Students
Mohi Ahmed Heading link

I’m a Senior in Bioengineering that is participating in the Orthopedics and Hematology/Oncology rotations of the Clinical Immersion program. As an athlete and avid sports enthusiast, my future aspirations are to enroll in a Masters program in Bioengineering pursuing the regeneration of cartilage and/or improving joint-replacements procedures with stem-cell based therapies in an attempt to prolong an athletes career as well as apply the same methods to everyday people. The plan with this is to get involved with start-ups focused around this idea. Long-term I’d like to get involved in consulting for a variety of biomedical/bioengineering topics from biomechanics to failure analysis of biomaterials.
Mohi Ahmed Blog Heading link
-
Mohi Ahmed Blog
Go with the Flow [Ortho W1 1/2]
Mohi Ahmed Blog

Summary:
[Covering Tuesday July 5th and Wednesday July 6th; Dr. Marcus is the attending physician]
The immersion program started to the less-than-auspicious information that surgery for our first day had been cancelled. Instead, we would be going on a tour. After observing general facilities we got to explore the lab of Dr. Marie Siemionow–famous for the first near-total face transplant. In her lab we met with two of her PhD students/post-docs that detailed the projects that the lab is pursuing: nerve regeneration and chimera cell transplants. It was reassuring to see this lab uses complex science to solve complex issues with the same skills I learned last semester regarding stem cell and cell culture procedures.
Bright and early, we were treated to a lecture by senior residents and attending physicians on surgeries and images (x-ray, MRI, MRA, etc.) for residents to analyze and diagnose. Later, Dr. Mejia gave a lecture on hand surgeries with pictures
full of goregalore. The most startling part of this morning class was that different physicians had different opinions on how to handle a given scenario. What one surgeon considered the safest approach to a solution was someone else’s last resort. This whole time I thought that there was an overwhelming consensus on what procedure to carry out for all scenarios, but I now see just how unique certain situations can be and why surgeons would be conflicted on what procedure to carry out.Finally we got to observe the clinic at full speed. Essentially your typical doctor visit, but looking in from the other side (the clinicians perspective). It turns out there’s long wait times on both ends!–more on that later.
Notable Observations:
- Residents can spend 30 minutes or more simply waiting in the hallway for patients to arrive.
- Dr. Marcus needs to work around procedures and surgeries performed by previous surgeons for a given patient.
- There is a narrow room with computers on both sides full of residents and attending physicians that I have dubbed “Homebase” as this room is where every member of the clinic reports to multiple times for a given patient visit.
- Plenty of times throughout the day, residents, technicians, and nurses report to Homebase and simply wait for the attending physician because he is with a patient in a room.
- A medical student, resident, and Dr. Marcus all perform the same tests on a patient meaning they are visited ~ 3 times before any real progress has been made.
- The room goes dead silent when an x-ray or MRI is being observed by Dr. Marcus as everyone is awaiting his explanation and diagnosis.
- Red and Green flags are at each patient room to signal whether a patient has not been seen, is waiting on paperwork/files/braces, or has been/is currently being seen.
- Typical game plan for a patient is rehab/therapy –> steroid injections (inflammation and pain) –> surgery. [Stopping wherever problem is solved]
- After meeting a patient and determining the need for an X-ray, residents must file for an x-ray before a patient makes it to the front desk asking about their x-ray.
- Residents carry out dictation, a process where the resident orally summarizes the patient visit over the phone to a transcriber that types up the dictation and sends back to the resident for logging.
Thoughts:
Due to the lack of surgery experience, we have been limited to observing the clinic. It is either a blessing or a curse that our entire focus as such has been improving workflow. At first I wanted to address how a medical student, resident, and the attending physician all assess the patient in the same way before a diagnosis is given. However, I realized this is a hands-on learning opportunity that probably should not be imposed upon.
I noticed that everyone likes to view x-rays on a certain monitor in the middle of the already crowded and cramped “Homebase.” I again realized that although maybe not intentional, this allows mostly everyone to see an image that the attending physician is examining and explaining to residents–again it becomes a learning experience. My only thought here would be to optionally “Teamview” the image to all other monitors instead of having residents huddled around a central set of monitors.
Dictation is carried out in “Homebase” as well, and this area can get very noisy. Dictation itself is already very fast and hard to understand for the transcriber, but additional noise I imagine only makes it worse. Perhaps dictation could be carried out somewhere else?
I think a solution I could focus on is a means for residents and technicians to know where the attending physician is essentially at all times (in a more eloquent way than simply putting a bell on them).
A more in-depth look at improving workflow will take place in the second half of this week’s post.
The Wave [Ortho W1 2/2]
Mohi Ahmed Blog

[This covers July, 7th, and 8th; Dr. Mejia and Dr. Goldberg were the attending physicians]
Summary:
We finally got a chance to see the clinic part of the work week run by other physicians and compare the differences between them. Surprisingly, there was not actually much of a difference. Under Dr. Mejia however we were introduced to a new workflow concept he had been attempting called “Wave Scheduling.” We learned that there are a few main types of patients: follow-ups, post-operations, new patient, and workers compensation. Essentially they range from brief conversations with the attending physician up to hour-long interactions with multiple procedures. Wave scheduling is the act of scheduling multiple follow-ups together around the same time, followed by one or two appointments of the longer variety. The result is the ability to see ~6 patients per hour and a pulsating flow of activity in the hospital; Dr. Mejia will be running around the clinic for a burst of time and then have ~10 minutes to stop and tend to other things before the next wave of patients come in. Apparently, other attending physicians are not fond of adapting this new style of scheduling. Thanks to Dr. Mejia, we also met with Jonathan Bode who is more or less in charge of scheduling and workflow in the hospital–among other things. He too was able to provide us various insights from a more administrative end of hospital operations. Lastly, we saw the stark similarities between how the hospital appears to run under either physician. I personally got to see a dislocated finger get put back in place with the help of x-rays and a cast being applied. I also got to see the administration of a numbing agent (commonly called a “Popper”) followed by the administration of a steroid injection to reduce pain in the hand of a post-op.
Notable Observations:
- A patient had an MRI that clearly showed a herniation and the attending physician recommended an injection, but the ER physician that addressed this patient determined that it would be ineffective and refused administering the injection. The attending physician at our hospital took another look at the MRI and saw again that there was clearly a herniation and could not figure out why the ER physician refused to administer the injection he recommended.
- For Spanish-speaking patients, the sole Spanish-speaking resident is assigned to handle the patient for obvious reasons until Dr. Mejia can himself.
- On a given day there could be twice as many residents as patients and also the opposite–we saw both occur in this week alone.
- There was no available face mask in a room when a patient requested one as they did not want to spread the common cold they were currently afflicted with.
- Dr. Mejia has to ask which resident saw to a certain patient.
- Stack of papers for Dr. Mejia to sign are left on his desk, unbeknownst to him, until he inevitably returns to his desk.
- For casting, the fiberglass with impregnated resin simply requires water to activate. However, it leaves a sticky residue on the gloves of whoever is administering the cast and requires them to be very careful where they put their hands unless they swap gloves.
- According to Jonathan, there is a need for a same-name signifier as two patients with the same name administered at the same time is not entirely uncommon.
- If a patient comes in having needed x-rays and this is not discovered until a resident talks to them and then gets sent to get x-rays, that patient has taken up a room for over an hour that could have gone to someone else if they had just been sent to get x-rays from the beginning.
- Dr. Mejia personally numbers doors with magnets to adhere to his wave schedule–if he messes up, the entirely system crashes until the next wave starts and he can reset the order.
- Jonathan has a team dedicated to to studying the time it takes for patients to come in and out of the hospital taking into consideration the attending physician and their specific patient classification.
Thoughts:
If the front desk has access to the records of an incoming patients, they should be able to determine if the patient has x-rays in the system or needs them so that they can be sent to get x-rays first before unnecessarily taking up a patient room.
There has to be a better way for Dr. Mejia and his wave schedule to avoid him personally having to change numbers on doors.As a team, we will look into this and plan on scheduling an outside meeting with him to pitch the schedule. Our solution should go hand-in-hand with the research study the Hospital Improvement Team plans on carrying out.
Perhaps a different resin can be impregnated into the fiberglass casts such that they do not leave a sticky residue on latex gloves. Latex gloves are cheap, but this impact could add up over the years to save money long-term.
I eagerly await Week 2 where we finally will observe surgery and see if we can notice anything notable there.
Slow it Down & Look Outside [Ortho W2 1/2]
Mohi Ahmed Blog

[This post covers July 11 and 12; Dr. Chmell and Dr. Gonzalez were the attending physicians]
Summary:
This week started off with Dr. Chmell in clinic where 1/3 of his patients did not show. This resulted in a relatively relaxed day for basically everyone. Dr. Chmell explained to us that an understated issue in Orthopedics is that certain people have an allergic response–usually delayed inflammation–to metals such as the one’s used in implants. A test to detect this allergic prior to operations has not come into full fruition though a few have tried. This issue occurs for a small percentage of people, but that does not mean it is a hurdle that can be overlooked.
The next day was our first visit to the scenic Illinois Bone and Joint Institute (IBJI) with Dr. Gonzalez attending. Compared to the normal University of Illinois Hospital clinic, this was a completely different experience. Essentially, all patients were post-ops (patients checking in their progress after undergoing a procedure recently) and there were not many patients in general to be seen. This resulted in an extremely auspicious circumstance where Dr. Gonzalez had time to give us two lectures on the human hands from an anatomy/surgery standpoint and also an engineering (biomechanics) standpoint. Furthermore, in between patients he even had time to intermittently educate us on small details in the field, his experiences, and advice, Overall, without the rush of a high volume clinic, both Dr. Gonzalez and his resident had time to spare in being more attentive and social with patients.
The view was worth the wait anyway.
Notable Observations:
- With a lower than anticipated volume of patients, residents are left with basically nothing productive to do for more than an hour.
- Very few hand sanitizers in the IBJI clinic relative to the University of Illinois clinic.
- The IBJI clinic has more sophisticated flag system (includes room order like Dr. Mejia’s magnets and also includes whether or not an injection or x-ray is needed). However, this system is rarely used in a sophisticated manner, the flags correspond to the order patients came in–not their classification (post-op, follow-up, workers compensation, or new patient).
- There is only one resident at IBJI compared to ~9 at University of Illinois Hospital depending on the day.
- Where special cases arise, Dr. Gonzalez uses is experience to make a call on how to go about modifying an implant to meet the new needs of the given special case. There is not an objective analysis that an be done in a timely manner; Dr. Gonzalez creates a model of the unique region he is attempting to implant into and decides how much to modify the dimensions and angles within an implant to accommodate the special case.
Thoughts:
It is my guess that there is less hand sanitizer at IBJI because it only really needs to be in one place and can still be efficiently used before and after seeing a patient whereas at the University of Illinois clinic this would be impractical as too many residents would be in need at the same time. This must be an advantage of a low volume clinic.
Again, the low volume of patients at IBJI is likely the reason the advanced flag system used is not fully implemented as there simply is not a need for it at IBJI whereas there might be a need at the University of Illinois Chicago clinic.
I noticed a dramatic difference in patient enthusiasm and response in at the IBJI vs what I have seen at the University of Illinois Hospital. This could potentially be due to the nature of appointments at IBJI compared to those at the high volume University of Illinois clinic–to confirm this I will need to compare it to the clinic run by Dr. Gonzalez tomorrow at the University of Illinois. The aforementioned low volume likely is the reason the attending physician could spend more time with a patient in a non-rushed manner and this is probablywhy patients seemed more upbeat. However, I would like to stress again it also very well could be due to the nature of their appointments as opposed to those at the other clinic and is very unlikely due to be dependent on the residents and attending physicians themselves. Again, this will be made apparent in tomorrow clinic with Dr. Gonzalez as the attending physician with an expected 60-70 patients scheduled.
Not sure if Surgeon or Very Specialized Engineer… [Ortho W2 2/2]
Mohi Ahmed Blog
[The following is about July 13th and 14th; Dr. Gonzalez and Dr. Marcus were the attending physicians, and Dr. Gonzalez was the surgeon on the 14th]
Summary:
We officially cycled through all attending physicians in clinic. This may or may not actually be true, but it seems that residents are not as lost when looking for Dr. Marcus or Dr. Mejia. This is simply an observation and may only be true on a given day and not generally true. It is at this point we have generally seen what weeks are typically like in clinic for the residents and attending physicians. We finally got to see surgery and wow was this a completely different experience. We started off by seeing a cyst get removed from a wrist which was a rather quick surgery. This was followed by a knee implant revision which was rather long (several hours) and then two knee replacements (arthroplasty). The last scheduled procedure was a hip replacement, but Dr. Gonzalez said it would be a long night if we stuck around for this and recommended we go home as it was already past our official “end” time. To briefly summarize my thoughts on surgery, and intended solely as a compliment, there is a point during fitting, adjusting, and installing knee replacements/revisions where it appears Dr. Gonzalez is not even a surgeon anymore, but rather an incredibly specialized engineer. It is as if he is just building a joint and installing it into a machine.
Notable Observations:
- Name tags on rooms are swapped out every morning depending on who attending physician is–for physicians such as Dr. Marcus this means the rooms he uses change a lot to the point that he has a special set of rooms he likes to use when he can to stay away from clutter and traffic.
- Suture removal is not worth numbing and pain depends on where sutures we embedded.
- There are times where there are a lot of residents waiting for patients, but everyone is still behind schedule.
- Residents do dictation every 3 to 4 patients. If done more frequently than that they are not seeing as many patients as they should; if done less frequently than that they do not remember the patient well.
- Special printer needed for printing prescriptions because of special paper.
- During surgery, the table the limb is on can move when bumped during sudden motions and can interfere with delicate operations.
- Metal prong/spoon to hold skin back must be held by someone.
- Extensive procedure undergone by those who “scrub in” to work very closely during surgery including lengthy sanitation prep and more materials worn to avoid spread of disease.
- During surgeries involving the knees, residents spent a lot of time just holding the leg up and moving it around for whoever is actually operating.
- Tools covered in blood slip out of hands during surgery.
- Delayed plate arrival seriously interfered with surgery.
- Rare, but still happens: gloves are hard to get onto the recently sterilized Dr. Gonzalez even with assistance.
- Relaxing music playing in the background during operations.
- During knee implant revision, cement used to put implant in must literally be hammered/chiseled out.
- Operation table cannot go as low as operating personnel would prefer–eventually end up using stepping stools.
- Sales representative from company that manufacturers implants is present to tell Dr. Gonzalez how to combine pieces to get what he wants and everything he needs to know about every component.
- A lot of guess and check for fitting knee implant in before making a final choice and permanently implanting.
- Dr. Gonzalez mixes cement to implant knee–someone else mixes a second batch as a reference for time until the cement dries.
- Extra IV drip bag used to hold cords up so nurses can walk under safely when cover is not available for them to placed on the ground.
Thoughts:
Perhaps a system can be in place where cords connect from their respective machines and then run along the ceiling (or say a hook hanging from ceiling 6.5 ft from ground) to the wall where they plug in that way they could be walked under but still reached–this assumes most of the machines do not need to be moved in and out of the room a lot.
I think Dr. Gonzalez’s work would be made easier on knee revisions if he had a compound that would liquefy/dissolve the cement of the previous operation so the cement could be sucked up instead of taking up time being slowly chipped away.
Perhaps a brace or locking mechanism could hold a patient legs in place temporarily instead of having a resident hold a leg for hours. This would have to be easily disengaged to move the leg around as needed.
Maybe tools could have a revised handle/holding point design to make it easier to hold when covered in blood. The metal prongs/spoons used to hold skin/muscle back could have a means of being secured to the table so that more hands are free and arms are not in the way of those operating.
I eagerly await the next and final day of surgery and hopefully I can I see a hip replacement like I wanted to. Surgery has definitely been the highlight of this experience thus far.
Winding Down [Ortho W3 1/2]
Mohi Ahmed Blog

[This post covers July 15, 18, and 19; Dr. Gonzalez was the attending physician]
Summary:
The orthopedic rotation is winding down. UIH (University of Illinois Hospital) clinic is getting very routine. Obviously the cases very, but it generally is composed of the same observations. We have begun work on our presentation and report about our observation, what we have learned, and what we think could be done. We also attended the Illinois Bone and Joint Institute (IBJI) for the last time and had a busier day than the last week. The patient volume was slightly increased, but the mood was still very relaxed relative to UIH clinic. I especially am excited about our final day observing surgeries as many different types are scheduled and this will be my last chance to see these procedures unless I am on the receiving end of it.
Interesting Thoughts:
- x rays are at one clinic, but not the other for a certain patient and must be sent over.
- x ray at IBJI has security feature that locks screen if a resident/technician/attending is not near.
- Dr. Gonzalez has patients call him to touch base with how they are doing.
- Cyst can only be removed when full, if drained must return before surgical removal–procedure is quick and takes a few days to heal.
- Cyst fluid can be thick and is difficult to remove, bone starts growing as well which needs to be shaved to prevent it from coming back. However, patient can refuse this and opt for repeated draining.
- Resident writes additional notes on each patient’s file and carries them with throughout the day until they can be transcribed via dictation (audio recording of patient interaction and details of diagnosis).
- For severe osteoarthritis, a certain amount of steroids can be used, but cannot exceed use in a given timeline. The alternative at this point is an injection of what is essentially synthetic synovial fluid into the joint.
- There are multiple injection sites in the knee.
Thoughts:
Up until now I did not even consider the existence of synthetic synovial fluid. Apparently the injection is very general, essentially all of a given dosage is injected into a joint. There is really nothing precise about it, but perhaps it does not need to be. It’s as simple as entering an appropriate location into the joint and dispensing the fluid.
Most of these days were routine so my final thought is an afterthought on Dr. Gonzalez following up with a patient via phone call. With insight from Dr. Chmell, our group thought of designing an app as a means of patients being able to easily interact with their doctors. The idea would be for post-op patients to get the app and essentially update their doctor and milestones they have achieved since surgery to determine if they are on track. The idea would be to eliminate unnecessary appointments that only involve 30 seconds of interaction to say something along the lines of “everything looks great, see you in 6 months.” Also it would provide doctors with data on how long after surgeries patients are achieving certain milestones such as walking again, climbing stairs, etc. This way, doctors know if a patient should come in sooner because they are not progressing as fast they should. This could help patients come in sooner rather than later if something is wrong.
I eagerly await my final day observing surgery–there is a lot of hand procedures scheduled along with hip procedures. I will be getting a great mix and be able to compare the similarities and differences of procedures to different areas of the body.
The End of Ortho, But There’s Still More To Do [Ortho W3 2/2]
Mohi Ahmed Blog

[This post covers the last few days of my orthopedics rotation; Dr. Gonzalez and Dr. Goldberg were the attending]
Summary:
We experienced a couple more hectic days in clinic at the University of Illinois Hospital (UIH) followed by our last day in the OR with a plethora of surgeries lined up: anterior and posterior hip arthroplasty, endoscopic carpal tunnel release, knee fusion, and several other hand surgeries. Overall in clinic I saw most of the same, delays for everyone caused by little nuisances that added up. Specifically, the clinic was backed up for at least an hour because 4 consecutive patients had to be sent to x-ray–and that was for just one resident, let alone the other patients from other residents. Getting sent to get x rays continues to clog up patient flow and is what many residents told me they’d like to get resolved. In only my 2nd and last time in the OR for orthopedics I saw multiple compensations that were not present the first time–more on this later. Clearly, there’s still more to see.
Interesting Observations:
- several patients had waited weeks after their initial injury and had made their situations much worse because of it–the afflicted area had healed improperly.
- A hip replacement where the patient was already able to comfortably walk and around and even dance just 4 weeks post surgery.
- Implants for surgery arrived well before start, but the company representative was not available and therefore surgery could not start on time–no point in equipment being there if it cannot be used by company rep.
- Lead vests and neck covers (for protection from radiation) are simply placed on a couple of racks throughout hallways. Lead vests can be taken at will, many neck covers missing.
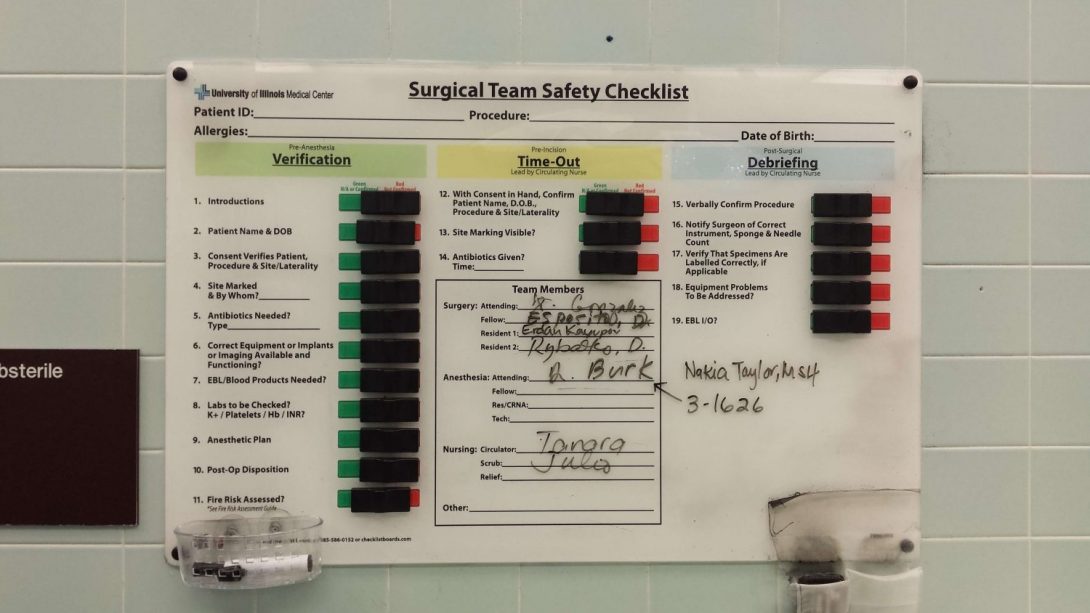
- Checklist procedure followed before, during, and after procedure to ensure right operation is happening.
- Equipment counted before and after operation to ensure nothing was accidentally left inside patient.
- Lots of equipment in the OR is on wheels and actually makes components difficult to move when other pieces of equipment are in the proximity. (Chairs and IV bags getting stuck together at the base because of how the wheeled-base is designed.
- no potentiometer for light on endoscope–because of lighting in OR, the available light is too bright.
- power supply for endoscope lights up tubing when in use.
- final drill guided by a guide-wire from previous, smaller drilled-hole.
- x ray guidance used when something like a pedestal (bone growth) is in the way of drill.
- Bed was in the way for a lot of x rays and required the x ray to be repositioned several times. This becomes increasingly difficult when a patient has a large leg as well.
- Doppler device used to audibly hear blood flow into area that was previously under tourniquet for blood flow restriction.
- Prep for an OR is essentially wiping down everything and disassembling operating table when a new one is needed. After one surgery, prep took 40 minutes.
- x ray covered in plastic wrap that protects the x ray from getting blood on it, but also makes it hard to see around and the covering wrap routinely gets in the way.
- special table was developed for certain operations that lets a nurse rotate legs and move them around without moving other parts of the patient or simply holding these body parts up themselves.
- Extra plastic shielding was used everywhere when the room needed special protection from blood (work-arounds seen here as well, described later).
- During surgery, an x ray of the ankle was needed while the leg was straight and elevated–because of the x ray, this required a resident to essentially hold up the leg with their sternum so as to get out of the way of the x ray.
- hammering pitch increases when a component is fit into proper place (components hammered into place).
Thoughts:
As far as delays go, addressing the x ray back up in clinic appears to have the most impact on patient flow.
A potentiometer in equipment involving a light in my opinion should be the standard as conditions from OR to OR can vary.
Lead vests could definitely be better designed to shield the user, but also not be as uncomfortable to wear for extended periods of times. Furthermore, a simple checkout and return of lead vests/neck guards could be implemented so that shortages do not occur at critical times.
I do not have all the facts, but perhaps when equipment for a surgery arrives it could be sent to the OR it is needed at with or without the company rep. What I saw was that the equipment for a surgery was in storage and unable to be moved by other people to the OR simply because the company rep was not there. When such a delay occurs a company rep must arrive, go to where the equipment is located, and then bring that equipment up to the OR causing further delay. If the equipment was already at the proper OR, time could be saved. I am uncertain as to how often this happens and if this type of delay is typical as I have seen other equipment sitting ready at the OR prior to surgery.
These plastic wrappings around x ray equipment could definitely be redesigned and vacuumed sealed as they otherwise obstruct the view of the surgeon and residents on top of just being in the way:
There could potentially be an extension added to surgical tables or something hanging from the sealing to attach covers onto when extra shielding from blood is needed instead of this:
Overall, if anything my last visit to the OR taught me, it’s that I have seen a lot these past few weeks, but there is definitely more to see and more that can be improved than just what I have noticed.
Rotate 180 Degrees Onco W1 1/2
Mohi Ahmed Blog
[This blog covers the first few days of the radiation oncology rotation; attending physicians are Dr. Koshy and Dr. Howard]
Summary:
This week specifically covers radiation oncology as hematology/oncology is potentially the next two weeks. We began observation of an entirely new department with a new group this week. We got a rundown of the typical happenings in this radiation oncology clinic and what to expect; we saw a few patients and attended some extra discussions. We experienced some hard talks to family when dealing with cancer and got to see just how tech heavy this clinic is compared to orthopedics. Overall, we got to see just how much contrast there was compared to the previous rotation.
Interesting Observations:
- The term for new patients is “consults”
- This clinic deals with planning radiation treatment, the diagnosis of cancer is usually a few weeks old by the time a patient is sent to radiation oncology.
- This entire clinic deals with coming up with a thorough and customized plan if radiation treatment is the designated means of treatment.
- Molds are used so that as a patient comes in for their daily treatments of radiation, they are lying down in the exact same position as every other day of treatment.
- Consultation takes 1 day and then planning (which usually takes a week more) cannot start until insurance is taken care of (usually a few extra days).
- Interestingly enough, in most cases there really is not an economy to treating patients a week sooner or later (according to the literature).
- CT, Pet, and MRI scans used extensively whereas Ortho used x rays and–to a lesser extent–MRA’s almost always.
- Treatment is done via a complicated software and an even more complicated machine. Essentially a tumor is seen on a scan, a resident will draw in on all relevant “slices” of the scan the boundary of the radiation. They will also include an additional few cm’s expansion of the original trace to include cancer cells that are beginning to spread, but are not appearing on scans. Finally an additional expansion is put in to account for movement of the patient.
- The residents plan of action is then reviewed and edited by the attending, this new plan is then double-checked that the plan will not make the robot possibly impact the patient while trying to target the tumor or other perceived issues.
- Finally, a team of physicists will look at the plan to ensure that the goal is being achieved and that the goal is feasible in the first place–if not the plan is edited again.
- Overall a plan takes a week per patient’s radiation treatment.
Thoughts:
I simply cannot get over how different a clinic this is compared to Orthopedics. First of all there’s 10ish patients a day as opposed to 60-80. Each patient encounter or talk is far more intimate than a quick 30 second follow-up. Whereas the tools and techniques in orthopedics can at times seem medieval, I was genuinely made to feel that in radiation oncology the devices and treatments are truly space age material.
I may as well be at NASA or CERN or Fermilab. Or at least it feels like it tech-wise.
We have seen a few areas we think we could improve and I will expand upon this in the next blog post. Pictures are coming.
Hint: It is notpatient flow.
Why Do You Put Up With This? [Onco W1 2/2]
Mohi Ahmed Blog

[The following covers the latter part of my first week in radiation oncology; Dr. Koshy and Dr. Howard are the attending physicians.]
Summary:
After we saw the brachytherapy of a tumor we were shown a sterilized toolkit used to spread open the human vagina and deliver a dose of radiation to tumors in certain areas while minimizing surface toxicity to surrounding tissues. Brachytherapy essentially involves a wire being strategically placed near a tumor where it can then deliver a radioactive isotope and then withdraw that isotope after the allotted treatment.Upon examining this tool, we noted complaints the residents had of using this device as it spreading mechanism and assembly appears flawed. It is difficult for the residents to lock the device into a certain position. Furthermore, it is uncomfortable for the patient as a certain component of its spreading mechanism pokes the inner thigh of the patient and is evidently very uncomfortable. To combat this outcropping piece and also make sure the tool holds properly, the residents wrap tape around this section. The disappointing part is that this tool is fairly recent in design.
Furthermore, during this brachytherapy, in order to keep radiation away from the thigh, the wire where the isotope travels through is kept away from the legs with just some sheets/padding with the intention of using the inverse square law to their advantage. At first I thought this was a significant workaround the residents were performing, but it almost appears as though unless the tool itself is redesigned, this problem is not economically worth solving with some kind of holding mechanism.
We also got to see a patient get radiated as a means of compromising the patient’s immune system and degrading the bone marrow in order to be more accepting of a relative’s bone marrow transplant. This procedure was essentially placing the patient in a secure room, blasting them with radiation of a specific dose and at a certain distance away for a certain time as they lay in a glass box. Blocks are strategically placed around the patient to trick the computer software into thinking the patient is shaped like a perfect rectangle to ensure no area of the subject is missed.
We also sat in on a Cerebral Spinal Fluid tumor board meetings. Like the previous tumor board, this meeting brings physicians from any related area regarding a tumor so that its treatment can be agreed upon by consensus. For example, a tumor in the brain requires that radiation oncology is present alongside neurosurgeons and other specialists to truly determine what the best course of action is for a given patient. This is only possible because of the low patient volume. However, some patients can be addressed at all if certain specialists are missing or if whoever is to be presenting the patient is unavailable. This happened a to certain extent at the meeting we went to and if it was any worse, there most likely would have been no point to the meeting in the first place.
We also got to see the translating service IVAN in use and simply put: it’s terrible.
Notable Observations:
- Ivan translator, press a number if language is not commonàgets outsourced to another translating service with same dialtone and again asking for common languages àselect uncommon language again àget connected, immediately disconnect and need to restart completely before finally getting a Ukrainian translator. Essentially the first 9 languages for the hospital’s translating service and the outsourced one is the same yet this is not taken into account when the call is outsourced.
- Login in time for residents is a redundant process that takes a full 2 minutes. This login is done fairly frequently as the computer logs out during the duration of each consult. There can be approximately three consults an hour which is 6 minutes spent logging in per hour. Over the course of an 8 hour day this ends up being ~48 minutes a day spent logging on to a computer through a very redundant process. This process involves signing in to several locations through software in order to have access to the next/current patient’s entire file and scans.
- The aforementioned spreading tool used with radiation has caps at the ends to prevent radiation build up. These are tan plastic caps that insert into a grey metal tube. They routinely get lost and are hard to see due to their lack of contrast.
- In consulting rooms, there are curtains used for what I assume is privacy if a patient needed to change into a gown. This curtain is position so that it can cover half of the room when fully opened. The location of the track these curtains follow however goes from a patient chair to the exit door. When not in use, this curtain always gets caught in the door.
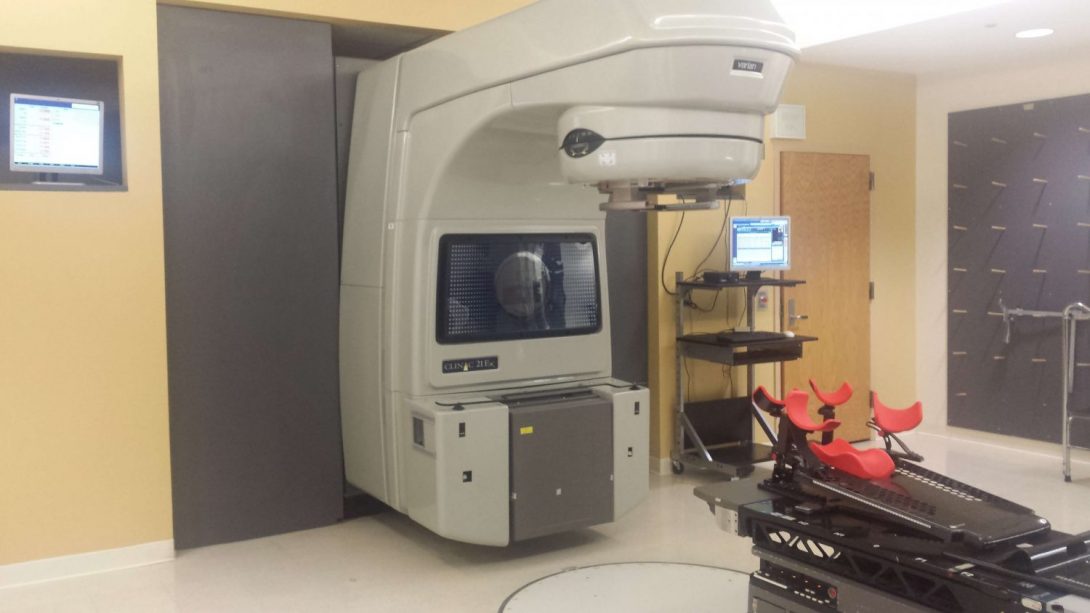
- The room with the linear accelerator has a vault door and lead shielding built into the building. The radiation cannot be turned on if the vault door is not closed.
- For radiation oncology, residents and the attending physicians spend a lot of time looking at different scans as they search for tumors and whether or not they have metastasized. They look through a human slice by slice and also sometimes inject a dye or a substance that shows up on scans to track if a certain fluid is moving where it should or if sugar is being metabolized where it should. I noticed that both the attending and residents spend a lot of their day scrolling due to the nature that the images are taken in slices.
- The scans are observed a large greyscale monitor. Why this monitor is in greyscale is unknown.
- Some scans are meant to be in color, but are again viewed on a greyscale monitor such that the high and low ends of the images color scheme or both dark grey—these scans require that the resident or attending view the images on a different screen.
Thoughts:
I’ll have to ask an attending next chance I get as to why these monitors so routinely used for scans are only in black and white when one fairly common scan, specifically of the brain, needs to be in color.
I believe the aforementioned tool used to treat tumors throughout the female reproductive system is flawed and rather than attempt to fix something in the clinic as a whole, this is one component that is routinely used that our group could improve upon significantly by modifying the tools functional mechanisms. This too is another area we will potentially focus on improving. Monday begins the start of a related rotation through hematology/oncology. I will have to compare the two rotations to see if there’s a better focus for the group to pursue. However, I will have to return to radiation oncology as I intend to interview the final people in the radiation therapy planning: the physicists.
[Author’s note: This post is missing pictures, they will be uploaded tomorrow].
Red Blood Goes In, White Blood Cells, Red Blood Cells, and Plasma Come Out [Onco W2 1/2]
Mohi Ahmed Blog

Summary:
This week so far has left me dazed. After a quick week in Radiation Oncology we’re now with Hematology Oncology with various physicians and events to observe. I plan on returning to Radiation Oncology to interview the physicists and see their role in the radiation plan.
Thus far we got a crash course on hematology oncology specifically with leukemia and bone marrow transplants and got to see white blood cell collection and the machines used to accomplish this as well as the cell counting and freezing procedure for this inevitable transplant. Tomorrow I believe we will actually observe a transplant.
Notable Observations:
- Autologous bone marrow transplants is the transplantation of one’s own bone marrow. The initial collection is done right before chemotherapy which then destroys the remaining bone marrow. The collected bone marrow stem cells are then injected back into the original host. This bypasses the need of having a donor and the chance of rejection. Under certain conditions, an allogeneic transplant is still required and sometimes will be done if there is only a half-match between the donor and recipient.
- There is a 25% chance a sibling can be a donor to another sibling. In this case, this allows the chance of the only transplant procedure where the patient takes in a new immune system.
- The Graft vs Tumor effect is that donor cells attack a host’s cancer cells because they are viewed as “foreign.” The risk is that these donor cells also can go on to attack other cells in the patient’s body known as the Graft vs Host disease.
- Chemo doses are periodic in nature because a strong dose would completely destroy the bone marrow and potentially kill the patient. Chemo must be dosed and then allow the body to heal before taking another dose.
- New blood collection devices can continuously uptake and separate blood into its cellular components (red, white, and platelets) whereas not too long ago this was an interval process.
- For cryopreservation this lab uses a controlled rate freezer to purposely cool a collected sample by 1 degree Celsius a minute (varying) before ultimately freezing with liquid nitrogen to -180 degrees Celsius. This is done to avoid damaging the sample.
- Two machines in the lab use disposable kits that require a new kit perpatient. One kit for one machine requires an expensive reagent putting the kit’s price at around 4,000 USD and the other machine has a kit that routinely costs 300-500 USD.
- Companies that manufacturer these devices stop supplying the kits when they create a new device to force hospitals to buy their new device and respective new kits.
- Sample is counted multiple times throughout collection and freezing; if anything goes wrong they can look back at what part of the process caused an error.
- The lab is evaluated by an outside company that essentially sends them a sample to analyze and compares their results to predetermined values.
- Navigating through insurance is a common topic in meetings for nearly every single patient.
- 7-AAD is a nucleic dye used in this sample collection and stains dead cells which are important to account for when prepping a sample for transplantation.
Thoughts:
I am left feeling devoid of deeper thoughts; a major portion of the lab procedure and environment for cell collection, counting, and storing is something I am already very familiar with.
Keep in mind it’s only been a few days, but compared to radiation oncology, we have only seen the surface of a variety of different fields so I do not even have an inkling of a potential innovative space.
That being said, our schedule is packed this week so there’s still so much more to see.
Clinic & Chemo [Onco W2 2/2]
Mohi Ahmed Blog

Summary:
Towards the end of our week in Hematology Oncology we got to see the clinic run by Dr. Rondelli as well as the contiguous chemotherapy infusion clinic. This observation period was split in half by our group of 4 where we had two of us alternate between the two clinics as a means of tracking observations throughout the entire day instead of isolating them to a given time period.
Under Dr. Rondelli, I personally saw the follow-ups for routine bone marrow transplants as well as the rarer haplo-donor transplant. The haplo donor is used when options are limited and the donor selected only matches “half” the markers for an ideal transplant. These usually do not work as well and are likely more symptomatic afterwards–but they may be the only possible treatment.
We also viewed how a chemotherapy clinic is run by following the lead nurse in charge of infusions and scheduling. I saw blatant troublesome areas making this nurse’s life more difficult, but it appears among the frantic nature of clinic this nurse would rather just work with the problems presented instead of spending extra time looking for a preventative means.
Notable Observations:
Hematology Clinic:
- Majority of hematology clinic patients are follow-ups (at least for this given day).
- Conversations with patients are very long and intimate.
- The ability to speak Spanish helps tremendously in terms of patient flow–this is likely specific to UIH and not general to all U.S. hospitals.
- Follow-ups continue well after procedure and a good outcome is achieved; the haplo-transplant patient was in for a follow-up nearly a decade post-treatment.
Chemotherapy Clinic:
- Head nurse has a main chart with room number and time as the X- and Y-axis respectively. This chart tracks what patient is in what room, is highlighted if treatment is currently going on, or crossed out when complete or considered a “no show.” Quite often patients need to be moved around resulting in arrows all over the chart making it more akin to an American football playbook.
- Chemotherapy sessions take at least 30 minutes; some sessions take over an hour and for these patients a room with a bed is reserved. When a patient is late, that entire rooms schedule is delayed.
- As an obvious work around, the head nurse bought themselves a kitchen timer for cases such as when a patient is not responding well to pre-chemo drugs and needs extra infusion time. The alarm is set and goes off alerting the nurse that the extended time is up and the patient should now be ready to actually start chemo.
- There are 9 rooms for chemotherapy. Only a few have beds which can be used for patients requiring longer infusion time. If the patient is immunocompromised or an inmate, they must be in a room alone. These limitations must be concerned when scheduling patients for the day.
- When a patient schedules a chemotherapy session, they are simply placed into a room without the aforementioned constraints taken into account. The head nurse then must reorganize the scheduling to meet the constraints the night before the day in question–hence the football diagram chart.
Thoughts:
I was told the reason for this chemotherapy scheduling conundrum is that if scheduling was taken into account up front, many patients would need to be turned away. Even after several clarifying questions, I still could not deduce why exactly this system was set up the way it was. I will attempt to truly get to the bottom of this.
It was interesting to see that the ability to speak Spanish was important enough that Dr. Rondelli made active efforts to speak it. Coming from an Italian-speaking background, it appears he has picked up on words and phrases over the years and then used is Italian background to try and fill in the gaps. I have seen physicians appreciating the ability to speak Spanish through other departments as well. This looks to be about keeping patient flow fast and at least in other departments all about avoiding using translator services.
“It’s All a Part of the Plan” [Onco W3 1/2]
Mohi Ahmed Blog

[Authors note: this is going to be an irregular post compared the previous ones focusing on radiation therapy planning. I finally interviewed the medical physicists on hand and now had a complete picture of the entire radiation plan.]
Summary:
Our time in hematology oncology is winding down and I thought this would be a good time to note the radiation therapy planning when a beam is needed (as opposed to brachytherapy which involves a guide-wire and a radioactive isotope). We’ve seen a variety of patients in a variety of locations during various points along the combating-cancer timeline.
Content:
When it comes to radiation therapy involving a beam, the idea is to use a linear accelerator which in simple terms fires electrons at tissue, dislodging other electrons causing the release of photons in the form of high power rays that purposely damage cancerous/necrotic tissue with heat. The amount of radiation is measured in Gray’s (Gy) and is a measure of Joules per Kilogram. The a lethal dose to the overall human body is as low as 10 Gy with serious complication and poor outlook with as low as 2 Gy.
A radiation therapy is put into effect for a list of cancers too large to list here. At first a resident goes through CT/MRI/MRA scans of and highlight areas of the cancer to be treated with the radiation. In general, tumors are targeted with much higher than the lethal dose of radiation such as 30 Gy simply because it can be localized to a target area and the volume being radiated with 30 Gy can be comprised of 30 beams each dosing 1 Gy each.
Next the attending physician looks over the contour plan and usually increases the volume given radiation to account for microscopic spread of the cancer not showing up on scans. Furthermore, they double-check that the beams will not be radiating vulnerable tissues.
Following that, a dosimetrist figures out what amount of beams, at what angle, and at what duration the radiation must be given to achieve the desired dosage to a given tumor. Quite literally this person figures out how to achieve the dosage to a tumor that the radiation oncologists want. The dosimetrist essentially runs the contour plan on a “phantom” AKA a dummy that matches previously done CT scans.
The medical physicists is the last cog in the machine. These people look at the plan, the dosage prescribed, and figure out if this is feasible. They make sure the machine will not accidentally physically damage the patient. The dosimetrist is technically a part of the physics team. With the dangerous nature of radiation, the physics end of the plan is entirely about double-checking everything. The medical physicists independently look at the dosimetrist’s plan to ensure that the calculations and plans are all in alignment.
This entire process takes an entire week. This may seem long, but when radiation is in use, it is clear shortcuts cannot be taken.
Kushal Basnet Blog Heading link
-
Kushal Basnet Blog
First Day
Kushal Basnet Blog

If I am going to be honest, I was pretty nervous coming into this program. I did not really know much about it and I am not comfortable going into things I don’t know much about. I did have some friends in the program, so it wasn’t all bad.
Waking up was pretty much the hardest part of the day. I was accustomed to staying up all night and waking up late, because it was summer time. I put that all behind and headed to orientation. My heart rate started to go up as I entered the innovation center, but my nerves calmed down after I saw some familiar faces inside the building.
The program started and it went as I was expecting it to until the guest speaker came in. The guest speaker had us do various activities to warm up things. Most of the activities were rather odd, but they did have some sort of a purpose behind them. There was one activity where we had to get into groups of two and one of had to play the part of a time traveler and the other had to explain to the time traveler what a cell phone is. The purpose of this activity, I like to think, was to help improve our communication skills. I soon found myself enjoying the orientation and was a little sad when it ended. The Clinical Immersion program had officially started and we were sent off to our rotations.
With my group of 4, I headed to the eye and ear clinical at UIC because I was placed into ophthalmology for my first rotation. We got to the clinical not knowing what to expect, but we soon found out Dr.Sugar, who is our clinical leader, is super nice and very willing to help. He showed us around the building and took us to each of the department of ophthalmology. The tour was very detailed and Dr.Sugar explained many of the equipments the doctors use at the clinic. He was also very much against the idea of taking notes during his tour, so I have to leave out much of the details. The whole thing took about 2 hours and after we were allowed to leave after.
My first day was full of nervousness and excitement , but I got though it and I found myself really enjoying my first day. I was so tired at the end of it I took a nap as soon as I reached home and before I feel asleep I thought about how much I am looking forward to the rest of the program.
The first week of Clinical Immersion Program
Kushal Basnet Blog
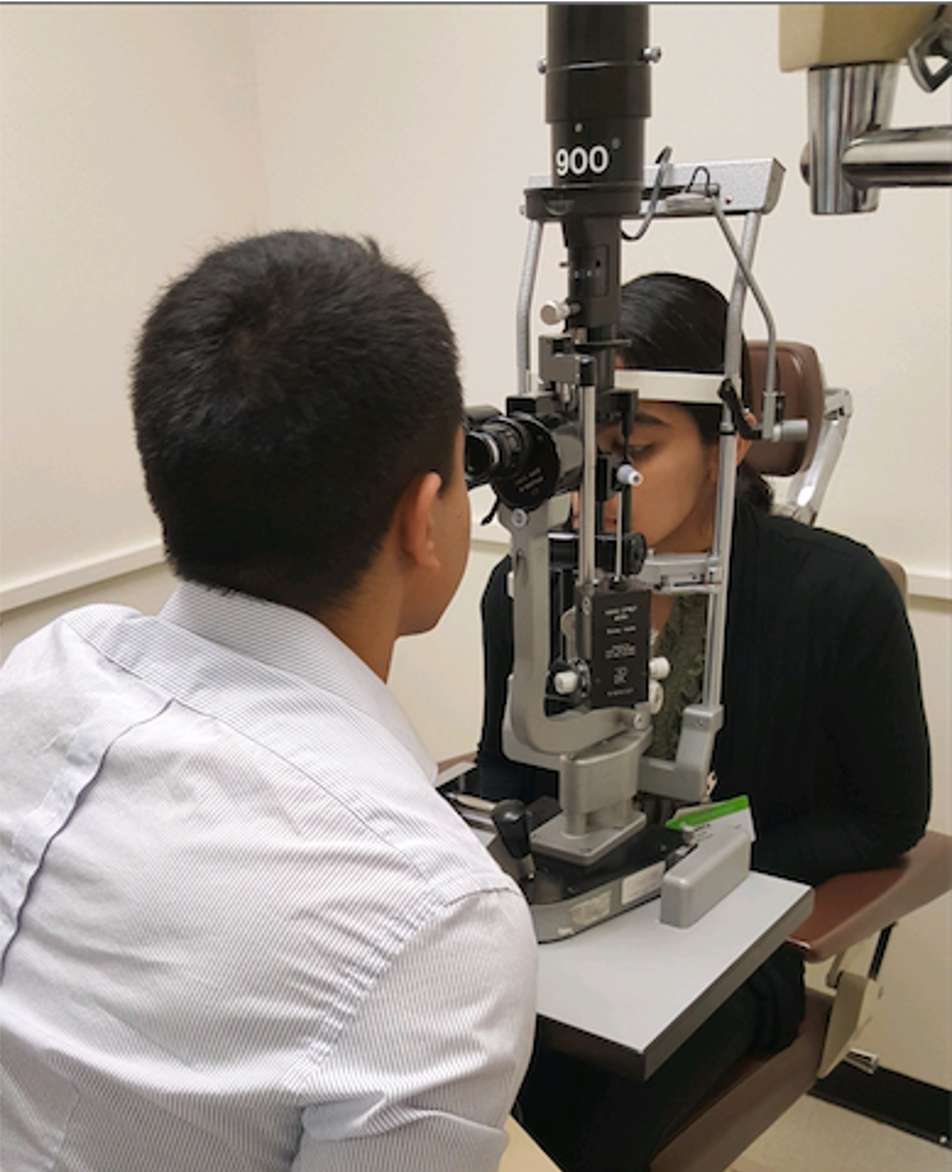
The next three days after orientation were rather hectic. I was put into the cornea department of ophthalmology with Dr.Sugar, who happens to be the head of the department, for day two of my internship. Before I go into detail about my time with Dr.Sugar, let me tell you that he might be the coolest doctor I have ever met. Most of the day I was in Dr.Sugar’s examination room observing the many patients that came in to get checked in. Almost all the examinations that Dr.Sugar did were through a medical device called a slit lamp, which is a lamp that emits a beam of light into the eye. This allows the doctor to view different parts of the eye and examine it for certain diseases and abnormalities. The slit lamp also has a side binocular; so multiple users can view through it. While Dr.Sugar performed examination of the many patients that came in that day, I got to view what he saw during the examination. It was a really exciting experience. I can’t go into much detail, because Dr.Sugar is very much against taking notes, but I ended up learning many new things. Most of the patients had cornea or lens replacement and you could see that using the slit lamp. If the patient had a lens replacement then a reflecting of light would emit from the eye when it was exposed to the light of the slit lamp. The whole day Dr.Sugar was very informational and sometime even threw in a joke or two. The whole day was a fun learning experience.
The next day my group and I had to go to UIC surgery to view different ophthalmology surgery that was taking place. I have never observed any sort of surgery, so I was looking forward to this. My group got a little lost inside the building, but we eventually found our way to the surgery floor. We got our scrubs and I got to try on scrubs for the first time in my life. They were not that comfortable to be honest. For the next five hours we watched Dr.Tu perform surgeries. He performed mostly cataract surgeries, which is a surgery to replace the lens inside the eye. The very first time I saw the surgery, I was mesmerized. Dr.Tu was very quick with his work and he would use all sort of tools to poke into the eye and replace the lens. While the surgery took place, I just watched the monitor tying to organize my thoughts. It was very interesting to say the least. Each surgery took about fifteen minutes and Dr.Tu performed six cataract surgeries. After the first couple of surgery it started to get repetitive, but it was still exciting to see how thing were done. At the end my feet were exhausted from all the standing, but I got to experience something that most people never get a change to see live.
The last day was a half-day, thank god. I was pretty tired from the entire week. I was placed into the department of retina with one of my group members, Sarita. The doctor we were shadowing that day was Dr.Chow and he was also very nice. It was a very busy day, so Sarita and I just ended up followed Dr.Chow around different rooms as he took on many patients. We got to talk to him only when he was done with a patients and it was only for a few minutes. There isn’t much to say about this day because it was very busy at the clinic and we did not want to get in the way of Dr.Chow. We did get to observe how Dr.Chow handled various situations in an orderly and timely fashion. This skill is very useful in the medical field. After the clinic was over Sarita and I met up with our other two members and we did a debriefing of our week.
The first week was very fun and informational and I look forward to the rest of the internship and blogs.
Week two
Kushal Basnet Blog
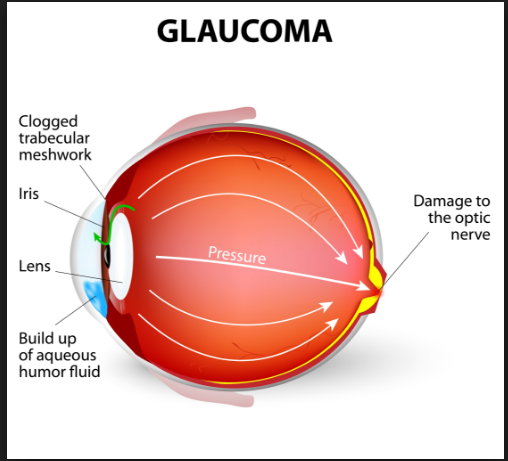
I was placed into the department of Glaucoma for my first day of week two. Glaucoma is damage to the optic nerve of the eye mostly due to high eye pressure. Dr.Sugar informed me that he did not have a set doctor for me to shadow in Glaucoma, so I basically had to walk around till I found a physician on duty. This was a daunting task because it was lunchtime and most of the physicians were out. I eventually came across Sofia, a technician, who allowed me to shadow her until one of the physicians was available. She was a bit skeptical about me after I introduced myself and told her why I was there, but she warmed up to me and was very willing to answer my questions. I asked Sofiaif she could identify any problems that she encountered in a day-to-day basis and she just started listing them all off. She was having problems with the slit lamp next-door, problems with her patients, and many more. I had only shadowed physicians before this point and after having met with the technician, I realized that talking to multiple personal, and not just the primary physician, can lead to better understanding problems that occur in and around the hospital.
After Sofia left, I started to shadow Dr.Wilensky and he was just as enthusiastic as Sofia about letting me know the problems he had. I didn’t want another long list, so I tried to limit my questions by asking him only his main problems. Surprisingly, patient compliance was a big problem. I wouldn’t think that placing eye drop was a big problem, but I guess it was. Many of the patients did not follow direction about the medication they were given, even when the instructing were clear. Dr.Wilensky said that as much as 40 t0 50 percent of the patients were not compliant and their recovery took a hit because if this. I spent rest of the day just following Dr.Wilensky around the clinic. I ended up with a long list of problems faced in this clinic and I was ready to come up with solution for each of them.
The following day was much more exciting than the day before. I was in the general eye clinic with Dr.Sugar. That day in the clinic was particularly slow because the old residents had left and the new residents had come in, so the front desk did not schedule many appointments that day. Dr.Sugar was doing a simple laser eye surgery today and I was really excited to see how that procedure worked. Unfortunately the machine was having a problem and we had to wait for the technician to come fix it. After an hour or two the technician found the problem to be some loose wires in the machine. I was a little surprised to see that such a small thing could lead to a big problem and that there wasn’t some notification on the machine letting the user know what might be the problem. After the laser was up and running, Dr.Sugar proceeded to use it on a patient. It was a fascinating process to observe. The laser was literally poking very tiny holes in the eye to remove small tissue. The patient didn’t feel and thing and the whole process took about 5 minutes. Dr.Sugar even let me use the machine to poke microscopic holes in a piece of paper, which was very cool in my opinion.
I identified many problems on the first two days of week two and I am looking forward to the rest of the week.
Code Blue
Kushal Basnet Blog
The OR is much different in real life than it is in the movies or T.V shows.
Dr.Sugar had made arrangements for our group to visit the OR this week. He wanted us to watch some pediatric ophthalmology and retina surgeries, so we can get the full scope of the department. We had gone to the OR last week, so it wasn’t anything new. My group didn’t get lost this time around and we made it to the surgery we were suppose to watch. The surgery that was about to take place was a Strabismus surgery, which is a surgery to fix a cross-eye or lazy eye. This was a routine surgery and the primary surgeon had done many, so it wasn’t very difficult for her. This operation was a two-man job, so there was another surgeon assisting with the surgery. The surgery started off great. The primary surgeon was singing along to a song that was playing and even teaching the resident how to perform the surgery. I was fortunate enough to get a spot right next to the primary surgeon, so I could see the full scope of the surgery. All the other surgeries I had seen were on a monitor, so this one was different experience for me. It was very strange watching someone dig into the eye with multiple tools and take things apart.
It was all very calm until the middle of the surgery. The primary surgeon heard a gurgling sound coming from the patient and asked the resident anesthesiologist to check to see if all the vitals were stable. As the anesthesiologist was checking the heart rate of the patient started to increase and the breathing stated to go down. The resident anesthesiologist realized that something was wrong and yelled at the nurse to get his primary attending. A code blue, which is an emergency, was called from the nurse and the room started to light up.
The patient started to flat line, so the primary surgeon and the other surgeon immediately stopped what they were doing and moved away from the patient. Ophthalmology surgeons are not trained to handle emergencies, so stepping away is the best option for them. Within seconds the room started to flood with other doctors and nurses. I made my way to a corner to get out of the way and was called out of the room by one of the doctors. The tension in the air was very high for the first few moments, because all the physicians didn’t know what was wrong. I was outside of the room and had no idea what was going on, but after a minute I could feel the tension fade away. Some of the physicians came out the room and the code blue was called off. It turns out the patient somehow was unable to breath during surgery, so his vitals started to drop. Thankfully at the end of all of it the patient was fine and the surgery was a success.
Something that I found interesting during this while situation was that even though the primary surgeon was a trained physician, there are times when even they must step away. Another thing to notice was the sheer amount of people that flooded the room after the code was called. I don’t know much about emergencies like this, but it seemed like there was more people in the room than that was needed. Most of the people were watching while a few were trying to fix the problem.
This week in the OR has been an eye opening experience and I still have another 4 weeks left to learn.
Second Last Day
Kushal Basnet Blog

Things have slowed down dramatically in the last week of this rotation. Most of the doctors in the Ophthalmology department are on vacation, so it is hard for Dr.Sugar to schedule us in with different departments. Thankfully I ended up getting placed into the Contact Lens and Oculoplastic department for this week.
I learned many things during my stay at Contact Lens. I shadowed Dr.Joslin, who was very friendly and was willing to answers any questions I had. That day I saw about 8 patients and gathered useful information from my observations. One of the patients that I observed didn’t find his new contact comfortable, but was willing to comply for the better vision it provided. The balance between comfort and function is an important aspect of engineering. After seeing this patient give up one for the other, it got me thinking about how many other patients have to do the same. Another patient that I observed was misinformed or not educated enough on how to put on his contact, so his contact ended up falling out and eventually broke. The lack of patient educating seems to be a prevalent theme in the hospital. It is mostly due to patient compliance, but there are certain cases where the patient really wasn’t informed on what to do. Coming up with solutions, like having a video instruction for each medication, could be beneficial to every aspect of the hospital. The rest of the day I observed many more cases and took notes of all the useful information that I could use to write my final report.
My time at Oculoplastic was more relaxed than Contact Lens. Raahil, who is a member of my group, and I were with Dr.Setabutr for most of the day. He was very intelligent and insightful on the problems he had. He was very busy so Raahil and I just sat around for most of the time, but every once in a while Dr.Setabutr would let us tag alone. One of the patients he was seeing that day had chronic muscle spasms in her eyelids, so she had to get 9 Botox shots around each eye. The patient also had to get those shots every 4 months. Raahil and I discussed potential ways we could help the patient. One thing we came up with was to create some sort of a device that has all the shots preloaded and with multiple ports. This way the patient only had to get one shot. We then spend the rest of the day identifying many more problems and trying to come up with solutions for each one.
I only have a couple of more days in this rotation and until it ends I will try to identify many more problems.
Overview of my first rotation
Kushal Basnet Blog

The past 3 weeks in the department of ophthalmology has been a great and fun experience. I learned various amount of things like the primary devices doctors use to examine the eye, how the hospital functions from an internal standpoint, and how surgeries operate. All of the doctors that I worked with were intelligent and they were excited to have me there. I got to experience things that most people will never get a chance to do.
The first week was a bit chaotic. I had never been exposed to the clinical environment, so I was very nervous going into the rotation. I started off in the Department of Cornea with Dr.Sugar in the first week. Dr.Sugar turned out to be one of the best doctors I have ever met. He was very helpful and very willing to answer any questions I had. He let me observe all the patients that he examined and taught me many things. Most of them were from the medical perspective, but he believed that learning things from the medical side would help me better understand the problems from the engineering side. The first week I also visited the OR for the first time in my life. As the days progressed through the first week, I adjusted better and better each day. I got used to being in clinic and by the end of the first week I had lost all of the nervousness that I came in with.
The second week was when I learned the most amount of information and identified the most amounts of problems. I was placed into the departments of Pediatric, General eye clinic, and Glaucoma. I gathered copious amounts of information from physicians and patients. Most of the problems had to do with ergonomics and patient flow. The devices that the physicians used were very staining to the body, which can lead to many physical problems in the future. Most of the patients complained about the wait time, but this is a universal problem. Things also got a little hectic in the OR. I witnessed a code and realized how stressful the hospital environment is.
The last week of this rotation slowed down by a lot. Most of the doctors were on vacation, so it was hard to be placed into a department. I still got to shadow doctors and see many more surgical procedures though. This week was more for reflection and analyzing the problems that I identified the first two weeks. Trying to sort out the main problems from the sea of problems to write in the report was the hardest part of this week.
Just when I thought I was getting in the hang of things, I will be placed into another rotation. The past 3 weeks went by fast and hopefully my next rotations will be good as this one.
Emergency
Kushal Basnet Blog

The Emergency Department (ED) at UIC is nothing like I was expecting it to be.
The first day started of with Dr.Gehm giving us a tour of the ED and I was overwhelmed by the amount of problems I saw during the tour. There were many small problems like, random carts and wheelchairs blocking the path in the hallway, random noises that seem to be going off for no reason, and many posters and signs on the walls. The structure of the department was not well organized. The hallways had sharp turns and not enough room for the gurney to comfortably move.
There were also some big problems like the supply cabinet in the hallway having a broken lock. The supplies in the cabinets were not properly organized and some of them were not properly sealed. During the tour Dr.Gehm mentioned that the lock had been broken for 6 months and they have even caught people trying to sneak supplies out. This shocked me because this problem is huge and it has a simple solution, but no one is trying to fix it. Another problem that was overwhelming was that most of the devices used in the emergency department was either outdated or broken. Some of the equipment were even ducked taped or had exposed wires.
The second day was a little different. Sara, my partner, and I decided to do a night shift to experience the full scope of the department. We started off talking to Dr.Lin and it turns out she is working on a medical device herself. She is trying to make a small device that can plug into any phone and it would take various vitals of the patient. The patient would use this device and then it would be relayed to their heath care provider. This idea was very interesting and I could see the usefulness of this device in the ED, where having a small portable vital reader would make a big difference.
Sara and I then went around the department to ask the staff about the problem they encounter in the ED. I will provide a list of complains below.
- · Lights were too dim. It was very hard to see the vain sometimes for IV
- · The room were too small and they didn’t provide privacy to the patients
- · There was too much noise and that could lead to noise fatigue
- · There was no place to hang the cords for the devices
- · The computers were old
These were just some examples of the complaints we got. Figuring out the good problems from the sea of problems will probably be the biggest challenge of this rotation.
The First Week of ED
Kushal Basnet Blog

The first week of ED was very interesting to say the least.
I had to move around quite a lot in the Emergency department, unlike my first rotation in Ophthalmology. It got pretty confusing at times on where to go, because there isn’t one physician Sara and I follow. We sort of just bounce from one physician to another while they go in to see a patient. We saw many patients this week and each of them had their own set of problems. Whenever I got the chance to talk to one of the patients, I asked them what sort of problems they encountered while they were at the ED and made a list.
- · Wait times. This was a big one and almost everyone said this
- · Space too small or not enough privacy
- · Beds were uncomfortable
- · Place was dirty
- · The lights were too bright or to dim in some rooms
- · There was too many annoying sounds
Sara and I also went around talking to the nurses on Thursday and asked them if they encounter problems. There were a lot of complains about how most of the equipment didn’t work. One of the nurses mentioned an interesting problem that caught my attention. Apparently a trend started at UIC ED a long time ago where when the nurses would draw up a patient blood, they would draw 1 or 2 more tubes than needed. This was done incase one of the primary tubes were lost or something. The nurses were suppose to leave the extra tube of blood on a tray in the room, but a big problem is that the tubes would always go missing or the nurse would place the tubes in random locations. So if you walk around the ED you would see random tubes of blood everywhere.
One of the other nurses was very adamant about how dirty the ED was. When Sara and I went to asked her to identify her main problem, she instantly said she couldn’t stand the filth. She talked about how many of the machine or chairs were full of dust. She told us about how many bugs or insects were in the lights or how all the curtains in the ED were never washed. At the end of her long rant she told us to just take a walk around the ED and look at how unclean the place was, so Sara and I did so. We did notice all the trash and dirt that was in the ED and we were shocked by the state of the curtains in the ED. There were many curtains in the ED and most of them were used to act like walls. We could see the amount of dirt that was accumulated on the curtains from use and we understood why the nurse was so adamant about the sanitation of the ED. If I were a patient in the ED I would have noticed the lack of sanitation and would have been very uncomfortable.
I identified many problems in the first week and hopefully the next two weeks will be just as informational.
Ultrasound
Kushal Basnet Blog

There really isn’t much to talk about from the first two days of this week. Sara and I were only at the ED for a couple of hours on Monday and we took the morning shift on Tuesday. It seems like the morning shifts are usually quiet, but there is an unspoken rule in the ED where no one talks about the ED being quiet or slow because of some superstition all the physicians seem to follow. It’s actually rather funny.
Sara and I did spend a considerable amount of time following one of the resident and a fourth year medical student, who were doing a ultrasound rotation in the ED. The ultrasound machine is often used in the ED because many patients come in with some type of a pain that was caused by impact and the ultrasound machine can be used to check for internal bleeding or damages to an organ. There are two ultrasound machines in the ED; one is new and one is not so new. Most of the physicians prefer the old machine for some reason. I speculate it has to do with comfort of using a machine that the physician has always used. The machine itself is rather old, dirty, and has a lot of cords and probes attached to it. However, the machine is decorated with lots of stickers and even bedazzled, so I guess it makes up for it.
We saw the ultrasound machine used many times this week. Every time the machine was used on a patient the resident would start off by scanning the patients bar code, then he would type out his name and the name of the attending on duty. The resident would have to do this every time and it didn’t take a considerable amount of time, but it did seem like a hassle. I noticed several things during our observations and made a list.
- · Lots of gel is used during the ultrasound examination. The gel would get all over the patient and would be wiped away with a towel at the end
- · After the machine is used, the resident would wipe down the probe with a sanitizing towel.
- · There was a basket that had many empty tubes of gel on the ultrasound machine.
- · Most of the wires hang out of the machine and it didn’t seem like there was a place to hold them.
- · The buttons on the machine were hard to press.
- · The probes are uncomfortable to the patients at times.
- The machine would have to be plugged into the wall after every use
I’m sure most of these problems have to do with budgeting and there are better ultrasound machines out there, but there doesn’t seem to be any direction on sanitation or maintenance of the machine. It’s hard to tell if that’s the physicians’ job or someone else.
One of the attending set Sara and I up with a bio-engineer that works at the hospital on Wednesday, so I am looking forward to that. Hopefully that will be informational and I will have more stuff to talk about on my next blog.
Bioengineering
Kushal Basnet Blog
Sara and I spent the whole Wednesday of this week with Sergio, a bioengineer that Dr.Kotini set us up with. We had some issue finding him at first because we didn’t know what he looked like and he didn’t know what we looked like, but we did end up meeting up. Sergio started the day by taking us to his office on the 7thfloor of the hospital.
His office was very interesting, because it actually looked like an engineering laboratory and not a hospital room. There were many broken devices and many tools that were used to fix the devices. Sergio sat us down and explained the many things he does in the hospital. He told us that he is in charge of fixing many of the broken devices in the hospital, but he is also an on-call engineer, so whenever a device breaks down and requires an immediate fix he will be called in to fix it. Even though he fixes many of the devices in the hospital, he is mainly in charge of the anesthesia machine used in the ORs.
Sergio told us an interesting story about how he was called in to fix an anesthesia device that broke down in the middle of a liver surgery. Apparently the screen of the device stopped working, so Sergio was called in. When he got in to the OR and inspected the device he found fluid, which he suspected to be saline, in one of the compartments. The saline solution ended up making its way into the transformer of the device and shut it down. Sergio realized that there was nothing he could do it fix it, so they had to replace the device in the middle of this surgery that was going on. The anesthesia device has parts that come off incase of emergencies like this, so replacing the whole device took about 10 minutes. The surgery ended up going well and the nothing happened to the patient. Sergio was upset because someone had put a bag of saline solution in a compartment that was not meant to hold liquid and it almost ended up really bad. It is interesting to note that there was no sign on the compartment that warned users not to place liquid. The General Electric representative came in that day to look at the device and ended up agreeing with Sergio’s assumption.
In the other blogs I had mentioned most of the doctors hated Cerner, the electronic medical record system. I found out that Cerner has a good device interface, while having a poor patient interface. All of the monitors that are connected to the patients in the hospital are connected to the Cerner’s database and Sergio could view each of them in his computer. If there was a problem with one of the monitors, Sergio could look at it in his computer and tell what was wrong. It seemed like that whole system flowed well and if there was a problem it could be fixed easily. All of the defibrillator devices in the hospital have a self-check interface, where the machines do a test run every night and prints out the results. The devices are also connected to the Cerner database, so Sergio gets an email if one of the machines doesn’t pass the self-check.
Problems like the anesthesia device breaking down seem to occur many times at the UIC hospital even though Sergio told us that most of the device had to go through regular checkups. 80% of the problems that come into Sergio end up being user errors, where the physicians or nurse don’t know how to use the device. This day was very interesting because we got to see the hospital from an engineering standpoint.
Anna Brzezinski Blog Heading link
-
Anna Brzezinski Blog
Inhalers: Learning how to breathe
Anna Brzezinski Blog

Breathing comes naturally. We take our first breath of air after birth, but long before that, at around 9 weeks gestation, the fetus makes breathing-like motions. Most of us don’t think about it on a day-t0-day basis unless we’re doing strenuous activity, but for many patients with pulmonary issues, breathing is constantly on their minds.
For many patients with issues such COPD or asthma, inhalers offer great improvement throughout the day or relief from attacks. However, patients often misuse inhalers due to several reasons. There are a variety of drugs and applicators of inhalers, making it confusing for the patient especially when taking multiple types of inhalers daily. For example, some inhalers use a propellant to expel the drug, while others are breath-activated. Some recommend spacers, other shouldn’t be used with spacers. One medication comes in the form of a tablet which the patient must place into an inhaler each time he needs a dose. This can be especially confusing to patients as some may not understand why they cannot simply swallow the tablet. New drugs and methods to administer them are constantly being released, and insurance companies change which medications they cover. As a result, inhalers are often misused and the drug may be incorrectly be determined not to be effective in that patient or require a higher dose.
Standardization of applicators across inhalers is unlikely, although it would be helpful to patients. Some companies provide the clinic with placebo samples for staff to educate patients on how to properly use the prescribed inhalers. However, oftentimes there is only one sample so the patient cannot actually test the inhaler in the clinic with the specialist observing and correcting technique. Because proper use of inhalers is critical to the health of patients using them, more resources should be put into educating them.
Code 1 and the Crash Cart
Anna Brzezinski Blog

Suddenly, everyone in the room becomes silent. Over the lout-speaker, “Code 1, room xyz” is repeated. All the residents and fellows rush over to help. A patient may be in cardiac arrest or have a compromised airway requiring emergency assistance. Fortunately, several minutes later, they return with calm faces and no bad news.
On the way to room xyz, I imagine someone picked up the red cart in the hallway. This crash cart contains common medications and supplies needed in case of code 1 emergencies. Contents include a defibrillator, airway kits for adults and peds, and medications such as Epinephrine and Atropine. If it is critical to have access to the contents as rapidly as possible, then why aren’t they in each hospital room? After all, hospital rooms contain a seemingly large supplies of spare materials. Each room in the Medical Surgical Intensive Care Unit (MSICU) contains a half-empty (at the least the one I looked through) cart with the basics, such as syringes, gauze, IV tubing, and blood drawing kits. It could easily fit an airway kit and some other supplies. I understand that for safety reasons medications cannot be kept in the room, but why not some of the other supplies, like the airway kit? Perhaps it’s due to the cost of the supplies. I am curious to learn over the next couple weeks about why certain supplies are and are not in every room or hallway and how it is decided.
Ventilators and Pressure
Anna Brzezinski Blog

I put on the mouthpiece, tried taking a breath, and it immediately felt different — breathing was exhausting. Taking a breath required work. After about a minute of testing different settings, I was tired and my airway felt irritated. My eyes were on the verge of watering.
Walking through the ICU, you see many patients on ventilators. What you don’t see is how exhausting it is to use one. I always thought that breathing with a ventilator would feel natural, almost passive, but I was mistaken. I was told by the respiratory therapist that it would feel like breathing through a regulator when Scuba diving, but as an experienced diver, I can confidently tell you that I disagree. Unlike normal breathing or even breathing through a regulator, ventilators use positive pressure. To put it simply, when we normally breath, the diaphragms contract, causing in a negative pressure in the chest. As a result, air passively flows into the lungs. However, ventilators pump air into your lungs, which causes a positive pressure in the chest that forces it to expand. In summary, airflow into the lungs is no longer a passive process.
The positive pressure created by ventilators can have negative consequences for patients, yet no modern ventilator uses negative pressure, which seems to be a desirable improvement by physicians and technicians. Ironically, the first ventilator, the iron lung, did. First designed for patients with polio, the iron lung was a large chamber the patient’s body, but not the head, was placed inside of. The pressure of the chamber decreased, causing the chest to expand and a negative pressure in the lungs relative to the atmosphere surrounding the head, resulting in air flowing passively into the lungs. Since then, ventilators have become much more compact and portable, but as mentioned, they now use positive pressure.The general principles are simple but the technology is impressive. There are numerous settings and data from any ventilator in the hospital can be downloaded easily into the EMR system. Inhalers, other than those that are dry powder, and nebulizers can easily be attached to the tubing, and a heat and moisture exchanger ensures the airway and lungs do not dry out. Although many changes have been made since the iron lung first appeared, many medical professionals expressed some frustration with the slow progress with the technology since the positive pressure ventilator hit the market. Since this equipment is integral to so many patients’ survival, it does seem as though attention should focus on improving comfort and reducing negative effects.
Communication Without Speech: Simple Tools for Significant Improvement?
Anna Brzezinski Blog

