A quick, yet thorough confirmation that the bladder was normal was all that was needed.
Lastly, I got to observe a staple of Urology, the vasectomy. In this procedure, a small segment of each of the vans deferens are removed. The most interesting thing I learned from this procedure is that the ends of the tubes that connect to the testicles are cauterized because sperm is immunogenetically foreign and can cause chronic pain. During this procedure I also saw another trick used by the surgeons that I found very interesting. Sometimes, while pinching some tissue with a pair of tweezers, they would apply the Bovie to the proximal or middle portion of the tweezers. The electric current would pass through the metal and cauterize the tissue in contact with the tweezers. This was an ingenious method of acquiring more precise cauterization.
Prostate Biopsy (8/10/15-8/12/15)
Sam Dreyer Blog

The most interesting procedure that we had the chance to observe during the beginning of our final week of the program was a prostate biopsy. The patient expressed elevated levels of prostate-specific antigen (PSA) and had difficulty during the prostate exam. These are both indicators of prostate cancer and he had to be brought in for a biopsy to confirm the presence of cancer. The biopsy is done with the assistance of a transrectal ultrasound probe. This probe is inserted anally and used to help the doctors target the prostate and ensure that the samples are taken from a variety of locations throughout the prostate.
This was very interesting from an engineering perspective mainly because of the difficulties with the biopsy instrument. To begin with, the instrument is not intuitive at all. It is a cylinder with a long extrusion that contains the forceps. The scrub nurse must first twist the bottom of the cylinder multiple times to load the spring. While there is a display port indicating if the probe is ready, this is also not clearly marked and caused confusion and delays at the beginning of the procedure.
Next, the doctor inserts the biopsy gun into a port in the ultrasound and maneuvers it until he can see it pressed against the prostate on the ultrasound. After clicking the fire button, the forceps spring out and bite off a portion of tissue. This is done twelve different times at six sites throughout the prostate. After the gun is handed back to the scrub nurse, the nurse must remove this miniscule bit of tissue from the instrument and transfer it into a specimen container. This also proved to be extremely difficult and time consuming.
Due to the size of the tissue sample, it is very difficult for the nurse to tell if an adequate sample has been taken, if at all! This is compounded by the transfer process. The scrub nurse can either swish the tip around in saline within the specimen container and hope it detaches, or they can wipe the tip against a piece of wetted cloth. In both instances, it takes an extremely sharp eye to confirm that the sample has transferred properly and that the biopsy gun can be handed back to the doctor. As you might have inferred, during this entire transfer process, the doctor is sitting there with nothing to do. While a second instrument might help decrease operating time, it would also increase associated costs.
All in all, it seems like a much better biopsy gun would greatly improve the ease and efficiency of this procedure.
Vasectomy Reversal (8/13/15)
Sam Dreyer Blog

For our final procedure in Urology, we had the chance to visit the operating rooms of the clinic located at 900 N. Michigan Ave. With only five operating rooms compared to the nineteen at UI Hospital, it made for a much more relaxed environment. Although it was difficult to fully assess the capabilities of this smaller space in only a day, it didn’t seem that the doctors or nurses lacked anything they needed which was encouraging.
After seeing our first vasectomy last week, it was very interesting to see the same procedure reversed today. The most shocking difference was the increased need to access the vans deferens. With the vasectomy, the vans deferens were pulled through the skin and clipped before being reinserted which kept the incision site very minimal. The reversal, on the other hand, needed incisions so large that they could completely pull the testicles outside of the scrotum. This is done because doctors need to actually find the location of the vasectomy.
After reaching the vasectomy location, a couple of issues need to be assessed. The main concern is the extent of scarring after the surgery. First, the vans deferens are cut on the urethral side of the vasectomy and saline is injected into the tube. If the saline flows easily, that means there are no significant “downstream” blockages. Next, the viability of the testes portion of the vans deferens needs to be assessed. To do so, the epididymis is massaged until it secretes fluid. This fluid is collected onto a slide and examined under a microscope. The doctors then look for the presence of sperm cells on the slide. If they are present, this means that there are no significant “upstream” blockages.
Assuming both of these tests are successful (as they were in our case), the ends of the vans deferens can be connected and the patient is once again able to procreate.
In our last week of this rotation, we spent a lot of time talking to doctors about why they chose to specialize in Urology. The common thread in their answers came back to the use of technology. Urology got its start by using scopes to see inside bladders, something that wasn’t commonly used in other fields. This trend of heavily utilizing technology has remained a staple in Urology as we saw with the utilization of things like the da Vinci robot.
All in all, it was a very enlightening and exciting program that I am very glad I could be a part of. Thanks for reading!
Translators in the Clinic
Sam Dreyer Blog
After being told the next patient wasn’t English-speaking, the resident quickly called for Ivan. A few minutes later, a tablet fixed atop a cart (see picture above) was wheeled into the patient room. Ivan is the department’s on-call option for translations. Once in the room, the tablet-based service functions as an audio call that connects translators to patients and physicians at the point-of-care. A few quick notes on the process can be found below:
-Restricted audio. While the patient was clearly relieved to be able to communicate her symptoms in her native tongue, I circled around the tablet to find a dial pad display on the screen. While the service is no doubt effective, one must wonder if a patient would feel even more comfortable if the translator were able to “facetime” in providing visual feedback to create a more organic interaction.
– Surprising quality in communication. Despite the fact that all patient-provider interaction was funneled through Ivan, the encounter may have been one of the clearest I have observed to date. While there were some issues with audibility at the beginning, knowing that everything he said had to be translated almost seemed to force the physician to communicate as clearly and succinctly as possible—a skill that could no doubt benefit patients who don’t need a translator as well.
-Limited interaction. While the content of the conversation was clear, it was admittedly asymmetrical. The physician would direct himself towards the patient when speaking, while the patient would direct herself at the translator (functionally, at the table on wheels) while speaking. The difference in attention no doubt capped the comfort with which patient-physician interaction occurred.
It was equally interesting to see how language can affect patient autonomy. As the translator spoke, I’m not quiet sure she realized that the individual she was speaking to was actually the patient’s family member, and not the patient herself. Healthcare technology is often seen through the lens of diagnostics, but Ivan is a great example of how technology affects care delivery, rather than any actual treatment.
Wali Badar Heading link
I’m looking forward to this summer’s clinical immersion internship. Stay tuned to find out about my radiology and urology rotations!
Wali Badar Blog Heading link
-
Wali Badar Blog
Week One: First Few Days
Wali Badar Blog

The first few days of the Clinical Immersion internship program have been very fulfilling. Radiology has been even more exciting than I anticipated. As soon as we got to the Interventional Radiology (IR) operation room (OR) we were greeted by Dr. Bui. He told us to go get scrubs on. As me and Ossama went to get our scrubs on we noticed that there were a lot of monitors. In fact, each doctor was in front of three monitors. There was one regular monitor and the other two monitors were vertically placed and were primarily being used to view x-rays. There was clearly emphasis on technology in this department.
The first procedure we witnessed was a kidney biopsy. We noticed that first the doctor would use an ultrasound to find a tumor of interest. When the doctor was dealing with soft tissue and the abdomen area he would utilize a ultrasound system. For me and Ossama it was very hard to see what the doctor was seeing. We were eventually able to see the tumor that aiming for. Once the doctor found the tumor mass, he used a biopsy gun to obtain the tissue sample. The biopsy gun mechanism is seen below:
The next procedure we say was an administration of a chemotherapeutic drug known as doxorubicin. The doctor used a lipid mixture as well as the concentrated dox to make a drug emulsification mixture. The lipid material was used so that the cells could take up the lipid/dox mixture since the favorable polarity. The drugs were mixed using a simple one way valve with two ports, one for each syringe. The drug was injected using a catheter. We were not able to go in the OR for this procedure because there was X-Rays being used. In order to be in the same room as X-Rays, a lead protection apron must be used.
My initial impression is that interventional radiologists are truly talented individual. From one day I was able to see that these doctors are experts on a vast array of treatments. This is made possible largely by the powerful ability of imaging modalities. Each imaging duality is used in each respective circumstance and procedure. At this point there is no specific need that is noticed but I anticipate that as we move forward a need will surface. The doctors seem to be very fond of us bioengineering students. They frequently encourage us by saying, “you’ll invent the next so and so, you just don’t know it yet”. The vast array of technologies being used such as the biopsy gun is a testament to this statement.
Week One: End of the Week
Wali Badar Blog

We have started to see more eventful procedures. The main procedure we are starting to see is known as ablations. Ablations procedures that remove a cancerous tumor mass by several means such as heating or chemical means. The two procedures that we’ve seen is ethanol ablation and radio frequency ablation. Ethanol ablation is less eventful and requires injection of ethanol to the tumor. RF ablation uses AC currents to generate heat to essentially cook the tumor. The picture seen above shows the RF ablation device inside the patient. He is receiving RF ablation to treat a tumor in his liver. The device is seen below:
This is the ablation device is inserted through a catheter system to the site of the tumor. Upon reaching the tumor, it has talon that are released. This is seen below:
Saline is released from the talons. This allows for equal conduction and heating of the tumor. The temperature is monitored using the following:
The machine maintains a temperature of 150 celsius. This is done for 8 minutes to adequately cook the tumor. The device is held in the liver as seen in the picture. The device is free to move externally but is anchored by the talons inside and so it will not move in the liver. As the device is pulled out it is very hot. We saw that as it was pulled out it burned the patients skin. This is definitely a limitation of the device, and I feel it can be improved. A smarter design must be used to reduce the burning the patients feel.
Second Week: Beginning of the Week
Wali Badar Blog
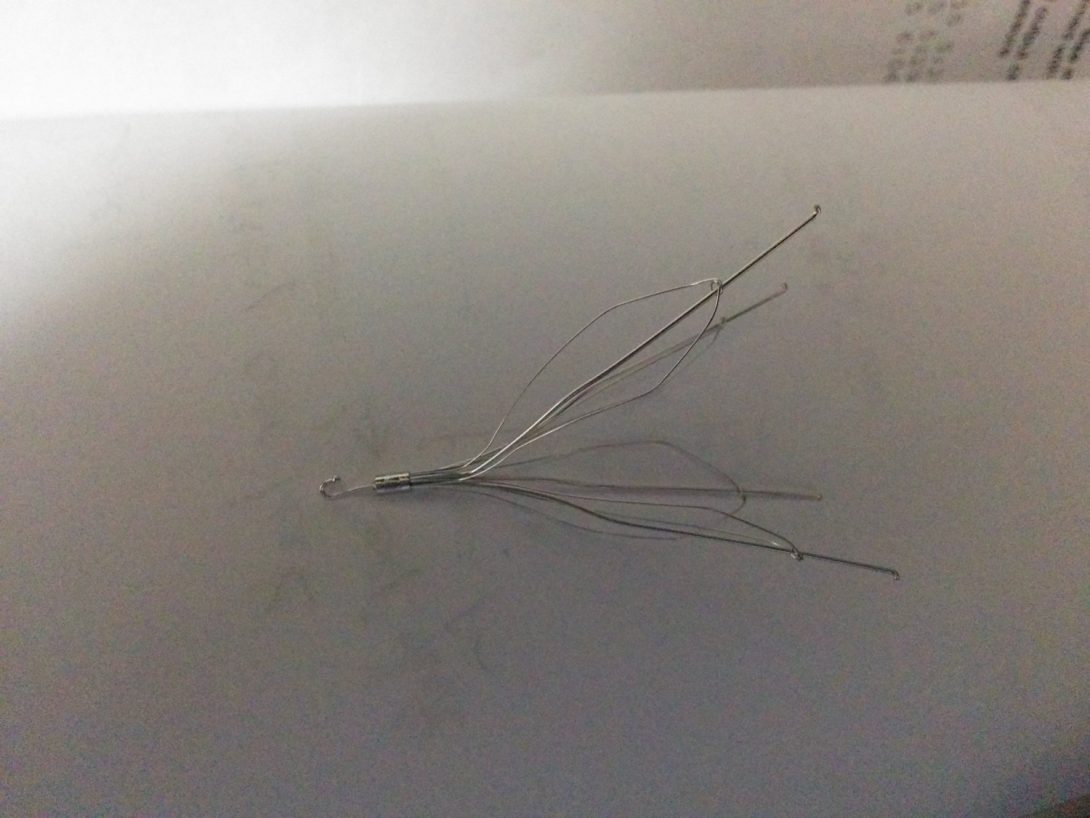
To start off the week we saw a inferior vena cava filter removal. This filter is seen above. The process is analogous to arcade claw machine. A lasso is fed through the catheter and is used to tie base of the filter. Then the flexible filter is fed through a sheath and the sheath is guided out of the jugular vein with the filter. While the doctor is doing this he is referring constantly to his live x-ray image of the IVC. The x-ray looks like the following:
The doctor must tighten his lasso when he sees that it is on top of the filter. This doesn’t always lead to proper hooking and instead often results in miss-hooks. A 2-D visualization of the lasso device and the filter does not adequately represent what the doctor needs to see to effectively hook on to the filter. There is a lot of trial and error that is necessary in order to hook on to the filter. This is not usually a problem but sometimes the filter can be pushed into the renal vein during the hooking trial and error process. This can be problematic. A more effective visualization technique will benefit the doctors in the filter removal process.
We have also begun to see several embolization procedures. This a process where an embolus is passed to a tumor to block of the tumors blood supply. This does effectively kill the tumor but it does take time, usually months. We have seen the doctors inject EMBOSPHERES as their choice of embolus. They are seen below:
You can see the tiny microspheres that create the embolus. They are roughly 400 microns in diameter. This is close to 6o times the diameter of the a red blood cell. The massive spheres can clog up the artery leading to the tumor. We have seen this procedure performed in the kidney, liver, and uterine. Uterine fybroid embolism has been the most interesting embolism procedure. This is because there were two different vessels supplying blood to the tumor and so two embolisms are made. To test that the embolisms have formed, the doctors inject contrast to the artery. If the is an impedance in flow, the embolism has successfully been created.
Second week: end of the week
Wali Badar Blog

We saw three interesting procedures this week. The first procedure we saw was transjugular intrahepatic portal shunt (tips). This procedure is used to treat hepatic Hypertension. Due to cirrhosis of the liver there is a back up blood in the hepatic artery. This causes compromised function in the liver. It is by far the longest procedure we’ve seen. It took over two hours to perform the procedure. There was a great deal of time spent trying to find the hepatic vein. The visualization abilities of a x-ray system are limited. It is hard to see the vein without a three dimensional representation of the vascular system. Also we saw them using a balloon angioplasty system to burrow through the liver tissue. A pressure device was used to control the pressure in the balloon. Also the doctors were using a pressure transducer to figure out the pressure gradient between the two veins they were shunting. The transducer was very similar to the transducer we had seen in instrumentation class. The other procedure we saw was a bone biopsy. We saw the doctor drill through the sacrum. The patient didn’t feel any pain. The picture of this is seen above.
Week 3: First Few Days
Wali Badar Blog
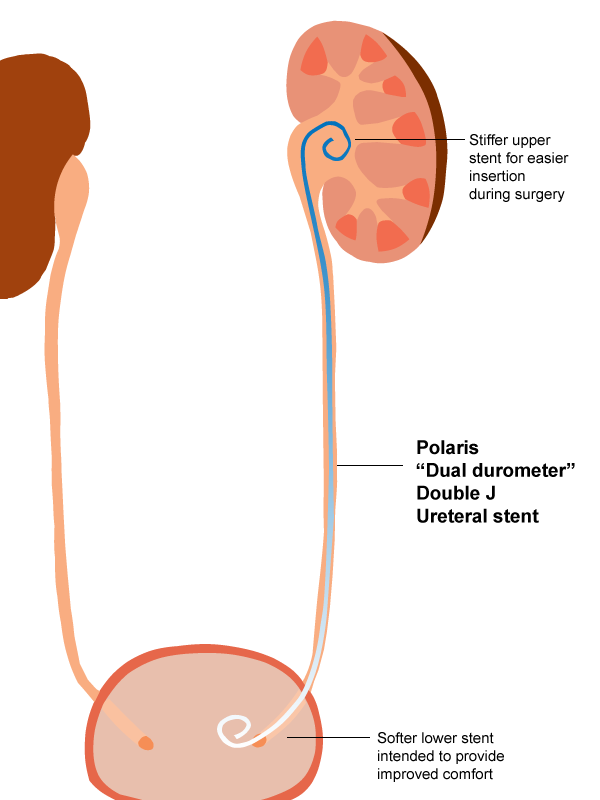
This week has been fairly eventful thus far. To begin with, we saw our first pediatric patient. She was in for a ureteral stent placement. This is for patients who have a blockage in their ureter. This results in a pooling of urine in the kidneys because there is a urine back up. The stent collects the urine in the kidney and creates a pathway for flow to the bladder. There was considerable tension that was apparent before the procedure. The parents were very reluctant to leave their daughter for the procedure. Next, when the anesthesiologist came there was some difficulty administering the analgesics to the patient. In order to properly place the non-rebreather mask on the patient, the doctors had to flip over the girl. After the surgery was successful, we talked to Dr. Ray regarding the procedure. He told us that it was a fairly stressful procedure for the following reasons: its very hard to see the ureteral stent with the fluoroscopy X-Ray system. This is definitely something that needs to be improved because the hard the stent is to see, the more X-Ray radiation the doctors have to administer to the child to try to visualize the stent. Perhaps there is some coating that can be utilized to more effectively see the stent system.
We have also seen a large number of biopsy procedures. This has been the most common procedure that radiologists perform. Image guided biopsies range in difficulty. For example a kidney biopsy can be pretty simple and can be completed by simply using ultrasound and a biopsy gun. However, there is one drawback of these biopsy procedures. The procedures require a dual needle gun. This needle has to cut through the tissue and cut a core of tissue. the problem with this that the gun makes a very loud sound as it cuts the core. This is a very intimidating and frightening sound. I was definitely startled when I first heard. The mechanism must be improved to reduce this noise.
Week 3: End of the Week
Wali Badar Blog
IR as we know is heavily dependent on technology. Since technology is being used to visualize and treat patients during procedures, there are ways to further optimize these technologies. Problems with visualization added to the difficulty of carrying out the procedures. Interventional radiologists use imaging techniques to assist them in the minimally invasive treatments of their patients. The minimally invasive aspect falls to the fact that the success of these procedures relies heavily on the quality of images obtained. A more radiopaque material or a three dimensional x-ray may be a potential step toward better visualization. The more x-rays used, result in more harm to the patient.
Other problems perceived include that of biocompatibility, which can be improved by adding a medicinal coating for scar tissue prevention. Scar tissue makes it very difficult for the intended device to function properly. In addition to that, scar tissue makes the removal of the device very difficult. Some devices, such as chest ports, remain in patients for years. Also, the microspheres that are used to administer chemotherapy can be improved. Only a few drugs are compatible with the microspheres. A better microsphere design will greatly improve the breadth of chemotherapy that is administered.
Thank you to Dr. Bui and the entire IR department for teaching us so much and allowing us this opportunity. The work these individuals do on a daily basis is truly amazing and being able to think innovatively while in this environment is an experience and a blessing.
Week 4: First Few Days
Wali Badar Blog

