Students: Part 1
Najah Ahsan

Najah Ahsan
My name is Najah Ahsan and I am a rising Senior in the Bioengineering Department at the University of Illinois at Chicago with a concentration in Cell and Tissue Engineering. As a Bioengineer, I am committed to apply my knowledge and experience in developing products that can improve the quality of life of people. It is imperative that engineers not only be able to design products efficiently, but also understand how each product functions in the environment for which it has been developed. Therefore, it is very important to understand the needs of physicians, patients and others involved in the treatment process for successful implementation of a medical device. The Clinical Immersion Program is an unique opportunity to observe clinical environment, participate in discussions with physicians, patients and other caregivers, and observe surgical procedures. The hands-on experience involving examination, diagnosis, and treatment provide insight about the needs of physicians and patients, and the participants gain invaluable knowledge about concerns that encourage them to start thinking about potential solutions. Please feel free to send me an email if you have any questions about my blog. Thank you!
Najah Ahsan Blog
Najah Ahsan Blog
Introduction To Program – First Few Days
Najah Ahsan Blog

The first few days of the Clinical Immersion Program have been wonderful. On the first day, I met the other members of my group (for the Pulmonary Critical Care rotation) and we were all introduced to the specific details regarding the program. We also went through a presentation discussing user-centered medical device designs. This was defined as being “an approach that brings the user’s needs into consideration at every stage of the design process of the project”. We also discussed how user-centered design and medical device development were different and that a good user experience could be reached at the intersection of technology, business, and human values. In order to better understand the design approach, we reviewed a case study about infusion pumps and answered the following questions in teams: “What is the systematic problem that needs to be addressed?”, “Who are the users?”, “What are the shortcomings of the existing design?”, and “How will the device be used?”. After lunch we went through fun exercises to bond as a group and discussed the aspects of the program that we were excited for and the parts that we were nervous about.
Najah Ahsan Blog

The rest of the first week in the Clinical Immersion Program has been very eventful. On Thursday (June 1, 2017), we went to visit the Pulmonary Hypertension Clinic. Initially, the team and I sat in a room where the Attending Physician (Dr. Machado) and fellows discussed patient symptoms and care plans. There were computers in the room for accessing patient information and monitors for viewing images. We were shown a patient’s CAT Scan of lungs (images showed heavy scarring) and then accompanied Dr. Machado when he went to check the patient. During the visit, we learned about a technique that is used to test for pulmonary hypertension called cardiac catheterization. It measures pressure in the lungs and can lead to a diagnosis of the condition. In addition, we learned that pulmonary rehab is an option for patients to strengthen their lungs. The physician mentioned that cardiac catheterization is preferred for diagnosis purposes because echocardiograms can be incorrect when determining the pressure levels in the lungs. Next, we went to visit another patient who had completed a six minute walk test earlier. The physician pulled up the patient’s previous records on his computer and compared with the most recent results for discussions. The third patient that we visited suffered from a rare condition called scleroderma and also suffered from pulmonary hypertension. It was explained to us that scleroderma causes hardening of the skin (texture becomes leathery) and arteries. Having both scleroderma and pulmonary hypertension is very rare. We went on to observe the visits of two more patients and observed the checking of their pumps and inhaler discussions.
During all of the patient check-ups, I noticed that the physicians were using the computer in the room (every room had a computer) to look up patient history. The patients were asked to sit on beds while getting their breathing checked. During one of the visits, the foot pedal was pressed to control bed position (move the top part forward), but the pedal/bed was not working. So, the physician asked him to raise his legs for observation.
For the second part of the day, we went to the PFT (Pulmonary Function Test) Lab. The technician was using various machines to test the impact of a patient’s asthma medication. The software automatically converted the units of the measurements (example: inches to centimeters). The first machine was to conduct a spirometry test (patient breathed in and out in the machine) and the software was capable of allowing “good” data from various tests to be attached with the best version of final data. As a result, the technician did not need to conduct tests over and over to get a good overall data set. The second test, the “diffusing capacity test” determined the patient’s lung efficiency. The American Thoracic Society has guidleine for what is considered an acceptable result for this test. A small level of carbon monoxide is used in this test, so the technician had the patient wait two minutes before conducting the next test. In the third test “body plethysmography”, the patient sat on a glass box-type machine and the test run was pressure based. For this machine, the technician mentioned that it would be convenient if the microphone that she used would turn on when she was using the screen (currently she has to turn on the microphone manually). After all the tests ran the first time, the patient used his inhaler and two of the tests were repeated to determine if there was any improvement. At the end of the visit, a printout of all the results were provided to the patient.
The technician said that 10 – 14 patients visit the PFT lab on average per day. She stated that the changes in the health care system has led to a decrease in the number of patients coming in for testing. We looked at the mouthpiece used by the patients for the machines and it was explained to us that the piece had a built-in filter for sanitary purposes. In addition, the first machine had a rapid gas analyzer. In terms of the software, the technician mentioned that the equipment was based on Microsoft, so it was easier to learn about and train others about the new devices. Before our time at the PFT Lab ended for the day, the technician told us that a pre-registration system for patient check-ins would make the process much more efficient and less stressful for everyone.
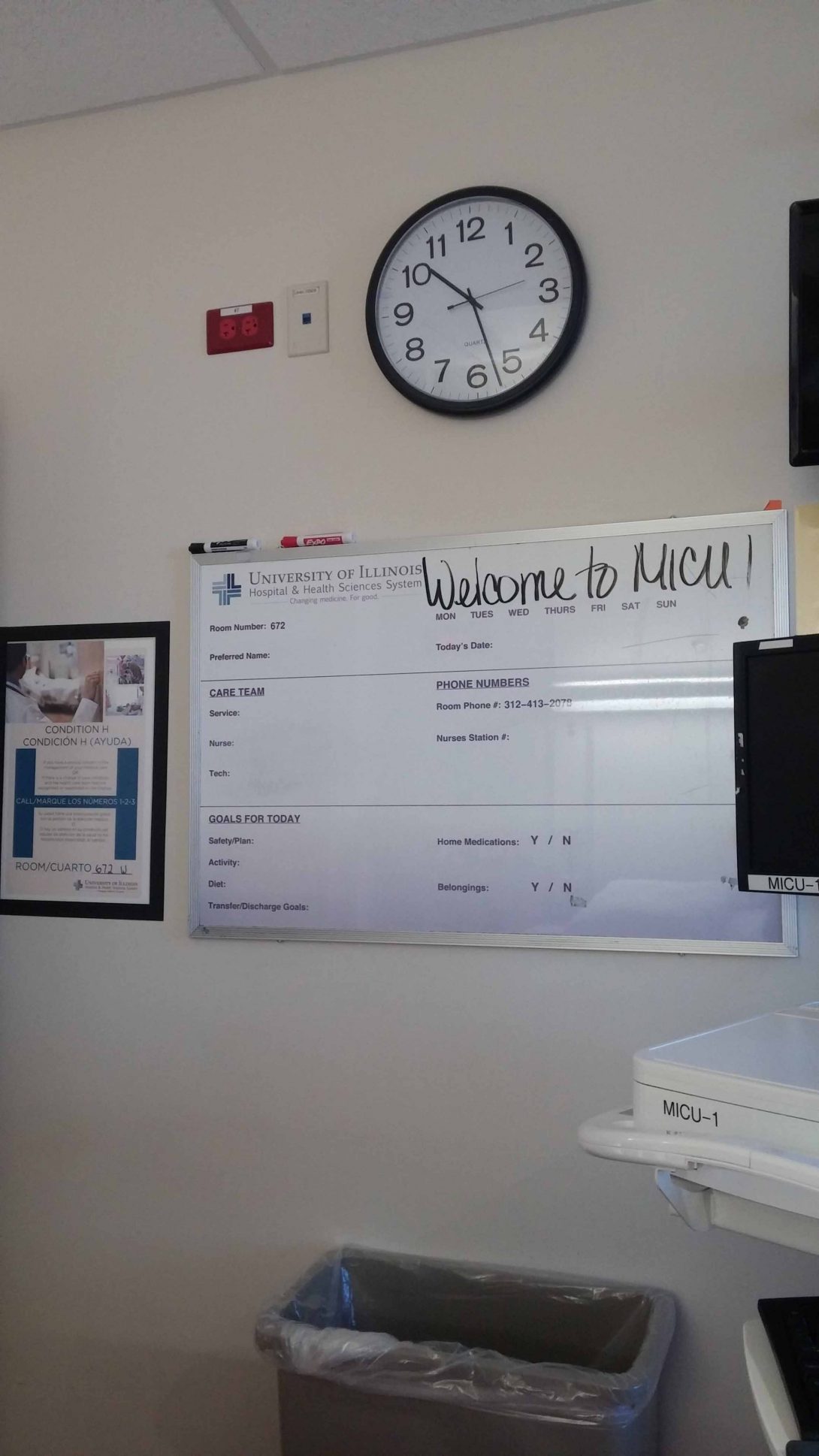
On Friday (June 2), our time was split between the MICU and the Sleep Clinic. In the MICU, we observed the morning rounds. A large group of interns, nurses, and fellows (at least 10 people) gathered in front of the patient room and Dr. Machado listened to the patient details and care plans that were being summarized. A nurse wheeled around a computer and Dr. Machado used a small table to write his notes on. I noticed that those listening to the discussion in front of the patient rooms frequently took notes (everyone was provided a printout of the patient information based on data from 6:30 AM). We went around the floor and the time spent on each patient seemed to vary based on the severity of each case. After discussion, Dr. Machado and a few others would go into the rooms to say hello to the patient. Each patient room had a window, TV and glass doors. Two monitors were placed on the wall for both sides of the floor and had all of the patient heart rate information displayed. The nurses’ station was located in the middle of the floor and the patient rooms were around it. A large screen behind the nurse station had the patient contact status listed (contact, non-contact, etc.) It was a little difficult at first to differentiate the nurses and interns because they were all dressed similarly. After visiting the patient rooms, the entire group went to a room to view the scans of patients on a big monitor. It seemed like they were unable to watch the Echo video because the computer did not have the required software installed. It appeared that the patients were assigned to one of two teams and kept track of that way (in terms of deciding whether they leave or stay in the MICU). Overall, the MICU was fairly noisy and I could hear the phones at the nurses’ station ringing at almost all times. In addition, there were always discussions happening during rounds and various alarms and beeping sounds coming from the rooms.