In most cases, communication between physician and patient is largely through speech. So, when a patient is intubated, is all communication lost? Based on my observations in Pulmonary Critical Care the past several weeks, my answer is almost certainly yes. Sure, the physician can still examine the patient, use vital signs as indicators, and talk to the patient and ask questions, but the patient is almost powerless in responding. Although some patients on ventilators are unresponsive, many are responsive. Over and over, I heard healthcare providers ask patients to nod their heads yes or no to answer, and while some were able to, others could not and tried to communicate with their hands, seemingly unsuccessfully at getting their point across.
This brought me to the question – why aren’t we providing tools to help intubated patients communicate? As one patient tried using small movements of her finger to signal yes or no instead of nodding her head, the medical team kept repeating the same question, unable to understand the answer. I asked a resident if they ever write “Yes” and “No” on a piece of paper and have the patients point to the answer. He said they could try it, and everyone proceeded to exit the room with no answer to “Are you having any pain?” and “Are you breathing comfortably?”
Although this summer program is focused on observations and not on solutions, I can’t help but think of simple ways we could empower patients to be able to communicate. For example, have a board with “Yes” and “No” written that the patient can point to, provide a diagram of a human and ask the patient to point to the area they have pain, provide a printed list of commonly asked questions the patient may like to ask the medical team that the patient could point to. Seemingly simple tools may significantly improve communication and provide the patient with some sense of control instead of what I imagine would be frustration.
Image from https://americannursetoday.com/post-intensive-care-syndrome-what-it-is-and-how-to-help-prevent-it/
Little Problems, Big Impact
Anna Brzezinski Blog
Oftentimes, we ignore the little problems in life — those that seem unequivocal. Some have existing solutions, but we are so used to dealing with them that we don’t even consider using them. But when you add up all those little things that interfere with the flow of the workday, they add up and can cumulatively have a big impact.
The past several weeks, a some “little problems” jumped out at me. First, patients in the clinic were struggling to sit on the exam chair. Although adjustable, even at its lowest height, the chair was too high for many patients. Even I had to hop on and off. As a result, many patients were examined in the chair they were sat in during the medical history. Let’s say the doctor needed to examine the patient lying down, the standard chair would not allow for that. Fortunately, this dilemma could be solved by placing a step-stool in the exam room. Another issue I observed was during the allergy clinic. After applying the allergen extracts on the patient’s arm, the nurse placed the applicator in the Sharps container. Each time was a struggle. The applicator was too large to fit comfortably in the container. An easy solution for this problem exists as well — replace the existing Sharps containers with larger ones in the allergy clinic.
A third problem I observed does not have an existing solution that I am aware of but could be improved from an engineering and design standpoint. The armrests for the beds in the bronchoscopy suite are difficult to attach. Every time we observed procedures and the armrests attempted to be attached, it required several people and time to accomplish the task. Once the mechanism was explained to me, I noticed that it was pretty simple to attach but there were some exposed parts on the arm that made it confusing to a user when looking at the piece. While all three of the problems mentioned seem minor, they all interfere with the flow of the patient’s visit and could be tackled relatively easily.
From the Lungs to the Brain
Anna Brzezinski Blog
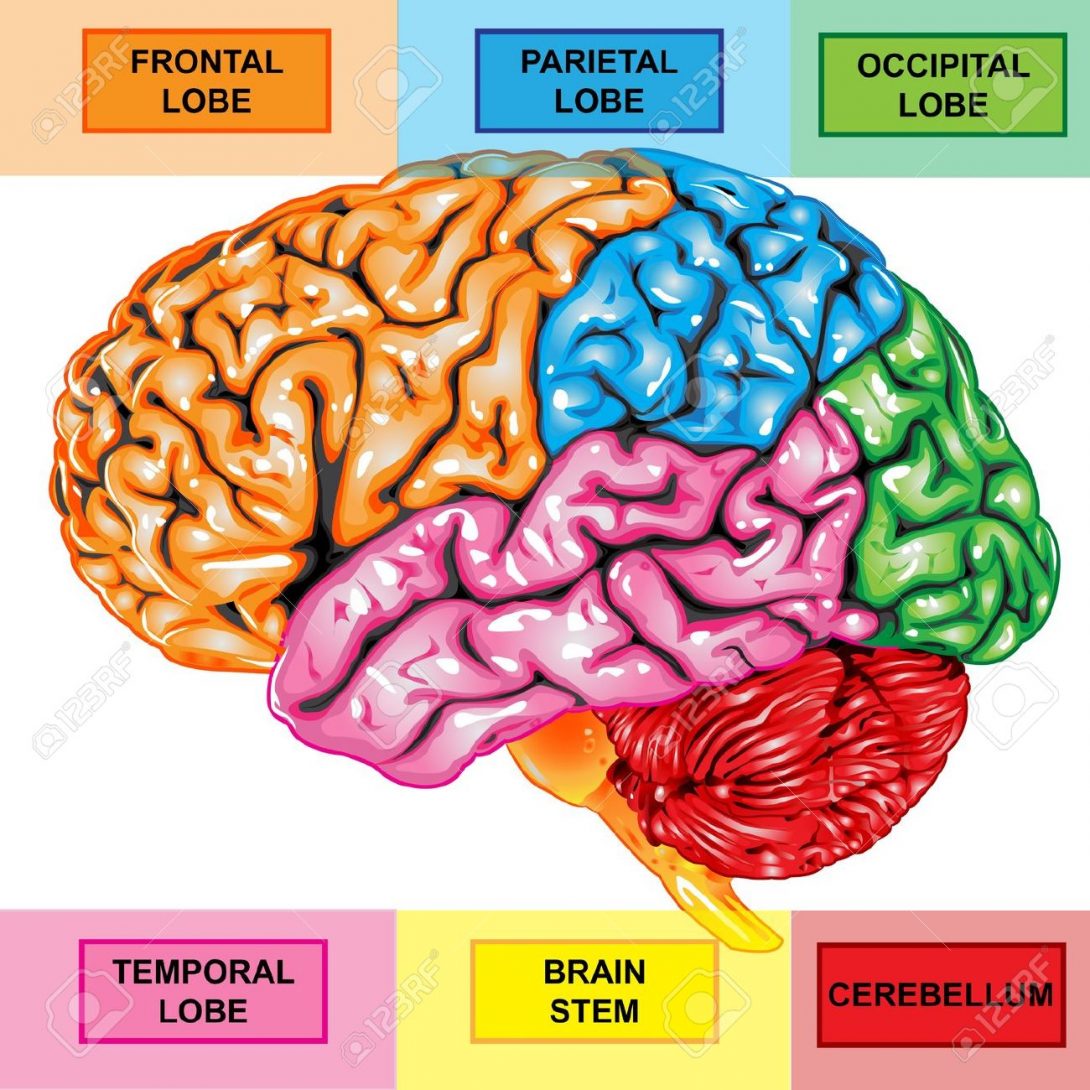
Probably the most surprising part of Pulmonary and Critical Care was the loss of communication of patients on ventilators. I discussed this and provided some ideas on how to improve communication in a previous blog post. What I didn’t expect was to see the same exact issue on my next rotation, Neurology. The past week, I rotated with the stroke team. Depending on the location of the stroke, patients lost different abilities — perhaps they couldn’t comprehend language, find the right words to say, move parts of their body, or a combination of many deficits. In some cases, there aren’t necessarily tools to assist patients with strokes with communication. However, in cases of expressive aphasia, which is due to damage to Broca’s area, I wonder if providing some tools like those I discussed in my Pulmonary post would be useful. Perhaps a printout of commonly asked questions by patients would help the patient feel less helpless — or maybe they would not be able to use the tool due to the stroke. I witnessed the frustration of patients with expressive aphasia as they tried to speak but couldn’t say the words. They opened their mouths but couldn’t form the words they were thinking of and all I could think of was if there was a way to help the patient communicate.
Although I’ve switched from the lungs to the brain, I am still spending a lot of time in the ICU. Beyond the difficulties in communication between patient and doctor, many of my observations still apply as many of the technologies in the ICU are the same, such as IV pumps. I am excited to see what other similarities and differences I notice in the next couple weeks.
Image: http://previews.123rf.com/images/medusa81/medusa811106/medusa81110600024/9807020-Human-brain-lateral-view–Stock-Photo-anatomy.jpg
Reading EEGs
Anna Brzezinski Blog
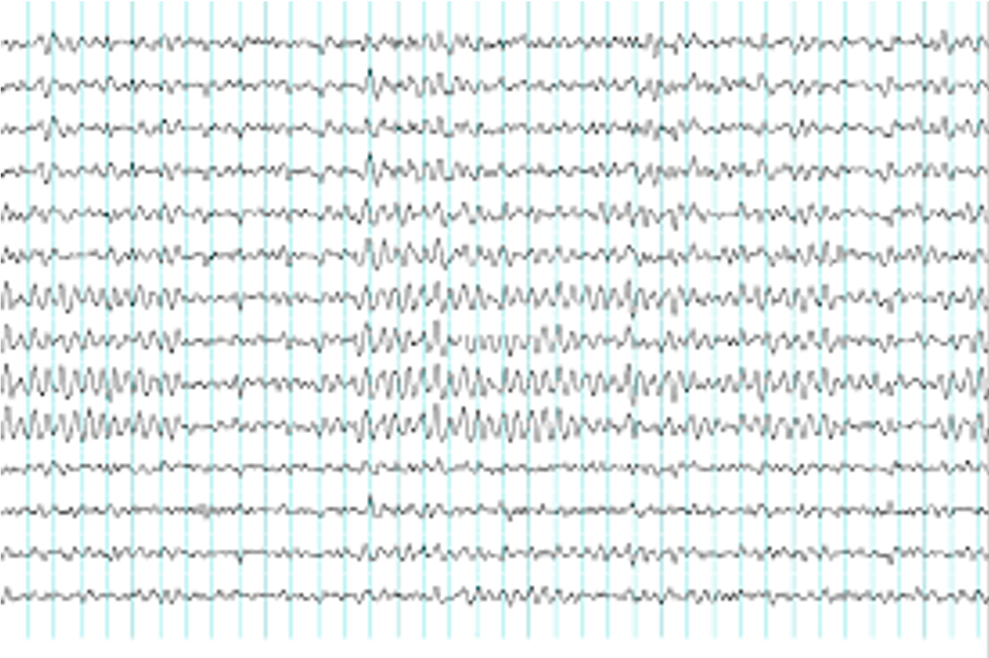
EEGs, electroencephalograms, are routinely performed on patients with seizures. Sometimes recordings last 20 minutes, other times they last 24 hours. Reading them is tedious. The doctor not only looks for seizures themselves, but also epileptiform activity that is present in patients with epilepsy. These occur sparsely and are not evident to the untrained eye. Watching a couple doctors read through several recordings, I was impressed by how quickly they scrolled through the recording, occasionally stopping if they suspected an abnormal waveform. I couldn’t help but also question whether some were glanced over and missed. Other than adjusting the gain and a few other settings to clean up the waveforms, the program didn’t do much. It didn’t point out where abnormal waves could be. According to the attending, software does exist for that purpose but doesn’t work well due to the variability in shape and waveforms and great amount of noise in the recordings. However, apparently for a given patient, epileptiform waves are usually rather consistent. I can’t help but wonder how to create a more accurate software to increase the sensitivity and speed of reading EEGs.
Image: https://www.google.com/url?sa=i&rct=j&q=&esrc=s&source=images&cd=&cad=rja&uact=8&ved=0ahUKEwjP5K_aup_OAhUr2oMKHbB5BsoQjRwIBw&url=https://www.epilepsy.org.au/about-epilepsy/medical-aspects/diagnosis&bvm=bv.128617741,d.amc&psig=AFQjCNHSvSHBE52GKwBzC0rEjYIl_O9DSg&ust=1470114808761662
VP “Shunt” Be So Static
Anna Brzezinski Blog
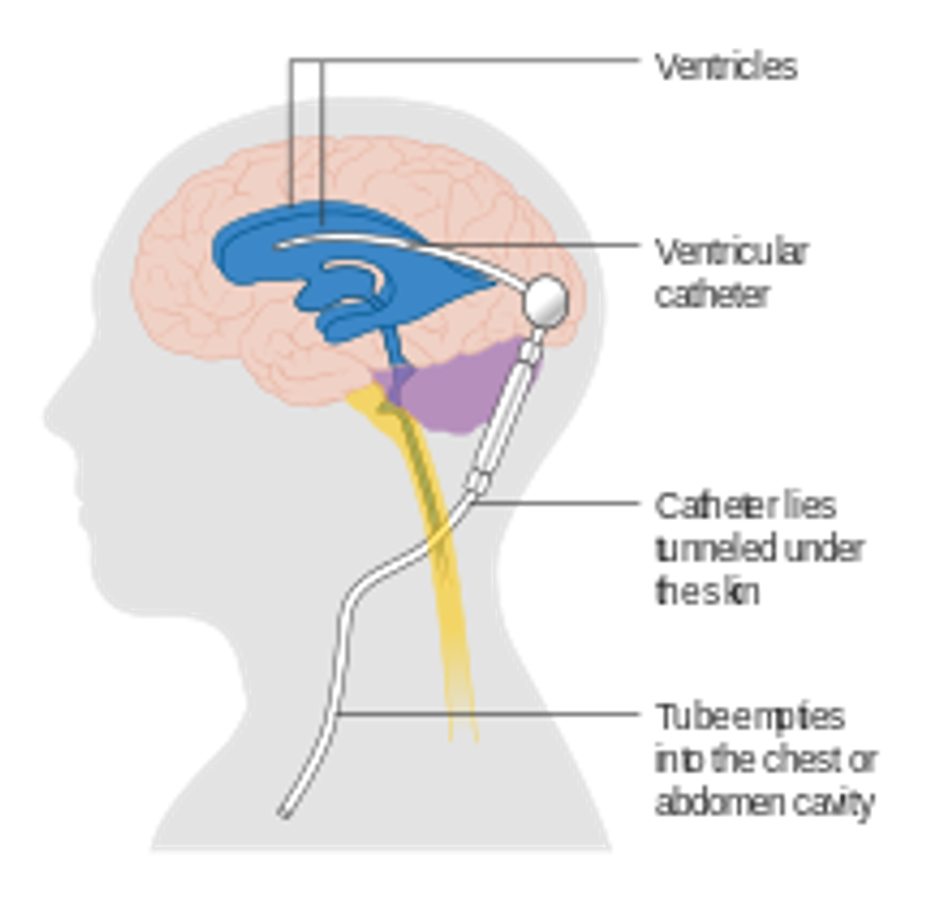
Ventriculoperitoneal shunts, aka VP shunts, are surgically placed in patients with hydrocephalus, a condition in which there is excess cerebrospinal fluid (CSF) in the brain’s ventricles. Throughout the course of treatment and after recovery, a patient may require different amounts of drainage or none at all. There are two main categories of shunts: non-programmable and programmable. The former come in various sizes, which is selected upon placement. The latter and newer model can be programmed to accommodate various amounts of drainage. It must be programmed at the hospital, and just like a pacemaker, must be reset after MRI.
Although the programmable VP shunt is adjustable, it truly is still static once it is set to a given size. I was surprised to learn there is no dynamic valve that adjusts drainage based on the conditions and has the capacity to determine the optimal size. Both over-draining, which can happen when patients stand up, and under-draining could be harmful to patients but no mechanism exists in VP shunts to prevent this in the dynamic conditions of the body. But “shunt” it? (i.e. Shouldn’t it?)
Image: https://en.wikipedia.org/wiki/File:Diagram_showing_a_brain_shunt_CRUK_052.svg
Occupational Therapy
Anna Brzezinski Blog

This week we spent time in Physical Medicine and Rehabilitation (PMnR). PMnR is truly a collaboration of physicians, nurses, and physical and occupational therapists. I walked through the doors to Occupational Therapy (OT) and suddenly I was standing in an apartment — well, sort of. OT’s role is to assist patients with activities of daily living (ADLs). In order to help patients learn how to perform ADLs, they need a bed, sofa, kitchen, laundry machines, etc., all of which are in the OT room.
In addition to the contents of the room, OT’s provide specialized tools to assist patients. These range from special utensils for individuals with tremors to walkers to splints. While many of these are pre-made, they sometimes require modifications to make them user-friendly to the individual patient. For example, the OT often bends the pole of the long sponge to allow patients with limited shoulder flexion to wash their backs. Some of the devices, such as a hand strengthener apparatus, appear cheaply made and often break, yet they cost thousands of dollars. For that price, it’s hard to think that there is no better device on the market, but the better option is more than twice as expensive. Patients that use walkers are limited to clunky accessories, such as tray tables and baskets that don’t fit properly. Improvements would not only help patients with walkers but could also help them feel more comfortable with them. Overall, I was impressed by the number of tools available to assist patients with ADLs but disappointed in their quality and the limited variety.
Elise Debryn Heading link

Hi! I’m a senior majoring in bioengineering at the University of Illinois at Chicago (UIC) with a concentration in cell and tissue. I am also a student in the Guaranteed Professional Program Admissions for medicine. My goal is to become a research physician and to create advanced medical technology to improve patient care.
Elise Debryn Blog Heading link
-
Elise Debryn
I Could Get Used To ThisElise Debryn Blog
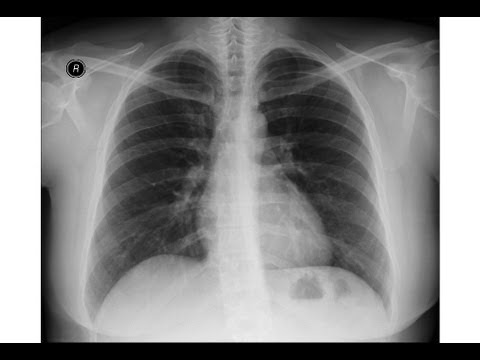
Week 1
7/5/16
The first day of my pulmonary/critical care rotation consisted of many unfamiliar faces/names, twisting hallways, and scary medical jargon. I was excited and nervous- excited to have the opportunity to work closely with physicians, and nervous I would mess something up or ask a stupid question. However, the staff was incredibly warm and friendly. My nervousness subsided for the rest of the day.
The first person we came across was an advanced practitioner nurse who immediately delved into the complications of teaching patients how to use inhalers properly. Apparently, many people forget the first crucial step of using an inhaler. The steps are as follows: 1. Exhale as much air as you can out of your body 2. Place the inhaler to your mouth to simultaneously inhale and blow two puffs of the inhaler into your mouth 3. Hold your breath for 8-10 seconds. Another problem is that there are several categories of inhalers and several more options within each category. Patients must learn how to use their specific inhaler properly or else they will be readmitted for another visit to the hospital.
The nurse suggested creating separate education rooms within the clinic so nurses or physicians can teach patients how to use their inhalers properly. Effective teaching methods will significantly lower health costs for patients and the hospital.
A little later that day we were paired with fellows working in Dr. Dudek’s clinic. The fellow I had the opportunity to work with was Dr. Usmani. For his first patient, Dr. Usmani had me follow him to a room where he greeted Mr. X and began his medical/family history. I really enjoyed observing how Dr. Usmani interacted with his patients and how he used given information to arrive at a diagnosis. He went through a general process of assessing initial medical information that was given to him about the patient, meeting with the patient to gain a full and complete history, and then finally studying the patient’s x-rays or scans with Dr. Dudek.
Patient x-rays were run through the computer system and displayed on one of the screens in the doctors’ office. They were fascinating, but I couldn’t see what the doctors saw. I didn’t have their specially trained eyes to decrypt the images. Dr. Dudek and Dr. Usmani gestured toward certain parts of the chest and lungs while noticing subtle differences in the patient’s anatomy. Sitting there I could only wish to gain their same ability some day.
Dr. Dudek mentioned how it is sometimes difficult to upload scans into the system because not all hospitals and clinics use the same software. CD-ROMs are even used to store scans but are problematic for physicians. Precious time is taken out of their day to tinker with the software when they could be helping a patient instead.
I still felt excitement by the end of my first day at the pulmonary/critical care department. I can’t wait to see more in the upcoming weeks!
Inhale, Exhale
Elise Debryn Blog

My second day of Clinical Immersion revealed the finer details of pulmonology. In the morning, we shadowed a respiratory technician who performed pulmonary function tests (PFT) on patients in a specially designed room. This room contained a transparent chamber, a sealed gas tank, and a computer. At the beginning of the PFT, the technician had the patient sit in the chamber with the door open and breathe into a mouth piece (shown below). The mouth piece had an internal filter that blocked any spit or bacteria from entering back into the machine. The patient had to go through different breathing patterns, such as taking a deep inhale and slow, deep exhale or rapid, quick breathing cycles. At the same time, a graph of flow vs. time was generated on the computer screen. The end measurements obtained from a PFT is the forced expiration volume (FEV), residual volume (RV), total lung capacity (TLC), forced vital capacity (FVC), and vital capacity (VC). The purpose of all of this is for physicians to interpret whether a patient has either obstructive or restrictive pulmonary disease.
Later on in the testing, the technician closed the door to the chamber where a known concentration of carbon monoxide (CO) or helium was released. A body pletismograph was obtained to measure lung volume and pressure changes.
The technician mentioned how he wish the whole process could be automated such that the computer could indicate breathing patterns and decipher between good and bad collected data.
Earlier that day, we observed a bronchoscopy, which is when a physician uses a scope to examine a patient’s airways to search for enlarged/unusual lymph nodes. The procedure admittedly looks uncomfortable. Imagine having a long cord placed into your trachea while partially conscious. Many patients cough during it, which is normal.
The patient lies down in the supine position with a guard placed over the mouth to prevent him/her from biting on the scope during the procedure. Anesthesia is administered moments before the procedure begins. The tip of the scope contains a 50 degree span ultrasound probe, a 35 degree needle, and a 30 degree camera. A physician holds a part of the scope (that looks like a game controller) near eye-level so that the scope remains straight while going into the patient’s throat. The “game controller” has many wires coming out of it that hook up to various connectors in the wall or to machines.
At first, the team was having difficulties setting up the scope. Nothing was showing up on the screen and when it finally did, the colors weren’t correct. Everything looked too pink. This obviously delayed the procedure and the physicians and nurses had to figure out what was wrong while attending to the patient. Once they were finally able to get the scope working (it was a matter of inserting the end of the scope properly into a machine), I noticed how uncomfortable it must be to use it. Imagine having to steadily hold a part of the scope with one arm bent at the elbow while fishing the scope with the other hand into the patient’s throat. In addition, it was difficult for the physician to see where he was going since the camera was not directly pointed at the end of the scope.
Near the middle of the procedure, a pathology team was called into the room. They rolled in a cart holding a microscope, various dyes, and containers. Once the physician obtained a biopsy from the patient, it was handed over to the pathologists for examination. It was intriguing to see how the physician and pathology team were able to directly communicate whether more samples needed to be taken and if the biopsy indicated a serious problem with the patient. Once the team was done, they rolled they equipment out of the room.
The attending would spend a little more time to allow the fellows to practice using the scope. Every once in a while, the nurse would have to suction saliva from the patient’s mouth. On the screen I could see the larynx lead into the trachea, which then leads into the bronchioles. The pinkish lumens of the bronchioles were fascinating. It looked like a maze of tunnels – each one branching off into more and more tunnels. Every time the patient coughed the bronchioles would constrict and rise towards the camera.
By the end of the procedure, I was amazed by how far medicine has come. A century ago, physicians could have never viewed the respiratory tract of a living patient. Their only option at the time was to conduct autopsies on cadavers. Although, I know even more can be done to improve current care.
Vent
Elise Debryn Blog
Week 2
7/11/16
We had the opportunity to try one of the ICU’s latest ventilators called the Nellcor Puritan Bennett 840. The 840 includes an HME filter that humidifies and warms up air to body temperature so patients’ lungs do not dry out. Each of us used a mouthpiece that connects to the ventilator. We wanted to experience what it feels like to have a machine breathe for us. Normally, humans breathe through negative pressure, which allows air to readily enter through the respiratory airway and the lungs. Ventilators, on the other hand, utilize positive pressure to push air into a patient’s lungs. If air is pushed too aggressively into the lungs, then the patient can suffer from lung damage.
A respiratory technician set the parameters on the ventilator and instructed me to hold my nose. A sudden rush of air entered my mouth, and, at first, it was too much to handle. I had to take my mouth off the mouthpiece to regain my breath. I tried once more. This time, I anticipated the sudden gust of air and exhaled slowly. It was absolutely tiring to be breathing on the machine. The technician eventually adjusted the settings so it was similar to the type of breathing one would experience while scuba diving. This setting was much more comfortable and felt more (although not completely) natural. The entire experience left me with more empathy for patients who have to depend on this machine.
An advantage to using the 840 is that patient ventilator information can be easily downloaded onto a computer at the nurses’ station. Physicians can also place ventilator orders for their patients on the computer. Information can be sent to and from patient rooms, decreasing foot traffic and increasing efficiency in the ICU.
Later that day, we shadowed Dr. Nyenhuis in the allergy clinic. I went with her to see a patient who was suffering from allergies. After recording the patient’s medical history, Dr. Nyenhuis walked over to the patient to perform a routine physical examination. I noticed during the examination that it was difficult for Dr. Nyenhuis to use the retinoscope and otoscope on the patient because both instruments were attached to the wall through a long, coiled cord. It was the kind of cord you would see on old landline phones.
During another physical examination, a patient received an allergen test. For this test, nurses apply a plate of small spikes, each containing a different allergen, such as tree pollen or dust, and press them into the patient’s forearms. The spikes only break the first layer of skin so it is a relatively painless procedure. I noticed it was difficult to dispose of the allergen plates in the biohazard waste container because the opening of the container was too narrow for the bulky plates. After 15 minutes, the nurses record any allergic reaction by measuring the flare and wheal of the bumps with a ruler. The sum of the measurements indicate a positive or negative result. An irregular circular shape (also called pseudo-podding) indicates a stronger allergic reaction.
Spike used to apply antigen to patient’s skin
Ruler used to measure flare and wheal of allergic reaction7/12/16We visited the ICU in the morning and learned more about pharmaceuticals. The pharmacy uses a relatively old-fashion pneumatic tube system to transport medicines all across the hospital. This method is more efficient than having a person deliver medications via a cart. The ICU also uses an Omnicell machine to store 50% of their medication. It is the most efficient method of retrieving medications because the machine stores pre-made medicine with long stability and can help track abuse. Physicians and nurses are able to keep track of sedatives and narcotics by making only one vial available at a time. I saw a resident restocking the Omnicell and questioned whether staff was ever afraid of stocking the wrong medication. The resident clarified that each medication is scanned and placed into its appropriate canister. Other canisters are locked to ensure medications are placed in their proper dispenser.
Omnicell machine
Later on, an anesthesiologist resident showed us a high resolution Guide Scope that is used for intubation. The end of the scope has a camera and a light that helps the user to visualize the vocal chords. Once the vocal chords are in view, an endotracheal tube can be put in place to open the patient’s airway. Th Guide Scope allows for greater precision so less harm is done to the patient, and physicians can restore the patient’s airway more quickly.
Guide Scope
A nurse in the ICU talked about new pumps available for the hospital that are better at protecting patient information. Pumps are individual units that deliver specific mediation at a determined concentration and rate to the patient. There is one pump for each medication. The hospital’s current pumps are a little more outdated and less protected from viral attacks. The nurse also explained that the current pumps are very heavy and have poor design. The front ridge of the pump may make for easy bacterial transfer because it is usually not bleached when the pumps are cleaned. Nurses must also go throw a number of steps in order to setup the medication specifications. Most importantly, the pumps do not indicate battery life and they have a relatively short battery life. Patients are in danger of receiving sub-optimal therapy as a result. For instance, there have been times where pumps have suddenly died while nurses are transporting patients. It takes a while for a new pump to be available, and the patient is deprived of his medicines for a period of time.
two pumps on a stand closer look at a pumpIt’s always very interesting to examine not only the machines and equipment different departments utilize, but also the processes that take place between nurses, physicians, and technicians. I hope to learn more about what can be improved and what has proven to increase efficacy in patient care.
Poking Around
Elise Debryn Blog

Week 2
7/13/16
There wasn’t much for us to do in the PFT labs so we ventured off towards the cardiac catheter lab. I’ve never seen or heard of such a procedure so I wasn’t sure what to expect. I learned that a cardiac catheter and dye are used to locate major blockages near the patient’s heart. The surgeon begins the procedure by inserting the catheter through the right femoral artery and snaking it up through the aorta. Once the aorta is reached, the dye is injected and an x-ray scan of the patients chest is shown on a screen in front of the surgeon.
On one side of the room there are technicians and nurses helping the surgeon prep for the surgery and to help visualize where the catheter is in the heart. A St. Jude’s bioengineer was on site that day and explained that she was using software to create a 3-D image of the heart by placing electrodes and several more catheters in the heart.
Their patient today had an arrhythmia that was producing tachycardia (fast hear rate). The arrhythmia may be corrected by burning/killing certain heart cells near the tricuspid valve. The bioengineer described it as stopping the heart from “short circuiting”.
I noticed that in the prep stage, the surgeon and nurses were having a lot of technical difficulties with troubleshooting. A cable would sometimes pull out of its socket or someone would forget to plug in a cable somewhere. Once they got the procedure going, the C-arm of the fluoroscope machine sometimes bumped into the screen monitors the surgeon was looking off of to view the patient’s chest x-ray. There were 9 monitors in total suspended form the ceiling, which I thought was a smart way of maximizing floor space. In addition, the x-ray itself is hard to use because it is 2-D and has no depth perception. So, the surgeon has to be very careful guiding the catheter around the heart.
As the procedure continued, it was amazing to see the 3-D image of the heart slowly come to fruition on the screen in front of us. The surgeon and bioengineer worked together to find all of the “hot spots” in order to kill heart cells. However, I did notice communication between the two could be improved. This is because the bioengineer and surgeon had to be separated by a glass window to protect those who weren’t wearing led-protected clothing from unnecessary radiation. The bioengineer had to keep pressing a button in order to speak over the intercom with one hand while navigating the computer with the other.
7/14/16
I walked into the clinic that day and met a very enthusiastic and amiable doctor near the front door. His name was Dr. Machado and he specialized in pulmonary hypertension (PT). Right away he began to explain the physiology behind PT by comparing the circulatory system to a circuit. I liked how he took the time to explain this all to us before we went to see patients. He kept everything in simple terms and made sure we understood what he was talking about. Once we did get to see patients, I noticed twice in a row that patients had trouble getting up on the examination chair. They were either too short or too weak to get up on the chair, and the chair couldn’t go any lower. It seemed to hinder the diagnosis process because the doctors had to improvise with a stool instead. I wondered what they would have to do if even a stool wasn’t available.
Sleep Center
Elise Debryn Blog

It was a blistering hot day. The sun was beating on our backs, and the humidity was smothering. We were venturing to the Sleep Center on West Harrison Street. Once we arrived, I silently thanked the cold air that blasted our faces. In the break room, Dr. Singla was busily typing up patient notes. He was incredibly friendly and introduced us to the fellows also working the clinic that day. I noticed that every patient room had a typical desk and chair in one corner and a giant bed in another. The beds, fancily decorated with old-fashion comforters, are used for sleep studies.
Most of the patients who visit the Sleep Center have sleep apnea: a condition where the airway is obstructed during sleep, causing the person to stop breathing and wake up. CPAP machines help prevent sleep apnea by blowing air, much like ventilators do, into the patient’s airway. Air is drawn into the machine and humidified when released into the face mask. Our group was curious to know as to why these machines do not use HME filters, something also found in ventilators. HME filters warm up and humidify air exhaled from the patient so that it can then be inhaled again for the next breath. These filters use an internal air source, which reduces the risk of infection for the patient. It is very likely that patients using the CPAP machine can contract fungal, bacterial, or viral diseases if the air is contaminated or if the machines are not maintained properly.
Overall, it was interesting to observe the many conditions/illnesses related to quality of sleep. Much of the current technology used to treat these ailments can be modified and improved upon for better patient care/treatment.
The Big Picture
Elise Debryn Blog

During clinic with Dr. Machado today, we came across a patient who was on many types of medication. Her only way of remembering all of them was by thinking of them in alphabetical order. It was a clever way of keeping track but otherwise seemed hectic.
I’ve noticed that physicians, nurses, and pharmacists all have a difficult time creating a complete picture of patients’ past and current medical histories. It’s not due to any lack of cognitive function by healthcare workers, but rather by the inefficiencies of the entire healthcare system. Lists of medications, tests, and diagnoses appear on most patients’ medical records. Dr. Jacobsen mentioned that many mistakes can carry over with the use of electronic medical records. Whether it’s the matter of copying and pasting “not” into a patient’s records, many mistakes can be quite harmful, even disastrous for the patient.
Dr. Jacobsen gave the hypothetical situation of a patient suffering from extremely low blood pressure in the ICU. Physicians administer many fluids to raise the pressure and over flowing the body with too much can lead to pulmonary edema, or fluid in the lungs. This is also symptomatic of congestive heart failure. Someone unfamiliar with the patient may very easily type in “congestive heart failure,” which will continue to exist in that patient’s medical record for future doctor visits. A patient who has never had congestive heart failure continues to be labeled as one anyway.
It’s difficult to get an entire industry, such as the one responsible for the incredible yet flawed electronic medical record system, to standardized their protocols and software. How do you get giant corporations to understand the importance of administering the highest quality of care? Of increasing efficiency in order to save both the physician’s and the patient’s time? Not all of this will come without the cost of cutting dollars on the side of these corporations. It’s unfortunate we live in a world where money comes before health-where life is at the expense of profit.
Hemodialysis
Elise Debryn Blog
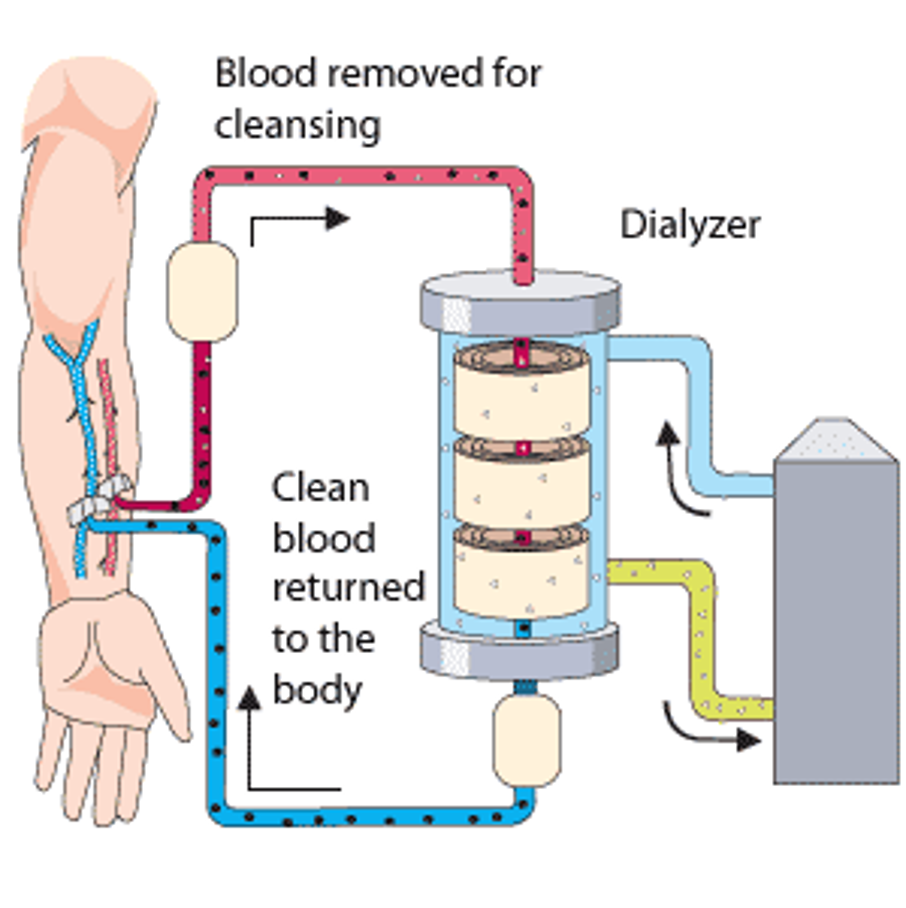
7/26/16
Today we had the opportunity to visit the transplant clinic with a few of the residents. For our first patient visit, I noticed that there were no hand sanitizers outside of the patient rooms, only inside. Although this may not seem like a huge design flaw (or even a flaw at all) I feel like it’s harder for the staff to sanitize their hands as frequently as they need to. Some of the hand sanitizers inside the patient rooms are difficult to access.
The first patient had a heart catheter, fistula, and graft done prior to the appointment. A fistula is when the vein and artery are connected to make the vein bigger over time. This enlarged vein is used for hemodialysis so that a strong enough flow can turn into the machine. Arteries are too deep to access so veins make for a better alternative. Grafts are another option, although they are more prone to infection because a plastic tube is inserted to connect the artery and vein. Introducing a foreign object into the body always poses a risk for rejection reaction. Heart catheters are a third object for hemodialysis but they can be very dangerous for patients because they provide an opening from the larger vessels to the external environment.
Another patient we saw had a very large, developed vein from being pumped with a high volume of blood for hemodialysis. We had the chance to place our fingers over the bulging vein and feel the turbulent blood flow.
In the middle of clinic hours, a couple of nurses were arguing with one another about room booking. One nurse complained that a patient had been on a liquid diet for days and now had to continue that diet until he/she came to the next appointment since the current one was cancelled due to a room booking conflict. Apparently, transplant patients took priority every other patient in the clinic. The nurses felt angry for their patients.
7/27/16
Today I got to catch up with my previous GPPA teacher, Dr. Andrew Gonzalez. He wanted to know what Clinical Immersion was all about and pitched some ideas to us during lunch. He mentioned how difficult it is to come across a long enough vessel for many bypass surgeries when bypassing arteries from the thigh to the foot. He sarcastically asked us to solve this problem in a couple of years by growing stem cell vessels using a long scaffold.
OR
Elise Debryn Blog

7/28/16
Today we got to see a living donor kidney transplant. The OR was an intimidating place. Everyone was scurrying to accomplish their respective duties all while maintaining the utmost sterility in designated rooms. Prepping for surgery seemed difficult because there were so many people who had to maneuver around one another and unused machines in the OR. Blue cloths were placed on tables that had to be sterile before and during the surgery. The attending Dr. Jeon wore a special kind of gown made with a different kind of material during the surgery. I wasn’t sure if this was because the material might have been more comfortable for the surgeon or if that’s just what he always liked to wear. The nurses took inventory of all the instruments that might be used during the surgery to make sure nothing is left inside the patient’s body. One nurse explained that one reason this is a very important task is because sponges shrink and crumble up once they’re soaked with blood. Those sponges can be easily overlooked once the surgeon is ready to stitch the patient back up. The anesthesiology attending and residents had a difficult time finding another catheter in the OR and had to call an outside nurse to bring another one in. I noticed that the anesthesiology attending inserted a metal device to separate and hold up the many tubes and wires attached to the patient.
Once the surgery started, I noticed that there were some staff who were wearing shoe covers and some who were not. It was an inconsistency in their hygiene policy for sure. We were confused among ourselves as to whether or not we should wear shoe covers. In addition, it was very difficult for the attending and residents to adjust the lamps looming over the surgery table. It was difficult to make minute adjustments to the lamp’s position and to even reach the lamp for some people because it was too tall.
7/29/16
The next morning we sat in on a donor/recipient transplant qualification meeting. Dr. Oberholzer, nutritionists, pharmacists, financial aid officers, social workers, and other staff members sat around a large table discussing individual cases. They looked at each patient’s past and current medical history to catch patterns of noncompliance, suicidal behavior, drug abuse, etc. All of the above behaviors make a recipient less likely to receive an organ for transplant. The committee tries to help these individuals with improving certain behaviors, such as having them work with a psychiatrist to treat depression.
At the end of the meeting, Dr. Oberholzer inquired as to whether the staff could find living donors who were rejected recipients in past cases. Staff members vocalized difficulties with finding these cases because they are not traditionally entered into the system. In addition, a nurse brought up the ethical dilemma of having donors lose weight before transplant surgeries. Hospital policy does not require donors to lose weight, but it likely lowers risks during surgery. However, an ethical situation might arise if the donor feels that the hospital promised him/her something in exchange for losing weight before the surgery. They all agreed they needed to consult with each other more on the topic. Finally, Dr. Oberholzer mentioned that other hospitals have implemented a practice called Donor Swap. This occurs in a situation where recipient and donor at hospital 1 are not a match, and donor and recipient at hospital 2 are not a match. However, donor at hospital 1 is a match with recipient at hospital 2, and recipient at hospital 1 is a match with donor at hospital 2. They two donors would thus switch their respective recipients. This method is more efficient and likely to save more lives since organs are in high demand and hard to come by.
(the image used for this blog post is not from the actual operating room we observed)
Da Vinci
Elise Debryn Blog

Yesterday, we had the opportunity to shadow another living-donor kidney transplant, this time performed by Dr. Oberholzer. When we first got into the OR, there were some technical difficulties with the automatic ventilator, and the anesthesiologist had to vent the patient manually. The anesthesiologist said it was difficult to initially figure out if there was something wrong with the ventilator or with the patient because the machine did not specify. The ventilator started to work three people and half an hour later.
Dr. Oberholzer complained that the organ flusher machine did not work on a negative feedback loop. The flusher functions to keep the organ cool while the surgeon works on the patient. However, this flusher would keep getting colder and colder instead of automatically turning off when it reached the ideal temperature. Dr. Oberholzer complained that this made it very difficult to preserve the organ while performing a surgical procedure because someone had to constantly monitor it.
Soon after, we saw Dr. Oberholzer at work on the da Vinci, synchronizing hand and arm movements all while maintaining a visual on the patient’s internal anatomy. Dr.Oberholzer said it was difficult to communicate through the da Vinci’s speaker system because it was quite muffled and required a very quiet OR. I got to view the surgery through the eyes of the surgeon as well because there was another da Vinci that allowed one to simply view the procedure. The 3-D view was amazing. The da Vinci provided proper depth perception and had good quality resolution. I noticed during the surgery Dr. Oberholzer would have to stop every now and then to take excess tissue off the cauterizer because it would collect on the device over time. In addition, Dr. Oberholzer’s view would become obstructed by the smoke from the cauterizer, and one of the nurses had to remove the camera to clean the lens. The opening in the patient had to be vented to allow the smoke to escape.
A technician talked to us about the patient beds in the OR. She said the beds often malfunction for high BMI patients: sometimes they won’t go any lower or can’t accommodate improper weight displacement across the surface area of the table. Sometimes surgeons have to stand on a step stool if the bed won’t go any lower, which is something they would otherwise never do. Also, the bed remote stopped working so someone had to climb under the sheets to use the control column on the bed.
There were definitely major equipment and technical problems this time around that should be fixed to allow surgeries to go more smoothly.
Fire Hazard
Elise Debryn Blog

Today was an exciting day in the OR! In the morning we got to see the removal of a graft. A graft is placed in hemodialysis patients and it functions to connect an artery to a vein. Blood flowing through the artery ultimately flows directly into the vein, causing the vein to bulge over time, and provides easy access to a high pressure blood source for hemodialysis. Grafts can also act like stents because they contain a wire mesh inside that keeps the vessel open. One patient’s graft had the wire slightly sticking out and was in danger of contracting an infection, so it had to be removed. I wondered if damaged is caused to the vein because of the sudden increase and decrease in high blood flow after the graft is inserted and removed. Veins naturally carry low blood flow because they are more compliant than arteries and can handle higher pressures better (they work against gravity to return blood to the heart).
Later on that day we got to see a tracheotomy whilst waiting for another transplant-related surgery. My friend Dr. Andrew Gonzalez allowed us to shadow the surgery. Another resident talked with me about the potential fire hazard of inserting a tracheostomy tube. I didn’t expect such a hazard to exist for this procedure, but he explained that there are three things to start a fire: air, fuel, and heat. This reminded of the article we were handed in one of our Monday workshops about the firefighter who saved his life in a wildfire by igniting embers to create a thin layer of oxygen around him. Anyway, a cauterizer is used to cut through the neck tissue to reduce bleeding and to make a clean cut. Meanwhile, the endotracheal tube has high pressure oxygen flowing through it. A combination of the sparks from the cauterizer and oxygen in the endotracheal tube is combustable and can cause a fire, which has happened before but not at UIC. It was scary to think that this could be a possibility during the procedure. The resident explained they can reduce fire hazard by temporarily stopping respiration or by reducing oxygen flow through the endotracheal tube. In these kinds of situations, it is very important the surgeons communicate with anesthesia.
This surgery had to be performed in the first place because patients can only have an endotracheal tube for up to two weeks before it starts causing major damage to the trachea. The endotracheal tube pushes against the trachea’s lumen, causing micro-movements that can create ischemia in surrounding tissue.
It was interesting to see the drawbacks of some of the medical equipment used in the OR. I was surprised something hasn’t already been implemented to reduce the potential for fire hazard in some of these surgeries.
Rounds
Elise Debryn Blog

Yesterday, we didn’t have much to do or see in the west wing of the seventh floor of the hospital. The attending, nurse practitioners, residents, and other staff members reviewed patient progress around an oval table while projecting patient info on a large monitor. One of the attendings expressed concern with administering tap water to a patient with kidney problems because he/she could potentially develop phosphate edemas. Another attending was concerned that a high BMI patient received a kidney from a very low BMI patient because a small kidney may not function as well. For their final patient, the attendings were uncertain as to whether or not the hospital has a protocol for an HIV positive patient donating an organ to an HIV positive recipient. This is one aspect of the transplant surgery process that seemed to have “fallen through the cracks”. An attending vocalized her confusion as to why an HIV positive patient should receive an organ from an HIV positive recipient.
Additionally, Dr. Tsvetkova took us along with him on rounds around the transplant and ICU wings. He talked to us about how it is sometimes difficult to access the pancreas in a recipient, so the pancreas is often attached in a more accessible location, such as near the kidney. Dr. Tsvetkova also went on to talk about an objective means of prioritizing which patients get a new liver. There are approximately 5,00 – 6,000 liver transplant annually. Patients are rated on a scale from 6 to 40, where 40 is the worst possible condition. Patients are rated based on certain characteristics of their blood work, such as bilirubin, creatinine, and iron coagulation levels. This method makes the transplant process more quantitative and less biased.
Sarita Deshpande Blog Heading link
-
Sarita Deshpande Blog
Patient-Centered Care
Sarita Deshpande Blog

Bioengineering (and engineering in general) has evolved to focus on user -centered design. In the case of medical devices/approaches in a hospital setting, the user can include nurses, physicians, technicians, and possible even patients. Regardless of how advanced the medical engineering equipment is in the exam room, the physician is still treating the patient, which is why it is absolutely crucial to remember that bioengineering devices should not distract from healthcare delivery, but rather enhance it.
Week 1: Visual Acuity and Visual Field
Sarita Deshpande Blog

This past week in ophthalmology has been great. I was able to observe in the glaucoma and retina clinics, which were both extremely busy. In the glaucoma clinic, I learned about the Ahmed shunt, the Baerveldt shunt, and Express Mini Shunt, which are all options for to lower the intraocular pressure (IOP). Typically, these shunts are inserted after IOP lowering medications and trabeculectomies are not enough. In glaucoma, IOP and cup-to-disc ratio are two quantitative values to measure the degree of the disease. Generally, two tests are conducted consistently for patients with glaucoma: the Humphrey Visual Field test and the Optical Coherence Tomography test. The Humphrey Visual Field measures vision loss, especially peripherally for glaucoma patients. The visual field test works by briefly shining light of different intensities. Patients must press a buzzer when they detect light. The instrument then provides a map of where the retina is able to detect a light stimulus, which provides the physician with information regarding peripheral vision loss. The Optical Coherence Tomography test is an imaging technique that is generally used to measure glaucoma progression and the layers of the retina.
The retina clinic was just as busy; I was only able to ask questions between patients. OCT was used again, but instead to quantitatively visualize the retinal layers. This would provide the physician with information about how healthy the retina, the ganglion cells, and bipolar cells are. In a condition known as age-related macular degeneration (AMD), the macula (an area on the center of the retina) is damaged due to age-related causes. In order to diagnose a patient with AMD, visual acuity and OCT are measured. Another procedure known as fluorescein angiogram is performed by injecting fluorescent dye into the patient’s vein and letting the dye run through the blood vessels in the eye. The ophthalmologist can now visually identify leaking blood vessels. With most patients in the glaucoma and retina clinics, the eyes are dilated. The ophthalmologist can now use a magnifying lens to examine the retina and optic nerve.
The image was adapted from wikipedia.org
Week 2: Cornea and Contact Lens
Sarita Deshpande Blog
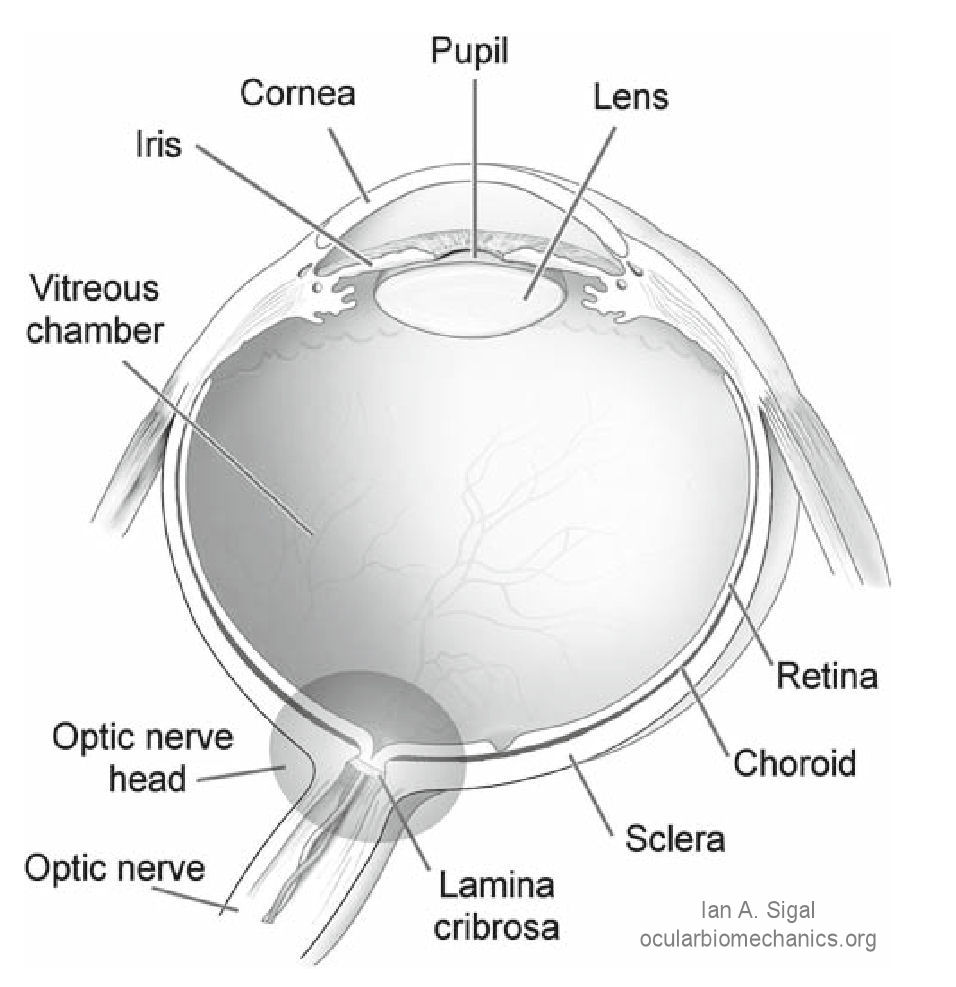
This week we switched rotations to the cornea service and contact lens service. In the cornea service, the ophthalmologist examines the integrity of the cornea and follow-up on post-operative surgeries. Some patients have had cataracts, while others have had corneal transplants. In the cataract surgery, patient’s lens that is cloudy and hazy due to age-related causes is replaced with an artificial acrylic intraocular lens (IOL). During the cataract surgery, the cataract is broken apart via phacoemulsification using a high-frequency ultrasound device. Suction is then used to remove all of the cataract pieces.The ophthalmologist then places one of several intraocular lenses. There are several types of IOLs, namely aspheric, toric, accommodating, and multifocal. Aspheric IOLs differ from conventional (spherical) lenses because the aspheric lens can incorporate changes in lens shape, providing better vision. Toric IOLs are used for astigmatism because they have scale markers for the ophthalmologist to adjust accordingly during surgery. Accommodating IOLs combine aspheric IOLs and haptics; haptics are the “legs” that protrude from the IOL and are used for support. Lastly, multifocal IOLs are used to correct for presbyopia because they magnify the lens (the patient may not need reading glasses after cataract surgery with a multifocal lens). When I spent time in the contact lens service, I noticed that some patients had a combination of ocular issues, so one contact lens could not solve all ocular issues; it usually only addressed a couple of problems. Patients did not feel comfortable with their contact lenses, which led to multiple extra visits with the optometrist.
The image was taken from the Laboratory of Ocular Biomechanics at the University of Pittsburgh.
Week 2: Oculoplastics
Sarita Deshpande Blog

During my experiences in the oculoplastics rotation, I was able to get a more wholistic perspective of ophthalmology as oculoplastics mainly deals with external ocular issues, such as eyelid, tear duct, and orbit problems. Some of the patients in the clinic were in for follow-ups after surgery to ensure that the complications are minimized and the targeted area is healing. I noticed that the time spent with each patient depended on the reason for the patient coming to the clinic. For example, if a patient is having trouble with their tears, such as excessive tearing or dry eyes, the physician can inject a saline-based solution into the lacrimal (tear) ducts to see how well the tears flow. If the tears begin to overflow by coming out of the eye, it means that there is either a partial or full blockage with one of the tear ducts.
One device that is commonly used in the oculoplastics clinic is the exophthalmometer; there are two types of exophthalmometers, the Hertel and Luedde rulers. I saw the Hertel ruler in the clinic. This device is used to measure how much far the eyeball is displaced out. It is commonly used for patients with thyroid eye disease, but it can also be used to measure the retraction of the eyeball inside the eye (known as enophthalmos). The device works by measuring the distance from the orbital rim and the corneal apex. One problem with this device is that it requires the ophthalmologist to hold the ruler up to the patient’s eyes and manually measure the distances. The measurements can be different depending on the physician, so the variability of measurement associated with this device can affect readings, which can then affect patient care. Another problem I had noticed in the clinic is that there is a need for better imaging to photograph the eyelids in a standardized way. Different health care providers measuring eyelid distances should get the same values.
I was also able to observe an exenteration surgery, which is one of three types of eye socket removal surgeries. It involves removing the entire eye socket, including external ocular muscles, tear gland system, and cutting the optic nerve. This is the worst possible scenario, and is generally performed to prevent cancer metastasis. An enucleation surgery removes the eyeball, but leaves the external muscles and the rest of the orbit. An evisceration surgery is when the contents of the eye are removed but the outside of the sclera (the white of the eye) is left. In the exenteration surgery, the patient was placed under general anesthesia, and the attending worked efficiently to balance teaching the residents and completing the surgery in a timely manner. After the entire eye is removed, a partial-thickness skin graft is removed from the thigh using a surgical tool called the dermatome. The skin graft is then cranked through a mesh, which expands the graft to its maximum size and removes any excess blood. The graft is then placed into the lining of socket.
I had noticed that the surgery generally went very smoothly. The attending was able to teach and let the residents/fellows perform the surgery as well. There was some time lost because the dermatome was not getting the right thickness of skin, so it took a couple tries for it to work. The skin would also dry up quickly so oil had to be reapplied to the skin graft every couple of minutes in case there was a delay in placing the skin graft into the eye.
Note: the images were taken from integralife.com and https://en.wikipedia.org/wiki/Exophthalmometer
Week 3 – Retina and Pediatrics
Sarita Deshpande Blog
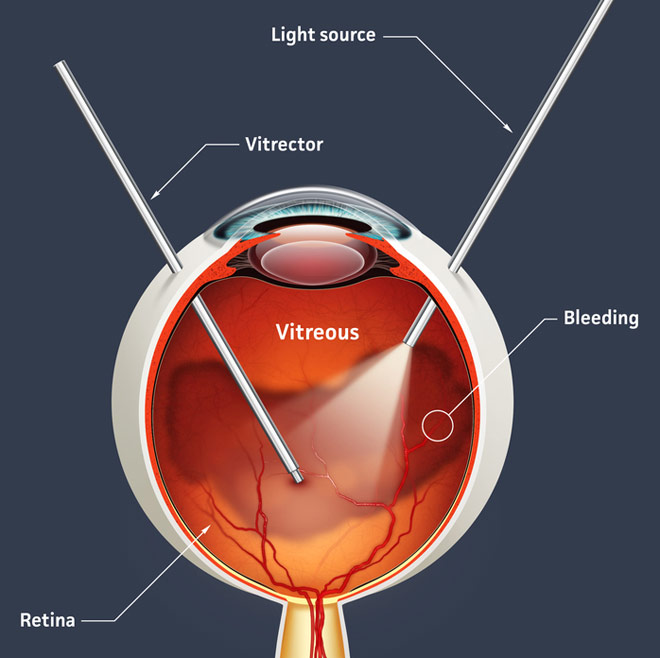
This past week I was given the opportunity to observe in more retina and pediatric surgeries. The majority of the retina surgeries we observed were pars plana vitrectomies, which is a procedure that removes the vitreous humor from the vitreous chamber (located in the back of the eye). A vitrectomy is performed to remove the vitreous humor; this may occur for retinal detachments or vitreous hemorrhages. It can also be performed when the vitreous humor becomes clouded or contaminated with blood. The image above shows how there are infusion “ports” through which the surgeon gain access to the vitreous chamber with the necessary devices. The ophthalmologist suctions the vitreous gel out. After (if indicated), the surgeon uses laser to treat any holes or tears in the retina via photocoagulation. Then, silicone oil or gas is injected to ensure that the retina remains attached to the back of the eye and does not collapse. If silicone oil is used, it must be removed after the retina has healed. There are, however, some complications with using the silicone oil. The oil can enter into the anterior chamber, causing an increase in intraocular pressure (IOP), which may lead to open-angle or close-angle glaucoma. Increased IOP has also been shown as a complication for intravitreal gas vitrectomies. The gas can alter scleral rigidity as well. There needs to be definite improvements on how the silicone oil is removed from the eye, preventing further complications.
For pediatric ophthalmology, the main surgeries performed are strabismus surgeries, which corrects the extraocular muscles for improved ocular alignment. Strabismus is when the eyes are not aligned; it is also know as cross-eyes or wall-eyes. One or both eyes can move in different directions, which often causes double vision. There are generally two types of strabismus surgeries: recession (muscle is cut and reattached further back on the eye) and resection (muscle is cut from extraocular portion and reattached closer to the front of the eye).
Note: the image was taken from www.allaboutvision.com
Opthalmology in Conclusion
Sarita Deshpande Blog

Several bioengineering technologies are commonly used throughout the ophthalmology clinics, namely the slit lamp, indirect ophthalmoscope, visual field exams, and imaging scans. These devices and technologies can be updated to improve patient care. For example, the slit lamp is used for an ocular examination with every patient. Yet there is still a high rate of cervical stenosis and scoliosis for ophthalmologists. This technology can definitely be improved to make both the physician and the patient more comfortable. The portable slit lamp serves as an excellent first step towards improving the slit lamp technology. With respect to user-centered design, medical devices or products can be personalized for the patient, such as for contact lenses. A possible research development is that contact lenses could be customized via 3D printing to address multiple ocular problems for patients.
A commonly noted problem in the ophthalmology clinics is patient wait times. The technician begins the examination by measuring visual acuity and visual fields. Many patients must also get an Optical Coherence Tomography which is a light-based imaging test that takes pictures of the retina before being examined by the physician. Research in ophthalmic imaging techniques also show options for high resolution imaging, which can be utilized to improve patient care as well. The current imaging instrument, known as the Optos, combines imaging techniques, such as ophthalmoscopy, fundus, fluorescein angiography, and indocyanine green angiography. The instrument can be improved upon with respect to speed of examination and ease of use.
After interviewing patients, physicians, technicians, and administrators throughout our three weeks, our team noted that the most common issue in the clinic was patient wait times and patient flow. The clinic would like to move completely to electronic medical records (EMR), but the financial costs involved are slowing the transformation.
In conclusion, my three weeks in the ophthalmology clinic has been absolutely amazing! I learned a lot about medical devices and technologies, and I am looking forward to my next rotation.
Week 4 – Introduction to Interventional Radiology
Sarita Deshpande Blog

The first week of interventional radiology has been going great so far! I am excited to learn more about this upcoming field with my new group as well. During the week, we were able to observe procedures in the IR rooms. Some of the equipment/devices that are commonly used are wires, catheters, imaging techniques (of course), stents, filters, sheaths, etc. Catheters can come in many sizes with different functionalities, but they all serve the purpose of either drainage or administration of drugs and fluids.
On the first day, I observed a renal angiogram for a hypertensive patient (see picture above for what a renal angiogram looks like). An angiogram is used to visualize arteries. In this case, the hypertension caused narrowing of blood vessels (also known as stenosis) in the kidney. For the procedure, the IR physicians used a balloon to open up and dilate the blood vessels. Contrast dye was used to better visualize the vasculature in the x-ray. The physician can then literally see where the stenosis is and where the balloon needs to be placed, which is known as balloon angioplasty. A balloon catheter is passed “over the wire” and then inflated once its target site is reached. The inflation causes the vessel to expand, and the balloon is then deflated and removed. One problem associated with balloon dilation is that there should be a way for the physician to know how much the vessel has been dilated. Yes, imaging is available, but if there were a more immediate way to deliver that information to the user, it could potentially lead to better patient care.
Another interesting procedure I observed was a transcatheter arterial chemoembolization (TACE). It is used to restrict a tumor’s blood supply by embolizing the vessels leading to the tumor, and it can also deliver targeted chemotherapy to the tumor, leading to atrophy. Generally, this procedure is only done in the liver because the liver is supplied by the proper hepatic artery and portal vein. The chemotherapy medication is bound to a drug-eluting bead, or microsphere, which then can deliver targeted drug therapy of high doses to the tumor. It has been used for hepatocellular carcinomas (HCCs). The catheter is passed through the abdominal aorta, and then through the celiac trunk and common hepatic artery, and then reaches the proper hepatic artery. Then the physician uses angiography to determine which smaller arterial branches are supplying the tumor and embolizes them.
From a bioengineering perspective, TACE is an interesting procedure because it involves targeted drug-delivery. This topic is growing in the bioengineering field as new research is constantly coming out. Some aspects of TACE that can be improved upon are including the use of biodegradable particles because technically, the particles never leave the body after infusion, loading multiple drugs onto one sphere, and increasing the specificity of the beads to ensure that the tumor is targeted appropriately.
Note: the images were taken from openi.nlm.nih.gov
Week 4 – Over the Wire
Sarita Deshpande Blog
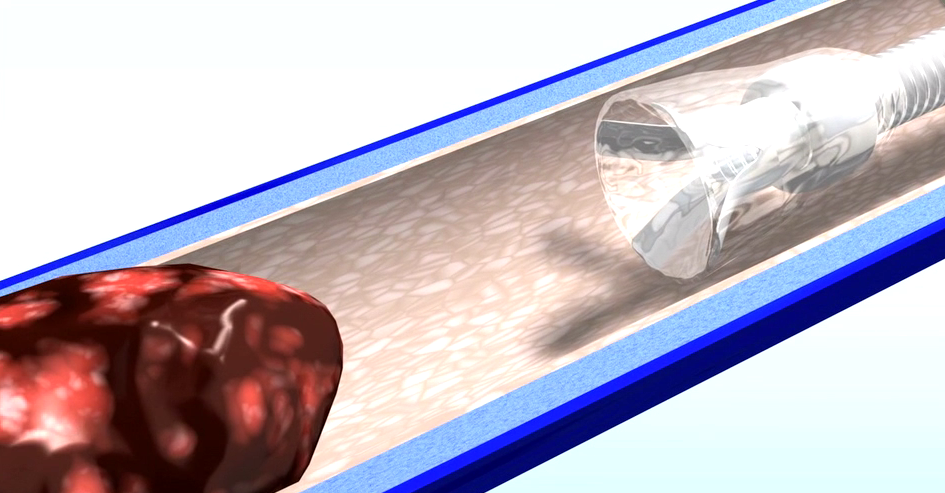
Interventional radiology is constantly being updated with new technologies and devices. For example, the AngioVac Cannula is a device manufactured by AngioDynamics. It is used to remove emboli, or clots, in veins. It works by using suction and vaccuuming up clots in large veins, like the superior and inferior vena cava. The tip is a balloon that can be expanded in a petal formation, which prevents the cannula from clotting from the emboli. One problem with this device is that it is fairly large, so it can only be used for large veins (IVC, for example). Perhaps the device could be made a bit smaller to allow it to perform more elegantly, which will also help the physician maneuver the cannula better.
I was also able to learn a little bit about the history of interventional radiology. One of the major advancements within the field is known as the Seldinger Technique, which was developed by Dr. Ivan Seldinger in 1953. It is used to obtain access to vasculature through a wire. A cannula/catheter/other device can be passed “over the wire” and the wire is removed. It can be used for angiographies, chest drain, or other procedures. Throughout the week, our group was able to observe in many procedures in the IR rooms.
Vascular access procedures are typically used when IV is not enough. In the cases I observed in, the physician placed a chest port to provide chemotherapy as a method of targeted drug delivery using image-guided techniques. The ports are devices that contain a reservoir attached to a catheter. It is subcutaneously inserted into the chest (in some cases, the arm as well) and the physician then guides the catheter into a vein. This procedure is used to deliver systemic chemotherapy, unlike transcatheter arterial chemoembolization.
This week has been truly amazing and the technology/innovation in this field is easy to see. I can’t wait to learn more!
Note: the image was taken from http://www.angiodynamics.com/products/angiovac
Week 5: VisualizationSarita Deshpande Blog
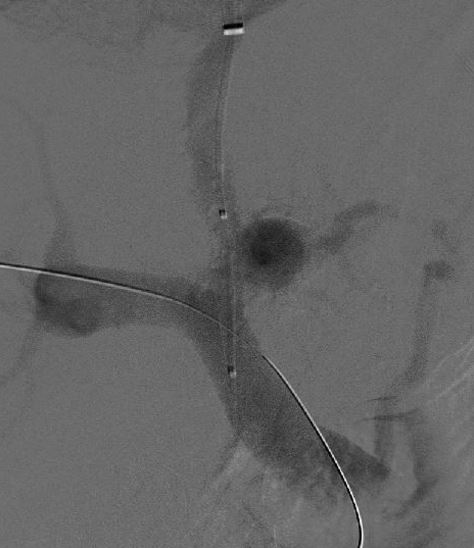
This past week was great so far! I was able to observe in some more procedures, including a transjugular interhepatic portal shunt system. It involves placing a stent between the portal and hepatic veins to correct for portal hypertension. The stent is a covered and contains a open-ended cage that is placed in the portal vein. The other end of the stent (covered) is placed at the very end of the hepatic vein. The stent is deployed using an inflatable balloon. Once again, the procedure is done “over a wire,” highlighting the finesse in the field. One of the problems I had noticed with this procedure is that it requires a blind puncture between the hepatic and portal veins. The physician had mentioned that it takes skill and practice to have a better understanding of how to navigate from the two veins, but there is still a lack of visualization. Another observation I noted was that the stents are static, not dynamic. They do not change according to the patient’s needs; for example, the stent is unable to accommodate for increased or decreased blood flow. If there were a way for the stent to regulate flow, it would definitely be an improvement and provide better, more personalized care for the patient.
I was also able to observe in on a hemodialysis reliable outflow (HeRO) device procedure, which was done in the operating room on the third floor. This procedure is novel, and it is used for patients who need an alternative form of hemodialysis. The HeRO device is an arterial graft connected to a central venous catheter. Overall, from my observations in the last 1.5 weeks, I have noticed that better visualization for the physician and more immediate and quantitative feedback about the device are potential problems.
The image was taken from wikipedia.org.
Week 5: Devices
Sarita Deshpande Blog
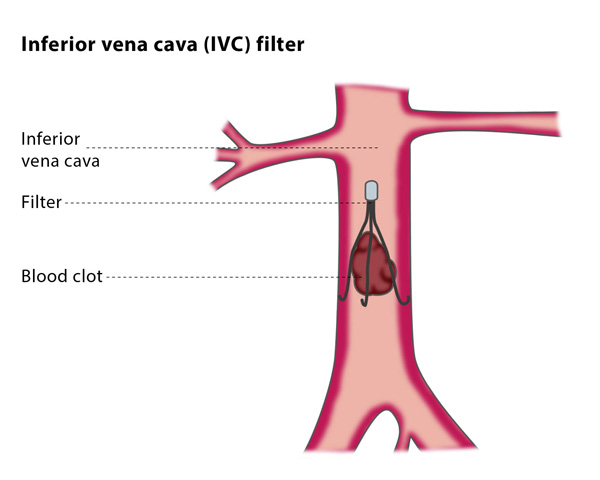
This past week, I was able to observe in even more procedures and gain a better understanding of interventional radiology as a whole. One experience that was particularly memorable was observing a percutaneous nephrolithotomy, which is performed to remove a kidney stnoe. The interventional radiologists prepared the patient by setting up a catheter and guide wire directing the position of the kidney stone. The urologists would then perform the nephrolithotomy in the operating room.
In the middle of the nephrolithotomy procedure, the urologists were forced to stop because the nephroscope was broken. The other available scope was being sterilized which could take up to 2 hours. It is problem to have missing/nonfunctional equipment that is necessary for the surgery because it impedes patient care. Eventually the surgery was performed and the kidney stone was removed. However, there were post-operative complications. The interventional radiologists went back in to determine whether the patient was bleeding, which the patient was. After doing a renal angiogram, it was determined that the patient had several sources of bleeding in the renal calyx, so the kidney was embolized.
I found this case to be very interesting because it highlights the collaborative nature of medicine. The interventional radiologists made the procedure minimally invasive, and the urologists are the ones who actually degraded and removed the stone. The interventional radiologists went back and treated any complications.
Some observations that I have made from my past two weeks in interventional radiology span from devices to processes/flow/communication. One device that I found interesting is the inferior vena cava (IVC) filter using for patients with severe embolisms and thrombosis. The filters work by mechanically acting like a barrier to break down the clot as it passes through. One problem is that for some patients, multiple IVC filters need to be placed in to be effective. Perhaps there is a better way.
Note: the picture is taken from http://www.pedesorangecounty.com/venous-treatments/
Week 6: Collaboration and Workflow
Sarita Deshpande Blog

I was able to see a nephrolithotomy from the beginning with IR to the end with urology. The last time IR participated in a nephrolithotomy case, the nephroscope was missing, so I wasn’t able to fully see the procedure. It was really amazing to see how the kidney stones were removed, both manually and with the laser. The urologist used the pathways set up by the interventional radiologist, which made the procedure minimally invasive. One problem is that the fluoroscein machines are not as advanced in the operating rooms when compared to the IR department. This can sometimes cause the machines to overheat because of overuse.
In general, the interventional radiology department works efficiently with respect to patient management and flow. However, areas for improvement include communication and equipment/waste management. Some patients require an anesthesiologist to be present during the procedure because of higher operative risks or underlying medical problems. The IR team and the anesthesiologist may not always communicate effectively, leading to lost time. Equipment may sometimes be on back order, so it may not always be available. With respect to waste management, distinctions are not made between regular waste and biohazard waste in the IR rooms. This leads to increased costs in treating regular waste as hazardous waste, that could be reduced.
Note: image taken from www.svuhradiology.ie
Interventional Radiology in Conclusion
Sarita Deshpande Blog