The beginning of this week has been a transitioning period for radiology to urology. After spending three weeks in radiology, I became accustomed to very short procedures. Spending time in the Urology IR has given me a true understanding of how lengthy and meticulous surgeries are. The first procedure we saw was a cyto transurethral resection prostate. This surgery was performed to remove lobes on the patients prostrate. The procedure required and endoscope and what is known as a green light laser. The urethra was dilated in order to place the endoscope into the urinary tract. Once this was placed, the green light laser therapy was used to effectively vaporize tissues. It was very cool to see the tissue literally disintegrate in front of our eyes. This procedure was very extensive and eventually both lobes were removed. The neat thing about this procedure is that the tissue is vaporized and so there is no bleeding. It was really interesting to see how extensive some surgeries can be. During the procedure we had to wear special eyewear because of the nature of the lasers.
I am definitely having to adjust to this new rotation. The amount of standing on your feet is far more substantial than radiology. I am looking forward to seeing more of the Robotic procedures.
Week 4: End of the Week
Wali Badar Blog
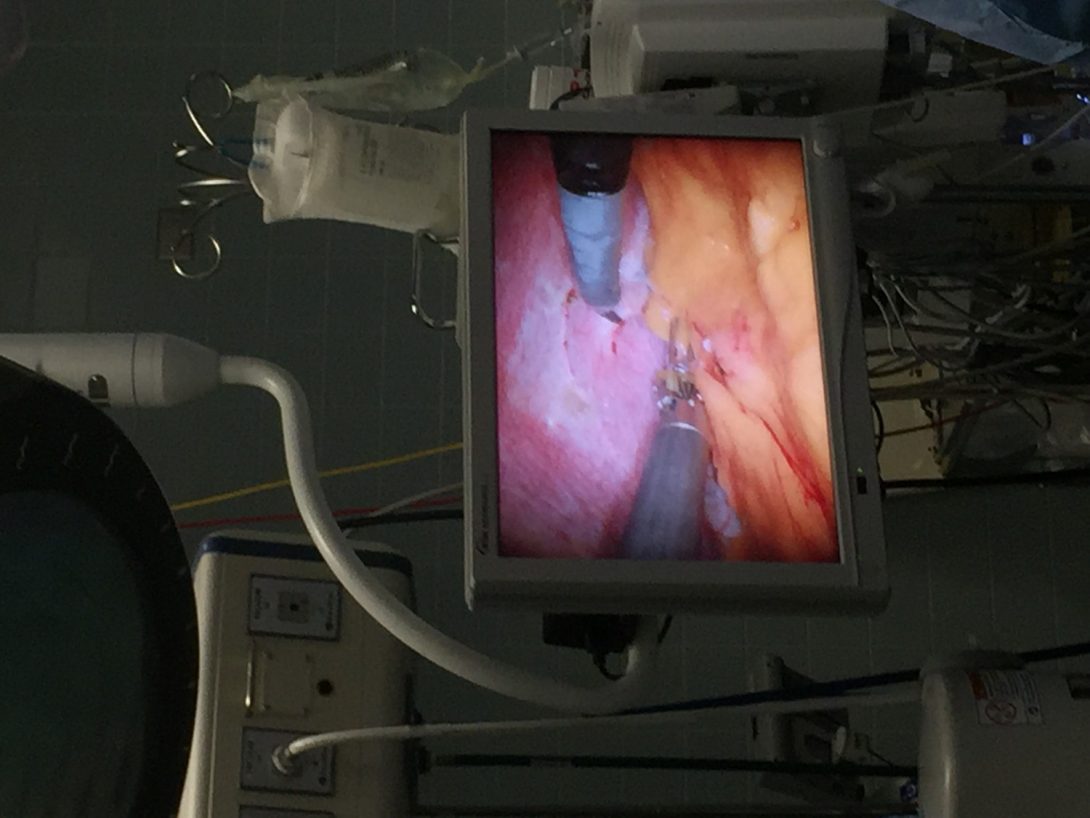
The end of this week has been quite eventful. We got to see an endoscopic procedure with the assistance of the di vinci robot. This is seen below:
The procedure was intended to remove a tumor that was growing on the kidney. This was the longest procedure we had seen thus far. Roughly two hours were spent gaining access to the kidney. In order to do this, the surgeons had to create three incisions in the patients back. Then the robotic arms were placed into the individual. The surgeon operating the robot is seen below
The surgeon has fairly complex controls. He has two joysticks which control the movement of the arms and three pedals. One pedal activates the camera, the other pedal activates one arm while the final pedal activates the other arm. The doctor is using a three dimensional view to guide his arms. The doctor can also see the tumors before he begins to cut into the lesion with the help of ultrasound. The doctors struggled to remove the tissue to access the kidneys. A better approach is necessary to apply tension to the tissues.
Week Five: First Few Days
Wali Badar Blog
More and more needs have become apparent during this second week in Urology. After completing my radiology rotation I believed that it was very technology heavy. However after this rotation, it is clear that there is far more technology used in this rotation. There is a very delicate nature associated with these procedures. For example most of the procedures that deal with the urethra require very meticulous work. A simple stent cannot be placed to counteract the closure of the urethra. Instead we saw a robotic procedure that was performed to mobilize the bladder and connect to the non-occluded part of the urethra. This seemingly simple procedure ended up needing heavy robotic machinery. The doctor informed us that a stent cannot be used to hold the occlusion open because it will tear the urethra. While they were performing the surgery, we noticed the tech was using markings on her table to measure her tools. This does not seem like a very efficient way to measure wire and tool length. An improvement is necessary to improve the archaic practices of surgeons.
Week 5: End of the Week
Wali Badar Blog

We saw an interesting procedures towards the end of this week. The interesting procedure we saw was a cysto transurethral prostate resection. We have seen this procedure before but what we had not seen previously was beginning of the procedure. In order to remove the bladder stones the doctors used red light lasers. They used this technology to obliterate the kidney stones. In a previous blog I described the green laser light that was used to destroy the tissue on the prostrate lobes. A different color of light was necessary because the stones had an entirely different composition. Therefore a different wavelength of light was necessary. In order to both these procedures, the green and red light laser, two large machines were necessary. This required personnel and space for operation. The doctors suggested that one machine handling both wavelengths would be ideal. This is a potential improvement that can potentially help improve the efficiency of the procedures.
Week 6: First Few Days
Wali Badar Blog

One of the problems perceived include that of biocompatibility, which can be improved by adding a medicinal coating for scar tissue prevention. Scar tissue makes it very difficult for the intended device to function properly. In addition to that, scar tissue makes the removal of the device very difficult. The medicinal coating can also be utilized to help patient deal with the painful process of having an internal stent. There is an issue with placing stents because they often result in some degree of rejection resulting usually in excessive inflammation. Cytoscopic procedures such as the one seen below are used to place the stent into the patient. We saw particularly the surgeons struggle to remove a metallic stent due to its texture and excess scar tissue.
Bioresorbability is another aspect in which improvements, such as the creation of resorbable stents, can be made. A patient receiving removal of a stent removal would benefit if this stent was resorbable. The removal process is fairly invasive and forgoing the process would be ideal.
Week 6: The End
Wali Badar Blog

This rotation has come to an end and I can honestly say that I have learned a great deal. Me and Sam recently visited Dr. Niederberger’s clinic located at 900 N Michigan Avenue. This was a completely different realm in comparison to UIC OR. Upon entering the building we amazed at the types of procedures that were scheduled at this location. Most of the procedures pertained to male and female fertility or cosmetics. These high end procedures were consistent with the high end location of the surgery center. The surgery we was was a non-robotic reverse vasectomy. An interesting fact that Dr. Kathrins told us was that the procedure will take 3 hours while the vasectomy itself only took 45 minutes. A picture of a vasectomy is seen below:
One of the problem that is not apparent in this picture but nonetheless exists is the microscope. The microscope is used to analyze the texture of the tissue the doctors are operating on. A problem with this device is that the handles for adjustment and focusing of the lens is above the surgeons head. This is very inconvenient for the surgeon and simply kills time. The longer the surgeon takes to adjust the microscope the higher the chance of infection and the procedure going astray. This is something that needs to be addressed in order to reduce the time spent on focusing the microscope. A more user friendly automated microscope is necessary. This is something that is of interest to me.
Christine Joseph Heading link

Gastroenterology/
Hepatology and
Hematology/Oncology & Radiation Oncology
Christine Joseph Blog Heading link
-
Christine Joseph Blog
WEEK 1A: The Virtue of Patients
Christine Joseph Blog

It’s our first week in the Gastroenterology/Hepatology rotation, and we are spending our time in the Outpatient Clinic. We have met so many people, all extremely diverse and interesting. Everyone does things differently; each doctor, each patient. That’s why it is so hard to standardize this extremely subjective process.
I spent some time in the waiting room, feeling the palpable frustration. I talked to some patients who disliked other doctors for not listening, not explaining, not apologizing. On the first day of our rotation I got a piece of advice passed down from Nurse Nedra Chaney: “We’re here to alleviate the fear of the unknown – that’s in every patient – build trust, and then treat the patient.” That first step is incredibly important, it sets the foundation for good trust and good treatment. Patients, for the most part, want to understand. They want to take ownership of their own healthcare. If you’ll check Namrata’s blog, you’ll see a homemade chart one of our patients made for herself, detailing the dosage and time to take each of the medications. But this isn’t always the case.
What remains constant is that they want to be listened to, they want to have their questions answered, and they want to be treated with respect.
We observed Doctor Stewart who tailors her approach to each individual patient. Her fellows are the ones who type everything up during the consultation, while she stands, sits, and engages. I watched her nod for a good 30 seconds at a patient to impress upon him the importance of cutting out fatty root vegetables from his diet. I thought it was a bit overdone, but at the end of that half minute, the patient quietly asked “Really?”, to which the doctor responded, “Yes!” with another 30-second nod for good measure. She brings up patients’ holiday plans and families and hopes for the future when they are feeling burdened with their diagnoses. She knows what questions to ask. She is the perfect mix of severe and jocular all at the same time.
We did rounds with Doctor Shastri, who excels in explanations. This takes time, but serves as an excellent teaching experience for the fellows and bioengineering students walking with him.
Doctor Nannegari is fantastic at establishing a rapport with the patient, especially during her direct examinations. She is cheery and personable, greeting everyone in the clinic, uniformly. She is focused on getting a thorough and efficient examination, but is also focused on the screen, typing as the patient speaks. I notice the patient’s voice tapers away, until the doctor looks back to his face.
Dr. Nannegari’s caring and explanatory demeanor didn’t seem to fit with her propensity to turn away from the patients. It’s then that I noticed that a lot of it had to do with the layout changes between rooms. Two of the four of Dr. Nannegari’s assigned rooms were set up so the computer screen faced the patient. This means that if the doctor wants to document on the computer (as opposed to those doctors that want to write on paper, or delegate to their fellows), she has no choice but to turn away from the patient.
Doctor Carroll seems too clinical behind the walls of the conference room, but I know it is an important part of the job – balancing compassion with equanimity.
The doctor looks at a patient. The doctor touches the patient.
That makes a big difference.
Often, as bioengineers, we focus on the mechanics of an issue. We look at the machines, not the man. But in Medicine, it is crucial to consider the importance of touch, of comfort.
It is easy to think that the jobs of these doctors can be automated: A simple list of yes or no questions that branch towards the final diagnosis, the final prescription. Surely even the subtlest of symptoms can be coded for.
But people lie.
And people are somehow less willing to lie to a doctor.
People have motives. It’s important for each patient to be their own advocate, as doctors have motives, as well. But the vast majority of doctors are there to help, and need to know all of the information in order to make the right decision – especially when the difference between the right and the wrong choice is subtle and dangerous to confuse. In this regard, there is a certain respect patients give the attending physician, probably due to the deferment and respect we all automatically give the doctors. Even the fellows, extremely accomplished in their own right, defer to the attending physician.
We had a consult with a man diagnosed a few years ago with liver disease, but strangely unscarred by cirrhosis. He took up alcohol as a coping mechanism after his initial diagnosis, and we watched as Doctor Stewart skillfully noticed the holes in the man’s timeline of when he stopped drinking. The man also said he’d stopped using cocaine many years ago, but after the struggle in determining when he stopped drinking, I’m not sure the doctor felt compelled to follow through with ascertaining that. I noticed he had an exceptionally long pinky fingernail, which is tempting to speculate on.
But no matter his health choices, his liver was thriving.
I guess he was just lucky.
There was a woman who was so bluntly honest and self aware and, frankly, hilarious. She KNEW she would never be able to drink the gallon of briny fluid required for the colonoscopy cleanse. She claimed that ALL she ate were meat and fruits, and she ONLY drank a single glass of water a day. When told to drink only clear liquids in preparation for her colonoscopy, she asked in loud earnest “if a tiny, little, piece of chicken somehow made it’s way into my broth, would that be okay to eat?”, leaving Namrata and I doubled over in laughter, and Doctor Nannegari to respond with a resounding “NO!”
That patient was the one who suggested we work as bioengineers to eliminate invasive colonoscopies altogether. We noticed that even though the electrolyte liquid is needed to properly flush the system, overall liquid imbibed is further compounded by the enormous quantities of liquid laxative the patients need to take. Here emerges a need for a simple laxative pill that can properly dissolve and disseminate with less water – something currently available, but left uncovered by most insurance and at exorbitant cost.
I noticed something equally striking in the Hepatology examination rooms. The general format of the examination is a consult in the chairs, an examination on the table, and a return to the chairs to explain the situation and address the patient’s concerns. On the wall is a chart meant to explain the progression of Hepatitis and the resultant cirrhosis. But this chart is behind the chairs, meaning that whenever a physician is walking the patient through, the patient must crane their neck. It’s a little thing, but little things become big things when compounded time after time.
It was here that I encountered a sweet woman, brought to tears by her diagnosis. Though her disease was still in the early stages, the worry about her future was very affecting. The pharmacist walked the patient through her new drug regimen. She explained that no herbal pills could be taken at the same time as prescription pills, and that changes would need to be made in her culture and lifestyle to supplement the pharmacist’s prescription.
We saw patients that were stoic and patients that were emotional. We met people who had lived with viral infections for the vast majority of their lives – only finding out now.
We met a convict, and he was just the nicest man. They brought him in with rigid handcuffs that were chained around his waist. His feet were chained, as well. When gesturing toward the painful area in his midsection, he struggled to move his fingers enough to point. Doctor Shastri helped him out, and was not afraid. It was really jarring to learn he was incarcerated for carrying heroin while other patients were candidly admitting to us just how much of the same drug they had done in the past. Perhaps he was a dealer, perhaps his use was more severe, but perhaps he was the only one they caught.
Unlucky.
We met a patient who had been removed from the transplant list due to his noncompliance in taking his medications.
These kinds of tough choices might better be made by a machine.
But where would be the comfort? And could we be sure that patients believed what they heard?
I’ll go into detail about some of the technologies and processes we’ve observed in my next post about Week 1 of this program. There are a lot of organizational and systematic gripes that become clear after a few days working in this small outpatient clinic. But what really makes up the heart of this clinic is the people who come to it, so I figured that would be a good (long!) subject entry to start with.
WEEK 1B: Organizational Systems and Operating Machines
Christine Joseph Blog
I noticed on the very first day that none of the doctors had the usual desk accoutrements – no pictures of family, no silly pens, no notes to self. We quickly understood that here is a severe lack of space in the work areas. This manifests itself, too, in the number of computers available to the doctors. No one has their own workspace, everything is communal, and first-come-first-serve. This is why some doctors insist on finishing their computer orders before they leave the examination room. There’s a bit of learned helplessness, here.
Doctors can check their list of scheduled patients at any time, but every morning, the Medical assistants put up a nearly finalized list on a bulletin board. They highlight the patients who have been called in, and have already been through a general examination. The priority goes to patients who arrive on time. Many are late, many are no-shows.
We had a patient in who had to wait, burdened with a painful gastric condition, for three months for an available appointment spot. Dr. Shastri talked to us about how quickly these spots get filled up, but given the high rate of patents not showing up, it’s unfortunate to think that those who play by the rules of the system get punished.
On Monday, we used an ultrasound machine to examine the man’s gallbladder. Dr. Carroll taught us how to decipher the images on the monitor, and showed us the different imaging modalities. I got the chance to freeze the frame and develop the image. We were even able to listen to the flow of blood through his descending aorta using the Doppler radar, which Namrata correlated with the man’s pulse.
Dr. Carroll also gave us the chance to work on creating a patient’s nutritional regimen. Namrata and I spent a morning working through formulas based on the patient’s health records and severity of illness. Dr. Carroll walked us through each variable, and explained why the numbers we had made sense. We talked about vitamin and mineral needs, and he gave us an article to read before our late clinic on Monday.
Even knowing to do so much, there is sometimes no conclusion to be drawn.
The most interesting procedure we learned about was a fecal transplant – using the unique properties of gut flora to address issues in the recipient system. There now exists an FDA-run repository for generic fecal samples. As the coming entries will show, regulation is a huge part of what doctors must deal with.
We learned about a swallowable pill that transmits a signal to a receptor worn around the waist.
We met Dr. Boulay on Thursday, and his style of working through problems aloud and using colloquial terms with the patients reminded me of Sherlock Holmes. He was another great teacher; respectful, understanding, and candid in his storytelling.
This is how all of the doctors we’ve seen sit:
We met a patient from a mental institution. We met a patient suffering from depression. We met patients who could not speak English. We were also able to see the interpreters in action – through a tablet screen.
There are more variables to weigh when it comes to patients more variable.
Dr. Velpari thinks there is a trend towards telemedicine, which gives me a lot to think about. I don’t know if it would be easier to lie to a machine – maybe the incentive to lie would even go down. But the prevalence of algorithms, and the need for cheaper alternatives and efficient support is a bit damning. The online records are a bit tricky to learn to use, but invaluable from that point.
Perhaps the way to move forward is in making these algorithms accessible to laymen. As it stands now, doctors are needed to separate the signal from the noise.
WEEK 2A: The Tools of the Trade
Christine Joseph Blog