The Sleep Clinic was a very different environment from the MICU. The office and rooms were very quiet compared to the MICU, and there was much less traffic in the hallways. The clinic runs nine rooms at a time and the exam rooms are used as sleep study rooms at night. Each room has a TV, bed, computer, bathroom and equipment for monitoring the patients. For testing, the EEG, EKG, and EMG wires are connected to a headbox which is connected to a base station.Two patients are assigned to each technician. We met with Dr. Najjar and he mentioned that the Electronic Medical Record was not very good and that there was a lot of room for improvement. For example, it was slightly inconvenient when Dr. Najjar was looking at his schedule, he needed to manually extend the columns to view his whole schedule. Our group of four was split in half and each group went with a fellow. There seemed to be a consistent routine where the fellows would meet with a patient, record new information on the computer in each exam room, then the fellow would meet with Dr. Najjar to discuss the plan. Then the doctor would go to have a conversation with the patient. I thought it was amazing how the sleep studies provided data that helped the physicians accurately diagnose issues like sleep apnea and narcolepsy.
This week was filled with new experiences and I am excited for next week!
Week 2 – Part 1
Najah Ahsan Blog
On Monday, each group gave a presentation about their rotations. It was a great opportunity to learn about their experiences in different environments. Later in the day, we completed an interview activity where we asked a partner to describe their perfect day. The last task on Monday was to use post-it notes to write down our observations and put them on a large white foam board. My group divided our notes into two categories, observations and suggestions, and divided the board into sections based on the various clinics and floors we have visited. I know this method will be extremely useful to maintain our notes in a more visual way.
On Tuesday morning, we visited the MICU. I could immediately tell that the group going through rounds was smaller than the group we had seen last week (it seemed like only Team 2 was doing rounds with the Attending Physician this morning). This allowed the group to move more quickly from room to room. All of the team members were once again taking notes on their patient sheets. This practice caused me to wonder if using technology such as iPads or tablets would make referencing patient sheets and note-taking easier. Some of the rooms being entered were “Contact Plus” rooms and I noticed that each of these rooms had a chest with gowns, gloves, masks and disinfectant wipes. The individuals entering these rooms would discard these items in the trash inside the room. Also, there were stethoscopes hanging above the beds in these rooms for physicians to use. I noticed that those entering the patient rooms carried a blue mask with them from room to room(some had it wrapped around their elbow). After rounds, we looked at the scans on the big monitor in the room where Team 2 sits. While talking to the Attending Physician and the Pharmacist, we learned that a new system that connects the electronic medical record to the infusion pumps will eventually be introduced to the MICU. The system will allow infusion pumps to control dosages automatically based on values changed in the record. This will help prevent medication mix-ups and human error in dose control. The Attending Physician also made an interesting prediction, stating that with the way that ultrasounds are used to get information, the stethoscope may eventually be replaced with hand-held ultrasounds. The last procedure we observed was a Diagnostic Thoracentesis where fluid was being drained from around the lung. An initial ultrasound was important to complete to get a good visual on the area so that the resident and fellow could avoid hitting an artery. The needle being used for the procedure was blunt to avoid puncturing the lung.
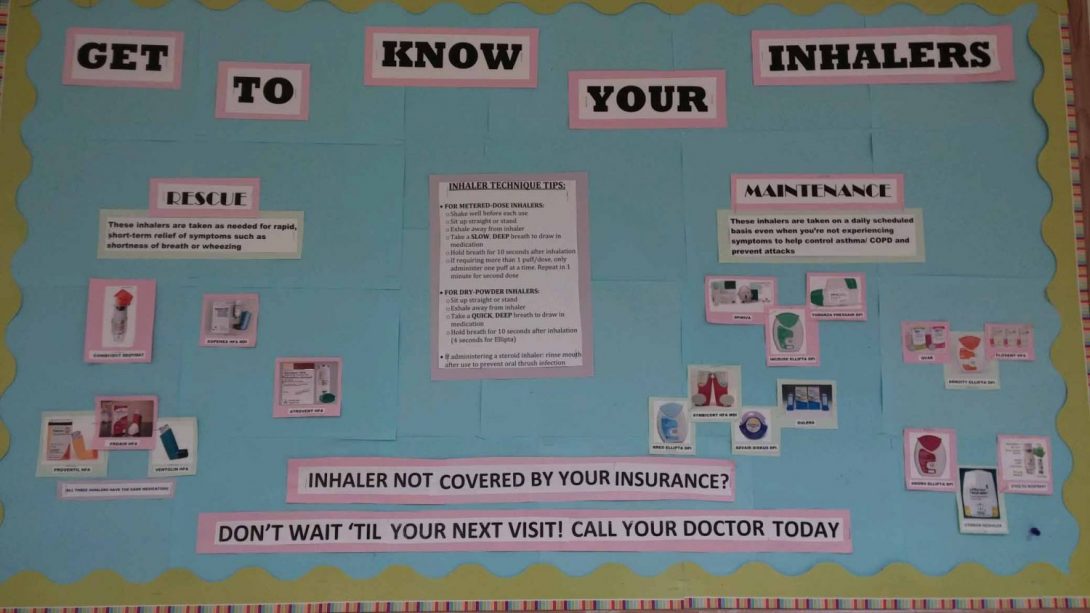
The second half of Tuesday was spent in the Pulmonary Fellows Clinic. The first patient we visited mentioned that her oxygen tank was inconvenient for her to carry. Unlike the oxygen tank that could be rolled around, the patient had to carry the smaller tank in a side bag. The patient also mentioned that the oxygen tubes got tangled fairly easily. Overall, it seemed that inhaler discussions were the most common in the clinic. A major issue that the Nurse Practitioner told us about was that many of the patients mixed up their inhalers (they would exchange the controller and rescue). In addition, she mentioned that it was important for patients to understand that they need to take care of their heath consistently. I noticed that a lot of documentation was involved in the patient care process (seemed that just as much time was required for documentation as for the patient visit), and the physician mentioned that these requirements were being increased.
On Wednesday, our time was split between the Pulmonary Function Testing Lab and observing procedures. We visited the other PFT Lab and it was smaller than the other PFT lab room. There were fewer piece of equipment, so there was enough room for the technician, patient and our group. The technician was running the same tests that were done last week (spirometry, diffusion capacity, body plethysmography, etc.). In this room, instead of using two different machines for the testing, only one was used (door for the Masterscreen Body Device was left open for first part and closed for the second part). The technician explained the tests as he did them and also stated that he has to adjust the ambient conditions for calculations and calibrate the machine every morning. This device is older than the one in the other room and does not have a sample tubing component. In the afternoon, we observed a bronchoscopy (BAL) where the physicians wanted to check a small nodule in the lungs. The tip of the scope for this procedure was able to move up and down with a button, but the doctor needed to physically turn the device if they wanted to move it left or right. The scope itself had a lens and another part that could take in and shoot out liquids (such as saline or numbing medication). The physician and technician mentioned that one of the other scopes, the EBUS bronchoscope (utilizes ultrasound), was leaking. As the department only has one EBUS scope, all the procedures using the device needed to be rescheduled.