This was the final week of the program, and my time in interventional radiology has been amazing. Our group had a great mentor, Dr. Bui. Today he showed us the basics on how to use/interpret an ultrasound. An ultrasound works by transmitting sound waves (generating by piezoelectric crystals in a transducer) that bounce off of tissues and bones at different frequencies. This allows the user to visualize distinct anatomy and physiology.
In summary, interventional radiology is a highly innovative field. From my experience, there is a company representative who proposes new devices or new applications for devices every week. However, there could be some improvements with devices. Stents are static, not dynamic; they do not respond to changes in flow or pressure, which is a potential area for further research. There are also challenges with deploying stents. For example, in some procedures, stents will spring forward unexpectedly. Generally, improvements could be made upon increasing the elasticity of devices (especially catheters) and increasing the efficacy of devices, such as inferior vena cava filters. Improving feedback and regulatory mechanisms in devices is an opportunity for innovation. For example, a kyphoplasty is performed to treat vertebral compression fractures by injecting cement into the bone to maintain shape and rigidity. The physician injects the cement until adequate pressure is felt. There could be improvements regarding changing the subjective nature of injecting the cement to a more quantitative, objective one.
Presently, two-dimensional (planar) imaging systems are used to navigate three-dimensional tissue and vasculature. This leads to limitations in depth perception when placing catheters/wires in vasculature and stents in certain procedures. Visualization in imaging is critical, so improving visualization should lead to better patient care. However, it is still important to keep the patient comfortable while obtaining images. In an angiogram, the patient must be apneic to obtain the best image; if not, the image must be taken again. The time spent for each procedure could be minimized, which leads to better patient care. Improvements in imaging may also refer to imaging techniques used for specific procedures. The transarterial chemoembolization (TACE) procedure is used to deliver chemotherapy to hepatocellular carcinoma. It works by restricting the tumor’s blood supply (embolization) while delivering chemotherapy via drug-eluting beads. It can be difficult to visualize the arteries leading to the tumor. Currently, there is a technology called the EmboGuide manufactured by Phillips, and it provides better visualization for the arterial feeders leading to the tumor.
From this program, I was able to better appreciate the the interdisciplinary nature of bioengineering and medicine; engineering feats are all over the clinic! From systems processes, such as keeping up with the flow of patient care, to device and imaging modalities, the opportunities for innovation in interventional radiology are endless.
Note: image taken from radiology.ucsf.edu
Emil Klosowiak Blog Heading link
-
Emil Klosowiak Blog
Post 1: Introduction to Anesthesia
Emil Klosowiak Blog
My first rotation is through Anesthesia. People in the medical field express that anesthesia contains a lot of physics and physiology, two thing I enjoy so I am particularly excited to learn more about the field. Also, from what I understand, anesthesia is unique because it allows for observation and monitoring of the entire OR in many different situations, creating the potential for a more wholistic view of the OR than say a specialized surgeon.
So far I am really captivated by the whole experince. I am learning a lot about the medicine of anesthesia. I can’t highlight enough how very important it is to be observing/interacting with someone who is willing to share their expertise in the field, especially at this stage of observation. Even though the primary purpose of the rotation is “needs assessment” a certain baseline of knowledge is crucial for making informed observations and deductions.
Quick note on morning lecture – predicting difficult airways; The day started with a very informative lecture on airway management intended for the new residents. In undergrad my senior design project was to improve upon existing airway management manikins so it was fun to hear about the subject again. At the end of the lecture the doctor and fellow did presentations for different airway management techniques using an airway management simulator. Having worked with the manikins in the past, it was no surprise to me when the doctors exclaimed about how the manikin texture was too sticky for intubation, the tongue unrealistic and the jaw and neck too stiff. These were all parameters that my design team and I found to be the problems with the manikins, all of which prevent realistic learning or practice to occur on the manikins. This may be a subject I might want to engage again.
Day 1 case- moyamoya bypass
Day 2 case – triple coronary bypass esophageal echocardiogram ultrasound guided IJV line placement
I watched two major procedures and one observation that really stood out to me was the fact that both cases required significant prep time once the patient was already in the OR. From some of the assigned reading, there seems to be a push for more efficient use of OR time. Boiling the idea down, efficient use of OR time would allow for more surgeries which allows for helping more patients and more $$. Therefore cutting down on inefficiencies would be beneficial. I can’t make generalizations after only observing two procedures but here are a few tasks that stuck out as opportunities for improvement and that I definitely want to keep an eye out for in days to come:
- sterile bagging of equipment (ultrasound, microscope)
- sterile field needed for IJV line
- lack of defined space for certain objects (“christmas tree” airway tube attachment for bed)
- pinning mechanism cranial cases: cumbersome, required three people, hair gets tangled
- interference of electrical equipment (IV tube heater) with electrical signal recording (EEG, SSEP)
- fiber optic headlamps require power cord, stand, re-plugging of fibers when surgeons move/switch spots
- placing arterial lines, placing IJV catheter
- tangled cables (IV)
- tangled cables (EKG)
- tangled cables
- IV tubes hang down on floor and are stepped on
- Power lines are tripping hazard and prevent easy mobility of mobile equipment
- Power lines on mobile equipment have no designated holster when equipment (bed) is wheeled around/out
These are some of my initial thoughts. Stay tuned for more.
P.S. Apparently we have to attach a picture with each post. I didn’t know that so for now I’m attaching a photo of the crazy mess of IV tubes on top of the IV pumps.
Imaging in anesthesia
Emil Klosowiak Blog
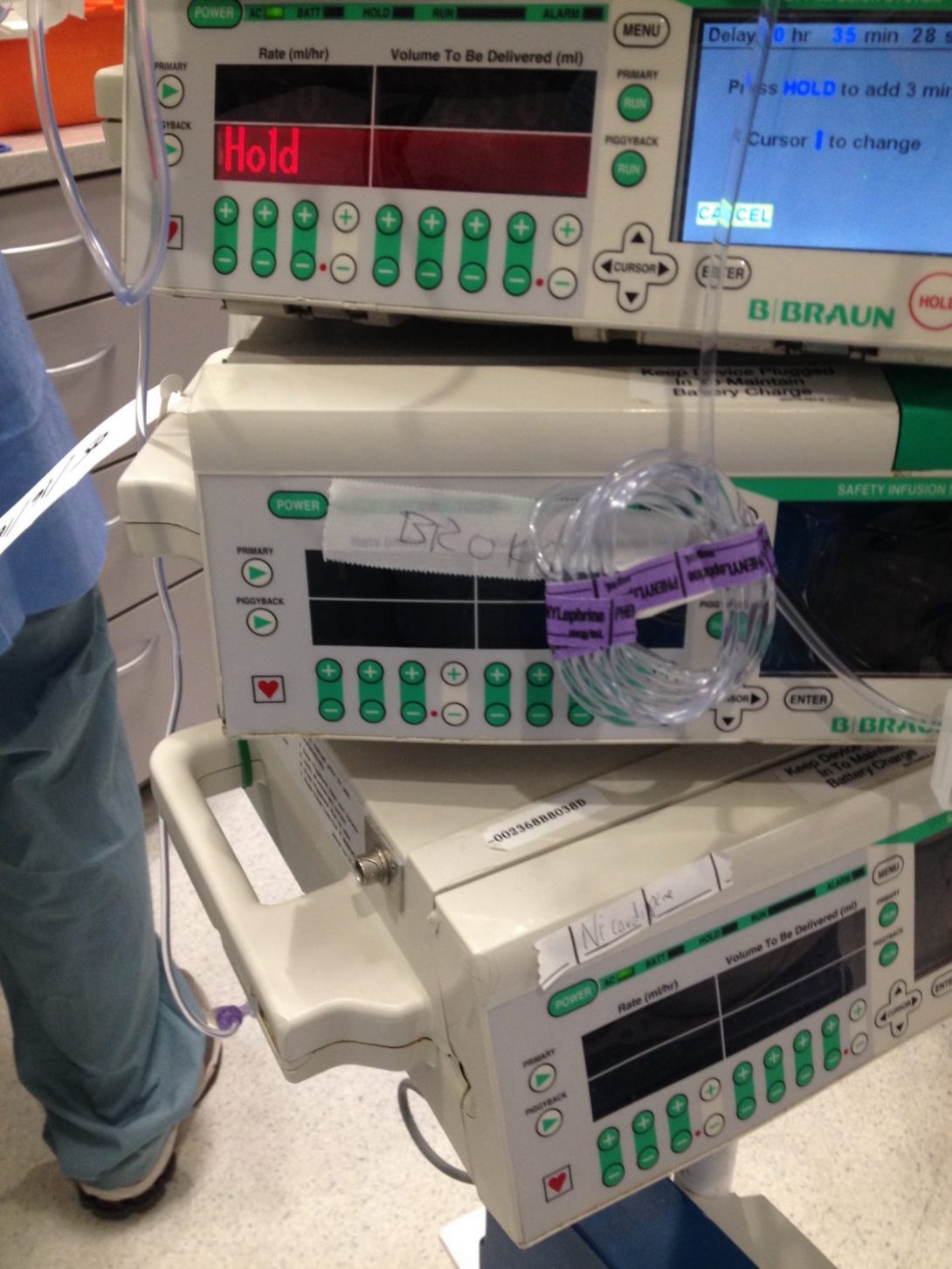
I was not expecting as much imaging in anesthesia as I have experienced so far. Imaging is used in what seems like two main categories: monitoring/diagnosing of patient’s condition and as an aid during procedures. Here are the types of imaging I have seen so far:
- Trans-esophageal echocardiogram (monitor the state of the heart during bypass surgery)
- Ultrasound of jugular (aids in placing jugular catheter)
- Ultrasound of brachial plexus (aids in regional sedation of arm)
- Ultrasound of wrist/forarm (aids in placing arterial line)
- Visualizing the airway (aids in intubation)
- Xray of chest for pneumothorax (check for possible pneumothorax/collapsed lung)
For the imaging that is used as an aid during procedures I was interested to learn about the efficacy of these “aids”. Does using ultrasound actually help in placing a jugular line? After a quick Pubmed search, Brass et al. found that “Based on available data, we conclude that two-dimensional ultrasound offers gains in safety and quality when compared with an anatomical landmark technique. ” . This seems to be true of the other procedures as well meaning imaging has a significant potential for improving patient care and making these procedures faster. However, even with the help of ultrasound (US) there still seems to be difficulties and complications that arise frequently. Sometimes it took several attempts to place an radial artery line, placing the IJV catheter was quite messy and took a long time and one arterial or venous line “perforate” (I think thats what they called it; probably venous bc arteries are usually not used for drug delivery) which meant that instead of supplying drugs to the circulation, the drugs deposited locally into the patients forearm. This created confusion because the patient stayed “awake” even after receiving large amounts of drug and the perforation was only noticed after several minutes of trying to figure out why the patient was not yet asleep. Point being, imaging is already proving to be a useful took in aiding of procedures but there is certainly room for continued improvement either in imaging and its application or in the procedures themselves.
Something that I found true for all the imaging was that it is not obvious and sometimes difficult to orient oneself in the image. The echocardiogram revealed a lot about the heart, its valves, its chambers, the vessels flowing in and out but only when the physician pointed out the landmarks. The probe was adjustable in three planes so the perspective changed continually. With training all these images can make sense, but to a novice the can be very confusing.
Certain imaging machines were not well labeled. As an example, the echo machine and dozens of sliding knobs, but non of them said what they do so I never actually figure out what they were for. I’ll have to ask next time.
The image I am attaching goes back to my last post. I observed a resident who was meticulous about his IV line organization and his strategy was to roll up the tube and then tape it up with tape that says what line it is (specific drug or saline).
DaVinci hernia repair and MI
Emil Klosowiak Blog

I was able to observe my first robotic (DaVinci) surgery today. It was during a bilateral inguinal hernia repair. The surgery was greatly complicated by the fact that the patient had COPD and congestive heart failure. Another complication was that the patient had to be in trendelenburg position, where the pelvis is elevated above the head. From what I understand this position is in order for the abdominal content to “fall” away from the sight of surgery (pelvis). The problem is that the abdominal content “falls” onto the diaphragm making it more difficult to ventilate the patient and with COPD the difficulty was only exacerbated.
The DaVinci was fascinating. I was impressed with how precise the movements of the surgeon were. I guess I was expecting frequent overshoot or undershoot of the robotic arms but it looked like almost all the movements were spot on.
In the last 1/4 of the surgery, the patient began to show elevated ST segments. After closing, the EKG got more erratic and eventually the patient went into VTAC. The defibrillator was used, the rhythm restored but VTAC occurred again. Within several seconds the patient restored his own rhythm, but preparations were immediately made for transfer of the patient to the Cath-Lab (interventional cardiology). There, using a femoral catheter, a block in the LAD was found and stented. It seems that the surgeries have been improved to great extents and are very efficient. The inefficiencies occur during set-up, take down and transfer.
During the hernia repair and in the interventional cardiology OR, I was reminded to speak very quietly because the surgeon had to communicate with staff from a distance in both cases. In both situations mic-speaker systems were in place but everyone had to be conscious of interfering with the mic-speaker system. It obviously necessary and possible to speak quietly, but it did make communicating and therefore learning more difficult.
I’ve continued to keep an eye out for repetitive problems/inefficiencies. I saw several medical staff trip, stumble or kick aside either tubes, wires or power lines in this one surgery alone.
I’ve also noticed consistent problems with the beds:
- no specific place for power cord (they are dragged along or put on top of the patient
- no specific place for machines (monitors, defibrillator, O2 tank; they are put on the bed next to the patient and while moving patient from bed to bed the machines have to be moved out of the way)
- IV pole has to be pulled along by a person so that lines don’t get disconnected
- no place for patient’s chart (it was misplaced by the time it got to the ICU)
- no place for patient’s belonging (inhaler was just put on the patient when moving)
- about a dozen cables have to be unplugged for the bed to be mobile (this took at least 5 min, preparing the bed for moving is quite the process)
- system problem: while moving bed with a patient experiencing an MI, they still have to wait their turn for the elevator while on their way to the Cath-Lab (interventional cardiology)
Some reoccurring problems I’ve noticed:
- medical workers try peripheral nerve stimulator on self
- drug trays/boxes are kept on the floor (see attached image)
- trouble ventilating patients in trendelenburg
- Anesthesiologists only saw the back of the screen in the Cath-Lab, the room is not designed to include the anesthesiologists, they kept walking around the entire table to come see what is happening (this was also true in the other radiology suite)
The root of the problem
Emil Klosowiak Blog
The root of the problem
Emil Klosowiak Blog
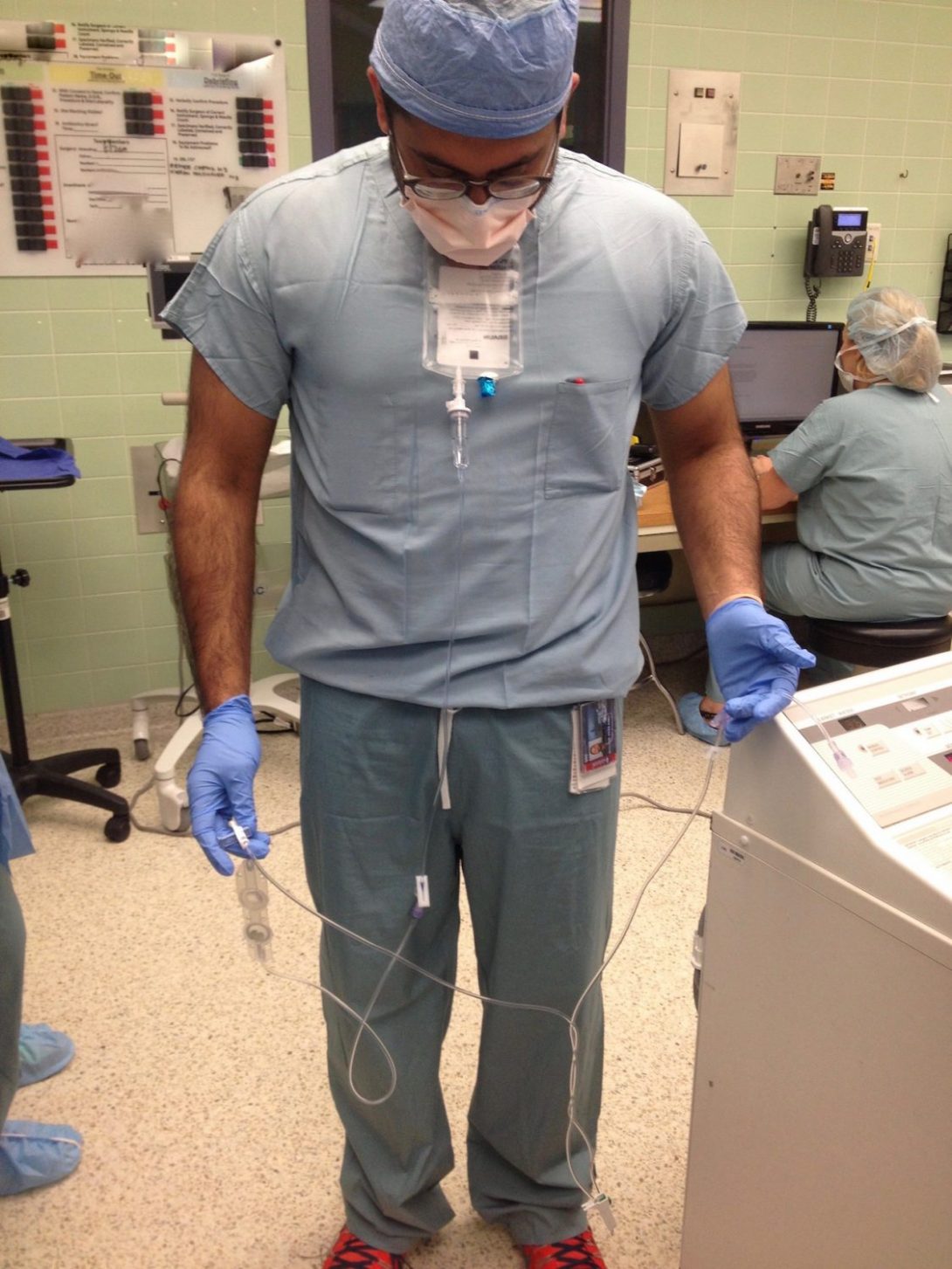
Image: The image shows a resident who hooked up a new bag of solution to an IV tube for the patient and now has to let the solution drain through the line so that air isn’t introduced into the patient. The IV tube is very long which means the resident has to deal with making sure each consecutive segment gets below the bag so that gravity can feed the liquid through the tube. So far I have seen physicians deal with this problem by dropping the IV on the floor or into a trash can and then pulling the tube up, thereby displacing the air. All the systems are effective but at what cost? is the sterility of the IV something to consider? Is it a foolproof method that removes all the air? As an outsider it seems like a silly yet simple maneuver.
To further a previous post, I saw another arterial line being placed again. It required many passes and two sites of insertion.
There is an issue I have been seeing over and over and it is medical waste produced in the OR. All waste in the OR is split into only a few categories: sharps, red bag waste (biohazard=blood/tissue), and trash. There is no recycling, not of unsoiled packaging or tubing. There is no collecting of of cloth/material that was not soiled. There is no collection of gloves. There appears to be a huge opportunity for collecting certain materials for reprocessing of some sort. Currently trash cans are somewhat randomly placed around the OR, but with come planning and placement, materials worth collecting can be identified and collection containers can become a presence in the OR.
The thing is, just like other big issues that come up (sterility, communication), they are a cultural phenomena and need cultural change. No matter how good a design is, culture has to change first. But I believe it has to be a top-down approach. If I work in the OR and want to recycle, its impossible. Even if I get recycling bins into the OR, others won’t recycling unless they are prompted by their superior. I think that is also true for creating a strict culture of sterility or a open and effective culture of communication. The “boss” has to dictate that “this” is a big deal and we want to see “these” improvements. Just a thought.
Anesthesia in summary
Emil Klosowiak Blog

Anesthesia has been a fantastic specialty to shadow for the last three weeks. By its very nature, anesthesia is involved in a lot of surgical and a few non surgical specialties from neurosurgery, to interventional cardiology to pain clinic. I have greatly enjoyed the diversity of cases that I got to see. It also an invaluable position to hold in the hospital. By necessity the anesthesiologist is well connected with hospital staff in various departments. This means that anesthesiologists are able to observe and identify cross-specialty themes and are also in a place to communicate about them with physicians in various specialties. In a way anesthesiologists are observers of the OR, maintaining the patient but also being an catch-all of the goings on. It is a prime position for identifying needs in anesthesia and the OR in general.
During our final talk with our mentor, he tried to sell on us why we should do anesthesia as as a specialty. His points include:
- diversity of patients from children to adults from every specialty
- you can take breaks during operations
- the strong ties to physiology in anesthesia
- he gets to wear pajamas all day
Anesthesia seems like a great place to innovate in with many new aspects to the field such increasing use of imaging during treatment, AI, better electronic records and increased evidence based practices.
New topic:
We spent a day in pain clinic. It was very different from OR anesthesia. We mostly watched procedures but supposedly its much more clinic based. The procedures we watched were mostly related to back pain. The patients were getting longer lasting epidural shots in order to deal with the pain. There was a lot of fear from the side of the patients. The procedures are only done with local anesthetic and even getting the local anesthetic is not very comfortable. There was a lot of wincing and grimacing from the patients. After all, they are getting a long needle stuck into their back. Its hard to make any great observations after only one day in the pain clinic.
p.s. the painting is from the hallway in front of the pain clinic. I thought it was cool.
Interventional Radiology
Emil Klosowiak Blog
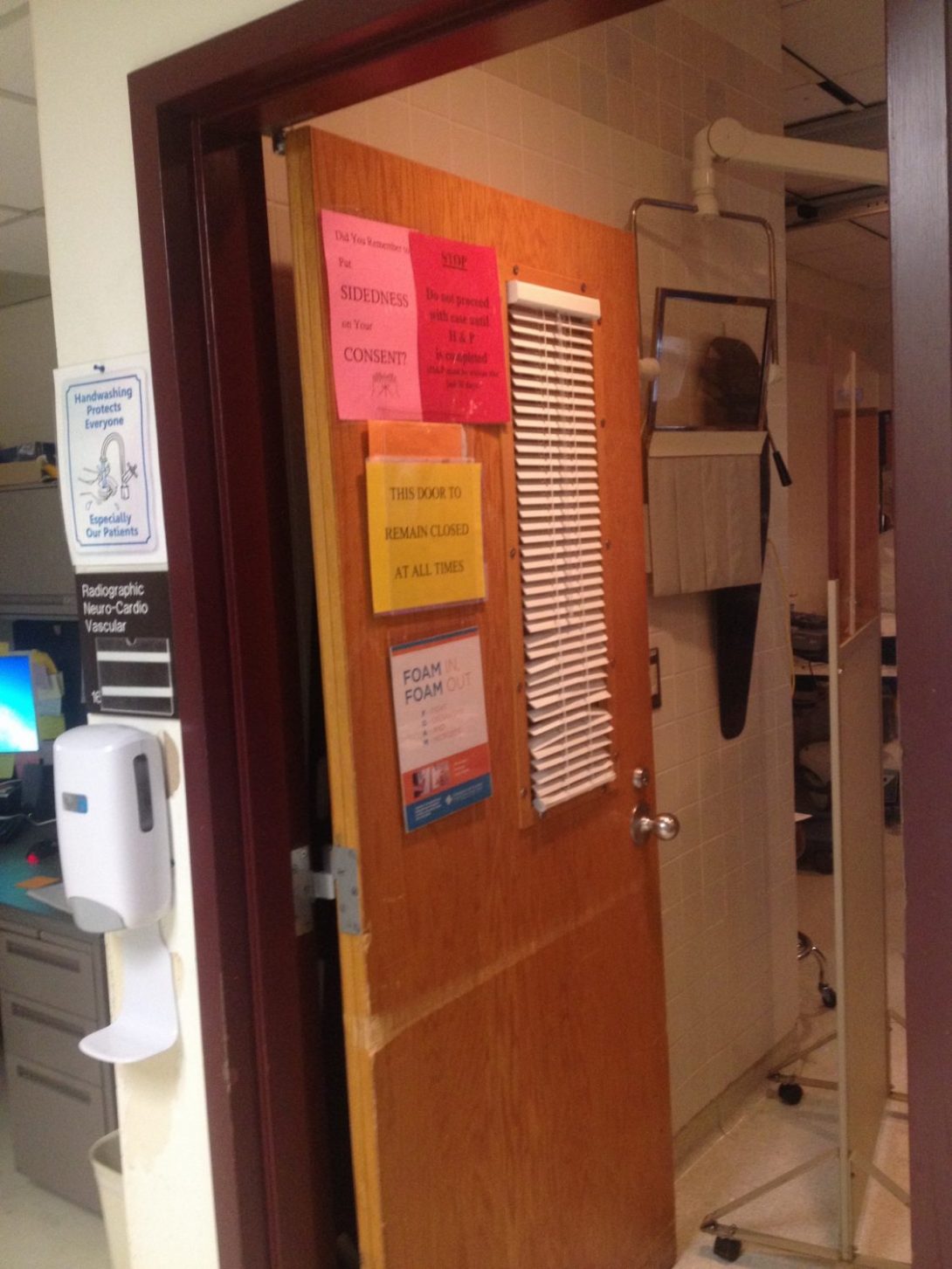
First impressions: IR is cool. The use of various imaging modalities to improve patient care and complete minimally invasive procedures is both efficient and effective. I have not seen them place central lines “blindly” but with ultrasound guidance. It seems much cleaner than doing it blindly which was standard practice in the OR. IR has a diverse scope of procedures so I am learning a lot and asking lots of questions about what is going on.
One of the primary tools IR uses are catheters or various kinds. The thin catheters allow the doctors to perform tasks “at a distance” in small areas that might be impossible to access otherwise. There is certainly skill involved in using the catheters, pushing, pulling and turning them to guide them in the correct direction. However, even the most experienced doctors require several passes at most junctions, simply by nature of the anatomy and fluid flow. It seems that a big improvement would be catheters that can be more precisely directed in the patient around tough obstacles. Balloons are also a common tool and they tend to be stiff, making them difficult to maneuver around obstacles as well, sometimes limiting their access to areas they are needed. I will certainly keep an eye out for this.
Another area that required some guesswork was blowing up balloon catheters in vessels. This is done for various reasons. The pressure of the balloon is seen and controlled. However, there is no feedback on the magnitude of force the vessel puts on the balloon. In one case, fibrous bands surrounding an artery had to be broken by use of such a balloon. Even with the burst fibrous band, the artery could return to the original shape. Therefore, telling weather the band broke or not was difficult. The risk of the procedure is pumping the balloon too much and bursting or dissecting a vessel. I want to continue to observe this practice and see if there is a need for more feedback from the balloon.
Doctors almost always have to kick the foot pedal around to get it into a desired location. Drs also trip on the pedal occasionally.
Patient is on the verge of coding after procedure. Patient had a history of trouble ventilating. Rapid Response Team was called- RRT. Dr. thought it was Respiratory Response Team. The patient needed to be intubated but nobody on RRT was qualified so only then was anesthesia called and they intubated. Classic inter-disciplinary miscommunication. With the code, at one point there was 40 providers in the room from 5 different departments. For each new provider of importance all the pts stats and info were shared over and over. Very interesting to observe.
Red bag waste is supposed to be for biohazard material including blood and tissue. Regular trash and red bag seem to be interchangeable in the IR suites. Something I hope to keep an eye on.
Photo: Doors tend to stay open in the OR even with signs that specify that doors stay closed at all times (open even with patients and radiation occurring inside). Perhaps because the doors have knobs to turn rather than levers. This means it would be impossible for doctors in sterile dress to open the door and leave. Doctors have to leave the rooms frequently when certain radiation modalities are used. Perhaps new door mechanism are in order to increase compliance of keeping doors shut.
hemodialysis and stabilization
Emil Klosowiak Blog
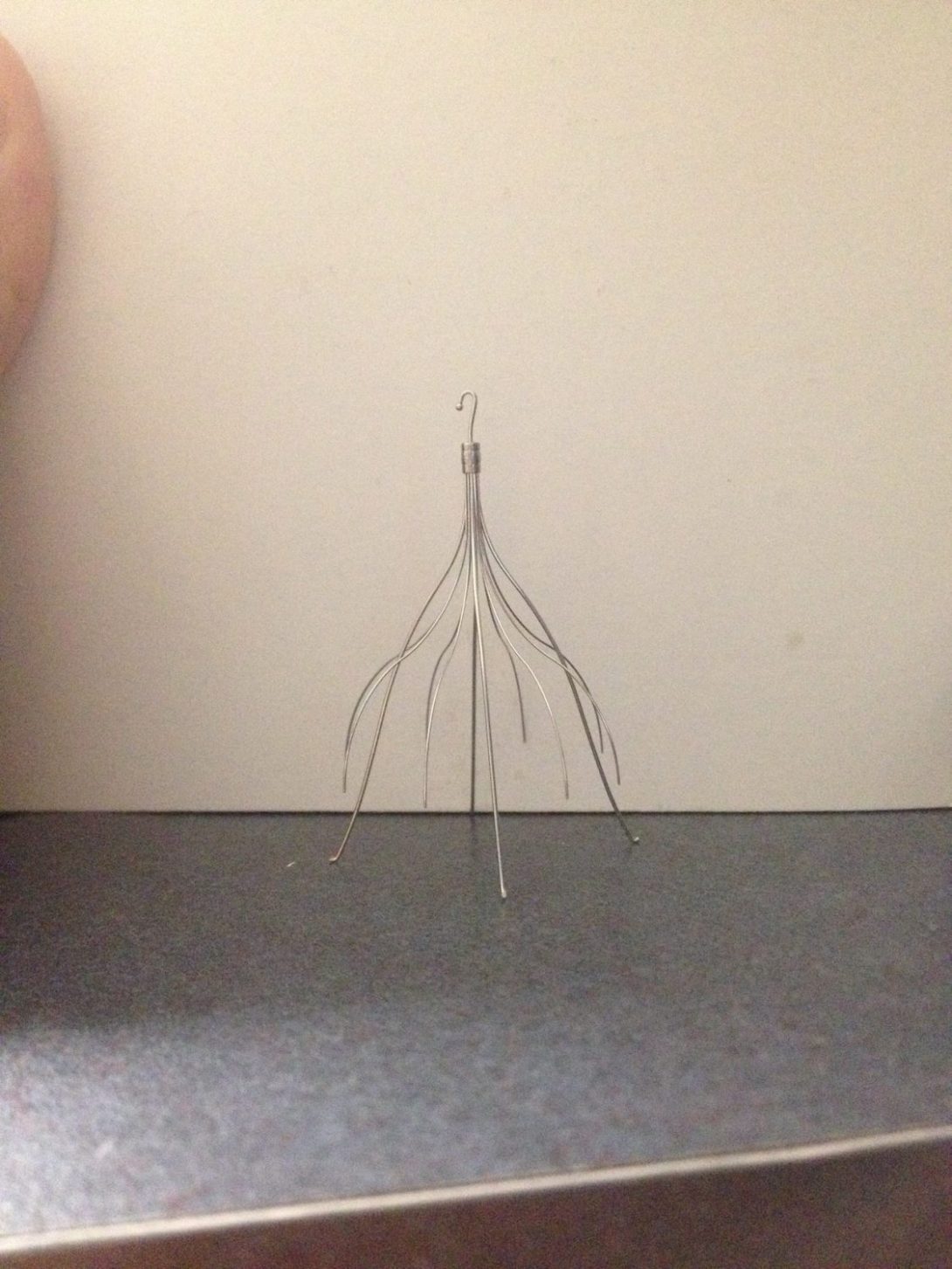
Hemodialysis is crazy. Hemodialysis is the filtering of blood which has to be done for patients with renal failure. Renal failure is frequently due to uncontrolled hypertension and diabetes. Patients have to get hemodialysis 2-3 times a week. They have to filter all of the bodies blood so we’re talking high flow rates which means big needles. Access to a good artery/vein for high volume blood draws 2/3 times a week in not natural, so an artificial access is created. This access can be anywhere on the body but are most frequently on the arm since that is the most convenient. There are two primary access types. Fistula where a vein is directly hooked up to an artery. And graft, where an artificial graft connects an artery and vein. There are major problems with both including clotting and aneurysm. A significant portion of procedures in the IR suites were related to hemodialysis. I want to learn more about the procedure and if anything can be done better.
All the procedures we have seen so far have not used any fixed guiding system. For example, a pt was getting the fracture vertebra filled with cement. The Dr. had to position the needle by hand using the 2-D single sided view in order to position and drive the needle into the vertebra in all 3 coordinate planes. I see the need and benefit to being adjustable in driving the needle, proceed a little, check the position, proceed a little more. But since the doctors had an existing scan of the vertebrae, I found that the procedure might have been augmented with the use of a guide which held the needle in place, especially during the initial positioning and hammering. Another place I though some “guide” might be useful is in deploying a stent. Stents are placed in very specific areas, trying to cover certain landmarks (clots) and making sure to avoid others (brach vessels). However, deploying the stents seems to be a little haphazard, especially for the residents. The un-deployed stent has radiopaque markers for the start and end of the stent which can be seen using x-ray imaging. However, when deploying the stent there can be movement of the patient, of the catheter, of the physician….so its not super stable. I thought that the stent designs might benefit from a stabilization component, either internal or external, which would allow physicians to more precisely deploy the stent, knowing exactly where the tip and end of the stent will be. The image is that of a venous filter, which is meant to catch large emboli in the venous system and prevent them from reaching the heart and also aids in the breakdown of the embolism. We have not seen the placement of one yet, but I was told it can also be an unstable deployment procedure.
Vasospasm
Emil Klosowiak Blog
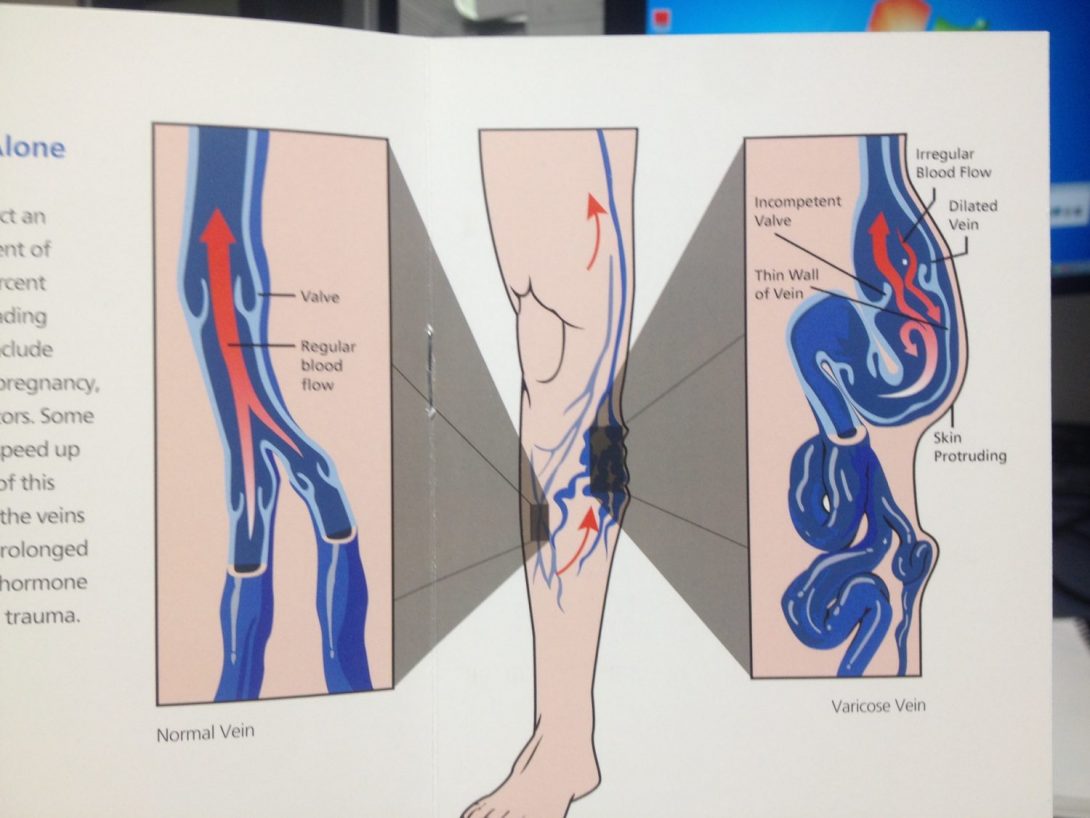
A problem encountered with IR is vasospasm. Vasospasm is a natural reflex of the arteries (and veins?) to constrict following physical irritation. For example, if a catheter pokes a thin vessel, the vessel can constrict and prevent access by the catheter. It is not a problem I have seen yet, but I have heard it mentioned several times and it seems that its something the doctors have to worry about regularly. I wonder how frequently it occurs and if “softer” catheters produce less irritation that harder ones. Another case of uncontrolled response to physical irritation is the heart and it contracting uncontrollably when touched. This circumstance is mentioned every single time any device gets close to the heart. This circumstance seems more dangerous than vasospasm because it can mess with the heartbeat.
Something I’m seeing in about 50% of cases is the doctor has to ask the nurse/tech for help with the imaging technology. The controls for the x-ray, the monitor and the bed are on one side of the bed but can actually be attached to the other side as well. However, when working by the neck, which happens very frequently, the Dr is far from the controls and asks someone else to maneuver the surgical layout. This seems silly.
Balloons and stents, devices that are used regularly, are stiff and therefore harder to maneuver around tight bends in the vascular/arterial system. Either making the devices more compliant so they can take sharp turns or make them more maneuverable is a need many of the doctors express. I’m still surprised by how little control the doctors have of the distal end of any of their devices. There are techniques to learn to maneuver the devices well but there is still some bumping around the vessels, especially at turns/branches.
IVC Filter measure of properties
Emil Klosowiak Blog
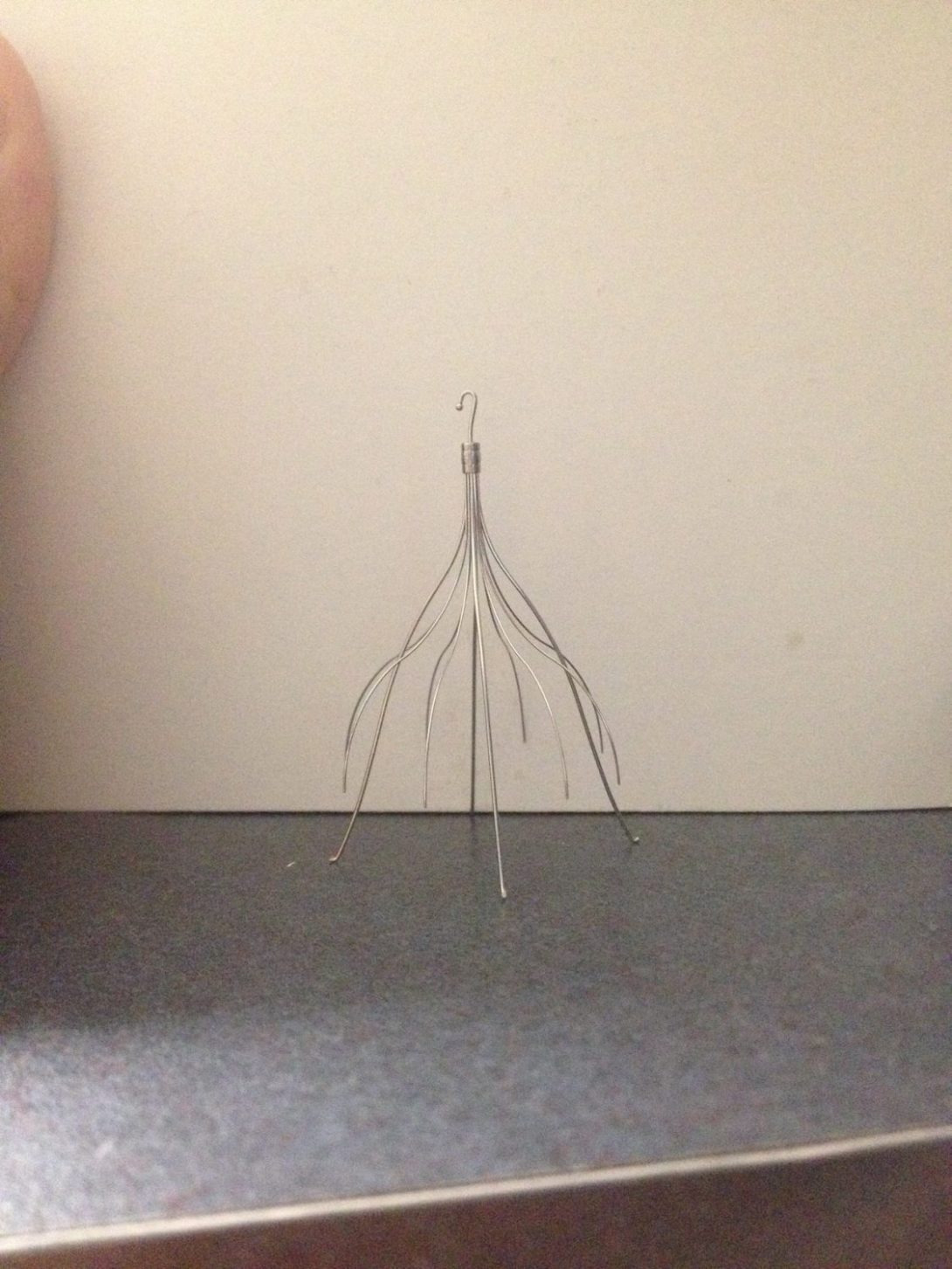
Our mentor mentioned a problem he thinks we can/should solve.
IVC filters are placed for various reason but in general, to catch freed blood clots from making their way up from the leg into the heart and then lungs. IVC filters look like the skeleton arms of an umbrella that is half open, without the handle and without the fabric. The ends of the arms bounce out and into the IVC, holding it in place. IVC filters are placed on a regular basis and can stay inside a patient for life if no complications arise. If complications do arise, such as further clotting around the filter, the filter has to be removed. Because of its umbrella shape, it should be removed from the top, meaning pulled up and out through a jugular vein for example. The tip of the umbrella has a tiny hook which aids in the removal. However, there are cases where the filter cannot be removed from the neck, for example if there is worry about passing the heart. In this case, the half-open umbrella has the be inverted and pulled back down and out. We saw x-rays of this process and it seemed crazy. All the arms have to be bent in half and back. There is risk of perforating the IVC. It looked messy. And one big risk is arms fracturing and flowing up into the hart. This can be prevented with a balloon, but our mentor believes that it would be useful to have “specifications” of a filters material properties. For example, there are ~20 filters on the market. When inverting each filter, it would be useful to know which one has arms that will bend and which has arms that will break? How much can they bend? I’m still not sure how much of a problem this is. It does sound like it may be good to design the filters in a way that they can be pulled out in either direction. Interesting topic that may be worth looking into.
Static Porto-Caval shunts
Emil Klosowiak Blog
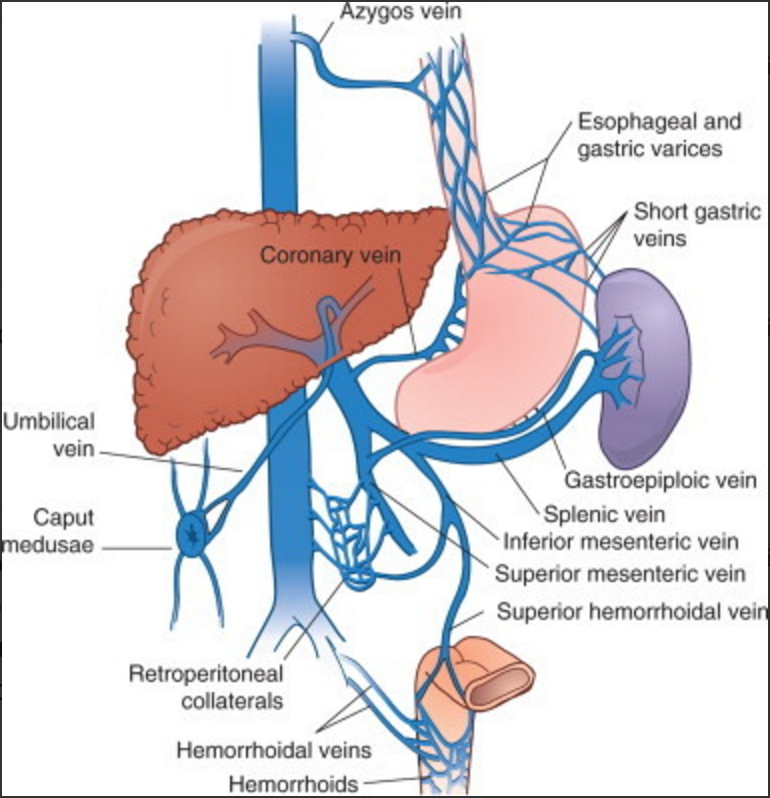
Portal hypertension is a common problem seen the in the IR. Portal hypertension is associated with liver disease. We have seen two stages of the disease. Portal hypertension leads to increased pressure in portal veins that is then transmitted back and increases pressure in other vessels. This backup of blood means that blood is not filtered by the liver but instead finds alternative routes back to the heart. This causes swelling (varices) in certain veins (esophageal) which are then at risk for rupture or it creates patent veins that should be closed (umbilical). A patient like this is at risk of hepatic encephalopathy, aka confusion/disorientation. This is caused by unfiltered toxic portal blood entering the CVS. How is this treated in IR? The varices and patent veins are blocked up, forcing blood to be filtered by the liver. Only problem is that the liver is still diseased, but its the best that can be done at the moment.
However, Portal hypertension can also exist without varices or unwanted patent veins. In this case the blood has nowhere to go. This is almost the opposite problem. The treatment? To place a shunt (tube) in the liver between the portal vein and hepatic vein, bypassing the liver, effectively mimicking the function of varices and patent veins. Patients that are treated like this are at higher risk for hepatic encephalopathy, but at least they have blood flow from the portal system and a decrease in portal hypertension. Besides the fact that neither treatment addresses liver disfunction, the problem is that this porto-hepatic shunt is static. Meaning once its in place, flow cannot be adjusted. This means that there is no way to balance the shunts flow for either too much or too little shunting, both of which would be problematic. It seems that this could be a valuable problem to address.
Image credit: https://quizlet.com/9551975/portal-hypertension-flash-cards/
Tooba Ghafoor Heading link

I will be in the anesthesiology and urology rotations this summer. As a computer science minor, I’m especially interested in how software and optimization are used to improve the clinical environment. I serve as the UIC chapter president of Tau Beta Pi, the national engineering honor society.
Tooba Ghafoor Blog Heading link
-
Tooba Ghafoor Blog
Anesth. Week 1 Part 1 – First Impressions
Tooba Ghafoor Blog

On our first day of the program, we met as a group in the morning and went over the importance of needs assessment and the innovation process. The anesthesiology group then proceeded to the hospital building for the beginning of our first rotation.
They had actually closed the operating room for a few days in order to reorganize supplies. Our mentor, Dr. Edelman, explained that it was worth it to lose out on those days of surgery, because in the long run it would improve efficiency and save more than they lost. We also spoke about the overall hospital design of UIC – it’s not very large, especially compared to Rush hospital down the street. However, this is actually a benefit for UIC, as it takes less time and effort to wheel patients from place to place.
We checked out the surgicenter, where patients go before the surgery. There are 17 slots for patients, but there’s not enough computers to track each patient, which becomes a major bottleneck. After leaving the OR, patients are wheeled to the recovery room. At this point, there is a transition in care from the OR staff to the recovery room nurses. This transition is ripe for miscommunication, as the OR staff verbally explains all about the patient and how the surgery went.
On Wednesday morning, we arrived bright and early at 6:30 am to listen to the morning lecture given to the med students on how to handle difficult airways in patients. I noticed that during the practical demonstration part, the presenter had trouble with the mannequin – the material it was made of was too stiff/sticky for her to demonstrate effectively.
We then got into our scrubs and proceeded to the OR to watch surgeries. The first surgery was a Medtronic drug pump replacement. Since the battery on the Medtronic pump lasts only for 7 years, the patient needs to come in every 7 years to get the entire pump replaced. I am curious to know what the challenges are in producing the pumps with a longer lasting/rechargeable battery in the first place. It took awhile to get the pump reprogrammed; it seemed that there was some electrical interference with the product rep’s programming device, causing it to freeze up//slow down.
During the procedure, the anesthesiologist checks the patient response using a neural stimulator. If there is no response, they first check to make sure the device is working properly by testing it on themselves. So, the anesthesiologists have to give themselves a small shock with the device often just to check if it’s working.
Since this was the first day or two, it took some time to get acclimated to the OR environment. Will update again with the next few days’ observations. Thanks for reading, until next time!
Anesth Week 1 Part 2 – Robots Reflection
Tooba Ghafoor Blog
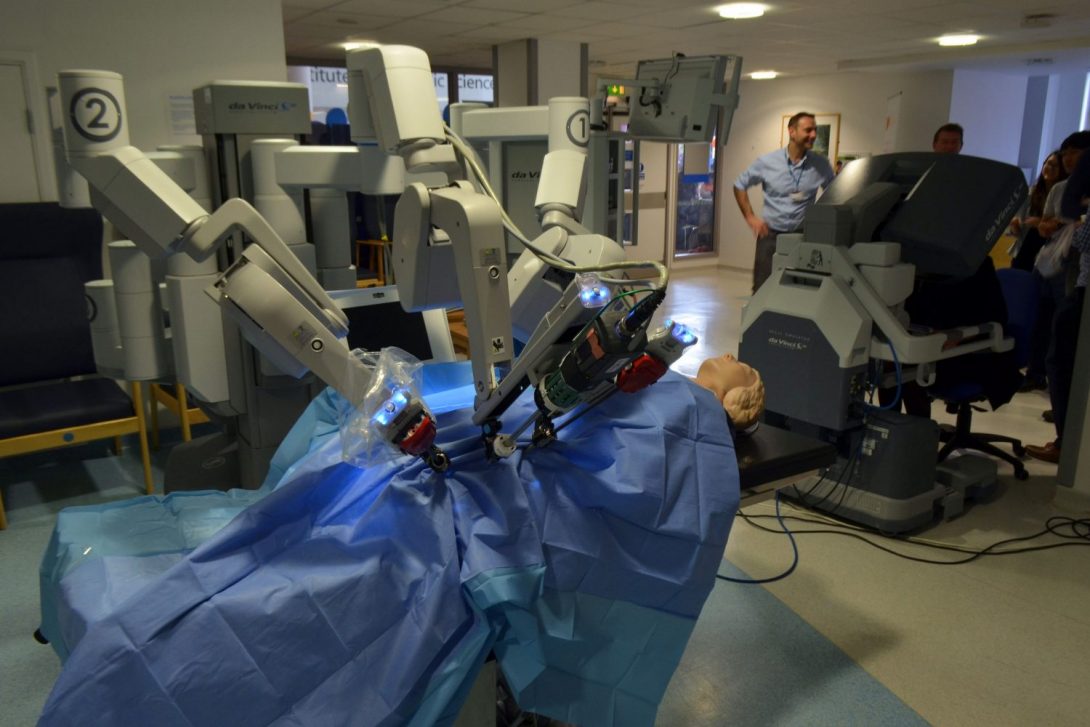
On Thursday and Friday, we got to see a kidney transplant and a hernia repair, both performed using a DaVinci robot, which was very impressive. The surgeon sits at the robot controller in the corner, where he/she has a 3D monitor showing the insides of the patient. There’s another surgeon sitting by the patient, who controls the camera. The view from the camera is displayed on multiple HD TV screens. Very cool.
Using the robot allows for better control, and prevents the need to make a large incision on the patient. However, one problem is that the camera gets splattered with fluids/blood on the inside of the patient, so it needs to be removed and cleaned often during the surgery. This seems annoying and wastes a lot of time. It would be good to have a mechanism for the camera lens to wipe itself when dirty.
Looking back on the week, here are some common themes/problems my group and I observed:
Annoyance with machines
I had the opportunity to speak with a very helpful anesthesiology doctor about the different needs of the regular hospital floor vs. the OR. Simply put, in the OR, every second counts. So, when screens on IV pumps and other machines take too long to load, or it takes many clicks to get to the important screen, it’s a big problem for the doctors. Another big problem is that the screen on the anesthesiology monitor lags behind reality by about 15 seconds. So, the effects of administered drugs aren’t apparent for awhile after they appear, and if a patient’s blood pressure suddenly shoots up, the won’t know until the monitor tells them 15 seconds later.
Cost vs. convenience
For many small problems we’ve observed, there actually is a solution available, but the hospital hasn’t implemented it, because either the problem is not big enough, or the solution is too expensive. We are interested in knowing how the decision is made on whether to adopt a new technology for the hospital.
Lack of space
There is a huge lack of space in the hospital. Walking down the halls of the OR, you see an equipment room, but it’s more like equipment hallway, with imaging equipment, beds, cribs, etc. lined up throughout the halls. In the locker rooms, people are doubled and tripled up on sharing a locker. Meanwhile, in the surgicenter, where patients go right before they’re wheeled into the OR, there’s not enough space to have proper rooms, so there are 17 slots roped off by curtains. It works out, but could be better.
Since this was the first week, we were just getting started on identifying problems. Will post new insights next time. Thanks for reading!
Anesth Week 2 Part 1
Tooba Ghafoor Blog

This week we got to check out the simulation lab, where the residents and students go to practice procedures on a mannequin. Our mentor, Dr. Edelman, explained that although the mannequin is obviously not a real human, research has shown that simulation still gets students’ stress hormones flowing, and can mimic the feelings of a live procedure effectively enough. They have both adult and child mannequins in the lab, but no obese mannequins. I thought that was interesting, as obese patients usually pose a much bigger challenge, especially for anesthesiologists in terms of intubation and maintenance of the patient.
In the OR, we saw a gastric bypass surgery, in which part of the stomach is stapled off and removed, which helps curtail hunger and allows obese patients to get to a much healthier weight and lifestyle. At the beginning of the procedure, there was a major hiccup: the tech/nurse (not sure of the exact position) was unsure of the exact prep procedure. In all the hustle and bustle before the surgery, she didn’t have a chance to ask how to prep the patient, which involves applying iodine and drapes/tarp to the surgical area. The surgeon was all scrubbed in just about to start when it came to his attention that the patient was not even prepped for the surgery. Understandably, this caused considerable frustration, as it took about 15 more minutes for the techs to then prep the patient, who was already under general anesthesia. This wasted time, and as the surgeon mentioned, was not good for the patient to be under anesthesia for any longer than completely necessary.
The reason this situation occurred was because the nurse/tech was scheduled to this room was usually in an entirely different department, so she was completely unfamiliar with laproscopic gastric bypass procedure prep. The surgeon said this situation has been occurring more often, and that the techs should be assigned only to rooms whose procedures they’re familiar with.
We had the opportunity to speak with the surgeon about the equipment he uses for laproscopic procedures. Of course, there is the laproscope: a long, thin instrument with pincers at the end, which they stick into the patient. There are many problems with this tool. Firstly, it has no flexibility, which makes getting around intestines, etc. very challenging. It also is counterintuitive: if you want to grasp something with the instrument and move it to the left, you would actually have to move your hand towards the right. Tools such as this should be as similar to human motion as possible, but that it not the case.
Additionally, I’ve noticed a few small hassles each time: the OR beds have detachable foot ends/head ends, but they’re really clunky and take considerable pushing to actually attach, which seems annoying. Also, the entire process to transfer the patient from the transportable bed to the OR bed (and vice versa) seems kind of medieval compared to all the other technology present: one person stands on each side of the patient, and there is basically a “1, 2, 3…pull” moment. It would be nice to have a machine do this job instead.
Anesthesiology Week 2 Part 2
Tooba Ghafoor Blog
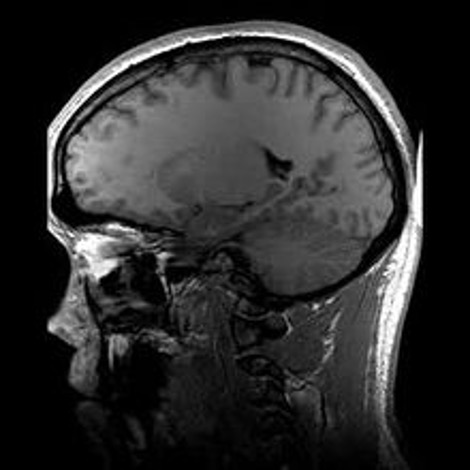
This week started off with an insightful talk given by a physician in the urology department about the value in finding the right problem. A good problem, he said, must be both simple and impactful. I’ve been keeping this in mind these past few days, and have realized that finding the right problem is a challenge in itself.
On Wednesday we had the chance to speak to a physician about the use of augmented reality (AR) in medicine. He explained that augmented reality would be much more useful in medicine compared to virtual reality, and that a lot of innovation is underway in this area. For example, this AR ultrasound: https://www.youtube.com/watch?v=hKH1e38B1is is much more useful than regular ultrasound, because it superimposes the ultrasound image in one’s own line of sight, rather than having to look back and forth between ultrasound monitor and patient.
We also spoke about the use of Google Glass in the OR for educational purposes. For example, a resident can perform a procedure while the attending physician looks on from a different room through the Google Glass monitor. However, the current problem with this is that the line of sight of the Google Glass points too high: unless the user looks directly downwards, it would be hard to see any of the actual surgery. I would definitely like to research more into the use of AR in the OR.
We saw an interesting procedure today in which a patient’s mandible had to be removed and reconstructed. In preparation for this, the entire procedure had been mapped out in 3D using VSP ® Reconstruction technology. Not only this, but a custom 3D printed model had been made for the patient’s new mandible, to use as a guide during the surgery. This was really cool, especially the interaction between surgeons and engineers that occurs in order to make all this preparation happen.
During the reconstruction procedure, it seemed that the instrument the surgeon was using to get a graft from the leg was getting too hot, and the surgeon had to actually put it down a few times to let it cool down. There was also some annoyance with the scope used to see into the trachea: it seemed from afar that it was spraying water to rinse the area, which is technically a feature of the instrument but was currently unwanted by the resident.
In terms of workflow, the patient seemed to have a translator before the surgery, but the translator did not accompany the patient into the operating room. This seemed like a problem, because right before they start the surgery, the nurses/techs are required to do a final verbal confirmation from the patient of what surgery they are having done today. It appeared that the patient did not understand what the nurse was saying when asked what surgery they were having done. One of the residents attempted to translate, and the message got across eventually, but a few minutes later the anesthesiology team was telling the patient to take deep breaths, and it was unclear whether the patient understood or not. I asked our mentor, Dr. Edelman about this, and he explained that it’s not worth it for the translator to get into scrubs and come into the procedure, especially since there’s only one human translator, and most of the doctors have picked up some clinical foreign language experience along the way.
Additionally, we also got to see the MRI scanners this week. Since pediatric patients can’t sit still long enough for an MRI scan, they go under general anesthesia to get an MRI. The biggest concern with the MRI is safety – one of the radiology techs had plenty of horror stories to tell us about accidental patient deaths that have occurred in other hospitals due to lack of care around the strong magnet. Although they have plenty of signs up warning of the danger, it seems interesting that it’s left up to humans to keep ferrous metals away from the magnet.
In the world of ultrasound for neural block anesthesia, we heard from Dr. Chiang of the current problems with ultrasound. Mainly, it’s annoying and inefficient for the anesthesiologist to hold the ultrasound probe with one hand, control the needle with another hand, and have to pump drug into the needle at the same time. There are plenty of improvements that can be made to this.
Anesthesiology Week 3 Part 1
Tooba Ghafoor Blog

At the end of last week, we got to see a spinal procedure. These procedures pose extra challenges because the patient starts off on their back, are then intubated and their arterial lines, etc. are placed. Then, once they have several lines and tubes sticking out of them, the team needs to flip over the patient onto the spinal procedure bed, so that they’re lying on their belly with their spine facing up. The surgeons then begin the procedure. However, one problem with this position is that in the event of an emergency, the patient would need to be flipped back over with their spine open in order to perform CPR. This is a very dangerous situation which could most definitely paralyze the patient, and everyone hopes it would never occur. It would be better if there was a safer procedure for dealing with emergencies during spinal cases.
For procedures such as scoliosis surgery, where they insert rods, hooks, and screws to hold the spine, they do continuous monitoring of the nervous system to ensure that screws are not accidentally hitting a nerve. Dr. Edelman explained that they used to have to wake the patient up during the middle of the operation and have them wriggle their fingers and toes to check on this, but now they have electrodes with which they can non-invasively and continuously monitor the patient.
This week, we got to see a cardiac procedure, in which the heart is “turned off”, the lungs are deflated, and the patient is placed on the heart-lung machine pictured at the top of this post. The heart-lung machine is pretty cool, as it oxygenates and pumps the blood for the patient. However, the problem is that the blood flow it produces is mostly laminar flow, while our organs are accustomed to the pulsatile flow that our heart produces. So, being on the heart-lung machine can sometimes cause neurological deficits in a patient.
One annoyance I noticed during the cardiac procedure was that the cauterizing-cutting device, which was attached to an “energy platform”, beeped really loudly every time the surgeon was cutting. It was even louder than the anesthesia monitors. Since the surgeon cuts a lot during the procedure, it is not useful for such a commonly used device to have a loud beeping sound produced.
Additionally, when the surgeon was opening the chest to begin the procedure, he had a sharp, flat instrument which he held against the chest, then used a metal mallet to hit it and crack open the chest. It was sort of medieval, and I thought it was interesting that there’s not a more advanced instrument used for this part.
Looking forward to the future, I’ve been thinking about ways that AI and robotics can eventually be useful in the OR. A lot of setup and retrieval of instruments can be done by robots. Eventually, we probably won’t need a person to keep fetching supplies from drawers, a robot can just retrieve it instead. One of the anesthesiology doctors even said that a lot of the work an anesthesiologist does can be done by a computer, because it’s mostly monitoring the patient and reacting to changes in their vitals. It will be interesting to see how robots play a role in the OR of the future.
Last Anesthesiology Post
Tooba Ghafoor Blog

In our rotation in Anesthesiology, we noticed a lot of problems related to the three themes of communication, technology/layout, and sterility. A lot of the communication problems we saw were between anesthesiology and the other surgery staff. It showed an insight into the culture of how anesthesiologists are viewed by other physicians.
We realized that problems with technology are multi-faceted: they are connected to funding, administration, layout, and other factors. So, when investigating a particular technology need further, an important next step is to determine whether the need has already been solved elsewhere, and is simply not being implemented at a particular hospital.
With sterility, there’s also a lot of factors playing into it. An important next step could be to determine the official sterility guidelines at UIC, and dig deeper into people’s attitudes regarding sterility. These attitudes could be examined in other hospitals as well, for comparison.
We enjoyed our stay in the anesthesiology department, and I look forward to urology!
Urology Week 1 Part 1
Tooba Ghafoor Blog

Our first few days in urology, we’ve seen a few surgeries and tried to investigate on some common problems that occur. A big problem is obviously delays in surgery, which are often caused by equipment not being in the correct place when needed. Our team was lucky enough to investigate this process and learn about some of the bottlenecks.
We visited the Sterile Processing Department (SPD), where instruments are decontaminated, sterilized, sorted into trays, and sent to the OR. They have a mini elevator that is supposed to be used to transport dirty carts directly down from the OR, and clean ones directly up. It requires no humans to actually enter the elevator, the only thing that goes in is the cart. It would be pretty convenient, except the elevator breaks down at least once a week. When this happens, a member of the SPD has to physically wheel the carts/supplies through the halls, up the elevator, to the OR, then come back down. With so much work to do, this wastes a lot of manpower and resources.
Another bottleneck in the sterilization process is physically scanning in the trays with supplies. They only have one computer for scanning inventory, and all supplies need to be checked in at 3 points in the process. This creates a lot of wait time where the SPD team members are waiting just to scan in instruments. They used to have 3 computers, one for each point in the process, but they also broke down and have yet to be repaired.
Additionally, as with the rest of the hospital, there is a general lack of space in the SPD, which also slows down the process and reduces safety.
On the OR side of the story, as I mentioned above, a big problem they have with equipment is just getting the correct equipment for each procedure. For example, having the correct instruments for a robotic laproscopic GI surgery vs. a knee replacement surgery. Sometimes this is due to a lack of education on what instruments are used for each surgery, and it’s also caused by incorrect entering of supply requests into the system, as well as unplanned changes in the procedure.
We hope to continue to investigate this issue, and are really grateful to everyone who has helped us in our search so far.
Urology Week 1 Part 2
Tooba Ghafoor Blog
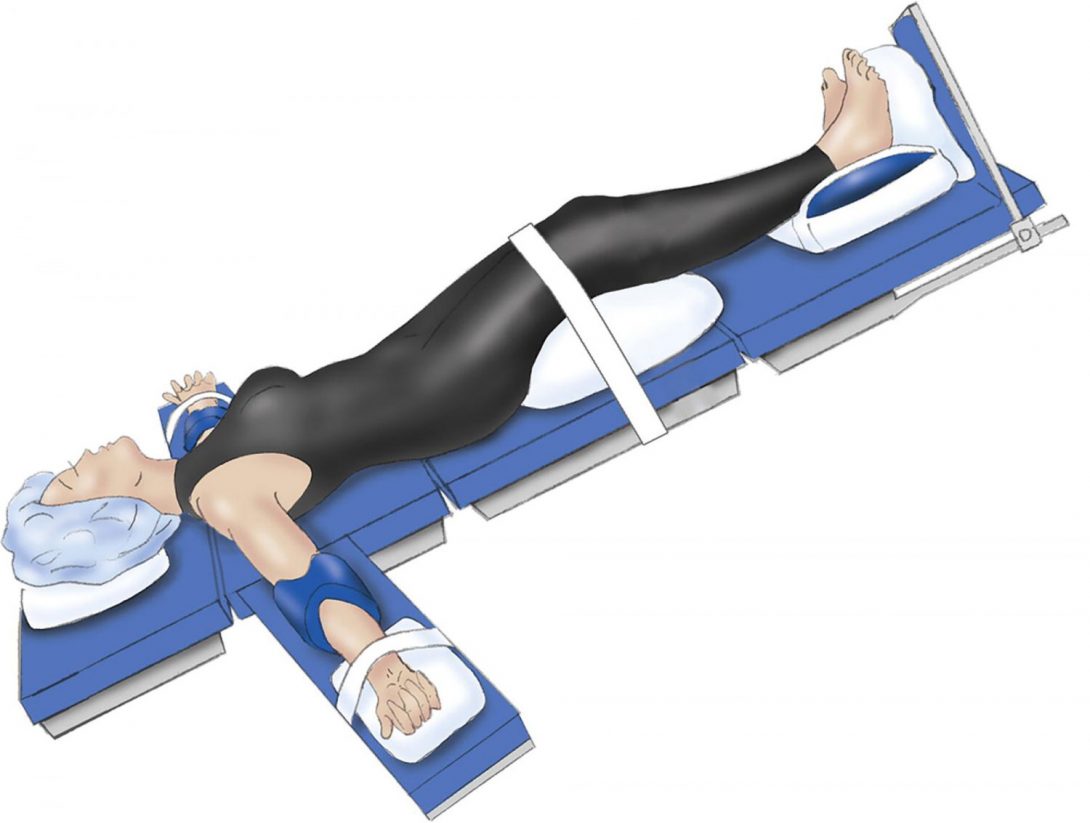
Last post, I wrote about the issue of delays due to problems with incorrect/delayed equipment. Here I’ll mention a few miscellaneous problems we’ve noticed during the urology surgeries:
Patient Transfer
Transferring the patient from the transport bed to the OR bed before the surgery, and back again afterwards, is a pretty unwieldy process. Especially in cases where the patient is obese (which is a lot of the time), it actually poses some risk to the OR staff, and can delay the surgery if the resident or even attending injures him/herself while moving a patient. There is a need for a safe way to get the patient onto a suitable bed for surgery.
Suturing
We’ve noticed that it takes a long time to close up the incisions after the surgery is over, and from a non-medical perspective, the current suturing method seems kind of old-fashioned. My team and I would like to find out if there are new methods to close incisions without the need of sutures, which would definitely save a lot of time during the surgery.
Emergence
Patient emergence time from their general anesthesia varies. Some patients take a long time to wake up after the surgery is over, which wastes a lot of time where the residents and anesthesiologists stand around and have to loudly say the patient’s name in an attempt to wake them up. It would be convenient if the anesthesiologists had a more exact way of knowing when a patient would awaken based on how much anesthetic they had been given, and adjust their doses accordingly.
Patient Positioning
Especially for urology surgeries, it often takes a long time to get the patient in the correct position for the surgery. Sometimes the patient’s head has to be tilted downwards almost to the floor, and it takes all kinds of rolled up blankets and tape put in different places to get the patient in the correct position. It would save a lot of time to have a way where the surgery team can quickly place a patient into the correct position without using many different types of materials to hold them in place.
My team and I are enjoying urology so far, and look forward to next week.
Urology Week 2 Part 1
Tooba Ghafoor Blog

These past few days, we saw a few more robotic surgeries and spent some time in clinic as well. In the robotic surgery room, one problem we noticed is that the screens that come down from the ceiling have long arms that often bump into each other, which sometimes is an annoyance when trying to move the screens around. Also, people often bump their heads on the screens.
In the procedure we were watching, the patient is tilted, with their head pointed down, and an instrument stand is placed near their head to protect their face from the robot, because the surgeon controlling the robot has no way of knowing if the robotic arms are about to hit someone. However, this stand is not very good at protecting the patient, as sometimes the robot arms just go under the stand, and sometimes it’s in the way and has to be moved away anyways. So, there is a need for a way to prevent the robot from hitting the patient or others.
In clinic, we spent some time discussing with our resident mentor, Dr. Wadhwa, about the need for improved communication in medicine. Communication breakdowns are one of the biggest causes of delays, and there’s a lot of space in this field for improvement using technology. My group and I hope to specify this problem further by analyzing the different circles of communication we see.
Last but not least, we had the opportunity to see one of the newest and most expensive devices in the urology clinic, the urodynamics/uroflow machine. This device gives a comprehensive report on the patient’s urine volume, flow, and bladder function. The test takes about 2 hours to do, because it involves a lot of explaining the procedure to the patient, and patient input on how their bladder is feeling during various parts of the procedure. Some problems with the device are that the catheters they insert into the patient’s urethra have no securing mechanism, so they have to be taped on very tight. However, if the patient moves around or the tape is not secure or gets wet, the catheter slides out of place. According to the nurse practitioner who was graciously explaining all this to us, a ton of time during the procedure is just spent repositioning the catheter. Considering the fact that the test costs the hospital $4000-5000 to run each time, it would be
Urology Week 2 Part 2
Tooba Ghafoor Blog
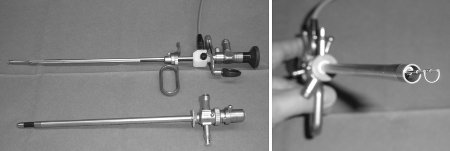
This week we continued to observe some of the common problems in the OR, including equipment delays. Often the missing equipment is something small, like a foam pad or some IV tubing, but it’s still essential for the surgery.
We also saw a few prostate resections, in which the prostate is completely or partially cut out, rather than fully removed along with the lymph nodes, as we had been seeing previously in the robotic prostate removals. In this procedure, a metal loop/hook is inserted through the urethra and used to scrape off portions of an enlarged prostate. This hook is connected via wires to a foot pedal, which has one pedal for cutting and one for coagulating. There’s a lot of hand-eye coordination involved, as the surgeon has to look at the screen, which is displaying video of the inside of the patient, control where the hook is going, and control the foot pedals at the same time to switch between cutting and coagulating. Devices such as this, which require the user the control many different parts, can be improved to be more user-friendly.
Urology Week 3 Part 1
Tooba Ghafoor Blog

This week we headed down to the Sterile Processing Department (SPD) again to further investigate some of the equipment delay issues we’ve been observing. Upon initially hearing about the problem, and visiting SPD once, it was tempting to jump to conclusions about the reasons for equipment delays and missing equipment. Some theories we threw around were lack of training, lack of documentation to check whether each cart of instruments has everything required, high turnover rate, employee satisfaction, etc. However, upon visiting for a second time, we realized we were wrong on many fronts.
For example, SPD has a checklist for each cart that they send up to a surgery, listing exactly what instruments are required for that surgery. They also send up a sheet with the cart that lists the items that are missing from the cart but which were on the list of requirements. So, it would seem that both the OR and SPD have the information they need. However, it doesn’t always work out, as we’ve still observed equipment delays/missing equipment. Also, many of the people we talked to on the SPD team have been working there for many years, and seem to have a system, so it’s not necessarily just a case of untrained employees. We continued to observe more resource problems in SPD, which can be a contributor for the equipment delays. However, this is outside of our scope. In the end, it seems that human error might be a big factor in the equipment problem.
The investigation at SPD was a useful exercise because it displayed the many layers of a problem, and the importance of not jumping to conclusions. Even though it doesn’t seem like something we’ll continue working with, I definitely learned a lot about how to investigate a problem.
Final Post
Tooba Ghafoor Blog
My experience in this program has been great. I’ve gotten to see behind the scenes of what goes into an operation with the perspective of an outside observer, which is pretty unique. Overall, I definitely feel that this program has given me a deeper understanding of the clinical environment.
I’ve realized that there are many factors that go into whether a medical device/software product is useful. There are the physical qualities, such as whether the device requires unreasonable hand-eye coordination or constant adjustment, or if performing a certain task requires too many clicks in the case of software. There are also workflow factors, as in whether a hospital has efficient processes to make sure equipment is kept track of and available when necessary, and patient compliance factors when the user of the device is the patients themselves.
In addition to this, there are many other aspects of the environment which can improve or impede the use of a device. In particular, communication between medical staff has many opportunities for improvement. As we move into the era of artificial intelligence, it will be interesting to see and work towards using more AI/software to facilitate communication between medical staff.
I’d like to thank both the anesthesiology and urology departments for their kindness and willingness to have us this summer, as well as the Clinical Immersion instructors for guiding us through the problem-finding process. It’s been a great experience, and I look forward to working in the field of innovation.
Raahil Kajani Heading link

Second year medical student at UI COM interested in helping improve the care physicians provide to their patients. Born and raised in Los Angeles, CA. Basketball enthusiast and Lakers fan.
Raahil Kajani Blog Heading link
-
Raahil Kajani Blog
What you see is what you get!
Raahil Kajani Blog
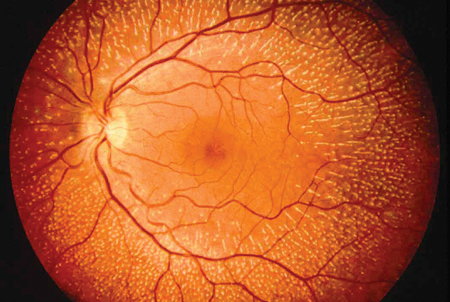
Welcome to my blog! This is the first post in a series of many that will chronicle my thoughts, experiences, and ideas during my participation in the Clinical Immersion Program. I’m really excited for this opportunity and thank you for taking the time to read my posts.
Before I dive into my experiences so far, I want to explain the perspective through which I’ll be sharing my thoughts. As this is part of the Innovation in Medicine program, I wanted to make sure that I viewed this shadowing opportunity differently from all the times I’ve shadowed physicians in the past. Rather than just observing patient encounters, my goal was to integrate the perspectives of the patient, doctor, and others involved in the care process to assess potential needs in medicine and the process of providing care.
With that being said, I’d like to provide a sort of introduction to my rotation in the Ophthalmology Department. As Dr. Sugar provided a brief orientation, showing us the various divisions in the department, he mentioned one thing that stood out to me: the major aspect about ophthalmology that differentiates it from other medical specialties is that “what you see is what you get”.
But what did he mean by that? After elaborating, I gained a greater appreciation for the anatomy of the eye. Although the eye can be categorized as an external structure, it is still an extension of the central nervous system. As a result, an examination of the eye can reveal information about the internal aspects of the body. Additionally, the structure of the eye is built in such a way that the interior parts of the eye, including blood vessels and nerves, can be appreciated using light and different lenses (which means the use of radiation is not needed).
In light of this, one could imagine that the use of visualization and imaging tools would be very important to an ophthalmologist. One instrument that I found to be commonly used is the slit lamp. The slit lamp, to my understanding, is the main diagnostic tool used by ophthalmologists to get a general idea of what is going on in the various parts of the eye. In the few days that I have spent inside the clinic so far (one day in the cornea division, one day in contact lenses), the slit lamp was used for almost every single patient.
Because the slit lamp is such an important device that care providers in Ophthalmology use, I was surprised to learn that this is technology invented in 1911 (source: http://eyehistory.azurewebsites.net/the-history-of-the-slit-lamp/). In fact, the most recent update to the slit lamp came in 1996 with the development of new slit lamp optics (source: “Eye Examination with the Slit Lamp”, Carl Zeiss Meditec, AG, p. 39, accessed: February 6, 2011). That means the most recent update was made 20 years ago!
Certainly, there had to be some way that something used so frequently could be improved or updated. The only way to know how was to use the slit lamp myself, both as an examiner and as a patient. Thankfully, the physicians and staff in the cornea department graciously let the students in the clinical immersion program spend time using the slit lamp. They even spent time teaching us how to properly operate and adjust various parts of the device, as well as the proper protocols used when seeing patients and device maintenance.
I had a great time learning all about the slit lamp. It was incredible to see the versatility and capabilities of the one single machine, especially since it was invented over 100 years ago. However, the one thing that immediately struck me after my time using the slit lamp was that it was very uncomfortable to use. Whether I was the patient or the examiner, it felt awkward to properly position myself when using the machine. Both users of the machine must lean forward in their chairs and position their heads in a way that is “comfortable” for everyone (which can be difficult with varying heights).
Although the various adjustments to the slit lamps and the chairs being used can be made, I still found it to be uncomfortable. The patient must push their face against the strap while their chin sits in a holder, waiting for a bright (but necessary) light to shine across their eyes. The examiner, on the other hand, must fix their heads to the eye holes of the slit lamp and move along with any movements the machine makes during the exam. The fact that ophthalmologists and their patients sometimes have to sit at the slit lamp for long periods of time (sometimes as long as an 1-2 hours if a procedure is being done) makes me think that there must be some effect this discomfort has on the people using them.
Therefore, I wasn’t surprised to hear a physician tell me that ophthalmologists have a high incidence of cervical disc disease compared to physicians in other specialties. After using the slit lamp, it was easy to understand why. I even noticed one of the doctors in the contact lens department was complaining about neck pain, only to proceed to use the slit lamp on every single patient she saw on that very busy day. As I did a little more research on the topic, I found that there are many ophthalmologists who complain about neck and back pain. (Source: http://www.reviewofophthalmology.com/article/will-ophthalmology-cripple-you). It almost seems that by trying to provide care to the patient, the long term health of the care provider has been compromised and/or neglected.
There must be an alternative, right? After all, it has been over 100 years, and I could not be the first person to ever think that using a slit lamp is uncomfortable. That is when I found out that there is an alternative type of slit lamp that is portable and can be used in situations where a patient can’t come to the clinic or sit in the large patient chair connected to the slit lamp (like when the patient is in a hospital bed).
While the portable slit lamp does provide diagnostic capabilities without all the arms, lenses, and moving parts of a traditional slit lamp, it can be difficult to use since both the patient and examiner must be still and stable. Additionally, because of this lack of stability, procedures which require both the patient and physician to use the slit lamp for long periods of time cannot be done.
These were some of the experiences I had during my first week. I had an amazing time so far and cannot wait to continue to share my experiences over here. Thanks for reading!
The Waiting Game
Raahil Kajani Blog