The first machine we used was actually last week in the Outpatient Clinic. Here’s a picture of the ultrasound machine, used to identify fibrility, and other unusual internal organ characteristics. Dr. Carrol showed us how it could also illustrate the flow of blood in different directions through arteries and veins, and enabled the doppler functionality to allow us to correspond the sound to the patient’s pulse.
We’ve found that, especially in a university hospital, diagrams are the norm! Being able to draw and redraw ensures doctors have the familiarity with the anatomy – crucially important when that anatomy is unusual in any way.
Fluoroscopy is a process where a continuous series of X-rays are used to illuminate a contrast agent in the GI tract. We observed Dr. Shastri walk Dr. Soudagar through a procedure to remove a stent trapped in the bile duct, and talked with Dr. Boulay about another ERCP procedure he performed.
Dr. Boulay showed us the stent he had placed to facilitate drainage, and explained how he had deliberately placed it incorrectly, so the device would fall out and be passed in a few days time.
It’s especially interesting when the most effective solution is an imperfect one.
Namrata and I were able to follow a specific scope, like we’ve followed specific patients through their routine. We watched the endoscopy, watched the preliminary disinfection, walked behind the bundled scope to the cleaning room, and talked to the lab technician about the process of testing the scopes for kinks, tears, and aberrations. An air pressure failsafe is used to test for holes, as submerging a broken scope in water will render it irreparable.
We were taken through the secondary cleaning process, using a thin brush to travel from port to port, cleaning the tubes within. Each scope is equipped with passages for air, water irrigation, thin wire tools (biopsy forceps, a net for retrial of stuck objects, clamps galore!).
There is a specific attachment for each scope, dependent on function and french size. The process includes through another round of attachment and scanning to make sure the correct scope and cleaning port has been used. This is important to ensure that the system remains closed, and no damage will come to the scopes.
The machine shuts tight and begins its washing cycle. The acid wash comes from the cabinet below the unit, and the device is cycled through different cleaning regimens.
Once sterilized, they go into a closet to await their next use. The wire attachments that are sent through the tubing are also sterilized, and sent to be decontaminated and sealed for reuse in a room downstairs.
The connectivity of the system as a whole is a bit lacking. The barcodes that must be scanned are stored in the individual CPUs of each washer, and some machines are not properly synced to the others.
These scopes come in different sizes, and the same basic design is used for the colonoscopes, the endoscopes, the pediatric scopes, and the nasal scopes. It seems self-evident, but the use of these scopes to peer into the body is a relatively recent development – without a useful optic method, only surgery could allow a look inside. Dr. Halline walked us through the timeline of scope development, explaining that the first scopes were rigid tubes with fiber optic cables running to the top, which were then viewed with a lens that could be modified to accommodate two viewers (halving the light input, but allowing for better instruction). The video advancements in even the past 20 years are wildly impressive.
Dr. Sleesman guided us through the process of labeling the checkpoints in the colonoscope’s journey. Pictures are taken at each “landmark”: the appendix, the small bowel, the ascending and descending colon, etc. This is a matter of patient edification, completeness in the procedure, as well as ensuring proper liability and protection. Dr. Halline spoke to us about transillumination – using the light from the end of a scope that glows through the skin and organs to identify the location of the scope. This process is difficult in heavier patients, and internal organs are not homogeneously close to the surface of the body. Here emerges a desire for a way to note the progress of the scope, that can be used in a heterogeneous population and still provide a map of the process in a physiologically relevant way.
Some other interesting devices and solutions:
Cords left in a pile/Cords tied up
Organization in the sterile storage room
Pre-procedure organization
Tape printed with the name of common sedatives, to label syringes in the procedure rooms
My next post will be more about the patients, the doctors, the procedures, and the system, as a whole! It will likely include a no-holds-barred, brutally candid, tell-all from Dr. Sleesman!
Just kidding, you can breathe again, Dr. Sleesman.
We’ve really loved our time here, and so much of it is contingent on the people who guide us, teach us, and challenge us. My next post will be a testament to their support, honesty, and skill – seen through the lens of their procedures, their successes, their strides forward, and the vexing difficulties that emerge from the scope of their work.
WEEK 2B: Closed Curtains
Christine Joseph Blog

We’ve seen a lot of procedures in our time in the GI Lab! The obvious ones are the colonoscopies and endoscopies, both of which I’ve mentioned in the past entries. A new observation this week was a PEG – where a feeding tube is threaded through the stomach wall and out through the skin. This surgery is like watching a spider weaving silk, or watching an ethereal woman play a harp. Every movement is deliberate, and precise. If a mistake is made, no one panics, but works calmly and smoothly to address it. We observed the transillumination of the tip of the probe inside the woman’s stomach, and watched as the doctors carefully marked the location for piercing with the tip of the tube. The spell then breaks as we watch the doctor pull at the tether with all of his might, stretching the skin and using force to guide the tube to its emergence. A guide wire is used to position the tube, and after the surgery, the loosely sealed incision is left to heal.
When the doctors perform a dilation, the primary remedy comes from a series of hard foam cones, slid down the throat in an ascending order. There is a push towards balloon dilations, where water will be used to stretch the walls of the balloon and the walls of the constriction.
Biopsies are painful to watch – the claw is magnified, and the site of extraction bleeds quite a bit. Dr. Sleesman reassures us that the nerves in the intestines don’t feel pain like we think they do.
We saw a few fluoroscopy procedures designed to remove blockages (usually from the bioengineered materials like stents moving awry within the body). These procedures are perhaps the most high-tech, with laproscopically scaled tools and constant imaging.
Because the University of Illinois Hospital is a teaching hospital, the organization of the overall system is a bit different than that of a traditional hospital or private practice. The fellows, residents, and medical students are funneled through the system, learning, teaching, and experiencing, all at the same time.
The Physician Quality Reporting System (PQRS) is a program designed to hold doctors accountable for the quality of their care. But even on a smaller scale, patients, themselves, have the capability to simply post on the internet their thoughts, feelings, concerns, and experiences.
It is important to maintain a level of regulation. But the balance is still a bit skewed.
There is so much information patients don’t know. And by the current system, there is no way they can take even the slightest peek behind the curtain.
These regulations simply compound with pressure from the FDA, campaigns run by lobbyists, and specific hospital guidelines.
The quality of medical records is something else that is severely lacking. This, in turn affects the difficulty of patient care. The most clear-cut decisions on paper might emerge as the most complicated in practice. This is why the work of a doctor cannot be reduced to algorithms or coded for clear outcomes.
And yet, as the costs of healthcare are ballooning, there is a saturation of lobbyists, and a decline in healthcare practitioners.
Some doctors feel trapped in this system.
Hoping to gain a brief respite from prison, a man swallowed some scrap pieces of metal. This was our first foreign body extraction. The doctors used an attachment threaded through the endoscope, with a claw end, to drag the metal out of the man.
I suppose his plan worked well enough, as he did end up in the hospital for a day and a half.
I cannot fathom the stifling feeling that might drive a man to such extremes.
The most salient thing we have learned from Dr. Sleesman is how to treat patients. Treat in the sense of prescribing cures for ailments, and treat in the sense of general human care. He does an excellent job balancing his responsibilities and proclivities as a physician, with his ability to make each case, each conversation important to those he teaches.
There will always and only be doctors who care.
WEEK 3A: Rounds and Ruminations
Christine Joseph Blog

Inpatient rounds are at 7 AM – a team of an attending physician, a fellow, a few residents, and the occasional bioengineering undergraduates set off. The resident explains any new developments in the case, and a treatment plan is made together. These rounds include discussions of the different pathologies and etiologies that will be encountered, and some gentle quizzing of the residents. The whole gaggle of us walks into the room, where the attending or the fellow generally begins the conversation with the patient. The new information is compiled, and they discuss in the hallway, their theories and considerations. The hall is small and lit with blaring fluorescence. We noticed a screen that displays the heart charts of all of the patients in the wing – a clear and easy way to keep everyone in check. There are landline phones in easy reach that do not appear to be sterilized after each use. The residents print everything out to write on. Their pockets are big, and we’ve seen a folding clipboard comfortably nestled in there.
An unsung marvel of engineering is that loud medical devices have a mute button.
There are mobile computer stations scattered throughout that provide a useful resource when considering the patient’s past records in creating their future plan. These mobile computer stations are meant to be adjusted based on height, but remain static for lack of time. Some chairs have been brought into the hallway. Empty beds wait in the hall, as well.
These hallways tend to get a bit congested, what with the different sets of rounds and consults, and miscellaneous chairs and hospital beds.
During rounds, they discuss the literature, and decide to consult with the oncology department before making a final decision.
They discuss which patients might be difficult to convince – especially when it’s simply the prep for procedure they find so repugnant. There are a few patients who cannot be trusted to follow through, there are a few patients who lie, and the doctors must account for that in their treatment plans.
Sometimes, less is more.
Many of the doctors at UIC also work at the Jesse Brown VA hospital. There is a completely different organizational system in place; from differences in the electronic medical records, patient population, and overall healthcare costs.
Many of the problems in the procedure room deal with the maneuverability of the tools. Another doctor suggested a combination snare and net. Dr. Watson, the senior resident, suggests a capsule endoscopy pill camera that can be controlled in the intestines a la Magic School Bus.
A neat thing done during procedures is layering gloves. This allows the doctors to remove a used glove, and not have to struggle with donning another. Generally, though, gloves are hard to work with; they are very necessary, but make the fingers a little less dexterous.
Sometimes keeping patients happy isn’t in their best interest. Here, the ideals of empathy and efficacy seem at odds. This is especially interesting in light of our Monday workshop about empathy in engineering.
We’ve seen patients, given a new lease on life through a transplant, taking poor care of their bodies. Some patients are dependent on narcotics, and some grow addicted to the protective cocoon of the hospital.
Consents for procedures are obtained and included in the patient binders, which are transported whole to the procedure room.
Some mornings, the list of patients is chock full of people who are indistinguishable on paper. The group must work to differentiate each patient, checking and double checking that their analysis is consistent with the records.
We heard a horror story about a patient accidentally being put on the wrong medication – medication that actually worsened his condition. The doctors work hard to ensure that this kind of thing never happens.
But there is only so much you can do when it comes to cross-departmental measures. Some GI patients are admitted in the ICU, some are still in the ER. Access to records and results is pretty immediate, especially in procedures don in this hospital, but some tests are not done in a timely manner. In one case we witnessed, in deciding the best imaging modality (here, between EUS, or MRI/MRCP), the onus lies on scheduling. The ICU doctors naturally, have their own priorities, and it is here that each doctor must be the advocate for themselves, and most importantly, for their patients. Resources – especially if something breaks – are spread disparately around the hospital. If a certain machine is not available in the GI department, they must get special permission from other departments with the machine to move a patient in, and use the equipment. Things, however, do get lost in the shuffle, and sometime the external department will deny access to machines, cancelling cases by their own metrics.
Just as the body works as a whole, the system of specialists that treat each constituent ailment or part must communicate to ensure the best care for the patient. This means too that the gastroenterologists must focus on what is best for the GI tract, and the cardiologists on the heart. Each doctor considers every etiology, every indicator, and every part – and it is actually the best-rounded doctors that really know how to approach any compromise, that defer and accept when they are wrong.
I was really affected by a consult with a young girl afflicted with catatonia. She was trembling, couldn’t speak, and could just barely flicker her eyes.
In a smaller, but similarly impactful way, I was struck by a patient struggling to reach her bedside drawer handle.
Dr. Halline reassures a patient who is afraid of a budding cancer. Explaining the difference between a carcinoma and a carcinoid. Answering to “Doctor whatcould have caused this?” with a clear and gentle “the tumor is… and it means…”
There are people come to the hospital as a last resort, and it really hurts me to see them in such pain. There are patients who know they are on their deathbeds. There are patients who don’t.
There are patients who struggle forward increasing the quantity of their lives while destroying the quality. Most everyone wants to die quietly in their sleep. But when given the choice, no one is quite willing to let go.
WEEK 3B: Medicine and Engineering
Christine Joseph Blog
Early Wednesday morning, we attended a lecture given by Dr. Boulay about cholangitis, a biliary emergency. He spoke to the fellows about the past, present, and future of treatment options.
In essence, giving these doctors the equations they needed to be able to apply to different problems.
An interesting procedure we saw concerned the deployment of an esophageal stent. From what we gathered, the patient’s esophagus was deteriorating, and the stent was needed to promote a healthy structure. The decision of which stent to use was a bit subjective on the doctor’s part – heavily dependent on the quantitative dimensions of the patient, but ultimately decided for by the physician. The stent began as a long and narrow tube, and when expanded, the qualities of the wire mesh made the end result shorter and wider. The rigid guidewire was inserted into the esophagus, and the scope was backed out of the system in a 1:1 ratio with the wire pushed forward. An external guidewire (in the form of a paperclip) was taped to the patient’s chest, and was able to be seen under fluoroscopy. An endoscopic view provides extra insurance. But sometime, the anatomy of a patient will not allow for further scoping.
The man had esophageal cancer, as well as an abnormal air picket. The stent was designed to dissipate the air and open up the esophagus. The stent was made of nitinol and coated with silicone – for biocompatibility. The gun was made considering the radiopacity of materials.
The procedure was a success, and the man was finally able to eat and swallow properly. This isn’t a permanent fix, but it’s where we are in Medicine today.
It’s been nice to search for answers to those simple questions no one thought to pursue. In our first week, Dr. Carroll asked us to explain how the pharmacy paper they use to print sensitive prescriptions on are unable to be copied – printing ‘VOID’ on the copy paper instead. We discovered it was due to miniature dots embedded in the paper’s design that became clear only when the bright light of a copier were exposed to the surface of the paper. Similarly, we were asked to explain why the lights at the end of the scopes flickered, and why the flickering was not seen on the video feed. We discovered the lights were LEDs, and that the shutter speed of the camera was coincident with the flickering of the lights.
We went through the process of capsule endoscopy, first watching the nurse attach the sensors to the outside of the patient and outfit him with the monitor. We watched him swallow the pill, and saw him off. We ran into him a few more times doing rounds and he joked with us that we owed him money for all the shows he was giving us! We sat with Dr. Sleesman as he explained the results of the capsule. Over the course of the thousands of pictures it was determined that there was a significant amount of bleeding in the small bowel. We attended the next procedure, where they attempted to access the site of the bleeding with a forced scope. When that was determined to be impossible, they scheduled the patient for a double balloon endoscopy, which allows for the use of balloons to inch the probe into the small bowel. We attended that procedure, as well, and watched as the doctors found the source of the bleeding, and cauterized it.
The screens are hypnotic, the journey through the body so familiar and clear.
I’m not yet ready to say goodbye to GI.
WEEK 4A: Blood and Guts
Christine Joseph Blog
The first few days in the oncology rotation have been hard impact after hard impact. Here’s what we’ve seen so far, in a slight departure from my usual style of blog.
I spent much of the first day learning about the way the department works. I sat in on the scheduling meeting. Each patient was discussed, and their needs assessed for the next month. The entire team works together, bringing up their specific and specialized concerns. The doctors defer to the director, Dr. Rondelli, but the discussion is especially spirited as everyone participates.
I learned that there exists a discretionary fund to help patients with their expensive treatments.
We attended a research meeting, where each project was checked, reviewed, and finalized. Goals were set and challenges were given.
We talked about the differences between the research done by the department, and the labwork that is done for treatment.
We visited the stem cell lab. We followed blood through the stages of collection, cryo-preservation, and will see the cells being infused in the coming days. The process is fairly methodical – but there is a lot of math involved, as the biological and hematological parameters differ from patient to patient.
We talked about the staggering costs of healthcare, and how the quality of materials plays into this.
We also talked about the accreditation process, and the investigations and quality-checking that go along with it.
On our first set of rounds we learned that there must often be substitutions for clinical materials, as some are discontinued, and some are simply not available anymore. Some treatments are so expensive, they are not given “in house”. there is a lot of balancing and maneuvering between departments, as each set of doctors must argue for their course of treatment. Time is a serious factor, as each doctor has so much on their plate. Sometimes procedures must be done by residents, instead of the designated therapists, simply because they can’t afford to come back to see the patient after the external procedure. These checks and balances allow certain patients to be cleared for certain kinds of imaging, and serve to make the hospital work more efficiently.
Wewere the witnesses for a woman’s DNR order.
We watched her come to terms with her diagnosis.
We watched her husband reach out to hold her hand.
There are a lot of devices that make soft, tinny noises. When patients are being given serious news, the sound becomes infuriating.
There is also no clear way to mark that the attending team is in the room, talking to the patient. The closed door ended up being opened more than four times in a single session by well-meaning nurses, technicians, and other doctors.
In oncology, it is important to make sure the treatments do not become toxic. There are drugs that increase the quality of life, but decrease survival. There are drugs that do the opposite.
It’s a heavy choice that oncology patients have to live with for the rest of their lives.
WEEK 4B: Risk/Reward
Christine Joseph Blog