Week 2 – Part 2
Najah Ahsan Blog

The majority of time on Thursday was spent in the Pulmonary Hypertension Clinic. Each patient visit consisted of a visit from the Pharmacist, Fellow, and both the Attending and Fellow. When talking with the Pharmacist, we learned that she goes to talk about the medications with the patients and tries to make sure that they know how to take them correctly. She follows a template so that she is able to maintain ten minute visits with each patient. When looking up patient information/records, the Pharmacist mentioned that it is much easier if they get all of their care at UIC (as records are easily available). The last patient of the day required a translator and the Fellow used the phone located in the exam room to call an interpreter. The interpreter translated for both the patient and physician and was heard via speaker. Overall the call worked, but I noticed that it was a little bit difficult to clearly hear what the interpreter was saying because of background noise coming from his office.
On Friday, our first stop was at the MICU. During rounds, the Residents, Interns, Nurses, Fellows, Attending and Pharmacists discussed the patient care plans for each patient. The Clinical Pharmacist made an announcement to the group about a new Nanosphere DNA Detection device in the Microlab that could be used for testing patients. We also observed the ventilator system and an ultrasound being conducted on a patient. The ventilator is an important part in Pulmonary Care and uses positive pressure for treatment (as opposed to the negative pressure the body uses for breathing).Within a few days, the ventilator system can cause issues for the patient.
In the afternoon we went to the Sleep Clinic. We were given the task of obtaining background information about the patients, their reason for the visit and completed the Epworth Sleepiness Scale form with them. We asked patients about their sleep schedules, snoring, breathing, etc. The Epworth Sleepiness Scale is a form with a series of scenarios that the patient ranks from zero (would never fall asleep) to three (high chance of falling asleep). The total score helps the physician evaluate their tiredness. After gathering the information, we reported our notes to the Fellow, who then went to see the patient for their exam. It seemed that the patients liked talking to us. This was a great experience and I enjoyed being to talk to patients and listen to the physician use the information to find a plan to help them.
Week 3 – Part 1
Najah Ahsan Blog

On Monday we listened to the presentations given by each of the groups about their rotations. It was interesting to hear about the patterns and issues that they were all observing. Everyone seemed to have a great time observing the surgeries and learning about devices that were being used. Afterwards, we learned about the components of a need statement and reviewed examples of underdeveloped and revised statements. Lastly, we went back to our observation boards, added more notes from the week, organized our post-its by category and wrote a few need statements for Pulmonary and Critical Care.
During our time in the MICU, we focused on asking the residents about ICU delirium. They stated that ICU delirium can occur in patients when they have been in the hospital for an extended period of time and seems to occur more frequently in elderly patients. The delirium can change on an hourly basis and patients can become especially confused during nighttime. To help prevent delirium, the residents mentioned that it would be beneficial if a good sleep/wake cycle could be maintained (such as by keeping blinds open during the day and closed at night) and patients feel as comfortable as possible (for example, sometimes it is helpful if the patient’s family would bring pictures from home). In the ICU, regulating the sleep/wake cycle is difficult because patients need to be woken up for testing early in the morning to have results for rounds at 8 AM. In addition, the IV poles beeping sound and bed alarms can wake patients up or prevent them from being able to fall asleep. One of the residents made it very clear that benzodiazepines were not good treatment options for delirium. She said that many professionals still used benzodiazepines because they were not well educated on the patient delirium issue and are unfamiliar with the treatment. When patients, especially the elderly, are treated with benzodiazepines they have a higher risk of falling. One of the other residents mentioned that another hospital that he had worked at had signs such as “Call, Don’t Fall” in the rooms and above the patient beds to remind confused patients that they need to ask for help before trying to go anywhere.
During our time in the Pulmonary Fellows Clinic, we went to see patients with both the Nurse Practitioner and Attending Physician. The issues that were addressed in the clinic included possible sleep apnea, problems related to COPD (Chronic Obstructive Pulmonary Disease), and sarcoidosis. For the patient with the suspected sleep apnea, the Nurse Practitioner mentioned that the patient would have to undergo a sleep study, but that it would have to be scheduled in two months because the clinic appointments are booked until then. It seemed that this could be related to the fact that the clinic only has nine rooms for the sleep studies that happen each night. One of the other discussions that appeared to be fairly common was the patient wondering which medications insurance would cover. In one of the cases, the inhaler that one of the patients had been taking (that had been benefitting them) had a significant price increase and he could no longer afford to purchase that brand. The physician and nurse told him that they would see what they could do in terms of getting the same medication or maybe seeing if there was another type that they could give him. Needing to check which of the inhalers or other medications were covered by patient insurance seemed to be a consistent part of the routine for the pharmacists and physicians.
We also had the opportunity to listen to one of the Fellows explain symptoms of Pulmonary Hypertension in more detail. To diagnose Pulmonary Hypertension, a right-heart catheterization needs to be done and the mean pulmonary artery pressure would greater than 25. Other tests to be done are: cardiac output, left ventricular end-diastolic pressure, pulmonary artery wedge pressure, resistance, and pulmonary vascular resistance. We then learned about the five pulmonary hypertension groups and the risks and test results associated with the conditions. The Fellow later explained that it is important to diagnose Group IV because it is treatable and can be cured. It can be treated through a procedure called a Pulmonary Endarterectomy or a vasodilator (for those unable to undergo the procedure). Group I (Pulmonary Arterial Hypertension) was also further explained to be associated with drugs, HIV, congenital disorders, collagen vascular disease (such as scleroderma), and cirrhosis. It was also surprising to hear that on the west coast, the most common drugs to cause pulmonary arterial hypertension are weight loss drugs. In terms of the pathophysiology of Pulmonary Arterial Hypertension, the Fellow explained the associated causes are nitric oxide deficiency, increased endothelin and prostacyclin reduction. The issue with the drugs being used to treat these conditions have not shown to improve mortality. Also, trying to conduct a large study for Pulmonary Hypertension is difficult because it is a rare disease.
Week 3 – Part 2
Najah Ahsan Blog

In the Pulmonary Hypertension Clinic, we saw a few patients suffering from various symptoms related to pulmonary hypertension. To fully diagnose and understand the level of pulmonary hypertension, patients need to undergo a test called right heart catheterization. The patients that needed to go through this procedure prior to their visit said that it was extremely painful. One of the patients also said that she had pain in her arm for a couple of weeks after it was done and felt that a few of her fingers were numb for that time as well. This was the first time in the clinic that I had heard patients complain about the pain associated with the test. While discussing with the nurse, we learned that anesthesia is not used for this procedure and patients can experience pain/discomfort.
During one of the appointments, the physician reliance on technology was clear. The patient in the room needed to discuss her recent test results with the physician, however while the physician tried to pull up the records on the computer, the machine turned off. The physician tried to fix the computer but was unable to turn it back on. As a result, he had to go find an empty exam room and move the patient there to complete the conversation. This made me wonder what would happen in the event that a backup computer in another room was not available and felt the need of a contingency plan in case all rooms were occupied. Once the computer dilemma was quickly resolved, the nurse came to demonstrate how to use an inhaler system for Tyvaso (prostacyclin). The nurse explained how to assemble the system and how often to administer the medication.
During our second visit to the MICU for the week, we listened to a presentation given by one of the Fellows about “Surviving Sepsis Guidelines”. We also talked to an anesthesiologist about her work and what she has seen with patients suffering from delirium during her time in the MICU. Similar to our conversation with the other residents, she mentioned that benzodiazepines could negatively impact the cognitive function of the elderly in particular. She also said that getting the patients out of the ICU, bringing family, regulating the sleep/wake cycle and re-orientation of the patient would help decrease the delirium.
The last stop on Friday was at a clinic where we were able to follow the Attending and Fellows for their patient visits. The physicians were extremely welcoming and explained each patient’s condition and scans with us. On the topic of ICU delirium, the Attending told us that when he was an intern forty years ago that the lights would be turned off and the nurses were very serious about making sure everyone was quiet and keeping doors closed so that the patients could rest.
This was an eventful week where we learned quite a bit from our rotation and look forward to the next week.