As the first week of my ophthalmology rotation in the clinical immersion program comes to an end, I find myself enjoying the time I have spent in clinic as well as reflecting on my observations. All the doctors and hospital staff that I have worked with have been awesome. They’ve really taken the time to explain diseases and answer any questions I had. It’s amazing to see not only how hard everyone works, but also how much they care about their patients. Physicians and staff in the ophthalmology department understand that many of their patients travel long distances for their appointment and do everything they can to decrease the amount of trips they make to the clinic.
However, for some patients, in order to get the treatment they need multiple visits are required. During my time in the contact lens division, I noticed many of the patients fell into this catergory. For example, patients with keratoconus need multiple visits in order to get the correct lenses that fit their eyes. Keratoconus is a condition where the corneal surface is not smooth but instead is irregular. In order to get the proper lenses that will provide the patient with comfort and restore vision, the patient must first have the topography of their cornea mapped using one a device. Once the cornea is mapped, doctors figure out which of the trial lenses they have available in the department best fit the patients eyes. Each time the patient tries on a different lens, a special dye called fluorescein is used to assess the fit of the lens. Based on this assessment as well as the patient’s preferences, a custom lens is made. Once the lens is ready, the patient must come back and this process is repeated.
Generally, these patients need at least 3 visits and can sometimes require up to 12 visits to get the lenses that they need. From the patient’s perspective, that’s a lot of times that will have to be spent traveling to and from the doctor’s office. This can be extremely frustrating for patients, especially considering that most visits will end without the patient having the contacts that would be best. If there were some way to create the lenses in the clinic, perhaps using some type of 3D printing technology, it would save many patients and their care providers a great amount of time. There are already devices that can map the topography of the cornea. If that date could be used as in input for a 3D printer that had the proper materials needed to create the contact, the lens could be customized entirely to the patients liking.
Building on this idea of a printer being used to customize contacts, it could also be useful for patients who have aniridia (people who do not have one or both of their irises). From a medical standpoint, patients with aniridia need special contact lenses that can limit the amount of sunlight that enters the eye. Additionally, these contacts are made to look aesthetically like the patients functional eye. The current process for making these lenses starts with the care provider taking high quality photographs of the functional eye. These are then sent to a company like TechColors, where an artist uses the images to hand paint the iris onto the lens (http://techcolors.com/ProductsandServices/HandpaintedIrisLenses). Next, the lens is sent to the clinic, where the patient tries on the contacts and compares it to the functional eye. If the patient is not satisfied with how it looks, they have 90 days to send it back as many times to make the changes. Below is an example of the hand painted lenses.
Once again, a printer that could create a design (like an iris) onto a contact lens using a information from a photograph would save everyone involved time. In fact, it could also save the patient money since the labor of hand painting the lens would be taken out. Whether or not a 3D printer which could create a contact lens and then print an iris on it is economically viable is a whole other topic in itself. There would be many factors to consider, mainly if there is a large enough market for either device.
The main take away is that there clearly is a need to help save people time. When I asked the front desk in the cornea department what the most common complaint they get from patients, they answered without hesitation: wait times. Fortunately, the physicians and staff in the ophthalmology department do make a conscious effort of reducing the wait times for patients. In fact, when I asked the residents where they felt time could be saved in the patient visit, one resident brought up the topic of translator services.
Currently, when patients who needs a translator comes to the clinic, a cart with an iPad that connects to translator services is wheeled into the room. The translator is then requested through the service, and within a couple minutes the translator is available and the patient visit can start. As of now, translators are requested on demand with the hope that a translator who speaks the language needed is available. Additionally, there is only one cart available in the cornea department, so if two patients who need it come to the office at the same time, there will definitely be delays. One solution posed by a resident stated that an appointment for the translator service should be made in conjunction with the appointment for the clinic. That way, when the patient comes into the clinic, arrangements have been made not only for the cart and the correct translator to be available at that specific time. Again, whether or not this specific solution is viable is an entire other topic.
Ultimately, I found that there are plenty of ways that patient care can be made more efficient. Whether it’s because a the patient’s full medical records are not available from the referring physician or because the translator isn’t available, these little delays can add up quickly. Addressing all of these delays will take a long time, but recognizing where they originate is a good first step.
Before I go, I’d like to make a quick shout out to Dr. Scanzera and Dr. Shorter in the contact lens department for spending time to answer every single one of my questions patiently! Thanks again for reading!
Lasers (and other awesome experiences) in the retina department!
Raahil Kajani Blog

In today’s post, I’d like to discuss one of my most memorable days so far into the clinical immersion program. Yesterday, I spent the day in retina, a division of ophthalmology that utilizes many fascinating medical devices (yes, including lasers). Thanks to the great doctors I got to shadow, I was fortunate enough to observe a couple of procedures that used technology that I didn’t even know existed. I definitely gained a greater appreciation for the kind of skill and dexterity required by ophthalmologists to perform certain procedures.
Before I discuss my experiences, I wanted to talk about the retina a little bit. The retina is a small area of tissue located inside of the the eyeball and is responsible for transmitting light information into a signal that can be interpreted by the brain via the optic nerve. Because of the it’s size and location, treatment of the retina requires an incredible amount of precision by the care provider. Fortunately, there are many tools an ophthalmologist can use to visualize and even operate on the retina using minimally invasive techniques.
One of the first procedures I learned about in the retina department is the delivery of medication to the interior of the eye by an intravitreal injection. This particular patient was sent to the retina specialist because he was worried about his lymphoma potentially spreading to his eyes. The physician explained that in the case that they found the lymphoma spreading into his eyes, it would be be necessary to supplement his systemic medication (which he receives during chemotherapy) with an intravitreal injection. This procedure requires a needle to travel through the anterior and posterior chambers of the eye into the vitreous chamber where medication can be delivered directly to the retina.
It’s clear that this is a relatively invasive procedure that requires the physician to deliver an injection to a part of the body that cannot be visualized without the use of at least an ophthalmoscope and a lens. Based on current medical technology, this is the best way for drugs to reach the retina especially since systemic medications do not always reach the eye in an efficient and effective manner. Some of the benefits of this procedure is that it can be done in a clinic, does not require any recovery time, and is effective at delivering medication. Unfortunately for the patient, this procedure can be painful. However, the physicians noted that there is research being done to develop a drug delivery method that is even less invasive. I wasn’t able to learn too much about it, but it basically would be a gel or eye drop that would use some sort of receptor or ligand based mechanism that allows the medication to reach the retina without affecting other tissue in the eye. It was definitely very interesting to learn that alternative methods of drug delivery are being developed.
The next procedure I observed was the repair of a small retinal tear using an argon laser. This was by far the coolest thing I have ever witnessed during my time as a medical student. Using a lens and what basically is a slit lamp equipped with a laser, the physician was able to stop the flow of vitreous fluid through the tear by coagulating the retinal tissue surrounding the tear. This is important because the flow of vitreous fluid through a retinal tear can cause the retina to detach. Amazingly, this is a procedure that does not require the physician to physically enter the eye and can be done in the clinic. The patient does experience some discomfort, but this is the only downside of the procedure. As I watched the procedure from an additional scope, I could not believe what I was seeing. It was definitely a sight to see.
What may be even more impressive than the technology itself is the amount of dexterity the physician must have when conducting this procedure. Before the treatment can begin, the tear must first be located. This is done by using the optics of the laser (which operates like a slit lamp) and a handheld lens. Next, the laser must be positioned correctly around the tear and set to the correct energy level. Once the physician is ready, he uses his foot to fire the laser while simultaneously moving it around the tear. To do this, almost all of the physician’s limbs are being engaged: the physician’s eyes are fixed to the scope with one hand holding a lens to the patient’s eye, the other hand controlling the movement of the laser, and one foot pushing a pedal to fire the laser. Needless to say, this requires an incredible amount of precision and proprioception by the physician.
As amazing as this procedure is, I definitely think there can be improvements made to how it is performed. First, the handheld lens being used inverts and rotates the image that the physician can see. I can only imagine how difficult it could be to hold that lens up the entire time, especially when you have to consciously think about which direction to move your hand when trying to appreciate all parts of the retina. A lens that is more intuitive to use for the physician could potentially help. Next, there has to be some way to make this procedure more comfortable for the physician. Perhaps if instead having to hold up the lenses needed to see the retina, the lenses could instead be incorporated into the laser apparatus itself. Additionally, it could be helpful if instead of having to look into a scope, the images being picked up by the apparatus could be shown on a screen. On top of all of this, it would also be helpful if a larger portion of the retina could be visualized during the procedure. From what I observed, only a small strip down the middle of the handheld lens would actually show the retina. These are just a few quickly thought out ideas and are by no means a comprehensive solution to this ergonomic issue. However, I do believe it’s important to examine how to improve the physician’s experience when performing this procedure.
These are just some of the thoughts that struck me during my time in the retina department. I definitely enjoyed my day there and hope I can spend more time observing more procedures. I’d also like to make a quick shoutout to the retina fellow Dr. Dunn for answering all of my questions and showing me some cool procedures. Thanks for reading!
Operation!
Raahil Kajani Blog
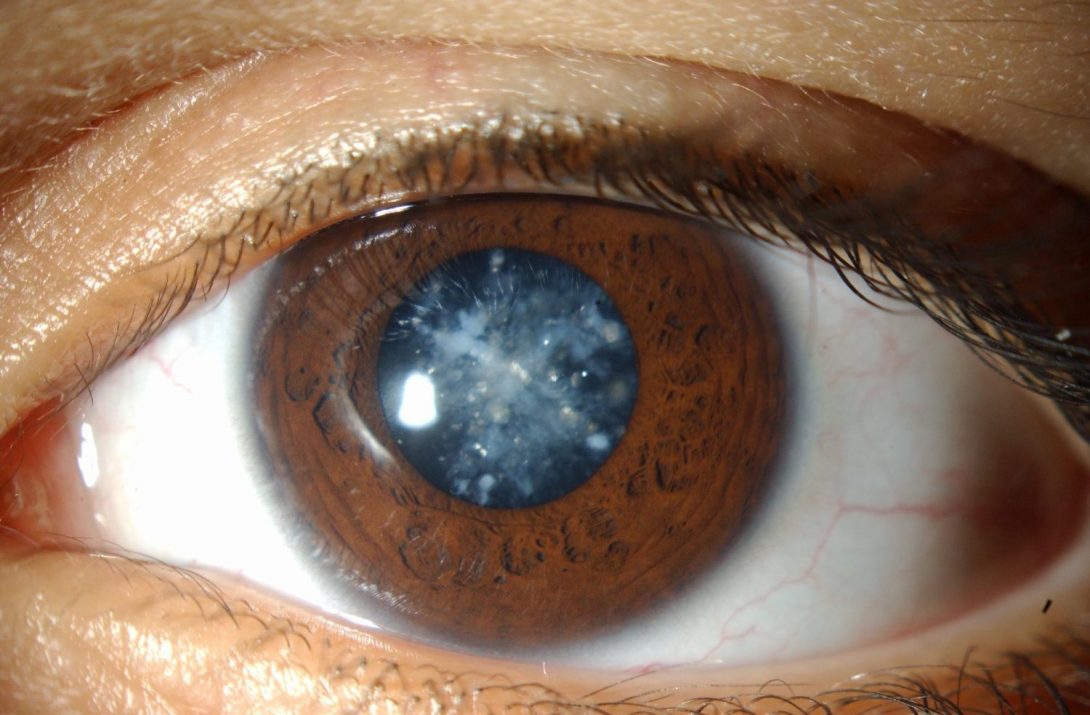
Hello again! I’d like to spend today’s blog post discussing an aspect of ophthalmology that I have not really touched on so far: surgery. For most of the clinical immersion program, I’ve followed physicians as they work in the clinic. However, for the last two Thursdays, I’ve had the wonderful opportunity to observe several different surgeries including cataract procedures and a corneal transplant.
The first type of procedure I’d like to discuss is the cataract surgery. In a nutshell, cataracts occur when the lens of the eye becomes cloudy, impairing vision. To correct this, the ophthalmologist must remove the patient’s cloudy lens and replace it with a plastic lens. Like all eye procedures, cataract surgeries require precision and so the use of medical devices are very important in aiding the physician to perform the procedure in the most efficient way possible. First, a small incision is made in the eye. Next, ultrasound waves are used to emulsify the lens, making it easy for the physician to remove the lens via a suction device. Finally, a plastic lens that has been selected for the particular patient is then inserted and the surgery is complete. Incredibly enough, this procedure only takes about 15 to 20 minutes to perform and has very, very few complications.
In the span of an hour, I was able to witness 3 cataract surgeries, including all the pre-op and post-op procedures for each patient. The attending physician was an absolute expert; he would explain each step of the procedure as he did it, looking through the scope the whole time while we admired his work on a monitor above. Every movement he made was deliberate and had purpose. There were only a few tools that the physician used, but they were all available to him on a table by his side. The assisting resident was seated on his other side, making sure that the patient’s eye did not dry out during the procedure. An anesthesiologist was also present in the room, but it almost seemed like a formality as she spent most of the procedure checking her email, looking for apartments, and reading Buzzfeed articles. If there was one word I could use to describe what I saw, it would be “routine”. Everybody performed their role comfortably and without worry. And with a surgery time that is only 15 minutes long and has a minimal recovery time with a patient, it almost seems that this is the best it can get. However, things can always be improved, no matter how efficient the current process is.
One thing that stood out to me about the cataract procedure (besides how easy the physicians made it look) was that the physician’s performed the entire surgery without wearing shoes. When I asked one of the residents about it, they explained that the chair used by the surgeon is controlled using different foot pedals. According to the resident, using the foot pedals is much easier without shoes because you can feel where everything is. Especially since the physician cannot see the foot pedals and must keep their hands sterile during the procedure, feeling the pedals through socks and not shoes is helpful. Now, whether or not the absence of shoes poses a potential hazard for the physician is something that can be evaluated. Off the top of my head, most of the equipment in the operating room is on wheels, so that may be a hazard. Also, especially since sterility of the physician and protection from hazardous body fluids are a concern, just wearing socks doesn’t seem to be the best option for the physicians.
While most ophthalmology procedures are considered to have low risk of complications, I did witness one procedure where there was a medical emergency. The procedure was to correct strabismus, a condition where the eyes do not look at the same direction at the same time (lazy eye), in a 20-month-old patient. Unlike the cataract surgery, this procedure is extraoccular, meaning it did not involve anything within the eye. Rather, the muscles external to the eye (these control the direction we look) are detached and then reattached to the eye so that the eyes line up like normal.
For the first hour of the procedure, everything was going as smooth as possible. Like my experience observing the cataract surgeries, everything seemed routine for everyone involved. The attending physician was teaching the residents and medical students about what she was doing as she did it. Calm music was playing in the background while the physician hummed along. The nurses were figuring out what they were going to eat for dinner after all the procedures were done for the day. Everything appeared to be going well.
However, just as the physician was suturing up the conjunctiva of the first eye (this is the last step of the strabismus procedure, but for this patient, both eyes were being operated on), she heard some gurgling noises coming from the patient. The gurgling sound was very soft and was something I could not hear from where I was standing, roughly 3 feet away from the patient. However, this is never a good sign since it indicates that the patient’s airway is obstructed. Immediately, the anesthesiologist goes to assess the patient and quickly finds out that something is not right. Almost 5 seconds later, we hear the heart rate monitor ping slow down as the patient’s heart starts beating slower. The anesthesiologist then sees that the patient’s pulse oximeter is at 60%, dangerously low (for reference, a healthy individual generally has a pulse oximeter reading of 99%).
The anesthesiologist then quickly says he needs to call his attending and immediately starts trying to resuscitate the patient. At this point, the eye surgery is no longer a concern and getting the patient to breath is the primary mission. The ophthalmologists step away and let those who can save the patient work. Almost 10 seconds later, we can hear the code being announced over the PA system. Seconds after that, almost 10 different people rush into the room and begin to assist the anesthesiologist. Fortunately, the emergency team was able to intubate the patient and establish a clear airway. The patient becomes stable almost 20 minutes after the gurgling sound was heard. Amazingly enough, the ophthalmologists completed the procedure after the emergency.
Reflecting on this experience, there were some things that stood out. First, the speed at which the emergency situation was addressed was blazing. It took maybe one minute after the attending heard the gurgling for the emergency team to be in the room helping the patient. Next, I commend the physicians who in the room for recognizing the warning signs as they happened. In a situation like this where every second matters, it’s so important that the physician heard the soft gurgling sounds and immediately let the anesthesiologist know. Had the ophthalmologist not said anything, the physicians would have only known that something was wrong when the heart rate monitor started slowing down. This happened only seconds later, but every second counts. These doctors were on top of their game, and as a result, helped the patient survive this scare.
However, there was something that concerned me. In order for the patient’s heart rate and pulse ox readings to drop as far as they did, the patient must have breathing struggles for at least a minute. This means that even before the physician heard the gurgling, the patient was struggling to breath.
Is there a way that this struggle could be identified before the patient’s heart rate and pulse oximeter reading drop? I don’t know the answer, but I have some thoughts. During the surgery, the entire patient’s body is covered; the only body part exposed is the eye that is being operated on. Therefore, it’s basically impossible to visually see the patient struggle since the patient is covered entirely. I don’t know whether or not this breathing struggle could be noticed if a transparent cover were used instead, but it is something that could be evaluated. The way the patient’s breathing struggle was identified in this case was the soft gurgling sound. I don’t know if this sound was present during the entirety of the patient’s breathing struggle, but if there was a way to alert the physician whenever a breathing obstruction is first present, it could be very helpful.
Overall, my experiences in the operating room so far have been impactful. I was able to appreciate the skill and efficiency of the cataract surgery while also seeing how emergencies are handled, even when they are not expected. Thankfully, all went well. Thanks again for reading! I apologize that I didn’t have any photos to share this time.
The Beauty in the Eye of the Beholder
Raahil Kajani Blog
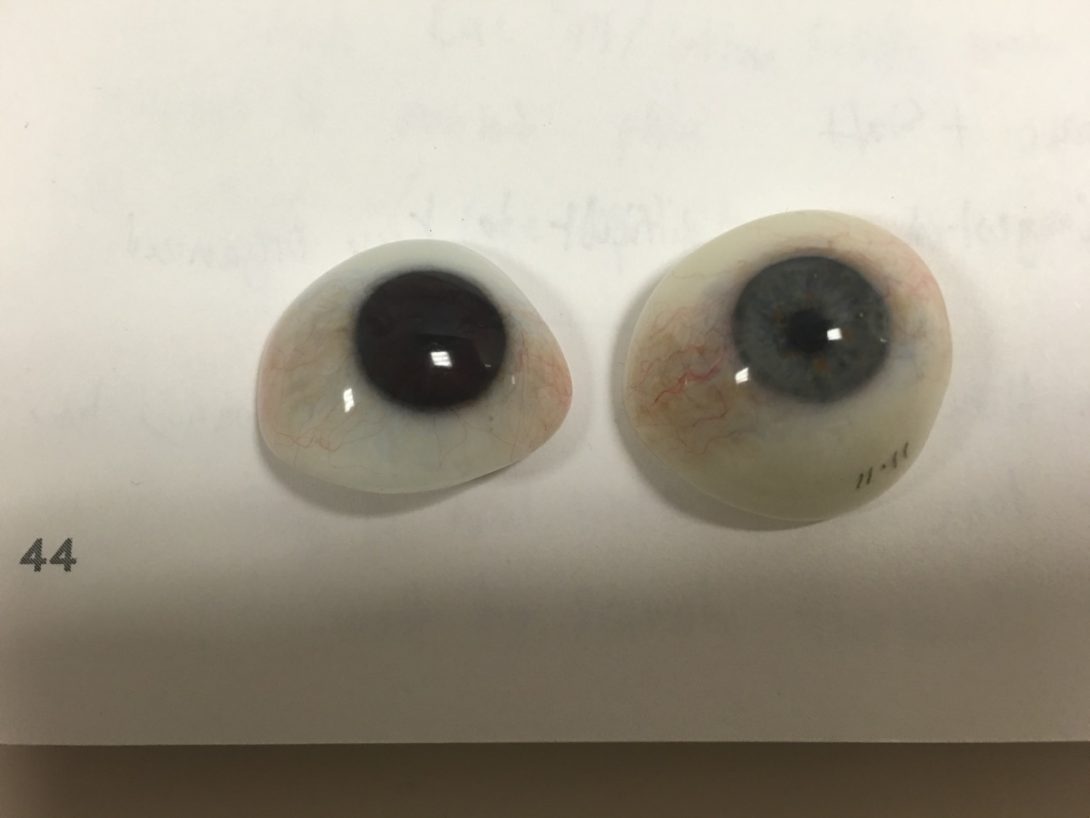
In today’s blog post, I’d like to share my experience in the oculoplastics division of Ophthalmology. Here are a couple of the thoughts and experiences that stuck with me.
As a specialty that is highly concerned with design and aesthetics, many patients who seen in this department have concerns with outwards appearances. For example, one of the patients that came into the clinic had previously had an eye entirely removed and was looking to get a prosthetic eye fitted. In a nutshell, the process of getting a prosthetic eye first requires a ball to be placed into the orbit and attached to the extraocular muscles. Once the proper size ball is placed and attached, the patient must wait for tissue to grow around and integrate this part of the prosthetic. Once this tissue has grown, a shell that is created to look like the patient’s natural eye is then placed onto the ball, completing the process.
While this method does allow the patient to have the appearance of a realistic eye, it’s not perfect. One capability this prosthetic lacks is the ability to have realistic eye movements. Since the shell is essentially sitting on the ball that is attached to the eye muscles, it does not always completely follow the movements of the ball underneath. One solution that the physician had discussed was to physically attach the shell to the underlying ball. This would require the physician to drill a hole into the ball and have the shell attach to it using a peg. While this solution creates realistic eye movements for the prosthetic eye, the hole that is drilled in the ball can serve as a conduit for infections. Another solution the physician posed was to add a magnet in the ball and the shell. That way, once the shell is placed onto the ball, the movements of both parts will be synchronized, creating realistic eye movements. From his knowledge, there is no prosthetic eye that currently uses this type of mechanism.
Another experience that resonated with me was when we observed a patient who had been experiencing eyelid spasms for several years. Essentially, the patient was blinking uncontrollably and needed routine botox injections to control the spasms. During the visit, the physician had to carefully inject botox into the eyelid and orbicularis muscle, making a total of 6 to 7 injections for each eye. After watching this minor procedure, I was shocked to hear that this patient needed to have this done about 4 times a year and had been receiving this treatment for the last 7 years. It’s very unfortunate that in order to maintain control of her eyelids, the patient needed to receive approximately 56 uncomfortable injections in her eye every year. Additionally, the fact that the physician must be careful to avoid nerves and administer the correct dose for each injection means there is potential for error especially given the high volume of injections. When I asked the physician what he wishes he could do to improve this treatment, he mentioned that it would be convenient for both the patient and the physician if there was a botox that could last longer. This way, the patient would need less visits for the treatment and therefore less injections.
Thanks again for reading!
Room for Improvement
Raahil Kajani Blog
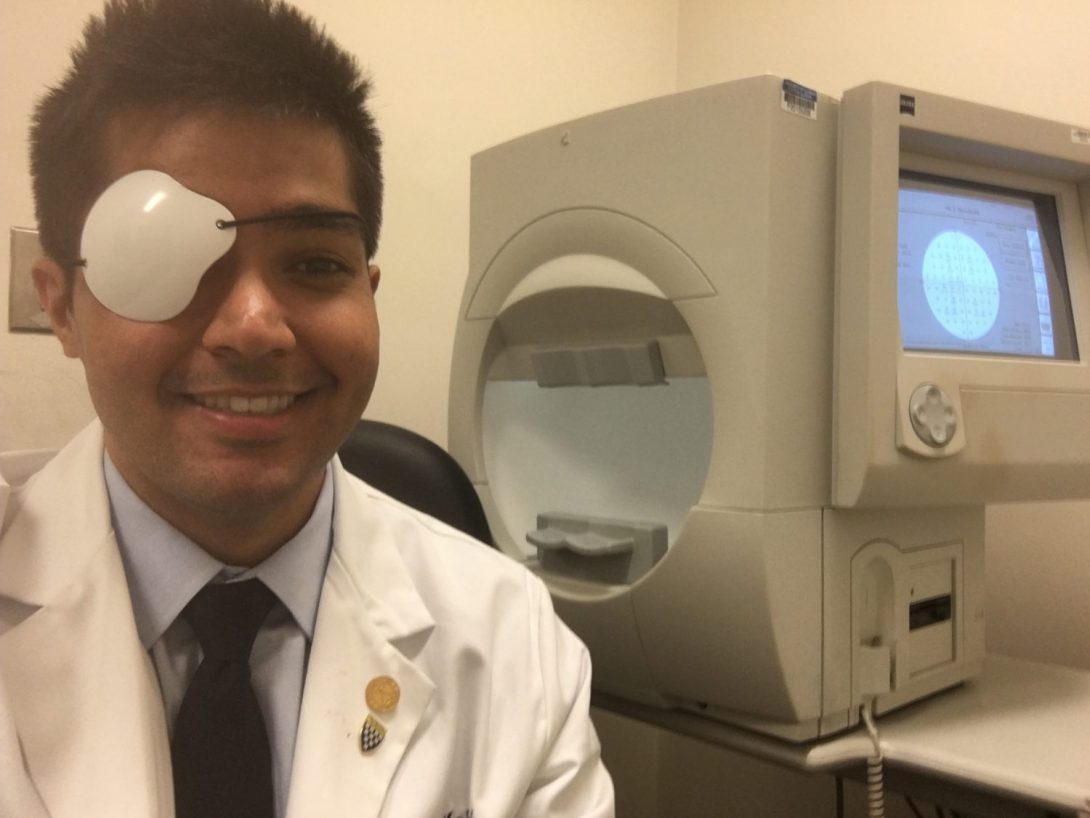
As the first rotation of the clinical rotation program comes to an end, I’d like to share some thoughts regarding my time in the Ophthalmology department.
Ergonomics is (surprisingly) a big issue in Ophthalmology, whether or not people will say it is. Just based on conversations that I had with practicing physicians during the rotation, at least half of the doctors were experiencing some sort of back pain or neck pain. Some people would even have regularly scheduled appointments with chiropractors and acupuncturists just to treat the pain. When I asked those with pain how it started, I was given a variety of answers, but most of them had to do with posture/positioning during surgeries and procedures. Just something as simple as having your chair too high or leaning over to have a resident look over your shoulder during surgery is enough to create constant discomfort for the physician. There has to be a better way, especially since this problem is so widespread within the specialty.
Patient flow is another area that has a great amount of room for improvement. By far, the most common patient complaint I heard about was regarding wait times. During my time in the department, it was clear that there were many inefficiencies that ends up wasting the time of both the physician and patient. Especially since many of the patients that come to the Illinois Ear and Eye Infirmary are referred by another physician, medical records for patients aren’t always readily available. Many times, patients will not remember exactly what the last physician they saw told them, and that requires the physician to perform the same examination to get information that was already obtained. So much time would be saved for physicians if they knew exactly what the referring physician’s concerns and treatment plan is for the patient. However, this information is usually not available (especially if the records are from another institution or medical system) and the onus is on the patient to make sure he or she has all the information they need to give to the physician.
While the need for better ergonomics and patient flow were clear, there were other areas that had room for improvement:
- The type of health records used in the ophthalmology department definitely needs revamping. The current system in place requires physicians to take their notes on paper. These records are then scanned and added to the patient’s digital folder. Even though this does technically qualify as an electronic system, the patient information cannot be searched electronically and information is only available once it’s scanned (which can take a couple days).
- Patients often had their time wasted because referring physicians would not know where to send their patient to get the treatment they needed. This was especially true with patients who needed to see a neuro-ophthalmologist. Generally, when a physician does not know where to send their patient, the default answer is to send that patient to the emergency department. The burden is then placed on the ED physician to assess the patient and find the correct specialist to treat the patient. This process can sometimes take days, with the patient wasting countless hours just finding the right physician that they need.
- Patients often need multiple visits to get the proper contact lenses that they need. Many patients require contacts to be customized by a third party company that fabricates the lenses. Doctors are limited in their ability to find an optimal fit for patients as they usually have to rely on trial lenses to estimate a fit for the patient. Essentially, a trial and error process is used to find the right fit for patients, a process which often requires a minimum of 3 visits.
Overall, I really enjoyed my time in the ophthalmology department. Especially as a specialty that uses a variety of medical devices, I was fascinated every step of the way. Thanks again for reading. Up next are my adventures in the Urology department!
Bodies in Motion
Raahil Kajani Blog
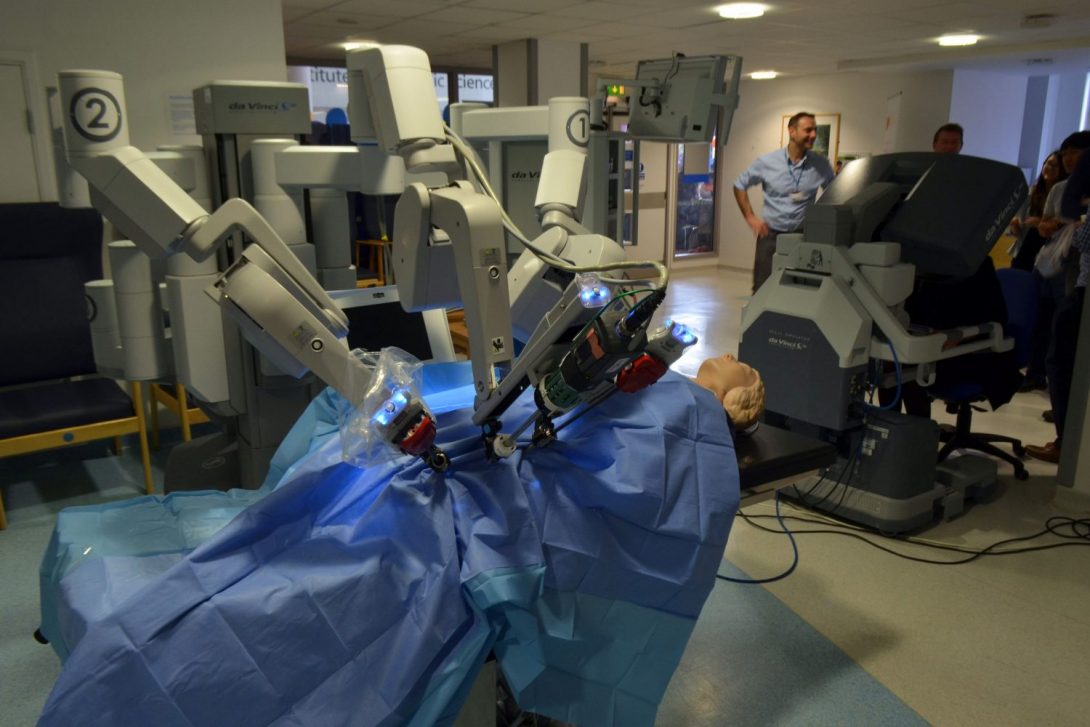
What’s up everyone! Today was the first day of my rotation in Urology as part of the clinical immersion program. Now that I have one whole rotation under my belt, I felt much more comfortable to dive into my assessment of needs in the clinic and operating room. Here are just a few of my thoughts and experiences from my first day of this rotation.
Since Urology is a specialty that includes a substantial surgical component, our team really wanted to evaluate some of the processes and work flow particularly in the operating room. Almost immediately after we started talking to some of the physicians and staff, some of the same needs that were identified during my rotation in ophthalmology started popping up again. In particular, communication between physicians and staff was a common complaint when I would ask people what they wish they could improve. In a clinical setting, communication regarding patient information (like medical records, prescriptions, etc.) tended to be the main issue. However, here in the OR, communication regarding equipment use and location was the core issue. I heard groans and sighs all day as various nurses and physicians recounted their stories of surgeries being delayed because some piece of equipment was not available. Often times people must hope that the equipment they need is available when they want to use it. If they can not find it, they must go on a search to find where it is, how long it is being used, and when it will be ready for them to use afterwards. This can be a time consuming process, especially when we consider that after use, the equipment must be cleaned and prepared for the next use. This is something our team definitely wants to evaluate as we continue our rotation.
The next experience that stood out to me was how one patient was being prepped for a procedure that involved the use of the DaVinci Robot. What made this experience so vivid in my mind was how inefficient and makeshift the whole process of positioning the patient was. First, the patient was wheeled into the room on her hospital bed. Next, a team of three people were required to lift the patient off of the bed and transfer her to the operating table. It did not seem as though there was a method to this maneuver as they pretty much just lifted her from the bed straight onto the table. Once the patient was on the operating table, various equipment was hooked up to the patient, including the heart rate monitor, IV fluids, and devices used to maintain the patients airway during the procedure. Once the patient was sedated and put to sleep, the team in the operating room then faced the task of getting the patient in the proper position for the DaVinci robot.
Since this particular procedure required the surgeons to work on the kidney, the patient needed to be positioned and secured on her side; this was a process that ended up requiring more improvisation than I expected. With the patient asleep and connected to various equipment, a group of 4 men needed to lift this patient up and onto her side. Especially since this patient was overweight, this was very difficult for all of the people involved. The physicians and nurses had to make sure they had a secure hold on the patient before making any movements. They needed to count down and make sure that they moved the patient at the same time. From my perspective, it looked like they were just trying to get the best grip they could before they moved the patient from place to place on the operating table. Once the patient was in an acceptable position, the next task was to secure the patient in this position. To do this, the doctors would grab whatever they could to make sure the patient would stay still. This included blankets, pillows, pieces of cut foam, and a big jelly looking roll type thing (I’ll try to grab a picture next time) that was placed behind the patient to prevent her from rolling onto her back. After all these pieces of support were added, the physicians then took multiple long strips of tape and used it to attach the patient to the operating table. Once that was complete, a drape was attached over the patient and was secured to two IV bag poles using what I could best describe as the clips I use to keep my cereal bags closed. It was definitely a process where the physicians and staff figured it out as they went along.
Needless to say, I was shocked at how much improvisation was required to get the patient in the proper position. Overall, the whole process took about 25 to 30 minutes. Especially when I juxtaposed this process next to the robotic surgery that immediately followed (a procedure that is all about using precision), it was eye opening. There has to be a better way to do this. I would imagine that the patient would not be happy to see how she was being moved around on the operating table. Additionally, the way everything was done, there seemed to be a high risk that one of the physicians could have hurt himself moving the patient around (in fact, I remember one of the other students talking about how Dr. Edelman hurt himself moving a patient a couple of weeks ago). This could be problematic, especially when the physician who hurts himself ends up being the person who must perform the procedure.
Other things that stood out to me today:
- Before the robotic surgery started, there was some trouble getting the robot into the correct positioning for the surgery. In particular, the arms of the equipment hanging from the ceiling (mostly lights and monitors) were getting in the way and had to be moved multiple times before the surgery could begin.
- Once the surgery did begin, the team standing around the patient would often bang their heads against the monitors that were closely behind/around them. This happened at least 3 times to different people within the first 20 minutes.
- The surgeon who was using the DaVinci Robot talked about how comfortable it was to use the machine. In fact, he stated that he could fall asleep because he would be so comfortable. This was a stark contrast to the Ophthalmologists who would complain of back and neck pain after performing various procedures.
Thanks for reading!
Equipped for Success
Hello again! In today’s post, I want to discuss a part of the hospital that most medical students and health care professionals do not usually get the opportunity to learn about: surgical equipment sterilization and processing. Although cleaning and organizing equipment is not the most glamorous or interesting aspect of hospitals, they are vital processes that are essential to patient safety and an efficient operating room workflow.
From a macro view, equipment use and processing at University of Illinois Hospital by UIC involves three major departments: the operating room, the sterile processing department (SPD), and the transport department. Over the past week, our team got to spend time in the operating room and the SPD, learning how equipment is organized in each department and where potential delays in equipment availability arise.
First, let’s start in the OR. Obviously, the OR is where all the equipment is used. This involves anything that comes in direct contact with the patient during surgery that is reusable including clamps, irrigation/aspiration devices, IV pumps, and many other devices. Over here, the nursing staff is usually in charge or locating the correct equipment and making sure that all the tools necessary for a certain procedure is available. This is not always as smooth of a process as it should be and can lead to many delays in the operating room. Some potential delays at this stage include:
- if sterility is compromised, new equipment is needed
- if crash carts are not assembled correctly, staff needs to locate and deliver sterile equipment
- if changes to surgery schedule are made, SPD and transport are not always aware of these changes
Ensuring that the physicians have all the equipment that they need is not an easy process and is something could be made more efficient. At this point in time, there is no sort of system that keeps track of where any piece of equipment is located at any given time. Additionally, if a tool is needed, it’s not always known whether there is one available. The only system in place is a loose inventory and scheduling system that is coordinated between SPD and an OR staff liaison.
This brings us to the next step of equipment processing: sterilization at SPD. Once equipment is used, SPD organizes and cleans the parts. After SPD receives used equipment, each item is scanned, marking it as a decontaminated item. Next, these scanned items are then sent to the proper location for sterilization. After the equipment is cleaned, they are scanned again. This second scan essentially makes a note that this piece of equipment is clean. Once sterile, the carts are assembled and equipment is handed off to the transport department, which takes the equipment back to the OR.
While there is some organized process here, there are still many delays and inefficiencies in SPD. One source or delay for SPD is maintenance of equipment that is necessary for SPD to do their work. For example, the equipment elevators that carry used equipment from the OR directly into SPD sometimes don’t work. When this happens, someone needs to physically transfer all the carts of soiled equipment from the OR through an alternate path to SPD, which ends up taking much longer than if the elevators were working. Another piece of equipment that also needs servicing are the computers that are used to scan equipment. When these computers break down, there are long lines to scan equipment for decontamination and sterilization and employees not always scan equipment. As a result, pieces of equipment can get lost while they are being cleaned and processed.
While some of these inefficiencies are a result of issues within each individual department, delays can be avoided by better communication between these departments. All of the surgeries in the OR rely on transport and SPD to make sure that the equipment they need is available when they need it. Usually, around 1 PM on any given day, the OR sends SPD a schedule with all the surgeries planned for the next day. Based on this schedule, SPD does it’s best to make sure there are enough crash carts available. However, SPD staff is not trained to tailor the carts to the procedures that they are being used for. For example, it’s clear that different procedures will require different pieces of equipment. However, SPD staff does not know how to assemble the carts for one type of procedure versus another. Instead, they are trained to just assemble a standardized cart that has the exact same equipment. When these carts are taken to the operating room, the surgeons and staff do not always have the specific equipment they need. Additionally, a lot of the equipment in the carts are sometimes not used and can get in the way.
Learning about equipment processing in the hospital was definitely an eye opening experience. Our team hopes to learn more about the transport department’s role in equipment processing in the future. Thanks for reading!
Urodynamics
In today’s post, I’d like to discuss a piece of equipment that is used to assess bladder functions in patients: the Urodynamic System. The Urodynamics System is the best device when it comes to finding out what is happening with the bladder and the factors that influence bladder related diseases.
First, I’d like to briefly go over what the machine does and how data is gathered using this machine. The type of patient who would require a Urodynamics test would be an individual who is experiencing problems related to urination, whether it be increased frequency or issues with voiding completely. The Urodynamics test takes objective data about a patient’s bladder and couples it with subjective information coming from the patient. Before the Urodynamics test can be done, the patient is instructed to come to the clinic with a full bladder to take a preliminary test, the Uroflow test. The patient is instructed to pee in an electronic toilet, where data is collected about the urine’s flow (volume, rate, etc.). After this test is completed, the Urodynamics test can begin.
In a nutshell, the Urodynamics test assesses a patient’s desire to use the bathroom as water fills the patient’s bladder. This data, along with other data collected in the test (including the pressure generated by muscles in the pelvis and the bladder wall) can tell the physician whether the patient has an overactive bladder or a different condition related to the bladder. To get all of this data, several catheters are used. One catheter is responsible for filling up the bladder with water via the urethra. A second urethral catheter is also inserted to measure the pressure generated by the muscles that make up the wall of the bladder. Finally, a third catheter is inserted in the patient’s rectum. This catheter measures the pressure generated by pelvic muscles that are involved in the voiding process. The difference between the pressures in the urinary catheter and rectal catheter is used to assess the pressure generated on the urine as it leaves the body.
As water is pumped into the bladder, the patient states how great their desire is to void (on a scale of 1-4, with 1 meaning “I feel a small desire to urinate” and 4 meaning “I need to go right now”). As the patient reports these sensations, the nurse marks this information, correlating the desire to void with the volume of water in the bladder. Once the patient can no longer hold in the water, the patient voids into the electronic toilet again, where the data from the urine flow test is gathered again. Based on the data collected, the physician can have an accurate and precise picture of how this patient’s bladder is functioning and can then make a diagnosis based on these results.
Although there is no better way to assess bladder functions, the Urodynamic test does have its limitations and can be difficult to use. The following are some of the aspects of the test that can be improved:
- The test, on average, takes 2 hours to complete. Part of the reason why this process takes so long is because patient’s generally require the procedure to be explained before the test can be conducted. This generally takes about 20-30 minutes, especially since patients can be frightened by the amount of equipment that will be place inside of their body.
- Calibrating the pressure-reading catheters is a difficult process. Before the test can start, the pressure readings on the two catheters must be equal. To do this, the placement of the catheters must be adjusted by either feeding the catheter deeper into the body or pulling the catheter out by a small distance. In order to take a preliminary reading of the pressure sensors, the patient is instructed to cough. Once the patient coughs and the catheters are secured at their specific lengths, the test can begin.
- Adjusting the length of the catheters is a challenge, especially because the anatomy of each person is different. To account for these differences, the nurse has estimates about how far the catheter must be inserted based on how tall the patient is and whether the patient is male or female.
- An additional obstacle for the nurse is securing the catheters at the proper length for calibration. Once the catheters are calibrated, the nurse secures the catheters by thoroughly taping them up. Once the taping is completed, the patient must walk about 3 feet from the examination table to the electronic toilet. In this process, the position of the catheters can change and the catheters must be recalibrated. This can be a frustrating and time consuming process for everyone involved. After discussing this with the nurse, she expressed the desire for something that can secure the catheters in a position by locking but also has the ability to unlock so small adjustments can be made.
- If the patient talks or moves during the urodynamics testing, it will be registered by the pressure sensors in the catheters.
These were some of the limitations of the Urodynamics machine in assessing bladder function. While it is an amazing diagnostic test, conducting the test can be a hassle. Thanks for reading!
Left to their own devices
In this post, I’d like to discuss some of the surgical devices our team has learned about after two weeks of our rotation in Urology. While all of these devices may not be as complex and sophisticated as the DaVinci Robot, they are important for the specific procedures that they are used for.
First, I’d like to discuss a tool that is used in minimally invasive prostate resections. A prostate resection is a procedure that is performed on men who have an enlarged prostate. In the procedure, a small scope with a cutting tool attached to it is inserted through the urethra to the prostate. Once the prostate is located, the surgeon looks at a screen which shows a live feed from the scope as a guide to remove part of the prostate. With the help of electricity, the surgeon will heat the cutting tool (positioned immediately in view of the scope) until it becomes red hot and then will start shaving off pieces of the prostate. As the surgeon continually removes small bits of tissue, the small blood vessels in the prostate begin to bleed. In order to control the bleeding, the surgeon electrically heats the tool to another temperature and touches it to the bleeding vessels, cauterizing the wounds. The surgeon is able to control whether he wants to cut or cauterize by using two foot pedals. With his eyes on the screen, his hands on the scope/cutting tool, and feet on the pedals, the physician carefully removes parts of the prostate. Once enough tissue is removed and all the bleeding is controlled, the surgeon removes the resected tissue from the patient and the procedure is complete.
The next medical device we learned about was the inflatable penile pump, which we were able to see implanted in one patient. The inflatable penile pump is an entirely internal implant that can be operated by the patient using a mechanical pump located in the patient’s scrotum. Attached to the pump is a reservoir that holds saline fluid that is used to fill the tubes that are placed in the penis’ corporal bodies. When the patient desires an erect penis, he simply squeezes the pump about 10 times to fill the tubes in the corporal bodies. When the patient wants his penis to return to a flaccid state, the patient simply pushes the release valve until almost all of the fluid in the tubes return to the reservoir. To successfully implant the device, the tissue in the penis’ corporal bodies must be destroyed to make room for the inflatable tubes of the implant. The main concerns for the physician and patient is to prevent infection during and after the procedure is complete. To account for this, the implant is generally coated in antibiotics before it is placed inside the patient’s body.
With regards to the device, the company representative was kind enough to speak about some of the common issues with the penis pump. First, the penis pump generally only lasts about 10 years before another one must be placed. One of the most common reasons for a pump to fail is that the material of the pump ruptures, causing the saline fluid to be released into the body. While the release of the fluid in the body does not put the patient at risk, the pump is no longer functional and must be replaced. Usually since most of the patients who want a penis pump are older, generally they will need only one implant. However, for those patients who have greater longevity, multiple implants may be required.
Another area where the manufacture wants to improve the device is in the design of the fluid reservoir. Currently, the fluid reservoir is placed between layers of connective tissue in an empty space within the pelvis. To properly place this device in this specific location, the reservoir must be looped into the inguinal ring, a site where hernias commonly occur. Placing the reservoir can be problematic if the patient has had a hernia in the past, which can be common for the elderly patients that elect for the penis pump implant surgery. The manufacture representative told us that the reservoir is currently being redesigned to be placed in another area of the body. As of now, the reservoir is shaped like a sphere and is relatively large. One of the approaches being taken to redesign the reservoir is that they are making it flatter and pancake shaped. The ultimate end goal is to create a reservoir that can be easily implanted and will not physically show up on the exterior of the patient.
The last surgical device I’d like to discuss are the lasers that are used to destroy kidney stones. For most kidney stone procedures, a scope equipped with a laser must pass from the urethra through the bladder and up the ureter towards the kidney. Once the stone is visualized by the scope, the laser is aimed at the stone through the use of a green light. The surgeon then adjusts the wavelength, frequency, and energy settings for the laser to ensure a safe removal of the stone. The laser company representative told us how higher wavelengths/low energy settings are starting to be used more frequently now to make ensure that fragments of the stone are not pushed back into the kidney as the laser destroys the stone.
These are some of the devices we got to learn about. Thanks for reading!
Some Assembly Required
In this post, I’d like to discuss our team’s second visit to the Sterile Processing Department (SPD). After our first visit, we still had many questions and thought it would be best to take a closer look at some of the processes SPD is responsible for, mainly surgery cart assembly and surgical instrument tray assembly.
As soon as we walked back into SPD this morning, we saw a whole fleet of surgical carts either completely or near completely ready to send up to the operating room. On top of each cart was a thick packet containing a checklist of the cart’s contents. These were the same checklists that the surgical teams send out to SPD the day before the surgeries are scheduled. Upon closer inspection, it was clear that someone had thoroughly gone through the checklist, making a mark to indicate whether or not a particular item was included in the cart. It was encouraging to see this especially after hearing the operating room staff talk about their frustrations regarding missing equipment/equipment availability.
However, one thing that was not so encouraging was the presence of another piece of paper on top of each cart: a missing instruments list. Almost every single cart that was either prepared or almost prepared for surgical cases scheduled to take place in a couple hours had a missing instruments list attached to it. When I asked if this was normal, the staff member told us this was a daily occurrence. I’m not sure exactly how much time the surgical team gets to try and find these missing instruments before a procedure is set to take place, but the fact that this is something operating room physicians and staff must prepare for before almost every surgery is a huge issue.
After learning about the various instrument lists for each cart, we learned a little bit more about how carts are prepared. One thing we found out was that the SPD staff are indeed trained to prepare carts for particular surgeries, at least to a certain extent. From what I understood, the carts are prepared for one particular surgical case rather than making a “one size fits all” style cart. However, the types of carts that can be prepared are the same for a particular department. For example, there is a cart for plastics surgeries, a cart for orthopedic surgeries, a cart for ENT surgeries, etc. While it is great that the surgical carts can be tailored for particular types of procedures, the hospital generally schedules similar types of procedures on a particular day. For example, today was a Tuesday, and the OR usually has many orthopedic cases scheduled on Tuesdays. This can pose a problem, especially since there are many surgeries that require the same equipment. This means that all available instruments for these surgeries are in circulation and will need to be cleaned and sterilized on the same day which can be difficult for SPD. Even though they do their best to prioritize those types of carts, turnover of sterilizing equipment is a long process. Surgical teams tend to request the soiled equipment to be ready in an hour. When I asked how long is usually takes for soiled equipment to be ready, the staff members replied that it generally takes three hours. As you can see, this is not ideal.
After learning about how carts are assembled, we then spent time learning how the trays in the carts are assembled. The best way to view how equipment is organized for surgeries is as follows:
- there are three levels to look at (from macro to micro): carts, trays, instruments
- individual instruments are organized into trays. These trays are organized to hold instruments for particular surgeries organized again by department. There is also a general instruments tray.
- When carts are being assembled for a particular procedure, a group of about 5 trays gets loaded onto the cart. Additional items are loaded onto the carts along with the trays.
Watching the tray assembly process was interesting. This step of the process occurs after soiled equipment has been sent and cleaned of any tissue or debris left from the last surgery. Ideally, instruments are sent back in the same tray they were taken from. This way, after initial cleaning occurs, the tray is scanned by the assembler (to document that it as been decontaminated and is now being assembled) and assembly can begin. The assembler then empties out the tray and can go through the checklist to ensure that all the items are included. However, it isn’t always the case that equipment is put back in the proper trays after surgery is complete. The SPD staff must communicate often to let other assemblers know what they are missing and what they may have extra. If OR staff were more thorough in putting away the equipment in the correct trays, time can be saved for the SPD staff to assemble trays.
While constant communication about the many instruments involved in tray assembly is difficult and can’t always be maintained, there is a system in place to try and organize this process. Currently, if there is extra equipment that does not belong in the tray, the tray assembler puts the extra equipment into an “extras” bin. Periodically, the extras bin gets sorted and the extra instruments are organized into bins with similar type of instruments (but not the exact same instrument; for example, microscissors of every length and size would be together in the same bin). On the other hand, if equipment that is supposed to be in the tray is not present, then the assembler must input in the system that the instrument is missing. Unless the assembler can locate it by communicating with other staff members, the tray is assembled without the instrument and sent to sterilization.
This is just a quick overview of some of today’s experiences. Thanks for reading!
Uro in Review
In my final blog post for the clinical immersion program, I’d like to discuss the key takeaways during my time in the Urology rotation. First and foremost, it was an awesome experience. I definitely learned a lot about medical devices and gained a better appreciation for the coordination it takes at the institutional level to schedule and perform surgeries on a daily basis. There are so many people who work hard to deliver care to patients and I definitely think that, even with all the inefficiencies we observed throughout this program, it is something to be appreciated.
With that said, here are some of the experiences/observations that stuck with me:
- The ergonomics of the DaVinci Robot console is something that can be applied to the medical equipment used in Ophthalmology. Although we spent most of our time trying to assess areas that need improvement, I thought it would be a good idea to see what is done well in particular devices. The console of the DaVinci robot is set up in a way that is very comfortable for the user. To quote one of the surgeons who frequently uses the DaVinci Robot, the console is so comfortable that he “could fall asleep using it”. Especially since ophthalmology is a specialty that is known to have physicians with neck and back problems, applying some of the ergonomics to equipment like the slit lamp could be beneficial.
- Transferring the patient from the bed to the operating table is a process that can definitely be improved. I imagine that if patients had the opportunity to watch a video of how they currently move patients, they would be surprised. From the few weeks we spent watching surgeries in the operating room, we saw that the best current technique is to have a group of people physically lift the patient and move them to the operating table. Most of the time, the patient is under anesthesia and is hooked up to various types of equipment, including devices that are used to maintain the patients airway. Additionally, the people who are moving the patient are generally the same people who will be playing a role in the procedure that is about to be performed. This can include someone as vital as an Anesthesiology attending. It’s been mentioned before, but the students who were on the Anesthesiology rotation saw an attending physician get injured moving the patient to the operating table. This is definitely a process people are already looking into, so it would be a valuable exercise to see the approaches people are taking to solving this issue.
- On top of transferring the patient to the operating table, securing the patient in the proper position for the surgery can also be a time consuming process. From what I observed, the current method of securing a patient is to basically grab whatever you can to support the patient in the position you want. Generally, foam pads, pillows, blankets, and other types of support equipment (like a large gel type pillow) are stuffed under and around the patient. The only thing holding all of these things together is multiple pieces of tape. Essentially, there is no method; the physicians and staff basically figure it out as they go. Again, there has to be a better way.
- Finally, the flow of equipment from the operating room to the sterilization department and back is a process that needs evaluation. Missing equipment is by far one of the most common causes for delays in the operating room. In fact, most surgical teams expect that some sort of equipment will be missing before they start the procedure and do their best to prepare for that. Although our team spent time asking staff in the OR and SPD about their work and how they hope to fix the issue of missing equipment, this is a process that requires more observation. In order to really get to the key issues in this process, we’d need to create surveys and collect data that can be analyzed and looked at.
These are the main experiences that stuck out to me. As always, thank you for reading!
Sara Mohamed Heading link

I am a senior bioengineering student that is doing rotations in Anesthesiology and Emergency Medicine during the 2016 Clinical Immersion Program. The human body is the most resilient and beautiful machine I hope to learn from every day.
Sara Mohamed Blog Heading link
-
Sara Mohamed Blog
Week 1: Four Stages of Anesthesia
There are four stages of anesthesia as explained by Dr. Edelman: anxiolysis, monitored anesthesia care, deep sedation, and general anesthesia. Anxiolysis describes minimal sedation, the patient is still able to breathe for themselves but they have reduced anxiety. Monitored anesthetic care is next level of anesthesia where the patient is sedated and is only responsive to physical stimulation and loud noise; the patient has a safe airway and can still breathe for themselves. Deep sedation is when the patient responds to obnoxious stimulation and may need assistance breathing. General anesthesia is a state when the patient is unconscious, unaware, numb, amnesic and needs the anesthesiologist to basically breathe for them. When the patient wakes from anesthesia, it is called emergence.
Let me tell you, waking up at 4 am to leave my home by 4:45 am and drive to the city by 6 am to park and walk 15 minutes to the hospital has put me in quite the trance this week. Especially with my religious holiday, Eid, having been on Wednesday, I wasn’t getting much sleep when I got home either, because of celebrations. So, every day felt like I was under some anesthesia probably somewhere around the second or third stage, where my thought process was slower and I could barely make out what I did each day. The first day of surgery, I saw an IV being put in. I have a serious fear of needles, I can watch an open heart surgery being done but once I see a needle entering a vein, I get very light headed and dizzy and want to throw up. Each day that has been getting easier. I’m starting to really get the hang of the schedule and watching some really uncomfortable procedures and hope to remain at the stage of anxiolysis, where I know exactly what is going on, but don’t get anxious.
So far, from what I have been seeing, Anesthesia is an art more than a science. Although there is a protocol for how to handle situations, I have seen many anesthesiologists playing it by ear, going with the “IV” flow, and making the most of the resources they have. But I have also seen so much time being wasted on detangling tubes and wires, making sure their devices don’t cause electrical interference for other devices, sitting there waiting on lagging equipment. Precious seconds that could save the hospital thousands of dollars and, in a life or death situation, save a person’s life. Anesthesiologists are natural problem solvers finding solutions for these problems all on their own, including using an unused ventilation tube and cutting it longitudinally to place all the IV tubes in when transferring the patient from the OR to the recovery room so people do not accidentally tug on the IVs. There are so many physicians, nurses, techs, and more that have really taken from their precious time to explain to us and teach us, and for that I am so grateful; Dr. Edelman especially has been very patient, understanding, and passionate to help us learn and grow.
This is a photo of how an anesthesiologist’s work station might look like in a small procedures operating room. Notice the tangling of tubing and wires.
This past week although hard, has been the most amazing and inspiring four days of my entire college career, with feeling truly privileged to see some procedures that most people do not see. I have come to deeply appreciate the human body for its strength and resilience. The human body is the most well oiled machine that is the greatest teacher for any bioengineer, and I look forward to learn more.
Stay tuned for another post with everything I have seen this past week.
Week 1: Noise
The first day of clinical rotation on Tuesday afternoon, was short and sweet. We met with our mentor, Dr. Edelman and he showed us the Surgicenter, where small procedures are done. The hospital had taken advantage of the long weekend and they were reorganizing for better efficiency. He showed us the monitors and the importance of balancing privacy and patient information. He voiced his concern of not having enough computers to complete patient paperwork, something the hospital could easily be avoided if the hospital invested in a tablet for each room to be used as the patients’ charts. We also noticed that each room was separated by curtains and there was not much privacy for the patient and their family and I can only imagine how loud it gets when each room is being used. Next, we saw a small procedure OR. The room was teeny-tiny and the anesthesiology station took up three-fourths of it. Although the computer automatically inputs all the ventilation parameters into the web chart, the IV data needs to be inputted manually.
Day two of my anesthesiology rotation started with a class about airway management and the devices that are used in maintaining an airway. We saw the mac and miller blades used to push the tongue back and open the mouth to the proper position to place an endotracheal tube. They were metal and the doctor teaching mentioned the caution needed because they can hurt the patient. We also saw a laryngoscope and a glide scope that showed video feeds into the mouth for better endotracheal tube placement. The main draw back I saw was that although the device had a small screen it still felt chunky, in the way, and inconvenient. The surgery we saw next was such a miracle to see, and also the one I thought could’ve been so much more efficient due to the little things. It was a Mya Mya, which is rare and an acute constriction of internal carotid to the brain. So the surgeon needed to make an opening in the scalp and connect the external carotid to the constricted internal carotid to supply blood to the brain. In order to identify the exact location of the donor artery, we saw the surgeon us a Doppler device; she struggled with it for a little bit and the sounds were not very clear, there was more interference than I expected. Also that day, anesthesiology’s IV warming device seemed to interfere with the EEG signals and cause noise. The prep of the patient took so long and the mess of tubes and wires did not help; there was some time spent with the surgeon try to find the best location to put wires and tubes so that it is not in the way of surgery. I also noticed the sterile pens used to right on the patient’s scalp would die out really quickly and they constantly need to get replaced. The pins used to the the patients head in place on the operation table was a very heavy and difficult contraption to maneuver that definitely made the surgeon’s life very difficult initially. Also there were some things I just did not expect to see, like when it was time to wash the patients’ scalp before surgery, the water just spilled onto the floor were a towel was just thrown after and the water dripped down the EEG wires, which I’m pretty sure could be very dangerous no matter how insulated the device is. I also noticed the light source the physicians had to use to power their headpieces was like a projector and each time the surgeon moved, someone outside the sterile field had to undo the connection and connect her to another one; something that can be made battery powered and wireless.
First week of observing anesthesia and surgery has been an amazing and impactful experience and I look forward to all the future procedures to see.
Week 2: This Is Morgan
The start to week two has been different and interesting. On Monday, we arrived at the hospital in time to tag along with some Anesthesiology residents to the Simulation lab. The Simulation lab is a facility dedicated to medical education using scenarios and mannequins. I was very impressed by how similar they tried to make the room look like an actual OR or examination room (refer to the image attached). That day we met Morgan and Alex, the adult Laerdal mannequins. They are made to simulate all signs actual patients might show in different scenarios except for movement and skin temperature. That’s what the simulation tech is there for though, she answers questions the students might have about the simulation without providing a solution for the task at hand. What’s interesting is that while discussing with someone from the Simulation lab, he knew there are better options out there, but UIC just doesn’t have them yet. This seems to be a recurring theme in the hospital. For example, the difficult IV pumps, an easy fix for better accuracy and more user friendly features comes in the new products. I think the reason it might seem like the hospital is a little behind in technology, is completely due to costs and politics. At the end of the day, the financial people in an office away from all the clinics and physicians can’t justify the cost of replacing all IV pumps. For example, every pump in the hospital would need to be changed for compatibility with all IVs in the hospital and to train all those people on the new device would cost a great sum. There is also a risk of inefficiency due to delays for the time it takes to simply replace them; similar to what we observed in the Surgicenter the first day.
Today, Tuesday, we were lucky to join a very passionate surgeon for a gastric bypass surgery. He was passionate for making sure the patient has a high success rate with their weight and health after surgery. He also took the time to voice his concerns for the technology used in laparoscopy. “In ten years, your students will go to the museum and tell you about this outdated equipment,” explained the physician while showing us the laparoscopy surgical instruments. We very obviously see that there isn’t a very wide range of motion with the long skinny graspers that go into the patient. The physician is in an uncomfortable and unnatural position leading to possible carpal tunnel. Coincidentally, the surgeon today had an injured wrist and had difficulty using the device. The movements associated with laparoscopy are also paradoxical, meaning that to grab something from the right the surgeon’s hand needs to go left; with this comes a large learning curve, making it a more procedure that requires more training time. Compared to the Da Vinci robot, the Da Vinci allows for a wider range of motion and more natural motions for the surgeon leading to comfort, accuracy and efficiency. It seems to me the concept of laparoscopy might become “ancient” as this physician said with the development of more advanced robots.
Laparoscope Instruments
Week 3: To Echo or Not To Echo, that is the question
The past week of anesthesiology has been a concoction of different experiences. We saw anesthesiology in pediatrics, in MRIs and in examinations. Being in the anesthesiology rotation is very interesting to me because spending everyday in the OR, I get to see things from the perspective of the surgeon, nurses and techs in there too. I can’t help but notice how resilient the human body is. We saw a surgery where the surgeon took bone muscle and skin from one part of the body and reconstructed it for another part of the body. Also the fact that the heart can stop completely during surgery and be started up again according to when the surgeon wants is amazing. In the case of stopping the heart, a perfusionist would take control over blood circulation and the drug control from the Anesthesiologist. The heart lung machine is this very large contraption with lots of tubing coming out of it, that when connect to the patient, the blood is circulated into this machine, oxygenating the blood and returning it to the body. What’s interesting is that our heart uses pulsatile flow according to the closing of its valves. However, this machine uses laminar flow with some turbulence; this isn’t the most ideal environment for the organs. The perfusionist needs to make sure the patient is producing urine to ensure the organs are still properly working. There came a time when pulsatile flow was used with the machine, but results showed that there wasn’t a very different trend than that of laminar flow machines and that it was just much harder to maintain. I think that the unnatural flow of blood regardless of the type of flow is what causes organ damage, and I would imagine that with better technology that would become more natural.
It is very interesting to see the dynamic of all the team members in an operating room. I would have imagined that with a big procedure happening there would be a better procedure or way of doing things. So many things are done perfectly, while other things seem like simple miscommunication that could have been avoided in the first place. In one surgery, a cardiology team came to insert an Echo scope down the esophagus to monitor the heart. It intrigued me that no one knew whether they needed an Echo at that point in time and were just like “Oh yeah sure we can do one, I guess, since you’re here.” I thought it would be known in the OR if the echo was needed and during which part of the procedure. Then the Echo team didn’t have the right sized scope, so they just tried to make it work, and when it didn’t, they called it a day, left and didn’t come back. If this was a necessary procedure, shouldn’t the proper size have been provided and an Echo completed. If it was an unnecessary procedure, why did they even try and irritate the patient’s esophagus.
These common themes keep popping up at us: communication, technology, and sterility. And it is very interesting to see how these things keep coming up over and over.
The image above was taken from: http://www.aviva.co.uk/health-insurance/home-of-health/medical-centre/medical-encyclopedia/entry/technique-surgery-using-a-heartlung-machine/
Week 3: Emergence
The anesthesiology rotation has come to an end and it was very bittersweet. In one way, I was very excited to share our findings with the rest of the Clinical Immersion team, but on the other end, I felt like I really was going to miss the rustle and bustle if the OR. I will miss everyone’s willingness to teach, explain and help. Dr. Edelman is an amazing mentor and his passion for his job is the positive energy I know I’ll miss. Today we gave our presentation to the Clinical Immersion team and I really thought about what the past three weeks consisted of.
We saw some branches of anesthesiology I didn’t know existed. Aside from pediatrics and cardiology, we also saw pain management anesthesiology. Spending the day in clinic, we saw a major problem with EMR, where the physician was forced to spend another 15 minutes after each patient typing, rather than the templates we saw being used in the OR. We also discussed with a pain management attending the multi modal structure that should make up a pain clinic: a team that consists of the anesthesiologist, a psychiatrist, a physical therapist, a social worker, and whoever else might help provide a more wholistic form of care.
We also got to do a later shift in the OR. The OR was backed up due to scheduling with surgeries that were scheduled for earlier in the day. Although that day had 12 ORs operating at 6 pm compared to the usual 4 ORs they have, it was still considered a slow day. What was interesting was that there was a “Gift of Hope” surgery scheduled; this is a removal of donor organs from what is considered a deceased patient. The surgery ended up being canceled right before its scheduled time. Dr. Edelman explained to us however, that because the heart would have been still beating, the anesthesiologist would need to maintain the heart rate and blood pressure to ensure the viability of the heart and organs. They would also need to provide a sedative for paralysis because there could muscle stimulation which is “outright creepy” as Dr. Edelman stated it. Besides that interesting conversation with Dr. Edelman, not much happened that night. But what we did notice was how crazy scheduling is and how some people end up working longer than 12 hour shifts with only a few hours break before coming back again. I thought the system for scheduling would be more defined with protocols for each scenario, but it was very much going with who was available and who was okay with working a few extra hours.
From what we have seen the past three weeks, we have seen three major themes: culture/communication, technology/layout, and sterility. They all go hand in hand in describing the overall needs in anesthesiology and the OR. We got to see some really cool technology in this rotation, but there is always room for improvement.
My first shift for my next rotation, Emergency Medicine, starts tomorrow and I’m very excited to see what it holds. It will be an overnight shift, go big or go home, right?!
By the way, the photo above is really cool because those are my brain waves on a bispectral index (BIS). Anesthesiologists use it when they want to know how “conscious” the person is. The higher the number the more awake and aware they are. Everytime I blinked or smiled, my BIS would change immediately, it was very cool to see.
Week 4: Organized Chaos
The first day (or rather, night) of emergency medicine has been one that comes with mixed feelings. As much as the emergency room seemed busy or crazy, there didn’t seem to be much going on. We started the evening by discussing with an attending physician what she feels is the biggest obstacle in the ER, we got on a tangent and instead discussed the possibility of having a monitoring system that was wireless using Doppler or ultrasound technology and sent the data to a cell phone. Although this was solution based thinking, it helped us realize the overall frustration of not having a more mobile modality to accessing patient information, especially as an ER staff member that is always on the move. The first thing we noticed walking into the ER was the lack of space, there are patient beds in the hallways, and there were not enough computers for ER staff to use. When it comes to space, an especially important aspect we noticed was the lack of space for family members that come with the patient. Another major factor is the beds flow. Beds flow includes the time it takes to get a patient in the waiting room on an ER bed and the time it takes to get a patient admitted and moved from the ER and to their respective place in the hospital. As one resident explained it, the ER looks for like “organized chaos,” and what was interesting is that despite the minor complaints, staff seem satisfied with how the ER is.
Since it is the first day observing the ER, there are a few things we saw, but we weren’t sure what to make of it. There was a pop up on the patient monitor screen that covered a room’s monitor readings; it stayed there for a bulk of the night without anyone getting concerned. The picture above shows the pop-up warning I am talking about. There were so many sheets of papers hung up on walls, on the main white board, and on desks giving instructions. I felt as though they could easily be ignored because there were so many of them around. It was the same way with the sounds: there are monitors beeping, phones ringing, pagers going off, cell phone notifications, and more that I can’t identify. With all the false alarms, there came alarm fatigue. We observed an emergency ophthalmology examination, it was interesting that the doctor used an app on his phone to check the patient for color blindness. But what really surprised me as it surprised me in anesthesiology was sterility. We saw an examination for an open wound on an extremity. The wound was exposed down to the fascia, yet the physician just used regular gloves to examine and touch the wound; I imagined the use of sterile gloves at that point. Another major thing I witnessed and thought would have been more streamlined was the fact that in order to take patient history and information, the doctor writes down everything they ask the patient on a scrap sheet of paper and go back to a computer and try to type it all out as fast as possible before they forget. Every examination had the same questions that follow OPQRST, an acronym that asks the important questions to understand why the patient is in the ER. Yet, for every exam the resident would have to rewrite their checklist and write the answers. I felt like the least that can happen is to have a template checklist typed out for them, if not a tablet device to take down patient info directly.
The next three weeks will be useful in better understanding what is an actual problem and what is just “organized chaos”.
Week 5: Sorry, hospital is full
A patient is in the waiting room, called in for registration, then seen in triage, sent to wait again, and finally placed in a bed. Every patient whether they have a large wound or just need their medications are placed in a bed. These beds are in shared rooms, private rooms, or the hallway. Of course running tests and labs might take some time due to lapses in another department running the tests/labs or receiving the results in a delayed manner. So in the ED patients that are not going to get admitted but are in a bed while waiting. At the same time, the larger issue appears to be the wait for open beds upstairs for ED patients to get admitted to. Some patients end up taking up a bed or room and stay for as long as 24 hours waiting to transferred to the department admitting them. It also appears that communication with those other departments are difficult and unclear. When an ED patient is ready for admittance, the doctor will literally call that department and just ask if there is a bed. Maybe knowing if the hospital is full before some patients are seen, ED could have provided a more efficient flow. Sometimes they do know and then they communicate with patients accordingly or even go on bypass. What really shocked me however was that when an admitted patient is unstable on the floors, they are brought down by the nurse to the ED where they need to wait to register and be seen by the ED and again take up a bed when they have a bed on the floor. I really thought the departments would have people who can react in emergency situations without having the patient come down to the ED. It seemed entirely inefficient to me, and it really crowded the ER when 4 floor patients were brought down at almost the same time. Now I better understand why people wait a long time in the ER, the doctors and nurses all work very had to see patients as soon as they can, but waiting for beds seems to be what slows them down.
Week 5: All you need is a voltmeter
This week we got to witness and experience a few things that were different than what we have seen so far in this rotation and the last. What really stood out to me was the fact that we got to meet a hospital biomedical engineer who maintains and fixes the devices and equipment in the hospital. We shadowed him for the whole day so we better understood the behind the scenes of device management. First, he showed us an anesthesiology machine with a monitor that stopped working in the middle of a big surgery. he explained to us the importance of quickly responding, identifying the problem and replacing the device or component that is causing the problem. It turns out some solution from an IV bag leaked onto the transducer in the anesthesiology machine. The biomedical engineer described how replacing parts of a device are so expensive simply because the company knows you’d rather buy it from them to avoid liability when the components are simple and inexpensive. We also saw the company field engineer look at the anesthesiology machine and decide the problem. It was interesting how first he needed to come look at the problem and then order the parts and then come back later to fix it. This delay can me very problematic especially if the type of device is sparse in the hospital and the spare would need to be used for some time. The biomedical engineer also showed us how he has access to all the monitors in the hospital for if a health care provider calls filing a problem, he can see what the problem is from his end before heading over to that location. It seems that most of his calls are user misuse of the device and not having the proper training on the device. I am sure there is a simple fix for this where time isn’t wasted on the health care provider waiting for the engineer. The biomedical engineer also does diagnostic tests on the devices to make sure they work properly. Some devices do it automatically every morning and sends a report to him. Other devices require a monthly “check up” from the biomedical engineer. The engineer preached the importance of us understanding the voltmeter and ampmeter, because that’s “all you need” to be an engineer. It was interesting to see the back end of medical devices in the hospital and how the processes run there.
Savan Patel Heading link