Inpatient rounds:
Some rooms have two doors to ensure safety and sterility for neutropenic patients.
Some smells and sights are particularly nauseating, but the doctors remain calm and comforting.
Some treatments are too expensive to be given in house. Some procedures rarely happen due to OR delays.
Stem Cell Lab:
The freeze mix is meant to preserve the cells, which are later sent to be infused.These infusions can be autologous, meaning derived from the patient’s own body. Other options involve infusions from siblings and compatible donors.
Every piece of equipment is expensive and must be cared for precisely.
Sometime, the lab rents equipment, and though the overall costs might be greater,
The Foundation for the Accreditation of Cellular Therapy is the regulatory body that oversees this division.
Research meeting:
On the impact of their research:
“what is the final goal? We have to make sure we know where we’re going”
“Where do you put the money? Realistic applications and a pragmatic approach”
Donors – regulatory openings, IRB consent
Data sharing from pharmaceutical companies
On presentation:
“they will try to make a story through the graphs, so we’ve got to be careful how we present them”
All of the imaging comes from Rad/Onc
Outpatient clinic:
We took a quick look around the infusion rooms. They’re set up to be comfortable to the patients. There are two rooms with beds, for patients who cannot sit up. There are eight other rooms with chairs, only two that are single rooms.
Jagan brought up the idea that communal infusions might be a comforting experience.
We sat in the most comfortable chairs that have ever existed.
In this department, patient comfort is of utmost importance.
There are politics in play at this state institution.
We watched a patient’s wife arguing loudly with a nurse, Dr. Quigley came out to reassure the woman that all that could be done was being done.
We met a patient with a tenuous social situation – a family disdainful of having to take care of her, and even willing to take advantage of her disability checks.
Dr. Bolshinsky talked to us about her experiences in Spain and Italy. The biggest difference she notices here is due to insurance. There, medical care is given freely. Here, patients must live with what they can afford.
Yasmin, a medical student from Brazil, talked to us about the system there. They enter medical school right out of high school. Medical care is funded by the government, but there is an overabundance of patients, as a result. She liked the chance to see medical care and teaching in a different light. In her experience, her teachers and mentors were never this welcoming and nurturing.
A patient’s son points out lies his father is telling.
Dr. Rondelli has so far revealed himself to be trilingual. He told us that he learned Spanish on the job, and it makes a huge difference in his ability to care for his patients.
On delivering a difficult diagnosis:
“It wouldn’t be honest for an oncologist to give a straight answer”
On helping a patient determine his course of treatment:
“this is something a doctor can’t decide”
The clinic is kept well-stocked, here’s the delivery cart:
Another mildly unrelated invention is the knee pads worn by the maintenance staff. They protect the shins, and were a real game-changer in the world of anyone who works on their knees.
Each patient has a special relationship with his/her oncology doctor – it’s about the human.
As cancer is not yet cured, a good number of treatments are experimental. Clinical trials are these experimental treatments.
The first iterations of chemotherapy heavily damaged the DNA.
Even nowadays, more is better, as dose limiting toxicity is linked to the number of treatments more than the intensity.
Dr. Patel explains that the current system of autologous transplant is a bit of a trick. The bone marrow is spared from the radiation, and taken for preservation in the stem cell lab.
Intensity modulated radiation therapy is now used to target the bone marrow alone.
Inter-departmental struggles are still abound. Sometimes doctors try to go over the authority of one another, sometimes their encounters aren’t adequately documented.
We met a patient whose vitiligo disappeared, as the donor cells changed the display of her skin cells.
We’ve noticed doctors attempting to change the angle of their computer screens, which isn’t a functionality currently in place.
Dr. Ghimire is a pretty new fellow, and it has been interesting following him around and taking notice of what he notices.
Young kidneys are only given to young donors, but things are changing quickly, as certain protocols are being developed to make older kidneys more viable.
Some doctors sit at eye level. Some tower over their patients.
Doctors must reassure patients that the medications didn’t cause the symptoms – because drug stewardship is very important in this department.
Some comfort can come from alleviating pressure.
Photophoresis is the process of exposing blood to UV light, and replaced into the system supplemented by immunosuppressants. The donor immune system reacts against the patient’s, at a positive outcome.
Hepatitis B resurgence comes from the effects of immunosuppressants.
Every determination of appropriate dosage, comfort, and intensity is based on physiological parameters. But it is also based on a great deal of weighing risk.
WEEK 5A: Understanding
Christine Joseph Blog
We were able to see the process of collecting the stem cells we’ve already seen processed.
This machine separates the stem cells and the plasma from the blood, returning the blood into the body.
We also watched the research technicians run stress tests on some old equipment. The experiment we watched involved testing the loss of liquid nitrogen in a transportation container with an imperfect seal.
Some of the different imaging modalities we’ve encountered are PET, CT, and gram staining. At the Tumor Board meeting, doctors and nurses take a look through each patient’s imaging and histories.
It’s here that they notice some patients who slipped through the cracks – where primary care doctors don’t know how to expedite the process through the UIC hospital system. It’s here that they talk about patients whose conditions aren’t accounted for in the literature, and it’s here that connections between these outliers are made.
There is often a difference in a person’s biological age and their actual age. The way our organs adapt to age is dependent on many physiological factors, and in determining the best course of treatment, the state of the body is often more important than the generalized considerations of age.
We got our first look of the specialized BMT wing in our rounds this week. The patients in this wing are all future transplant patients, and are kept sequestered by necessity as well as convenience.
Sometimes doctors and nurses orders are illegibly written.
The whole system of rounds in this teaching hospital is an interesting exercise in contribution and gaining experience. Each person on the team does a different thing, each brings their specialty to the talks in the hallway. I worried it would be a situation of too many cooks, but it turned out to be more of a balanced, helpful use of everyone’s talents.
The mobile computers in the hallways are not sterilized often.
During rounds, we heard the pharmacy students with us get admonished for not sanitizing their hands. We learned that a C. difficile outbreak had made its way around this unit. We caught an undercover agent scoping out the unit, checking that people took the appropriate disinfectant measures.
We waited outside the sequestered rooms to save costs on yellow gowns and decrease chances of infection.
We spoke with Mr. Manju, the director for Patient Care in the Oncology department. He talked about the difficulty of selecting between options when all the options are about equally good – just in different ways.
We talked to a groundskeeper, here, whose real calling in life is selling shoes. He told us how hard it is to move up in his line of work, maintaining the hospital grounds and building, but also about how those in the upper echelons of responsibility don’t even get to garden.
A small focus group of the bioengineers headed over to the Hospital Administration office at the tail end of our lunch break. We got the chance to talk to one of the secretaries, and ask any administration-related questions we had. The tiered system of accountability in this hospital sometimes allows for ideas and improvements to slip through the cracks, but altogether, the system seems to be as sound as it can be. There is an avenue for any of the hospital employees to submit grievances, and an administrative team always visits the unit in question before making a decision. The biggest problem we could see was a function of the incredible amount of emails that are sent to the administrative office – when all problems are thrown into the same bag, it’s difficult to distinguish the large from the small.
WEEK 5B: Comfort
Christine Joseph Blog
After our first encounter with them last week, Jagan and I decided to seek out the Palliative Care team.
We talked about the difference between living and putting off death.
There is an algorithm for measuring adequate care; a checklist that, when efficient, is less personal, less cerebral. What makes sense for health doesn’t make sense for policy; the goal is to promote health by preventing disease, which isn’t easy to quantify. Some doctors are too focused on numbers, on outcomes. It is easy to view a hospital as a business investment, especially from an administrative perspective. There are certain expectations for returns.
The Bone Marrow Biopsy was a real shock to the system. Make sure to take a look at Jagan’s post for his account of the procedure, as well as the vasovagal response, and research into the parasympathetic nervous system. For me, it was just a little horrifying how gruesome and visceral the procedure was.
This procedure is used to assess treatment options.
Dr. Zia, the fellow, performed the procedure, with some residents and students observing. A biopsy technician stood by the side, waiting to prepare slides and samples.
Tactile: the lower back was pressed to find the site, this site was marked with a pen.
Sterile: the tools are packaged together and triple wrapped.
Effective: the syringe is coated with heparin to prevent clotting, the needle attachments are color-coded and lidded.
Then comes the lidocaine, the tiny dagger, measurement with a needle, and the boring with the biopsy needle. A core sample is removed, and then aspirate fluid. The needles is twisted out and samples are taken in tubes, slides and a dish.
In the middle of the procedure, the phone started to ring, and ring, and ring. It stopped eventually, but seemed to go unheeded for too long.
Another problem we observed was that the biopsy needle didn’t fit into the sharps box. The doctor has to wrap it loosely in plastic, and carry it to another disposal bin.
We were also finally able to see a stem cell infusion. The cassettes are removed from the holding tank, and transported in a cooled cylindrical tank. They are thawed by the patient’s room, and infused into the venous system.
The diameter of the IV tube determines the rate of infusion. It is controlled based on the time and amount of liquid needed.
The viability of the cells decreases quickly with time. Time-saving ventures are definitely worth exploring – for instance, we watched Grace, one of the research technicians, struggle to unscrew a specimen tube with one hand, while having to hold on to the sampling syringe in another.
To test viability, cells are dyed and counter in quadrants – an improvement here could lie in the development of graphing notepads for consistent notation.We talked to a few more doctors that had worked in different departments, and different hospitals – they all spoke of Dr. Rondelli’s influence on them as a team as the driving force for the program here.
So I spoke to Dr Rondelli about his reasons for being here, his reasons for building the program just so. He is a pragmatic thinker, but never lets that stand in the way of his
Much like Mike and Misia’s testimonies, my conversation with Dr. Mahmud was humbling and inspiring and infuriating all at the same time. He gave me a quick tour of his research lab, where I was able to see the tools of the trade, and the innovative ways they’re hidden to deter theft. I met his research team, and we began to talk about the work they do there. There is a conventional understanding in the field of stem cell therapy that a differentiated cell can never become undifferentiated again – but this understanding has influenced the work of researchers hoping to propagate stem cells. Dr. Mahmud’s lab seeks to understand the homing aspects of stem cells, as well as work to perpetuate viable stem cells. He explained the limitations of the circulatory system, and we spoke about the inevitability of cancer with age.
We talked about finding a niche, about how intuitive it is for the cells to return to their geneses, and how hard it is for myself to do the same.
WEEK 6A: Lines and Rays
Christine Joseph Blog

I’m sure you’ll remember the ceiling fish from my predecessors’ blog posts -today we heard a great story about how they were installed to the perspective specifications of someone facing in the exact opposite direction of a patient lying supine on the table. This gave the impression that the fish were dead and floating at the surface of the water. The tiles had to be rotated, and a valuable allegory about considering the patient was born.
The machines here are just incredible.
The physicians look through the diagnostic CT scans and make their recommendations for dosage and intensity. These recommendations head to the dosimetrists, who formulate a viable treatment plan, which is then sent to the physicists, who review the angles and targeting.
We came in early to watch the machines turn on. We walked through the Quality Assurance procedures, checking every component and every possible malfunction.
Because red wavelengths are wider, green lasers make clearer and crisper lines.
The engineer on the staff told us a terrifying story of patients dying on the table during routine radiation therapy. In that particular machine, therapists were allowed to modify treatment during the procedure, changing the intensity of the concentrated beam. However, in a few cases, the machinery malfunctioned and the protective screens did not deploy. The patients were struck with a high-intensity ray, receiving lethal dosages of radiation in minutes.
The scariest part of it is that it wasn’t noticed at the onset. And that it happened more than once.
In this increasingly technological world, it’s tempting to allow computers to do their work, unwatched and set to their own programming. The engineer on site was once called down to investigate a burning smell, thought to be coming from the vents, but it turned out to be a machine malfunction. That’s why today – when we heard a loud, pounding noise, disturbing the patients and the peace – we ventured into the tunnels and moldy stairwells hidden underneath the hospital, to find a jackhammer in action. A formal complaint was sent straight to the source, but there wasn’t much else we could do.
Another review of a stem cell infusion:
We boarded an elevator at the third floor, heading up to the eighth, with a patient in a mobile bed set to be taken to the seventh floor. The wheels of his bed jammed themselves into the space between the elevator doors, and the patient winced and let out a cry of pain. Apologies were quickly uttered, the bed rammed through the obstruction, and the patient sent on his way.
It’s either the unevenness of the elevator floors or the diameter of the wheels at fault here.
The insulated transportation container could definitely stand to be lighter and have a retractable handle to reach the arm level of the research technicians.
Even after the warm water bath, and the melting through of the cells, a small frozen piece remains in the nozzle. Youngmin prods at it until it melts. She explains that the color and saturation of the blood is variable; dependent on the unique RBC concentration in each patient’s sample. She twists the cap off of the sampling tubes before she begins to use the syringe.
The DMSO used in the freeze mix begins to smell strongly of garlicy sickness as the infusion goes on.
The IV bag is a little difficult to pierce through during each change.
Suddenly the floor is in an uproar – the internet connection has failed and no one can log in to update vitals. They quickly switch over to a paper-based system as an interim measure.
WEEK 6B: The End
Christine Joseph Blog

Radiation is a little horrifying. And a little amazing.
Conventional radiation machines concentrate and bend ions – not actually using any radiation.
The actually radioactive materials are stored in the Isotope storage room, and are contained in tiny seeds inserted into the body’s orifices to irradiate the cancerous cells.
We talked to the medical physicist, Brett, about automating processes. He uses Python to make his job easier.
He has the daily report automated and analyzed for his review at the end of the day. He runs a check to see where errors occur, and is working to isolate these variables further to solve these tiny, almost-imperceptible problems. He compares this verification and recording with the original device specifications.
We learned that the diagnosis of cancers like prostate cancer have increased considerably in the past few years. Because everyone in the country must now have health insurance, more people are being screened for those cancers that almost inevitably develop with time. This reminded me of my father telling me that absolutely everyone in olden-day India died of a heart attack, simply because the final cause of death was always the heart stopping.
The engineer, Simeon, showed us what’s inside the machines. He brought out relevant textbooks to explain the theory. There is an incredible amount of engineering that goes into the process of maintaining these machines.
Some problems with the machines are almost impossible to address, simply because they are so new, and even Simeon isn’t an expert. They have found creative solutions to problems, but everyone seems aware that these solutions are not permanent.
They purchase the machines by lowest cost, there is a higher governing body that determines how much they choose to spend.
The mask they use to immobilize the patients is rigid and can make the patients feel claustrophobic. The problem lies in the fact that the nose and chin must be held in order to ensure the most static fit.
We also sat in on chart rounds, attended by doctors virtual and corporeal. It was interesting to note the topography and intensity of each image, and their use in diagnostic and prescriptive measures.
An automated tool cannot yet adjust contrast. There are too many false positives. Auto fusion of images also does a poorer job than a human’s touch.
At present.
The big question is how to reduce radiation time, for both better clinical efficacy and safer common use.
Investigational PET scans are an example of this innovation, displaying different isodoses.
Outside the brachytherapy room, there is a radiation field that bounces off of the lead inside the ceiling, creating hot areas outside of the door. There is talk of putting down an x-ray field to plot a gradients and analyze the dissipation of this radiation.
The three tenets of radiation are time, distance, and shielding – and these are all taken into consideration when formulating a treatment plan, especially when the isotopes are used.
Consistency in procedure is maintained by a tentative predictiveness in published scales.
These last few weeks in Oncology have really hit hard. But the last six weeks, altogether, have made a real impact, as well.
I have had an incredible time working with and growing closer to everyone in this program. It was an unbelievable experience that we were all thrown into understanding together. I have learned so much and grown in so many ways.
Julie Wagner Heading link

Hi! I am a senior bioengineering student at UIC. I am concentrating in neural while doing research with pulmonary arterial hypertension. In addition to this, I am currently the president of a student organization, Engineering World Health (EWH) after a year as treasurer. Besides academics I enjoy playing volleyball, running, hiking, and cooking. For this clinical immersion internship I will be participating in the anesthesiology and ophthalmology rotations.
Julie Wagner Blog Heading link
-
Julie Wagner Blog
Scrubs
Julie Wagner Blog

Week 1
7/6
My partner Tiana and I were assigned to the anesthesiology rotation of the clinical immersion internship. Needless to say we were excited about it. This was the one we really wanted and for good reason. With anesthesiology we came in thinking that there would be a multitude of different surgeries we would see as well as the vast amount of technology that is used during a surgical process the anesthesiologist uses.
The moment I entered the hospital I was a little bit anxious about what lies ahead. I wasn’t to sure what to expect but I had a feeling it wouldn’t be anything like what was on surgery based shows. As soon as we met our mentor for the next three weeks we hit the floor running (actually speed walking would be more accurate). Without hesitation we went to get scrubs to change into. To be honest putting scrubs on for the first time is an exhilarating experience! It was as if this program officially started and I was excited to get started (just look at the picture for proof!).
After a very quick tour of the maze-like surgical floor we took a trip into a near by OR that was performing a spinal surgery. While here we were informed about the rules and regulations of an OR. Something that surprised me was the fact the entire room was not sterile. They did in fact have a sterile field that had very strict rules about who can even go near the field. The sterile field consists of any open uncovered tray or anything that is facing the patient. Since the entire room is not a purely sterile environment only those who entered the sterile field needed to scrub in.
We went to another case right after this introduction to an OR setting and this case was eye-opening to me. Before we met the patient our mentor did prep us for how sensitive this case was going to be. This was the first time that I was exposed to an extremely emotional clinical setting and it was only day one. This patients family was visibly worried and nervous about them undergoing this procedure (brain surgery were there was a build up of CSF in the ventricles due to a cyst). Although they were worried they tried to be strong and supportive for the patient while at their bed. The patient themselves were another story. They were terrified and crying. This was very hard for me to see and I was very thankful to have my face mask on during this time.
Although this was a very difficult time for the family and patient my mentor surprised me even more then I could imagine. I had this preconceived notion that anesthesiologist were more behind the scenes and did not interact with the patients except to walk them through the anesthetizing process. I could not have been more wrong. He was there before going into the OR and talking with the family and patient about the procedure and was there to comfort them in such a difficult time.
Once in the OR with this patient they were still scared but the procedure continued as planned. Some interesting observations was that the room was very cold compared to everywhere else and the vast amount of wires seen throughout the room. These wires made moving the patients table very difficult.
Although we did not stay for the entire operation there was some valuable information that was gained about the preparation and thought process of anesthetic treatment that goes into each patient. After observing a good amount of the surgery we retired the scrubs for the day only leaving eager to return in the morning… at 6:30 AM.
Well that Escalated Quickly
Julie Wagner Blog
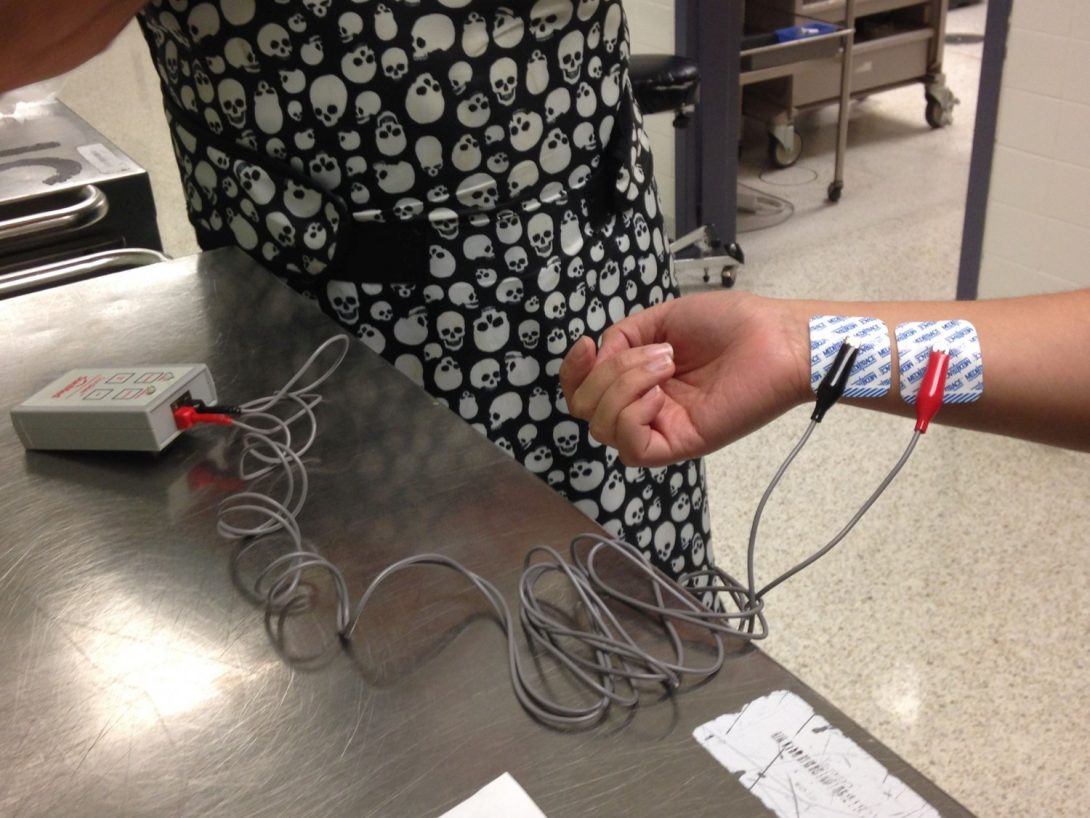
Week 1
7/7/2015
No one should be a full functioning adult by 6:30 in the morning. It takes enough effort to function as is at a normal hour of the day let alone when your brain should be turned off and sleeping away. With that being said I was at the hospital on the Anesthesiology floor ready for the morning lecture by 6:15 like a crazy person.
The anesthesiologist we are following around, Dr. Eldelman enters the conference room about two minutes after me and probably noticed the half asleep gaze or maybe I hid that well enough with some enthusiasm to learn, since I was the only crazy person there, either way he knew the desperate need of coffee I was craving. He showed me to the glorious kitchen that they have for the department with the constant flow of coffee. Obviously the clouds prated and a beam of light shown over that coffee pot.
In the morning lecture Dr. Eldelman was the one who was presenting on the type of anesthetic drugs that are used for the practice of anesthesiology and made special note one those used at UIC. Here is where I realized how the bioengineering classes I have taken so far all connect with a medical specialty.
When the lecture ended we changed into our scrubs and got moving. It started off chaotic. We went downstairs to the radiology department. Dr. Eldelman’s cases were switched at the last minute so he was quickly reading over his knew case file and so multiple problems. The main one was that this patient had some serious health concerns yet did not go in for necessary testing before coming in for this new procedure.
Anesthesiologist need to take multiple factors into account before even letting the surgery take place. Some of them are as followed:
-the patients medical history
-previous operations and whether there were complications intubating
-a patients physical state
-anesthetic drugs (the amount necessary to put them under, how much is necessary to keep them under, how long they need to be sedated, after so much time will they need to be awoken, and any possible reactions that the patient might have with the medications)
-the type and duration of the surgery
Since this patient had Sickle cell and came to the hospital in regards to a brain aneurism with a possible hart complication, this made the process a bit more complicated. By choosing not to go to the medical tests that were required before the procedure Dr. Eldelman along with other professionals decided it was best to wait for testing before proceeding with any surgery.
We proceeded to another surgery were the patient came in because of an abnormal heart due to either its shape or size. We arrive just as they are getting ready to intubate the patient. The doctor was using a video camera laryngoscopy (VCL), which uses video assistance in order to intubate the patient. This seemed to take a little longer then usual so Dr. Eldelman began as he put it “mooshing” the neck to prevent the patient from vomiting. “Mooshing” is where someone massages a part of the neck. This did not help put in the entubation tube. They quickly switched to using a fiber optic cable to get a better view. This still did not allow the tube to pass the vocal cord. Things start to become a bit more panicked and the real chaos begins. Dr. Eldelman steps up on the stool that was already by the head of the operating table semi-tripping on the cords on the way up. Since the fiber optic assistance did not work they switched to an airway rescue (what they call when the patient is not getting any air into their body and the anesthesiologist needs to reestablish the airway). Dr. Eldelman decided it was best to bag the patient and start to manually ventilate with the goal being to awaken the patient and intubate them awake instead of under anesthesia.
When the patient became awake and responsive they were told the news and was in good spirits about the situation, maybe because this was their 13th surgery within the past year. The steps for an awake intubation are as followed: numb the throat and mouth, use a video guided scope in order to intubate, and then to finally intubate the patient while they are still awake and responsive. After this was completed the procedure of the surgery was as followed: the surgeon would stimulate the arrithmia, create a 3D rendition of the heart based on this data, find the defect based on the rendition, burn the defect, and test the heart once complete. We actually did not see this part but instead left after intubation. Honestly this was probably for the best because I was freaking out silently while the true chaos was going on.
Dr. Eldelman walked us out of the room and told us exactly what happened and why this became an emergency situation. I think he noticed that we were a bit caught off gaurd and let us have a coffee break while we did some research on anesthesiology (reading from the giant textbook he gave us). I for one was thankful because I needed the time to process and get everything straight again.
After our nice break we talked about some of the technology that we saw in the brain surgery yesterday. Pictured above is a nerve stimulator that is used to detect the amount of paralysis that a patient experiences throughout a surgery. As seen above the sensors are attached to a nerve in the forearm and allow a current to flow through. When checking for paralysis a button is pushed that allows what is called a “train of four” to pass. This is four stimuli that go to the nerve at equal intervals. This stimulus will be reflected by the amount of movement seen in the thumb. In order to see the full effect and what they patient would be experiencing we were able to test it out.
After this sun experiment we observed a neck dissection for thyroid cancer and a lumbar epidural that was used for a gun shot victim. By the end of this I was exhausted but thrilled to see so much and have all sorts of ideas running through my mind. Most of these will be explained later as I document the rest of the week and they become more pertinent then. Now I am just looking forward to the rest of my time here and hopping that it never ends!
Suction
Julie Wagner Blog