Week 4 – Part 1
Najah Ahsan Blog
We started off this week learning about the needs that the other groups had identified during their rotations. It was really exciting to see that our weeks of observations have allowed us to identify potential improvement that we could begin to address. Our team initially identified four areas of need related to MICU delirium, patient inhaler usage, physician time with patients, and physician visibility during pulmonary procedures. Although these are all extremely interesting topics, we felt that it would be the most feasible to focus on two topics instead of attempting to address all four of the identified needs. Therefore, our group decided to focus on patient delirium in the MICU and patient inhaler usage. In terms of patient delirium, we would like to find a way to decrease/prevent delirium in order to positively impact the patient’s recovery. For the inhaler use, we would like to educate patients on the proper way to use their medications to allow them to receive the most benefit from their treatments.
The first clinic that we visited this week was pretty busy. There were three Fellows, a Nurse Practitioner and an Attending seeing patients. The majority of patients that I observed had a history of smoking and were visiting the clinic due to issues such as shortness of breath, Chronic Obstructive Pulmonary Disease (COPD), Obesity Hypoventilation Syndrome, and asthma. One of the first patient for the day was a first time patient and the physician needed to ask a series of background questions to establish a record for the patient. I noticed that she explained why she was asking each question and how it related to the patient’s care. The physician later explained to me that she did this to make the patient feel comfortable. She said that when asked personal questions, some patients feel that the physician is judging them for their choices and she wants them to know that these questions are necessary and that she makes no judgment and wants to help them. A few of the patients required oxygen tanks, but did not bring them to the office and admitted that they do not like carrying around the tank. the large rolling tanks seemed to cause more inconvenience, but the smaller tanks need to be refilled more often, which is also a source of inconvenience. A patient who were still smoking were made aware of the Smoking Cessation Clinic and offered help to quit. the physicians tried to convince them to stop smoking as it would greatly help in preventing further damage to their lungs. The patient seemed interested in the clinic, but wanted to try to quit by himself before coming back to seek their professional help.
In the MICU, we focused on looking further into the environment and noise levels. The first thing we noticed was the doors to the MICU were wide open. We entered an empty patient room and tried to determine what the patients would hear from the outside. When the door was closed, the noises from the hallway were significantly muffled. In the hallway in front of two empty rooms, we tested how far noise could travel by having one part of our group discuss in a normal tone of voice and the other part of our group walk in the opposite direction and they reported that they could move 15 – 20 feet away and still be able to hear us vaguely. This indicated that patients in the MICU who have their doors open during rounds would most likely be able to clearly hear the physicians and nurses discussing in the hallway. I also noticed that one side of the MICU floor had sliding glass doors while the other had regular wooden doors. The glass door rooms allowed light from the hallway to enter the rooms and had curtains that surrounded the patient bed for privacy. The curtains were not open around most of the patient beds and the doors were kept open in the majority of the rooms. I wonder if there is a reason that the curtains are kept just around the bed and not just in front of the door (seems like it may be easier if curtains were placed in front of the door). The majority of the rooms seemed to have their lights off. It was interesting to see that there were new observations that we were able to make about the MICU environment once we focused in on one particular topic in that area.
I look forward to the rest of the week!
Week 4- Part 2
Najah Ahsan Blog
During the second half of the week, I paid close attention to the environment in the clinic. In the Outpatient Care Clinic, I noticed that the hallway had lots of natural light and the hallways were very wide. There is also seating available in the hallway in addition to the seats in each of the clinic rooms. The clinic room that we visit each week is located in 3C (the Pulmonary and Allergy Clinics are held here). Along the hallway there are multiple clinic rooms/offices and are labeled 3A – 3F. Overall, I noticed that the building was very well organized.
We spoke with one of the Fellows about the topics that we have identified as potential areas for improvement. On the topic of MICU delirium, the physician mentioned that in terms of treatment, he believes that most people should know not to treat patients with benzodiazepines. He also thought that our idea to have family pictures in the patient’s room (to make them feel more comfortable) would benefit the patients. He also suggested we look into the impact of calming music on patient health. When we discussed regulating the sleep/wake cycle for the patients, the physician mentioned that lights are generally turned off at 7 or 8 PM and they are not so good at turning them back on during the day. To prevent noise disruption for the patients, we discussed with the Fellow about the possibility of providing the patients with ear plugs. He thought that this was a good idea, but cautioned that they would need to be visible to the physicians to prevent any confusion about the patient’s responsiveness.
With respect to the need for better patient inhaler compliance, the Fellow mentioned that one of the pharmacists in clinic demonstrates proper inhaler technique to patients. However, the pharmacist is only in clinic on Friday, so not all the patients are able to benefit from their demonstrations. The Fellow mentions that he plays YouTube videos for his patients about proper inhaler technique in their exam rooms while they wait, but he is not sure if other physicians do this. He thought a box to store inhalers would be beneficial (similar to daily pill boxes) and also thought our idea about labeling Controller and Rescue inhalers with a “C” and “R”, respectively, would be very helpful to prevent confusion. We also met with our mentor, who had a positive response to our ideas. He also mentioned that education was important in terms of letting patients and physicians know about the inhalers and delirium issues.
We were able to watch a procedure where an Endobronchial Ultrasound (EBUS) was used to identify lymph nodes for biopsy. This patient had previously had a biopsy done on a tumor in one of his lungs, but it only brought up dead cells. Therefore, the lymph nodes were being targeted this time to try to get a better biopsy. I noticed the ultrasound monitor was placed behind the physicians which seemed a little inconvenient (they needed to turn their heads while holding the scope).
I look forward to the next week and further developing our ideas.
Week 5 – Part 1
Najah Ahsan Blog
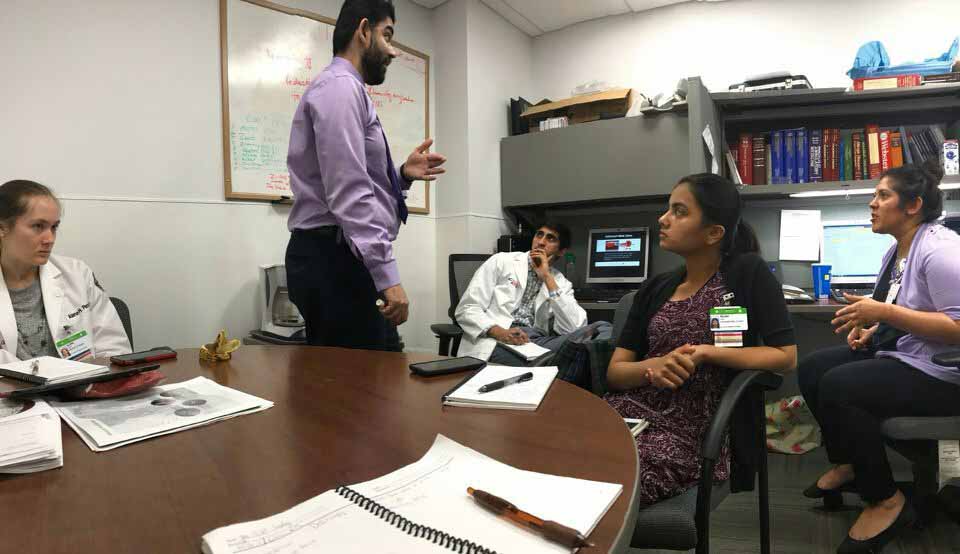
As our time in the hospital is coming to an end, this week was important to make our last observations and analysis in our rotations. The importance of communication between the Fellows, Residents, Interns and Medical Students (Fourth Year) was extremely clear. I have noticed that the “Fellows Room” is an extremely important place for them. They discuss every patient, ask questions about care plans, discuss with other departments via phone and fully discuss the patients prior to seeing them for consultations. This is also the area where the Fellows explain various concepts and field questions from the Residents, Interns, and Students. Throughout this week so far (as well as in other weeks), I have observed that the Fellows gladly answer any questions and make clarifications, and are able to do so in a more relaxed environment in the Fellow Room.
In the first clinic, the Nurse Practitioner suggested a color scheme for the inhaler stickers that we mentioned last week. She mentioned that it may be nice to have the Controller (C) stickers to be green and the Rescue (R) inhalers to be red, for it to be easy for the patients to identify the color and letter on the side of their inhaler. She also told us about a “smart pill” that has begun to be offered at Rush University Medical Center that alerts the patient when they forget to ingest a pill. It was interesting to think about the possible elimination of patients forgetting to use their inhalers or other medications if such a technology were introduced to UI Health System. One of the Fellows showed us how to tell the difference between an ICD and pacemaker on a scan as it is important to be able to determine which piece of equipment they have before treatment or further tests. During one of the patient visits, we were able to observe a different type of translator. During Week Two of this program, we saw that the physician called a translator and the patient spoke to him on the phone. This week, an “In-Demand Interpreter” system where a translator was video-called was used. This system took a few minutes to get and setup, but the video and sound quality was very good. The patients seemed very comfortable as they were able to see the translator. Overall the conversation flowed much better than the phone conversation that we witnessed a few weeks ago. The aspect of the conversation that seemed a bit confusing for both the physician and patient was the medication review. It was hard for the patient to understand the medication names. So, the Pharmacy students were given the task of reviewing the medications with the patients after the Fellow visit (this is normally the case).