A second year med student interested in the small things that have big impacts. If I’m lucky, I’ll one day get to work with folks to leave something of value behind that didn’t exist when I first got here.
Health tech, non-fiction books, and the Chicago Bulls.
Savan Patel Blog Heading link
-
Savan Patel Blog
Problems Are Precious
Savan Patel Blog
A week into our clinical immersion program, it’s become clear that no process, no procedure, is quite perfect. Our group has been lucky enough to begin with Urology, a unique specialty in that it demands two unlike environments—outpatient clinic and the operating room.
While the majority of our first week was spent quietly observing procedures (quiet being code for trying not to interfere in the operating room, a near impossible goal in a room with 15 attendings/residents/nurses/students/techs) and follow-up visits in the clinic. When you’re a hammer, the world is full of nails, and when you’re a clinical immersion student, the process of care is full of solutions waiting to be had. While it’s all too early to thematically organize any observations we’ve made, I’ve been trying to push myself to organize that which I do see against a few questions:
- If this problem goes unsolved, to what extent is patient care actually harmed?
- If there exists a better way to do this, how are we defining better?
- If a solution didn’t exist, what answer would I dream up?
The first has been incredibly important in that the small things—a process tweak or new device that I can be fooled into thinking will be life-changing—that I’ve observed this week have often times been isolated inconveniences that don’t necessarily affect patient care.
The second provides a proper framework to not let the initial goal get lost in noise. With its many users (providers, patients, payers), it’s easy to get lost in the noise of healthcare. Just a personal opinion here, but it seems important to keep in mind if better means an improvement for providers, patients, payers, or all 3.
Finally, the third is powerful for two reasons. As the inexperienced ones, a team strength is that we’re blind to what has always been done. While that may lead to some silly-sounding questions, it also is a great strength in that we get to see things for the first time, allowing the suboptimal to appear a little brighter than it may for folks who’ve been staring at the same picture for many years. Secondly, we often underestimate how powerful seemingly antiquated technology is for its users. Take the beeper, the cockroach of medical technology. Seems odd to carry a brand new iPhone 6 in one pocket, with an old beeper in the other. But if asked to create a solution for reliable hospital-wide communication, the function of the beeper and the updates it carries seem to make a little more sense. If you measure the difference between the solution you drafted and the one currently being used, you either come up with a great idea, or have a stronger appreciation for the process in place.
With the sprint that has been week 1, many observations were had and many opportunities for progress were recorded. But as 2 of my teammates pictured discovered, sometimes you just have to sit patiently and wait for the right topic to tackle.
Problems are precious. Choose yours wisely.
Keeping it Consistent
Savan Patel Blog
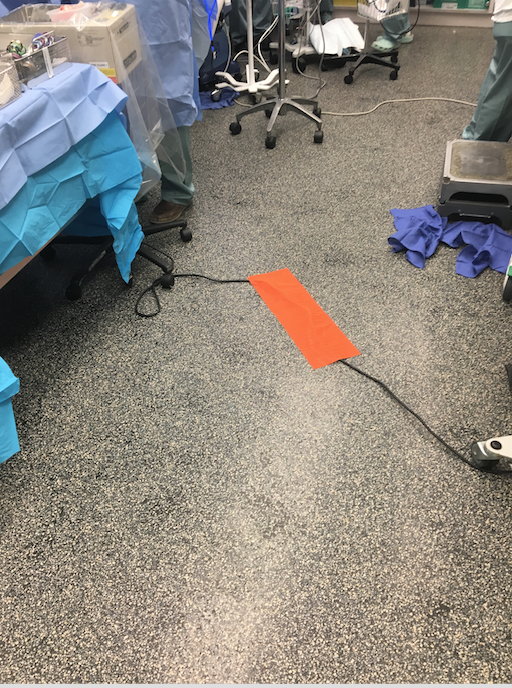
Bundle of wires in the OR, 1. Everyone else, 0.
After seeing an anesthesiologist trip over a wire in the OR, I remember thinking of the mini wire covers (the ones that look like speed bumps!) that you often see at concerts or events backstage that use a lot of wiring. I quickly scribbled a note to look into the use of similar material in surgical rooms as I moved onto the next operating room.
And of course, the first thing I saw was the cover pictured above.
A common theme this week has been that a problem in one OR is clearly and actively prevented in another. The variability is something I’m excited to use as a learning opportunity. Does the variability rise as a function of personnel (different staff, different likes)? Was it specific to the procedure being used? Is it simply a matter of “nice-to-haves” vs. “need-to-haves?”
On the other hand, the wire cover is just one example. The lack of consistency could be traced to other observations including counting lap tissues used in procedures, as well as the availability of different surgical trays for more complex cases. With the covers, it seems as if they should always be used if people do in fact trip on wires, and if it’s not so much of a problem, it seems irrational to spend any funds purchasing the covers in the first place.
With the examples above, it’s more the frequency than the scale of the problem that I find interesting. As an IMED student, we often discuss innovation in terms of technology, and technology in terms of sexy devices and software. However, it’s important to remember that sometimes the most creative answers are rooted in how we use the resources we already have.
Finding the Bright Spots
Savan Patel Blog
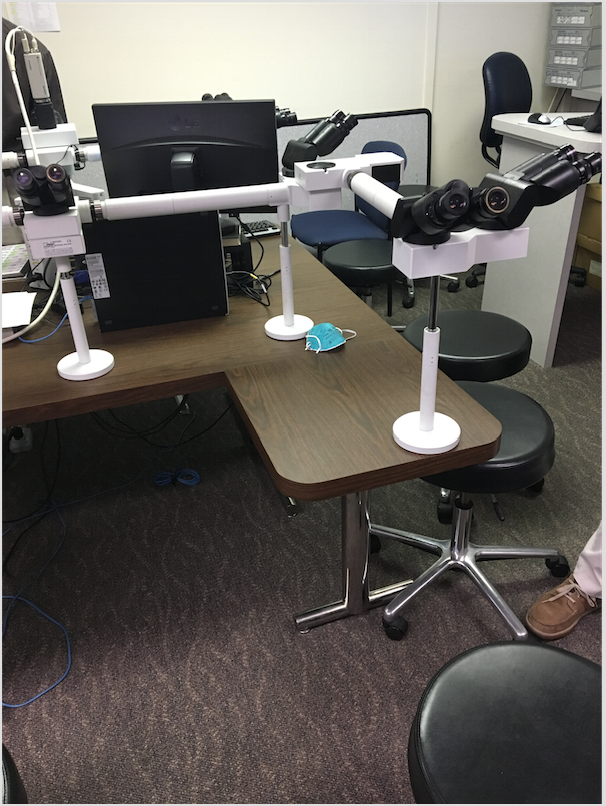
We’re here to observe. To be the relentless shadow that absorbs everything without actually making its presence known. It’s often too easy to note the mistakes, the gaps in processes that could use fixing. As an observer, it’s just as useful–sometimes even more so–to find the most fluid (successful) and seamless processes. Identify what makes them so great. Apply to other situations. Repeat.
A bright spot from early this week was the Tumor Board, a weekly group that meets in the pathology department. The board had multiple players, including doctors from a specific specialty (in our case urology), radiation oncologists, techs, pathologists, and others. The group conferenced around a set of shared microscopes (pictured above) to investigate the nature of various tissues that had been previously biopsied. A few quick notes on what made the board so effective within the hour or so we met:
-Expectation. All parties came in with a clear list of the cases to be discussed and the nature of each one.
-Coupling Expertise. There were many questions, from what specifically allowed one expert to classify a certain cancer as stage 4, to requesting input from colleagues regarding an image interpretation. What made the session impressive to watch was that each physician from a different field was able to simultaneously explain his or her rationale while also teaching a colleague from a different specialty.
-Uniformity. Everyone was viewing the same image at the same time, with only a single case being discussed at any given moment (in the clinic or the OR, multiple individuals may be running between multiple surgeries at once).
-Familiarity. It was clear that the majority of the personnel worked with each other on a consistent basis, allowing for a routine that seemed to make things more fluid.
When looking for ways to improve, it’s easy to start with that which seems most broken. And yet, sometimes it’s even more useful to identify what works well and why.
Start with the bright spots.
Veni Vidi da Vinci
Savan Patel Blog
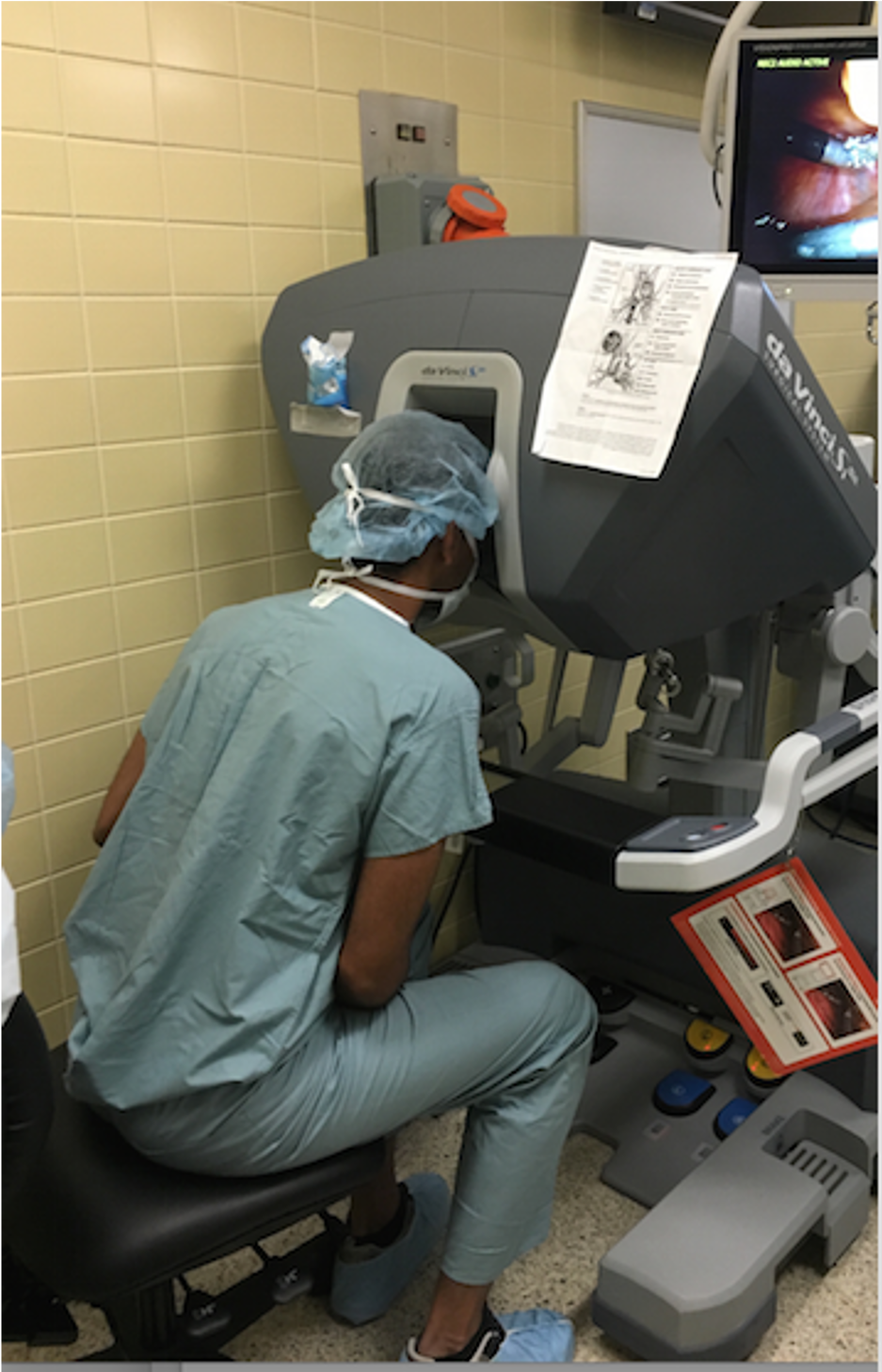
As documented by many of my colleagues, observing a robotic-based operation was something I was looking forward to from the first day of our urology rotation. While seeing the da Vinci system in action raised many unanswered questions (what does training look like? If the same procedure is done both with and without the robot, what governs when either occurs? How much does it cost to set up the entire room?), I’ve compiled a few notable points below:
-Learning. There exists a feature that allows the attending to annotate directly onto the tv screens that display what the camera inside of the patient is broadcasting. While simple, I thought this was an incredibly powerful teaching tool—it allowed the attending to give specific guidance without physically taking the reigns from the resident.
-Degrees of freedom. Ask any surgeon what they love about the robot, and someone is bound to mention mobility. When you stick your hand into an open body during a traditional surgery, you simply can’t manipulate the surgical tools at the many angles and directions that one can when using the da Vinci robotic system.
-Less blood lost. With smaller incisions and greater dexterity, many da Vinci operations don’t even call for extra blood to be in the room because so little is lost compared to traditional operations.
-Traditional requirement. The system still requires one surgeon to scrub in and manually manipulate certain tools during the procedure. Put otherwise, the procedures are more robot-assisted then they are robot-run.
-Operational cost. In a stroke of malicious genius, Intuitive Surgical designed its da Vinci system so that certain parts have to be replaced every ten uses, thus limiting the number of surgeries you can do without repeat purchases.
These of course were observations based on the Si system. In knowing that the OR possesses multiple models, I look forward to observing the others in use.
Final Deliverable
Savan Patel Blog
Last week we concluded our 3-week urology rotation by presenting our final deck to the department residents and the medical students on service. While we highlighted the process by which our observations were recorded, as well as the insights that came from them, I thought it’d be appropriate to share 3 of the major themes of our needs assessment below:
[As a quick aside, while these were extracted from our time in one specific department, many of these are well-accepted trends in delivering care, rather than localized themes from one corner of a specific health system]
1. Miscommunication between staff members or between patients and their providers can lead to lower patient satisfaction and avoidable return visits. Communication is integral to success in any field, and medicine is no exception. Whether it be instructions on where to go next, how to use a certain implanted device, or coordinating prescription availability with the pharmacy, many of the opportunities for improvement we saw were less technology-based and more communication-dependent.
2. Practice begins on patients. The technical expertise developed during residency is by no means small, and much if not all must inherently come from practice in real time while delivering real care under attending supervision. However, we saw an opportunity to create outlets for more simulator-based practice for those looking for additional training opportunities.
3. Effective care is slowed by non-comprehensive technology and equipment. Often times, test 1 is only useful if results from test 2 exist, thus capping the value either can have as they depend on each other. Furthermore, if the process/machine that yields results for test 2 is unavailable, then test 1 becomes uninformative. In that way, we saw great value in the potential for more comprehensive technology that would lessen the time it took to compile desired results, as well as limit invasive procedures that may not ultimately inform the final diagnosis.
With our deliverable shared and feedback received, we feel prepared to go forth and begin our next and final rotation!
Lines vs Paintings
Savan Patel Blog
We’re a few days into our neurology rotation, and it’s becoming clear that angles matter. Each day, we’ve been rounding with the morning team after the course of treatment has already been more or less finalized.
Let’s quickly consider the picture above. When seen from the side, it would appear to be a thin black line segment (side of the frame). Nearly flawless, two endpoints, with a perfect line connecting them, the side angle doesn’t include much noise to sift through. Rotate the frame ninety degrees, however, and you’ve got a wealth of different hues, all combining to form an image that informs a story as seen above.
The neurology team is an incredible group, communicating effectively and swaying between patient rooms with an admirable efficiency as rounds are completed. After a few days of the same morning routine, something didn’t seem quiet right. It was almost uninformative to see daily updates on care during rounds, as opposed to full start-to-finish delivery of care and the corresponding decisions that go into such a process. As each of our 4 team members seemed to come to this conclusion independently, we became more proactive in our discussion with the team to see where the problems they encounter arise. After doing so, it became clear that much of their frustration could be found at the interface of their own patient plans and the care plans of other departments managing the same patient. I was surprised after a few specific conversations to realize that being so deeply embedded into a certain team actually had drawbacks—it was constraining to only see the frame from the side, and not the actual photo.
As we move forward to the final two weeks of our rotation, we’re coming to appreciate the context in which observe nearly as much as what we’re actually observing.
An Overview of Video EEGs
Savan Patel Blog

One of the most common tests we’ve seen done so far is the Video EEG. The apparatus (shown above) is an electroencephalograph coupled with a video recording of the patient. Often used to capture brain wave recordings to explore weather a patient is having true seizures, the technology seems to be a commonly used one in the neurology department. A quick overview of some Video EEG observations can be found below:
-Capturing. First and foremost, the test is only useful if you actually record an episode. Often times, there’s not much one can do if a patient has been recorded for multiple days in the hospital without an actual episode. At that point, the attending essentially makes a judgment call on whether or not to curtail the test.
-Reading. While some Video EEG’s call for short observation periods, others span days. That’s a lot of data. We visited the EEG lab and saw how demanding parsing 4 days worth of data (imagine multiple layers of a continuous line graph for hundreds of pages) can be on the technician. The physicians we spoke with noted that EEG’s were too nuanced to teach to a computer. However, given its pattern-based nature, it seems like it could in fact be a great process to couple with some sort of machine learning/software solution, where you’d imagine the computer would just get better and better with each successive EEG that it reads.
-MRI-compatible EEG leads. There exist MRI-safe leads whose safety and efficacy has been confirmed by much literature. However, they haven’t yet been FDA approved, an obstacle that (understandably) keeps some from embracing their use.
Low Expectations
Savan Patel Blog
“The expectations are so low, people don’t even know these things exist.”
In the rehab portion of Neurology & Rehabilitation, we met with an occupational therapist (OT). While showing us a supply room filled with small prosthetics and malleable tools to help patients with activities of daily living (dressing themselves, showering, etc.), she showed us the item pictured above—a folding bottom wiper for patients who require assistance while using the toilet. While the device itself was simple enough, it had a powerful impact on patients who previously had no means of wiping their bottom, no doubt making going to the bathroom an even more miserable experience.
In describing its simplicity, she noted, “The expectations are so low, people don’t even know these things exist.”
It was incredibly well said.
Yes, for patients utilizing occupational therapy services, but also for surgeons and nurses and technicians. As our summer of needs assessments comes to a close, the OT had articulated so quickly what we’ve seen time and time again. Too often does a very large-scale problem with a very small-scale source go unsolved because there exists no positive inertia to seek out what helpful things already exist. As a classmate of mine once observed, much of medicine is learning how we’ve always done things. We have high expectations for outcomes and surgical devices and providers themselves, but our expectations fall short for the simple things. A surgical tray not being sent to the correct operating room. A specialist failing to coordinate the use of narcotics with a patient’s primary care provider. A patient slipping through the cracks as two departments share her care. Solutions for so many of these communication-based problems exist. But if we accept them as they are, we’re not demanding enough.
Too often, our expectations are so low.
An Afternoon of Prosthetics
Savan Patel Blog

Following a morning of Physical Medicine & Rehab, we were able to swing by a company contracted to run the prosthetic and orthotic program at our university hospital (pictured).
The place was incredible.
The mechanical equivalent of medical surgeons, the group works to tirelessly outfit various patients with custom-fit prosthetics optimized for everything from walking to playing the drums. While we didn’t have much time, the visit sparked my interest in a few follow-up questions. Note-to-self, things to read up on:
-Insurance. Third party payers often don’t help patients pay for physical therapy (PT), a notion that becomes much more interesting when the patient in question just got outfitted with a full leg prosthetic. Look up if there’s any data here, because given the incredible cost of these prosthetics, I’m wondering if having PT meaningfully affects prosthetic limb use.
-Who ideates the purpose of the prosthetic? With something as specific as a prosthetic that can help the patient workout at the gym, does the patient come in with the suggestion, or does a provider make the recommendation after observation?
-FDA Approval. Does it relate to prosthetics?
-Recycling. These bad boys are expensive. Can they be recycled?
Cheers to future reading!
Program Reflections
Savan Patel Blog

With the summer winding down, the penultimate post seemed to be an appropriate time for a quick reflections note:
-Physicians are incredibly well placed to innovate. Not only do they hold the unique position of being the user, but they are also a nuanced group in a field with an incredibly high barrier to entry. The nuances that propel a high volume clinic, or a well-run operating room are anything but intuitive. A problem is incomplete without its context, and context is often foreign to an outsider in a space as noisy as healthcare.
-Problems are precious. As was noted in post 1, it’s easy to be misguided by the opportunity to “improve.” Often times we’d see a silly problem that could have a meaningful solution. But then you have to step back and ask, “What’s the consequence of letting this problem go unsolved?” If it’s large, you’ve got something worth exploring. If not, move on.
-Observe problems before you ask about them. Few healthcare workers will struggle to rattle off a list of 5 annoyances. The danger here is that they’re often framed as solutions. Claiming, “We have to wait too long for our patients to urinate for the test” masks the underlying problem of proper appointment preparation. A simple example, but the logic quickly extrapolates to the point where abstracting a solution from someone else entirely cloaks the fundamental problem, and by extension, clouds your ability to provide a true solution.
Final Deck, Neurology
Savan Patel Blog
With the final day of presentations upon us, I’ve taken a few of our insights from neurology and summarized them briefly as follows:
Opioid exposure can result from poor inter-provider coordination. Over prescription doesn’t happen in a vacuum. Whereas antibiotics can be isolated to whether or not a single provider is prescribing the right drug for the right condition, narcotic prescriptions would often build because patients would arrive with multiple opioid prescriptions prescribed by a non-neurologist for neurological problems.
Quality of communication influences quality of care. As one provider noted, “80% of neurology is history taking.” However, intrinsic to many neurological conditions are limitations to patient speech, requiring that complete histories often be taken anecdotally from a family member. Furthermore, drastic changes in care—such as the transition to hospice—are difficult to navigate in cases where a patient is unable to communicate due to an expressive aphasia.
Savan Patel Blog
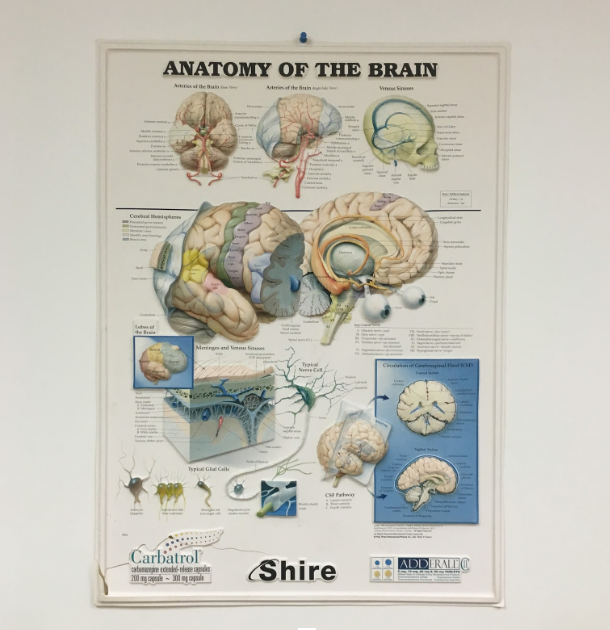
Readings/Recordings are subject to individual user bias. In the case of MRI, brighter objects are naturally perceived as being larger than equally sized dark objects. Additionally, one cannot see what is not present on the scan. If a scan is abnormal not because of an unnatural presence, but instead, an unnatural absence, a reading error is more likely to occur. There also exists conflict between subspecialties when reading scans. In the case of the regional cerebral blood volume (rCBV) exams, a radiologist may note they see tumor, while a neurologist may disagree. However, once mention of tumor growth is placed in the medical record, retraction is difficult.
Christine Massie Heading link

I’m a senior in bioengineering with a concentration in cell and tissue engineering. Gastroenterology/Hepatology and Radiology are my two rotations. I chose these two rotations because my research in the past has dealt with liver and colon tissue samples and I wanted to see how the entire system works in the human body, and radiology has always interested me because its so cool how you are able to show what’s happening with in the body. I’m very excited for this program since I aspire to become a physician, and I can experience the clinic environment first hand.
Christine Massie Blog Heading link
-
Christine Massie Blog
First Day
Christine Massie Blog
Just with any new beginning there are several emotions involved. I was basically split 50/50 between excited and nervous. Excited for the opportunity and journey I was about to embark on, nervous because I wasn’t sure what to expect since this program is so open ended.
Based off the information given for the GI/Hepatology rotation, we were to report to the clinic. Ideally, someone at the clinic would know we were coming and be familiar with the program. However the information we received was from the previous year. However, a registered nurse gave us a suggestion to go to the new fellow’s office in the hospital. Once we met the fellow, Dr. Khan, things quickly turned around, emotions turned form nerves to pure excitement. The fellow was truly our saving grace to the rough start of the day. He wasn’t aware of the program, but once we described what we were doing, he seemed just as excited to have us in the department. He mentioned he had a few suggestions of some clinical problems he had noticed from his own experience.
Once the introductions ended, we talked more about GI in a general sense. I took a physiology course last semester, and it was amazing to see these concepts I became familiar in class discussed in real life. During the afternoon we became more familiar with how the hospital works with the dynamic between the primary care team and a consult team. The primary care team is just as it sounds, they deal with all the primary care and make the final decision for the care. Whereas, the consult team deals more with checking in and analyzing the situation and decide what care plans they would enroll and communicate this with the primary care. I felt that this system was very efficient since there are two separate teams working on the same patient so the care can be maximized with this collaboration. We consulted with a few patients in the hospital, one of them being a native Spanish speaker. Even though an interpreter was easily accessible, the fellow did a fantastic job speaking with the patient when he, himself was not a native speaker. I feel that it is important in medicine for the physician to connect with the patient on a personal level. There must be a trust present, despite not knowing each other for more than possibly a few minutes. Currently I want to go into medicine because the overall fields of medicine and technology interest me, but I want to be interacting directly with the patients opposed to indirectly like a bioengineer could.
Since Dr. Khan mentioned he had a slower day, he didn’t have much after consulting with patients. We made our way back to the clinic hoping for better luck than earlier in the day. Sure enough we had great luck! A physician in the clinic that wasn’t around when we checked in earlier was now there, and she knew who we were and what to do with us. We shadowed a few physicians in the clinic for the rest of the afternoon. This process was pretty routine, just seemed as if times it picked up and others it slowed down. With it being a teaching university I thought the dynamic between the fellows and attendees was interesting. The fellow would consult with the patient first and discuss the case with the attendee. They would then suggest what they would like to do with the care plan. From what I saw there usually agreement between the fellow and attendee, except for specifics. However the one thing that made this part of the day memorable was seeing patients with Nonalcoholic Steatohepatisis (NASH). Currently at research my main project deals with liver biopsies from patients suffering from NASH. I only deal with the disease on a very small scale, but I was actually able to see it in live action. I was able to see what problems these patients run into and why these symptoms occur. One of the reasons why I chose this rotation was because I’ve dealt with colon and liver samples and wanted to see it more in real life and make personal connections.
Overall from the beginning of the day was a little rough since we had the wrong information, but we received the new updated information! It turned out to be an awesome first day! Now it can be a little funny how lost we were the first day, but we somehow made the day a success. Since the first day was finally out of the way, I was extremely excited to see how the rest of the week would unfold.
Week 1: Work Flow Within the Clinic
Christine Massie Blog

For the rest of week 1, we were in the clinic for a most of the time, except for the few times we got to observe procedures. The clinic had different paces with different dynamics between the physicians. During faster paced days, efficiency was truly key. One morning we were shadowing the attendee, Dr. Nannegari, which this pace was much faster than shadowing the fellows. Dr. Nannegari was going from patient to patient quickly, I was amazed how she kept everything straight. Another day I was shadowing a fellow, Dr. Skef, but the pace within the clinic was faster than other days. The patients kept coming in constantly. Dr. Skef understood how important efficiency was in these times. Typically the fellow would consult with the patient, discuss the care plan with the attendee, and both the physicians would go in to talk to the patient to discuss the plan. However during the faster paced times, Dr. Skef would double check his care plan with Dr. Nannegari. Once the plan was agreed upon, Dr. Skef would go into the room alone to speak with the patients one last time, so Dr. Nannegari could see other patients to maximize productivity.
One problem I noticed while shadowing Dr. Skef in terms of efficiency was the interpreting phone service they use in the clinic. It was Dr. Skef’s first time using the service, but he didn’t have problems figuring it out. However the service disconnected mid-conversation. Once this happened, Dr. Skef had to follow through with the entire process again. The process consisted of dialing the number, selecting the language from the menu, and once an interpreter answered they listed their name and their ID number. The interpreter asked for the department, physician name, and patient identification number. With Dr. Skef’s name, the interpreter had to ask how to spell it which took even more time. This time is not only inefficient, but could potentially make the patient feel uncomfortable since there’s added time to build up anticipation. Even though efficiency is key in a clinic environment, the patient should be comfortable as well. One thing I noticed was that you select the language you need for interpretation by selecting from a typical phone menu, #1 was for Spanish. I thought it was convenient for #1 to be Spanish since it seems that it is the most popular language in the area. The #2 option was Mandarin. I’m not sure if the demographics of the patients that come to UI Health were used while making the menu, but that would be very beneficial. For example, if the second most popular language is Polish, that should be #2 on the menu instead of the last option. That way the physician doesn’t have to listen to all the selections before getting to Polish. Another way for helping the efficiency is the interpreting service should have a list of phone numbers that they can recognize what departments the calls are coming in from. I’m not sure if these calls come in as a caller ID or not, but it would help if the interpreting service could see the department that the physician is calling from instead of asking for during the conversation. If it is critical for the interpreting service to have the physician’s name, then each physician could have a four digit code which could be entered during the process. Entering four digits would take less time than spelling out names.
Besides efficiency, communication between the physician and the patient is important. Sometimes it can be difficult to explain pain to others and give specific details. Sometimes pain can be described very well, other times pain may be indescribable. Especially with GI describing symptoms may be uncomfortable, since it is very personal. The appointment starts as a usual appointment would, the physician asks how the patient is doing and why they came to the clinic. After this, things get a little bit more personal. Even though these questions may make the patient uncomfortable, it is essential for their care that they open up to the physician. Even though efficiency is important for a clinic to run smoothly as a whole, the interactions between the patients and physicians are important more for the individual getting the best care possible. Physicians must work efficiency in the clinic, but they must also take time with the patients to understand what is truly going on within their body.
Week 2: Introduction to the Endoscopy Lab
Christine Massie Blog

For week two I have been in the endoscopy lab observing different procedures and learning about the equipment used. However when the clinic was slow during week 1, we did have the chance to watch some procedures. The first procedure I saw in the lab was an esophagogastroduodenoscopy, commonly called EGD. This procedure consists of using a scope, the knob is in the featured image of this entry. The other end of the scope contains a flexible end with a light and camera, which is controlled by the knob. The picture from the scope’s camera is projected onto a monitor for the physician to examine, this image is inverted. The knobs are used to move the scope up, down, left, or right. For this patient, she was only partially sedated with drugs administered by the nurse. These drugs help with pain, and actually the patient will not remember the procedure. Benadryl was also available to help the patient feel sleepy. Before the scope is interested into the mouth, a mouth guard was placed to protect teeth and the scope. The patient was then laid on her left side, and a cushion was placed behind her back back to help her stay in that position. Once the patient seemed to be sleepy, the scope was inserted into the mouth and went through the esophagus, stomach, and duodenum. While doing this procedure the physician was looking for any abnormalities and taking pictures with the scope that were saved onto a software. However in the middle of the procedure it seemed as if the patient started to have discomfort. She started to move around and attempted to raise her hand to grab the scope. Overall, I thought the procedure was amazing. I have never seen an endoscopy procedure before so I was not sure what to expect. I was surprised that she was just partially sedated and that worked fine; I expected an anesthesiologist to sedate the patient. However during a different procedure I observed later, a physician explained more of the sedation process. Patients are sedated for comfort and prevent the gag reflex. Apparently back in the day EDG were done without sedation. Some countries today still perform EDG without sedation, which I’m glad I won’t be getting an EDG there any time soon!
The second EDG I observed the patient was fully sedated with help of the anesthesiology team. For this procedure an attendee and fellow were in the room, the fellow mainly performed the procedure. The attendee said this procedure was a better teaching environment with the anesthesiology team there. She could focus on teaching the fellow opposed to making sure the patient did not move too much due to pain. However there was a problem trying to make a turn during the procedure. The fellow was having problems and the attendee was not able to describe the procedure to get around the turn in words. The attendee then tried making the maneuver and succeed. However I felt that this movement was quite difficult, the physician had to move both knobs in opposite directions and physically turn the body to the right. I was truly surprised that physicians have to sometimes turn their entire body to move the scope. During this procedure some biopsies were taken which was quite interesting to watch. A wire with a clamp at the end was fed through the scope. The physician had to keep feeding the wire in blindly until the clamp showed up on the monitor. Then the physician had to direct the technician or nurse to open and close the clamp as needed. Once the clamp was closed and part of the tissue was in the clamp, it was raised to remove it from the wall. This would usually cause some bleeding, but the patient would not feel this at all. When the scope was being taken up, the patient had some problems. The anesthesiologist mentioned she had an asthma attack, I wondered if this is usually common people getting EDG with asthma, and if so why did the attack happen.
Both of the above EDG procedures, I observed the first week so I was not familiar with how the lab actually worked. During the first two EDG, I just went back into the procedure room without observing the lab. The start of the second week was observing how the lab worked. A nurse showed us how she would prepare for a patient. A drug bank is used to retrieve the sedation medication in which the nurses have finger print access. However the nurse had problems with the finger print so she entered her ID. I thought the finger print for the system was nice because it could potentially save time. However, in our case it probably added on time since it took a few tries, but she ended up entering in her ID. The nurse then selects the patient from a database. The nurse would then select the drug and the amount on the computer. Once this is entered a drawer opens with the drugs. During this time, the patient has a magnet on a white board behind the desk placed at the waiting room they are currently in. So if this patient was waiting in room A, their magnet would be right next to the magnet letter A. Once they are moved into the procedure room, this magnet is moved to indicate what procedure room they are in. As we were describing to the nurse we were bioengineering students looking for problems within the clinical environment, she immediately mentioned the wires being on the floor. This seems to be a common problem in all departments. I noticed some wires were zip-tied together to keep them localized. Even though I noticed wires being on the ground was a problem in most procedure rooms, I did notice one room had a cable cover. But the cable cover wasn’t covering any of the cables so it was a waste. This particular patient was getting both the EDG and the colonoscopy. The physician examines the large intestine during the colonoscopy. The EDG is performed first, and once this is complete the scope is unplugged and the patient’s bed is turned completely around. While turning the bed a complete 180 degrees, you can really see how small the procedure room is. During this colonoscopy a polyp was taken out. Since this polyp was bigger, a bigger trap was used. Smaller ones are taken out by the same type of clamp used for the biopsy I described earlier. However this bigger trap looked like a diamond that the physician would adjust so the polyp was in the middle of the diamond. Once polyp was in the diamond, the physician would instruct the nurse to close the clamp and retrieve the polyp.
Another EDG I observed the patient was not responding well to the sedation medication. The physician asked if the patient takes any pain medications or drinks alcohol frequently. I thought this question odd since it seems more like a screening question on overall health of a person. This particular patient had drank recently. The physician then told us that drinking alcohol and in taking pain medications can actually make the patient more tolerant to the sedation medications. Also, this patient had a higher blood pressure so this was monitored very closely while administrating the sedation medication. The physician said he would attempt the procedure, but he was not sure how the patient would be during it due to the tolerance to the medication. However this scope did not last long since this patient had his stomach taken out, which the physician was not expecting this. The patient had a small section of the stomach connected to the side of the small intestine. The physician said it is better to connect things from side to end opposed to end to end, meaning it was better to have the side of the small intestine connected to the end of the stomach.
Overall the start of week 2 was fantastic! This was a completely different environment opposed to the clinic. It was interesting to see how even in the same department can contain such different routines. I’m very excited to see where the rest of the week takes me!
Week 2: A Lot of Acronyms
Christine Massie Blog

The rest of week two was spent in the endoscopy lab watching a lot of procedures. With all these procedures came a lot of acronyms. The two most common procedures were esphagogastroduodenoscopy (EGD) and colonoscopy, which I explained in the first post of week 2. Different procedures I was able to observe were endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasound (EUS), EGD with dilation, flexible sigmoidoscopy, double-balloon enterscopy (DBE), and capsule endoscopy preparation, a procedure for a bedside patient, called by the department as “roadshow”. It is called a roadshow since there is a cart with all the equipment on it, and the cart is taken on the road. Overall it was a very busy week. It would be very long to go into a describe all of these procedures, I discussed an EGD and a colonoscopy in my previous blog “Week 2: Introduction to Endoscopy Lab”.
The most intense procedure was the ERCP. The reason being is the physician is trying to get into the bile duct, pancreatic duct, and gallbladder, which is out of range for the scope. Radiation is used to visualize the location of a wire that is fed through the scope. Everyone in the room needed to wear a lead outfit due to the radiation. During this procedure the physician was looking for stones, removing those, and looking for other abnormalities. The reason why this is so intense compared to the others is because it is a very difficult process for the physician to do these maneuvers. The physician will know if stones are present in the gallbladder, but may not know if there are stones in the bile duct. The reason why the stones cannot be seen in the duct is due to it being overlaid by the duodenum. Usually ERCP procedures were the longest procedure. The scope used for the EGD and colonoscopy has the camera looking forward and a light that flashes, but the scope for the ERCP looks over to the side, but the light does not flash. The reason why it looks over to the side is to help the maneuver to the duct. I’m not sure why this scope does not flash though. During one ERCP I observed the catheter buckled in, I believe in the bile duct. The physician had difficulties getting this out, but after a while he was able to remove it. With this long procedure, somewhere between 1.5-2 hours, I realized how heavy this lead truly was. I was just standing in the room, I couldn’t imagine being someone active during this procedure and moving around with the weight of the lead. It would truly be a workout, and the two physicians I saw do this procedure were sweating after.
The least intense was the capsule endoscopy preparation. The patient had to swallow a pill and let it go through the entire GI tract and exit in body waste. The pill had a small camera on it that would show the same thing you could see from an EGD or colonoscopy. The pill remains active for 12 hours in the body, and electrodes (possibly 6) are placed throughout the GI tract. The GI department at UIC does the wired-capsule with the electrodes on the body, but a wireless capsule technique does exist. The reason why the UIC department chooses the wired technique is because it is easier to detect the location if an abnormality is present. All the preparation was done by the nurse, except one of the fellows received the patient’s consent. All these electrodes are wired and feed into a little box. The patient has to carry the box around, there is a strap for it to go over the shoulder. The box contains all the information of the pill. This box has a flashing blue light at the top that means everything is good with the pill. If the light turns off, the patient was directed to call the lab. I am not sure if there is some type of audio warning when the blue light turns off. I feel that this would be useful because the patient may not check the blue light for a while, and it could be turned off. The pill was quite large, and it seemed as if the patient had discomfort swallowing it. Also the department currently has 3 of these sets and one is currently broken. They depend on the patients returning the sets to the lab the next day. I’m not sure how common these procedures are, but I wonder how hard it is to schedule a capsule if there is a limited amount of sets.
A very interesting procedure was the double-balloon enteroscopy (DBE), the picture above is the scope used. This technique allows the physician can see more of the small intestine. During the EGD, they can only see the beginning of the small intestine.
The balloons are inflated and deflated throughout the procedure to advance the scope. This procedure required the most amount of physical maneuvers for the physician. There was a key pad the physician could control the inflating and deflating of the balloons. However the key pad had an altering sound to possibly note the tension of the second balloon was tight. The physician found it much more of an annoyance than a help. He would usually listened for the balloon inflating and could tell when the balloon was close to its maximum. At first the physician simply pushed a button to turn the sound off when it went off. As the procedure went on, things got more intense because it was very difficult for the physician to advance. From this stress, the sound did not help. It was evident he was getting much more frustrated by it. He even told us one time during this type of procedure years ago, he actually pushed the button down so hard from being so frustrated the button went completely into the pad and broke. This procedure set up was most difficult for the anesthesiology to move in and out of the room with their rotating groups. There was one time an anesthesiologist had to move the key pad to get to the door to exit, and it seemed as if the physician was annoyed by that. If I was the physician I would be annoyed too because I would want everything to be in the correct spot and to stay in place.
As much as I would love to expand on the other procedures I observed throughout the week, there just isn’t enough time to type all of them out. However I will expand more on some information one of the medical technicians gave me. She stated the biggest problems the lab has are scheduling and space. An example of a scheduling problem, one morning the nurses had a staff meeting and were not back into the lab until about 9am. One patient came at 7:30am and was not brought back into the procedure room until close to 9am. Space is a huge issue in this department. There is a lot of equipment and just enough space for the bed. The technician said she worked at another hospital that for a double scope, an EGD followed by a colonoscopy, they had enough space to turn the bed a complete 360 degrees without a problem. However in this department, it can be tricky to switch from an EGD to a colonoscopy. I asked her what she would do to change the setup they have now. She said it could be helpful for the housing unit for the scope and the cart with everything on it to be set up against the wall. This would give some more space and keep the wires more located to up against the wall. She also suggested the power coming from the ceiling, which I personally thought of too. These set ups already exist at other hospitals. Another interesting point the technician made that I found very interesting was about the gowns the physicians, nurses, and technicians wear during procedures. The gowns are very frugal because they can be washed and reused. However these gowns are yellow. She said it could be helpful for the gowns to be a different color. The reason why they should be a different color is because usually gowns used for isolation contact patients in the hospital are yellow. She stated the yellow gowns for the procedure could give a confusing message since these patients are not on isolation, but they are only getting a procedure. I really liked this point because I never thought about it before, but it really does make sense. Additionally she stated that the area they work in during procedures is very dim, to help the physician. However this dim setting is not helpful for the nurses or technicians. During the middle of the procedure the physician may say he/she wants a specific device to remove a polyp or take a biopsy. The nurses and technician have to prepare for this collection. This collection involves getting the specific device and labeling the container for what the collection is for. The technician said she has seen other set ups that use color coded glow in the dark to organize the devices and such. Not only would the glow in the dark be helpful, but the color coding would be more efficient for organization. With this increased organization it would decrease the amount of time wasted looking for things during the procedure.
Overall, week two was a success! This dynamic was much different from the clinic. It was very insightful to get a taste of the clinic and the lab. Next week our tentative schedule says we should be doing inpatient consults which will be another change in dynamic! I cannot believe my time within GI is already half way over, and I only have a week left. It’s been truly amazing and insightful. I look forward to making the best of this last week within the department.
Week 3: On Service
Christine Massie Blog

The start to week three was a complete switch in dynamics. We were shadowing one of the fellow’s on service. The fellow would need to see all the patients that would be using GI care as the consult team. This week has involved a lot of walking and talking to people. Monday was actually the first day the fellow was on service, so he was nervous since he wasn’t sure how the system worked. He also felt that the hospital was hard to maneuver around. Monday consists of seeing a few patients and the fellow would discuss with them that the GI team would be assisting in his/her care. The day was concluded with rounds. Rounds happen every day, and I felt as if they can be overwhelming because it’s a lot of information being presented very quickly. This week I’ve been able to observe rounds for the GI department and also the Hepatology department as well. A difference I noticed was Hepatology goes more in depth and more problems can arise. What I mean by it goes more in depth is because not only does the liver have issues, but they try to understand why the liver is having these issues. Sometimes these patients suffer from serve addictions to alcohol so withdraws can cause symptoms aside from being sick.
Week 3: Farewell to GI
Christine Massie Blog
Cannot believe my time at the GI department has come to an end. The past three weeks went by way to fast. I learned so much from this rotation, mainly the anatomy of the GI tract. The last day was very interesting. We did our presentation in front of most of the GI fellows and our supervisor, Dr. Carroll. After the presentation, the fellows had to attend a workshop on foreign body objects. This workshop consisted how to get random objects out of the body if a person swallowed it. A problem that they run into at UIC is some prisoners swallow whatever they can find so they can spend time in the hospital. Some of the fellows actually mentioned some prisoner kept swallowing whatever they could find and racked up $1 million in medical bills. There was an article on him in the Chicago Tribune. Some examples of foreign bodies that were discussed were toothbrushes, batteries, and buttons. The person that led the workshop actually said that toothbrushes are commonly swallowed by people who suffer from bulimia, since they usually lose their gag reflex. The objects that they used to grab these objects were very interesting. There was a lot of choices for the physician to use. However some of the physicians were a little nervous to use was a claw similar to one used in a claw crane. Some felt if this claw was used, the object could possibly fall out as it is being pulled up out of the body.
One of our last notes for GI was seeing a colonoscopy for someone that was bleeding in their colon. This was very interesting to see since we always heard the physicians usually described patients as a “bleeder”. I felt as if it was hard to determine if there was abnormalities in the colon since the blood covered most of the lining of the colon. A lot of blood was suctioned out of the body.
Overall, my time at GI was a blast! I’ll remember this rotation for a lifetime. The procedures I got to see were so fascinating, and the physicians I met were even better. As of now, I’m still interested into going to medical school this rotation made me realize how much I love medicine. I’m very excited to start my rotation in Radiology, but the GI team set the bar very high!
Week 4: New Rotation at Radiology
Christine Massie Blog

Week 4, means starting my new rotation at Radiology. I was very excited for Radiology because imaging is very fascinating to me, and I’m also taking a biomedical imaging class in the fall semester. The physician that is the primary contact for this program, Dr. Bui is very interested in interventional radiology. Our first day in the department, he gave us a quick lecture on interventional radiology, some examples of procedures done, and the techniques used. He asked us what we wanted to observe; he thought interventional radiology would be more beneficial to us. Our group decided we would start in interventional radiology and decide if we want to observe the diagnostic end of radiology. Interventional radiology (IR) is using imaging techniques to help visualize during a procedure. IR is really cool because it is very minimally invasive, but the procedure has such a high impact for the patient’s health. This rotation is a lot different from my past rotation in GI, since they were always dealing with the same track and usually similar problems. However, one common denominator was I did see ERCP’s in GI in which radiation is used to help the physician obtain the bile and pancreatic ducts, which is a similar set up to IR.
One of the first procedures we watched was a chest port placement. This is a catheter connected to a plastic reservoir. The port is inserted under the skin. For this particular port placement it was to be used to administer chemotherapy. Another procedure we observed was a transcatheter arterial chemoembolization (TACE). This was really interesting for me because during my GI rotation some physicians were discussing a patient could receive TACE for a treatment of their liver tumor. It was very interesting to see this applied. This procedure restricts the tumor’s blood supply. It is localized way of administering chemotherapeutic drugs. However the tumor will not disappear, but it will decrease in size. This is a very cool way to deliver chemotherapy and treat a tumor since it is minimally invasive. This area seems to growing, since this technique is mainly used on liver tumors. It should be interesting to see in the next few years if this procedure treats multiple types of tumors.
Week 4: Stents, Filters, and the AngioVac
Christine Massie Blog
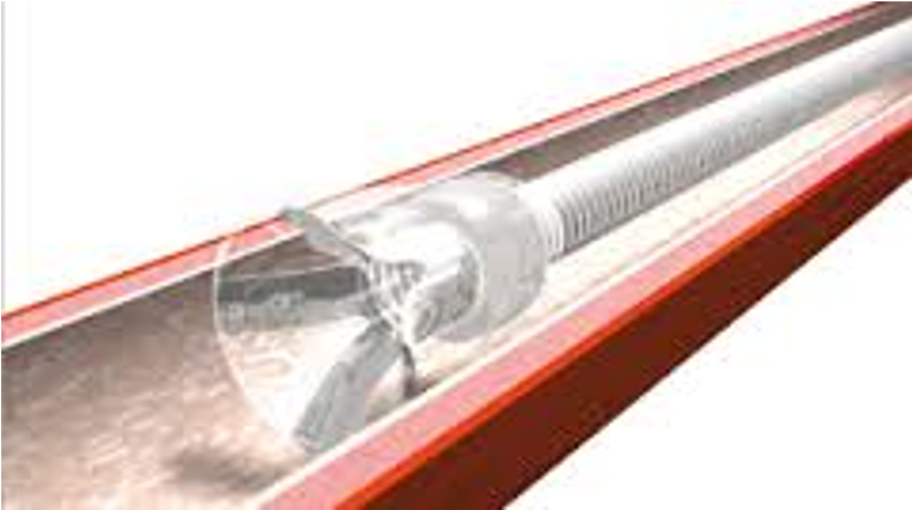
By the middle of the week I felt pretty comfortable around the IR lab and was finally getting the hang of things. The first few days were a little overwhelming because it was a lot! IR does some pretty amazing things. On Wednesday, the department had an in service in which a company representative came in to discuss a product and how to use it. The particular product was a laser that helps treat varicose veins. The beginning of the in service was a little boring since the representative mainly discussed how the nurses and technicians should operate the product. However once the nurses left we got to ask a few questions and see some other products. The most interesting product we saw was the AngioVac, which is the featured image of this post. This device basically acts as a vacuum to suck out large blood clots. Dr. Bui actually showed us a case that he used the device. The patient had a huge clot, and we were able to visualize some of the suction from the radiation pictures that were saved. Dr. Bui expressed how he would find it beneficial for the device to be made a little smaller. There is a device similar to the AngioVac however the suction technique is much weaker. Dr. Bui explained how the device can be difficult to maneuver since it is quite large. Additionally Dr. Bui stated it would be beneficial to have a smaller device so it can help with smaller clots.
We got to see other devices used, mainly stents and filters. The picture I had for the filter did not insert properly. But the design creates laminar flow and there is a hook at the top so the filter can be easily removed. I thought this design for the filter was interesting, I saw a similar design for an object in GI however it was used to trap foreign bodies. Some stents were saw are pictured here
The stents with the white covering are considered closed. The more interesting stent we saw was the stent used during Transjugular Intrahepatic Portosystemic Shunt (TIPS). This stent serves as connection between the hepatic vein and the portal vein in the liver. A picture of the stent is here:
The image for some reason is inverted. But the open part of the stent is released first and it expands. Once the open part of the stent is deployed, they will pull back and feel the stent get caught on the liver. Then they can deploy the rest of the stent. This design is very interesting since the open part allows blood to flow in and out, but the closed part prevents bile from entering the blood. Despite this great design, this particular stent comes only in one size. This can be difficult because not everyone is the same and too big of a stent may have too much flow; whereas too small of a stent may not have enough flow.
Overall, it was very interesting to see the stents, filters, and other devices used during procedure. My first week at interventional radiology was amazing, and I’m very excited for these next two weeks.
Week 5: More Elegence of IR
Christine Massie Blog
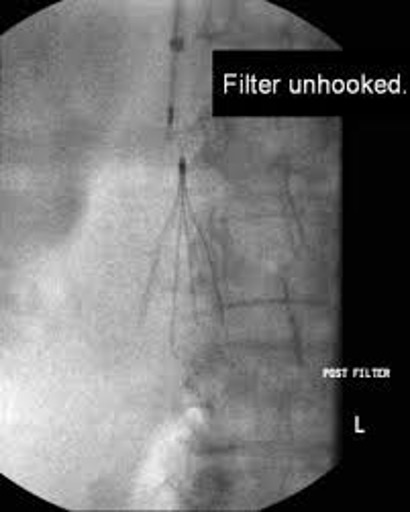
By the second week in the IR lab, we were able to observed majority of the procedures. Since our group already saw some problems and took note of a lot of observations, we asked Dr. Bui if we would be able to observe general diagnostic radiology for a day. We all agreed it would be beneficial to get some exposure of the field. We’ll be with diagnostic radiology for the day tomorrow.
This week we actually got to go into the OR for a procedure. This was actually my first time in the OR, since GI had procedures in their own lab. Dr. Bui had to insert a tube into the patient before the surgery team started operating. This was interesting to see the change in pace and work flow between the two different operating settings. The IR team brought all the supplies that were going to be used during the procedure to the OR. However, they did not bring a proper sized balloon catheter, and the technician had to run back down the IR lab. This was the only time I observed miscommunication between the IR team.
Another interesting case we saw was a kidney biopsy for a patient with an intraperitoneal, transplant kidney. Dr. Bui called the transplant surgery team to communicate with them he was preparing for a biopsy and there would be a chance the patient would start bleeding. If this was the case, the patient would need to be brought to the OR immediately. However, this biopsy went fine. The device used to take the biopsy had an inner needle that is deployed when the outer needle is in place, working like a spring. However when the inner needle is deployed it makes a large click noise. Dr. Bui actually notified the patient the device would click and showed them before the biopsy was collected. Even though this click noise may not hurt the patient much, the noise makes it sound a lot worse than it is. Even though the patient heard the sound before, they did flinch when Dr. Bui collected the biopsy. Another procedure we got to watch was an inferior vena cava filter (IVC) filter being placed. I mentioned this filter in my last blog post. This procedure was very elegant and swift. The deploying device was placed properly, and it only took a few seconds for the filter to deploy.
An interesting point Dr. Bui made was only 40% of de-clots have a success rate after 3 months, which this seems very low. It would be interesting to look into what happens with the other 60%, what exactly goes wrong, and if there’s a common problem. Another interesting point Dr. Bui made was about the transjugular liver biopsy. He stated that there is progression being made on the engineering side of the procedure. He stated that they are working on getting a hand-held spectrometer to scan the biopsy and be able to read the diagnosis instantly. I feel that this would be very beneficial and interesting to observe.
Week 5: Going to the OR
Christine Massie Blog

During my time at IR, the team prepped a patient in their lab before they went to the OR. In this case this patient was getting a large kidney stone removed. IR had to insert a tube to serve as a guide for the urology team to use in the OR. The IR team had some problems placing the tube properly because they were trying to place it in a specific orientation around the stone. This portion only took about 15 mins. After the IR team was done, the patient was going up to the OR. Dr. Bui suggested we go to the OR to see the urology end of the care because he said their work is really cool. Dr. Bui suggested we go check the OR an hour after he placed the tube. An hour went by and we checked the OR board and the patient was not in the room, so we decided to wait a bit. After some time the patient was finally in the room, and the operation started about an hour after the scheduled time.
The urology team started the procedure and they came to a point when they had to use a scope. Turns out the scope’s lens was broken and only ¼ of image was displayed. The physician asked the company representative to find out where the other scope was. The other scope could not be used immediately since it was not sterilized. The physician asked if it would take 2 hours for it to be sterilized, and the company representative said it would probably take that long. The physician asked the rep if they checked the scope beforehand, which they did not. This seemed absolutely absurd that no one would check the scope before starting the procedure, instead of realizing in the middle of the procedure it was not working. The representative was going to call Rush to see if they could borrow a scope from them, but I feel like this would affect the sterility process negatively. It seemed that was the game plan the team decided on, my partner and I ended up leaving the room since tensions started to rise. We went to get lunch and went back to IR. We saw Dr. Bui and he asked if they were still missing stuff and we explained everything. He said it was probably best to stay in the IR lab since that OR would be very tense. This makes me curious what would’ve happened if this circumstance occurred in a rural hospital where they wouldn’t have a neighboring hospital nearby to borrow one. There was plenty of time for the scope to be checked anyways since there was a large chunk of time between when the patient initially got into the room to when the procedure started.
Week 6: Biopsy Needles
Christine Massie Blog

After Dr. Bui collected a biopsy, he let us look at the devices. During this particular procedure, the first biopsy needle being used had problems collecting tissue. They switched to a different needle which worked much better. After seeing both needles, I think the second needle that was used is much easier to use. The second needle used is very similar to the featured image for this blog post. The two grey buttons are pushed down, and either the yellow switch on the side or the button on the very bottom can be used to collect the sample. However the reason why I thought the first needle used was harder to manipulate was because there was a safety piece you had to pull out and lock and push back in. It was really cool to see the mechanism behind collecting the tissue and deploying the sample into the dish.
There was an in-service for a new stent that was going to be used for a biliary duct. The company representative considered this to be a closed stent. However this did not look like a typical closed stent, but it was more of a material coating. This type of coating would make it easier to deploy the stent. Currently some stents want to spring forward and tend to be misplaced, but the coating prevents this. This was cool to see, because during one of the procedures our team observed stents being misplaced due to the deploying mechanism.
Final Thoughts: Innovation in Rural Medicine
Christine Massie Blog

The past 3 weeks in IR went by just as fast as the weeks spent in GI. The last day in IR was very enjoyable because we were able to observe a procedure in the OR, and Dr. Bui showed us how an ultrasound works. It was really helpful to see how the ultrasound works, I was always confused looking at ultrasound images. Overall my time at IR was great! The physicians were very eager to teach us and very welcoming. I was not too familiar with IR before this program, so it was amazing to get exposure to the field. After going through this rotation I’m very excited for my Biomedical Imaging course in the fall semester.
Overall, this program was great! I came into the program with the goal of become a physician, which this is still my goal. I am very passionate about engineering, but I have a deeper passion for patient care. Innovation in medicine is truly a growing field, which is is very exciting. However after completing this program something I became much more interested in is innovation in rural medicine. Coming from a smaller town, I can imagine the huge limitations in rural medicine, technology wise, since resources can be sparse. I think it should be interesting to see how innovation in medicine grows, and I really hope this grows and even focuses on innovation in rural medicine. I will be applying to medical school a year from now. After this program I’m heavily considering applying for a rural medicine program, just because I see the huge potential in innovating in rural areas. Even though rural medicine may not be as diverse as urban medicine, physicians ultimately need to maximize care with limited resources. Granted rural areas are not as limited as austere environments, but limited in comparison to urban medicine. Typically when someone from my hometown area gets very sick, or critically injured they initially go to our hospital in Kankakee. However on a couple occasions patients need to be transferred to Chicago land hospitals, sometimes this happens in an urgent life/death situation. After completing this program I’m becoming more interested in what protocol is taken for this transfer, because I never really questioned in before. There have been occasions in which people get into car accidents on country roads and they are air lifted immediately from the crash site; whereas other times patients are brought to Kankakee hospitals first and accessed. Another problem dealing with car accidents, is sometimes the ambulance drivers cannot find the exact location of the crash scene because there are not landmarks or intersections the caller can describe to the responder. Time is so valuable during these times, and wasted time finding the crash site is just added time that could ultimately be the deciding factor if this patient lives or dies. I personally believe a lot of innovation can happen in rural medicine, and I think after completing this program this is something I would like to look more into moving forward. Someone should not receive lower quality in health care because the area is smaller in numbers.
Michael Rooney Heading link

I am a rising second year medical student at the University of Illinois College of Medicine in Chicago. Unlike many other members in the Innovation Medicine group here at UIC, I do not have a formal background in engineering. Rather, I studied biological sciences and physiology during my undergraduate years, andI hope this can allow me to bring a unique perspective to the group. At this point in time, I envision myself pursuing a career in radiation oncology and I hope to get involved academically as my career continues. I not only am interested in direct patient care but also the development of efficient technology and academic research in the realm of oncological treatment outcomes. I hope that my experience in IMED and the summer immersion program can provide me with a foundation to make large scale contributions in this field during my years in medical school and beyond.
Michael Rooney Blog Heading link
-
Michael Rooney Blog
Blog Entry 1- Orthopedics Week One
Michael Rooney Blog

This is the very first week of the clinical immersion program and, to be honest, I was not quite sure what to expect from my first rotation in orthopedics. Overall, I have been quite pleased with the progress we have made as a group and I am excited to get more feedback from the UIC orthopedics staff moving forward. I believe we have found some interesting issues in the clinic that may very well lead to concrete projects in the future.
More specifically, our time spent in the first week has been almost entirely in the orthopedics clinic with various attending physicians and residents. In my first day of the rotation, I worked with staff under Dr. Matthew Marcus. My original focus as an immersion student with Dr. Marcus was to focus on procedural issues in the physician-patient interaction itself. I observed a few visits and unfortunately felt discouraged because most of the time spent in the visit was simply conducting a patient history. It felt like there was little room for innovative thinking in this space and I truthfully became a little discouraged by the end of the first day. I discussed this feeling with other members of my team and overall it seemed that this was a shared sentiment.
However, the second day in the clinic proved to be an entirely different situation, as we spent time with physician Dr. Mejia. Right away, I was very impressed with his demeanor and ability to concretely articulate ideas and communicate with residents and students alike. The day really became exciting when another member of my group, Zaid, noticed a small bag of magnetic characters (numbers and letters) that were sitting at the nurses station. He asked a nurse on staff what those magnets were used for and she explained that Dr. Meija had developed a system for himself to maximize efficiency of patient flow. He would use the magnets as signals to tell him which patients should be seen in which order and also provide basic information about that patient. For example, if the patient is second to be seen and needs an operation, Dr. Mejia places a magnetic “O” and “2” on the door of the room. He then has to manually update the system after each patient interaction by replacing all of the magnets on the doors.
Right away, the members of my group were intrigued by this system. The simple fact that a physician felt compelled enough to develop such a process indicated to us that there was likely an underlying process issue that needed to be addressed. We approached Dr. Mejia about his system and he was very receptive and excited to work with us and potentially find means of improvement. He shared with us briefly his thoughts about what flaws exist in the patient flow of the UIC clinic and encouraged us to think critically about how he can get involved.
At this point, we have only just begun our discussion with Dr. Mejia but we have planned to meet more in the future to discuss the possibility of more actively tacking this systemic problem. I personally am very excited by this prospect and feel as though my group could very well be on track to improve efficiency in that clinic.
Orthopedics 2
Michael Rooney Blog
Not much has changed since my last post so I will keep this one short. I begin the second week of rotation tomorrow after a morning meeting with my team and the rest of the immersion group in the innovation center. I am excited to share our first week experience with the other students and am eager to hear about their perspective as well. This formal meeting time should be very beneficial for our group as we not only get more time to discuss our goals for the rest of the rotation but also hear from Dr. Kotche about her advice moving forward.
The next two weeks of rotation in the orthopedics department should be very interesting, as we are formally assigned to work under Dr. Gonzalez who was out of the clinic last week. I think it will be very beneficial for our group to have consistency of attending physicians so that we can make longitudinal observations. Hopefully, Dr. Gonzalez will be as open to discussion as Dr. Mejia was last week so we can continue our conversations about work efficiency in the clinic.
Along those lines, I am perhaps most eager to continue our work with Dr. Mejia from last week. He seemed very excited to get involved with our program and recognized a major need for improvement in the process design of his clinic. We as a group have reached out to him this weekend with the hope of sitting down for a brief meeting outside of the clinic. A more formalized meeting with Dr. Mejia could lay a great foundation for our ideas moving forward. This week could prove to be very productive for our team and I look forward to getting started!
Orthopedics Week 2- Looking Back
Michael Rooney Blog

Unfortunately, this week has been quite busy so it has been awhile since my last post. However, my time in the orthopedics department, despite the long hours, was quite exciting. Our team spent most of the week with Dr. Gonzalez who is the head of the department here at UIC. I really enjoyed the longitudinal experience of working with the same attending throughout the week. Unlike the first week of the rotation where we worked with a different attending every day, our experience with Dr. Gonzalez provided much needed continuity for the rotation. We were able to get a better picture of what his life is like everyday and have more in-depth discussions about the types of obstacles he faces as an orthopedic surgeon.
Throughout the week we spent some time in the clinic with Dr. Gonzalez who is extremely efficient with patient flow. He sees upwards of 60 patients in a single day and, despite a few hiccups with scheduling, seems to maintain a steady pace throughout the session. Unlike Dr. Mejia who uses the magnet system for managing his schedule, Dr. Gonzalez relies solely on the traditional system to guide his progress. We spoke with a few attendings about the necessity of a new system (e.g. magnets, etc) to manage flow and received very different feedback. Some attendings do believe that formalized orders can increase efficiency but others feel comfortable without any external guidance. For me personally this was a bit disheartening because during our first week we spent so much of our efforts focusing on this issue as a potential space for innovation.
On Tuesday, we had quite a different experience because rather than going to the UIC clinic we spent the day with Dr. Gonzalez at the Illinois Bone and Joint Institute on Michigan Ave. This clinic time was so different than UIC mainly due to a huge decrease in patient volume. Dr. Gonzalez only saw a total of 15 patients throughout the day, which paled in comparison to his 60-70 at UIC. Since he was not as rushed with seeing patients, Dr. Gonzalez was able to not only spend more time with each patient but also spent time with us discussing our experience thus far. He comes from an engineering background himself so he was very excited to share his perspectives regarding the role of engineering in orthopedics. He showed us some of his own work in the field and discussed the possibility of innovation in that sector. Furthermore, he even described some of his own patents for medical devices that are useful in surgery. Overall, I was extremely pleased with my experience in the private clinic and am looking forward to spending more time at IBJI in the coming week.
The most exciting part of the week for me was Thursday where we spent all day in the OR observing as Dr. Gonzalez performed a number of operations. We were lucky enough to witness two total knee replacements and a total hip replacement which were extremely intriguing, especially since I may want to pursue orthopedics as a career choice down the line. Although I was quite ignorant as to the details of these procedures, I did try to maintain a critical eye throughout the day, focusing on details of the procedures which seemed inefficient. At the end of the day, we were able to discuss some of our ideas with Dr. Gonzalez, who was more than open to hearing our thoughts. We had written down a few ideas, such as concerns about guidance of drills through bones, and to each question Dr. Gonzalez was quick to respond with references to literature about how our questions had already been addressed professionally. This was not discouraging, however, because he seems to really support our enthusiasm in the OR and wants us to succeed as students. We have decided to do some academic reading before our next day in the OR so we can have a more educated perspective coming in. He will be performing a number of carpal tunnel surgeries so we will try to focus on this procedure in particular. Hopefully this will lead to further questions and we can start finding real issues to potentially address with the team. I definitely have high hopes for the week to come and think that our work with Dr. Gonzalez will certainly be beneficial.
Orthopedics Week 3 Part 1
Michael Rooney Blog
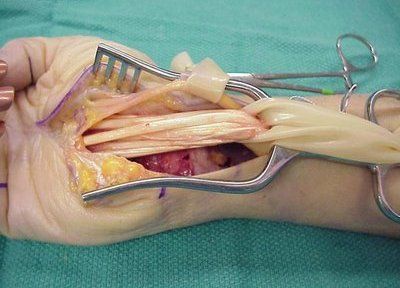
Unfortunately, this is already the start of my final week with the orthopedics department and as expected the time has flown by. I still feel as though I am just getting acquainted with some of the staff members in the clinic and am very appreciative of the time I have had thus far. Nonetheless, I do have high hopes for the remaining days in this rotation and hope that we can continue working with Dr. Gonzalez to find real time problems in the clinic and operating room. I feel as though I have not only learned a great deal about the clinical aspects of orthopedics but have also grown significantly as a critical thinker and innovator. I have a newfound appreciation for the process of needs assessment and will carry this experience forward through my career.
Today, we worked with Dr. Gonzalez in the Illinois Bone and Joint Institute just as we did last Tuesday. Unfortunately, today had a slightly higher patient load compared to last week so we had more limited face-to-face time with the doctor throughout the day. I did, however, get the chance to discuss some of my ideas with Dr. Gonzalez about upcoming surgeries I will be observing on Thursday at UIH. In particular, I noticed Dr. Gonzalez would be performing a number of carpal tunnel procedures this week so I decided to do some journal reading regarding biomechanics of the carpal tunnel during this survey. I found a huge array of articles pertaining to this procedure and focused on a few which I thought were specific and targeted with the potential for innovative ideas.
In particular, I noticed that the current carpal tunnel release procedure results in complete destruction of the transverse carpal ligament which runs laterally across the wrist. The proposed physiological role of this ligament is to not only provide protection of nerves and tendons below, but also push the ligament closer to the bones of the fingers. In this way, it is acting as a pulley to prevent bowstringing of the tendons when the wrist is flexed. Intuitively, I imagined that cutting of this ligament during surgery would result in decreased range of motion at the wrist, so I asked Dr. Gonzalez about whether patients had complained of this problem after the procedure. Unfortunately, this never seems to be an issue for patients and studies on cadaver wrists have not shown significant changes in physiological range of motion. Zaid, another member of my team, asked other questions as well and Dr. Gonzalez was quick to respond with references to literature about what type of work had already been conducted which addressed our concerns.
It is very easy to view this experience as a letdown, as none of our ideas regarding the surgery seemed to be real problems in the clinical realm. However, I view it as a learning process and a chance to practice my abilities of questioning and maintaining a critical perspective during observation. I am confident that if I continue honing this skill, I will become more capable of making contributions in the future as a physician and innovator.
Orthopedics Week 3 Final Days
Michael Rooney Blog
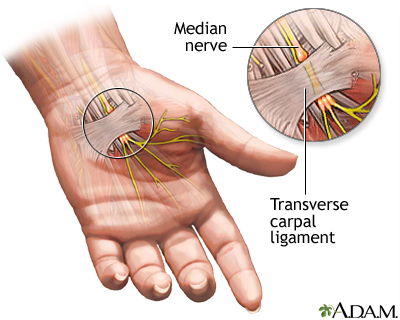
These last 3 weeks in the orthopedics department have flown by and unfortunately it is already time to shift gears. I am very thankful to the staff at UIC and IBJI for allowing us to spend time in the clinic and operating room. As a group, I think we learned a great deal not only about how orthopedic clinics are run but also about the process of thinking like an innovator. This experience has been invaluable to me as a student and I am confident that I am more prepared to approach problems in the future.
On Thursday of this week, we were fortunate enough to spend another day with Dr. Gonzalez in the OR. We watched a number of procedures and were able to discuss with the doctors potential issues during the procedures. Dr. Gonzalez was especially helpful in showing us the details of the surgeries and explaining the biomechanics involved in each step. One case which I found particularly interesting was the carpal tunnel procedure. Hand movements themselves are extremely complex given the large number of muscles and bones involved in coordinating precise actions. Carpal tunnel syndrome is associated with increased pressure in the tunnel connecting the wrist to the hand. In order to compensate, surgical cutting of the transverse carpal ligament can increase the area of the tunnel. This relieves the pressure on the contents of the tunnel, hopefully leading to resolution of symptoms.
Intuitively, I would imagine this procedure would cause major limitations in hand movements, especially when the wrist is flexed. However, based upon Dr. Gonzalez’s vast experience in the field, he rarely receives complaints by patients following carpal tunnel syndrome. There seems to have been little work done comparing grip strength in flexion following the surgery. Zaid and I discussed this issue and are hopeful to conduct some clinical outcomes or cadaver research in future to get a more precise picture of how carpal tunnel surgery affects hand function.
Overall, I was very pleased with my experience in the orthopedic department and am looking forward to starting in the oncology department for the remainder of the program.
Oncology Week 1- Looking Back
Michael Rooney Blog

This week we were assigned different teams in a new department for a second 3 week rotation. Fortunately, I was matched into my top choice of hematology/oncology which is a field am interested in both clinically and academically. I envision myself pursing a career in radiation oncology and I hope that this program can give me a unique perspective about needs assessment and innovation in that workspace.
We have been working primarily with two attending physicians, Dr. Howard and Dr. Koshy, and their respective residents in the department. Every staff member has been very open to discussions with us and has provided insights about clinical knowledge and needs in the field. I am very grateful for the time and effort they have invested in our experience and I am confident that our team will continue to learn as the rotation continues.
Compared to my first rotation in orthopedics, this week has been much less hectic and has allowed for more time of reflection. I think this is simply a result of the nature of the specialty rather than a specific trait of UIC clinic in particular. Radiation Oncology has a significantly smaller overall patient volume and each case is quite complex taking longer time. Furthermore, every case is a collaboration between multiple oncological teams, including surgery, medicine, and radiation. Integration of these therapies is necessary for optimal outcomes for patients. However, this complexity also comes with a price. Communication becomes increasingly important as the level of integration increases so any errors in communication can be extremely detrimental to patients.
Throughout the week, the observations I was most excited about involved patient immobilization techniques during external beam therapy. In short, during therapy a patient must be in precisely the same position for the radiation beams to be accurately targeting the tumor and not normal tissue. Currently, there are a number of devices which are used to this end and at UIC I believe the most common method is a casting system. During the planning stage of treatment, the patients are asked to undergo a simulation, where they lay down on a casting material. The material expands and hardens over the course of about 10 minutes so that it creates a mold of the patients body. Thus, each time they come back they can lay down in that mold and reproduce the body position from the previous treatment. The casts are indeed quite cost efficient as they are made of relatively inexpensive materials. However, they do require storage in between uses and ultimately disposal at the conclusion of therapy. Furthermore, in pediatric cases, general anesthetic is used to prevent patient movement during the treatment. This seemed not only very expensive for the hospital given the cost of medications but also very extreme for the patients and parents. I imagine that most parents would not enjoying having their child receiving anesthetic on a consistent basis. I discussed this issue with one of the residents at length, and he ultimately had the view that this is the best solution to the problem, given other alternatives such as forced immobilization which would be traumatic for the child. At this point, I do not see a simple solution to maximizing efficiency of immobilization but I am excited to pursue these issues moving forward. Perhaps this area could be a longitudinal project for my career in medical school and beyond.
Oncology Week 1- Looking Forward
Michael Rooney Blog

Unfortunately, our time scheduled in the radiation oncology department has come to a close and we are now beginning with a new experience in the hematology/oncology department. While I am extremely interested in the clinical and engineering problems of radiation, I am looking forward to beginning a new chapter this week. I expect that the pace of the clinics will be quite different from that of radiation and that the patient volume per day will be large. This should allow us to stay busy throughout the rest of the rotation and observe a large variety of patients and procedures.
Admittedly, I am quite ignorant about the details of hematology and medical oncology so I am glad to have a chance to work in this department. Hopefully the staff will have time and be receptive to questions about how hematologic disease and cancer are handled medically. I imagine that there are a huge variety of treatments available to tackle these devastating diseases and I hope that as a team we can begin to scratch the surface regarding any potentials spaces for innovation. As we have discussed in our open classes, I think that sometimes ignorance in a field can be very beneficial for the success of the team as we are not limited by biases of experience. We have not been trained to do things in a certain way so it may be easier for us as outsiders to recognize problems that may not be so easy for regular staff to appreciate. Taking advantage of this perspective should be beneficial for our group as we prepare observations and ultimately deliver assessments about possible inefficiencies in the clinic.
This week I am most looking forward to working with the medical oncology team since I have an interest in pursuing a career in oncology down the road. I am not only fascinated by the physiology of tumor dynamics but also recognize the clear importance of cancer management in our society today. There are huge efforts being made across the globe to create better cancer outcomes and perhaps we as a team can begin to contribute to the conversation. Given this knowledge it is important to have unrealistic expectations about our experience in the coming weeks. We almost certainly will not make a groundbreaking change in cancer care but that does not mean our efforts are not important. Rather, as long as we can keep the scope of our observations within reasonable limits, I am confident that we may indeed be able to make a positive impact on the delivery of care. I am looking forward to beginning that process tomorrow afternoon!
Oncology Week 2 – Looking Back
Michael Rooney Blog

My second week in hematology/oncology was definitely a major shift from the first week spent solely in radiation oncology. On Monday we met with Dr. Rondelli who was extremely helpful in explaining the basic science of medical oncology and bone marrow transplants. This knowledge would prove to be very important as we continued throughout the week and observed in the clinical arena. He also discussed with us some of experiences of past students in the program and explained which areas he felt would be interesting to us from an innovation standpoint. Overall, I think our group was very thankful for this initial meeting because it laid a strong foundation for the rest of the week and helped us be more prepared as we observed.
On Tuesday we spent some time in the stem cell lab and blood bank to get some insight into how blood marrow transplants are prepared. This part of the immersion experience was particularly interesting to me due to my interest not only in the basic physiology of the immune system but also due to the level of complexity of preparation from an engineering perspective. Blood samples are processed in a very careful and reproducible way involving not only human handling but also complex machinery designed to extract particular blood components. One example which I thought was quite impressive is a machine designed to use monoclonal antibodies which bind CD34 (a cell surface receptor) to extract only stem cells from a patients blood sample.
Our next stop on the hematology/oncology rotation was with rounding with Dr. Quigley at the clinic. Personally, this part of the experience was not my favorite, mostly due to my own ignorance of the clinical scenarios playing out in front of me. I am not familiar with most medical protocols for treating cancers or hematological diseases so most of the discussions between Dr. Quigley and residents were over my head. Furthermore, with all 4 members of our team rounding, the rooms quickly became packed with residents and students so it was hard for us to observe most of the interaction. This is not the fault of the medical staff but was simply unfortunate for our team of students. Overall, I think it was definitely a valuable experience clinically but from an innovation standpoint it was quite difficult.
On Thursday, we spent the morning with Dr. Rondelli in his clinic and in the Infusion Area of the Outpatient Care Center. This experience was definitely good for clinical needs assessment because there were many patients and a vast number of blood pumps being used to administer chemotherapy. One issue that jumped out to us right away was the troublesome scheduling as we have seen in many departments throughout this experience. The charge nurse was responsible for manually assigning patients to rooms at times throughout the day, trying to accommodate for specific patient characteristics. For example, she tries to match male patients with other male patients in the same room and keep certain immunocompromised patients in their own rooms. At times theses accommodations make her job quite difficult as she must weigh certain preferences over others. Furthermore, the entire system is done by paper and pencil, with her copying information from the computer check-in and scribbling down names as the situation changes. At the end of the day, her schedule is marked with eraser shavings and red arrows indicating last minute changes to patient rooms. We imagine that this scheduling system could easily be improved and would drastically improve the efficiency of the clinic.
At the end of the week, we actually decided to spend more time back in the radiation oncology department because overall our team felt more productive in that space. The patient load is much lower so we have more time to discuss with residents and physicians the problems they see on a daily basis. I expect that we will continue to spend time in this clinic in the coming week and am excited to continue where we left off last time.
Oncology Final Week – Looking Ahead
Michael Rooney Blog