Since we started this internship there have been moments when people come to use and say this is what is wrong or this is what we need about a product or technique. One such instance not only effects anesthesiologist but trauma surgeons as well as those who are in the ER.
A suction device is used in most surgeries, especially those that require the patient to be opened up. The device takes excess fluid and small particles out of where a surgeon is operating on the table and places it into a sealed container. For the suction device pictured above when anything is added to the container it will display the amount in mL on the screen. As seen in the picture, there are two containers where the suctioned substance can be collected and that is determined through the initial set up, for this case the bottom container was the only one utilized.
I should also point out how the bottom container is much larger then the one on top, this is because the suction machine is used throughout the day without draining the liquid until the very end of the day. Although this is convenient in the sense that there is less clean up required throughout the day and between surgeries I couldn’t help but find this method wasteful. As strange as that may sound I kept thinking that there could be some way to reuse the blood that is entered into the container. Maybe so that it can go back into the patient similar to a bypass machine so that there is less of a blood volume and hemoglobin loss. The problem with this is that there would need to be a way to completely remove the blood from any irrigation that was used, tissue particles, and small bone fragments that could have been picked up from the suction. Although this might sound easy the fact is that some of the particles are so small they have the possibility to pass through a filter.
This was something that I couldn’t help but notice while Dr. Eldelman was explaining an enhancement to the machine that would quantitatively benefit those who monitor it. As previously mentioned there is more then just blood that enters the suction device therefore, the total volume that is displayed is not purely the blood loss the patient has experienced. This is a concern for anesthesiologist because they are worried about the patients blood volume as well as their hemoglobin levels. They do have ways to estimate these measurements but they are not exact. Even if the estimation is close there are still those cases where the anesthesiologist are wrong and the hemoglobin drops below 8 after drawing blood and checking the hemoglobin level (on average a normal hemoglobin level is 15 but 8 is still good especially during surgery).
What was proposed by Dr. Eldelman is a way that the hemoglobin level could be displayed on the screen with the blood loss as well as the total volume collected by the suction machine. This way would provide qualitative measurements so the anesthesiologist know exactly how much hemoglobin to give a patient. By doing this patient care becomes more efficient.
In order for something like this to work there would need to be a hemoglobin scanner and a red blood cell detection system. Although this might sound simple Dr. Eldelmen assured me that it is much more complicated then it seems.
Monitoring
Julie Wagner Blog

Besides being able to watch what Anesthesiologist do and their technology we were able to be exposed to intraoperative neuromonitoring during a STA-MCA bypass surgery. Before seeing the technology being used we were lucky enough to talk with two specialists, Ashley Selner and Faisal Waseem, about how the devices they use work and what it is they do. Intraoperative neuromonitoring utilizes sensors that are inserted next to a set of nerves cortically, subcortically, and a peripheral point of interest. These senors detect potentials from the nerves that they are next to (pictured above).
In order to get waveforms that can are easier to understand the signal is amplified, put though a low pass filter, and averaged. This allows the small potential (uV) to be read more easily. The main job for the intraoperative neuromonitoring specialist during surgery is to monitor these waveforms and alert the surgeon when there is unusual or abnormal activity that is seen.
The STA-MCA bypass surgery that used the intraoperative neuromonitoring was done a a nine-year-old kid. Before the day began Dr. Edelman warned us that this would be a tough one because of their size and age. At nine, the vessels are small and frail making it very difficult to operate on.
In the operating room there was a lot of tension due to this, which could also explain why they prep time took much longer then usual. Approximately three hours were used to place in all of the necessary tubing, IV’s, and intraoperative neuromonitoring sensors. Although it was heartbreaking to see them loose a lot of blood because of the difficult placements, the hardest thing to watch was shaving their head. That’s when the whole experience became very real since this was the youngest patient we have seen undergo surgery and not to mention it was a very serious surgery too.
Once everything was set up and the surgery was underway the overwhelmed feeling of what was happening became much more manageable. Seeing how the monitoring was going about was very interesting to me because of the signal processing and waveform interpretation is something I enjoy learning about. After seeing the sensors in action and talking with the specialist this is something I am planning to continue to look into as a possible career choice.
Modeling
Julie Wagner Blog
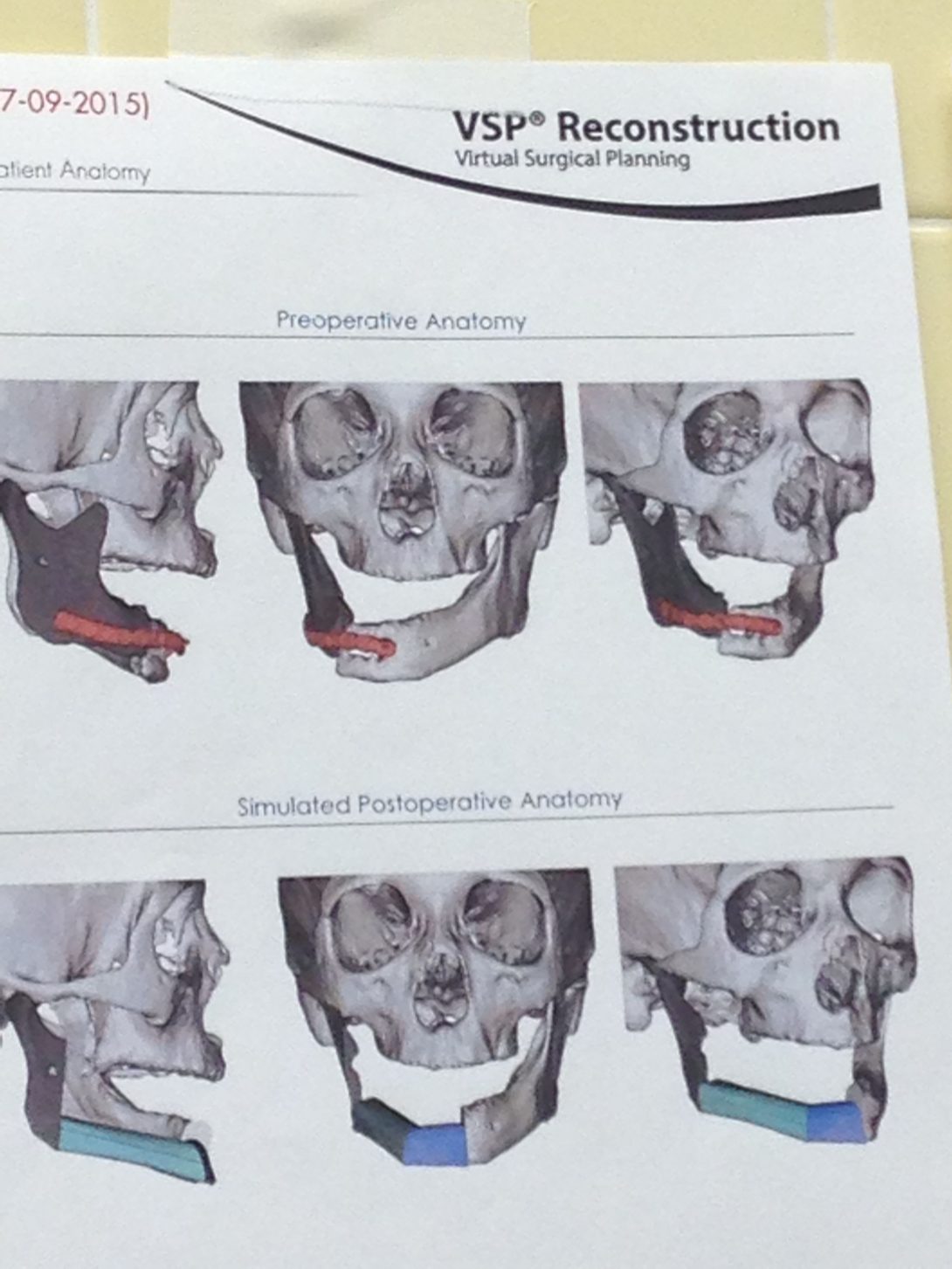
Going in for the usual morning lecture on Wednesday I was exhausted and ready to fall asleep, especially knowing ahead of time that this lecture was going to last an hour and a half long. Coffee in hand I went in with the mind set that I was going to have to try really hard to stay awake. To my surprise it was much easier then I thought. What help is that the presenter kept cracking jokes throughout the entire time. I mean when you compare spinal anesthesia to “the cats meow, the bees knees, for you younger generation the older ones of you would say it’s ‘da boom’ and for you even younger ones it’s ‘the shit'”. After that I knew this day was going to be one to remember.
Once the lecture was over we went straight to the OR as usual. Unlike most days we stayed in the same room the entire time. The surgery being performed was a mandibular resection/reconstruction for a patient with a jaw and neck tumor. A quick summary of what they were going to do is remove some surrounding tissue of the jaw as well of part of the jaw bone itself. The jaw would then be replaced by the patients right fibula.
Since the surgery was concentrated with the neck and jaw it was decided to sedate the patient with an awake tracheotomy. The patient had additional surgeries in the same area before with tracheotomies as the form of sedation, this lead to a difficult tracheotomy. After the tracheotomy there was still a good amount of prep that needed to be done before the main procedure could begin. This included placing multiple IV’s and arterial lines as well as a gastrostomy tube (G-tube) to provide the abdomen with fluids.
The main procedure had two different surgeries going at the same time. Simultaneously, one set of surgeons were working on removing the jaw and tumor while another set of surgeons worked on extracting the fibula. We were unable to see the entire surgery since it was projected to go until 8:00 pm. The rest of the procedure included microvascularization of the vessels in the jaw to the reconstructed jaw, taking flow measurements, and closing the patient up.
On the wall of the OR was something that caught our attention. Before entering the OR the surgeons gathered and discussed a plan of action they saw fit for the surgery as well as modeled what was necessary for the reconstruction. This part was what is really interesting. By using VSP Reconstruction (Virtual Surgery Planning), they were able to plan exactly how much of the fibula was needed, how to cut it in order to get the proper structure and function of the jaw, and what the dimensions of the metal brackets to hold the bone in place. These diagrams can be seen below.
These models really resonated with me. I enjoy modeling (even if it is not exactly this type of modeling) but more importantly it got me to thinking. The only type of modeling we have in the curriculum so far is in BIOE 101 with SolidWorks. After seeing this in the OR I feel like it would be very beneficial if we had more of a modeling class, even if it was only an elective, that would incorporate real world applications such as this. In addition, it could include how to test a medical prosthetic with static and dynamic aspects.
Anesthesiology
Julie Wagner Blog

Looking back on my past three weeks in the Anesthesiology Department, I cant’ help but feel sad about leaving such an amazing experience. I was exposed to multiple interesting procedures both in and out of the operating room. Some of my favorites included a spinal fusion, a craniotomy done to help someone with moyamoya, the local anesthesia nerve blocks, a quadrupedal bypass, witnessing the Da Vinci robot during a kidney transplant, and the mandibular resection/reconstruction. Each of these surgeries, as well as the many others we were fortunate enough to see, provided me so much insight into the clinical world and how surgeons are able to help their patients out in ways that surprised me at some points.
Form these surgeries I realized that more then just memorization is necessary to be a good medical practitioner. For instance, they need to be able to think quickly when things go wrong and know what each little sign or physiology change means to their patients health and well being. Besides that what I have noticed is that the anesthesiologist and surgeons are a master of their technology. By using the equipment every day they know exactly how it works and what needs to be improved upon it. In more cases then I thought they even knew about the circuitry or mechanics behind the device they were using. In addition before complicated surgeries the operating team would get together and plan the surgery out with great detail. They would know each step of the procedure as well as who would be performing what at approximately what time that would happen and what technology they would be using. This was all incredible to see in person.
Besides seeing all of the different surgeries and the technology that was used in there we were able to be taken aside and go in-depth into what the technology actually did. Sometimes we would be taken into a hallway or the storage room were we would get this explanation while other time we were able to try it out for ourselves. We would be set up in a room and practice the same techniques for anesthesiology that are used in the OR with the technology the anesthesiologist would use too. Doing these simulations was one of my favorite things to do. We were able to practice using an ultrasound, spinal epidurals, nerve stimulation, putting in a subclavian vein and an interior jugular vein central line, and ultrasound guided epidurals. By doing this I was able to see first hand what the shortcomings of either the technology that was used or the methods themselves were.
After having all of these amazing experiences I will miss my time in the Anesthesiology department very much. I would not have been able to do any of this without the help and guidance of Dr. Edelman. He was an amazing and knowledgeable person to shadow and observe. I would like to thank him for all of his time and effort during these past three weeks because they have been one of the best experiences I could have hoped for.
Eye Opening
Julie Wagner Blog
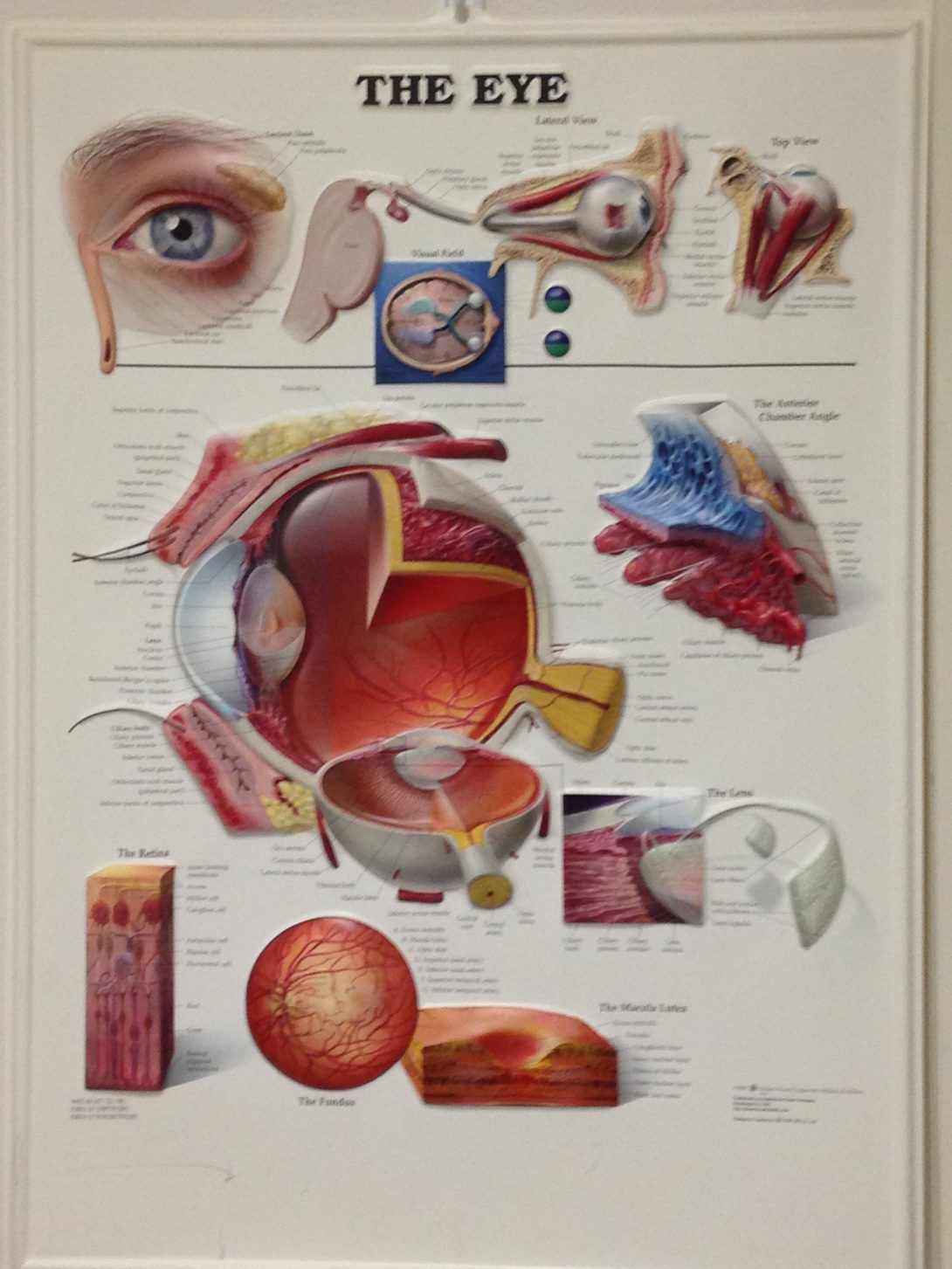
It’s the beginning of week 4 and I am starting my new rotation in ophthalmology with my new partner Mike. When we arrive to the eye clinic it’s definitely something that I was not used to in anesthesiology. We meet our mentor for the next three weeks, Dr. Sugar, in the cornea clinic where he is an attending. After our introductions he takes us on a tour of the other specialties that are at the University Hospital.
In the cornea clinic we were able to see how the patients were assessed and the quality of care they receive. I’ve noticed that Dr. Sugar’s care varies with the amount of time he has had with a patient. For instance, one patient he’s had for over twenty years and they were in the room joking around and giving each other a hard time like old friends. In contrast, another patient he hasn’t had for quite as long, Dr. Sugar is more formal about what is going on.We also had the opportunity to visit the retina clinic with Dr. Meiler. Compared with the cornea clinic, the retina clinic was much busier. Within an hour and forty-five minutes we were able to see a total of twelve patients and kept this pace the entire time I was there.
One device that is common between the cornea and retina clinic is the use of the indirect ophthalmoscope. The indirect ophthalmoscope allows the doctor to see the retina in the back of the eye. In addition, this is a headset device that shines a light on the eye of the patient through a handheld lens. The actual headset is bulky and hard to control for those who haven’t had a significant amount of training with it. When I asked a medical student what made it so difficult he told me that a lot has to do with alignment. You first have to align the headset on yourself, then make sure you can see the light through the lenses on the headset as well as the hand held lens, finally it all needs to be aligned with the specific spot on the eye that the retina needs to be seen. To make things more difficult for those who are new to using this device, the lenses are inverted. The medical student I talked to expressed how this takes a while to get used to.
Although I spent most of the time in a clinical setting it wasn’t as boring as I would have imagined. There are a lot of opportunities for improvement on the devices that are used daily, such as the inverted ophthalmoscope. In addition, I think it is a good change for me to be in a more clinical setting opposed to an OR. During these next three weeks I will be able to see how these medical devices affect patients who are awake opposed to those anesthetized during surgery.
Let’s See Some More
Julie Wagner Blog