Similar to previous weeks, scheduling and appointment/procedure times seemed to be difficult to predict. While reviewing consultation times, a Fellow noticed that a patient who would require a translator was only scheduled for a 20 minute slot. However, patients requiring a translator should be given a 40 minute slot. The Fellow then requested that the appointment be updated to reflect the time required. I thought it was very helpful that the appointment durations could be selected to reflect the need of the patient. Also, the procedures (such as bronchoscopies) often run later than scheduled due to factors often outside of the physician’s control (patient arrival time, preparation time, etc).
I look forward to the rest of the week.
Week 5 – Part 2
Najah Ahsan Blog

During the second half of the week, in one of the clinics the physicians and nurses were mentioning the importance for patients to understand that they need to take control of their health. During one of the appointments, a patient mentioned that he had stopped taking his medication, missed his scheduled tests, and had not seen a primary care physician for some time. This particular interaction stood out to me because it was very clear that the physicians were concerned about this patient and were trying their best to convince him to be more involved in taking care of his health (especially to avoid a previous health issue from happening again). Although the patient said that he would start going to a doctor regularly and taking medications, it was still a worry that he would not. In general, the physicians were concerned that the patients were not following instructions in their care plan.
During the procedures for this week, we were given an opportunity to assist the physicians a little bit during one of the bronchoscopies (filling syringes with saline, lidocaine). It was a great opportunity to be able to be a little involved in the procedure and help the physicians with a procedure that we have seen so many times during this clinical experience. The Attending and Fellow were extremely clear with what they wanted prepared and showed me exactly what was needed prior to the procedure itself.
I look forward to preparing our final presentation and appreciate the clinical experience.
Thank you
Najah Ahsan Blog

I feel truly grateful to have been able to be a part of the Clinical Immersion Program. Everyone we encountered in our Pulmonary and Critical Care rotation was extremely welcoming and accommodating. This was such a wonderful opportunity to be able to shadow the physicians and identify potential solutions to improve the patient care in the hospital. Our final presentation to our mentor and to the rest of the members of the program was very successful and we were excited to share our observations and solutions. We look forward to continue this effort and implement our designs.
Usman Akhter

Usman Akhter Blog
Usman Akhter Blog
Wednesday 05/31 Week 1 Blog post 1
Usman Akhter Blog
Wed. 05/31 – Week 1 blog post part 1
These first few days of Clinical Immersion have been eventful. Day 1 at the Innovation Center was introductions to our new teams and discussions of what to expect. I am in Urology with Ben and Shana. We talked about design and went through examples of hospital waiting room designs. Seeing waiting rooms with activities for children and iPads was nice, but most of us agreed these things are probably too expensive for hospitals. I also think it’s a problem of hospital management time and prioritization. When building a hospital, CEOs probably find a mentor/advisor who built a successful hospital and copy their actions, including the building blueprint and interior design. Going back after the fact to renovate individual hospital sections might be low priority compared to managing insurance, for example. A 2005 studylooked at hospital design effects and frictions, and they found that, among other issues, there is insufficient compelling evidence of evidence-based hospital design benefits. Being honest about whether we’re going to make any substantial impact is probably one of the hardest parts of design thinking.
On Wednesday, our first day of actual immersion, we went to Mile Square and did not find Dr. Niederberger, but fortunately, Dr. Kocjancic and his team took us under their wing. They sit in an open room with computers against opposite walls, then a hallway further down, then another identical room of people. They don’t know each other despite sitting so close. The team is Dr. Kocjancic, 2 residents (Niki and Ryan), and about 5 MAs (medical assistants; Marisol, Gaby, Mario, and others). Doctors get 3 rooms in the clinic and variable residents per attending. They had 37 scheduled patients, and the nurse handles walk-ins as feasible. It looked like Dr. K spent over an hour signing EHR messages. This entailed repeatedly copy-pasting “I saw the patient and confirm…” and hitting sign, patient after patient. They use Powerchart EHR. One resident says the “templates suck” and are clumsy when loading lab data and so prefers EPIC. Most of the team speaks Spanish and made several phone calls to patients in Spanish. In general, I notice everyone seems pretty happy and relaxed, at least compared to my hospital visits earlier at UIH in internal medicine.
The first patient I saw had a right kidney complaint. The MA took vitals, and if patient asks, resident then comes in to get a urine sample, but the patient didn’t ask for it, so she left. The next patient had a ureteral stent for kidney stones, but the flimsy string part hanging through the urethra came out. She had to go to the ER w/ a 103 fever. Niki says this can be common because the string is so flimsy. People often forget to call for a follow-up appointment after a few months to remove the stent. Gaby says it’s not usually an issue because if the patients forget, the team will catch it and contact them.
Niki showed us an IPP, inflatable penile implant, and we noticed the pump part is very hard to press. Still, malleable implants, which stay the same size and just get bent as desired by the patient, are less frequent despite seeming easier to use in my opinion. Implants are used only after pharmaceuticals like Viagara and Cialis are tried. We learned sexual dysfunction is an ambiguous, hard to measure, quality of life issue, so a questionnaire is necessary to quantify satisfaction in some way to get insurance coverage. For whatever reason, a female questionnaire does not yet exist. We learned that psychological basis for dysfunction is uncommon, but when it exists, it’s much more prevalent in males than females.
When looking at MRIs/CTs, the team finds prostates hard to find because they need to look for darkness/shadowing. During a prostate exam I saw, Ryan couldn’t simultaneously hold the man’s penis while adjusting the flexible cystoscope, so the nurse had to help him. Another patient had pilonidal disease. Dr. K injects collagenase, which he said is very expensive, and asks the patient to physically contort the penis to make the calcification dissolve and break apart. The last patient was female and was probed to check if past surgery was successful. They usually keep the lights off to see the monitor for the cystoscope better, but this time had to turn all the lights on to get a better view of the urethra. The nurse says the tools for water in injection/release on the cystoscope and general communication with her team are great and she doesn’t run into any problems or have any complaints.
Fri 06/02 – Week 1 blog post 2
Usman Akhter Blog
On Thursday, we went to the surgical center downtown. We immediately noticed it was quite fancy and swanky. The men’s changing rooms were a bit cramped. The first surgery was a varicocelectomy, with FSH/LH levels around 16, way above the threshold of 4.
After wheeling him into the surgery room and putting him under the anesthesia, the residents shaved his hair. There weren’t enough chairs so they brought one in. They must attach to these large black pads sideways from the table so that the residents/doctor and have arm support as they’re working. I noticed before Dr. Neiderberger walked in that everyone seemed a bit worried about what might make him upset. Dr. Bakare insisted it was just kindness for others, but I suspected it had to do with him leading the surgery. They had to undo all the straps around the patient when Dr. N said the patient was about 1.5 inches too high. They unstrapped him, pushed him down the bed a little further, and re-strapped him. I wondered why they didn’t use the button to lower the bed level. Dr. Bakare was too short to properly maneuver the big head lights on top, so someone helped her. There was no space on the tables for Dr. N’s laptop and camera, so they had to clear stuff up. The anesthesiologist put a large inflatable air bag over the patient’s head. Dr. N mentioned in a past surgery the lights failed, so now they do light checks.
I noticed just set up for surgery (sterilization, placing sheets, strapping patient) takes a long time, at least an hour, though they weren’t in any rush. When scrubbing in for the surgery, you can’t touch anything in the room before getting your gloves and lab coat on, so I imagine it’s easy to accidentally contaminate and have to re-scrub again. Also, you need someone to help you with your gown so that the part you touched with your hands gets covered up as you tie up your gown. We were told to watch out for the wires on the ground sticking up a bit, because we might trip. They placed lines with a marker on the patient’s stomach where they wanted to cut. I wondered if they used permanent marker and what happens if they make a mistake. Do they have erasable markers? As the surgery started, the anesthesiologist kept her hand on the green air bag to monitor patient breathing and checked vitals once in a while. She had a lot of downtime and spent it doing a crossword. I noticed Dr. N get a little frustrated when they wouldn’t get him the right utensil during a particularly tricky, time-sensitive position. Clear communication was important. I also noticed Dr. N’s hands shaking when using the microscope – maybe because the microscope distorted his vision and orientation. The second surgery was testicular sperm extraction and went much faster. The anesthesiologist places tape over the eyes to prevent the cornea from drying out, which I thought was a pretty neat, easy solution.