This program has flown by thus far and unfortunately we are already entering the last week of our second rotation. I have enjoyed my time in both the orthopedics and oncology departments and am looking forward to continuing in this final week. I think my group has been successful in our goal of assessing clinical needs and ultimately have found some issues that can we can work on in the months and years to come.
For my last week, I hope to spend some more time in the radiation oncology department to further observe any apparent clinical needs. I think that my interest in the field helps me be creative in my thinking and will allow me to be passionate as I move forward to tackle some of the problems I encounter. As of right now, I think the area of radiation oncology that I think can be improved most easily is the immobilization techniques for patient simulations and external beam therapies. When I discussed this issue with the residents of the department, they seemed to be under the impression that the casting system for abdominal and lung cases had “acceptable” outcomes so there was really no need for innovation especially given the low cost of production. To me, this response felt like it was a result of biases from being in the field for a long time. These immobilization devices have been in place for as long as the residents have been practicing so it may be difficult for them to imagine anything else being viable. I hope to continue discussing this issue with the staff next week because I personally am very excited about getting involved in this innovative space during my time as an IMED student.
Another area I hope to get more exposure to in the coming weeks is the various tools used for administering brachytherapy safely. We have only seen one brachytherapy procedure conducted for cervical cancer which involved some primitive tools such as stacked towels used to minimize radiation exposure to the patients’ legs. Similarly, we have seen a few patients with ocular melanoma which require brachytherapy administration via surgical implantation of a radioactive plaque directly onto the tumor of the retina. Unfortunately, we have never been able to actually watch that procedure in the OR so hopefully this week we will be able to get that experience. Ocular melanoma is an extremely rare condition but UIC/UChicago actually has a fair number of these patients given their experience in the treating the disease. I imagine that there may be a space for innovation in this space due to the required coordination between the radiation and surgical team. Furthermore, there are some fairly limiting side effects of treatment such as permanent vision loss and potential extreme eye pain that may lead to eventual removal of the eyeball itself. Any method to minimize undesired radiation exposure to peripheral tissues would certainly reduce these devastating effects.
While we unfortunately only have a few days left in the program, I am excited to continue my experience with radiation oncology and am hopeful for some interesting findings the days to come!
Nina Scalise Heading link

I am a second year medical student from Chicago. I have an undergraduate degree in Biomedical Engineering from Northwestern University, where I participated in several team-based design projects that addressed physician and patient needs. Before starting medical school, I worked in clinical research for an orthopedic surgeon with a focus on the use of stem cells for cartilage repair and regeneration in the knee. I look forward to incorporating the practice of interdisciplinary problem solving and design into my medical school training through the IMED program.
Nina Scalise Blog Heading link
-
Nina Scalise Blog
Week 1 Part 1: Intro to Ophthalmology
Nina Scalise Blog

“What you see is what you get.”
Our team’s introduction to Ophthalmology at the U of I Eye and Ear Infirmary on Tuesday 7/5 began with this quote from our physician supervisor. Earlier in the day, we were introduced to our teammates and discussed our motivations for being in the clinical immersion program and goals moving into the first rotation. I was excited about starting in ophthalmology because of the prevalence of advanced technology in imaging, biomaterials, and surgical techniques.
Our supervising attending is a cornea specialist, and also has an active role in training residents – our first day in the rotation also corresponded to the first day for the new class of residents. The attending educated our team on basic principles of optics including visual acuity, field, and stereopsis, as well as various examination diagnostic instruments from the basic slit lamp to optical coherence tomography (OCT) and fluorescein angiography. He also highlighted issues such as the continued dependence on paper charts due to limitations in ophtho EHR software, and the tradeoffs between resolution and intensity among the various imaging modalities. “What you see is what you get” is particularly relevant in ophthalmology since the eye is the only place in the body in which blood vessels can be directly viewed using non-invasive techniques such as via the slit lamp or OCT.
7/6/16: Slit Lamp Demo Retina Clinic
Our team attended the morning slit lamp training for residents led by our supervising attending. This device is the primary illumination device used in the standard eye exam (see attached photos). During the training, the attending demonstrated some of the following shortcomings of the device to our team:
- Providers often “overcrank” the light source knob when they first turn on the lamp, and this can contribute to a blown fuse — it is actually rarely necessary to move beyond the first brightness setting but many of the docs have become accustomed to this
- When the provider grabs the slit lamp table to slide it toward the patient to begin the exam, the plugs attached to the base of the table are often accidentally pulled out since they are in an inconvenient location
- The lamp itself moves on a series of pins, and over time the track becomes stiff and difficult to maneuver smoothly with the joystick
- Within the illumination tower, there is a small metal disc that is in contact with a light bulb — the gradual oxidation of the disc can contribute to the failure of the light source, which can be prevented by scraping the oxidation residue from the disc
- Adjusting the height of the slit lamp is especially difficult for very short or wheelchair bound patients. The current workaround is a portable slit lamp (see attached), which has existed for ~20 years, but doesn’t have a chin rest, so it is necessary to manually stabilize the head with one hand and control the device with the other hand
Our team then had a chance to adjust the slit lamp and “examine” each other to get a sense of the coordination required to control the various elements of the machine. Some machines also have a side viewing scope for teaching purposes. The attending also made a point of how prevalent cervical disc disease and neck/back pain are among ophthalmologists due to the postural strain associated with the exam, especially holding the condensing lenses up to the patient’s eye to visualize the retina.
In the retina department, I followed an attending through her extremely busy clinic day that included office visits, anti VEGF (vascular endothelial growth factor) injections, and laser treatments. This clinic also utilized primarily paper charts. A few interesting observations from retina clinic are as follows:
- During the anti-VEGF eye injections, I was instructed not to breathe on or near the patient to maintain sterility. The physician had a tech assistant who would prepare the injection materials and cover his/her mouth while giving the patient instructions. The injection process only lasts a few minutes, but I wondered later if there was a reason masks were not used to maintain sterility
- The retina attending reiterated what our clinical advisor expressed about neck back strain from years of performing the exam. The strain is even more severe for retina specialists who have to manually hold fundus lenses up to the patient’s eye while seated and looking though the slit lamp.
- A few thoughts on improving this are possibly creating a stand or attachment for the fundus lenses that could be adjusted either on the slit lamp itself or on the headset that doctors use to examine the back of the eye.
Week 1 Part 2: Surgery Contact clinic
Nina Scalise Blog
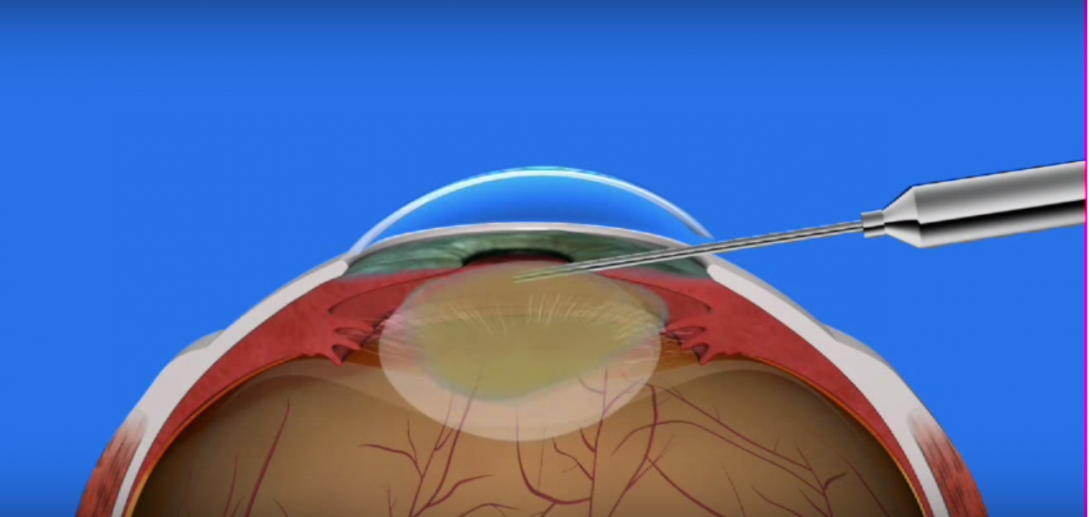
7/7/16: Cornea Surgery
On Thursday, our team observed one of the cornea attendings in the OR at UIH. The majority of his cases that day were cataract surgeries, and we also observed a partial cornea transplant. The attending and assisting resident or fellow are seated at microscopes for the duration of the procedure, and the cataract procedures were especially streamlined, lasting 15 minutes or less. During a cataract surgery that does not use laser, an ultrasound instrument is inserted into an incision in the limbus (the border of the cornea and sclera), and breaks up the center of the cloudy lens (which contributes to the vision impairment). After the cloudy lens is suctioned out, the surgeon replaces it with a prosthetic intraocular lens (IOL) typically made of plastic or acrylic that becomes a permanent part of the eye. From an outside perspective, the procedure itself seemed extremely efficient, especially when performed by an experienced surgeon. A few additional observations:
- The instrument that is inserted into the limbus at a slight angle to the horizontal has a straight tip, which doesn’t provide much mechanical advantage for suctioning, etc — our group speculated about the potential benefits of a curved tip instrument
- One cataract case necessitated a 3 part IOL since the diameter of the patient’s eye exceeded what is considered “normal range” of up to 24 mm.
- The tower that provides suction and ultrasound must be wheeled as close to the surgical field as possible, and the cords that extended back from the machine could have posed a hazard for the scrub nurse/tech to move back and forth if necessary
- During cataract surgery, the patient is usually under “twilight” sedation and is able to respond to questions/commands — some patients respond well when told to keep their eye focussed directly on the light above and others have more difficulty and their gaze drifts off center, which can contribute to longer surgical times
The partial cornea transplant involved isolating the endothelial cell layer (single cell layer important in keeping the cornea clear) from a donor cornea and suturing it into place in the recipient’s eye. This procedure required a separate small worktable adjacent to the surgical field where the surgeon prepared the donor graft. It is essential to have this area close to the patient for efficient transport of the donor cornea.
7/8/16: Contact lens clinic
I was able to observe several patient office visits in the contact clinic; all of the patients I observed wore RGP (rigid gas permeable) contact lenses as opposed to the soft lenses I was familiar with. I learned that the rigid lenses are beneficial especially for patients with corneal pathologies since they provide superior vision quality, O2 permeability, and less microbial keratinitis, with the major drawback being comfortability of the lenses. One interesting case was a patient with scleral lenses, which cover the whites of the eyes and are used for patients with corneal issues such as keratoconus (a bulging out of the cornea). The way to insert a scleral lens involves the patient bending forward with eyes looking down, filling the lens with sterile saline solution, and using a plunger to insert the contact (see attached). This method is standard for this type of contact but seemed burdensome for the patient and physician.
In addition, for patients with corneal pathology, contact lens fitting is often a more challenging process and requires trial and error with lenses of varying size and curvature. I was able to observe a patient whose contacts fit too tight around the edges, and this was evident from the more prominent, bulging vasculature around the edges of the lens. I wondered whether preliminary topographic imaging for such patients would reduce the trial and error component to the contact fitting process, or if this was simply not feasible or cost effective.
Week 2 Part 1: Cornea Clinic and Glaucoma Clinic
Nina Scalise Blog
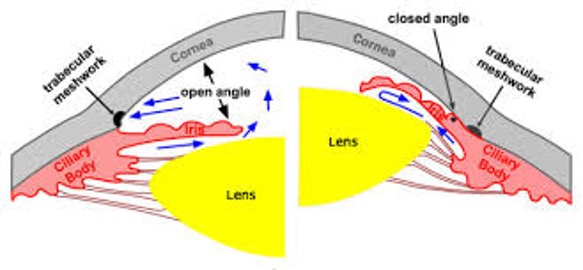
7/11/16: Team Debrief Cornea Clinic
We started the second week with a team debriefing session and talk from Dr. Neiderberger of urology on needs assessment and problem identification. He discussed the importance of identifying a problem that is simple yet impacful, and also talked about a mental exercise called ‘subtraction’ where you remove the essential piece of a device or system and re-imagine how it can be done. We also discussed the deliverables for the end of the rotation and how the presentation and report should revolve around one high level theme — for ophthalmology, I see ergonomics and comfortability during routine examinations as a primary theme that recurs in several of the subspecialties I have observed.
I spent the afternoon in the cornea clinic observing routine office visits with our clinical mentor. As was mentioned in a previous post, it is especially difficult to examine patients with kyphoscoliosis using the slit lamp and I observed in clinic how it was difficult for such a patient to lift his head for the exam. In addition to patient comfort issues, I noticed the majority of rolling chairs in the cornea exam rooms lack any back support, which could contribute to strain for the provider. My attending dealt with a variety of cases including severe astigmatism, diplopia (double vision), and pemphagoid (an autoimmune condition affecting the extra cellular matrix of tissues such as the cornea).
7/12/16: Glaucoma clinic
On the glaucoma service, the metric of highest importance is the intraocular pressure (IOP), measured in clinic by a technique called tonometry, where a tip with a mini pressure sensor is applied to the center of the cornea. For patients with advanced glaucoma, the target pressure is < 18 mm Hg, while for mild-moderate glaucoma, the target pressure is in the mid teens. The primary method of treatment that I observed was a regimen of different eye drops thats providers often referred to in terms of the color of the bottle cap: “purple top”, “orange top”, etc. I would often hear that a patient was “maxed out” on drops, meaning they were on the maximum combination that could be safely prescribed. My attending noted that patient compliance with the drop regimen can be low especially among elderly patients. I did not see any new patients in clinic that day, but I wondered if there was any form of educational materials given to patients besides the instructions on the prescription bottle. The dosage/frequency of the drops is often adjusted at office visits and confirmed with patients verbally; I imagined a possible solution to this where providers could give patients a pre-printed template sheets with colored circles and designate the frequency of each drop below the circle. Additional observations from the glaucoma clinic:
- I saw a couple cases of “narrow angle glaucoma”, the less common form of the disease in which the angle between the iris and cornea (iridocorneal angle) is smaller than normal (see attached photo). This angle was assessed in clinic using a Zeiss indirect goniolens that employs 4 symmetrical prisms that visualize the angle in 4 quadrants of the eye. The goniolens is slowly applied to the surface of the eye, forming suction, and is often used simultaneously with the slit lamp for visualization.
- Narrow angle glaucoma is particularly dangerous because the drainage angle of the eye can be blocked resulting in an accumulation of fluid, spike in intraocular pressure, and damage to the optic nerve. Pupil dilation presents an increased risk for such patients to have an acute angle attack, and it is therefore critical that pupil dilation in the clinic is either avoided or done with extreme care for these patients.
- For patients with narrow angles, a procedure called laser peripheral iridotomy (LPI) is recommended, where a hole is “punched” in the iris to allow an alternate vent for fluid to drain from posterior to anterior in the eye. It was stressed that this procedure would not completely eliminate the chance of an acute angle closure attack, but rather is a preventive measure.
Week 2 Part 2: Peds Clinic surgery
Nina Scalise Blog
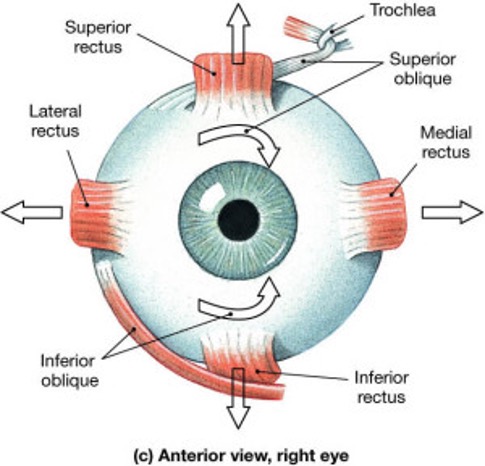
7/13/16 7/14/16: Peds Ophtho Clinic Surgery
Our day in the pediatric ophthalmology clinic revealed new methods of delivering care as well as new challenges. Most of the younger children are too small to use the autorefractor that determines a patient’s refractive error for glasses/contacts, so a direct retinoscope must be used. Children who are also too small to be examined using the standard slit lamps are examined with a portable one. The limitation of a portable slit lamp is that you can’t do a fundus/posterior eye exam and it is sometimes necessary to stabilize the patient’s head with one hand if they are unable to sit still. In addition, the majority of patient families we saw needed some degree of translation to fully understand the extent of their child’s condition; rather than calling dedicated translators, the surgery scheduler and techs were often called into the rooms to translate for families.
The attending we followed in peds was a strabismus specialist, who surgically and non-surgically manages the condition that prevents a patient from directing both eyes to fixate on the same point. One eye can deviate outward (exotropia) or inward (esotropia) and this can contribute to double vision or a condition called amblyopia (lazy eye). Babies born premature are especially at risk for high myopia and strabismus but usually progress to 20/20 vision by age 5. The typical treatment for strabismus is wearing glasses with a corrective prism that straightens the gaze of the deviated eye, and also techniques to stimulate the visual cortex in the brain. This usually involves patching the “good eye” for a few hours per day to force the patient to exercise the weaker eye. There were cases we observed in which the child tolerated the patching well and others where parents reported that their child would try to rip the patch off. The alternative in these cases is to use atropine drops in the good eye that will cause it to blur when focussing on a close object, forcing the patient to utilize the weaker eye.
If the strabismus is severe enough, surgery is used to relax or tighten the extraocular muscles (typically the lateral or medial rectus muscles). It is preferable to do this type of surgery before the patient reaches visual maturity, typically around 7-9 yrs old. Our team was able to observe part of a strabismus procedure in the OR, but the room was especially crowded with visiting physicians, residents and senior medical students. The surgery is extremely intricate and the duration is dependent on how many muscles need to be re-positioned. The measurements of how to adjust particular muscles are made one week prior to surgery, but we did not observe this being done that day. It can also be necessary to make fine adjustments to the muscles immediately following surgery in the recovery room utilizing adjustable sutures in order to ensure the gaze remains straight.
In the first case we observed, the attending was finishing the first eye and noted that she heard some gurgling coming from the patient. In a startling sequence of events, the patient’s pulse ox dropped and a code blue was called in the OR. The anesthesia attending and numerous other doctors flooded the room and we were confined to a corner and eventually left the room until the situation was under control. The patient was ultimately intubated and recovered from the incident which was thought to have been caused by secretions produced by the patient that temporarily blocked the airway. I have observed a significant number of surgeries and never witnessed a code being called in the OR; I initially felt a wave of panic and helplessness but appreciated the swift action of the team to address the problem and stabilize the patient.
We later observed a vitrectomy procedure for a retinal detachment. This involves removal of the vitreous humor (the fluid in the back of the eye) and replacement with either gas or silicone oil, followed by treatment of the retina with laser to flatten areas where it had become detached. Although this was a procedure we had not yet observed, my mind was still on the blur of activity surrounding the previous case and the state of that patient, who was a young child. Thankfully, we found out later the patient was able to finish the surgery after being intubated and monitored further.
Week 3 Part 1: General eye clinic surgery simulation
Nina Scalise Blog

7/19/16: General eye clinic oculoplastics
For the first half of the day I followed our clinical supervisor Dr. Sugar between his regular cornea clinic and the General Eye Clinic (GEC). The GEC is primarily run by the residents, but each patient must ultimately be examined and signed off by an attending.
At some point during the day there was a communication breakdown and Dr. Sugar was not called/paged when he was needed in the GEC and as a result, a couple of patients left after waiting for an extended period of time.
In oculoplastics, we met a team of engineers/scientists who were working on honeycomb shaped molds in which to deposit patient lacrimal cells in order to grow a lacrimal gland (tear gland) that could ultimately be reimplanted into a patient experiencing issues due to chronic dry eye.
7/20/16: Surgery simulation
Our team was able to practice surgical skills and techniques on the same equipment the residents use for training: the Eyesi surgical platform. Manual dexterity and depth perception are the essential skills that are tested using this simulation and our team greatly enjoyed being able to demo the various surgical modules (see attached image).
In the afternoon, we also observed a demo by a new language translation service that offers 24/7 video support from interpreters in 16 languages, and audio support for many more. The interface is a touch screen monitor on a rollable cart with an external speaker. It was unclear how many of these systems would be provided to the Eye and Ear Infirmary, and if this was a UIH system-wide overhaul. Our team has previously discussed and written about the inefficiency/lack of dependability of the current translator system, and how office staff were often used as temporary translators. This new system solves the issue of translator availability, since there are interpreters staffed in Chicago and Seattle.
Week 3 Part 2: Wrapping Up
Nina Scalise Blog

Our last days in ophthalmology were spent presenting our observations to Dr. Sugar and having a final debriefing with him about our experience in the department. We also spent a final day in the OR observing cornea and retina procedures. In particular, we were able to talk with Dr. Rosenblatt, a cornea specialist and the head of the ophthalmology department, who also has an engineering and business background. He shared with our team his views on the future of stem cells for corneal nerve regeneration, unifocal vs multifocal intraocular lenses (for cataract surgery), and the use of lasers in eye surgery for increased precision. He also touched on the burdens of the current EHR situation at the hospital and the importance of efficient access of patient records.
I enjoyed the rotation as a whole and feel that I learned a considerable amount about a field that most medical students don’t explore on a deeper level. I appreciated the exposure to the many subspecialties within ophthalmology, and gradually became more comfortable with my role as the weeks progressed. However, it was sometimes challenging to reconcile my roles as a medical student and as an outsider identifying problems; having limited training in medicine and engineering made it difficult at times to recognize if my insights were actually significant or if change could feasibly be implemented. Medicine and the technology behind it is constantly evolving, but adoption of change is a much more hesitant process, especially in the face of a limited budget and resources.
The process of observing in clinic was unique, since most of the providers I encountered were eager to explain any clinical findings and discuss where they see room for improvement in their practice or the field in general. Sometimes it was more difficult to communicate with the providers especially when they also had a fellow, residents, and other senior medical students on their service (such as in pediatrics and neuro). There were days when I played a mostly passive role so as not to interrupt the flow of clinic, but this was balanced by opportunities to observe procedures and ask questions between patients. The senior medical students and residents were also great resources throughout the rotation who would explain basic concepts or walk us through a surgery.
Week 4 Part 1: Intro to Radiation Oncology
Nina Scalise Blog
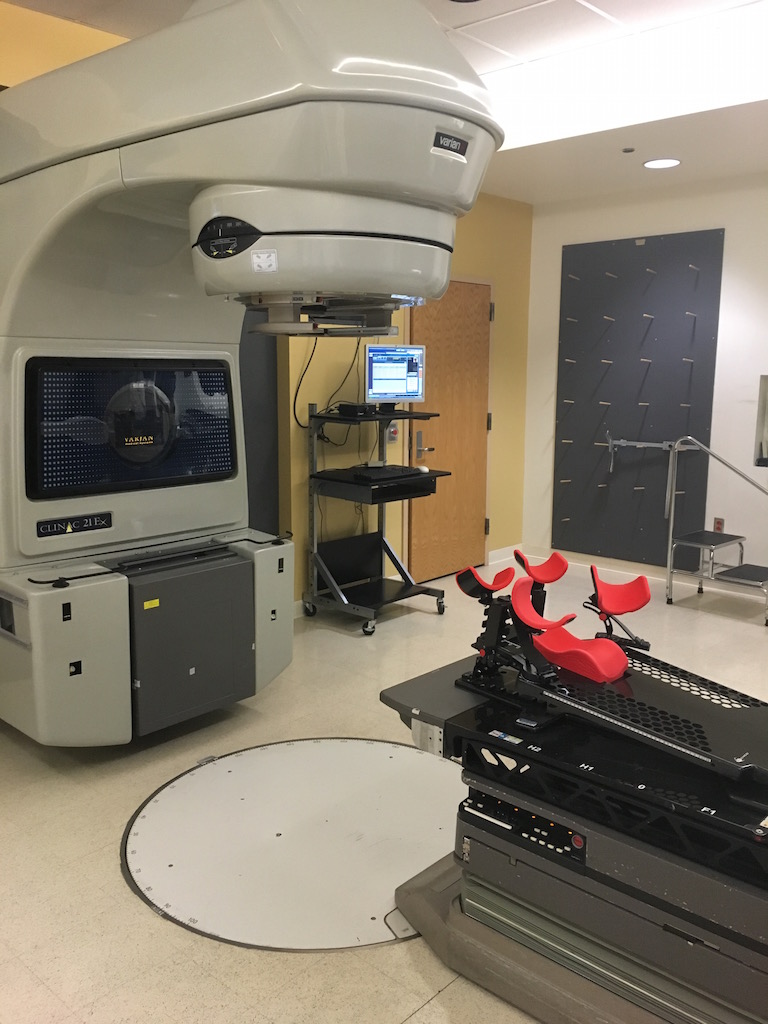
I was definitely excited to move on to our next rotation of the program and experience a new clinical environment and unique patient population in the oncology departments. I will miss the access to surgery that ophthalmology offered, since radiation hematology/oncology are clinic based, but there is definitely not a shortage of activity high-tech care delivery.
Our first week is spent in radiation oncology — the rad onc program at UIC is a joint residency between UIH and University of Chicago, so the residents spend 2-3 months out of the year seeing patients at UIC. I was immediately struck by the calm, quiet atmosphere of the rad onc clinic, especially when compared to the often hectic pace of the ophthalmology clinics. The volume of patients at the UIC rad onc clinic is typically lower than the UChicago clinic, so the appointments are generally not rushed and wait times are not a significant patient complaint. This also meant that I observed fewer patient encounters, but there was a certain gravity and sensitivity that surrounded the visits that was unlike what I had previously experienced.
We met the head of the radiation oncology department and the 3 residents, who were all extremely welcoming and eager to share the intricacies of their specialty with our team. Each attending has one “academic day” per week to catch up on academic duties such as grant writing or paperwork, so their resident has a more flexible schedule that day; we benefited from this, since the residents were often able to spend significant time explaining concepts to us such as tumor staging or the physics principles that go into making a radiation plan. Compared to other specialties I have experienced, the residents in rad onc are very academically oriented and well-versed in the literature of the field — we observed this during the weekly tumor board meetings in which oncology cases are discussed with a multidisciplinary team, and during “chart rounds” where the residents review their patients who are scheduled to start treatment that week and the indications for a particular plan.
When describing the aims of the clinical immersion program to the residents, they were generally interested in helping us recognize needs, but they also highlighted how radiation oncology has evolved even recently as a field to optimize care delivery. This includes the advancement of image guided radiation therapy (IGRT) to ensure that the patient is in as close a position to their original planning CT as possible so that the radiation is precisely delivered to the same location each time. Another example is the use of multi leaf columnator technology (MLC), in which metal “leaflets” interlock in a way that shapes the radiation beam as it exits the linear accelerator; this also allows targeted delivery of the radiation to a defined tumor area, and spares normal peripheral tissue. In response to the prospect of optimizing current practices, one of the residents offered a unique perspective that “perfection is the opposite of good enough”. He meant this in the sense that minor improvements often don’t amount to measurable outcome changes, so it is important to tackle a problem that has the potential to
A few additional notes/observations are as follows:
- When planning the radiation treatment margin, an advanced software is used to contour the tumor, and then buffer layers are added that surround the initial contour to account for molecular spread of disease as well as for minor patient movement during treatment.
- In order to ensure the patient remains in the same orientation for each treatment, they are placed in an immobilization “cast-like” structure that holds the head, limbs, etc in a certain fixed position that can be easily replicated. The department has carbon fiber immobilizers for breast cancer patients (shown in image), and these are lightweight, sturdy, and radiolucent (although expensive). For other cases, a large plastic garbage bag is filled with a mixture of compounds that produce an effect similar to wall insulation and the patient lies on it in the desired position until it hardens and forms an imprint of the patient. The immobilization molds are then labeled and stored on shelves for future use.
- Although the initial immobilization process appeared streamlined, it still struck me as “crude” to use bags with an inflatable compound and store them for each patient for the duration of their treatment
- Movement during radiation treatment (especially breathing for lung tumors) presents an issue for delivering consistent dosage. Motion tracking and motion compensation technologies are key innovations that address this, including Vision RT that images the patient and reports parameters in real time to gate the radiation.
- Pediatric patients can receive radiation as well, although it is generally not given under 3-4 years old. However, they usually must be anesthetized for each treatment, since keeping a constant still position each time is often too difficult for children. This surprised me, since although anesthesia has become safer it poses an additional risk as well as an additional cost associated with the treatment
Week 4 Part 2: Tumor Boards and Brachytherapy
Nina Scalise Blog

Our week in radiation oncology continued with multidisciplinary tumor board meetings, observing patient visits, and discussing treatment technologies with the residents and techs. Tumor boards are meetings in which oncologists, surgeons, pathologists, radiologists and more review cases and discuss treatment options for patients. Our first meeting was focussed on GU (genitourinary) cancers, with an emphasis on prostate cancer. In this particular meeting, attendings and residents were seated around a table with microscopes at each seat so they could easily view the pathology slides from patient biopsies. The radiologist would highlight key findings on CT or MRI and different surgical vs nonsurgical treatment plans were discussed among the various specialists; the images were also projected on a monitor so we could follow along. Later in the week we also attended a CNS (central nervous system) tumor board.
We also discussed the use of brachytherapy for cervical cancer, in which radioactive seeds are inserted into the tissue itself and a high dose of radiation therapy is delivered to the tumor. One of the residents demonstrated the use of a “tandem and ovoid fletcher suit set” (as pictured), where the central tandem component goes into the cervical os and measures the depth of the uterus, and the white ovoids are inserted into the vaginal fornices to further spread the radiation dose to the side of the cervix. Our team discussed a few of the following features and shortcomings of the device:
- There are two screwable “gear” pieces that hold the bars together in the preferred configuration and the bottom gear was consistently found to not tighten effectively
- In a certain position when the gears are tightened, a metal piece sticks out from the bottom gear and can rub against the inner thigh and cause discomfort. The current solution is to tape over the metal piece and bottom gear to provide stability and ensure greater comfort. The patient is generally under anesthesia when this device is being used to deliver radiation
- The rigid cylinder ovoid pieces come in different sizes and allow for precise positioning, durability, and easy sterilizability
- The bottom ends of the device connect to a machine that dispenses the radiation dose — the 3 prongs of the device are matched to the machine according to the number of engraved rings around the post (1,2, or 3). When they are not connected, there are light tan caps that cover the ends but are difficult to see and therefore easy to lose.
We also witnessed radiation treatments being delivered to patients. In one instance, the patient’s head had to be secured in a frame for brain treatments and because this patient’s planning CT was taken slightly off center, the patient had to be manually adjusted for the subsequent treatment in order to match the position of the original CT. X-rays are then taken directly by the machine and overlayed with the planning CT to confirm proper positioning. I asked if there was a way to input the degrees of shift and the machine would automatically adjust the patient without the technician having to go back into the room. This is actually possible with the current technology, but the technicians prefer to manually adjust the patient if necessary since if the machine auto-adjusts, there is a chance the table the patient is laying on will collide with the linear accelerator as it is rotating around to deliver the radiation.
We also witnessed a rare case of total body irradiation (TBI) for a patient with severe sickle cell anemia with recurrent vaso-occlusive pain crises. The point of radiating the whole body is to deplete the immune system in preparation for a stem cell transplant, which will provide the cells that will ultimately differentiate into functional blood cells. For the TBI the patient must spend half the time prone and half supine for an adequate distribution. Rice packs are also packed around the patient to create the illusion of a “rectangle” shape that facilitates uniform radiation distribution and also to partially spare sensitive areas such as the head and genitals.
Week 5 Part 1: Stem Cell Lab Hem/Onc Rounding
Nina Scalise Blog
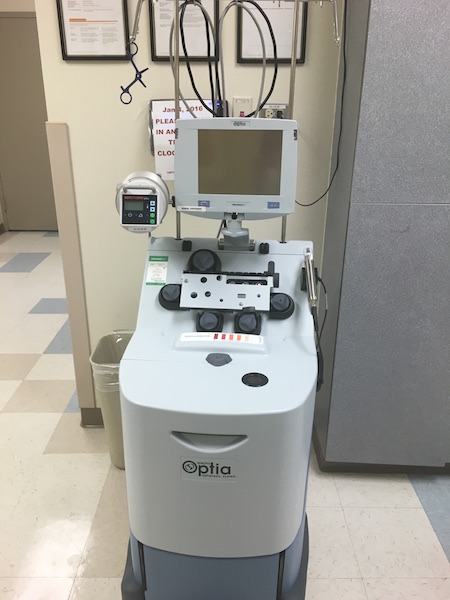
We began our second week in oncology with a tour of the hemotherapy center and stem cell labs. In the hemotherapy/hemaphoresis center, leukemia or multiple myeloma patients are given a drug to boost and mobilize their white blood cells, after which their blood is extracted, spun down in a centrifuge (see attached picture) and ultimately selected for CD34, which is a marker on hematopoietic stem cells (HSCs). A similar process can also be done for red blood cell and plasma exchanges as well. In the lab, the cells are frozen, initially at a controlled rate, and then stored in a freezer attached to a liquid nitrogen tank for 1-2 weeks, after which they are thawed and reinfused back into the patient. In general, an HSC transplant can be used for blood diseases, severe immune deficiencies, and sickle cell disease; the stem cells can be derived from bone marrow (usually extracted from the hip bone), peripheral blood (using the machine pictured), or umbilical cord blood. Transplants can also be autogenous (from one’s own cells) or allogenic (from a matched donor).
We were walked through all of the components and machinery involved in the stem cell processing and I was impressed at the extensive quality control measures built in to ensure consistency and viability of cells for the patient. For each sample, the reagents and patient plasma are saved and sent for sterility testing in order to pinpoint the source of contamination in the event a sample doesn’t pass sterility testing. The process itself from cell counting to freezing is highly protocol driven and has been optimized over the years; a few additional observations are as follows:
- All of the freezers are equipped with alarms that are triggered when the temperature falls out of a specified range and these alarms are linked to a central computer in the lab that produces an alert sound and then automatically calls lab staff members if it is not disarmed in a certain amount of time. Currently, the lab staff cannot disarm or control the system remotely and must physically come into lab to do so, although this does not happen often.
- For some of the machines such as the CliniMACS CD4 cell selector, the cell solution must be placed in a plastic disposable tubing kit that then fits into the machine — this preserves sterility but produces considerable waste and adds to cost. In addition, we were told the reagents for some of the cell processing machines can cost up to $4,000 and after so many years the company changes the reagents, forcing labs to upgrade the machinery.
- In addition to an automatic cell counter, the lab has a microscope connected to a monitor for manual cell counting, since the differential count is done manually for each collection. Manual cell counting is typically not a significant challenge for the techs, but with the current system they can only visualize a small range of cells – ideally, the range that is visible at one time would be larger to expedite the counting and reduce errors.
The following day, our team accompanied the hem/onc team as they rounded in the bone marrow transplant unit of UIH.
- The group consisted of an attending, junior and senior residents, fellows, clinical pharmacist, pharmacy students, and our team
- One resident wheeled around a portable computer workstation to refer to patient charts and everyone else had paper copies of patient info that the residents would alternate presenting before we entered the rooms
- Many patients on the floor were immunocompromised due to prior stem cell transplants and the list of relevant precautions (contact, gloves, etc) is visible on each patient’s door — some patients required that visitors wear disposable gowns, which are stacked in cabinets outside each room.
- Sometimes the residents noted holdups in obtaining patient records from outside hospitals and miscommunications during patient handoffs between shifts. On one occasion, a patient was given a dose of a very expensive drug by an overnight fellow because he was not aware of the plan made earlier by the team to administer a different (and much cheaper) drug.
- Generally lots of moving parts in the care of inpatient cancer patients, often requiring consults from nutrition, pharmacy, social work, etc. and ultimate management by the medical oncology team
Beny Romo Heading link

I am a senior in bioengineering at the University of Illinois at Chicago (UIC) with a concentration area of neural engineering. I will be taking part in the Gastroenterology/Hepatology and the Neurology rotations throughout the Clinical Immersion Internship.
Beny Romo Blog Heading link
-
Beny Romo Blog
Introductions of all kinds
Beny Romo Blog

The first day…WOW
Walking in to the Outpatient Care Center was definitely an adrenaline filled moment.
Not knowing exactly what to expect, tired from waking up waaayyy too early for the first time in months, and standing in front of the GI and Liver Clinic next to my partner, which I had only really just met earlier that day. It really gets your heart pumping.
Too bad that just a few moments after we enter the clinic my heart dropped to my stomach in a matter of seconds. After introducing ourselves to one of our listed primary contacts, she said the one thing that I absolutely did not want to hear. With a confused look on her face she let us know that she had no idea who we were, what this “Clinical Immersion” thing was, or what we were meant to do there. After a clearly needed much more detailed introduction and a bit of thinking. We figured out that the information that we were given was from the previous year. She then suggested that we pay a visit to a conference room next to the Endoscopy Lab.
More introductions, again with many puzzled looks. Luckily a new Fellow, Dr. Khan, and an Attending, Dr. Nannegari, went along with it and really helped us out. We were able to talk to them for some time while they were filling out some notes on patients. Dr. Khan gave us a brief overview of GI and some quick notes on how the hospital functions. Inpatients, outpatients, consults, pretty much the basics.
We accompanied Dr Khan on a few of his consults. This also served to give us a quick tour of the hospital, introduce us to the Residents, and to get to know him better. These consult visits were quick, mainly just to review the patient’s condition and ask them a series of basic questions. Once we did that, Dr Khan just had to give his assessment to their primary doctor at which point they would then decide on a course of action.
Alas, Dr Khan gave us a heads up that it had been a slow day and did not have much left to do besides writing up the notes about his patients. He did however invite us to go and watch him perform an endoscopy the next day. We said our goodbyes and since it would have felt way too unsatisfying to leave our first day at that, we went to talk to the residents again. We asked them some pretty general questions about the hospital and the patients. Because many of them had actually just started we did not get too much information from them besides the fact that tubes and wires were all over the place during procedures and that the infusion pumps were annoying to deal with; nurses often ignored their alarm because they went off so often. Ironically we were given both of those problems as examples earlier in the day before we even got to the hospital. Even though we did not actually get much, we were able to a good reading off of the residents and give them an idea of what to look out for.
Once we were done there we wanted to take another crack at the clinic again and ask a couple of questions there. As soon as we entered the office portion of the clinic, with all the doctors and computers, Dr Jong to our surprise immediately knew who we were, with no introduction needed. She quickly set us up with a fellow each and sent us on our marry way to meet some patients.
To say the least, the day picked up a bit.
I was paired with Dr Skef, a brand new fellow from Canada. The process at the clinic was pretty simple. First, Dr Skef got a patient and looked up previous information in their record. We then went to go see said patient and asked a couple of routine questions to properly assess the nature of the visit and to develop a proper plan for the patient. Once that was done we went back to the office and reviewed the plan with Dr Jong, the attending physician at the time. After the plan was verified in a somewhat verbal exam type manner, we paid a visit to the patient, this time with Dr Jong as the main point person. Finally, Dr Skef put in his notes of the patient into the computer and once again the process starts from the very beginning.
The most obvious problem that emerged was difficulty in using the hospitals program to see all the patient’s information and to order medicine/tests. Dr Skef mentioned that he was still learning how to use it, however after a while I noticed that even Dr Jong had some difficulties and was not fully aware on how to use it. Beyond that the layout has many tabs and is very saturated with text.
Another problem was the difficulty to communicate with the attending in the narrow hallway of the office; especially if another doctor had to pass through as well. Trying to not be in the way of someone is clearly not easy.
To sum it all up, it was a bit of a roller coaster.
None the less, I could not be more excited.
The Answer Is in the Stool
Beny Romo Blog

For the rest of the short week I found myself mainly at the GI/Liver clinic going from patient to patient.
On day 2, I was shadowing a Hepatology fellow named Dr Martis in the morning. We met with 4 different patients; each of them at the clinic for different reasons. The length of the appointment varied depending on the reason for the visit, the questions that the patient had, and the availability of the attending physician, Dr Naveed at the time.
Every day I was with a new fellow and attending, but the process was still the same. When we met with a new patient, the fellow asked them a few pretty general questions. Regardless of the point of their visit these questions did not change much from patient to patient. The first thing that the fellow needed to know about was the patient’s stool, the shape, color, texture, and the number of bowel movements a day. The color and form of the stool is really important because it can indicate bleeding in the upper or lower GI, celiac disease, chronic pancreatitis, or bile duct obstructions. From these questions the physician may want to take some scans or upper/lower endoscopies to verify any problems in order to properly diagnose the patient.
Many of the patients expressed dissatisfaction towards the wait time, and this was consistent throughout the week as well. When looking at their waiting time, it mainly accumulated when the fellow needed to confirm his plan with the attending, but they are busy with another patient.
After asking one of the patient what one of the most difficult/annoying parts of visiting the clinic was, she let me know that she thought that simply talking about what specifically was wrong was the hardest part. She went on to explain the the topic itself is very private and hard to open up about.
Another difficulty that I saw was the patients compliance with their medicine and more importantly their diet. The patients diet was such a big deal for the patients that some patients were there specifically because they no longer wanted to stay with it and wanted to ask the doctor if they could do something else. Depending on the case some patients had to deal with it and others could try different foods, but with caution.
There was another patient that I met had a very interesting case. He was a prisoner. I hadn’t originally noticed this until I went to shake his hand and saw that he was wearing handcuffs that were attached to a chain belt around his waist. This really limited his area of mobility making it difficult for him to gesture to the area where he had pain. It also made it more difficult to examine his abdominal area.
The times that we weren’t in the clinic we were able to see two endoscopy procedures with Dr Khan and Dr Nannegari and an endoscopic retrograde cholangiopancreatography (ERCP) with Dr Boulay.
During the endoscopy procedures there were a couple of things that I noticed. First off, the scope and all of its features are tested to make sure it is functioning properly before the procedure starts. There are two knobs that control the movement of the end of the scope (approximately 4 cm) making it flex up, down, left, and right. The scope also has a flush feature, which means that it shoots out water from the tip in order to clean up the view if it gets too messy. It also lets out air at the tip in order to inflate the stomach/intestine to get a better view. During the procedure there were times where the doctor had to not only turn both knobs, but turn their entire body in order to twist the scope in order to maneuver throughout the duodenum. It took a couple of attempts from the attending to explain it with words and for the fellow to properly execute. There were times in the procedure where the patient would begin to drool so like in the dentist office the nurse had to suction it out. The difference that I saw was that the nurse put the suction back into its packaging and then placed it either behind the patient’s pillow or below the mattress.
The ERCP was very similar to the endoscopy at the beginning, however once the end of the scope got to the duodenum the Dr Boulay began to look for the major and minor duodenal papillas. Using live x-ray images Dr Boulay then needed to insert a catheter into the bile duct in order to remove and gull stones that were present. Once the stones were out a stent was placed in order to keep the duct open. Now all this doesn’t sound all that bad, but the hole was approximately the size of the tip of a ball point pen making any movement seem very large. The condition of this patient made the procedure much more difficult than normal. The whole procedure took over 2 hrs and all the people in the room had to be wearing lead the whole time, even though the x-ray machine was only on once the catheter tip was inside the duct, making standing there quite a challenge.
It may have been a short week for us, but we saw alot of patients, but no matter what we always started off with their stool.
Exploration of the Alimentary Canal
Beny Romo Blog
For the first half of this past week, were in the Endoscopy Lab basically the whole time. The Endoscopy Lab is were all the GI related procedures happen, for both inpatients and outpatients. During an average day there were approximately 20 patients. Even though there were that many patents I commonly was only able to see about 6 each day depending on what the procedures were.
Instead of going through each of the patients that I met, I am going to talk about each procedure separately in hopes of making this more organized.
Starting off, the colonoscopy is by far the most common procedure that patients needed. This is because it is recommended that everyone gets a colonoscopy at the age of 50. After that, depending on their findings another colonoscopy is recommended. If everything was healthy another one is not necessary for 10 years. If some polyps are found they often say 5 years. Beyond that it is usually a couple of months to keep a close watch. During the colonoscopy the patient is placed under twilight sedation, so they are pretty out of it, but they can sometimes follow simple directions from the doctor or nurse. The patients also experiences retrograde amnesia, which makes them forget their experience during the procedure.
The biggest difficulties that I noticed during the colonoscopy were actually knowing what part of the colon the end of the scope was at and having full control over scope. Just so everyone is aware the colon basically looks exactly the same regardless of what part of it you are in. To make it even harder, there is often a great deal of back and forth in order to get past some of the more complicated bits. In order to get around this problem the doctor makes his/her way to the cecum (i.e. the end bit of the colon that connects to the small bowel) and then they look closely for polyps, among other things, on their way out. This allows them to take their time and focus, while easily keeping track of their position inside of the colon; after all going out is much smoother than going in. While observing one of the colonoscopy procedures the patient suddenly exclaimed that he was feeling pain in his abdomen. This went on for a bit while the doctor tried to figure out the cause. On the way out of the colon we noticed “skid marks” caused by the scope on one of the walls of the colon. After the procedure was completed the doctor explained that from time to time when moving deeper into the colon the hose like part of the scope can twist on a sharp turn in such a way that it forms an alpha-loop. Now if the doctor tries to push forward once this loop is formed this alpha-loop just gets bigger, causing the patient pain, and the tip of the scope does not move forward as much. Pulling the scope out would also cause the patient pain because of the way the loop would unfold. The doctor mentioned that there was a maneuver that was used in order to minimize the size of the loop and then you could undo it with the least amount of damage to the patient.
I was also able to observe multiple endoscopy procedures. This procedure was much simpler than the previous because there are much less curves involved. The hardest part of it, for both the patient and the doctor in actually getting the scope into the esophagus. The patient commonly gags on the scope and puts in a good amount of effort to take it out even though they are under twilight sedation. Once that part was over, the rest of the procedure goes pretty smoothly. One of the patients we saw previously had a gastrectomy, which thoroughly confused me while I was trying to follow where we were. This cut down the procedure to about 10 min or less, the bulk of which was getting in the scope. The only other thing that I noticed was that if the doctor needed to take biopsies for whatever reason they inserted biopsy forceps into the scope and took their samples; while they were inserting the forceps into scope, the doctor kept inserting the wire until they saw it on the screen, which lead to an overshot making the tool hit the wall in front of the camera. This was also consistent when taking biopsies in the colon as well.
Another trait that both the colonoscopy and endoscopy have in common is that the nurses need to be paying attention to the level of the fluids that were sucked out of the patient. These fluids go to a canister that can hold about 1200 mL, if it were to overflow the fluids would go into the suction system and would damage it. I haven’t seen it get to the level that it needs to be replaced, but there have been a few cases that the level got high enough (about 1000 mL) that it made me ask the question of what could happen and if there was any indicator of its fill level .
Just to be clear, these canisters are replaced for each patient.
From time to time a patient would need both colonoscopy and endoscopy. When this happens, the endoscopy is always preformed first because it requires more anesthesia. The room is set up with two scopes from the very beginning in order to save some time. After the endoscopy in complete, the nurses quickly turn the bed around to that the patient in now facing the other direction. It is important to note that these rooms are tiny and turning the bed around is very difficult especially when trying to work around all of the tubes and wires. While this is happening the doctor hooks up the second scope and does some quick checks to make sure all the features of the scope are working.
I was also able to observe another ERCP, which was just as intense as the first one. This time I were able to talk to the doctor a bit more before the procedure started so I found out a bit more about the procedure itself and about the tools that they use. For instance, a special scope is needed for this procedure because in order to find the papilla that lead to the bile duct we need to be able to see sideways, so this scope has its camera on the side of the tip instead of right in the front, as shown in the diagram below.
It also has an extra knob that controls the elevator adding more sensitivity to the movement of the catheter when it is used. While all of this is fine and dandy, it also makes it harder to get to that point because you cant easily see where you are going.
This specific patient also had the added challenge of having a couple of tubes coming out of his chest for a multitude of reasons. I didn’t mention this in the last post because it was not that relevant, but during the procedure the patient is lying on their chest. In order to protect those tubes and therefore the patient, these foam doughnuts were taped over the tubes, this just seemed kinda weird to me and very improvised. During the procedure I also noticed that it was very focused on trial and error. The doctor literally tried more or less the same movement over and over again in order to get the catheter around a bend until it worked. There is very limited control over the catheter, at one point it buckled and made a U shape while inside the bile duct. This was clearly very frustrating because it got stuck. The doctor inserted a stiffer wire into the catheter, which ended up fixing the problem. This patient needed a stent to make sure that stones didn’t get stuck in that area. The stents were inside a normal sterilized package, but that package was also inside its own box. This stuck out to me because everything else in the room didn’t come in this extra box casing.
The only other procedure that I was able to observe was an endoscopic ultrasound (EUS). This procedure is usually preformed in order to take a close look at the pancreas. Again this procedure needs its own special scope which has an ultrasound probe at the end of it right before the camera. Now this is where I really got lost, I could not make out most of what was on the small ultrasound screen. It looked a bit like a mess to me. The only thing I can say about this procedure is that in order to properly see the image a balloon at the tip of the scope needs to be filled with water because ultrasound does not work with air. When this balloon is inflated for the first time, it is filled mostly with air because even though the water line is hooked up, there is still air in the pipes of the scope from before it was connected. Removing the air takes some time and is an annoying process for the doctor.
Besides observing the procedures, I was able to talk to the doctors a good amount, mainly about anatomy in order to get a good understanding of what was going on in the procedures. I also learned about a procedure that doctors didn’t particularly like, Dr. Boulay was at the VA in the morning and he had to insert a rectal stent. The reason that this procedure isn’t very well liked is that there is no way for the patient to prep for it, so once the rectum is opened everything comes out. Needless to say it can get pretty messy.
I am almost certain that I learned more about the anatomy of the GI tract in those two days, than I ever have before. Initial exploration was clearly a success.
Different Scopes for Different Folks
Beny Romo Blog

For the rest of the week we spent it in the GI lab, observing more procedures. Although we had already seen some of the procedures being preformed, watching them for a second, third, or even fourth time still revealed different insight on the procedures. Another benefit of watching a procedure more than one was the ability to verify if a previous observation is consistent though out a greater amount of samples. They also had the added benefit of being pretty cool to watch as well.
After looking at a couple of colonoscopies again, there were a couple of extra details that I noticed. For one thing the doctor preforming the procedure commonly holds the hose part of the scope with a small washcloth. This is done in order to get a better grip of the scope and to not get lube on the gloves. Another little trick that I saw was that if the doctor is having trouble around a difficult bend the nurse will apply pressure onto the patients belly so that the scope has something to push back on; making it easier to ride the colon, as described by one of the attendings. There was also the fact that when removing a polyp it is completely up to the doctors best judgment whether or not it has been sufficiently removed. If the polyp was not completely removed it can easily grow back making this part more delicate.
I actually didn’t see any more basic endoscopies, instead I was able to observe a couple of more advanced procedures like another EUS, a double balloon endoscopy, and an EGD dilation.
During each of these procedures a different endoscope was used. They all basically looked and functioned the same, but they each had a extra little thing that was vital for each specific procedure.
In many of the procedures, most noticeably in the double balloon endoscopy, the physician preforming the procedure ran into a good amount of obstacles. For example, it was common that a second person would need to hold/insert/operate an extra tool that was placed into the scope. This made things difficult because the physician would need to tell the second person exactly what to do and when to do it. At times the people would not be in sync and the procedure took longer to preform.
Another thing was the difficulty of manipulating the scope around difficult areas. In the double balloon endoscopy there was visible bruising to the walls of the small intestine where the scope commonly got stuck. Luckily the patient cannot feel any pain in that area, but it will take some time to heal.
Meeting the Inpatients
Beny Romo Blog
For the final week at GI, we mainly shadowed Dr Skef during his inpatient rounds and consults. The mornings always started off the same. Rounds. This was where the residents, the fellow, and the med students all presented on their patents to the attending and then everyone discussed in order to create a preliminary plan of action. With all the talk of LFTs and sodium levels, I quickly got relatively lost. These presentations lasted quite a while, because of all the patients that were admitted into GI or were being consulted by GI.
After the presentations we went from patient to patient to review exactly what we had just talked about. The attending reviewed the questions for the patent that had already been asked to verify the status once again, and then they would explain the plan that had been discussed previously.
Having the attending, the fellow, and all the residents going around from room to room, sometimes stopping right in the middle of the hallway outside a patents room to discuss, seemed pretty overwhelming and many times cluttered. The residents were each assigned a small amount of patents so they didn’t necessarily need to pay attention when it wasn’t their patient, but it did give them greater exposure by being there.
During the madness of shuffling around, I was able to notice that the inpatient beds where larger than the ones we had seen in the GI lab. These beds were also more difficult to move around, especially because patents are almost always hooked up to IVs.
Playing with the Toys, and Goodbye to GI!!!
Beny Romo Blog
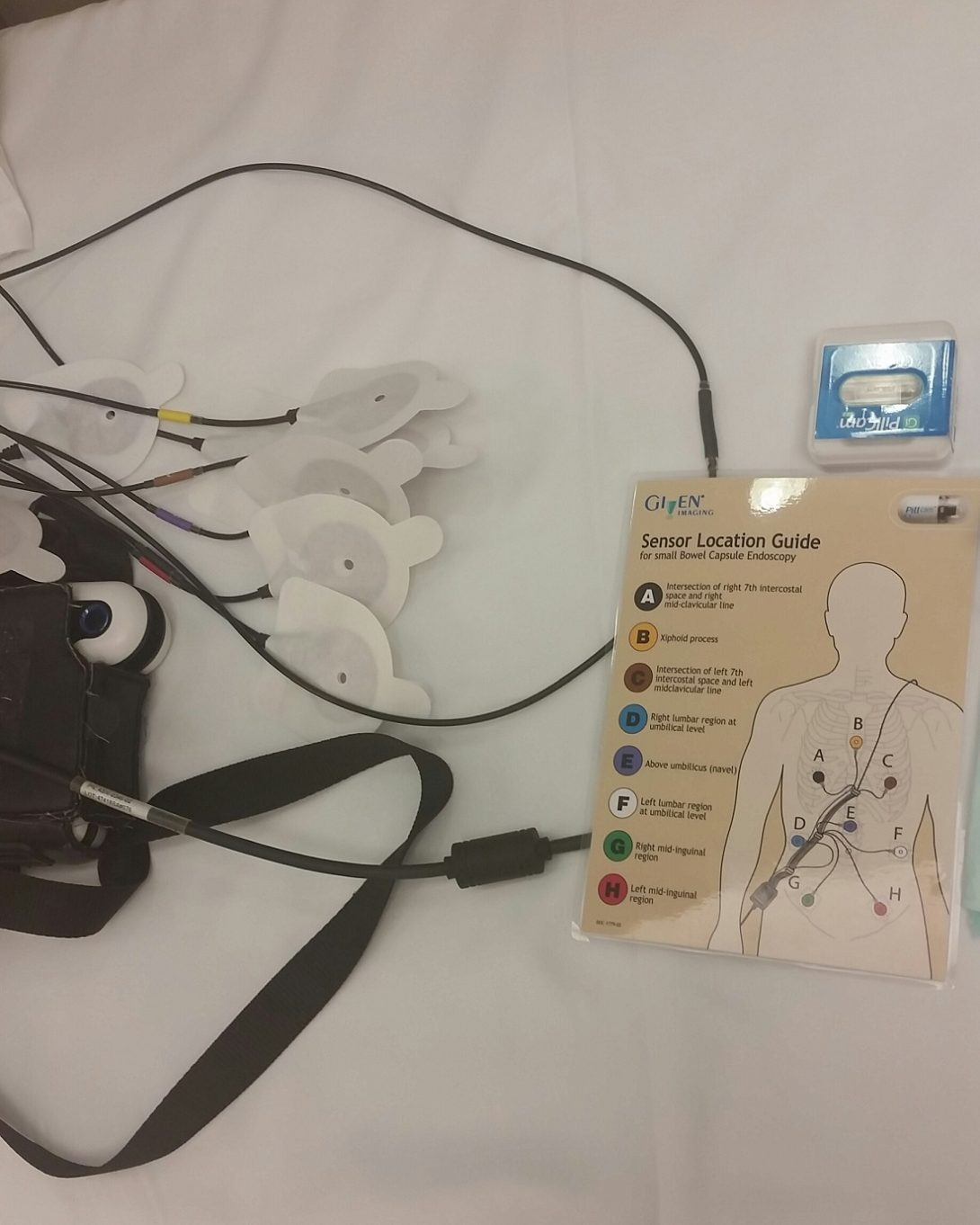
In the last days of the GI rotation, we spent most of the time with the inpatients, however we were also able to finally actually take a very close look at some of the instruments and devices that are used during some of the procedures.
Most notably I was able to see how all of the scopes get cleaned; during this time I also got the opportunity to hold a scope and actually feel what it is like to control it. The knobs used to control the tip of the scope actually had a higher resistance than what I had originally expected, but they also didn’t slip back to its original position if I let go for a second. After a bit of using it I also noticed that I was actually holding it backwards in my hand…I’m sure this doesn’t happen to real doctors though. Holding it properly made it more comfortable to move around, as it should, however, it still felt like it required a large set of hands to turn the knobs with ease.
Let The Neuro Begin!!!
Beny Romo Blog

Making it to week 4 means that I am in Neurology now!
It also means that I am no longer on a two person squad, but now in a four person team and I get to work with the IMED students. This is defiantly going to be different than the last rotation for sooo many reasons, but they are also all reasons to be excited.
We started the rotation off in the ICU in the mornings and in the neurology clinic in the afternoon working with all kinds of patents.
I was with the stroke team specifically, during rounds in the ICU. The patents that they commonly saw were patients who were at risk of stroke (i.e patient who has suffered from some kind of aneurysm or hemorrhage) or had recently had a stroke. The interactions between the patients and the attendings were very different from those in GI. In Neuro, the attending commonly experienced some difficulty while trying to communicate with the patients; at times compliance was the issue, but it could also be due to aphasia.
This was not the only difficulties in communication with patients that physicians ran into; the reliability of some of the patients was questionable at best sometimes. Because specific details and patient history is so important, physicians need to track down family members and/or witnesses.
This is clearly not something that can easily be resolved, but it is a very prevalent problem.
The Wonders of the Brain
Beny Romo Blog

During the rest of the week we continued the same basic schedule, stroke ICU inpatients in the morning and then clinic in the afternoon. The specific type of patients at the clinic varied from day to day, one day it was epilepsy patients and the other was neuromuscular patients. We also got the chance to look at some EEG recordings and learned the very basics on how to read them and what physicians are commonly looking for in these graphs.
During the time that we spent going through rounds with the stroke team, the physician commonly preformed a series of quick reflex and physical exams. These exams had very little quantification and the score given was also subjective. The patient’s physical exams are rated on a scale of 0 – 5, zero being unable to preform the task and five being preforms the task normally. For the reflex tests it was a bit more complicated since there is a possibility of the reflex being hypo-reflexive, hyper-reflexive, or some other potentially abnormal variation.
The EEG readings were, in my opinion, one of the more interesting things we have seen so far; mainly because it has alot of potential for growth.
A Day In Radiology
Beny Romo Blog
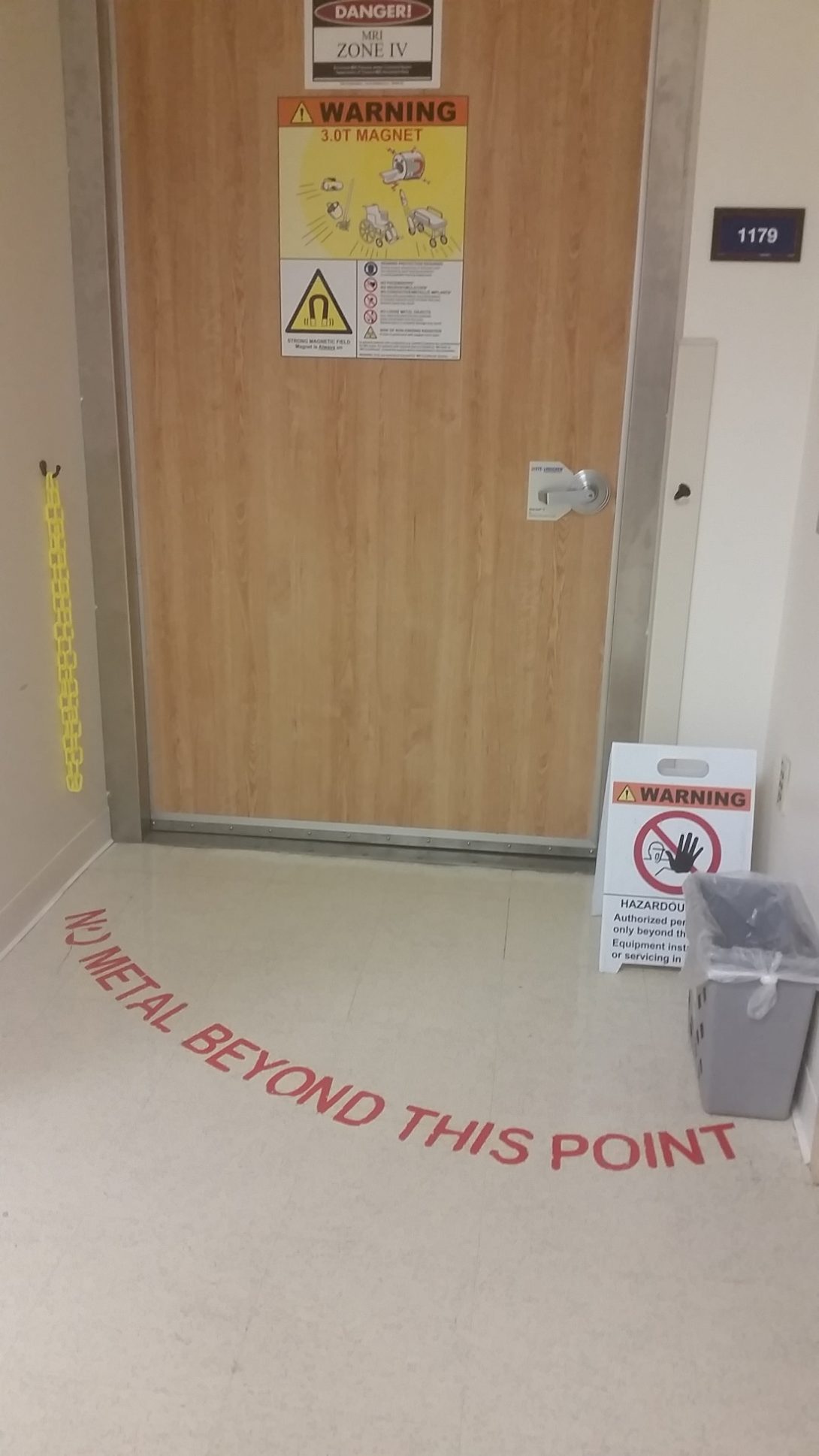
For the most part this week has been a continuation of last week. By this I mean that the days mostly consisted of inpatients and clinic. However we were also able to spend some time with radiology seeing that in neuro the physicians commonly need to use multiple imaging techniques to help with their diagnosis.
During our time with radiology, we mainly focused on the different types of MR Imaging and on how the machine actually functioned. We then were able to spend some time with one of the techs that actually take the images. During this time we learned about the different precautionary measures that were taken due the high risk of injury that comes with using these machines. The MRI magnet is always on, and produces a magnetic field that is ~50000 times stronger than that of the earth. If a person were to enter the room with a piece of metal on them, it would quickly accelerate towards the center of the MRI machine reaching bullet like speeds.
“Can you read my mind???”
Beny Romo Blog
Instead of just sitting around reading the EEGs we were actually able to see some being preformed!
While watching the setup of the EEG, it was clear that patients don’t often know what the EEG does to them and how it works in general. The technician told us that first time patients often were very nervous about what was going to happen to them. They would ask things like “Are you going to be zapping my brain” and “Can you read my mind”.
Annmarie Scully Heading link

I am a senior in bioengineering focusing on cell and tissue engineering. My first rotation is orthopedics and my second rotation is urology.
Annmarie Scully Blog Heading link
-
Annmarie Scully Blog
First Impressions
Annmarie Scully Blog
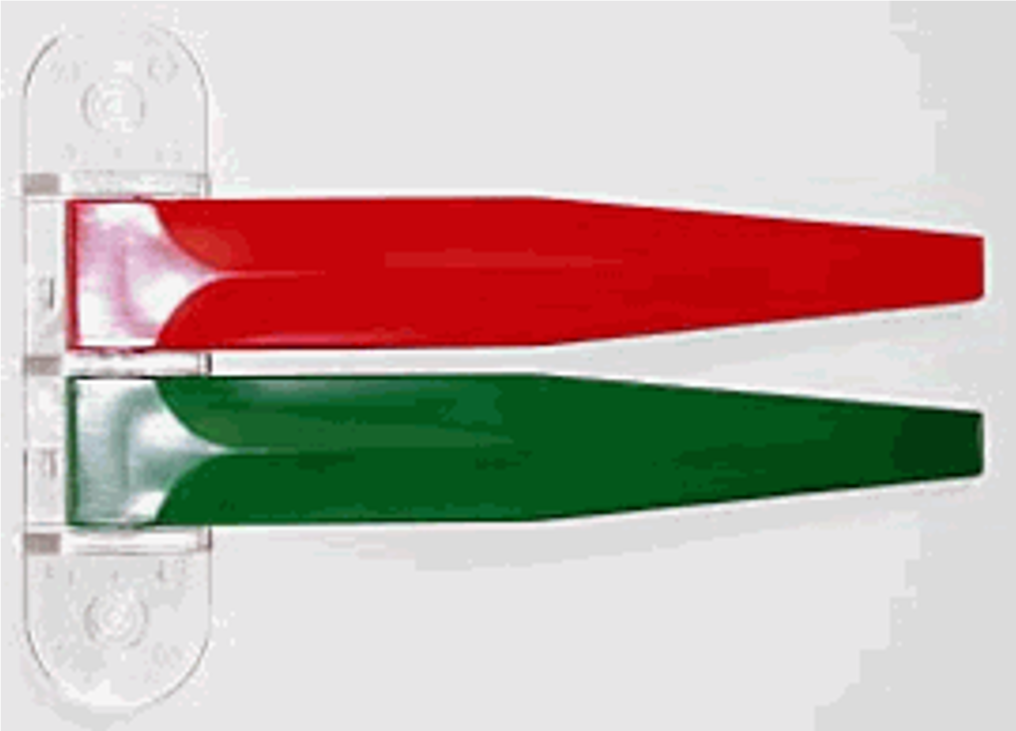
The first day in orthopedics we were scheduled to observe a surgery but unfortunately the operating room was closed. Instead, we got a tour of Dr. Siemionow’s lab, who performed the first near total face transplant and she focuses on hand surgery and peripheral nerve surgery. To get straight to the point her lab was amazing! She had her students, Ava and Anna, show us around the cell culture room and the microsurgery room where they perform surgeries on arteries and veins in rats.
The second day in rotation we sat in conference during the morning. A few different doctors talked about shoulder instability, skin grafts, and skin flaps. I never realized how many different techniques and tools were used to perform certain grafts or flaps. I was overwhelmed with all the information that was given within the short four hours but also gained insight of all the information medical students have to learn to perform, what i thought, were simple procedures. During the afternoon we got to observe medical students, residents, and Dr. Marcus in the orthopedic clinic. I learned that residents are assigned to an attending and as patients come in residents will see them first, collect history and problems they are experiencing, conduct a brief examine, look at x-rays and/or MRI’s, and report back to the attending with all the information. Outside of the patient rooms two flags were hung on the wall, one green and one red. When the patient first arrives the green flag is shown to indicate that the patient has not been seen, when the resident/doctor is in the room or already saw the patient the green and red flag is shown, and when the patient is waiting for a brace or surgery papers only the red flag is shown. This system presented a problem with the system flow because sometimes no one would notice the green flag was up and a patient was waiting or it was forgotten to change the flag color if a patient saw the doctor or changed rooms. Another problem that was presented was patients who made an appointment with the call service were given a spot with Dr. Marcus but should have seen a different orthopedic because Dr. Marcus did not specialize in their injury, misusing the doctors and patients time. This is due from a lack of information and history in the call center to correctly place the patient with the proper doctor.
All in all, the first two days have been very enlightening and shadowing the “behind scene” work has given me a new perspective of a doctor visit. I have already learned so much and I am excited to learn more about their system and problems in the coming weeks in different clinics and environments.
Week 1
Annmarie Scully Blog

Concluding our first week in the orthopedic rotation our group has identified many small problems that greatly effect the flow of the clinic. Problems like trying to track down the attending, not knowing if someone is in the cast room, and/or not being able to see if anyone is in the rooms around the corners effect the speed and wait times for the attending and patient.
When we observed Dr. Mejia’s clinic he presented his method of seeing his patients in a timely matter. He places refrigerator number magnets on the door frame to keep order of what patient is next. He also uses the letter magnets ‘b’ and ‘o’ to indicate brace or operation. This system seems to be effective by meeting with the patients in the correct and most effective order. But, as patients leave Dr Mejia has to run around and switch all the numbers to the corresponding door. This seemed like a lot more work than it should be and somewhat confusing if a number was misplaced.
As the first week came to an end I became intrigued by how the residents and attending worked during busy and stressful periods and how they worked around certain inconveniences differently. I have also observed how different doctors tackle different problems and situations. I look forward to examining how Dr. Gonzalez handles these problems and the issues he has with the current system within the next couple weeks.
Starting Week 2
Annmarie Scully Blog

Starting week two everyone got the chance to inform each other about their rotations. It was very fascinating hearing everyone’s experiences and problems they were observing. In particular, it was interesting to hear about my second rotation, urology, and see what their first impressions were.
After our group meeting we were able to attend Dr. Chmell’s clinic. He was very informative and willing to discuss current issues he observes as an orthopedic surgeon. One problem he discussed was material sensitivity, which is how different patients react to different material. For example, a lot of people are sensitive to nickel when it contacts the skin but they do not have a definite test to see how the body would react when it is in vivo.
Another problem he explained to us was how he cannot tell a patient’s progress after surgery until they come in for a follow up. An option he presented to fix this issue was a designated app where the patient could routinely enter in their progress and the information directly gets sent to the attending/resident. Dr. Chmell provided us with a lot of good information and our group is excited to get input from the various orthopedic surgeons about these issues.
On Tuesday we got to experience the Illinois Bone and Joint Institute (IBJI) with Dr. Gonzalez. The pace and experience was the opposite of the clinic at the hospital. We went from watching the attending/residents handle 87 patients the day before to one attending/resident handling 15 patients. One thing we did notice was the difference in their flag system. They had eight flags instead of only two, the top two were the different colors, the next four said “Room #1”, “Room #2”, etc., and the bottom two said injection and x-ray. Since they did not have as many patients the flags were not as useful as they were at the UIC clinic. With more downtime at IBJI Dr. Gonzalez was able to explain a lot more anatomy and functions of the hand. I look forward to learning more from him throughout the week and seeing his surgeries on Thursday.
End of Week 2
Annmarie Scully Blog

Wednesday we observed Dr. Gonzalez in a completely different atmosphere. We were at the UIC clinic and he was seeing three times the amount of patients than the day before. He was working at a completely different pace and had minimal time to talk to us unlike his clinic at the Illinois Bone and Joint Institute. As I followed Kyle, a 5thyear resident, he explained how their lack of resources, for example, tablets and/or more computers, made their job inefficient. This problem presented a scenario where there is the technology to improve the situation but the department does not have the funding for it.
Kyle also explained the ICD 10 (diagnoses) and CPT (procedures) coding system. They recently upgraded to the new version and the amount of codes grew immensely. He told us that they do not have a good system to look up these codes and usually have to google or look in the book for them. They also do not receive adequate training for the level of coding they do so it takes extra time they could be using to see more patients.
As Wednesday came to a conclusion, I was able to see many different patients with different diagnoses. I saw a cast removal and someone who got a cast, I was in the room for an x-ray, and saw a patient who got injections into her knees for arthritis. I look forward to observing more in clinic throughout our last week in the first rotation.
Thursday we finally got to experience our first OR day. We saw a cyst removal from a wrist, plates inserted for a tibia fracture, a knee revision, and two knee replacements. I found it interesting that throughout most of the day he had two surgeries scheduled around the same time and would switch between rooms. Also, it was fascinating to see the different atmosphere in each surgery. The cyst removal was relatively quick and the doctors were pretty relaxed. As we moved onto the tibia fracture and knee replacements the amount of tools used were quadrupled (it looked like a hardware store) and I could tell they were more serious procedures. Most of the time during the knee revision and replacements the residents were there holding up the leg into a bent position and Dr. Gonzalez did the majority of the surgery. Quite a few times during each surgery he would stop and explain to us what he was doing and how the knee replacement worked. It was really cool to see all the different components of a knee replacement and how they all fit together like tinker toys. A lot of time was spent guessing and checking with the trials to see what size knee replacement would fit and then they would insert the actual replacement. One problem we did notice was the wire situation. They had wires hanging from IV stands so the anesthesiologist could easily walk underneath them but on the other side of the room they had some on the floor and I saw Dr. Gonzalez get caught in them a few times.
Watching surgery for the first time was amazing. I have always heard how orthopedic surgeons just saw and drill into bones but seeing it in person was so fascinating and I was amazed by the different techniques and tools that were used. Watching surgery and all the technology that is used has been the highlight to this rotation thus far. I cannot wait to experience it again next week and hopefully see other technology being used.
Last week in rotation #1
Annmarie Scully Blog

As we start our last week for the first rotation I never realized how fast this experience would fly by. I have seen a lot of repetitive diagnoses in clinic but also some really interesting ones. Being able to experience both the UIH clinic and IBJI clinic was an awesome opportunity since we got to compare the difference in patient flow and resources which are a main issue at the UIH clinic. Also, being at IBJI gave us a chance to learn more about certain procedures and anatomy from Dr. Gonzalez since the patient amount was significantly lower. Our last day at IBJI there was an increase in patient volume from the previous week but Dr. Gonzalez was still able to inform us briefly about the different surgeries we would see this week. So far I have enjoyed the IBJI clinic more because of the fact that Dr. Gonzalez is able to sit down with us and discuss the different procedures and teach us about injuries that can happen to a hand.
Today we were back at the UIH clinic. I learned and observed a few new things and also saw problems we initially pointed out. Some new things I learned were that residents rotate the pager every couple days instead of having it the entire rotation, they have not tested to see how weather or other circumstances affect the patient no show rate, and they do not have a system to transfer images to other departments (other than running over there) if the images are from outside of UIH. One of the main problems we have noticed the past couple weeks was a big issue today. People who are scheduled to get an x-ray before the visit but do not, which wastes resident/patient time and room space. Our group discussed how this could easily be fix if they made this order prominent on the patient chart so the check-in desk or nurse could easily see that they should get x-rays before they are given a room.
I am excited to observe one more day in surgery especially after Dr. Gonzalez gave us more information about the procedures. We are lucky enough to get the chance to see a variety of operations that pertain to different parts of the body.
Last day in Ortho
Annmarie Scully Blog