As we go further into the week we start to see more of the different specialties. Dr. Sugar decides to break us up for the better part of the week so we can see what different specialties have to offer on our own. In addition to some additional time in cornea and retina, I spent some time in glaucoma and contact lenses.
Glaucoma is a disease of the eye that is caused through an increase of eye pressure and can lead to blindness. Once glaucoma develops there is no way to retrieve any of the loss vision but it is possible to try and maintain the disease so that no more vision is lost. During my time in glaucoma there were a couple of things that got my attention. The main one had to be the amount of patients that asked about marijuana as a prescription. Dr. Aref (the attending I was following around for my time here) informed each and everyone that although marijuana does lower eye pressure it only does so for a couple of hours and is not a good solution. Upon hearing this one patient put it “so you would have to be lit up around the clock,” which wasn’t the most medically correct way to put it, it was an accurate one. This was a big misconception to all the patients that asked about this form of treatment. After we left the room of the first patient that brought his up Dr. Aref told us that this has become a very popular topic among patients ever since the ruling to legalize marijuana in Colorado.
Another interesting condition of glaucoma is that it can affect the drainage system of the eye. If there is an extra build up of fluid in the eye from improper drainage or an increase of fluid production, can lead to an increase in the pressure within the eye. When this happens there are two different options. The first one is to to create a tiny hole in the eye in the filtration angle (where the cornea meets the iris). This hole is generally not noticeable to other people. The other option that we saw was to insert the tip of a tube in between the cornea and iris. This tube is attached to an implant that allows for the fluid to drain properly. This device can only be seen under the microscope and even then it was hard to do so! I thought that this device was amazing at how it was able to drain fluid without creating a larger hole like with the other technique.
When I went to contact lenses I wasn’t sure what I would gain from it. According to Dr. Sugar there isn’t a lot of technology that is used there, hinting that it may not be interesting or valuable. In contrast to what Dr. Sugar said, I found contact lenses to be very enjoyable! The atmosphere was generally very happy and welcoming and the patients for the most part seemed to be in a good mood during their visit. Although there wasn’t a lot of technology present, there was some things I find rather interesting.
In order to fit the contact lens properly a corneal topography test (photokeratoscopy) is done to measure the eye. It uses a lighted bowl with a concentric ring pattern that projects data onto the eye in order to map it (pictured above). Although this generally works for those who have “normal” eyes there are multiple artifacts that can alter the reading. These artifacts include: eye lashes and people who have poor topography. The last one was especially surprising to me. This machine is being used to measure topography yet, according to Dr. Joselin, it can have poor result with patients who have poor topography. Due to this inaccurate reading, there can be an extended amount of time needed to fit someone for a hard contact lens. There was one case I was were the person was getting fitted and based on the readings the left eye was easy to fit while the right eye took a much longer time. This was because the reading in his right eye was very off.
In addition to this Dr. Joselin talked about an interesting technique called “piggy backing”. This is were the user wears a soft contact lens underneath a hard contact lens. The purpose of this is to help the hard contact lens adhere better to the eye so that it will not fall off during regular use. The soft lens acts as saran wrap and shapes itself to whatever topography they eye already has. Oppositely, hard lenses will have a smooth outer surface no matter what and is rigid in place. This makes fitting a hard lens user more difficult because the steepness of the eye place a large role as to how well the lens will fit. The reason why more physicians do not prescribe this kind of treatment is because taking care of four different lenses is a lot of work. In addition, the soft lenses are not oxygen permeable like the hard lenses are. This makes the care and use of each lens more challenging since there are different protocols for each type.
I hope to spend more time in glaucoma and contact lenses during my time in opthalmology. I feel like there is a lot of potential for improvement in each of these and it is really exciting to think about!
Parking Lot
Julie Wagner Blog
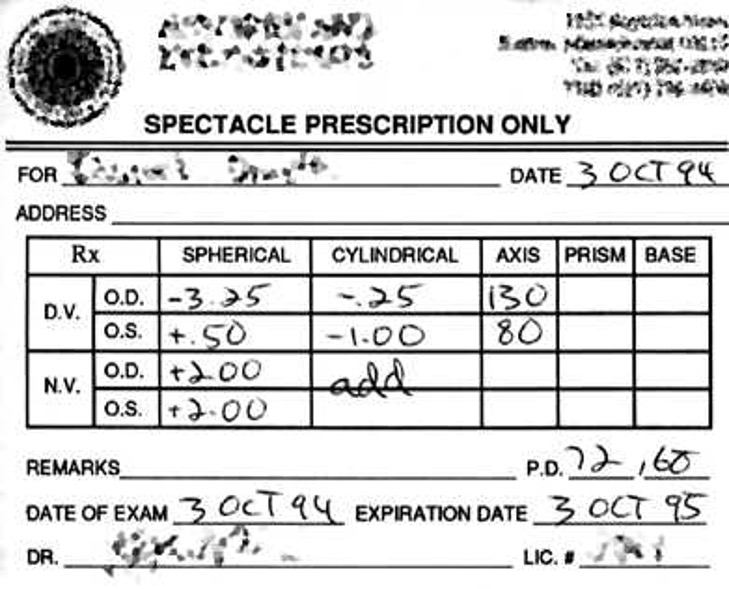
During my time in Ophthalmology I had the pleasure of seeing a lot of different specialties within the field. So far I have been in Cornea, Retina, Glaucoma, Contact Lenses, Pediatrics, Plastics, Cataract surgery, Vitrectomy (Retina surgery), Glaucoma Surgery, and an Enucleation. While I was here there were some problems that I noticed. Some of which I already talked about with the contact lenses. Two of the problems that I talked with some of the physicians about are a double barrel needle and electronic charting system.
When I was in Retina with Dr. Lim we discussed a few different improvements that she would like to see. The one that caught my attention was the double barrel needle. It is important to keep eye pressure in mind when injecting antibiotics into the jelly-like fluid filled space in the eye. In order to reduce an increase in pressure in the eye some fluid needs to be removed before injecting the antibiotic. This way approximately the same amount of fluid is within the eye therefore keeping the same amount of pressure. Unfortuently in order to do this the eye needs to be stuck with a needle twice: once for the fluid removal and another time for the antibiotic injection. This results in an increase in chance of infection (even though this is still small it is still an increase) and healing time. In order to remove these concerns Dr. Lim mentioned that a double barrel needle would be ideal. One part of the needle would be used for fluid uptake and the other for injection. Her concerns were that she did not want any cross contamination and it had to be able to use a small needle size because the eye is so sensitive and small.
While I was in Pediatrics with Dr. Abbasian we talked about the current charting system and she’s not the only one. The charting system at the hospital is very outdated and according to Dr. Sugar it would take $3,000,000 in order to update it. Even with this update the charting system would not be made any easier. Right now all of the patients charts are hand written and then scanned in order to be put into the system. This takes time away from the receptionists as well as the physicians when it comes to reading other physicians handwriting and after seeing some of their handwriting it’s surprising that anything can be deciphered at all! Dr. Abbasian said that it would be ideal to have a system that could be written on, typed on, and have spaces for their drawings of their patients eyes (which they do a lot). In addition it would be convenient if this could all be done on a tablet. That way it is portable and have the ability to switch between stylus writing and keyboard typing. In addition since it would already be electronic it would be even easier to send to outside physicians, cut down on the time it takes for scanning, and can potentially reduce the amount of paper that is used in the hospital.
**Note the image above was taken from https://upload.wikimedia.org/wikipedia/commons/a/af/Specrx-prescription2.jpg and is used as an example for the written charting system. **
Pediatrics
Julie Wagner Blog
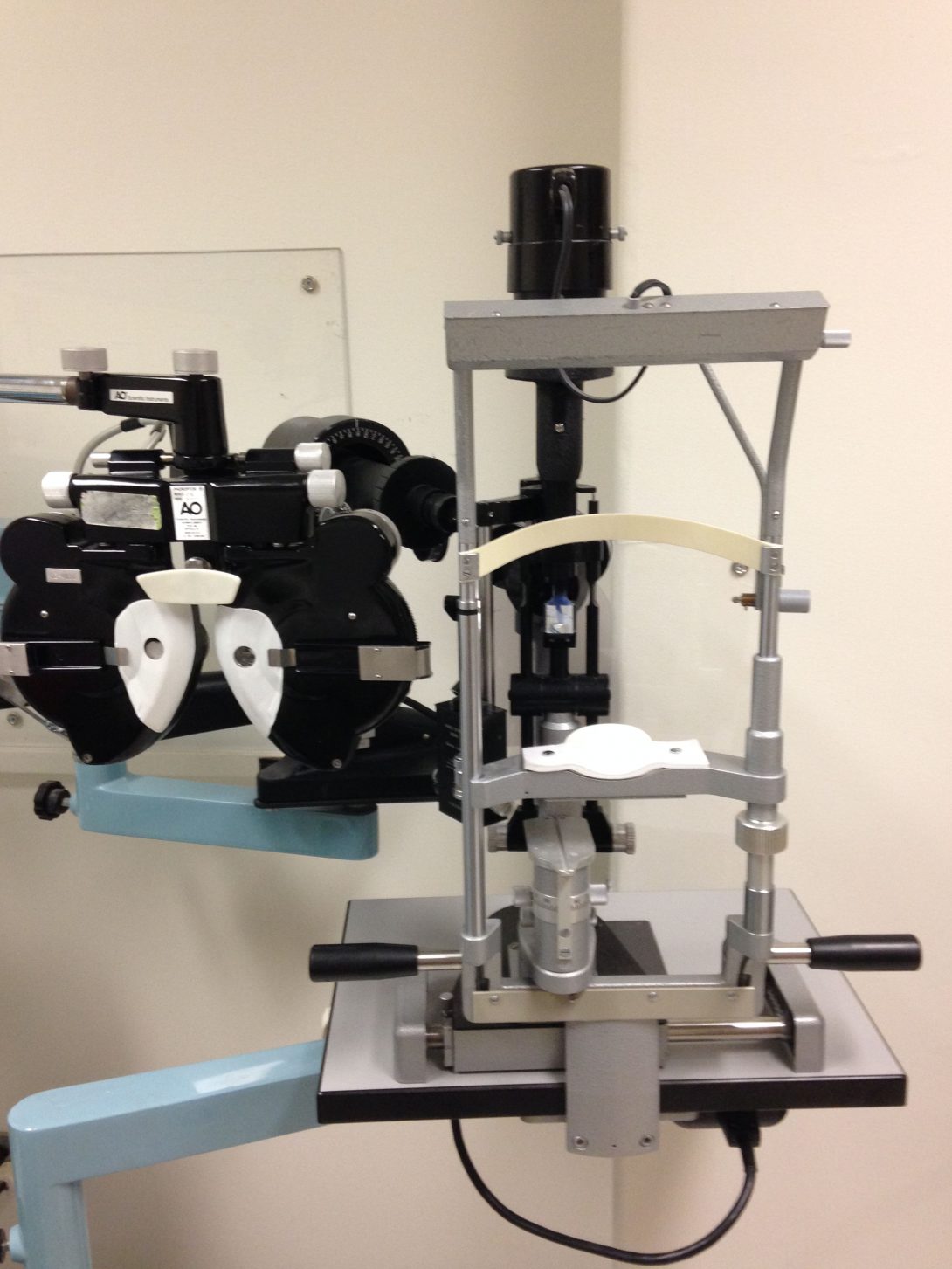
Pediatric Ophthalmology focuses on children’s (newborn to 18 years old) eye health. They see a variety of cases from glaucoma to strabismus to regular eye tests for school. Due to this most of the technology they use can be seen in the other specialties as well in addition to some special technology just for kids. For instance, when a kid is uncooperative and unable to allow the ophthalmologist to use the slit lamp to examine their cornea and retina they will use a portable slit lamp. This allows the ophthalmologist to have more mobility when the kid is being extra fidgety. Although it does not solve the problem if they are not keeping their eyes open this technology does allow a greater chance of cooperation.
Strabismus, a misalignment of the eyes, is a big portion of pediatrics at this hospital. In order to test for this the physicians use different prism block thicknesses. What they do with these prisms is hold it up against one eye in order to distort their vision in that eye and not the other. Then the ophthalmologist looks to see if the eye moves and focuses. If the eye does move and focus then they do not have strabismus. This is because the eye is refocusing to adjust to the distorted image. If the eye does not move it is because the brain is already used to an unfocused image. Although this is a good way to measure the misalignment it is not the best. Since there is not quantitative way to measure strabismus, the physician is only able to diagnose based on what they see. When I asked a fellow about this they said that these movements are very hard to see which can make it difficult to determine in the cases that the strabismus is fairly minor.
The hardest part of observing pediatrics was observing the kids that were scared. Some were scared of the doctors themselves, others were scared of the instruments, but most of them were scared of anything that came close to their eyes (mainly the drops). It seemed that about 85% of the kids did not want their eyes dilated. When this happened they would scream and cry, some even kicked their legs in retaliation. Since they did not make it easy for the physician to put the drops in it resulted in the kids being restrained by their parents and/or other medical professionals. This was so hard to see. I felt so bad for the kids whenever this happened. All I wanted to do was to help them but this wasn’t possible because they needed the eye exam in order to make sure everything was ok. This usually happened in little kids (about 6 and younger). I think it was because they really do not understand what was going on like the older kids do.
Furthermore, the younger kids could not perform all of the eye tests easily. The main test they could not perform well was the typical eye chart test. When they are really young they do not know all of their letters or are to shy to communicate what they see very well. Due to this the doctor do not always get the most accurate prescription for their glasses. there is a test they do before hand that allows them to get a general idea on what the prescription should be but it does not mean that this test is the most accurate. Often after they do the preliminary test they fine tune the reading in order to get the correct prescription, if the kid does not know the letters they do not do well. In some cases the family is sent for with some worksheets with the letters on them in order to practice. This works better when the child actually sticks to practicing everyday with the letters and helps the exam go much smoother.
Although pediatric ophthalmology is hard sometimes it is still a very interesting field of ophthalmology. It’s even a great experience when the kids cooperate and have fun with the doctors.
Let’s Be Surgeons!
Julie Wagner Blog

On our last week of Ophthalmology Dr. Sugar gave myself and my partner Mike a surprise. We went to the simulation laboratory on the first floor next to the general eye clinic not knowing what to expect. To our surprise we enter a room filled with practice equipment for medical students, residents, fellows, and whoever wants to improve their skills. The room itself was large and spacious and not to mention dimly lit (mainly cause no one turned the lights on).
Dr Sugar gave us a quick tour of the place. There are rows microscopes that are used in the actual surgeries at each station as well as a platform for the doctors to have a place to practice on. We were informed that the students could practice on research tissues or a model.
One very amazing piece of simulation technology was a virtual simulation machine. This device allows the user to practice most surgeries that will be performed on the eye in this hospital. The system breaks up each surgery into smaller portions that helps the user practice individual skills in addition to the entire surgery. Each time you practice you are tested based on how well you handle the microscope, surgical instruments, tissue handling, efficiency, and if you completed the objective of the particular practice simulation or not. At the very end a score is tallied up and lets you know how well you did.
Myself and Mike were able to try our own skills out. The test we had was to put red block around the edge of the cornea into a wire basket they had in the middle of the eye. This was to simulate the first part of a cataract surgery. Our first couple of attempts were bad…. After the first try we realized that while we are performing the surgery there is a comment line at the bottom of the screen that lets the user know what they are doing wrong in real time. For instance we got a lot of the “do not hit the lens” reminders as well as “close the instrument when leaving the eye”.
We treated this exercise as a bit of a competition and I would like to say that I caught on a little faster then Mike did. My advantage was being right handed while Mike is a lefty. For me it was easier to hold the instruments and operate the simulation. For our last try I did amazing. I was able to finish in a rapid 22 seconds with what I thought was a good score. Before Mike’s last try Dr. Sugar came in and help Mike out with the instrument positioning and gave him some pointers to go along with it. Since Mike is left handed, Dr. Sugar made it a rule that he gets doubled the time I was able to complete the surgery in as a handicap. Sadly Mike beat me badly. He did take longer but his tissue handling skill was much more gentler then mine. I for one was shocked.
Although we were not in the clinic or the OR I gained a lot of valuable information and experience from this. I realized that surgery is more intricate then I could have imagined. The small incisions that they make do not leave much room for mobility in the eye. Also we were lucky enough to have a stable eye opposed to someone moving theirs in the operating room because they are uncomfortable. Most importantly I learned that eye surgery is not meant for me. It was fun and exciting but I do not think I am gentile enough for this.
Tiana Wong Heading link