On Friday, I watched a prostate surgery with a daVinci robot by Dr. Abern. The patient had to scooch from the rolled-in bed to the surgery bed, which looked a little difficult for him. The anesthesiologist had to keep a mask on him tight around the mouth with both hands, leaning back with her back to hold it tight. She got worried because she switched to intubation but forgot to switch off the ventilator because it was in the back and the switch is not easy to see. Another doctor came in and showed her what happened – she says this happens occasionally. She also mentioned that patients without teeth are sometimes harder to intubate/ventilate. I overheard the doctors talking about a recent case complication where a pubic vessel and artery got mistaken for one another because there weren’t clear landmarks on the body. I overheard Dr. Abern mention this a couple times during our surgery as well. I wonder what doctors do in tough-landmark cases. They were missing a razor in the room and had to go get one. While chatting with me, the doctors talked about how some random people will walk in to the hospital with no credentials and start interviewing people or sometimes to steal babies, which I thought was crazy.
I learned the scrubbing process is very specific. You must wash both your hands, then use your back to push the door open, otherwise your hands might be contaminated by the door. I noticed a ‘Stryker’ on-site vendor specialist for machines in the room. I wonder what he does and if he’s in the room for all surgery set-ups. Setting up took about an hour, the same as yesterday. When cutting open the stomach, the doctors/residents used metal clips to pull on the sides of the cut – it looked like it could be somewhat annoying. After another 45 minutes of surgery set up, they pulled up the da Vinci robot and spent the next 3 hours cleaning out adhesions. Apparently, this guy had so many surgeries in the past, that adhesion connections formed and they had to spend 3 hours removing them. During surgery, nurses had to replace the arms of the robot with the necessary utensil. Once they finally got to the prostate and found the cancerous part, they cut it with some tools and used this cool internal bag system that bagged the cancer and sucked itself dry around the cancer. The nurse told me they remove the bag last at the end of the surgery. I noticed the doctor having to point to a monitor next to the resident using da Vinci. He occasionally had trouble explaining the angle he wanted him to point the cutter or probe with his fingers. I wonder if you can draw on the screen like ESPN to show the person on da Vinci on their screen where to probe/cut.
Wed 06/07 – Week 2 blog post 1
Usman Akhter Blog

Wed. 06/07 – Week 2 blog post 1
Our first Monday after shadowing was presentations and group exercises. I noticed Interventional Radiology and our team both recognized difficulties identifying things on MRI/CT scan due to black/white imaging not being clear enough to identify some organs. We did group brainstorming of how observations fit into categories, and our peer practice interviews were a fun practice for when we do the same on our rotations.
On Tuesday, we were at the Urology clinic at Mile Square. There were 26 scheduled patients, way less than the 37 last week. 6 were no-shows, and 6 were seen/complete by 11 am. Nadine, a nurse, told us how important it is to start a new patient with good notes, because later all the doctors are relying on that to get a baseline understanding of the patient. Sometimes, the team forgets to make prescription orders. The lab calls later because the patient shows up, but I imagine there might be times when both sides forget. It looks like residents/fellows take patients first-come first-serve and initial their name on the list of patients so the others know who’s taking that one. Occasionally, I hear grumbling about taking a patient based on their condition or because the resident remembers them being annoying last time, but besides that, it seems like an unbiased fair system of patient assigning. I’m curious if there’s evidence of improved outcomes for randomized patient assignment, but I think it would slow down workflow because no-shows and longer-than-expected visits would screw up any pre-assigned ordering.
The first patient was angry because he came to see the doctor twice, and both times Dr. K was out, and he’s got to miss work each time. He claimed to Nadine that he never got a stent procedure and refused to talk to anyone besides Dr. K. When Dr. K showed up and spoke Spanish with him, his demeanor completely changed and he admitted more symptoms. Nadine says you can note “only wants to see Dr.” in the patient notes so we know to only schedule him when the doctor is in. I imagine this can become a problem if it’s a pattern, because Dr. K can’t see everyone everytime. Plus, it might create longer periods between visits to fit them in the schedule, which might exacerbate their conditions. Wait times listed on the EHR seem to be underestimates. A lot of patients walk up to us and complain they’ve been waiting too long. The team uses MRIs on CDs the patient gets from their primary care physician. One almost didn’t work but after about 5 minutes of tinkering on the computer, we got it loaded up.
A patient with erectile dysfunction half-jokingly gave the idea of a remote-controlled penile prosthesis. The IPP has high satisfaction, but we noticed it’s pretty hard to pump, and a remote control would probably make things easier. Dr. Abern uses myprostatecancerrisk.com, which is supposedly a validated website, to justify biopsies. Nadine takes a long time to write personalized letters for patients explaining medical excuses or embassy permission so that their family can come visit them. She says she doesn’t do templates because each case is pretty unique, but I imagine I could come up with a general enough letter that could be useful. UIC does not use phone media, only mail and pamphlets for patients, but they’re hoping to work on it in the future. I asked Dr. Abern about if he can point things out remotely on daVinci, and he said there are dual control robots but they weren’t available that day in surgery.
On Wednesday, Shana, Ben, and I split up, with me staying at Mile Square. A man had no visible blood in urine, but some amounts were detected microscopically, so the man could have prostate cancer. It could’ve been easy to overlook it because he doesn’t see the blood, but when we found out his wife is a smoker, we realized it’s important to always ask and test. One man says his appointment was at 9 but our computers said 9:45 so he was waiting for an hour. Jelena schedules surgery appointments when anesthesia is involved. She says, understandably, patients often miss appointments for non-invasive, diagnostic procedures, but show up for cancer surgeries. She often gets finance phone calls and has to email Pat, an insurance lady in Indiana. It’s a problem because Pat has no phone number, so Jelena can’t refer patients to her directly. She isn’t allowed to talk about side effects and dangers of no-shows, but she says repeatedly calling people is pretty effective at making them come. She can tell by the tone of their voice whether they care or not about the appointment. I also learned that when medicare doesn’t cover Viagra, we use a cheap generic, sildenafil, from a California compounding company. Having read a bit about the insane patent protection practices on drugs, I wonder how people make generics and how they get approval to sell them in hospitals. The saddest part of the day was when a lady with a long history battling cancer was told her urethra was clear, but she needs CT scan and cystoscopy, because a cancer might be elsewhere in her urinary tract. She reluctantly agreed only to a delayed test because she didn’t want to hear any bad news. Dr. K and Dr. Niki spent about 10 minutes trying to persuade her to do the test before she finally agreed.
Fri 06/09 Week 2- Blog Post 2
Usman Akhter Blog

Thursday and Friday were both in the OR at UIH again. A nurse during the first surgery pointed out a few problems she runs into with the saline bag cart. Basically, there’s a large warning notecard that lies between the hooks, and when the button is clicked to raise the bags on the hooks, the bags get caught on the notecard and rip up, causing all the fluid to fall out. She said this has happened to her a few times. A radiation surgery was scheduled to obliterate kidney stones, but as they went in to find the stone, they couldn’t find it. A large X-ray machine was operated by a tech person and Dr. Abern had to regularly call out “spot,” after which the tech would hit a button to take an x-ray. They checked whether their uteroscope was properly inserted by double checking these x-rays to make sure they didn’t puncture through the ureter, which supposedly is quite common. Once inside the kidney, they couldn’t find the kidney stone, and said it might’ve gotten scooped out when they removed the stent. I was surprised that there’s no confirmation they removed the stone besides not being able to find it with the uteroscope.
96
Normal
0
false
false
false
EN-US
X-NONE
X-NONE
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-parent:””;
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin:0in;
mso-para-margin-bottom:.0001pt;
mso-pagination:widow-orphan;
font-size:12.0pt;
font-family:Calibri;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;}
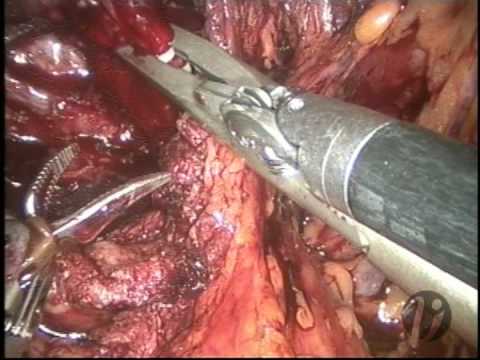
On Friday we saw a prostatectomy with Dr. Abern, Tony, and Niki. Niki helped explain the actual procedure to me as they were cutting past the bladder to the prostate. When removing the prostate, a lot of care was needed to avoid the large arteries, external and internal iliac, and nerves in the area. I heard robotic surgeries might increase risk of cancer spreading, and Niki denied it. The nurse and Niki told me that the trochanter arms on the DaVinci often smack the doctors in the face as they’re working. I asked if the range of motion is limited by all the arms in the way, and Niki said it’s usually not an issue – you can just switch to another arm.