Unfortunately, we had our last day in the OR for orthopedics but luckily we were able to see a variety of surgeries that differed from the week before. When we first arrived a sales representative from Stryker had new helmets for the doctors to try. The helmets they use keep air circulating through their suit so the shield does not fog up. The new helmets were designed to weigh less and have added functions like a head light which the doctor seemed to like.
I also observed how patient flow affects the OR similarly to the clinic. Before the first surgery a tech was late which postponed the preparation and delayed the surgery about an hour which pushed everything else back. Factors like this, late patients, contaminated and/or missing tools effects the doctors/patients time schedule.
After the two days we spent in the OR we saw two hip replacements. One was done by an anterior approach and the other posterior. One interesting thing I learned about these cases was the different operating bed they use for the patient. The posterior was done on a normal operating bed but the anterior was done on an operating bed that had two boots to hold the legs in position. These boots allowed them to rotate, push the leg in/out, and change the traction. I thought this was very useful for the surgeons so they could make sure the hip was in place and that it would not dislocate.
Being able to experience the variety of surgeries was an amazing learning experience especially because Dr. Gonzalez would take his time to explain how the tools and prosthesis worked. It was also fascinating to watch doctor interactions during high and low pressure situations. I have learned a lot in this first rotation and I am excited to observe Urology for the remaining three weeks.
Urology Week 1
Annmarie Scully Blog

The start to the second rotation in Urology was awesome. Harp (one of the 6thyear residents) provided us with a lot of information and was willing to coordinate anything to give us the best learning experience.
We started this rotation in the OR and we were able to discuss possible needs with some of the nurses. Here are some issues they frequently run into:
- Communication: switching between computer programs for different tasks
- Communication: physician talking to patient, language, culture, hearing problem
o An anesthesiologist suggested it would be beneficial to have a button device that had simple commands in different languages that they could press to communicate easily with the patient
- Sending wrong tools or missing entire tool sets
Our team also noticed a lot of other inconvenience for the surgeon and/or patient:
- Lifting patient from bed to bed which could potentially injury the doctors especially if the patient is overweight
- They use pillows and towels tapped up to get patient in the right position
- They tapped a patient to the bed so she wouldn’t fall over
- It took them about 30 minutes to position the patient which we thought was a long time but one of the residents said that was normal
- They used a bed with boots to position legs which was similar to the bed I saw in one of the orthopedic surgeries
- One of the residents was telling us how comfy the Da Vinci was to use that he could fall asleep using it
The first day in Urology was very informative and I was really interested seeing the Da Vinci perform a surgery since that was the first time I saw one. I am excited to see how our remaining time will be spent and to learn a lot more about Urology.
Urology Week 1 Part 2
Annmarie Scully Blog

Day 2 in Urology Harp and Norman had it set up for us to visit the Sterile Processing Department (SPD) where they sterilize all the equipment. We talked to Yolanda who explained some issues they face in this department.
- Their elevator breaks at least once a week so they manually have to push all the used equipment from the OR to SPD which is in the basement
- Not enough room
- They do not have enough shelving so they stack trays on top of one another
- They share space with materials (disposable equipment) when they do not have enough space in the first place
- They are suppose to be on a schedule that coordinates who gets what at certain times but it is never followed
- Only one computer to scan and log all equipment
- Everything is scanned for each process they go through: decontamination –> assembly –> sterilization
- This scanning process allows people in the OR to see where their tools are and how long it will take to finish cleaning
- They had 3 computers for each station but 2 broke a few months ago and they still have not been fixed
- Hours are lost each day because there is only one computer
- It gets so busy in SPD they have to wait in line to scan and some employees do not want to wait so the tray does not get scanned and then no one can find it
We also spoke to Cyndi who is the liaison for SPD and the OR and she said the main problem she sees is that the trays are not correct and if people (in transport) had more education about the tools and surgical departments it would reduce this issue.
The next step after going through SPD is transport and they handle placing the tools in certain trays. We have not been able to visit transport yet but we are hoping to speak to them before our rotation is over so we can see their view and compare their needs with SPD.
Urology Week 2 Part 1
Annmarie Scully Blog

Starting week two we finally were able to shadow in the Urology clinic. We saw how they had communication issues, for example, they had three different residents ask the same attendee the same question about the same patient. Harp also explained to us how communication is a huge issue in medicine especially the lack of communication between institutions.
We were then able to show Harp our flow chart we made after the visit with the Sterile Processing Department (SPD) last week explaining all the different needs we found between the OR and SPD. He explained how tiny improvements could dramatically fix some of these needs and he is willing to set us up with a time to present our flow chart to a board that deals with quality improvement. Harp has been amazing and he is doing everything to give us the best experience.
After lunch Nadine (a nurse practitioner) offered to show and explain how the Urodynamic device works. They use this device when every other test is normal and when previous treatment is not working. It checks the bladder to find out why it is acting a certain way. She first explained the Uroflow test, which is done when the patient has a weak stream. To perform this test the patients have to come in with a full bladder which is at least 100 ml so they get accurate results. They have the patient urinate in a portable toilet (which connects to the computer/program via Bluetooth) and that records the flow rate and volume. The next test she explained to us was the Urodynamic test which is when a patient has a function problem or over active bladder. With this test they inject catheters that have sensors into the bladder (measures pressure inside) and rectum (measures pressure outside). Because these catheters have the sensors they do not have a balloon at the end that holds the catheter in place so Nadine has to tape the catheters really good so they do not move. Before the catheter is placed they make sure the bladder is empty. After the catheter is in they sit on the toilet and water is pumped into the bladder through the catheter. The patient then has to inform Nadine when they initially feel the urge, two more times when the urge gets worse, and when the patient cannot hold it any longer. Nadine marks this on the data and then the patient is allowed to urinate. This test measures the pressure in the bladder, pressure in the rectum, the difference between the pressure in the bladder and rectum, and when they leak/urinate. Nadine explained how uncomfortable and tedious this procedure is because the catheters fall out and move easily so she has to stop the test often and untape the catheter, reposition (to make sure the bladder and rectum pressures are the same when the patient coughs to get the correct results), and to tape the catheter back up. Also when the patient urinates it goes around the catheter so it gets on the toilet seat, floor, and catheter. We also noticed how the toilet does not accommodate heavier people because of the handles and Nadine said when they do not fit they have to squat over it.
I am so glad Nadine was able to take time to explain pretty much everything about this device especially since I did not even know it existed. I am excited to learn more from her and the attendees/residents when we go back to clinic.
Urology Week 2 Part 2
Annmarie Scully Blog

The past couple days we were back in the OR and were able to see a variety of surgeries. After our talk with Harp he started to point out when tools were missing so we could realize how frequent and how much of an issue it is. He was explaining to us how the doctors have a preference list for the surgeries they perform so they could assemble the cart with everything they use. One example we saw was a foam mat that was missing from the cart and the surgeon uses that specific mat every time he performs this surgery so a nurse had to go down to the Sterile Processing Department (SPD) to locate one which delayed the patient from moving over to the operating table. I was able to realize more and more throughout the day how this is a huge issue for the OR because it causes so many delays. We were also able to talk to Norman about our observations in SPD and he is going to set up a time where we could go back down to SPD and specifically follow one tray/tool through every process to examine how tools get miss placed.
One interesting thing we learned was how the penile pump works. We were able to talk with the sales representative and she explained how it functions and the main reasons for failure which are infection and/or the silicone ripping exposing the fabric underneath. I am really happy we were finally able to see more of a variety of surgeries this week and I cannot wait to see what our final week has to bring!
Urology Week 3 Part 1
Annmarie Scully Blog

Our last week in Urology we were able to revisit the Sterile Processing Department to better understand the process of getting the instruments from the OR to SPD back to the OR. The first thing we noticed is the checklist they had attached to each cart displaying which tool and how many are in each tray/cart. We also saw how they have a bright pink sheets on the carts that list all the tools that are missing on that particular cart. Yolanda told us that the operating rooms are informed before the surgery about the missing tools and they can then decide whether or not to use the tray.
We then were paired up with an employee and watched the process of cleaning and organizing the instruments. The instruments first get hand washed and then go through a wash machine to remove all the blood. After, each tray is checked for blood, dirt, cracks, and/or broken instruments. If something is broken it goes into a “needs to be fixed” bin and a company comes once a week to fix them, if something has blood or dirt on it, it will go back through the whole washing process.
Once everything is checked they start to assemble the trays. Every instrument is in their system and they go through the list for that particular tray and check if it is either there or missing. If they have extra instruments they have to go around to see if anyone else is missing them because their system does not have a button for the extras. Juan had each of us go through the process of looking at the number on a tool, finding it in the computer system, checking it, getting the correct quantity, and putting it in the tray. It was interesting to actually be able to do part of the process they do over and over everyday for every instrument.
After everything is in the tray it is locked, tagged, and brought to the sterilization machine. Juan was explaining some things that could potentially go wrong in SPD.
- The lock is white, after it goes through sterilization it turns black
- If the lock is still white when brought to the OR it is not sterilized
- If there is no tag on the tray it is not sterilized
- Single use items come down to SPD but they should have been thrown away after the surgery it was used for
- Instruments are placed in the wrong trays in the OR so SPD has problems finding them because someone else has it in their tray
Overall, being able to spend more time in SPD was very useful and I now understand more about the cleansing process.
Final Blog
Annmarie Scully Blog

Unfortunately this program went by too fast and we are approaching our last day. The past few days in Urology we were able to spend it in the OR and presenting to Harp. After our presentation we received good feedback from him and was able to use it to improve our presentation. Throughout our two rotations I was lucky enough to observe many different departments. For example, in Orthopedics we were mostly in clinic and in Urology we were mostly in the OR and SPD. This gave me many opportunities to compare the different environments and departments and learn a lot more about these two specialties. It was also very cool to see the variety of different surgeries especially in Urology and all the different technology they use. I am very happy I had this opportunity and I am sad to see it end.
Joel Severson Blog Heading link
-
Joel Severson Blog
First Day!
Joel Severson Blog

When I first started we, me and my group, went to four locations before we located the resident that we needed to be in contact with for our Clinical immersion urology rotation. I understood quickly that in order to get as much out of this program as possible a more persistent learning style would be needed. Even though this program has just started I am amazed at the equipment and technology that is being uses. Many procedures and technology seemed almost futuristic and serial. The more I saw the prouder and more excited I became about future project I would be working on and as a aspiring bioengineering.
The first patient I saw needed a prostate biopsy. The patient looked very uncomfortable. Already ideas were coming to my mind for how to make this process easier for the patient and doctor through changes in the equipment. During the prostate biopsy there was a large needle that was use to grab specimens for testing. There was a loud clicking sounds that went off when the needle went in to take the specimen. This obviously made the patients tenser. I am sure a design could be made that does not make a sound and could be more silent.
Another complication with the prostate biopsy was locating the suspected cancers region of the prostate. The MRI imaging gives the information about suspected cancer and then the doctor sets an appointment to get the specimen. However, during the biopsy, they cannot location the suspected cancer region found on the MRI. Which forces them to take 12 samples (all different regions) in case the cancer is currently isolated to a certain part of the prostate. What would be helpful is if during the imaging process there was a way to flag the location that the doctor is concerned about, i.e. Leave some sort of indicator for the ultrasounds machine (which is used for taking the prostate specimen) to better isolate the desired location to test.
The ultrasound probe had a unique design. After it was inserted and you located the prostate the probe allows the needle to go through the ultrasound prop so the needle is guided to the exact location the the ultrasound shows.
Another potential concern is the chance of infection since the needle will have to go through the rectum into the bladder. They give him some medication to try and clean out the rectum. But there is still a chance of infection which is concerning.
There is a test that is done called the Prostate-specific antigen (PSA) that has to be done every 6 months and forces the person to come into the clinic. What would be curious to find out is if this test could be done at home similar to a glucose level test that can prick your finger and test the PSA and alter you if there is a need to come in and it send that information to the patient’s doctor and the doctor can review the information independent of the patient’s presence.
This clinic also has a very nice setup where all the nurses, attending, residents and schedules sit together this helps speed up communication and efficiency of the office.
Operating Room!
Joel Severson Blog

This was my first day of going to the Operating Room (OR)
*I am searching for the surgery I am observing by doctor’s name, I walk up to a nurse*
“Do you know where Dr. ____ OR is?”
Nurse, “ He will be in room 8 and 4”
Me, “He will be in both OR 8 and 4 at 8:30?”
Nurse, “Yes”
My first thought in the OR was how normal of a room it looked. The only special parts of it are the sanitation and the equipment. I expected the room itself to have a more surgical focused design. The surgical bed had a lot of attachments. There were arm extension that could be added on and straps that had to be added on manually. I became curious if it would be easier if all these attachments were not removable.
When the patient was asleep, there was a specific location the surgical team required the patient in for the surgery. They spend some time manually adjusting the patient to get them in the precise location they want them in for the surgery and also removing pressure off of pressure points on the body so that the patient does not wake up and feel sore from that constant pressure on their joints.
When the patient is positioned correctly they make an incision in the abdomen to insert a tube that fills the abdomen with CO2. This allows separation of the epidermis from the internal organs. Then the da Vinci Xi is used.
The da Vinci Xi machine is a robot that assists with laparoscopic surgeries. This device has a total of four extensions that enter the body through small incisions near the surgical area. The extensions can rotate in every angle. Then the instruments at the end of the da Vinci Xi extensions have seven degrees of freedom. These instruments are the part of the machine that will be accomplishing the surgical objectives such as locating the desired region or organ, cauterizing, and suturing. The reason why this machine is so useful is because the incision sites are so small so there is not a large scar. Probably the best part of this is that the instruments that are used on the end of the robot’s extensions are millimeters in size. Much smaller than the space a surgeon’s hands would need to complete the same surgery. Two extensions that are constantly being used are the camera and suction. The camera has great resolution and is displayed on several monitors surrounding the patient in the OR.
This image is also displayed at the da Vinci operating table. This is a table where the surgeon operates the robotic extensions and and instruments at the end of each extension. He has is own three dimensional image that he sees, through a device similar to a microscope. Both of his hands are on two joysticks that control the extensions the surgeon wants to move. The surgeon can move this in every direction that the extension and instrument can move. For the instruments that open and close they are sensitive to the surgeon’s squeezing the joystick. At this separate operating table, the surgeon also controls when to cauterize. This cauterization presents some difficulty during the surgery. Since the abdomen is filled with CO2 the smoke produced by cauterization makes the air inside the abdomen harder to see through, because of the smoke (just like smoke at a fire would).
The suction tool that is inserted into the abdomen just like the robotic extensions provides a partial solution. This suction extension is dependent on someone besides the surgeon at the robotic operating desk. This person must move this extension independent of the robotic operator. If this extension is not close enough to the device that is cauterizing, then the camera become smoke and the surgeon is forced to pause and wait for the smoke to clear. A potential solution is to have the suction extension combined with the cauterizing so that the smoke can be cleared during cauterization and the operator of the robot does not have to wait.
Patient Focus
Joel Severson Blog

I have not seen many surgeries. Actually Last week was the first surgery I have every seen and I only saw a couple more that week. I am very new to this realm and awestricken by the complexity, talent of the medical staff and resources poured into it. There are is so much attention on the instruments, sanitation, paperwork, personnel training and communication between medical professionals. The goal is one thing, a successful surgery.
The surgery has stolen attention from the patient. From what I have observed, I have seen patients pulled into the Operating Room (OR) obviously nervous and reluctant to have an operation done. This patient is pulled into an OR where individuals are talking on the phone, running around getting things in place, and telling jokes with each other. I once saw a patient not yet under anesthesia and one of the medical staff removing their coverings to sanitize their genitalia. I am curious how this patient receives those activates. I am concerned that the patient’s unease is not accommodated correctly.
I would think that a patient would be more comfortable with a silent and low movement OR at least until they are sedated. Could protocol change so that the genitalia are sanitized after sedation? I think the surgery has stolen a lot of the attention from the patient and that protocol could be changed to be more conscientious to the patients themselves.
I Didn’t Know
Joel Severson Blog

I learned a couple unique things surrounding urological health that I could not believe I did not know. Living in the city and being a college student, trying to save money as many ways as possible, I decided to become an avid bike rider. Unaware to me urologist believe there is a correlation between bike riders and erectile dysfunction (ED). A urologist gave a presentation about the reasoning behind this suspicion, the logic made sense. Now of all the cyclists out there I am curious how many are aware of this and other damage that type of exercise can have on males’ urological health. Base on my small sample size, myself, not many do!
During my time at the clinic urinary track infections (UTI) are incredible common in women. From the doctors that I shadowed I gathered that somewhere around 90 percent of women will get at least one (UTI) in their life time and the reasoning for this is because they have a much smaller urethra then males. The treatment is more or lease easy, however still cumbersome. Although I am not a female, I feel like I should have known this information. Whether it be due to ignorance or a lack of education I think it would be informative to know if females know this about their urological health and if they don’t how can we better educate and prevent this type of infection?
One day we had a large about of ED patients. It is eye opening how many males have this condition and the many types of treatment. The first step they usually take is to provide an oral medication. However once that method no long works they perform a test to identify their future options. If the test goes well then, the patient has the option of do self administered injections. If the test does not go well then, the patients only option is to have a inflatable penile prostatic surgically implanted. I was only aware of the first form of treatment. The other two seems pretty extreme.
The doctors told me that when a patient tells them they smoke a pack a day that they know they have or will soon have ED. Now I don’t know about everyone else but I was not told that in my health class. Now I don’t smoke that much, mostly as a casual social activity. However, that information about smoking and ED gave me enough motivation to not want to smoke anymore. Would smoking be such a problem if people knew about the full extent of its affect. I was told that smoking is bad for me but I was never told that it could contribute to ED. That is a far better motivator then an ambiguous “its bad for me” statement. However, that made me think about what not being health does. Not just smoking but not being health in general. It would make sense that if your body is not health then the “nonessential” parts would go first.
Inconclusive Diagnostics Technology
Joel Severson Blog

This week we gave a presentation to some of the individuals working in our urology rotation. One of the themes we talked was how lots of the technology used is not conclusive in their diagnostics. This means that there are multiple medical devices but individually they provide no clear diagnostic. The down side to this is that the doctors are being crippled in their ability to treat a patient because one device does not give them a clear answer. They have to rely on that device and others or devices and an exploratory surgery to get close to the diagnostics and then can ultimately start treatment.
One example of this is when we were in clinic there were using a urine flow test and bladder scanner. However, the bladder scanner was broken. The clinic still went forward with the urine flow. The results from the urine flow were inconclusive with the bladder scanner. This forced that clinic to have all the patients come in again when the bladder scanner was fixed. This delayed treatment.
Another example of technology not being conclusive in it’s diagnostics is a CT scan and a tumor location. I saw this one surgery and similar ones to follow where the patient had to come into the operating room, be sedated, and operated on for nothing more then being able to identify whether a structure, tumor, was inside or outside of another structure, kidney or bladder. The necessity of surgery to simply identify the location of a tumor seems a bit extreme.
These examples are not scarce. It is not only a problem of streamlining the diagnostics process but is it also a problem of consolidation of technology and diagnostics procedure.
Reflection
Joel Severson Blog

As I reflect on my time in my Urology rotation I think back to how I entered the program. I was afraid that I would not be able to identify needs or that I would not ask intelligent questions. I was unsure in my abilities to accomplish the task we were charged with. It seemed like I did not have the skills to go into a certain department and identify larger problems at hand. But not that I am done with this rotation I know all those thoughts were unsubstantial.
I looked over my notes and blog post and see evidence of my task being complete. I look at the presentation my group prepared for the Urology unit and our final paper for the immersion program and am confident my group was able to identify larger needs at hand not only in the Urology department but the hospital as a whole.
This makes me excited for my next rotation. Excited to go in with more confidence and experience. I think this will increase the quality and meaning of our observations and needs assessment.
Rotation Style
Joel Severson Blog

My first week with transplant surgery was very different then my other rotation with Urology. The Urology clinic was always packed with patients and they had multiple Operating Rooms (OR) with patients constantly in them. I remember having to quickly walk with doctors between patient’s rooms and the computers, for note taking, and having that small window to ask questions. This is how I thought the hospital and clinic would operate, very fast pace and constant care delivery.
The first week in the transplant surgery unit was very different. Due to the nature of this unit they have to constantly be prepared for an emergency transplant. This forces at least some of the doctors to be available for such a surgery. Because these patients have a lot of health problems sometimes they cannot make their appointments not only that but these appointments are a little longer then the appointments I am use to. These differences give a unique environment to the transplant unit.
Donor
Joel Severson Blog

During our first week I was in a meeting discussion patients that should no longer be on the waiting list. There are strict guidelines that a patient has to follow in order to stay on the transplant list. If a patient does not follow these guidelines, then they are brought up in this board meeting to discuss whether they should stay on the list. Financial, nutrition, surgery and social services are just a few of the departments involved in the monitory of the patients on the transplant list.
What amazed me was the next meeting. In the next meeting they discussed a way to increase the possibility of patients receiving an organ sooner. This process is being implemented at several other hospitals as well. The thought is if a patient has a willing donor but they are not a match they could switch donors with another patient in the same situation. Because as of now if you do not know someone that is willing to donate an organ to you the only other option is the transplant list. However, if this process could be implemented then you would only need to have a willing donor and it would not matter if you were a match because you could just switch donors with another patient that has a willing donor and is a match with you.
Hemodialysis
Joel Severson Blog
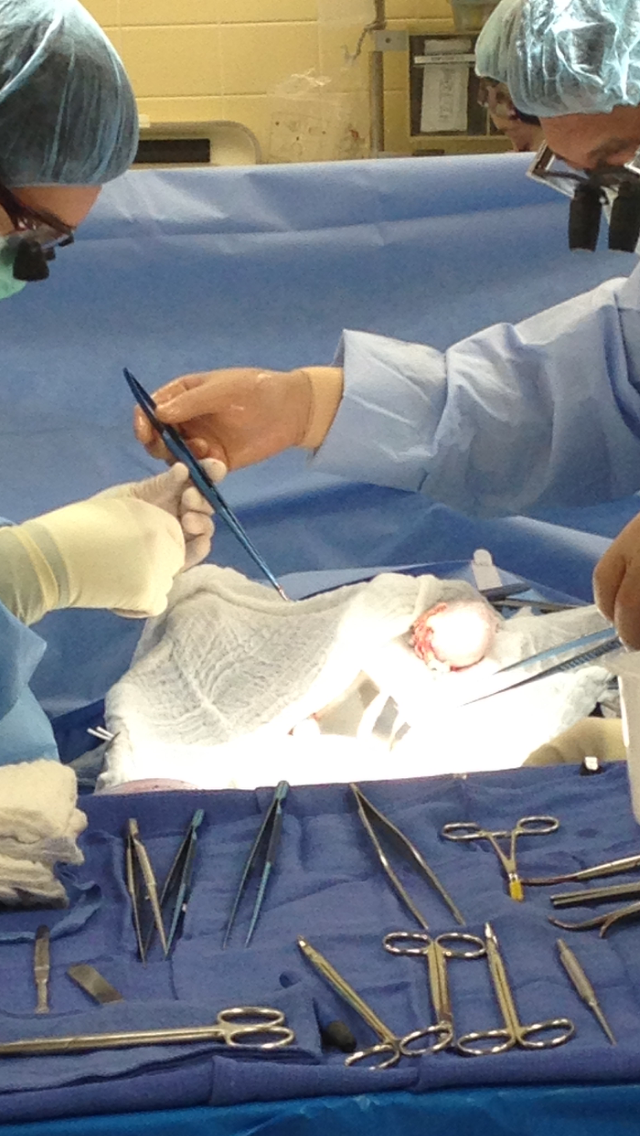
One of the clinics that we were able to see was the Access clinic for hemodialysis. Hemodialysis cleans the blood since the body can no longer clean the blood itself, which is why they need a transplant. Access is a very important part of hemodialysis because it is where the blood is removed to be cleaned and then pumped back in. However, in order to take out enough and pump enough back in the access has to be large enough. This is done by implanting a larger plastic tube or a enlarged vein in between an artery and vein.
These temporary solutions are insufficient. The artificial implants that are used for access are great because they can be used almost immediately for hemodialysis however they can get infected very quickly. Now if they used the patients own vein to make it enlarged and relocate it for access this works for a while however because of how often the patient has to go in for hemodialysis the vein gains a lot of scar tissue eventually making it impossible to use anymore.
Many times a patient has to get an exploratory surgery before implanting the type of access they are going to get. Then they have to get a surgery to implant the access. Once the access becomes infected or covered with scar tissue they have to remove it in surgery. And then go through the whole process again to gain access for hemodialysis.
Obesity
Joel Severson Blog

Laparoscopic surgery has changed the way transplant is done. Surgeries can be done with more precision and give the patient a quicker recovery. This style of surgery has also opened opportunities for obese patients. Previously open transplant surgery was not possible with obese patients because it increased risk or infection and surgery failure. We were told that UIC is one of only a few hospitals that are rising the BMI limit for transplant surgeries. It is incredible that Laparoscopic surgery has opened up this opportunity for obese patients in the transplant surgery realm.
Slush
Joel Severson Blog

There is one item in the OR that I thought needs improvement. The first item is referred to as the slush machine. This machine is actually very important. The organ that is being transplanted into the patient is placed into this machine to be kept cool. However, this machine does not have a negative feedback. This machine just gets colder and colder. This forces an employee in the OR to constantly watch the machine and turn it on and off so that the organ being transplanted doesn’t freeze.
Da Vince Integration
Joel Severson Blog
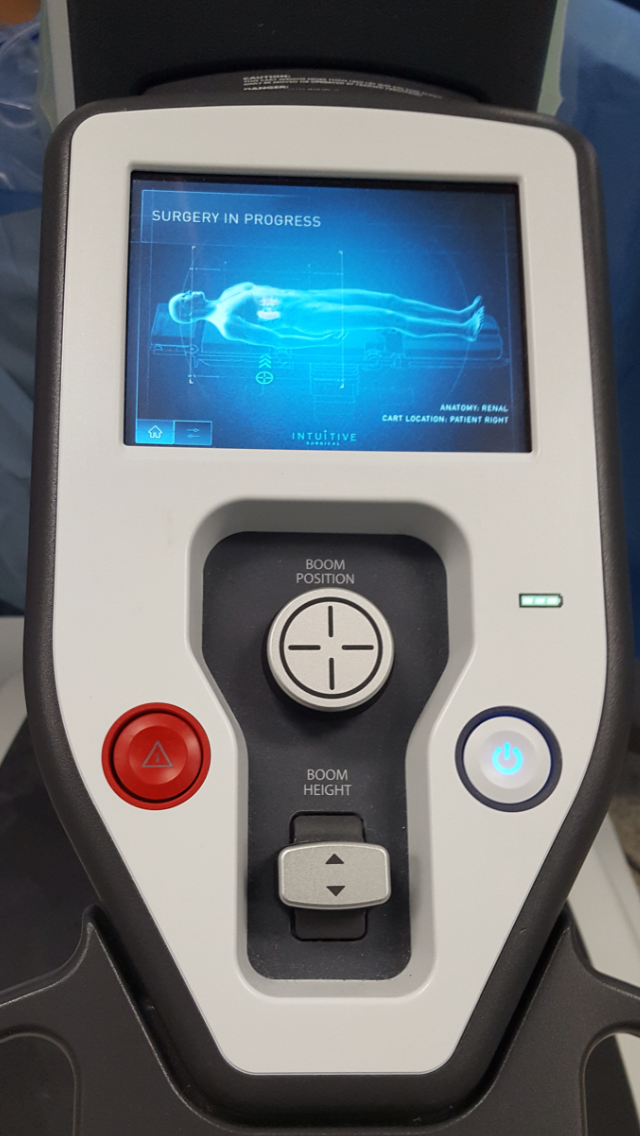
The Da Vince machine has many features that need improvement. It is an amazing machine but some of the features do not integrate the best into the OR. Many of these features I have talked about in my previous posts. There is one fault to this machine that came to my attention in one of the transplant surgery. In this surgery the transplant attending already had the Da Vince machine all set up and was ready to being the surgery. However, the anesthesiologist found out that the patients was to close to the ground. Once this problem was identified the transplant surgeons had to remove all the work that was done so the Da Vince could be separated from operating table. This wasted a lot of time because then they had to reinsert the Da Vince machine into the patient. If the Da Vince machine could be rotated with the operating table, then this would prevent the delay.
Cody Schopf Blog Heading link
-
Cody Schopf Blog
Week 1 Part 1: Beginning Urology
With an extended holiday weekend, the Clinical Immersion teams started their first rotation on Tuesday. At the beginning of the day, the participants of the programs met at the UIC Innovation Center for a brief overview of the next six weeks in the clinic along with a discussion of the expectations of both students and the program’s faculty. By mid-day we split up into our groups and made our ways to our medical departments. My first rotation would be the Department of Urology, involved with health of the urinary tract system from kidneys to urethra along with most male sex organs, which share the same piping.
Soon after finding this day’s Urology clinic at the Miles Square Health Center, the group met with Dr. Wadhwa to briefly discuss the interests of the program and immediately we were off to follow various doctors as they met with patients. From talking with the doctors I followed, I made a couple realizations fairly quickly. First was that the UIC Urology residency program was unusually long at six total years. For asking why this is, the immediate response was for practicing the surgical procedures. Before starting this program, I assumed the urologist routine was more in line with the specialties associated with internal medicine having a larger focus on lab-work. But instead one of the attending urologists I followed estimates that 80% of his time is involved with surgical procedures. Even in the clinic, the urologist is expected to do multiple digital rectal exams, prostate exams, and cystoscopies on any given day. On this first day I was able to witness by first prostate biopsy, which involves using an ultrasound probe through the rectum to visualize and obtain tissue samples from the prostate. Looking back at this procedure, my initial thought goes to “discomfort”. Aside from a local numbing anesthetic, there is little that can be done to help relieve the patient besides finishing the biopsy as soon as possible. What was really striking was the sample-taking. The biopsy probe uses a spring mechanism to quickly punch a hole into the prostate and obtain a string of tissue. Although this is supposed to be quick and relatively painless, the pressure of the action is still felt and the rather loud snap of the mechanism had an obvious depreciation to the patient’s mood. Overall, the procedure can only be described as unpleasant while multiple tissue samples needed to be taken.
The second day on rotation found myself in the clinic again with Savan as we followed Dr. Abern and Dr. Halgrimson. Similar to yesterday, many of the appointments are for follow-up visits for patients currently with, at risk of acquiring, or recovering from prostate cancer, a form of cancer that typically goes unnoticed without any symptoms until the patient is first screened for blood PSA (Prostate Specific Antigen) sometime during middle age. Along with these patients were more prostate biopsies. Interestingly, although a tumor cannot be distinguished from the prostate on an ultrasound, with clever manipulation of an MRI image taken previously, the doctor can orient the MRI image (with greater contrast of the tumor mass to prostate) in-line with the current image generated from the ultrasound probe to help determine where to properly take biopsies of the tumor. Once the two images are aligned, tracking software follows the movement of the ultrasound image and automatically adjusts the MRI image to match the new placement of the ultrasound. This nifty technique could perhaps be used in a multitude of surgical procedures to help align information from two separate images to the physician’s benefit.
Overall, the first couple of days have been an interesting first glance at the field of Urology. But the momentum is just starting to grow with the next couple of days to be in the OR watching much more elaborate procedures.
Week 1 Part 2: First Look at the OR
After spending a couple of days with urology in the clinic, I finally had the chance to see some of the more sophisticated procedures in the OR. On Thursday I followed Dr. Abern and Dr. Wadhwa along some of the longer surgical procedures, taking up half a workday a piece. At the beginning of the day, we headed to the Surgery Center where they keep all of the patients prior to operation. It’s a long room with patient beds circling three of its walls. From an outside perspective the place seems like control chaos with beds being rolled in and out along with doctors, technicians, and patient visitors constantly moving here and there. A half-hour later our patient’s bed is the next to move out and we headed to the OR.
My first impressions of the OR felt only a little less chaotic compared to the Surgery Center. The anesthesiologists were already preparing the equipment and the patient for surgery. At the same time, the surgeons were walking in and out, reviewing the patient information and prepping for sterile surgical technique. Finally, the pre-operation “time out” was called to review the surgery information and Drs. Abern and Wadhwa made the first incision. For the first procedure, I was able to see a laparoscopic adrenalectomy. A laparoscopic procedure utilizes three small incisions that act as ports into the abdominal cavity in which a camera probe and two other tools can be used at any given time for surgery. The abdomen is then inflated with carbon dioxide for greater visibility and mobility of tools. Surgical procedures involved with removing all or part of the kidney or adrenal glands can be difficult. Both organs are secondarily retroperitoneal, which in essence means the surgeon has to go through multiple layers of membranes, fat, and other tissue in order to reach the organ. This difficulty was noticeable early on as the surgeons had to gently probe the abdominal cavity, pushing between other organs in order to find the adrenal gland to be removed.
To actually cut into the tissues to reach the adrenal gland, the surgeon uses an interesting tool. On the end of one of the probes is a blunted pincer. On the inner edge of the pincer is a metal wire that rapidly heats up upon running an electrical current through the tool. When triggered, the tissue grabbed by the pincer is burned through while at the same time any vessels within the tissue are cauterized to avoid bleeding. The outside surface of the pincers is insulated from this heat in order to avoid burning the surrounding tissue. This very convenient tool, however, still seems to have its own constraints. For one, some of the larger vessels may require a second burning to fully cauterize. The tool also has some restriction in mobility. It’s a straight rod that is limited in movement based on the location of the port it used to access of the abdomen. Once inside, the surgeon can alter the angle of the probe from the port, but otherwise can only rotate the pincer. To reach any tissue that is covered by an organ, the organ has to somehow be moved aside in order to reach the desired tissue. This was a major difficulty for the adrenal gland, which is so deep within the posterior abdominal wall. As well, the cauterization of the tissue can result in smoke and steam which can sometimes fog/cover the outer lens of the camera probe. It then needs to be removed from the abdomen to be cleaned. This cauterization can also leave burned remains on the pincer, which will also eventually need cleaning to avoid impairing its cauterization function.
Overall, even with the constraints of their tools, the surgeons worked efficiently at cutting the assortment of vessels and tissue surrounding the adrenal gland. After a couple hours, the gland was finally removed and extracted through one of the incisions previously made. The team very efficiently closed the incisions on the patient and followed a routine of post-operative checks. Not an hour later and the patient was being wheeled out of the OR for recovery. The surgeons and left soon after while the remaining technicians stayed behind to finish cleaning the room and preparing for the next patient of the day.
Week 2 Part 1: Tumor Boards and AndrologyThis week I had a chance to observe a weekly meeting known as “Tumor Board” where urologists and other associated physicians meet at the pathology department in order to analyze current patient cases. As the meeting name suggests, the cases presented are patients that have or are expected to have benign or malignant tumors within the tissues associated with urology. Through these case studies, the physicians pull together any prior imaging records (MRI, CT, PET, or otherwise) to identify the suspected tumors or tissue abnormalities. From this reference, the pathologist can move to the findings from biopsies of the abnormal tissue. These biopsies are stained and presented on microscope slides via a multi-headed teaching microscope that allows up to 13 pairs of eyes to look at the slide around a discussion table. This interesting setup promotes a close discussion between the physicians in the room.
Dr. Abern headed this Tumor Board, presenting a few of his patient cases from the past week. Two of the cases looked at patients with different stages of prostate cancer and another case presented kidneys with multiple cysts with a concern for potential malignancy. Within the first case of prostate cancer, limitations in the examination were quickly brought up. The Tumor Board brings together various departments including urology, pathology, radiology, and radiation oncology who all have different preferences in the examination. As mentioned in a previous post, the prostate biopsy is not a comfortable procedure for the patient. Therefore, the urologist prefers a biopsy probe that only takes a small tissue sample from the patient which would is less painful and more convenient for the patient. This small strand of tissue, however, makes the pathological assessment difficult. A biopsy from the prostate can perhaps only be a handful of cells in width and prone to fragmenting during processing. Therefore, the pathologists would prefer a larger biopsy which would be too painful for the patient using the current outpatient procedure with local anaesthetization. So where is the middle ground in this dilemma? Perhaps there is a limitation in the current procedure or biopsy technology that needs to be addressed. A few of these points of difficulty were brought up throughout the meeting.
In the afternoon I also had the chance to visit and observe the University Center for Urology outpatient facility at 900 N Michigan Ave. Unlike the other facilities I have observed, this is a half day clinic open only once a week because of its narrower patient population focusing strictly on male reproductive health. The typical patients that seek help at this clinic are males with infertility difficulties. Many of the patients are initially referred by reproductive endocrinologists after gaining interest in in vitro fertilization. There were some other noticeable differences to the patient population. As these examinations are largely voluntary, the most obvious difference I found was that these patients were much more compliant than in other healthcare settings. There is also an obvious nervousness as the men are waiting for the doctor’s findings. This nervousness seems difficult in relieving, even with good news from the doctor. But it’s easy to understand their stress. Most of these patients have already spent months if not years trying to conceive a child without success. Regardless of how well their hormone levels are recovering or their increase in sperm motility, the only way to truly ease their stress would perhaps be that one viable pregnancy that could still be months away.
Week 2 Part 2: Profits of Robotics
Over the past couple of weeks, I’ve seen a good number of different surgeries and medical procedures for urology. The trade is fine-tuned to increasing the efficacy of a procedure while being as minimally invasive as possible. By location, the surgeons can often take advantage of the laparoscopic tools to tinker with the patient’s abdominal organs. The major advantage of smaller incisions is countered, however, by limited usability. This week I had a chance for the first time to observe a couple of surgeries with robotic assistance. Both were laparoscopic procedures, but the capabilities compared to a physician’s hands were so much greater.
The da Vinci robot systems are interesting sets of equipment. They require a fairly significant investment from the hospital. The bulky size can take up most of the OR and the price tags begin in the millions. It’s a bit surprising that these systems are ever purchased, but that’s without consideration of their potential. The system I observed was the da Vinci Si, which allowed up to 4 arms to be controlled during laparoscopy. At the same time, a second surgeon would stay at the patient’s side to manually hold other laparoscopic tools. When walking into the room mid-surgery, all you can see is a circle of equipment stands and tables around the center. Above the patient is a mass of metal and plastic elaborately set up to control an assortment of tools within the patient’s abdomen. Above even that is a halo of monitors to give everyone scrubbed in a view of the surgery. It has a different feel compared to a regular surgery, and that’s probably due to the head surgeon sitting off in a corner while using this awesome control terminal and giving commands over the speaker system.
Once set up, the robot can fly, quickly and accurately moving by the surgeon’s control. Tedious work with manual tools can be done efficiently, allowing the robotics to take on much more sensitive tasks instead. One of the surgeries I witnessed was a radical prostatectomy. The prostate and bladder are practically glued together with only thin fibrous tissue layers found between. But the robotic arms were able to precisely and meticulously separate the two organs.
However, the robotic system isn’t without its own constraints during surgery. One of the obvious issues is that the robot is big. It really is a tangle of large metal arms that crowd over the patient during surgery. This might cause some limitations in its movement due to hindrance of the neighboring arms. But more importantly it can make the work of the hands-on second surgeon much more difficult as he works around this bulk of the arms. Luckily this isn’t usually an issue as the surgeons are constantly talking back and forth. The laparoscopic tools themselves carry similar constraints as their hands-on counterparts. There is extra mobility near the end of the tool, but the tools are still limited by its port of entry. The camera as well tends to fog up and requires removal for cleaning. More complicated actions such as suturing are slowly and carefully executed in the confined space of the abdomen, but the arms have a lot of strength. The suture can sometimes snap under the stress. Only later would I learn that the da Vinci (at least the Si model) doesn’t have some form of haptic feedback, which could relate back to the surgeon if the arms are using significant force.
With all that said the da Vinci robots are worth the added costs and effort. After the initial setup and a good exchange of directions from the two surgeons, the operation advances like a well-oiled machine, able to do some of the most elaborate procedures I’ve been able to observe.
Week 3 Part 1: Moving Parts
Over the last few weeks I’ve been able to see a wide variety of activities that the urologist takes part of. One thing I’ve noticed is the common need to move across the medical campus throughout the day. The doctors could have multiple patient populations to see on any given day. The morning begins in the hospital with residents and medical students doing the rounds for the In-Patients. The group of 4 or more float from one floor to the next within the main hospital to check up on their patients, most of whom come from a recent urology surgery. Soon afterwards it’s time for the main assignment for the day either in the clinic or in the OR, and sometimes those roles last only a half day with another clinic duty at a different location in the afternoon. After those duties are over, it’s not unusual for the doctors to head back to the main hospital to do consultations from other departments as were requested throughout the day or for the residents to do the second set of rounds with the In-Patients.
By the time the day is over, many of the doctors would have come to and from several different locations on campus to meet their patients. Overall this movement from one place to the next is generally accepted by the doctors, but the time can add up. One time in particular that created a large hassle for one of the physicians I was following was during a patient consult. In the hospital, a patient was scheduled for a CT scan that required a urologist on site to overview a cystogram. For this procedure, the urologist injects a radiopaque dye into the bladder that can be used in a CT scan to discover any leaks or fistulas from the bladder. Unfortunately, when the urologist arrived at the CT room on time for the procedure, the patient was nowhere to be found. It wasn’t until after talking with the patient’s nurse that a miscommunication was discovered. The nurse originally expected for the urologist to confirm his or her ability to make it to the procedure prior to calling for patient transport. As no confirmation was made, she presumed the cystogram was called off.
At this point the urologist was in a dilemma. Either he would have to wait on site until patient transport can finally bring the patient, which could take up to an hour, or he would have to find a way to transport the patient himself. He chose option B to cut down time. But even then, the urologist had to find where the patient was located, talk to the nurse in person, and then travel around the hospital until he could find a free transport bed for his patient. By the time he could bring the patient down for his CT scan and have the CT room prepared again, the procedure was already delayed by almost an hour. From talking with the CT technicians, it seems these sorts of delays are constantly occurring.
It’s hard to say where the major setback occurred. Was it a miscommunication between the nurse and urology? Is the patient transport service too busy for a quick response? Are other transportation capabilities and equipment properly available if needed? There are many points of potential improvement, but I keep reminding myself that the hospital is composed of a bunch of moving parts, all with their own agendas and directions, and that helping out one small area of healthcare might have unexpected benefits to the system as a whole.
Image from Wikimedia.org
Week 3 Part 2: Lost in Translation
We are at the end of the first three weeks of the clinical immersion program, which leads to the end of our first department rotations. The last three weeks of urology has been an interesting look into a field I didn’t know very much about prior. From only these few weeks I’ve been able to see a broad range of the activities related to the practice. At the clinic these ranged from the simpler follow-up visits to more serious meetings involving the risks of cancer to more voluntary appointments looking into patient fertility. Many of the procedures are done via outpatient appointments that are over in five minutes. Other surgical procedures relied on more advanced equipment and techniques including the usage of the da Vinci robotics, laser lithotripsy, and different imaging strategies. I was even able to witness a more specialized procedure at the UIH, a male-to-female gender reassignment surgery partnering urology with plastic surgery that lasted all day and went into the night before completion.
However, regardless of the different activities associated with urology, communication with patients is a potential struggle. The University of Illinois health system is one of the top billers of Medicaid in the country and its patient population is reflected through this with a very large percentage of patients incapable of speaking English. Fortunately, there are staff members within the urology department, nurses or doctors, that are able to speak Spanish or a few other languages, which can help streamline patient care for these non-English speakers. Yet, most of the time the doctors must rely on telephone interpreting. This phone translation system usually works very well, and its use is well established. Sometimes, though, there are unique circumstances in which a typical phone translator cannot be used. This week I observed a follow up appointment with a Spanish-speaking patient who was also deaf. This was an already established patient in the UIH health system, but the urology staff were stumped on how to communicate with the patient. How does one find a translator to sign Spanish? Ultimately the nurse practitioner heading this appointment had to rely on writing down the questions and instructions to the patient during his appointment. Luckily the follow-up appointment brought up no major concerns or other questions from the patient, allowing for a somewhat smooth interview. With that said, there was still a lot of mouthing of basic English and Spanish words and rudimentary gestures to give the patient instructions.
So what exactly is available for the health practitioners when there are such major restrictions to providing care to a patient? All of the clinics I visited over these past weeks had fairly new VoIP phone systems in every room. The phone console has a small monitor and webcam that in theory could be used for video calling. Yet, none of the hospital staff working at the clinic or that I have talked to knew how to set up a video call with the console. Even if they did, they weren’t sure if the phone translating services used by the health system were capable of video calls or had a translator who could sign Spanish. In theory, there is possibly a way to properly translate a conversation with this deaf Spanish speaker. But this experience showed me that, although technology and resources might be made available to health providers, if the staff aren’t aware of the full uses of equipment or services, then those resources could be wasted, much to everyone’s disappointment.
Week 4 Part 1: First Look at Transplant Surgery
This week begins the second rotation in the Clinical Immersion Program, which brings a new group of student observers together and a new medical department. To begin our exploration into the department of Transplant Surgery, Dr. Hoonbae Jeon introduced us to the origin and current use of some tools used in transplant surgery. The presentation explored hemostats, current electrical cauterizing tools, and methods of organ preservation and transport. His consensus of all these tools is that everything could still be improved. The discussion impressed upon us the constraints from a surgeon’s perspective: costs, ease-of-use, capabilities, precision, reliability. Although medical equipment is rapidly evolving, it’s hard to check off all the boxes, especially when each physician has his own preferences and ideas.
One example that comes to mind are the current electrical cauterizing tools that are commonly used in surgery. These tools are various forms of electrodes used to run an electrical current through tissue, essentially acting like a cauterizing scalpel “slicing” through the tissue it burns. It can otherwise be used for spot cauterization to stop any bleeding from the cuts made. In general, these tools are much bulkier compared to the classic surgical tools that people know: metal scalpels, hemostats, forceps, etc. But it is the ergonomics of those classic tools that Dr. Jeon would like to repurpose. Those tools, he argues, almost become extensions of the surgeon’s hands over years of practice since the earliest dissections in medical school. That familiarization, that finesse, is hard to reproduce with these electrical cauterizing tools, the smallest of which is similar in size to a soldering iron. For most surgeries this doesn’t seem to be a major issue, but transplantation requires tissue preservation, which can be a delicate process when working with the smaller vessels attached to or within these organs. Finer work can be done with robotics, but that isn’t always available. These surgeries are executed as fast as possible as every minute counts from the moment the organ donor is called. Robotics may not always be available or plausible given the window of opportunity for organ transplantation. So what can be improved? Smaller, portable instruments tailored to the surgeon’s preferences could shave off more than a few minutes to surgery completion. When some of these organs have a transplantation window of only a few hours, those minutes can make the difference.
Over the next three weeks I’m hoping to have the chance to see the transplantation process from beginning to end. My previous three weeks’ experience tells me that delays in the OR are bound to happen. But it will be good to see just what are the true limiting factors in play during transplant surgery.
Week 4 Part 2: Screening Patients
This Friday I had a chance to observe a weekly meeting in the department of transplant surgery. Starting at 7:30 in the morning, a group of thirty or so members associated with kidney and pancreas transplantation come together to monitor and screen potential transplant recipients. What I quickly learned was that transplantation screening is no easy process. To begin with, the meeting was composed of multiple professions including the transplant surgeon, a cardiologist, multiple nurses and administrative workers, pharmacists, pathologists, social workers, and psychiatrists. Each of these members played a part in the screening process.
During the meeting, the talk would consider one patient at a time and determine their transplant status: Active (waiting for transplant/donor), inactive (on hold till concerns are addressed), or closed. For this review, the staff discuss the patient’s physical wellbeing, any contraindications from other health issues, psychological wellbeing, and likelihood of finding a donor organ among other aspects. Just one problem in the patient’s profile can completely halt any progress for transplantation. Most of the candidates reviewed were placed on the inactive or closed categories, often for similar reasons such as comorbidities in obesity or heart failure, the usage of certain illicit drugs that puts the patient at risk during surgery, or complications in mental health.
Ultimately, the main constraint for most of these transplant patients is the absence of a suitable organ donor. Living donors are common in kidney transplants, but the majority of kidney transplants are still from cadavers. Finding a suitable donor then is matter of chance. However, after the meeting was over, the head surgeon at the meeting discussed the idea of starting a Donor Swap Program at the university. The proposed program would offer a one-to-one swap between two hospitals. If two living donors are found suitable for the other donor’s potential recipient, then the two pairs of donors and recipients would be incentivized to “swap” the donated organs to everyone’s benefit. By expanding this program to multiple hospitals, the likelihood of a suitable donor swap would be greatly increased. This seems like a very interesting method to help resolve the shortage in suitable organs.
But it seems strange to me that this sort of program isn’t already in place. Kidney transplantation has been possible for over half a century now and the suitability of organs has always been a concern. That said, programs like this are already implemented. However, the occurrence of these programs seems to be specific to only a few hospital systems around the country. Again, it seems strange that such a program isn’t more pervasive in healthcare, but perhaps this goes back to the common issue brought up since the beginning of this immersion program: That of poor communication between healthcare systems. In many ways, it feels like hospitals are fairly exclusive, acting fully independent of any other healthcare systems nearby or otherwise. But I have to wonder if programs such as this Donor Swap initiative, which focus on the community aspect of healthcare, are strongly crippled without the necessary cross-talk between the healthcare communities. It might be time to address this issue. We are well into the 21stcentury, but it amazes me how reliant hospitals still are on the fax machine for obtaining medical documents from outside the healthcare system.
Week 5 Part 1: Back at Robotics
After some time in the clinic, the team was able to watch a few kidney transplantations. Because the body normally begins with two kidneys, it is possible two having a living donor along with kidneys from a cadaver donor. Regardless of its source, organ transplant surgeries definitely have import in the OR. A living donor is scheduled at the beginning of the day 6:30 sharp and the recipients are prepared well ahead of the organ being available. There is definitely the coordination to expedite the procedure and maximize the organ’s viability.
For these procedures, the da Vinci systems are used most often. Unlike previous surgeries seen, these transplant surgeries usually have two attending surgeons. Like the usual robotic assisted laparoscopic surgeries, one surgeon is on the console, controlling the robot. The other surgeon however does something I wasn’t able to see in the urology department. The second surgeon’s main hand is wrapped in a surgical drape and pushed into the patient’s abdomen to help assist the robot. The main purpose of this is to easily remove the kidney once it is cut away from the body, but there was definitely a lot of added benefits throughout the procedure. The hand is much nimbler in pushing away tissues and orienting the kidney for the robot.
However, the benefits for the surgeon on the robot come at the expense of the surgeon at the bedside. In order to get the hand invested in the patient’s abdomen, the surgeon must lean over the bedside for multiple hours during the procedure. Even with a chair, the surgeon was clearly not comfortable for the main duration of the procedure. On top of this, the bedside surgeon has to always be aware of the moving robotic arms, which can be right beside his arm or face. Of even more concern from at observer’s perspective is the close proximity of the surgeon’s hand, covered only in surgical gloves, to the robotic instruments. Although I know the surgeons on these transplant procedures are experts at the da Vinci system, it still can be worrying seeing the bedside surgeon’s hand so close to needles, sharps, and cauterizing instruments throughout the procedure.
Overall the robotic system definitely helps streamline the entire procedure, but supplemental instrumentation might be needed to help the assisting surgeons work around the added difficulties of the robot.
Week 5 Part 2: Accessing Hemodialysis
Transplant patients are composed mainly of those with kidney failure. Although there is a high demand for all organs currently used for transplant, the availability of living donors and usually 2 kidneys from a cadaver means access to a kidney is somewhat easier than say a heart or liver. But there is still a major shortage. To get by without a kidney transplant, the many patients with chronic kidney disease have to rely on dialysis to filter the blood in place of a functioning kidney. Hemodialysis isn’t easy. To stay in good health, patients usually come into a clinic multiple times a week for hemodialysis. They are hooked up to a large machine for up to 4 hours at a time and their blood is circulated out and back in one cleaned. To minimize the time needed for hemodialysis, the machine requires access to larger vessels. Veins are easier to find, being close to the skin, but they lack blood flow. Arteries have that blood flow, but are found deeper in the body. To remedy this issue, the transplant surgery department created an AV Access, which is an artificial connection between are larger artery and vein, which will increase the blood flow to the vein needed for hemodialysis. AV Access can be created in two ways, by a direct connection of artery and vein called a fistula or by engrafting a, usually teflon, tube between the two vessels.
There are several benefits and problems associated with the fistula method, but this blood will be discussing the troubles of an artificial graft. A fistula is usually the ideal method of access, but can often be unsuitable for the patient. These polymer grafts make an arterial-venous connection more possible, but are artificial. The major difficulty of these grafts is it’s guaranteed expiration. The commonly used polymers like PTFE, i.e. teflon, are not suitable with the constraints of hemodialysis. Each hemodialysis requires needles entering the vessels to circulate and clean the blood, and teflon can’t properly handle these pictures. It’s an artificial avascular material that cannot self-repair. Those pictures, occurring multiple times a week for years and years, eventually wears down the integrity of the graft.
It’s is almost guaranteed that a long term hemodialysis patient with an AV graft will have to undergo surgery again after a few years to replace the graft. A replacement will usually also be at a different connection point, but potential areas of an AV access are limited. Overall it’s a losing battle for hemodialysis patients.
Week 6 Part 1: Visiting the ICU
For transplant patients, the transplant surgery itself is obviously incredibly important, but it takes up a very small portion of their time in the hospital. The transplantation team has its own area of the hospital known as the Transplant ICU where patients associated with organ transplant are kept for extended periods of time. These patients could be waiting on the transplant list, be recovering from a recent surgery, or be returning patients that require constant care and surveillance because of their transplant. All transplant patients are under immunosuppression, which means that certain lesser complications become much more dangerous. If one of those patients are admitted into the hospital because of any infection, they are almost certainly taken directly to the Intensive Care Unit. It’s simply too big of a risk otherwise.
There are multiple ICUs within the hospital, but they all have similar routines. Unlike other areas of the hospital, the nurses in the ICU never have more than two or three, patients to monitor. This allows them to give a much better level of patient surveillance. And this surveillance is needed. One of the physicians I talked with noted that instructions for ICU patients will almost never last a full 24 hours. Changes are constantly made based on how the patient is fairing at any given time. The overarching patient instructions are mainly directed by the daily morning rounds, which brings together transplant surgery, nephrology, pharmacy, and other consultants to go over the patients currently kept under the transplant unit.
With this system in place as is, there are some components of the ICU workflow which can cause difficulties. Because of the large number of hospital staff that follow the ICU at any time of the day, there is a lot of hand-offs from one staff member to another or because of a shift change. On a few occasions, this has led to certain patient instructions for one patient to be forgotten by the new staff members taking over for the next shift. Blood work and urine analyses are needed often multiple times a day and can be crucial for monitoring the patient’s health. Specific measurements could get lost in the fray, and it’s up to the morning rounds to make sure everything stays on track. Easier methods of communication for patient hand-offs could be useful.
How the ICU manages its patient numbers can also be tricky at times. Hospital beds are categorized based on the amount of care needed, with the ICU holding the most care. Due to the limited number of beds in the ICU, newer patients can sometimes bump older patients that may no longer needed the full care of the ICU to a lower level of supervision in the hospital. Although these patients are typically already on track to be moved over, the added pressure to admit a patient in a more critical condition can sometimes be non-ideal for the care of other patients. Overall, the ICU is a very dynamic operation in the hospital with a lot of moving beds and staff members to keep everything on track.
Week 6 Part 2: Observing the Hospital Rounds
Rounding is a common routine for any department that has patients staying in the hospital. For transplant surgery, there are daily morning rounds that bring together surgeons and nephrologists along with a team of residents, pharmacists, and nurse practitioners. A consultation with a physician from infectious diseases is also common given that the majority of patients are under immunosuppression for their transplant. Rounding begins with “Table Rounds”. It’s a whirlwind of information during these meetings as each member says their piece about the patient currently assessed. Overall, the individual pieces of information with the meeting headed by the attending surgeon and nephrologist come together nicely to quickly, but smoothly, run over the list of current patients. After about an hour, the group moves on to walking rounds as they visit the individual patient beds. Rounding typically occurs without major bumps or hurdles, but there are still areas of improvement.
Timing is an interesting issue when it comes to the morning rounds. Rounding cannot officially start until one of the attendings has arrived. There is no official start to the morning rounds, but generally is scheduled for some time between 8 and 9 o’clock. The transplant unit members know when rounds are scheduled for the day, but the actual arrival of the attending physician and his or her readiness for the meeting is not easily predicted. Although the wait isn’t usually long – no more than 15 minutes perhaps – and the members can often find something to do in the downtime, it is still interesting the see a half dozen medical personnel more or less on standby till the head physician arrives.
The other notable observation is the attendance for these rounds. As mentioned previously, the number of members in these meetings is sizable for the transplant unit. Yet, there is definitely a need for each of these people. Transplant care is inherently multidisciplinary due to the high level of care needed to keep these patients and their new organs happy. As it’s an academic hospital, each of these components to the transplant unit will also have their own students and residents. In general, it’s a sizable group of people which makes the meetings highly informative but can be quite daunting during the actual walking rounds. In the eyes of the patient, it can be quite uncomfortable having more than a half dozen people present during the daily interview any subsequent physical examinations. On more than one occasion I’ve seen the patient noticeably tense or stunned by the flock of white coats entering their room. However, this is one of the small sacrifices expected in admission at an academic hospital. But I have to wonder if a protocol should be implemented to limit the number of people that actually enter the patient room at any given time. White Coat Syndrome is a common concern and the added stress by the sheer number of observers can make some parts of the examination more difficult and the overall patient satisfaction lowered.
Charlotte ter Haar Blog Heading link
-
Charlotte ter Haar Blog
Week 1, Part 1: An Introduction to Anesthesiology
Charlotte ter Haar Blog

Thanks to the long weekend celebrating America’s Independence, we started the Clinical Immersion Program on Tuesday. All program participants (Innovation in Medicine/IMED students and Bioengineering students) met at UIC’s Innovation Center for an orientation to the Clinical Immersion Program. We discussed teamwork, expectations, hopes, fears, logistics, and did a little improv, which is always fun. Tuesday afternoon, I started in the Anesthesiology clinic. The Anesthesiology & Surgery departments took advantage of the long weekend, and the operating rooms were closed on Tuesday for cleaning/organization. Therefore, on Tuesday afternoon, Dr. Edelman showed us around the department. He took us to the Surgicenter, which is where patients are prepped for surgery, a small procedural room (not a full-on operating room), and the recovery room. Since the operating rooms had been closed, the Surgicenter and recovery room were also both empty.
Above shows the surgicenter, where patients are prepped for surgery, and an Anesthesiology cart in a small procedure room.
Wednesday morning was when the real fun began. We started off the day in the conference for residents, which gave an overview on Airway Management. Dr. Banchs discussed several factors pertaining to airway management, including the anatomy and innervation of the airway, differences between adult and pediatric airways, predicting whether it will be difficult to mask ventilate or perform a direct laryngoscopy, and a comparison of different blades used for intubation. Since managing the airway is such a key component of the specialty, it was a great lecture to kick off this rotation.
Following the lecture, we split up to pair one IMED/medical student with one bioengineering student, so we wouldn’t be adding four people to any one operating room. Tooba and I saw three neurosurgical procedures. A fourth-year anesthesiology resident and a fourth-year medical student on his anesthesiology rotation were also both in the operating room for all three procedures, and they were really helpful in explaining all the various parameters that the anesthesiologists track on their monitors, as well as some of the physiology, physics, and pharmacology behind those parameters.
The first procedure, we saw a patient who had a morphine pump that delivers morphine to her spinal cord for pain management. The battery dies after 6-7 years, so it was time for her to receive a new pump. The resident knew that previous anesthesiologists had difficulties intubating her, so he used the GlideScope from the beginning of the procedure, which is a video laryngoscope that allows for real-time video feedback. It was interesting to see the intubation from the GlideScope screen, and with this device, the resident intubated the patient without difficulty. There was a tech advisor from the biotech company that produces the pump – I didn’t catch who – but she was having trouble activating the pump prior to having the surgeons place it in the patient. Eventually, she asked for the LED lights to be turned off because she was concerned that they were interfering with her procedure.
One really neat feature of the anesthesia monitors is that there is a beeping that corresponds to the pulse oximetry, but the beeping changes pitch based on the saturation. With so many numbers to watch, I thought it was cool that there was also some audio feedback.
There is a device called the Bair Hugger that is used to keep patients warm during surgery – operating rooms are often quite cold, which is nice for the surgeons who are working hard, but it is important to keep the patient warm. The resident mentioned that it takes an hour for the Bair Hugger to work, so it was not used in any of the procedures that were expected to take less than 60 minutes. However, an attending came in to one of the later surgeries that was supposed to take 45 minutes and put it on the patient just before the surgery started. It is interesting to see these variations in practices, and it makes me wonder which choices are evidence-based and which are based on what a physician is used to doing.
This rotation is off to a great start, and I am looking forward to seeing other facets of this specialty. I hope this post didn’t put you to sleep!
Week 1, Part 2: Da Vinci on the Mind
Charlotte ter Haar Blog

“There are three classes of people: those who see. Those who see when they are shown. Those who do not see.” – Leonardo da Vinci
After my first experience watching the Da Vinci robot in action, I find myself reflecting on the famous artist/innovator/intellect’s insightful words on observations. I strive, both in this program and throughout my career, to fall into the first class that he mentions. Now, on to my observations…
On Thursday we sat in on the resident’s conference about inhaled anesthetics. Following, conference, I watched a kidney transplant surgery, which took about six hours. The surgery was laparoscopic (minimally invasive), using the Da Vinci robot. The surgery itself was really interesting to watch, but it was also interesting to see how different circumstances in a surgery can change the job for the anesthesiologist. For example, in laparoscopic surgeries, the patient’s abdomen (in this case) is insufflated with carbon dioxide gas. This allows the surgeon a space within the body to navigate the instruments for the surgery. Some of the CO2 from the abdomen can be absorbed into the tissue and removed by the respiratory system, but this can drive up to CO2 readings on the anesthetic monitoring. Knowing this, an anesthesiologist is more comfortable seeing slightly elevated CO2 readings during laparoscopic surgeries.
During the kidney transplant, the patient was in the Trendelenburg position (see image below, from Wikipedia), which allowed the surgeon the best access to the surgery site.
In this position, the weight of the abdominal organs slides up to rest on the diaphragm. Since a patient is not breathing on their own when they are anesthetized, the anesthesiologist ventilates them using positive pressure breathing. Note – our normal breathing is negative-pressure breathing – we create a negative pressure in our lungs that drives new air in. When the patient was in Trendelenburg position, it was even more difficult to positive pressure ventilate, since you have to push the diaphragm against more weight. Placing the patient in this position is best for the surgery, but it introduces an additional challenge for the anesthesiologist.
From a medical standpoint, I thought it was very interesting that neither of the patient’s existing kidneys were removed. Prior to seeing the surgery, I assumed that one kidney would be removed so the transplanted could could replace it. Rather, the vessels of the transplanted kidney were sewn onto the external iliac artery and vein (see image, from Mayo Clinic website).
This is logical; it would take longer to remove an existing kidney and shorter surgeries typically mean better patient outcomes. In addition, if the patient has any remaining kidney function, it does not make sense to remove their original kidneys.
At the end of day on Thursday, Dr. Edelman gave us an overview of the stages of anesthesiology and situations in which different levels of anesthesiology are indicated. The four basic levels are:
- Anxiolysis
- Monitored Anesthesia Care (MAC)
III. Deep Sedation
- General Anesthesia
At different levels of anesthesia, patients have varying abilities to maintain their own airways, feel pain, and respond to stimuli. It was helpful to get an overview of these stages to better understand what we are seeing in the OR.
Week 2, Part 1: Where does the Anesthesiologist Belong?
Charlotte ter Haar Blog

In the standard operating rooms, the surgeon and anesthesiologist typically work out a place for the anesthesiologist to “set up” that will work for both parties. Typically, this is behind the patient’s head, but adjustments are made if the surgeon is operating on or near the head. I have been surprised by the two experiences I’ve had outside the standard ORs: in the “embo” lab and in the “cath” lab. In both of these rooms, there is still a designated space for the anesthesiologist, but it seemed to be far from optimized. In the embo lab, the location of the anesthesiologists meant that tubes and cords were stretched across the room (see image above). In the cath lab, the anesthesiologists could not see the screens that the interventional cardiologists see, meaning that they did not always know what was going on in the procedure. In addition, the anesthesiologists’ arterial line was removed in order for the interventional cardiologist to gain access to the arterial system, which meant that the anesthesiologists lost their blood pressure readings on the monitor, as well as the “cardiac index” reading. Both of these measurements are important for patient monitoring. I find it surprising that in these operating rooms, where patients are often in critical condition, the anesthesiologists often seemed to have to carve out a niche for themselves within the room. After all, the anesthesiologist is an essential member of the patient’s care team!
Week 2, Part 2: There are 100 ways to skin a cat
Charlotte ter Haar Blog
Today’s blog post will focus on two quotes that I wrote down while observing the anesthesiology team this week.
“Just as there are 100 ways to skin a cat, there are 100 ways to manage a patient well under anesthesia. While a lot of the anatomy and pharmacology can be considered cold, hard science, how to actually manage your patients is where the art of anesthesiology comes in.” – 4thyear resident at UIC.
I felt like this conversation really brought new insights about my observations over the past two weeks. Often I have wondered why an anesthesiologist is making a certain decision – how do they decide at what oxygen level they will ventilate the patient? Is it better to try and push the oxygenation level closer to room air, or are there no problems with keeping it at 50%? Why do they choose one muscle relaxant over another? If you can adjust either the respiratory rate or the positive-end-expiratory-pressure and get similar results, why do you pick one over the other? I have found that the anesthesiologists we have been observing care greatly about their patients, and understand all of the measures that they are taking to provide quality care, and yet, are not always able to say why they choose one path over another. Maybe it would be possible to do more research on which methods are “better” in certain situations, but at the same time, I do see how many different variables they are attempting to control at once, and I wonder how effective such a study would be in truly ascertaining variable patient outcomes.
The second quote that really stuck with me this week was from a conversation with Dr. Feld, an attending in anesthesiology. While discussing innovation with him, he said:
“If you want to get to the real root of the problem, come up with solutions to avoid surgeries.” – Dr. Feld, UIC Attending in Anesthesiology
Talk about problem-based thinking! I love this quote because he is thinking about the big picture, he is not limiting himself to an idea that surgeries will always be a necessity in medicine, and he is truly thinking about a world that would be most ideal for patients. I also love that it is problem-focused. I have spoken to several residents and physicians who suggest devices that they would like to have, that they perceive would improve their delivery of care – whether through more accurate peripheral nerve blocks, by improving efficiency, etc. I find that it is a constant struggle for me, as someone is describing a device they want designed, to try and delve deeper and to understand the root of the problem. Why do they want this designed? What is the problem they are trying to solve? How would this change the delivery of healthcare for the patient? For the residents? For the physician?
That’s all for this week! I am looking forward to one more week with Anesthesiology.
The image: We saw a scoliosis surgery today, where the patient must be in prone position to allow the surgeons access to the spine. I was interested in the piece of foam that the patient’s head rests upon – it as a cutout for the face, to prevent ocular injury from pressure on the eyes during a long surgery. It also has a cutout in the side of the foam (not viewable in image above) that allows the breathing tube to pass through the foam.
Week 3, Part 1: Simulation and MRIs
Charlotte ter Haar Blog
We had the opportunity to see the anesthesia residents in the simulation lab last week, and I am still struck by how advanced and yet insufficient these simulators are. They can cough and blink, they have heart, lung, and bowel sounds, and you can put IV fluids in them, and yet I still don’t think they are adequate for training students. While I think there is huge value in using simulation equipment, the faculty at UIC seems to unanimously accept that the simulators are not realistic for practicing intubation. As a disclaimer – I may be biased, as I worked on a simulation project for teaching intubation in my undergraduate curriculum – but I find it so interesting that students are asked to learn skills on manikins that do not mimic the experience on a real human patient. If anything, I fear that students will learn to use too much for a given procedure, since the mouths are difficult to open and the skin is hard plastic. I think the idea behind simulation equipment is genius, and I am curious about the role that virtual reality will play in medical education & medical simulation. I predict that the field of medical simulation will look very different in 15 years!
Our team also went to MRI for a half day to observe the role of anesthesia for MRI procedures. Most young children who need an MRI will get anesthetized – it can be quite scary and overwhelming to be in that machine for 45 minutes, and the MRIs can be useless if the patient moves too frequently, which can also be a challenge for pediatric patients. As such, the department now schedules all pediatric MRIs for the same day, so they know that they will have a pediatric anesthesia team at the ready. This significantly speeds up the entire process! It’s always satisfying to see schedules worked out like this in the hospital, ones that truly improve efficiency. Adults who know that they are claustrophobic are also often scheduled on the same day and may be anesthetized. It was really cool to see how many non-ferrous devices and equipment have been specifically designed for the MRI rooms. In our discussion with the MRI technician, we found out that one technology that is still lacking is an MRI-safe pacemaker. There are certain pacemakers that are “MRI-compatible” or “MR – conditional” and allow patients to get MRIs under very specific conditions (according to the MRI tech, patients with these pacemakers can typically get MRI scans of their brain but not much else), but if a patient does not happen to have one of those MR-conditional pacemakers, they cannot get an MRI.
Week 3, Part 2: Pain Clinic & Patient Communication
Charlotte ter Haar Blog

We spent one day in the pain clinic, which deals more with patients with chronic pain, rather than the acute pain involved with surgery. The pace was very different in pain clinic – it was the most patient interaction we had on the whole rotation, as it was an outpatient clinical setting rather than the operating room. One thing that I found frustrating was the lack of patient education and communication. For example, there were two procedures cancelled because the patient had only stopped taking their blood thinners the day before they came into clinic. The attending that day prefers that the patients are off their blood thinners for three days before the procedure, as there is risk of bleeding into the thecal space. However, this is not a set requirement for this procedure – the fellow in the pain clinic told us that the society for regional anesthesia sets guidelines every couple years, but that the guidelines are not necessarily evidence/research-based. Therefore, what happens is largely provider/attending-based – that is, if a different attending had been there that day, maybe those two procedures would not have been cancelled. A few thoughts on this:
- It is very reasonable for a provider to only do a procedure on a patient that they feel is a comfortable and safe procedure.
- Why are the guidelines not evidence-based?
- Why is there no standard of practice within a given pain clinic for how long patients must be off their blood thinners prior to these procedures?
- Why are patients not told to stop taking their medications three days ahead of time, if that is what the provider is expecting?
It was especially frustrating to see this, as one of the patients was an inmate who had two guards escorting him. That wasted time for all three of them, not to mention to providers that saw him that day. I also imagine that rescheduling that appointment is even harder as an inmate.
Photo: I forgot to take any photos of myself in pain clinic, but here is one of Emil with a partial skeleton.
Week 4, Part 1: The Elegance of Interventional Radiology
Charlotte ter Haar Blog

I have started my second rotation in Interventional Radiology (IR), and I am already impressed by this specialty. Once again, I can tell that I got lucky with a fabulous mentor – Dr. Bui has been great at getting us acclimated to the department & understanding the basics of his specialty. In addition, everyone that we have interacted with has been incredibly helpful and happy to explain the procedures to us. On our first day, Dr. Bui was talking about the development of interventional radiology as a field and why he likes it, and he said something quite striking – “If you see a procedure that is not elegant, there is a better way to do it.” His words have stuck with me this week, and give a perfect illustration of my impressions of IR – the procedures all seem quite elegant. It is fascinating how much they can help a patient with such minimally invasive procedures. The one challenge that seems to come up in procedures is the navigation of the catheters and wires through the vasculature. Sometimes the physicians have to take a few passes to get into the right vessel, and certain procedures offer additional challenges. For example, in a case with portal hypertension, the interventional radiologist may want to insert a balloon catheter into a shunt vessel – a vessel that is normally not there, but has opened up to allow the backed-up venous blood from the portal system to return directly to the heart without passing through the liver. These vessels sometimes have 90 degree turns, and the balloon catheters are quite stiff, making it difficult to navigate that turn. Moreover, these shunt vessels are not typical vessels, so they are often more delicate. Note: the image above, from Boston Scientific, shows a wire coil being inserted into a vessel through a micro-catheter, a procedure we saw performed to occlude shunted vessels.
Week 4, Part 2: Navigating 3D space with 2D imaging
Charlotte ter Haar Blog
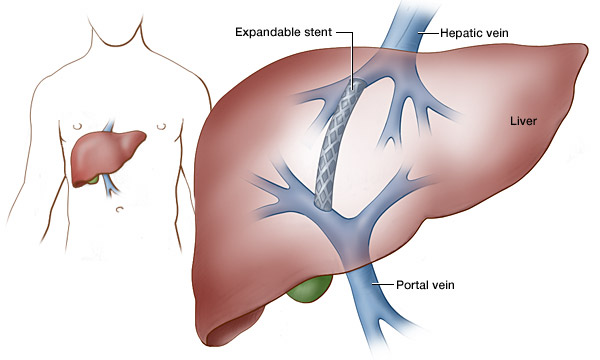
Lately, I’ve had Pokemon Go on the mind. I am fascinated by the implementation of augmented reality and what it could mean for imaging in medicine, especially in Interventional Radiology. I have been struck by the lack of dimensionality in the imaging techniques used in IR. That is to say, in any given image, an entire dimension is lacking – the images have no depth. To me, this seems like a limitation, as our anatomy is unquestionably three-dimensional. For example, in a transarterial chemoembolization (TACE) procedure, the Interventional Radiologist must find the arterial feeder to the tumor, but with the two-dimensional imaging, it can be difficult to discern which exact artery is actually going to the tumor. If the imaging of the arteries also had depth, this would be far easier. While we saw a cone-beam CT used once; however this was the exception, not the norm. The cone-beam CT gave more of a three-dimensional view of the liver (in that case), but the software took a very long time to process the images and generate the “3D xray.” Another example where 3D imaging would be an asset is the transjugular intrahepatic portosystemic shunt (TIPS) procedure. In this procedure, a shunt is created between the hepatic and portal veins, the bypass the liver. While the interventional radiologists can see a 2D relationship between the hepatic and portal veins, they cannot see depth, so creating the access point between the two veins can be very challenging.
Being able to read images and perform the procedures that I have discussed in this post are two components of the “skills set” of an Interventional Radiologist. They require training, practice, and finesse. Sometimes I wonder whether physicians (or any skilled worker, for that matter) feels a conflict between the development of a new technology that advances their field, but may make some of their current skills less relevant.
Image: From VIRChicago, showing the placement of the stent in a TIPS procedure, between the hepatic and portal veins.
Week 5, Part 1: In the vein of IR
Charlotte ter Haar Blog