I am Bioengineering student at UIC with a focus in Neural Engineering. I am extremely excited to participate in the Bioengineering Clinical Immersion Program. Join me for the next 6 weeks as I explore the Anesthesiology and Orthopedics departments.
Tiana Wong Blog Heading link
-
Tiana Wong Blog
Day 2: Jumping right in
Tiana Wong Blog

Tuesday begins with a brief anesthesiology lecture for the residents. Of course the lecture is at 6:30am. I mean, because why not? Residents are coming into the room in scrubs ready to start rounds once the lecture is over. And in the kitchen there are two beautiful pots of coffee just waiting for people to drink it. It appears that coffee is a requirement around here.
After the lecture, we head to the radiology department to prep for a surgery. Unfortunately, the surgery is postponed, but we still get to look at the set up. There are a great number of tubes, each one long enough to extend from the anesthesia machine to the patient beyond the lead panels. Lots of tubing appears to be a norm for surgery, I’m more surprised that the anesthesiologists are limited to a single cart for their supplies and drugs, and their machine. While prepping before the surgery, calls had to be made to get some missing supplies from a different floor. Although it seems like an inconvenience, there is not enough free space to fit much more in the room.
In search for an awesome find, we find a cardiovascular oblation patient who is ready to be intubated. This time a video assisted laryngoscopy (VAL) was performed. For some reason, the tube does not pass the vocal chords, so the process is repeated with the standard laryngoscope. The tube still doesn’t pass and the doctors must perform an airway rescue. The anesthesiologists work to ventilate and wake the patient. While people rushed to prepare for an awake fiber optic intubation, the patient woke up, consenting to the procedure. The patient was absolutely amazing, completely understanding the need to do the procedure and even cracking jokes. After the tube was inserted, the patient was anesthetized once again.
Ten o’clock rolls around and we head back for more coffee. After the pick me up, we head to the OR. We head first to see a neck dissection for thyroid removal. The doctors use an EMG to alert the surgeons when they are too close to nerves and vocal chords. When the muscle is touched a deep beeping noise goes off. The surgeons purposefully test this before incision and during the surgery. There are four people standing around the patient during surgery, two with headpieces for magnification. With so many people around I was constantly nervous that someone would trip over the tubes or wires. Everyone calmly maneuvers around with ease, because obviously, unlike me, they have done this before. Still afraid of tripping, we stand on a stool far from the wires watching the surgery. Watching the surgeons dissect and remove the thyroid was fascinating, but had me holding my neck by the end.
We leave the neck dissection to see a CSE (continuous spinal epidural). The CSE is an epidural procedure that inserts a catheter that allows pain relief when needed. The diameter of the epidural needle is one over the length in inches of the needle! Honestly, looking at the needle was intimidating enough. This doctors begin by first inserting a nerve block where they intend to place the epidural. The epidural needle is then inserted until there is no resistance, the spinal needle is fed through it to puncture, and is removed to insert the catheter. With the catheter in the space, the epidural is removed, and the catheter is taped to the patient. After the catheter is in place, we take off for the day, prepping for another early start on Wednesday.
Epidurals
Tiana Wong Blog

The first time watching a CSE (continuous spinal epidural) I felt uneasy and freaked out. There was a huge needle being pushed to the patient’s spine until the doctor felt a “loss of resistance”. That’s not vague at all. If the doctor pushes further, the epidural turns into a spinal tap and can produce a spinal headache due to loss of CSF. It appears that the only way to be good at performing epidurals is by continuously practicing.
Even then, those who have been in the field for years can also have difficulty with such procedures. Anesthesiologists use surface landmarks and spinous processes to determine the location for the epidural. After cleaning the location, the doctors feel for the process and numbing the area. Once again checking for the spinal processes, the epidural needle is placed. Depending on the location of the spine, the angle of the needle insertion must be different. We had seen a case where a CSE was being placed in the thoracic region. Due to poor landmarks and the patient leaning to the side, the epidural needle did not properly pass the ligament all the way. After several attempts of placing the needle, the catheter was placed and the patient was taken to surgery. We asked the anesthesiologist why the procedure was so difficult and she stated that for patients with no distinct landmarks, doctors have to depend solely on the spinous processes. In areas of spine where the spinous processes are pointed downward, it proves challenging to get the correctly angle for the needle. With larger patients, patients with curved backs, or any patient that moves during the procedure this process becomes even more difficult.
Julie and I were able to use the epidural simulator that residences use to practice epidurals and spinal taps. The extremely high tech simulator was a plastic lower back and butt with a tube inside filled with water. We were told to search for two spinous processes so that we could place the epidural needle in between. The goal after was to successfully pass through the ligament, which would supposedly crunch like if I were walking on sand, until there was no more resistance. So, after inserting the needle about 2cm inside the back, a tap-tap-advance technique was used. To check for loss of resistance, two taps are done using saline and an air bubble in a hub and then the needle was advanced slightly. Instead of busting out the saline, we settled for air. It worked just fine for our experiment. This technique is done until there was both a loss of resistance and the drug easily leaves the hub. Afterwards, the spinal needle was inserted. This needle unlike the epidural needle has a pencil tip with a hole in the side to allow drug to enter the system. But since we were practicing a CSE, we added the spinal needle and then inserted the catheter. Using a very sophisticated push catheter- pull needle technique, the CSE was complete. For our next attempt to become anesthesiologist, we placed a spinal needle between two spinous processes and advanced through the tissue. The spinal needle is much thinner and moves more easily than the epidural needle so it was difficult to ensure that it was going in a straight line. We continued to push the spinal needle through the ligament, feeling the crunch, until there was a slight loss of resistance. This was a lot less subtle than with the epidural needle, and I really had no idea when I needed to stop. After the loss of resistance, we were to push a little farther until there was resistance once again and puncture. When the needle was in the correct location, water (actually CSF) comes out of the needle where it is collected.
My thoughts throughout this experience included:
“What exactly am I supposed to feel?”
“Is this far enough?”
“Did I just paralyze my patient?”
“Was that a loss of resistance? Oh wait, nope; have to keep going”.
To imagine that before this simulator there was no way to practice epidurals is absolutely horrifying. Do not sign me up. One suggestion to improve the simulator was to make the feel across the tissue and ligaments more realistic. Apparently, giving an epidural to a patient, if they were completely still like the plastic model, is easier than performing one on the simulator. The simulator also does not take into account the movement of patients, especially those in pain. Other suggestions included using catheters with pressure gages or ultrasound to determine where in the spine the doctor is so that there would be less error.
Oh My Eyes
Tiana Wong Blog

So far in our anesthesiology rotations Julie and I have had the opportunity to see numerous surgical cases. Whether the cases were brand new to us or if they followed a similar procedure as another case, they provided a new experience. In medicine it cannot be stressed enough that each person is different; therefore, even if the end goal is the same, the way to go about it may be different. Even the same procedure on the same person can have variations. For example, one patient was having a procedure for the third time and the amount of anesthetic needed to put them asleep was significantly higher than his other two procedures. While it may be simple to predict how the procedure may go, nothing is for certain.
On Tuesday, we had the opportunity to view two cataract surgeries back to back. There were a few commonalities between these cases. Both used a topical regional gel anesthetic that comes in a tube and is spread around the eye. There is a temporary loss of sight when this gel is used. Thank goodness. This method is used for regular or simple cases. Another option for regional anesthesia is to insert a nerve block at the corner of the eye. If the patient is an adult and has no problem, it is best if the procedure is done while awake. Anesthesiologists need to be prepared in case the anesthetics do not work properly. They can give more sedative, give pain medication, or perform general anesthesia. At least the patients are awake to notify the surgeon. The surgeon requires that the patient does not attempt to strain their eyes during the procedure, which could cause delays in order to prevent accidents. I would like to avoid imagining myself in that situation so I need to look into some preventative measures for cataracts soon. Cataract surgery is an outpatient surgery. So after the procedure is done, patients are sent to recover and go home as soon as they can.
The first case used a laser to detect the location and thickness of the cataract. The machine then gives the parameters to the surgeon. The laser cuts a cylinder in the cataract with four pieces. This allows for about 40% of the surgery to be performed outside of the OR. The patient is then transferred to the OR where the topical anesthetic is used. The surgeon then makes small incisions to the eye and removes as much as they can of the cataracts. An emulsifier is then used to remove the rest of the debris from the eye. This machine was pretty awesome. There were three functions that were operated using a single foot pedal. The first provides fluid to the eye so that it maintains its shape, the second function “eats”/ vacuums the soft tissue, and the third function uses ultrasound energy to break down the soft tissue. After the surgeon removed all the debris, the lens was folded up and inserted into the eye. After the lens was unfolded, the surgery was done. The second case did not receive the laser treatment in the beginning so the procedure was more invasive. Extra incisions were made to insert hooks to keep the iris open during the surgery. The cataract was broken down slowly and shaved away until the cataract was gone. This surgery had more tools and we got to see the different tips that could be used with the emulsifier. The surgeon continues to break down and remove the cataract and then the lens is inserted like the last case. Very thin sutures were used on this patient.
Can We Do It?
Tiana Wong Blog
As technology continues to progress, there have been discussions about using technology to perform certain medical jobs. As other groups have mentioned, it seems as if there are certain roles, such as interviewing a patient that could be done using a computer. While in theory this seems like a logical improvement to the medical field, this topic is quite controversial. These discussions have been brought to various specialties including anesthesiology.
There are various benefits of automating some of the processes in the anesthesiology field. One example of this would be the use of machines to automate the administration of anesthetics. This could reduce the number of people within the operation room; therefore, reducing the chances of contamination. Using medical history and comparisons to similar patients would help decrease the “trial and error” nature of general anesthesia while allowing the anesthesiologists to focus on other cases that are more challenging or require a person to perform them. People who are pro-machines have said that by training a non-anesthesiologist to perform the tasks of the anesthesiologist as preparation for the surgery, a lot of money could be saved, and the doctor could work on other cases.
The thing with anesthesiology is that there are many factors to take into consideration before anesthetizing a patient. While after some time a nurse may be able to situate a patient in proper sniffing position to incubate a patient, or place catheters on the patient, the drug administration portion of anesthesiology is very important. It is also extremely important to remember that despite prior medical history or other patient files, a patient could require more or less drugs for sedation. For a GI procedure we saw, one man required 4 MACs before his procedure started. At one point the patient burped and moved (but didn’t wake up), and one more MAC was given. Firstly, the patient’s records showed that the patient has not always needed such a high dosage of medication. If after administering the first MAC, the GI doctor or a nurse would have to get the machine to give another dosage. But at which point is there enough medication? Or is there not enough? These questions can be easily answered when the anesthesiologists are present. The GI doctor was a little nervous when the patient began moving. The endoscope was already deep within the patient’s intestines performing a surgery; there was no way to drop what he was doing to help sedate the patient further. Thankfully the anesthesiologist was nearby to quickly administer more drugs before more movement occurred. Another problem is that if there are no anesthesiologists in the rooms, if a problem such as the ventilator pump stops working or the patient is no longer breathing, there is no one in the room to quickly help the patient. When a doctor is called, there is still a few minute delay before their actual arrival.
There is also an issue with the empathy component of the anesthesia process. Before procedures, the anesthesiologists meet with the patient and review records. After explaining the type of sedation that the patient will have for the procedure, the anesthesiologist often walks with the patient’s bed until they reach the room. If needed, the anesthesiologist calms the patient, especially if the patient is nervous. By understanding the patient’s body language, the anesthesiologists are able to react and make the experience less painful for the patient. The interactions between the anesthesiologists and the patients are often understated and neglected while trying to improve the process. As a potential OR patient, I feel more secure with a person putting me to sleep than a machine. The machine might have accuracy, but it does not undergo the stress and pressure that anesthesiologist go through day in and day out as they put people to sleep, wake them, or even control their breathing process. I know that even if they might not remember my name at the end of the day that they still cared for my life and the fact that I woke up. For example, a patient who is nervous about their procedure would require more drugs to help them calm down. While a machine might be able to detect an increase in heart rate, anesthesiologists also have to quickly take into consideration the patient’s medical history before administering more drugs.
Apparently there are already machine prototypes that are used to aide in the general anesthesia process. The anesthesia machine provides the patient’s vitals that are taken into consideration when sedating the patient, which could be interpreted by a machine. However, taking into account how the surgery is going and the actual science behind anesthesiology requires more than a computer algorithm. While this seems ingenious, a lot of improvements need to be made.
So This is How It Happens
Tiana Wong Blog
So far this week has been all about the needles. Generally when I think anesthesia, I automatically think ventilation tubes; however, anesthesiologists have to be pretty handy with a needle. As we followed different anesthesiologists in the past few weeks, we have seen various nerve blocks, epidurals, and even a few arterial lines. Sometimes the process took a matter of minutes. Other times, we watched as the anesthesiologist continuously tried to find the right location. It was not only a matter of the anesthesiologist who did the procedure, but also the patient. Occasionally in the OR we would her the attending tell the resident something along the lines of “Well it took me awhile to get it, it wasn’t just you. They were a difficult stick.” With the relatively new technology introduced to the field, such as using an ultrasound to determine where the needle is located inside of the patient, you would imagine that everything would be smooth sailing. However, all this new technology still requires lots of training.
To practice being anesthesiologists we used simulations. The first one that we tried allowed for us to practice extracting from the subclavian vein and internal jugular vein. We had seen an internal jugular vein catheter inserted in a surgery awhile back and it looked relatively straight forward. Before we even took an ultrasound of our own internal jugular vein. Depending on the patient’s position the vein would either expand to a giant circle or lay flat like a pancake. So we get to the simulation and the only thing that helps us identify the vein is the apex of a muscular triangle. So inserting the needle, not too deep and off to the side, we pull back the syringe. You are aiming for a blue liquid to come through the syringe, which means you got the vein. Red liquid means that you stabbed the artery. If nothing comes into the syringe, you haven’t hit anything. If air comes back, it is possible you punctured the lung. So after a punctured lung or two, I managed to get the vein! This was definitely a lot harder than I was expecting. During the surgery that we watched the anesthesiologists didn’t use an ultrasound to help them, which I find really impressive. Apparently, only those are not confident in finding the vein or if faced with a patient with no landmarks do they then use ultrasound. The subclavian vein was even harder. No ultrasounds were used here. On this simulation, ultrasounds have terrible resolution and it’s better to find the vein based on landmarks. There should definitely be better simulations for residents. I’m sure that real patients are nothing like muscular chunks of plastic. For the subclavian vein, you have to find the curve of the clavicle and go underneath it until you reach the blue liquid. If you go too far, then you’d probably hit the artery. So this was a little easier in my opinion, but I won’t be trying to do this again anytime soon.
So we moved on to practicing ultrasound guided nerve blocks. Before ultrasound, these blocks were done blindly. Patient feedback would be used to determine if the correct nerves were blocked. Now with the ultrasound, anesthesiologists are able to see where they are putting the drug. We have seen various nerve blocks since we started our rotation, and the process is never straight forward. First, different patients have different ultrasound resolutions. There were two patients back to back that needed a block in the same area. The first patient had a very blurry ultrasound and it was difficult to see the nerve. However, the next patient had such a clear ultrasound that even I could differentiate the different layers. After finding the nerve, the next hardest task is knowing where your needle is. The needle needs to follow the centerline of the ultrasound probe in order to register on the screen. The trick is to keep the probe steady and advance the needle. If the needle bends, then the tip of the needle is lost and you have to find it again. There are also false tips. It means that you think that your needle is in one location, but it actually further down. We had to check this by moving the needle back and forth ensuring that the tip that we saw was actually the tip of the needle.
Although these simulations and ultrasound guidance has made regional anesthesia easier, it is a difficult specialty and needs lots of practice. Hopefully more technology will come around to make the process simpler
A sad goodbye
Tiana Wong Blog

The past three weeks were spent primarily in the OR observing different procedures from various specialties. By the end of the third week it felt like we had seen everything that we could see and were ready to become anesthesiologists ourselves. However, in search for fun things to watch we were able to discover things that we had not seen before.
We were able to watch a mandibular facial reconstruction. The patient had part of their jaw removed previously due to cancer. During this procedure more of the jawbone was removed. The medical company was able to 3D construct the patient’s bones and plan where the metal and replacement jaw would go. Previously, during surgeries the surgeons would have to use tongue compressors to make measurements and bend metal. Now, the metal comes pre-shaped and the types of screws, where they are located, and how the bone is cut is planned ahead of time. These plans were placed on the wall in the OR. Whenever there were questions with the surgery, the surgeons would either defer to the wall or ask the company representative. One team of surgeons worked on extracting the fibula while the other worked on the jaw area. Once the fibula was extracted, it was cut with a shape guard to ensure an accurate cut. The bones were then placed above the metal on the jaw to remodel the jawbone. The fibula was used as a bone donor because apparently we do not really need our fibulas to walk…
Since all of our time was spent in the OR, I had never though about what occurs when a patient is experiencing chronic pain. At UIC there is a pain clinic that helps these patients by either providing the refills that they need to relieve the pain or giving them a steroid injection. In the cases that we saw cortisone was injected into the patients’ area of pain. For one patient, they injected the cortisone near the peripheral nerves on both sides. The other patient received the injection as an epidural. The procedures are very short and are performed in a small room. There is a desk, procedure table, monitor, x-ray machine, and cart in the room at all time. The patient is led to the room by one of the doctors and asks about the pain that the patient is feeling. Once the patient enters the room, the x-ray technician stayed in the room with the patient and talked to them. I felt that rather than leaving the room this made the patients more comfortable before seeing the doctor. Once the anesthesiologist comes in, they ask the patient once again about the type of pain they are feeling. Afterwards, x-rays are taken of the patients back while the doctor is in the room. From there, the spinal area of cortisone injection is determined. The x-ray is left near the patient to help the doctor place the needle in the correct location. This requires changing the angle of the x-ray to constantly. When the cortisone is being injected, a live scan is performed so that the anesthesiologist can monitor the distribution of the steroid. There is still pain after the procedure, and it takes a few days for pain relief to begin.
The pain clinic also makes lesions on pain causing nerves. We didn’t get too see this performed, but hopefully one day I will. I was surprised by how many procedure cancellations there were at the clinic. There was a long list of patients that the clinic sees for the entire day. Many of the patients were refills, which doesn’t require an elaborate procedure. However, there were still several procedures that were scheduled to occur that never showed up. Considering that these patients are experiencing chronic pain, I thought that they would definitely show up to relieve them of their symptoms.
I have learned so much in the past few weeks in anesthesiology. I really appreciate Dr. Edelman and entire anesthesiology department for showing us around. It was truly an amazing experience I won’t soon forget.
Starting Again
Tiana Wong Blog