Wed 06/14 Week 3 Blog Post 1
Usman Akhter Blog
Monday at the Innovation Center we spent more time narrowing down our problems in Urology. Ben, Shana and I agreed that patient education regarding bladder removal/prostate cancer, inflatable penile prosthesis (IPP) design, ureteral stent design, and patient turnover in OR rooms were some of the most frequent and biggest issues that we want to address. We found it interesting to hear the pulmonary team talk about inhaler device use problems. By coincidence, we are interested in patient education more generally and find that inhaler technique is a common issue for patients. We wonder what sorts of solutions might work: better handout materials, take home videos, how-tos over text, or anything else.
I was sick on Tuesday but came back to the Mile Square clinic on Wednesday. I saw a patient using the IPP for the past 2 years with no success. He was upset and felt his urologist in Indiana did not properly do the procedure. The IPP didn’t wrap properly around the glans, but Dr. K said this is a common complication and not a mistake on the part of the surgeon. The patient appeared very disappointed and frustrated, claiming he got divorced, though Dr. K didn’t believe him. Nurse Nadine says it’s common to see wives leave due to erectile dysfunction. Regardless, the man didn’t seem to have much say in choosing the IPP originally. Dr. K gave him two options: fix the IPP so it wraps around the glans and improves erections or remove it and give him a malleable prosthesis instead. I could tell the man had in his mind this idea of a botched surgery (Dr. K was offering the man a 3rdopinion), and wanted someone to redo the surgery properly. Dr. K didn’t give that option and finally explained that he’d probably want the malleable. It seemed like a pretty spur of the moment decision where the patient just trusted Dr. K. I wonder if complications could have been explained earlier so the man could’ve understood his options earlier.
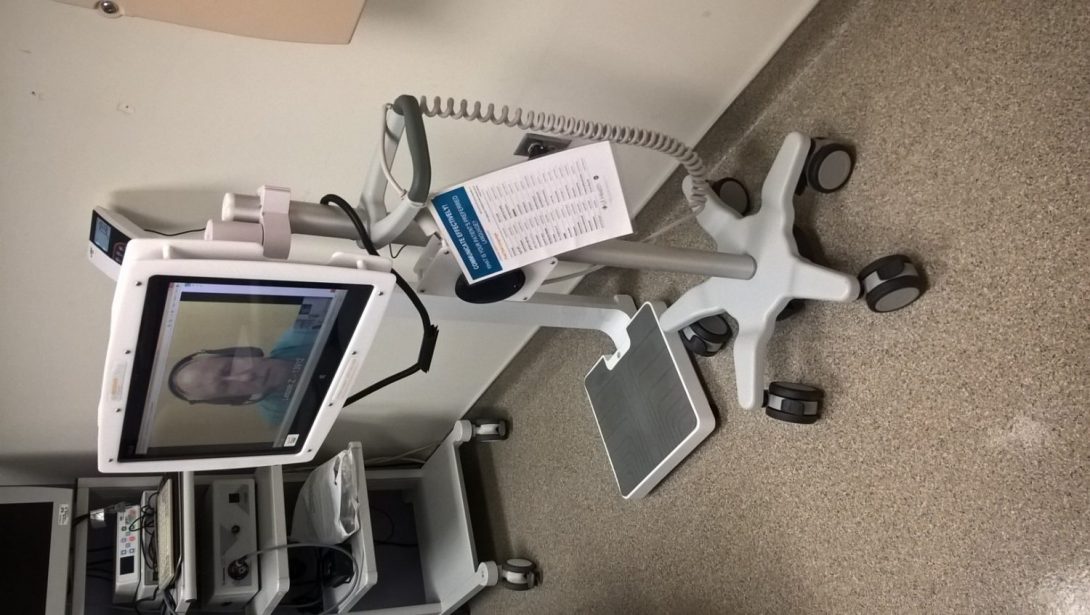
A Polish man with glioblastoma and kidney problems came in and needed a virtual translator. We had a pretty nifty monitor video system set up (pic attached) so that a translator could see and talk to him. It was a good communication exchange, but I’ve noticed that phone exchanges are much worse. The translator doesn’t know if the doctor is just making a quick comment or actually wants the comment to get translated. With multiple people in the room, it gets confusing, so the video facilitates better communication because everyone can see each other.
Fri 06/16 Week 3 Blog Post 2
Usman Akhter Blog
On Thursday we saw a urethroplasty, made out of some of the patient’s ileum. There were no issues, but I noticed sewing up the man’s incisions after surgery takes a long time. Usually, the doctors leave and let the residents do it. It took Niki around 30 minutes to finish up the suturing. I wonder if any portable sewing machine-like devices exist that could make this easier and faster. Essentially, they take a wire and snake it through both ends of the incision that they want to seal tight, just like with any sewing.
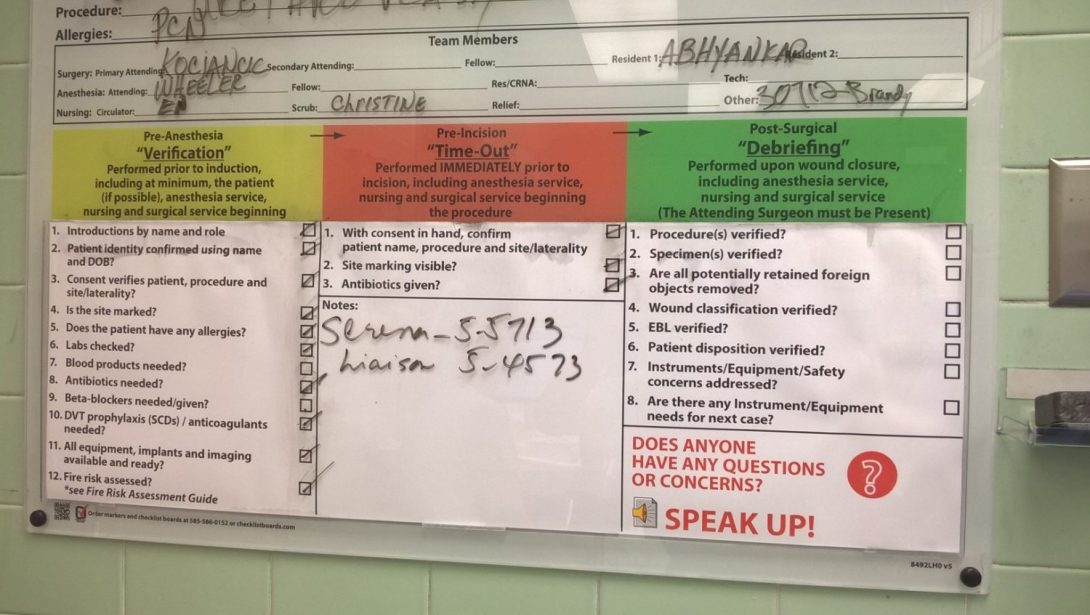
Surgery equipment checklists are a validated benefit, but I see it done inconsistently. It was done for the next Urolift surgery with the nurses checking that they had a kit and the Urolift box for surgery, but still we ran into the most time-consuming problem I’ve seen yet in the hospital. The Urolift box comes with the clipping tool to clip the prostate lobes but not the metal extender that actually enters the urethra, so UIC puts it in a separate kit. The nurses never did this surgery before and didn’t know which kit to get, so they accidentally got a similar but wrong one. The metal tool was too short, so we had to ask equipment offices to get a new one. It took no longer than 5 minutes for them to confirm they have one and are bringing it, but it took 45 minutes for them to bring it up for some reason, so we just waited around. Niki said we did the checklist at the beginning (called a ‘time-out’ – pic attached), but they don’t thoroughly check every kit and every material to make sure they have every item. They’re satisfied just knowing the box is in the room. In this way, the checklist system was flawed.