We had the opportunity to hear from a company rep for Angiodynamics about their “VenaCure” laser for ablating superficial varicose veins. Essentially, a laser is inserted into the vein & then turned on while slowly pulled out of the vein, and the vein becomes destroyed. The blood that was drained from this region will find a new way back to the heart through deeper veins. Varicose veins are the result of venous valve insufficiency, which causes blood to pool in the veins near the feet, and builds up pressure on the walls of these insufficient veins. While the laser treatment is interesting, it got me thinking about deep vein valve insufficiency. You cannot ablate a deep vein with valve insufficiency, so there are currently not many options, other than monitoring and attempting to ameliorate symptoms & prevent the formation of ulcers. The technology for artificial heart valves is tremendous and widely explored – while an insufficient heart valve may be more life-threatening than insufficient venous valves in the legs, I am interested by what I perceive to be a relatively unexplored space for treatment options.
Image: From Diagnostic Imaging Services, showing the before and after of superficial varicose vein treatment using the VenaCure EVLT.
Week 5, Part 2: Repeating procedures
Charlotte ter Haar Blog
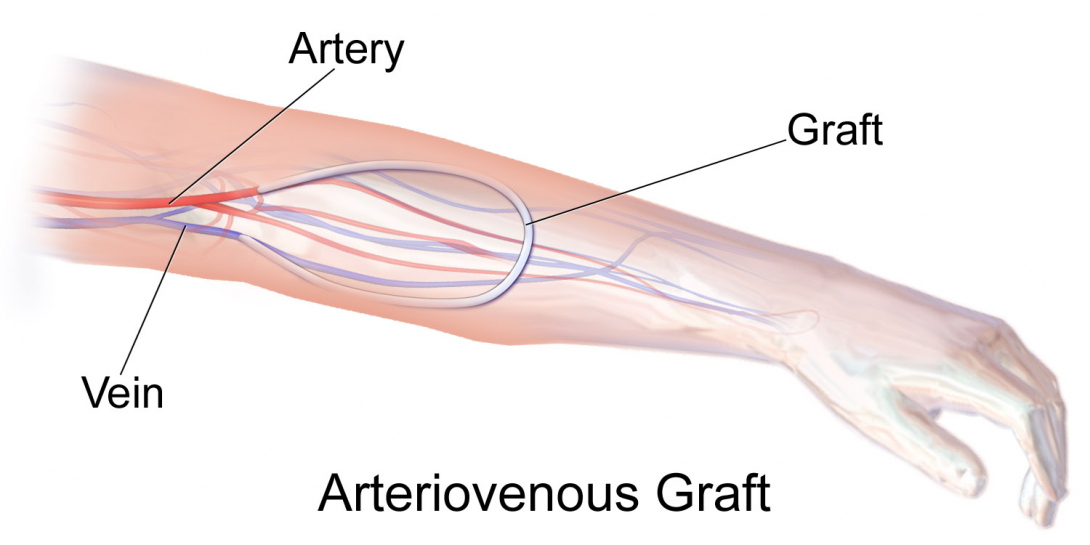
We have seen several dialysis patients in IR, which was a surprise to me at first. Patients who receive hemodialysis often have a connection made between their artery and vein – called an AV (arteriovenous) graft or fistula. An AV fistula is the direct connection of a patients’ artery and vein, and an AV graft is a connection made with plastic tubing. A patient’s native veins cannot handle the blood flow from hemodialysis long-term, so AV grafts and fistulas allow for increased blood flow and better hemodialysis results. Many patients develop blood clots within AV grafts and fistulas, which can significantly impede blood flow during hemodialysis. As such, IR often sees these patients in order to declot their AV graft or fistula. Dr. Bui told us that the 3 month patency rate following declotting is 40%. That is shockingly low – 60% of patients who require a declot must return in less than three months for a repeat procedure! I am curious if there is a way to improve the long-term patency of these AV grafts and fistulas – or even better, a way to avoid hemodialysis in the first place.
Image: Shows an AV graft, from Wikipedia page on Hemodialysis
Week 6, Part 1: Representation
Charlotte ter Haar Blog
I’ve been struck by the lack of females in Interventional Radiology. I haven’t met any female attendings in IR at UIC and neither of the fellows are female either. Since I’ve only spent time in the IR department at UIC and having a sample size of n=1 is typically never a good idea, I took my questions to the internet to see if I could find some more robust numbers. A physician and a certified medical laser safety officer (CMLSO) published an article in December 2013 in the Seminars in Interventional Radiology, titled “Pregnancy and the Working Interventional Radiologist.” The article cites that 2% of all interventional radiologists are women. While that statistic is disheartening, the conclusion of the article declares that a practicing interventional radiologist can stay productive throughout her pregnancy, providing that a few additional measures are taken to reduce injuries “related to the anatomic and physiology changes of pregnancy.” This conclusion is uplifting – I suspect that some women are wary of the radiation exposure in such a career. (Side note – interventional cardiology, which has a similar length-training, also requires a fellowship following residency, and also has significant radiation exposure, has females represented at approximately 4%, not a much better showing than IR).
Note: The image is of Dr. Spencer from Riaendovascular, because I think it’s important to see women in roles in which they are not often found.
Week 6, Part 2: Taking an active role
Charlotte ter Haar Blog

While I understand the value in observing in the clinic, it has been fun to interact with the technology when we are given the chance. Earlier in our rotation, a rep from AngioDynamics was in the IR suite to demonstrate the VenaCure laser ablation system for varicose veins. We also go to talk to her about the AngioVac device. Earlier this week, we spoke with a rep from Gore, who showed us several stents that Gore produces. I got to deploy one (not in a patient, obviously), which was pretty cool. We have also had the opportunity to handle two different biopsy devices, and to practice using the ultrasound. Actually interacting with the technology always given me a better understanding of the learning curve required to use any new technology. For example, I did not find either of the biopsy devices to be intuitive, and had to go through several trials until I understood which buttons/levers to push and when.
Overall, I am very thankful for the opportunity to shadow in IR and for the wonderful mentorship I received in this program!
Image: Dr. Bui demonstrating the ultrasound on Emil.
Lindsay Tryon Heading link

Lindsay Tryon
I am a bioengineering student at UIC, concentrating in neural engineering. I look forward to gaining a better insight to how medical devices are implemented in hospitals and how engineers can help improve patient and staff satisfaction.
Lindsay Tryon Blog Heading link
-
Lindsay Tryon Blog
First Impressions
Day one of clinical rotation in urology started off in the Mile Square Health Center where we shadowed several doctors. Once we arrived we began right away by seeing a prostate biopsy. I noted how uncomfortable the patient appeared to be before and during the procedure. He was very nervous that he would be in pain and even asked the doctor if it would be possible to do the procedure under general anesthesia. The patient appeared to be made more nervous by the sight of the equipment, especially the long needles. The needle used to extract tissue for biopsy made a very loud clicking noise when it was prepped, when it extracted tissue, and when it released the sample into the specimen cup. The noise made me feel uneasy, so I imagine it did not help the patient’s nerves during the procedure. It appeared to me that the tools used, although functioning effectively, could be improved for the patient’s comfort.
Day two of clinical rotation in urology was spent in the OR observing a prostatectomy and pyeloplasty assisted by the da Vinci Xi robot. Halfway through the prostatectomy I was beginning to wonder if it was possible to be in love with a machine. The robot is absolutely incredible and the engineers who designed it thought of almost everything (but not quite). The robot basically allows the surgeon to gain a third arm, plus control of an incredible camera. The instruments inserted into the patient are tiny and have seven degrees of freedom, which allows the surgeon to do much more than is possible with basic laparoscopic surgery tools. Furthermore, the robotic instruments have the ability to cauterize, which helps keeps blood out of the workspace. The doctor told us that during open surgery the amount of blood present limits visibility and, thus, precision. This leads to the surgeon taking more tissue than is medically necessary, which, of course, is not optimal for the patient. During robotic assisted surgery, visibility is further increased by the fact that the surgeon at the control desk sees the camera footage in 3D. The surgeon pointed out some aspects of the device that he believes need improvement. He told us that his biggest frustration with the robot is that the camera gets foggy from the cauterization. Several times during each surgery the camera must be completely removed to be cleaned . He also mentioned that the instruments can only be used ten times before they must be replaced. After ten uses the robot will no longer recognize the instruments if they are attached. He attributed this protocol to the fact that only one company produces the robots and the instruments, so the replacement regimen generates more income for the company.From the first two days in rotation it appears that listening to conversations amongst nurses/attendings/residents generates some of the most valuable observations. I noticed the staff frequently making comments to each other about annoyances (big and small) with procedures or equipment. They also frequently offer outright suggestions for changes they would like to see. Before starting clinical rotations I had worried that it would be difficult to find significant clinical problems/needs, however I have already made a multitude of observations. One thing I noted was the lack of a way to identify the different organs/tissues/veins/nerves inside the body during the procedure. It appeared that the only way to be able to identify structures was through extensive hands on experience. Several times during the day the resident, who has been assisting and performing surgeries for quite some time, asked the attending how he knew that a specific structure was such. While the resident was performing the beginning of the procedure he started to cutting through tissues to access the prostate by “following the vest”. He knew this route would lead him to the prostate so he felt safest going this route but the attending had him go a different way because he said it was much shorter. The medical student who was assisting in surgery was asked to identify structures (for practice) and had difficulty in doing so. The medical student also mentioned between procedures that one of the reasons he was assisting in surgery was to get a better understanding of human anatomy as it actually is. This difficulty in learning to identify structures makes for an extensive training process and this process also increases surgery times. The attending said it takes him around two hours to perform a prostatectomy, but having a resident assist in surgery can significantly lengthen the procedure. It appears to me that everyone from patients to staff to stakeholders would benefit from a device that helps surgeons identify (or learn to identify) structures more quickly and accurately.Thus far this experience has been phenomenal. Besides being one of the most interesting things I’ve ever had the opportunity to participate in, it has already been an incredible learning experience.Getting the Hang of ThingsThe rest of week one went as wonderfully as the beginning. Day three was spent in the clinic shadowing Dr. Garvey, who sees about twenty patients a day. He mentioned to us that his biggest frustration is electronic medical records. Although he stops seeing patients at 4pm, he stays in the office until midnight typing up his notes. Prior to electronic record keeping he would dictate notes into a tape recorder and hand them off to someone else to type. He said it is still possible to hire a scribe to enter dictated notes into the system, but the service isn’t used at this location. Several patients were scheduled on Thursday to have a uroflow exam. For this exam the patient urinates into a special toilet which records the flow rate and output volume. If this test yields abnormal results, a bladder scan must be done to see if the patient is retaining urine in their bladder. The bladder scanner happened to be broken this day, so any patient who had abnormal uroflow results had to be rescheduled to repeat the Uroflow test and to have a bladder scan. It appeared to me that the Uroflow machine could be improved so that it did not require the use of another device in order to provide useful results. It was suggested by one doctor that having a bladder scanner built into a smartphone would eliminate the issue of having to wait several days for a repair.
Day four of week one was spent in the OR observing three cystoscopies. Normally a cystoscopy is an outpatient procedure performed using local anesthesia. The Mile Square location is not approved for these types of procedures because of issues with the drainage and ventilation systems, so patients are sent to the OR for the exam. During one of the procedures an abnormality was seen on the lining of the bladder wall, so a biopsy had to be taken. First, three or four samples were gathered using a clamp, then the doctor went back in with a cauterizing tool to cauterize each biopsy site. The longest part of the procedure was relocating each site for cauterization. It seems that having one tool that could collect the biopsy and cauterize the site immediately thereafter would be more practical.The first day of rotations our team was split into groups of two and had been alternating days in the clinic and OR all week. Friday afternoon was the first time all four team members were able to come together to compare observations The other two students had seen different operations so it was interesting to compare notes. It seemed that one of the hardest things for all of us had been making observations without immediately jumping into possible solutions.I can’t wait to see what week two will hold!Week Two: The ClinicMonday and Tuesday of week two were spent at the Mile Square Health Center. Because the rooms at this location are on the small side, the four students had to alternate going in to see patients. One of the patients, who had a history of kidney stones, had a stone visible on a CT scan. It was suspected the stones could be uric acid stones and not the typical calcium stone. To check which type of stone was present the density was checked on the CT scan image and compared to that of bone (a calcium stone would be comparable to bone). The x-ray was also checked because a uric acid stone would not be visible, but a calcium stone would. It was convenient that this information could be found on the computers in the office, instead of having to be sent back to radiology. The rest of the patients I had the opportunity to see were consultations or follow ups. These appointments help me get an idea of how the procedure/treatment went, or is going, for the patient.
In the evening we went with the doctors to make rounds at the hospital, which was another good opportunity to gain insight to the patient’s perspective. During week one Cody and Savan were present for a nephrectomy and during these rounds we had a chance to check in with the patient. It was nice to come full circle and get a patient’s perspective on the tolerability of the procedure.
Week Two: The OR
The second part of week two was spent back in the OR. It was nice to switch it up for the latter half of the week. I had the opportunity to witness the da Vinci robot in action once again, only this time it was the Si model. One notable difference between the two models lies in the camera. The Xi camera automatically focuses, while the Si camera has to be focused manually. The operating room that the surgery took place in had two consoles connected to the Si robot. Only one of the consoles was in use, so we were able to take turns watching the surgery through the lens, which shows the footage in 3D. The 3D image made an incredible difference. Sitting at the console also gave us a chance to get a closer look at the controls used by the surgeon, which are an incredible work of art.
This week our team was able to watch a prostatectomy performed by a different doctor than we had previously observed. I noticed some differences, especially in the amount of blood present in the abdomen. I believe this was in part due to personal preference and technique, but also could have been related to the different patient. It was good to have a second opportunity to watch the procedure since the first time through the amazement at what you’re watching can be a bit distracting.
This week we had a chance to finalize our thoughts on some of the themes that came out of our collective observations. It proved difficult to narrow things down and most of the themes seem to be so connected that their almost inseparable. I look forward to presenting out findings to the Urology department next week!
Noticing Differences
The final week with the Urology department was again split between the OR and the clinic. This week I had the chance to observe some procedures for a second or third time. As I mentioned previously, it is nice to see procedures more than once because you may pick up something you had previously overlooked. It is particularly beneficial to see the same procedure performed by a different doctor because there are so many ways to perform the same procedure. One of the things that stood out most to me during this last week is how differently things are done by staff within the same department. From patient interaction to procedures, there are many differences between the staff.
While observing different doctors in the clinic, I noticed that each has a different style. Some doctors list all of the treatment options available to the patient, make recommendations, and then ask the patient to choose. Others tend to tell the patient only about the procedure/s they feel would be the best, most beneficial option/s. I think both of these approaches are great, but it is interesting to note the variation.
Doctors also have great variation in their approaches to surgery. When talking to one of the doctors about the prostatectomy he explained some of the different approaches surgeons take to get access to the prostate. He said there are hundreds of ways to perform a prostatectomy. I imagine this makes learning more difficult for the residents because they must keep track of manners in which each doctor performs each procedure.
Final Thoughts
In the final week of the rotation, we presented our findings to several members of the department. Our presentation focused on four general areas that commonly give rise to frustrations for staff and/or patients: (1) communication among staff and institutions; (2) patient involvement; (3) non-comprehensive diagnostics; and (4) steep learning curves for procedures and equipment. Of these four areas, I am particularly interested in the steep learning curves for procedures because of what I observed in the OR. I also think that this area has some exciting potential solutions.
The first time I went into the OR I noticed that medical students and residents alike had trouble identifying structures in the body. Due to the nature of how anatomy is taught it is very difficult for students to re-learn to identify organs as they appear in vivo. It seems there could be a better way to teach incoming medical staff about anatomy so they have more time practicing procedures under an attending as opposed to spending much of their time re-learning the anatomy.
Of course, we are not supposed to be thinking of solutions, but I did want to mention one idea my teammate and I discussed. I had noted that it would be ideal if the robot could tell the user what structures they were viewing. Generally, the surgeries performed using the robot are recorded. Joel suggested that having medical students review the footage, identify structures, and upload the annotated footage to the robot would help the students learn and also help the robot learn to identify structures. The trouble, of course, is that there is so much variation in anatomy from human to human.
The first rotation was very exciting and I had a great team with whom I was able to identify several clinical needs. I am so thankful to the Urology Department for being so welcoming and helpful to us. I am very excited to start my next rotation!
Getting the Hang of Things…Again
The first week in Neurology rotation has been going quite well. It is a very different experience than my time with the Urology department. One reason for this difference is that in Neurology the patient’s history is one of the most important parts of their diagnosis. According to our mentor, Dr. Shapiro, 80% of the diagnosis is based on history. For this reason, the doctors spend a very long time in the room with patients as compared to what I am used to. Of course, during some routine follow-up appointments this is not the case. During general inpatient rotations, when the attending arrives to the hospital in the morning, it takes between 25-25 minutes for the residents to present each new patient.
Because so much of diagnosis is based on patient history and how the patient is presenting, there seems to be very little equipment used in clinic and hospital settings. The most frequently used technology that I have seen so far is the video EEG. Today we had the chance to go to the EEG lab and learn a bit about reading them. We noted that the readings are done manually and the doctor must sometimes scroll through hours worth of output looking for epileptiform discharges. Muscle movement also causes constant noise in the signal, which must be filtered out. However, this filtering causes the EEG reading to be less accurate.
So far its has been difficult to asses clinical problems, although there have been a few I have noted. As I’ve mention, patient history is very important, however, because of the nature of Neurology, many of the patients have altered mental states. It can be difficult to obtain medical history for this reason.
It seems that many of the problems we will be identifying will come from the lack of technology available in neurology!
Subjective Assessment
Thus far, one of the biggest problems I have noticed lies in the exams. To asses patients in neurology there is a standard series of exams that are done to check muscle tone, reflexes, and vision. To check muscle tone the patient is asked to push back or pull on the doctors hand with various parts of their extremities. As previously noted this can be very difficult when dealing with non-compliant patients. Furthermore, the persons tone is scored out of 5 based on how much effort is given and how much resistance there is. The scoring system is subjective and there is no way to quantify the results. The system does seem to be rather standardized, but sometimes a resident will present a patient with one score and the attending’s evaluation will result in another. This makes it difficult to track a patient’s progress accurately.
I also had a chance to observe a memory evaluation this week. When patients come to the office and are concerned about changes in their memory function, there is a short, 15-25 minute, test that can be given. Depending on the results the patient can be sent to get a more extensive evaluation. The in-office evaluation has sections to test the patients verbal memory, computational memory, etc. Part of the assessment requires the patient to identify animals. It is intended to be a bit difficult so the animals are a bit rare, and the patient’s ability to answer can be influenced by their educational background. The physician mentioned that it can be difficult to score the results when you are unsure if the patient has answered some of the question incorrectly because their memory has changed or because they didn’t know the information to begin with.
Learning More About ImagingThis week we had a chance to learn more about MRI testing. First, we learned how to tell different types of MRI scans apart and got some practice in identifying abnormalities. Of course it would take much, much longer than we have to learn how to identify all of the abnormalities one might see. Nevertheless, it was interesting to learn about the variation in human anatomy as well as about the many different types of scans can be done with MRI. After learning some basics about the images produced by MRI we had a chance to go to the MRI center and sit in with a couple of technicians to learn how the scans are done. One of the techs explained some of the physics on how the machine works and how the different types of images are produced. I’m unsure how it is humanly possible that someone figured out how to get such amazing images in such an abstract manner. He also talked to us about how the room is designed which was nearly as mind blowing. There is a copper mesh lining the insides of all of the walls so that radio frequencies from outside do not effect the machine’s readings. The technician also explained to us that the MRI room is the only place in the hospital where you can die just from walking through the door. The magnetic field is so strong that if someone walks into the room with metal, it will be drawn toward the magnet at such a high velocity anyone in its path could be injured or killed. He shared plenty of stories with us where breaches in safety protocol ended in death (not specifically at UIC). After scaring us to death, he brought us into the room and showed us how strong the field was by having us hold up a very small metal key and try to manipulate it. When we asked the technician what, in his opinion, is the biggest problem for him he told us it was lack of safety education for hospital staff. He said that although staff may be told the dangers of going near the machines without a technician’s clearance, is not enough. He thinks all staff should be brought to the MRI center for an orientation where the strength of the magnetic field is demonstrated in a similar way to how it was demonstrated to us.EEG ExamsThe first week of the rotation we noticed that the video EEG is frequently used in the hospital and clinic for diagnostics. Last week we had a chance to read EEGs and this week we were able to shadow a technician while she set up the EEG exams in the clinic. She told us that the best readings happen when the patient is able to achieve light sleep. During this time your brain is the most likely to emit epeleptiform waves. Sleep can be very difficult to achieve in a doctor’s office or hospital in a 30-45 minute window of time, which makes me think this exam would be more effective if done in the patients home. The technician also noted that her biggest frustration with the testing is the noise interference. She said it is particularly difficult to eliminate interference in the hospital when so much other equipment is being used and so many people are coming in and out of the room. The field is disrupted when a nurse, physician, or anyone else comes to close to the machine or wires and noise is created. Braiding the wires together can help cut back on artifacts in the recording, but is not done because it makes it more difficult to place the electrodes correctly. Further, the EEG is completely unreadable if the patient moves. Therefore, if the patient has a seizure and is jerking around, the EEG shows nothing and information about the seizure must be taken from the moments just before the clinical seizure (movement) begins. I assume this could present a problem if the patient happens to be moving for an unrelated reason right before the seizure begins.Modern Day MacGyverThis week we had a chance to spend some time learning about the rehab side of neurology. It has been interesting to get to see a completely different side of the department. Thus far, this side of neurology has been a bit more uplifting because there is more that can be done that allows us to see direct improvement to the patients quality of life. The occupational therapist who showed us around was incredible and very innovative. She helps patients regain their ability to go about their daily activities in several ways, including by providing them with various tools and devices. She told us that many patients don’t realize all of the types of equipment that is available to assist them with activities, so they don’t even mention struggling with certain activities. That being said, when the tools are available for people, they don’t always meet the needs of patients because each person’s needs are so different. For this reason she designs tools for her patients on the fly and creates many of them by using thermal plastic or sewing. She also mentioned that she sometimes modifies the existing equipment to better meet each patients need. She noted that sometimes the people coming up with the original design don’t know how the patient will actually be using the device in their homes. Because of her direct interaction with the patients and her experience in home health care, she has a more clear idea of how patients will use the equipment and how it can be modified to meet their needs.
The therapist said the biggest problem she faces is funding. She said as culture is changing the facility hasn’t been able to keep up with the patient’s needs. For instance, many people will be using their laptop or tablet at home but the OT department doesn’t have either at their facility to work with patients on. She also said that funding can be such a problem that she sometimes will use her own money to purchase items she finds to be necessities. I was so impressed by her, her innovative mindset, and the work she does to help her patients get back to their daily lives.
Wrapping Up
This week in rehab we saw some amazing technology, including the hyperbaric oxygen chamber. Unfortunately there were no patients so we didn’t get a chance to see the chamber in action, but we did learn about its uses. The patient is placed in the chamber and it is pressurized to 30 ft below sea level and filled with 100% oxygen. This causes the patient’s plasma to become saturated with oxygen which helps them heal after surgical procedures.
This week we were also able to spend some time withthe Shceck and Siress prosthetics team at UIC. This was probably the highlight of my time during this program. The patients we spoke with were wonderful and very willing to answer any and all of our questions. In talking to them we learned a lot about the changes in prosthetics that have occurred over the years. Everyone we spoke to made a point of telling us how amazing David Rotter, the prosthetist, was. He has designed many different customized prosthetics for many people.
Overall, this experience has been an incredibly positive one. I have had the opportunity to see things that I may never again have the opportunity to see and learned so much about problem identification.
Wasuwat Siewsrichol Heading link

My name is Wasuwat Siewsrichol and I am a senior bioengineer. Currently, I am in the Pulmonary and Critical Care and Hematology Oncology/Radiology Oncology department. I am very excited to be apart of the program because the experience will help me gain more insight into the advancements of medical technologies, and the current issues associated with these technologies. I plan to pursue a career in the field of pulmonology in the future, and I hope to use the skills that I learned during the internship to enhance my career as a physician.
Wasuwat Siewsrichol Blog Heading link
-
Wasuwat Siewsrichol Blog
It’s Simplest Things that Gives Us the Biggest Headache
Wasuwat Siewsrichol Blog

The first day of the Clinical Immersion program started out with Dr. Kotche and her colleagues explaining the whole goal of the program and what we are expected to do in the clinical setting. We first had to define why we are here and what we stand for. Next, all the engineering and medical students went through exercises that teaches us to be in the moment, and how to communicate with each other effectively. The exercise were very fun and enjoyable because it taught me how to think on my feet, but honestly, all I could think about was the clinical rotation that I was about to embark on this afternoon. The morning session ended with all of us discussing all of our hopes and fears about the program, and for me, it was very encouraging to see that a lot of people had the same hope and fears as I do before we start our clinical immersion.
Finally! It’s 1p.m. and it was finally time for us to meet our physician mentor for the next three weeks. I was very excited that I was placed in the Pulmonary and Critical Care rotation with my good friend and senior bionengineer, Elise DeBryun, and medical student, Ana Brzezinski, who also has background in bioengineering. Our mentor for this rotation was Dr. Dudek, the chief of the pulmonary and critical care unit in the University of Illinois Hospital system. We entered the clinic ,and we were immediately greeted with a warm welcome from one of the nurse practitioner. She then explained to us about her current research and clinical experiences, and she told us about one of the biggest frustration about being a health care provider: patients who have to be readmitted because they do not know how to use their medicine correctly. I kept this thought in mind while I was shadowing Dr. Zaidi, a third year pulmonary fellow.
Dr. Zaidi’s first patient was a male patient in his mid to late 40s experiencing sarcoidosis, an autoimmune diseases that mostly affects the respiratory system, and the disease is very unknown to the medical community. While in the room with the patient, I felt empathy for the patient because he described his symptoms as “ feeling sharp pain like pins and needles in my chest every time I take a deep breath.” Then that got me thinking if there was a way that doctors can examine the lungs without it hurting the patient. I discussed the problem with my group members, and we concluded that it would be impractical to use a different method other than the stethoscope because of its ease of use and time-saving benefits.
As Dr. Zaidi and I saw more patients, something became very clear to me: patients are not using their medications properly, and that is one of the main reason why their conditions are not improving as fast as they should. Specifically for patients with asthma or lung related diseases, most of the patients either do not know how to use the devices that administer medications, such as an inhaler, or are not taking their medications on a consistent basis. That’s when I noticed that the first problem that needs to be addressed are the instructions on how to use the inhalers. I took a look at the directions and I thought that it was not complicated to understand, however, I realize that patients are less likely to read the instructions because it is very lengthy and sometimes do not give clear instruction on how to properly use the inhalers. My teammates and I discussed this situation, and we thought that one improvements we could make to the instructions is to add more diagrams and pictures, or even a link to a video tutorial of how to properly use these inhalers. Other than misuse of medications, I did not notice any major problems in the clinic today.
After we finished seeing all the patients, Dr. Dudek showed us x-rays of the lungs of patients with various pulmonary disorders. He told us that one the thing that really slows him down from his daily practice is the incompatibility of each images that were sent to him. He told us that he gets images such as x-rays and CT scans all the time, but most of them are generated from different programs and it is very time consuming to configure how to open and analyze these images. The team and I talked about it, and we thought that the best way to solve this problem is to generate a program that converts all types of data files into one consistent file that the doctors can use every time he gets images sent to him from different department.
At the end of the day, when one of the fellows told us about a very graphic story of what happened to him during his trauma surgery rotation on 4th of July weekend. I won’t mentioned it here because it doesn’t really relate to the pulmonary clinic, but his story really opened my eyes to the other extreme side of medicine and that the need of advancement in medical technology more than I had ever expected.
First Hand Experience: Bronchoscopy and PFT
Wasuwat Siewsrichol Blog

On the morning of the second day of the program, my heart was already racing at 8 am in the morning because today is the day that we will be visiting the bronchoscopy lab. This is the first time in my life that I will be observing a medical procedure so I felt nervous, and at the same time, excited to see what the doctor does and how he uses medical devices during the operation. The procedure involves the physician inserting a bronchoscope into the patient’s lungs to collect tissue samples from enlarge nodules found on the lumen of the airways. The bronchoscope consists of a camera, light source, ultrasound probe, and a suction mechanism for the excess saliva.
Once the procedure has started, I immediately saw that the doctor was holding the main body of the bronchoscope in his left hand while controlling the catheter that is going into the patient’s trachea in his right hand. If the procedure was a short five to ten minutes, the setup with the doctor physically holding the device would not be a problem, however, this type of procedure took approximately thirty to forty-five minutes to complete. Therefore, for the doctor to hold the bronchoscope for a long duration of time would be an inefficient setup because of the toll that the weight of the scope would have on his arm. Our team discussed this problem, and we thought that one solution would be to develop a flexible stand for the scope so the doctors could perform the procedure more efficiently.
One shocking thing that I saw during the procedure was how much the patient was violently coughing from the buildup of saliva in the trachea. Luckily, the patient was under sedative medication so she did not feel the discomfort, but the image of the patient choking was very disturbing to me. That is when I thought that there must be some way that the bronchoscope can be improved. One of the ways that the scope can be improved is in its suction mechanism located near the tip of the catheter because it seems to have a very low suction power. Next, the actual catheter itself is relatively thick and could possibly cause a major obstruction in the airway. These are the two issues that I saw with the current bronchoscope, and if these two issues were addressed, I believe that the patient would feel more comfort, and the time of the procedure would be greatly reduced.
Later that afternoon, we visited the Pulmonary Functioning Test Lab. We were greeted with two pulmonary technicians, and we were on our way to observe the pulmonary lung functioning test. The procedure was relatively simple with the patient breathing into a big machine, and the computer would generate the flowrate and pressure of air as the patient produces. The PFT machine was also equipped with a mouth piece with a pyramidal filter that will ensure that the machine stays clean of saliva. Near the end the of the session, I noticed that the patient was absolutely exhausted from all the hard breathing into the machine. The pulmonary technician and our team discussed this issue, and he told us that one of the problem is that this style of testing requires so much sample size from the patient that they get very exhausted at the end of the testing session. The pulmonary technician suggest that we should come up with a new way of sample collection that will reduce the amount of work outputted by the patient. At the end of the day, one good thing that I noticed during the PFT testing was the great instructions that the pulmonary technicians gave to their patients. The technicians were so energetic and charismatic that I couldn’t help but smile at the interaction between the patient and the technician.
Keep Calm and Breathe On
Wasuwat Siewsrichol Blog

The morning of day three of the clinical immersion program started off with us spending time in the intensive care unit (ICU). The ICU was filled with residents, fellows, and attending physicians that morning, and our team asked them what they thought could be improved about the ICU. One major theme that showed up was improving communication. As I was doing rounds with the ICU team, I noticed that communication between departments in the hospital was not very consistent. For instance, one of the fellows seemed very confused and frustrated when he found out that the other department had given his patient too much of a drug before admitting patient into the ICU. Another communication problem that everyone seemed to agree on is the pager system. The physicians believe that if pagers were replaced with cell phones, the communication between them and the hospital would be greatly improved. Next, one of the fellows mentioned that monitoring vital signs is crucial to the health of the patient, so he suggest that vital monitors should be placed in every room in the ICU.
While walking around the ICU, I noticed that almost every patient was intubated and are breathing with an assistance from a complex and sophisticated ventilator. The ventilator was probably the most advance medical equipment that I have seen in the department. The ventilator works by pumping air into the lungs of patients who cannot breathe on their own. The ventilator has several breathing settings such as: 1) automated breathing: the physicians adjusts the flow rate and frequency of the air that is flown into the patient’s lung 2) assisted breathing: patients do some of the work, while the machine takes care of the rest. For example, the machine can sense that the patient has started breathing, but then it gives the person an extra push of air so they can take their own breath 3) Pressure mediated breathing: This setting is similar to the automated breathing, but doctors can designate the pressure gradient that they want in the lungs so the lungs can expand and contract based on the changes in pressure. Out of all these three settings, the assisted breathing would be the most comfortable for the patient because they are breathing on their own, when compared to the other methods where the machine forces air into the patient.
One of the most surprising thing that I noticed in the ICU is how calm and in-control the attending physician and the senior fellows are. Even in emergency situations, I saw that the doctors seem very patient and composed. For example, while the senior fellow was showing us how the ventilators worked, the patient that he was working on stopped breathing. Earlier, when we entered the room, the patient was very responsive to our presence, but now he just laid there. He was completely still. He looked dead. At this moment, I began to panic, and I looked at the fellow. To my surprise, he kept his composure, and he calmly went to work on the machines by pressing various buttons. A few seconds later, the ventilator produced a huge puff of air into the patient’s lungs, the patient’s chest exploded upwards, and he began breathing again. Watching the patient laid unconscious on the bed with no active vital signs was probably my most stressful experience that I went through during this program thus far.
Following the dramatic experience with the patient not breathing on Thursday, on Friday July 8th, we headed back to the bronchoscopy suite to observe a thoracentesis. The procedure involved inserting a needle from the patient’s back to remove the fluid from the bottom of the lungs. The doctor started off my using an ultrasound probe to locate the fluids the lungs, and then marking that spot on the patient’s back, which indicated the location that he will insert the needle. During the procedure, I saw that the doctor had taken out a huge needle, which was about ten to twelve inches in length. I was shocked by how big the needle was. The next surprising thing was that the doctor simple inserted the needle directly into the patient’s back, and then he uses a syringe, catheter, and three-way stopcock to remove the fluids from the body into a drainage bag. Before the procedure, the doctor told us that he estimated there would be approximately half a can of coke worth of fluids in the patient’s lungs. After the drainage, the total fluids that was removed from the lungs was approximately one liter! It was very surprising to me that the lungs can hold that much fluid given her small body shape. After the surgery, we went to a lecture given to the all the new fellows on the anatomy and mechanisms of the lungs. I thought that it was interesting that even doctors who recently finish their residencies still need to review the basic anatomy and physiology of the lungs.
Breathing like the Patients!
Wasuwat Siewsrichol Blog

Monday July 11th – Wednesday July 13th: I am very excited to go to the ICU today because our mentor has scheduled us see a live demo of the ventilator that we saw last week. After a the pulmonary technician taught us how the ventilators worked, he actually allowed us get on the machine and try it ourselves! Awesome! Jerry handed us a sterile mouthpiece, and we pinched out nose to simulate what patients would feel like if they were on the assisted breathing system. I tried the two modes of breathing: automated and assisted breathing. While under the automated breathing, I felt very uncomfortable because it felt weird to have cycles of air forced into my body. Especially when the automated is not in sync with my own breathing, it felt like I was choking because I would be breathing out and the machine would simultaneously push air in. That feeling was not very comfortable at all.
The next mode I tried was the assisted breathing. The assisted breathing uses sensor to detect the negative pressure generated from your lungs, and then the machine a puff of air that is supposed to be in-sync with your body. This mode was much more comfortable for me because it felt like I could take air in and out without much resistance. After being on the ventilation machine for approximately five to ten minutes, I decided that I needed a break because I felt this weird tightness in my chest and a little bit fatigue. This has made me realize that being on that machine was exhausting! I cannot believe patients can tolerate this much discomfort while being on the machine. Dr. Dudek later explained to our group that the reason that we feel so much discomfort while using the machine is because it uses a positive pressure system to put air in our lungs, while the human lungs uses a negative pressure system to bring air into the lungs. Even though the ventilator is a great system that helps the patient breathe, the discomfort level is extremely high, and a negative pressure-based ventilator system needs to be introduced to increase patient satisfaction.
Later that afternoon, were assigned to visit the Allergy Clinic to observe Dr. Nyenhuis, an allergy and immunology attending physician. While in her office, I did not notice much technological problems. However, one aspect that I noticed about the allergy clinic that could be improved is the allergy testing itself. There were two types of allergy testing that was provided in the clinic: skin test and the patch test. The skin test involved applying different allergens to the skins of the patient with a brush. The nurse described tool as a small brush/needle with a blunt tip. Then, we asked one of the patient that was doing the allergy test if she felt any discomfort during the procedure, and she said everything went well. Next is the patch test, which involves putting a big piece of cloth filled with different allergens on the patient’s back. The cloth is then covered with an elastic tape for a duration of 3 days, and then the patch will be removed. After the removal of allergens, the doctor wait for 2 more days until she can read the results. One of the problems that I noticed for this test was the duration discomfort for the patient. The discomfort does not involve pain, however, the patient has to be very careful not to get the patch on their back wet. Therefore, I thought that the test methodology could be improved by reducing the duration because time it takes for the test to work.
On Tuesday, we went back to the ICU again, and after usual morning rounds, we sat down with one of the senior fellows to talk about problems that he has been experiencing during his time here. Surprisingly, he did not mentioned any technological issues, but he said there are problems between the communication between the residents. He said that residents are typically works in the ICU for about sixteen hours, and when his or her shift is over, the resident would then pass on the information about all the patient that he is taking care off to the next resident that is scheduled to take his place. He mentioned that this method was extremely ineffective because some information about the patient could be lost during the transition phase. Our team discussed this issue, and we could not come up with a good solution to this problem. This has made me realize some simple such as passing on information from one person to another could not be easily solved to a device.
Next, one of the emergency response team member, an anesthesiology resident, showed us what was in his emergency response box. The response kit has various emergency medicines in it, devices, and equipment that could be useful during emergency situations. One of the most advanced device that I saw in the kit was a glidescope with an attached camera and small screen on it. The resident told us that having the camera and monitor on there is a huge improvement to the old version because he could easily intubate the patient faster and at a more successful rate. One improvement that I would make to the scope is to improve the resolution of the screen on the scope, or even add wifi capabilities to the scope so it is able to transmit data to other departments during emergency situations.
On Wednesday, we spent the majority of the day in the pulmonary clinic. During my time in the clinic, I did not notice any significant problems that needs to be addressed. However, I did notice one technological advances that I have never seen before. While I was shadowing a pulmonary fellow, I saw him drew blood from a patient. After he was done, I noticed that the needle on the syringe adapter had automatically snapped back inside the adapter after the fellow was done drawing blood. I remembered one of my professors mentioning that there is a big problem with injuries relating to uncapped needles, and after seeing the problem being addressed in the clinical setting, I am happy to see new innovations that addresses the current health issues.
I Could Feel Its Heart Beat
Thursday July 14 – Monday July 18th: This Thursday consists of our team spending time in Pulmonary Hypertension Clinic with Dr. Machado. Once we entered the Clinic, Dr. Machado immediately gave us a quick lecture on Pulmonary Hypertension (PH), and his lecture was great because the information he presented to us fitted in well with the materials I learned in my BIOE 310 course.
Our first patient was Hispanic and recently underwent a surgery on her lungs. The patient did not speak any English, but one of the resident did, and so she translated all the patient’s information to the fellow. After watching the resident translate to the fellow, a thought came into my head. Would practicing medicine be more efficient if the medical students are required to learn a second language before they graduate? There are translating devices or mechanism out there that the hospital can use, but I feel that some information from the patient, such as their symptoms and its severity, may be lost during translation. Then again, requiring medical students to learn a second language before they graduate may put too much stress on their already work-filled schedule.
One issue that I noticed while in the room with the patient has to do with patient comfort. I noticed that with the first and second patient that we saw could not get up on their examining chairs because the seat was too tall. The doctors tried to lower the seat to its lowest setting, but it was still now low enough for the patient to comfortably sit on. One simple solution that out team came up with is to add a pull out stool to the examining seat. Next, the major issue that I saw in the clinic that day was with a patient and her oxygen tank. After examining the patient, the doctors said that the flow of oxygen needs to be increased. However, when the patient tried to increase the flow, she realizes that the oxygen tank does not go any higher. So then the doctors had to spend time ordering another oxygen tank that would accommodate the patient’s needs. I thought that this was huge issue because if the patient does not get enough oxygen to her lungs, she could have a major injury that could lead to death. Therefore, the solution to lack of flow from the tank is that tank needs to be engineered so to produce a wide range of flow to assist the patients in all her needs.
We spent later that afternoon in the ICE, and once we got there, we heard the intercom reported that there was an emergency situation on our floor. After the announcement, I saw approximately fifteen to twenty people rushed into one room, and as I walked slowly to the action, I realized that it was just in the right place at the right time. The emergency was actually a simulation given to the residents and fellows as part of their training a few times a month. The devices used in the simulation was one of the most technologically advanced pieces of equipment that I have ever seen. The simulation uses a human model that is able to produce measurable vital signs such as heart rate, blood pressure, and blood flow. I tried laying my hand on the model’s chest, and it felt so real that I could feel the model’s heart beat! The human model can also undergo various medical conditions, which is controlled by the medical technicians. The doctors can even administer drugs to the various parts of the body, and the technician can control how and if the model will respond to the given drug. If the physician performs the correct procedure in that scenario, the condition of the model will improve, and if the physician performed the incorrect procedure, the model’s condition will get worse. After examining the model even further, an improvement that I could make to this model to add bleeding to one of its capabilities.
On Friday and Monday, we spent our time again the ICU. One the things that I noticed that needs to be improved is the communication between the patient and the physicians when the patient is intubated. I saw one patient who was raising her arm to get the doctor’s attention, however, the doctors tried asking the patient what’s wrong, but they could figure it out. The attending tried to use various methods such as having the patients nod for yes and shake her head for no and holding up one finger for yes and two for no, but none of these methods worked. Therefore, our team discussed this problem and we thought that it would be a good idea to put a yes/no diagram for patients to effectively communicate with patients.
Is That Bed Even Clean?
Tuesday July 19th – Thursday July 21st:
Tuesday morning, we spent our time doing rounds with the residents. While rounding, one of the attending physician mentioned that one of the patient was not eat well, if at all. The patient was under a ventilator, she could not feed herself, and they could not pull the ventilator out because the patient cannot breathe on her own. As I was listening to their discussion, I thought that machines like the ventilators should be equipped with feeding tubes because the caretakers have to be able to provide proper nutrition to the patient. In the end, the doctors decided that only thing that they could do for her right now is to give her liquid glucose because that is the solution given her ill condition. I would guess that giving liquid glucose to the patient would give her enough energy for the body to do its basic metabolic functions, such as breathing, but what about for patient who are under her condition for a long period of time? I would think that giving the patient just liquid glucose would hinder the recovery process because the body would not have enough nutrients for recovery. Therefore, a feeding tube should be implemented into the breathing system in future devices.
We headed to the sleep clinic later that afternoon and I was excited because I was curious to see the technologies that is involved in monitoring sleep. Unfortunately, there were no sleep study scheduled at the time that we were there, so I did not get to see patients using the various machines. While there, I was paired with one of the sleep fellows, and we saw patients who are experiencing sleep apnea. Sleep apnea is a condition where patients stop breathing while they sleep, and the disorder can contribute to other pulmonary diseases, such as asthma. While in the clinic, one of the patient had brought his CPAP (continuous positive airway pressure) machine with him. I took a look at the machine, and I thought that it was a very innovative machine because not only does it allows the patient to breathe at night, but it also takes data of how often that patients undergo apnea. The data is then obtained from the doctor by removing a memory card in the back of the machine.
One way this machine can be improved is to add wifi capabilities to the machine, so the patients can send their sleep data to the doctors prior to the appointment to improve the efficiency of the appointment. Other than that, another issue the patient brings up is that the face mask for the CPAP machine does not fit his face very well because of his beard. Therefore, the simple solution to this problem is to get a bigger mask to accommodate his beard.
There was one issue that I keep coming up as I saw more patients, which is the sanitary of the beds that the patients are sleeping in for the sleep study. The clinic is set up so that each room had a bed in it, so during the day, the doctors who do his normal clinic work in this room, Then at night, they would use the same room for the sleep study. Then I saw a sign on one of the beds that read something along the lines of “Please do not sit on the bed. Bed has been sterilized and used for for sleep study patients only.” This sign got me thinking because if the doctors use these rooms to see patients during the day, and if the bed sheets have been sterilized in the morning, wouldn’t sterility of the bed be compromised if the bed is exposed to patients during the day? I don’t know if this is a problem, or if the staff replace the sheets before the patients undergo the sleep study, but this is one of the biggest issue that I saw at the Sleep Clinic.
On Wednesday, we were in the ICU and the Pulmonary Clinic. Not much happened today because all the issues that I have been seen have been noted in previous blogs. Problems with the communication between hospitals are still a reoccurring issue that needs to be addressed in the healthcare system for efficient patient care.
On Thursday, were back to the Pulmonary Hypertension (PH) Clinic Shadowing Dr. Machado. Clinic went on as usual, and I did not notice anything out of the ordinary other than the fact that communication between hospitals still needs improvement. Today, one patient had gotten her tests done at an outside clinic, and when she came to the PH clinic, she was missing some tests that the outside hospital had told her that they had given her. Therefore, her visit was wasted because the doctor could not have treated her until he receives all results of the test. If only all the hospitals have the same communication system, the healthcare system would work much more efficiently for the patient and the doctors.
Goodbye Pulmonology, Hello Oncology
Friday July 22nd– Tuesday July 26th: We’ve finally made it to the end of the Pulmonary and Critical Care Rotation! It was an unforgettable experience, and I have learned so much from the physicians, fellows, and resident in the department. I am truly grateful for taking part in this department. Today was also the day that we give our presentation to Dr. Jacobson, one of the attending pulmonary physicians. Our presentation went very well, and Dr. Jacobson said that we mentioned all the crucial issues that he has been experiencing, such as the communication between hospitals and the lack of patients’ education.
My next rotation after the Pulmonary and Critical Care department is the Hematology and Radiation Oncology department. We will spend our first week in Radiation Oncology, and then the next two weeks in Hematology. On Monday, we visited the Hematology Clinic and our mentor was Dr. Koshy. Dr. Koshy showed us around the clinic, and I have to say that this department has one of the most technologically advanced medical equipment that I have ever seen. Specifically, the radiation machine, which is approximately 6 – 8 feet tall, and the clinic itself also has a built in particle accelerator which surrounds. The particle accelerator is used to power the radiation machine, which is said to be 100 times more powerful the normal x-ray machine.
After Dr. Koshy showed us the radiation machine, he mentioned that one main problems that arise when using the machine is the patient’s stability during treatment. The patient has to first get a CT scan, and then the radiation oncologist marks the CT scan with the location that they want to administer the radiation. As a result, the patient has to be in the positioned in the same location that he or she took the CT scan in so the radiation can be applied to the previously marked location. Currently, the clinic uses a self-hardening polymer that the patient lies on, and then the mixture a foams up and harden in accordance to the patient’s body position. However, the doctor did mention that this method maybe in effective when patients lose or gain weight after the initial CT scan. In addition to looking at the radiation machine, one of the resident also explained to us the physics behind the technique of administering the medication, which I found to be very interesting and complicated.
Entering the clinic on Tuesday, I felt a bit nervous because today was the day that I will get to interact with patients. I was nervous because I know that this clinic deals with cancer, which is an emotional topic for me. I saw three patients today, and surprisingly, all of them went smoothly. I did not notice much problems in the clinic, except for the usual communication issues that I have mentioned in the previous blogs in the Pulmonary and Critical Care department. For example, one patient that we saw was a bit drowsy during his consultation because he just came out of the emergency room. Therefore, communication between the doctor and patient was compromised.
One issue that I did notice with the technology during the administration of radiation was with one of the tools that the doctors use give radiation inside the body. The tool was similar to tweezers, but radioactive isotopes can be administered at the end of each rod. The two rods on the side are meant to separate the tissues surrounding the tumor, and once the doctor has isolated the tumor itself, he would tighten a knob at the end of the device to lock in the two rod’s position. However, the locking mechanism often does not work because the pressure between the opening of the tissue is often too large that the two rods would snap back to its original configuration. The doctor would then have to manually tape the two rods apart so that they would stay open during the operation. As a result, the current method to stabilize the equipment was an inconvenience for the doctors to always have to use tape during the surgery, and the safety of the patient is also compromised because I am unsure of the sterility of the tape being used.
Full Body Radiation
Wednesday July 27th – Thursday July 28th: The start of wednesday was exciting because it will be the first time that we will see a full body radiation being done with a patient with sickle cell disease. The patient will be penetrated with low dose of radiation to completely wipe out her immune system so she could get a stem cell transplant later that week. Sadly, we did not get to see the stem cell transplant, however, observing the full body radiation was very interesting. First, the patient is placed in a rectangular box. Then, the radiation technician places rice bags around her body so the machine would recognize the patient as a symmetrical rectangle. The reason that the patient has to be placed this way is so the machine can recognize the symmetry of the object that it is radiating. I’m not sure why the patient’s body has to be oriented that way, but I feel like the software of the machine could be improve so that the technician would not have to manipulate the patient’s body in such a way that the sensors can recognize it.
After the total body radiation was over, I noticed that the patient gets out of the glass box, and then immediately gets covered from head to toe with a face mask and towels. This method of protection concerns me because I feel like the patients should be put in a full body suit that fully protects her body, and does not leave any of her body open to the outside world. Next, the patient was transported to an open waiting room where people can simply walk in and out without even noticing that there is a patient in here that has her immune system erased, and is highly susceptible to infection. Therefore, I thought that it would be better with regards to the patient’s health is she was placed in a more sterile environment rather than in open space.
In the clinic during these past two days, there were somethings that the residents mentioned that is really slowing them down: insurance policies and the Cerner system. The residents said that they have to complete a lot of paperwork for the insurance company, which really slows down the treatments of the patients. Next, the major issue in the clinic is the flaw in the Cerner system, which is a communication system that the UI health hospital uses for all medical communication such as writing notes, and retrieving test results. The residents mentioned that the system takes a good amount of time to load and log in that the process of configuring the system during the day could take up to 30 – 45 minutes of their time, which they could have been used for patient care.
On Thursday, we were able to watch a full body simulation, which is where the doctors take a full body CT scan, and then use this scan to plan for the radiation treatment with the least amount of damage to the surrounding tissue. As mentioned in the previous blog, the patient has to be stabilized while laying sideways on the CT scan. The patients lay on a blue bag with a polymer mixture that inflate as the mixtures cools down. The technician has mentioned that the mixer bottle has once actually blown up because someone kept the cap on the bottle for too long after mixing the two chemicals. As a result, the pressure generated from mixing the two chemicals cause a small explosion that splattered in the room. Even Though the explosion did not cause major damage, I would think that if someone was in the room during the splatter, there could have been injuries. As a result, I believe that the mixing bottle of the chemical needs to have a safety unlocking mechanism that safely removes the lid if the pressure in the bottle get too high.
Efficient But Not Perfect
Monday August 1st– Tuesday August 2nd: We spent our time last week in the Radiation Oncology department, and this week, we will see the other side of cancer treatment in the Hematology and Oncology department. Our mentor for this department was Dr. Rondelli, and he gave us a quick lecture that afternoon about the overall field of Hematology and all the diseases and treatments that are currently given in his clinic. After his lecture, I was pretty surprise that UIC is one of the few centers in America that do non-chemotherapy stem cell transplant procedure, and our mentor is one of the few people that are trained to do it.
On Tuesday, we were arranged to be in the blood bank at UIC. Surprisingly, the blood bank that is on the first floor of the hospital is not affiliated with UIC, but to an independent company. While in the blood collection center, we saw the various machines used for patients such as different kinds of centrifuges. I thought that it was awesome to see that the centrifuge was so advanced that it is able to draw blood from the patient, extract various compounds that the physician asks for, and then puts the blood back into the patient. The machine was also able to detect if it draws too much blood at any moment and if the patient is in ischemic conditions. In addition, one of the physicians told us that they also have the advanced centrifuge machine at other facilities in the area as well, however, when the other facilities have to use it, UIC has to send one of its nurses over to the other facility to perform the operation. I thought that this was an inconvenience for the nurse and patient because it does not make sense why the other facility that has this machine does not train their own nurses to use it since the machine is already there.
Next, we headed to the blood laboratory, and the technician was very helpful and open to all of our questions. She showed us the kit for obtaining the stem cells from patients and the process of preparing and freezing the specimens. I did not notice anything that needs to be improved during these processes except for one thing: the sound that the freezer makes during the freezing process. The freezer makes a very weird and loud exhale of gas sound that I thought was a little disturbing. Moreover, the freezing process takes about an hour because the specimens have to be frozen at a slow pace so the cells does not die. I asked the technician about it, and she said that the noise does not bother her and her colleagues. One of the issues that rarely comes up, but when it does it becomes a big burden for the staff working in the blood bank in the monitoring system for blood storage.
The monitoring system has a detection mechanism that first makes produces a loud alarm when it senses that something is wrong in the blood bank. After 15 minutes, if no one comes to the machine and tries to fix the problem, the machine has an automated system that calls the staff to rush to the machine immediately. The technician said that this occurrence rarely happens during the year, but when it does, it’s usually happens over the weekend at night. Therefore, a staff member has to come into the hospital at night to manually turn off the alarm. The technician mentioned that every time the alarm goes off, it’s always due to an error in the software, not the blood supply itself. As a result, I think that a better monitoring system that can be manually controlled from one of the staff’s phone and a specific report of the type of error should be sent to the technician when the alarm goes off. Other than the freezer noise and the alarm on the monitoring system, the work flow in this blood bank seems to be working efficiently.
Eyeopening Experience
Wednesday August 3rd – Thursday August 4th: On wednesday morning, we spent time participating in rounds in the ICU with the Hematology and Oncology team. I also did rounds in the Pulmonary and Critical Care department, and I noticed that rounds in both departments were pretty similar. Issues such as communication between the fellows and the attending, and between various departments in the hospital is still prevalent and needs to be improved. However, I did notice that rounds in the Hematology and Oncology differ from the Pulmonary and Critical Care department by the amount of patients that each department does at once. In the Hematology and Oncology, the attending does go through the history of about three patients, and then he sees the patients afterwards, while in the Pulmonary department does each patient one by one.
After the morning rounds, we headed back to the stem cell lab. There, Dr. Mahmund gave us a lecture about the current treatments that they offer for blood cancers, and the complications that come along with these methods as well. One major issue that he mentioned was that for someone to get a stem cell transplant, the donor’s blood must match with at least half of the human leukocyte antigen (HLA) that present in the patient’s blood. Dr. Mahmund said that there is a blood donor bank that has all the donor’s data of HLA, however, the human body is so complex that finding a match between donors and recipient is extremely difficult. If a patient does find a match, but the donor does not live in the same area, Dr. Mahmund said that is is very difficult to transport stemcells across the country or the world because survival rates for these cells once they out of the human body is low if they are not kept in extremely cold temperatures. Next, he mentioned that stem cell collection and the actual transplant itself is rarely done in third world countries because they lack the resources such as liquid nitrogen and a refrigerator to keep the stem cells in. Therefore, he proposed that a new method of refrigeration without the need for liquid nitrogen can potentially bring the treatments for blood cancers to third world countries.
On Friday, we spent our morning in the Hematology and Oncology Clinic with Dr. Rondelli. Issues that I saw in the clinic was the scheduling process. The nurse mentioned that scheduling in this department is absolutely hectic because when a patient is late or miss their appointment, it will disorient the whole day. Furthermore, the nurse does her schedule on a large piece of paper, and manually writes out which patients goes into which room. As the day progressed, we noticed that the schedule has become a big scribble mess on the wall because of the rearranging of patients. I thought that a computer program that automatically does the scheduling for the nurse is useful to implement, but the nurse was against the idea because she believes that there are too many outside factors that goes into scheduling patients in each specific room.
After the Hematology and Oncology clinic, we headed back to Radiation Oncology. Today was a pretty emotional day at the clinic because I saw a patient who is at a late stage of lung cancer. She was in extreme pain during her examination, and it was very hard for me to watch. Seeing patients like her really makes me appreciate life more, and it really made me realize how lucky I am that my family and I are in good health. Before I started this rotation, I knew that I would be faced with difficult situations like this, and I actually regretted choosing this rotation at first. Now that I have seen cancer patients coming into and out of clinic for past two weeks, I could not be happier that I choose this rotation because it really opened my eyes on how difficult the lives that these cancer patients live, and this experience really made me treasure the life that I have.
Last Days in a Great Department
Monday August 8th– Thursday August 11th: For our last week in the Clinical Immersion Program, we spent our time in the Radiation Oncology department. We saw patients again on Monday, and we attended the prostate cancer tumor board on Tuesday afternoon. Usual problems such as slow computers and poor internet connectivity is still an issue during the meeting because the physicians need to connect to the internet to get patients’ information. As mentioned in the past blogs, the setup for the tumor board involved a conference table with a microscope at each seat. All the microscopes are attached to one another, and then the pathologist explains what he sees in the biopsy. There were less people at the tumor board this week, and so I got the opportunity to look under the microscope itself. Even though I was very confused when the pathologist explains his interpretation of the biopsy, I thought it was very unique to see all the specialties to have an input into the care of each individual case. The specialties that was there during this tumor board were Radiation Oncology, Surgery, Pathology, and Intravenous Radiology.
On Wednesday, we had a small meeting with the head clinical physicist, and he told us that one of the issues that he sees on a regular basis has to deal with patient flow. He said that there is no protocol that happens when a patient is placed in a room, and the doctor has to have an emergency call in the inpatient unit. He said that in most of these cases, the patient sits in the room waiting for the doctor to come back to the room, and the nurses and other staff members could does not do anything about it. Even though patient flow is not a problem in this department, I feel like a protocol should be created to deal with these emergency situations.
Thursday was our last day in the clinic. Walking in today, I was happy that we did our jobs well by identifying problems in the clinic, but I was sad because I will be leaving this amazing department. The day stated off with a very tough case of a patient in the late stage of lung cancer. What was difficult about this situation was that the patient was very resistant to the treatments proposed by the doctors. He seemed to be against the doctor’s suggestion of him to stop smoking and using drugs. The doctor was afraid that the drugs could hinder his ability to come into treatments in the long run. Radiation treatments consists of the patient coming in five days a week to receive treatments, and the doctor was concerned that the patient would not come to his treatment consistently because of the neurological effects of the drugs.
After seeing the interaction between the doctor and patient, I realize that the situation was very tense because the patient did not want to give up his bad habits. I would not know what to do if I was the physician, but luckily, the patient’s family members were there to help the doctor convince the patient to be compliant with the doctor’s orders. The patient mentioned that he did try to stop taking drugs with one of the programs that the hospital offers, but it did not work so I thought there must be a better way of helping the patient to get over his addiction.
Later that afternoon, we gave our presentation to one of the resident because our mentor was busy with an emergency case. The resident gave us very good feedback about our presentation, and then we discussed our next step solutions with him. The resident gave me some really good ideas on a senior design project that I could pursue in the upcoming school year.
In the end, I thought that Radiation Oncology and Hematology/Oncology was a great exposure to the field of cancer technology. I learned so much from the resident and the attending physicians, and I am very happy with all the experience that I gained during this rotation.
Thank you, This was Amazing
Finally! The Clinical Immersion Program has come to an end. I have learned do much from this whole experience, and I am very grateful to be a part of this program. This last blog post will be a reflection of my experience for the whole program.
In the Pulmonary and Critical Care department, one of the main ideas that I got out of that rotation was patience compliance and education plays a major role in the care of the patient. Patients need to be able to trust their doctor’s orders and be educated on the medications that they use. Similarly, since there are new medications that are constantly being introduced, continuous education to the healthcare providers is also necessary to provide the best quality of care.
On the technology end, one of the biggest issue I saw in this department was the lack of integration between various devices during some procedures. A good example is the Bronchoscopy suite, where there are monitors that show view from the bronchoscope and ultrasound, which are located in different parts of the room. The locations of the monitors are a problem because the physician have to constantly turn his head back and forth between screens while performing the operation, which is a big inconvenience for the doctor.
On the other hand, my experience in Radiation Oncology is much different than the Pulmonary and Critical Care department. First off, the environment in this department was much more relaxed and more technology focused. Coming into this department, I thought that I would be facing difficult conversations with the doctors and patients, but to my surprise, the conversations went very well. The doctor and patient interaction in this department seemed more extensive because treatments for each patient was very unique and depends on a lot of different factors, such as the progression of the disease.
The department did not have many technological problems that I saw, however, reproducibility was one of the major factors that is taken into account when treating the patients. Since most treatments take roughly four to six weeks to complete, all the initial parameters from day one to the last day of treatment must be consistent. Therefore, I thought that the stability polymer that was used to stabilized the patient while they are getting radiation could be improve. The stability polymer takes approximately half an hour to fully conform to the patient, I think that there must be a better way of improving this technology.
Overall, I thought that Clinical Immersion Program was an amazing experience because it really taught me how to look for needs in the medical environment and how to focus my future device design with the user in mind. In the end, I want to thank Dr. Kotche, Dr. Dudek, Dr. Koshy, Dr. Rondelli, Susan, and all the staff members that my team and I met these last six weeks. This has been an wonderful and unforgettable experience, and I am excited to use what I have learned during this internship in the future.
Zaid Zayyad Heading link
-
Zaid Zayyad
The Clinic and Its Many Doors
I spent my first few days of IMED rotation in UIC’s Outpatient Care Center. There I sat in the orthopedic dept.’s clinic and watched as residents ran back and forth to their attending physicians while patients worked their ways in and out of the clinic’s many rooms. At first it didn’t feel like there was much to observe. Everything that happened seemed completely routine and the system chugged along in a relatively regular fashion. In an effort to better understand the inner workings of what was happening, the engineer inside of me gravitated towards the most stressed out looking person in the vicinity.
I walked past what seemed like thousands of residents to the one and only scheduling nurse Jackie. Jackie had a lot on her plate. She moved patients into the clinic, collected information from them, and occasionally directed residents to specific patients’ rooms. I spoke with her while she worked and it soon became clear that there were plenty of little inconveniences in many aspects of both her work and the work of other employees in the clinic. As we spoke I noticed what seemed to be a misplaced bag of refrigerator magnets on her desk. “Oh these? Dr. Mejia uses them to label doors when the clinic is busy.”
I soon learned from Dr. Mejia that keeping track of patients in the clinic was not as simple and straight forward as it seemed. After I pointed out the bag, he was more than happy to stop what he was doing and demonstrate the purpose of his refrigerator magnets on Jackie’s desk, in this clinic, at UIC’s Outpatient Care Center.
In short the magnets were numbers he used on the door frames to signify the order in which patients entered the clinic. A few of them were letters which he occasionally used to mark a room for what its patient needed next. The numbers ensured that everyone could keep track of which patients arrived first and that they were addressed in a timely manner. Here I’ll recall a resident’s account of the occasionally forgotten patient, in the room of the clinic that just happened to be skipped one too many times. Dr. Mejia’s creative solution is an attempt to prevent that from occurring too occasionally. For him it works, and his marking of the rooms with O’s (Operation) and B’s (Brace) are helpful in maintaining the steady flow of patients in to and out of the clinic. In a structure with so many doors, his solution seems to convey a helpful bit of information that is just enough to keep things running smoothly for him and his residents.
While it’s convenient, it’s also kind of not. Every time a patient leaves, each number suddenly belongs on a different door. This amounts to a lot of walking as Dr. Mejia or Jackie try and make this shift of numbers possible. Watching Dr. Mejia make this shift happen for a situation with just four patients seemed like more work than most physicians would sign up for, but to him it was worth it because of the benefit it brought to his patients.
My first few days of watching the dept. of orthopedics functioning have been a learning experience in several ways. In trying to imagine an orthopedic specialist at work, most might picture a surgeon in the OR sawing and drilling in an effort to make some kind of repair to a damaged or dysfunctional segment of a patient’s musculoskeletal system. While this description is partially accurate, I’ve learned it may not encompass many aspects of a surgeon’s work he/she may consider most stressful. Managing patients in a clinic, I’ve learned, is one of those aspects. I look forward to further analyzing our findings together as a team in future conversations with Dr. Mejia and other physicians.
Strengths of Working With a Group
Our first week of immersion has been productive and fairly interesting. I’ll use this entry to quickly mention the diversity of small issues we’ve identified as a team. One thing I’d like to point out is that I’ve noticed our diversity as a team allows us to identify a fairly wide variety of problems that one person alone would not be capable of seeing. Brief and intermittent group discussions about our finding are incredibly useful in getting to the bottom of a lead someone might have. Here are a few of our findings.
The attending often has issues with rooms that are around the corners. He said that keeping them in mind was hard because they were not in the same hallway as the majority of other doors. For that reason, rooms that are around the corner are most likely to be missed for a little bit longer. Michael pointed out that a simple mirror could solve this issue and easily make looking down a single hallway sufficient. One resident pointed out that people sometimes bump into each other near those corners. This could solve that issue as well.
Mohi realized pretty early on that no one really knew where the attending was at any given time. Plenty of people both residents and nurses would regularly ask for his location amongst each other, yet his whereabouts in the clinic always seemed to be information that simply was not available to everyone. His responsibility in the clinic makes it so that it would definitely be useful to know where one could find him at any given time.
Upon speaking with a resident, Annmarie noticed that patients wasted a lot of time waiting for a resident or physician to send them to x-ray, when they’ve been told they need one before the visit. It would often be marked on their main sheet and yet they were sent to a room in the clinic to wait, upwards of 20 minutes sometimes, for someone that would just move them along in the process. Being sent directly would be helpful.
There were lots of other issues we identified that would improve overall efficiency of the clinic and I’m sure even more that we haven’t. A realization I made this week is that a group of different people is definitely helpful in identifying non-obvious problems.
A New Clinic
Today our team visited a separate orthopedics clinic with Dr. Mark Gonzalez. The clinic, Illinois Bone and Joint Institute (IBJI), was located at 150 N Michigan Ave in the middle of the city. It was interesting to note the many differences between this clinic and the one we had visited previously.
The overall environment in the clinic was the first difference we all noted. At IBJI there was only one resident and about 15 patients scheduled for the entire day. The atmosphere was incredibly relaxed and the physician had plenty of time to sit down and personally look at x-rays for an extended period of time compared to physicians at UIH’s clinic. At UIH some of the physicians we spoke to scheduled upwards of 60-70 patients per day. This along with the 10-15 residents and students that would regularly walk the halls and collect information created a much more cluttered and busy environment. We definitely got the impression that this was a less stressful environment because of the nature of the work.
Additionally, the rooms at IBJI had flags outside that marked the room number. The numbers indicated which patient was in first. This was a system analogous to the one Dr. Mejia had come up with using magnets. The flags at IBJI were managed by a PA and not the physician nor the resident themselves.
As a side note having less patients gave Dr. Gonzalez a chance to talk to us about some of his research. He also presented to us slides from his lectures and gave a brief presentation on engineering in orthopedics. To me it was incredibly helpful in getting a good idea of the types of innovations that are happening in ortho right now.
Overall I look forward to returning to the clinic next week and seeing more of the inner workings of this specialty.
The OR
On Thursday we spent some time in the operating OR with Dr. Gonzalez. It was definitely a change of pace. We all arrived at 6:30 am ready to see the types of surgery that people we had seen in the previous two weeks needed. There were full knee replacements and a hip replacement.
In full knee replacements I noticed that very little was ever estimated by the surgeon. The cuts made on the tibia and femur were completely guided by jigs that were standard. The alignment of the jigs was determined by a computer which could be mounted on the tibia. As the surgeon shifted the patient’s leg forward and back, side to side, the computer used information it collected to compare the motions to it’s database of previous patients. Based on this the surgeon knee where to place the parts of the implant.
One thing I noticed was that the spacing for the polyethylene plates often required several tries before the correct size was determined. To get a good idea first, the surgeon spread the tibia from the femur using a specific tool. Once the space was apparent, the surgeon estimated the size of the plate and tried several. He tested the size by extending the leg and seeing if it could fully extend. To me this part of the process felt very qualitative. It seemed like the only step which required some kind of guess and check.
Overall our first day in the operating room was amazing. I really enjoyed seeing the variety of surgeries that were performed.
Two Methods and One Goal
During our second day in the operating room we saw a set of procedures we had not previously seen. We saw two complete hip replacements, one of which was done anteriorly and one which was done posteriorly. We learned that the anterior method was slowly becoming the more preferred procedure because fewer muscle had to be cut and reattached to the femur. Instead a pocket could be made anteriorly between muscles.
The tools used for both types of procedures were impressive. Since the anterior method required more movement of the leg, the patients leg was attached to a lever which made changing the orientation very easy. The procedure seemed to take a longer time, but many of the residents had not done it previously which could have been the reason.
We noticed that during both procedures several steps required estimation. This included orientation of the cup and placement of the implants into both the femur and the pelvis. We felt that this estimation could be reduced to improve results. Particularly in obese patients, we noticed it was difficult to estimate where bones were and how they were oriented using only surface anatomy.
Overall it was interesting to see two ways of putting in the same type of implant.
During our second day in the operating room we saw a set of procedures we had not previously seen. We saw two complete hip replacements, one of which was done anteriorly and one which was done posteriorly. We learned that the anterior method was slowly becoming the more preferred procedure because fewer muscle had to be cut and reattached to the femur. Instead a pocket could be made anteriorly between muscles.
The tools used for both types of procedures were impressive. Since the anterior method required more movement of the leg, the patients leg was attached to a lever which made changing the orientation very easy. The procedure seemed to take a longer time, but many of the residents had not done it previously which could have been the reason.
We noticed that during both procedures several steps required estimation. This included orientation of the cup and placement of the implants into both the femur and the pelvis. We felt that this estimation could be reduced to improve results. Particularly in obese patients, we noticed it was difficult to estimate where bones were and how they were oriented using only surface anatomy.
Overall it was interesting to see two ways of putting in the same type of implant.
Intro to Transplant Surgery
Tuesday was our first day in transplant surgery. We met in Dr. Jeon’s office and he began to to talk to us about the history of transplant surgery. We discussed cauterizers and the difficulties involved with keeping an organ alive as it transitions from donor to receiver. Additionally we talked about the system that transplant surgeons go through when an organ is ready for transplantation.
Dr. Jeon described to us two types of cauterizers currently in use. He started by giving us the background we needed to understand how they worked. In simple terms cauterization is the heating of tissue using electric current which passes from one part of the tool into the other. When using a monopolar cauterizer, the current travels through one tip and into a plate on the patient’s leg. In the dipolar type, current travels from one tip to the other and the tissue in between is heated. In order to prevent tissue damage by overheating, the cauterizers have been made to pulsate current which allows them to heat tissue more slowly. Dr. Jeon felt that this was a space that could benefit from innovation.
Next we talked about keeping organs alive as they are transferred from one patient to another. We talked about what an organ needs to remain functional and various methods people have tried and the problems they ran into. In the end we got valuable insight on how these limitations effect the lives of transplant surgeons. When organs can last for a few hours outside of the donor’s body, it means surgeons have to be on call all the time in case the match comes in one day, even if it happens at 4am in the morning. As it is right now, completely random events dictate the schedule of transplant surgeons.
Hemostats
On Thursday we saw our first kidney transplant surgery. The surgery was about 6 hours long and took place in two separate operating rooms. In one of the rooms a patient’s kidney was removed using robotic surgery, and in the second the recipient received it. Two surgeons were required for the length of both surgeries.
As Dr. Jeon performed the second half of the surgery on the recipient I noticed that he would occasionally use the hemostat as a channel to conduct the current from a cauterizer. It is, as he mentioned in our talk, very useful to be able to spread the heat of a cauterizer so that it could target a specified area between two plates. Closing a vessel often requires a hemostat. He simply extended that purpose by using it in combination with a cauterizer.
Periodically throughout the operation when he felt he had the hemostat in a position he felt was suitable, he gave the signal and a resident would touch the cauterizer to the hemostat. It seemed to work well as nothing unexpected happened and the method was used throughout the surgery. I did feel it was interesting that although so many products were constructed for this very purpose, Dr. Jeon preferred the familiar feeling of a hemostat in his hands. I remembered his claim that it was the first tool ever made specifically for surgery. To me it makes a lot of sense that he’s most comfortable in continuing to use it in place of newer, less familiar equipment.
Dialysis Clinic
In hemodialysis clinic patients come to use dialysis machines do to impaired kidney function. I learned that these patients come to clinic a few times each week for a total of 12 hours in order to filter their blood using a dialysis machine. In order to send out enough blood, patients have to allow access to a large artery. Sometimes the subclavian is used, but that happens to be incredibly inconvenient for the patients as the port would be on their chests.
The solution to this is creating a fistula. A fistula is the joining of an artery to a vein in order to create a higher rate of blood flow. Generally these fistulas are created in the arm of the patient. It can happen by directly connecting an artery to a vein or by using synthetic tubing between the two in a graft.
The potential problems associated with creating a fistula are many. For one blood can be directed away from the hand sometimes leading to ischemia. The second is increased diameter of the vessel leading to increased preload to the heart which may lead to heart failure. Most commonly however, the site is very vulnerable to infection. A large percentage of fistulas become infected very early leading to corrective operations. One patient we saw had come in 3 times only to be in for another infection the day we visited. The fistulas are also often cosmetically unappealing as they are raised above the skin and surrounded by scar tissue.
It interesting to see how complex taking blood out and returning it to the patient can become. I do feel that there is potential for better solutions to this issue.
Discussing Our Experiences With Dr. Jeon
On Friday we discussed our ideas with Dr. Jeon for the first time. Several interesting ideas surfaced. One of the things we talked about first was the way Dr. Jeon used hemostats during surgery. As noted in an earlier blog, Dr. Jeon cauterizes tissue by first making contact with his hemostat and having an assistant touch the cauterizer to the tool. The tool passes current through to heat the targeted area.
Upon discussing this, we realized that surgeons from all fields of surgery use this very same technique to cauterize tissue. To us it was just interesting enough that surgeons would use these tools together in this way that they were not meant to be used, so we continued to ask if there were any drawbacks. To our surprise there were many.
Dr. Jeon said that in many instances, the current might momentarily pass through his fingers instead of the patient. Additionally he said the hemostats sometimes reached a high temperature. The photo above shows his index finger with several small burns from surgeries he performed.
Our discussion eventually led to talk about existing solutions. We learned that there were many, but that this was still the simplest and most sure way to go. We feel that continuing to explore this issue may lead to important conclusions.
Wrapping Up
Yesterday we gave our final presentation to Dr. Jeon. During part of our presentation we mentioned deficiencies we noticed in the da Vinci system. After the presentation we continued on to discuss robotic surgery and it was interesting to hear about Dr. Jeon’s thoughts.
To Dr. Jeon robotic surgery is nowhere near being used for all types of surgeries. He still believes that kidney transplants are actually more effectively done by hand. Part of the reason he says, is the design of the robot itself. He brought up several good points.
First off he mentioned that changing the instruments takes too much time. “It’s not a robot” he said, “if can’t do that on its own”. He brings up a good point. Many robotic surgeries actually take longer than their hand counterparts. This could be a reason why.
Along the same lines he mentioned that in robotic surgery, the surgeon is not in complete control. He began to describe the differences. In surgeries done by hand the surgeon is right up against the operating table he is the closest to the patient. Whatever he needs is handed to him by an assistant instantly. With robots there’s just too much lag. From our observations I could not agree more.
Finally he brought up what we had noticed in the OR. Communication is just too difficult with the da Vinci system. The speaker system is not built for direct communication with so many people in the OR doing their jobs.
Overall I can understand and agree with Dr. Jeon on a lot of points, but in the end we both came to the conclusion that it is a system that is slowly improving every day.