This week began my orthopaedics rotation. During the first rotation a few groups discussed that they enjoyed being able to see the interactions between patient and doctor. While I was able to get glimpses of this before the patients were anesthetized, it was never to the extent of the other groups. Going into orthopaedics, I was excited to finally experience the clinical aspect of the hospital that I had missed during my anesthesiology rotation.
The first afternoon was a little rough. Some people seemed confused that new engineers had shown up instead of the old group. I feel that this is a problem that several of the groups have faced during this clinical immersion program. Dr. Chmell, the attending we followed Monday, is a hip and knee specialist. In the few hours that we were in clinic we were able to watch the doctors drain a patient’s knee, give cortisone injections, and watch “The Gel”. The gel, actually called SYNVISC, is used for patients with knee problems, often osteoarthritis of the knee. First used in racehorses to increase their racing career, SYNVISC is marketed to cushion the joints. However, the gel actually changes the pH of the fluid surrounding the joint. The injection contains sodium hyaluronate which in theory will help the hyaluronic acid within the body. The doctor first locates the area of injection, clean it, and numbs it with “freezy spray”. The needle is placed and the gel is placed behind the patella. The injection is given one of two ways. The first way, the patient lies on the table and the area opens up. The needle is then placed above the kneecap and inserted towards the center from the inner thigh. The second way has the patient sitting on the table and the needle is inserted from the outside in. Both ways were painful for the patients, so it was really a matter of which way was the lesser of the two evils. In order to get the gel out of the syringe, the needle was big and so it was predicted that a lot of the pain comes from that. One patient complained that it was not necessarily the needle that hurt her, but rather the pressure from the gel once it entered her bad knee. While several patients received the gel injection, others prefer to stick with the standard cortisone steroid injection. Studies have not shown that there is a significant difference between the cortisone injection and the gel injection. In fact, some countries do not even offer the gel.
Monday afternoon was considered a slow day even though we got to see a handful of patients. I would like to see how this changes from day to day for the next few weeks. I enjoy the communication aspect of the clinic. For anesthesiology, we often met the rest of the surgical team and the anesthesiologist in the OR after the patient had already given consent for the procedure. In clinic you get to hear all of the patient’s concerns and questions regarding their conditions and/or procedures. Sometimes of their thoughts spark curiosity and others just make you laugh for hours. I can’t wait for the next few weeks.
Surgery Day
Tiana Wong Blog

Ossama and I just finished our first week with the Orthopaedics department. While most of our week consisted of observing the attending in the clinic, I think that it is safe to say that we were both excited to see the surgical procedures. Thankfully, Thursday we were finally able to go to the OR. I was looking forward to seeing similar surgeries to those we saw patients in clinic recovering from and scheduling. I was surprised to find out that although orthopaedic surgeries are invasive, patients are allowed to leave as soon as the procedure is done and go in for a follow-up within a week. Because of this, I was really excited to see a few procedures and possibly see the follow-up the next week.
Although I have had the opportunity to spend a lot of time in the OR with anesthesiology, the experience was still extremely new. After arriving in the OR at 7, we got to watch a total knee replacement in progress. The doctors had just used a knee align device that ensures that the leg is positioned properly and not at an angle. From there, there was a lot of hammering, sawing, clamping, and drilling.A trial knee replacement, both the femoral and tibia components, was placed on the knee. The doctors then bent and straightened the leg and moved it from side to side. The movement seemed very rough on the leg but it was necessary to check the fit of the knee replacement. The entire process to check the fit of the prosthetic was very rough and repetitive. If the replacement wasn’t the right size or the shifting of the knee was not normal, corrections were made and checked by moving the leg over and over again. Once the correct implant was chosen, the doctor tells the medical vendor the sizes of each of the implants. The vendor has a pretty good idea of what kind of knee replacement that will be used but in case the implant size changes, there are a variety of implants in the room ready for use. The cement is mixed and applied to the patient’s knee. The implants are placed inside and the patient sutured up. During the procedure, the vendor said that there were different types of knee replacements for men and women. The knee replacements for men were narrower than women knee replacements. Since people have different bone structures and frames, these characteristics have to be taken into account when considering the knee replacement.
During the course of the day we were able to watch a few surgeries. The digital nerve repair and cupital tunnel release surgeries were very fast, taking a little over an hour at most. The nerve repair procedure was interesting since it utilized an absorbable implant tube to guide two ends of the digital ulnar nerve back together. However, the most impressive surgery in my opinion was the hand reconstruction. The patient had rheumatoid arthritis. Her hand and fingers were bent in various directions and angles, not allowing her to be able to use them. The procedure consisted of the doctors replacing her metacarpals with silicone transplants. An incision was made across the knuckles and one by one the knuckles were removed and holes were drilled for the implant to connect the fingers and palm. As each metacarpal was removed, the prosthetic size was determined. After all the fingers were prepped and measured, the doctors checked the sizing of in the trial implants one more time. The actual implants were installed in the patient’s hands and motion was tested. In order to straighten the hand some more, suturing was tighter on one side of the hand than the other. This helped to straighten out the hand instead of allowing it to go in different directions. While suturing the patient, potato starch powder was sprinkled at the incision site. I would really like to know about the reasoning behind this.
Overall, I wish that we had more OR time. In clinic there is not a great deal of technology, especially in comparison to the OR. While I feel as if I better understand the clinical aspect of orthopaedics, the surgical aspect still has a lot that is explored. I feel that at least one more day in the OR a week would allow for a more in depth analysis of the technology used.
Clinic with a side of clinic
Tiana Wong Blog

While most of our time in the orthopedic department is spent at University of Illinois Hospital, every Tuesday we follow Dr. Gonzalez as he does clinic at the Illinois Bone and Joint Institute. The first thing that I noticed about the clinic was the amazing view that overlooks the lake, museum campus, and soldier field. I immediately felt that this place was completely different from the hospital clinic. With only eight rooms available, only a couple of physicians were present to attend to patients. Unlike the university hospital where we see about 80 patients a day, we saw about 20. The schedule wasn’t extremely packed and there would be downtime in between spurts of cases for the resident to dictate.
The Illinois Bone and Joint Institute has orthopedic doctors in various specialties in different locations around Chicago to attend to patients. Like at the university clinic, we see a lot of knee replacement follow-ups, carpel tunnel follow-ups, broken bones, etc. So far in this rotation we have seen quite a few trigger finger case. Trigger finger occurs when the causing the finger to be stuck in the bent position and extremely painful to straighten. The tendon develops a nodule that can cause irritation to the sheath that provides a tunnel. This irritation can lead to inflammation and the tendon can no longer fit through the tunnel. The first line of treatment for trigger finger is a cortisone injection. This both numbs the hand and reduces the inflammation. If the condition does not improve then the tendon is released from the tunnel.
Another case that we saw the first week was cupital tunnel release follow-up. At that point I had no previous knowledge that this was an actual condition. On Thursday we were able to see the procedure for this. It occurs when the ulnar nerve is being compressed, much like the conditions of the more standard carpal tunnel release. After watching the diagnostic testing for carpel tunnel syndrome, I would like to observe the diagnostic process for cupital tunnel. No advanced technology is used to diagnose a patient with carpel tunnel. The doctor generally tests for tingling or numbness. First he taps the patient on the wrist to see if the patient gets tingling in the fingers. Then, he holds both arms out, hand facing down to see if there is tingling there. If there is, he generally gets the patient to stand up and bends their neck side to side. If there is tingling in the fingers when he does this, it could be indicative of a neck problem. If patients do not get tingling or possibly have lost sensation in their fingers, he uses a paperclip test. Using the paperclip that holds the labels to the patient’s records, he bends the paperclip so that there are two prongs. He then has the patients close their eyes as he places either one or both ends of the paperclip to different areas of the finger. If the patient’s condition is very bad, they begin to lose feeling in their fingers. For some patients, it is not until this test is done that they are convinced that they have carpel tunnel. The doctors may also send the patient to get an EMG. The problem with the EMG is that 10% of people with carpel tunnel have regular EMGs. In general, the diagnostic testing for carpel tunnel is very simple, utilizing the limited resources within the department, but also effective.
One thing that stood out to me the most during clinic at IBJI was the way layout. Each office had two or three desks for the different physicians at the clinic, although each time we have been there the other physicians are not. The patients are sent back to a room, which is located in hallway near at the end of the suite. After the resident attends to the patient, Dr. Gonzalez will look at an x-ray that is near the hallway if there are any or will directly see the patient and talk to them. When explaining the patient’s condition, he tries his best to explain the condition to the patient. Occasionally, he draws pictures to show what is happening to the patient. Other times, however, it is best to show the patient the x-ray. The patient walks into the hallway where there is a cart to look at x-rays. Now at the university clinic, there are 2 x-ray monitors for 22 rooms. Since all the residents and physicians have to share the monitors in order to check on their patients it is difficult to get time or room in the attending room to have the patients look at their x-rays. When I was a patient, looking at my x-rays helped me to realize how bad my condition actually was and later reassured me that things went well during the surgery. There is a reason people say a picture says a thousand words. When a patient is told that they have to undergo surgery, they are often hesitant or unwilling. Other patients are convinced that there are things wrong with their body that aren’t and want surgery badly. Being able to show pictures or patient x-rays could reduce the amount of time consulting with patients telling them that their knee is no longer good or that there is no real problem with their bones.
Learning New Things
Tiana Wong Blog

On Thursday we were able to go to the OR once again. This week three total knee replacements and one hip replacement. After having already watched a total knee replacement the previous OR day, we were able to observe more of the actual procedure rather than being lost in the environment.
The procedure begins by making an incision to the knee. Apparently different surgeons have preferences on the length and location of the incision, which was surprising because all the patients, even ones that did not have surgery at University of Illinois Hospital, seemed to have similar incisions. The patella is shifted and flipped to the side while the surgery takes place. Knee Align, a disposable device, is put on a tool on the knee that ensures that the cut that will be made on the bone is straight. If the bone is at an angle after it is cut, the bone has to be shaved down until it is leveled. Before, if the bone was uneven a wedge was placed under the implant to level it out. This method was ruled out several years ago due to shear stress. While Knee Align is especially useful to show the residents and medical students the ideal alignment of the knee before a cut, this tool is used by attending primarily to ensure accuracy. To ensure that the femur is aligned correctly, a rod is placed in the femur all the way to the tip to keep the leg straight. This practice is still used in many ORs. Over the years, and through practice, the alignment of the knee becomes easier and more accurate. The use of Knee Align, in our experience in the OR, is used to confirm the surgical decisions already made. Of course, not all surgeons use this device. I wonder if the use of Knee Align will become more popular with younger surgeons, much like the use of other new medical technology. I have noticed that the tools that are often used in orthopaedics are very simple and basic. The tools for surgery are similar to those of carpentry and the tools used in the clinic are also very simplistic. With training, even the use of some of these tools are not completely necessary.
One thing I noticed during surgery that I found interesting was the use of ARISTA. Last week I brought up the use of a potato starch that the surgeons put on the patient before suturing the outer layer of skin. At that point I wasn’t sure if the “fairy dust”, as some jokingly called it, was actually made of potatoes or if it was just another joke. This week I found out that the product is called ARISTA. It is a hemostatic powder that helps in the healing process for various surgeries. The powder helps with clotting during surgery. Once in contact with blood, the fluid is absorbed and turns into a gel type mixture. This is used as a precaution during surgeries before the tourniquet is taken off. I believe that this product is relatively new in the department based on how much it is talked about and how surgeons have told other surgeons to try it out.
The hip replacement surgery was a very quick procedure. After the incision was made, the entire implant placement process took less than an hour or even 45 minutes. Unlike the knee replacement surgery, it is much harder to watch a hip replacement surgery since it is not as exposed. A saw was used on the hip and the femoral head was taken out. The surface of the femoral head is supposed to be smooth. In this case, there was an indentation on the surface of the bone because the hip was collapsing on itself. The hip implant components include a hemisphere, a liner, and a stem. In order to create a compressed fit, there are drills that resemble the stem and the hemisphere that allow the bone to reach the ideal shape for one of the implants. Once this is done, the hemisphere is inserted at a forty degree angle. It has to be forty degrees and not more to replicate the natural physiology of the hip. After inserting the hemisphere, the liner is placed to prevent any metal on metal interaction between the implants.
I cannot wait to see what the next OR day has in store for us!
A doctor’s work is never done
Tiana Wong Blog
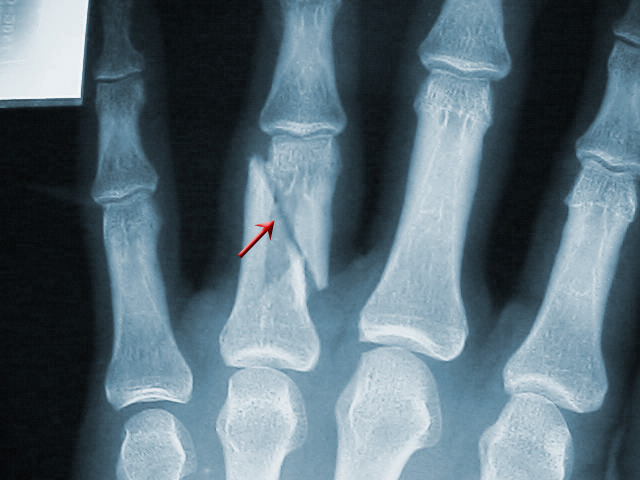
After two weeks in the orthopaedics department, and five weeks total in the immersion program, I thought that I would come into my final week well prepared and ready for what was coming this week. But I was definitely wrong. Compared to last weeks, this week’s clinics were jam packed with patients with various symptoms and ideas with how they wanted their treatment to be.
Monday’s clinic, albeit just the afternoon, was mostly filled with surgical follow-ups and older patients that were experiencing pain. What I noticed was that some patients come into the clinic with a problem, but have certain limits on the type of treatment they wish to receive. Whether or not their desired treatment option is available or not is a completely different story. While many doctors consider cortisone injections as minimally invasive for joint pain, some patients do not agree. While many patients seem more than satisfied to accept physical therapy as a treatment option, others request pain medication. The complication that I have seen regarding medication prescription is that not all patients understand the rules that the physicians must follow in regards to prescription. While it is sad to see patients in pain, the physicians cannot risk their licenses. I think that it is important that some level of health care informs patients about such specifics, their privileges, and constraints.
Going back to patient desired treatment, patients with carpal tunnel are often hesitant to undergo surgery. One would hope that a pain in the wrist or tingling of the fingers would have a simple solution, but this is not the case. For these patients, there is no real in-between period. Doctors always want to ensure that surgery is not performed when it isn’t needed, so they perform diagnostic tests, ask for history, and order for an EMG to be done. Unfortunately, physical therapy does not help since their symptoms arise from the compression of the nerve by the ligament. The doctor does not tend to push towards surgery until the patient begins to lose feeling in their fingers since this could put the patient at risk for injury. While this is more of a doctor directed problem, it would be great in order to improve patient satisfaction and quality of life.
Last week on Thursday, we were only three knee replacement and one hip replacement surgery. After Tuesday’s clinic, we reached a total of 10 hand procedures to be performed this Thursday. Hand surgeries are much shorter than total joint surgeries so having ten procedures is normal for these surgeons. The patients that were added to the schedule on Tuesday were cases in which the risk of complications increased the longer the surgery was put off and since our mentor will not be available the following week, they had to be scheduled. A few of the patients that we saw were cases in which the patient had put off their appointment because of work scheduling, improper diagnosis elsewhere, or denial of injury. One case that stood out to me was one patient who was screened at a physical therapy location to see if their finger was fractured or not. They were given a splint and told that their finger was only sprained. After several weeks, the finger did not improve and patient still experienced pain. Coming into the clinic, the patient’s x-rays showed that they had a dislocated fracture that was beginning to heal in place. In order to go about fixing the fracture, the surgery will most likely include rebreaking the bone, aligning them properly, and pinning or screwing them in place. At this point even I had to agree that a proper diagnosis cannot be made without an x-ray.
Between scheduling conflicts and patients thinking that they didn’t injure themselves too badly, patients can go several months without seeing a doctor. If the patient waits too long, the risk of the procedure increases or the procedure may not be performed at all, which could cause more problems done the road.
Time For Goodbye
Tiana Wong Blog

After a rather slow second week, our last and final day in the orthopaedic department was spent watching a multitude of surgeries. It was probably the best ending of a rotation that I could have asked for. The first surgery was a hip surgery. It was interesting to see how different surgical “teams” interact with each other. By changing just one of the members in the team, the dynamic within the OR is completely different. Regardless, the operation passed quickly with no complications. The second surgery was a carpal tunnel and a DeQuervain release. I was extremely exciting to finally see a carpal tunnel release surgery after hearing how simple it was from the people from the last rotation. The incision for a carpal tunnel release is no longer than an inch long at the wrist. Once the incision was made, a cut is made to the ligament and an endoscope is used. The endoscope had a single camera, this made it difficult to see if it got dirty, and an extremely bright light so that the doctor can see where the scope is when inside the wrist. When the scope is far enough to decompress the nerves, a blade is engaged and the scope is pulled out. The scope is reinserted into the wrist to ensure that the surgery was done completely. This entire process took twenty minutes.
I found the carpal tunnel surgery rather impressive in comparison to the hip replacement surgery. There was less technology to perform the surgery, but it required more attention to detail. This was only proven further when a nerve repair surgery was performed on a child. Previous nerve repair surgeries appeared difficult enough to perform when done on an adult. However, my favorite surgery overall was the tendon repair. Not only did it entail a repair of the tendon, but pinning as well. This procedure was often referred to as a goalkeeper. The tendon had separated from the thumb and had to be sutured back together. There is a ligament that lies on top of this tendon and when the tendon breaks, the ligament shifts down. With the ligament moved down, the tendon cannot repair itself. The finger was pinned to ensure that the tendon was repaired straight and correctly. The ligament was then cut so that the tendon could be sutured first. The tendon rolled back on itself, so this was essential for proper healing. The ligament was repaired next. This was a complex surgery and by far the most interesting in my opinion.
I truly enjoyed my time in the orthopaedic department and this internship. In the orthopaedic department I was able to experience the clinical side of the medical field that I wasn’t able to see in anesthesiology. I learned so much about the medical field and gained an interest in industry medical device design. I hope to use the knowledge that I learned in this wonderful program next year in senior design and for all my future endeavors. This was a wonderful experience that I won’t forget!