Another huge problem that day was that someone accidentally tossed a culture sample from surgery. Apparently, the nurse marked in the computer that she has it and has sent it before sending it. She then forgot to do it, and someone tossed it. Even if she did send it, there’s no step along the way to confirm it’s been properly transported and received. Without a confirmation and flagging system along each step of culture transport to the lab, it seems easy for this to happen.
96
Normal
0
false
false
false
EN-US
X-NONE
X-NONE
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-parent:””;
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin:0in;
mso-para-margin-bottom:.0001pt;
mso-pagination:widow-orphan;
font-size:12.0pt;
font-family:Calibri;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;}
On a side note, I’ve felt personally that the face masks are very annoying. I can’t see behind my head, so it’s hard to tie the straps and takes about a minute each time, and everyone’s required to wear it in the OR. During surgery, if it comes off, you need to get someone to help you tie it back on (I helped Dr. Garvey get one of his straps back on). I feel like Velcro straps would be way more convenient.
Wed 06/21 – Week 4 Blog Post 1
Usman Akhter Blog
On Monday, our team narrowed down our focus for needs assessment and settled on lab/drug ordering notification. Often, the doctors will get back to their computers and in the commotion of collaborating and addressing short-term needs, they forget to make the order for the patient who they just spoke to. The lab might eventually call when the patient shows up to ask what’s going on, but at that point, a lot of time has been wasted and the patient may be suffering as a result of their waiting. In response to this problem, we propose a voice transcription system that takes existing dictation software on phones and creates a note on the doctor’s desktop post-dictation so that they have a reminder to order and won’t forget at the end of the day.
In clinic Tues/Wed, we noticed a few more interesting cases. A Chinese man with high PSA walked in but we didn’t have clear info from his 20-page or so referral from his primary care physician. As a result, we sat there for about an hour in total just trying to figure out why he was in the office. Even with the translator, it was a huge struggle. Fortunately, his wife spoke decent English and cleared things up for us. Still, our time was probably tripled due to the language barrier. When reading through his referral packet, we searched for PSA levels due to the benign prostate hyperplasia consult, and after 3 of us searching thoroughly for about 15 minutes, we never found it. It’s a common problem that doctors are searching for 1 or 2 key facts from these packets amidst a lot of pages, and often never find it. We ended up having to call their office to get the information, which begs the question of why we have these huge referral packets in the first place.
Another issue we noticed when clearing the urine from a man’s catheter was that the urine jug can’t stand on its own. I’m not supposed to be stepping in as a helper, but the nurse and doctors often need me to do simple things like hold something in place. In this case, Nurse Nadine needed an extra hand while she used both of hers to open the tube for urine to leak out. I had to keep the jug steady. Only when the jug has urine can it stand on its own. This seems like an annoying problem that should be easily fixable.
In regards to Nadine spending lots of time writing letters, we asked her what notes she would most value if there was a template. She showed us the return to work/school form (pic attached) and showed us how the EHR lets you autosave some text in as a template. In this way, you can type up a sample letter for the patient and leave blanks where appropriate. We are considering writing up some short templates for work/school and embassy permission to speed up the typing process for Nadine.
Fri 06/23 – Week 4 Blog Post 2
Usman Akhter Blog

Thursday I went to 900 N. and saw another testicular sperm extraction surgery. Dr. Neiderberger was only briefly in the room to observe and give pointers, but it was entirely done by the residents. I took more careful time notes to keep track of time. Setting up utensils took 10 minutes, preparing patient before call-out took 20 minutes, more materials prep for another 10 minutes, and then the procedure started 40 minutes after starting set-up. I noticed an excessive number of people in a cramped area. Of the 5 people in a tight space near the man’s groin, 1 was a tech who helped pass out the utensils to the fellows, 2 were fellows doing the surgery, 1 was a resident to help with the watering syringe, and 1 nurse collected samples. I think 3 of those roles could’ve been done by 1 person (utensils, watering, sample collection). I met Dr. Shapiro for the first time, and he confirms the stereotype of Urologists being funny surgeons who make inappropriate jokes. I noticed suturing took by far the most time – 56 minutes in total. Some of this might’ve been slow due to training, but it’s remarkable how no one complains about this. Instead, I heard Dr. Bakare complain about the microscope adjustments required between users, which seemed to take at most 2 minutes per resident/fellow. I also noticed you can’t touch the large arms of the microscope because it is not sterilized – only the microscope part at the end and its handle arms are sterilized with the plastic-bag looking items around it (pic attached of Dr. Bakare almost touching the arm part).
On Friday, I saw a vaginoplasty sex change from male to female at UIH. It was remarkable to see Dr. Schechter take the skin from the man’s penis and form a vagina out of it. In the surgery room, it all looks believable, but when I stepped back to think about what we’re doing, it was incredible to take it all in. I asked Dr. K what happens when the patient feels gender dysphoria after surgery. He didn’t quite know the answer and said that’s what the surgery is meant to address. Dr. Schechter said there is often some depression post-surgery but no significant gender dysphoria. For the first time, I saw the recovery room. It is just a separate room where we roll the patient and keep them there to recover with nurses assisting. I wondered if these procedures are covered by insurance, like Medicare/Medicaid, and Niki confirmed they are. Supposedly, these surgeries are most common in Iran despite the conservative religious culture, because it is done as a corrective measure (or maybe castigation?) for homosexuals. During the surgery, the skin of the penis needs to be plucked of all hair follicles so that it’s not hairy when re-inserted as a vagina. This looked tedious, time-consuming, and error-prone.
When I asked about clinical needs, Dr. Schechter mentioned the need for better retraction tools. They use a bunch of surgical instruments/scissor-looking clip devices to hold together sutures and keep the surgical area open without tying up people’s hands. Dr. C from Urology at UIC supposedly invented a suturing sewing machine device and won a prize for it, but Niki doesn’t know where it has gone since then. I hope I can speak to him about his progress on it. When speaking to some nurses, I also noticed them complaining about inefficient employee assignment. Nurses on flex were not on call during an overtime period, but the full-time nurse was being held overtime instead (they noted she probably gets paid higher and doesn’t want to be there overtime, so it’s a waste keeping her on call instead of the flex nurse).
96
Normal
0
false
false
false
EN-US
X-NONE
X-NONE
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-parent:””;
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin:0in;
mso-para-margin-bottom:.0001pt;
mso-pagination:widow-orphan;
font-size:12.0pt;
font-family:Calibri;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;}
Week 5 Blog Post 1
Usman Akhter Blog
At Mile Square, I took note of physician time per patient for Dr. C. He got through 10 patients between around 8:00 through 11:45. That’s 22.5 minutes / patient on average. 5 were no-shows, so 1 doctor can get through 15 ‘scheduled’ patients in 4 hours, or almost 4 scheduled patients/hour. I think that’s on the faster end, usually doctors can’t get through that many patients. In total that morning, the doctors got through 17 patients in the 4 hours of the morning. I didn’t track how many doctors/nurses, so this isn’t very meaningful.
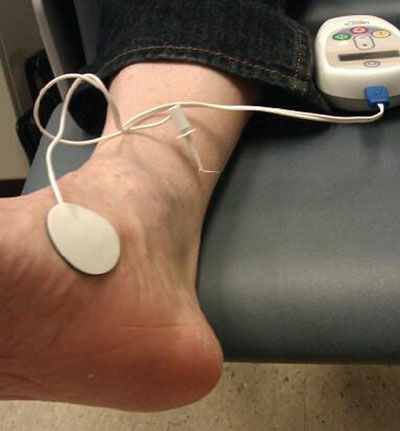
One woman had a neural issue with her bladder. No options exist besides using a catheter forever if neuromodulation doesn’t work (pic of device). She didn’t seem to fully understand that a ‘procedure’ still counts as a surgery, as they insert a pacemaker-like device to control bladder contraction. In general, I get the feeling a lot of patient knowledge comes from Googling stuff at home.
96
Normal
0
false
false
false
EN-US
X-NONE
X-NONE
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-parent:””;
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin:0in;
mso-para-margin-bottom:.0001pt;
mso-pagination:widow-orphan;
font-size:12.0pt;
font-family:Calibri;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;}
When we presented our voiding idea to Dr. K, he mentioned how volume is important in addition to flow. We’ll continue brainstorming our ideas.
Week 5 Blog Post 2
Usman Akhter Blog
96
Normal
0
false
false
false
EN-US
X-NONE
X-NONE
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-parent:””;
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin:0in;
mso-para-margin-bottom:.0001pt;
mso-pagination:widow-orphan;
font-size:12.0pt;
font-family:Calibri;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;}
We spent remaining time researching our ideas and would prefer to keep that research private. (pic of our brainstorming attached)
96
Normal
0
false
false
false
EN-US
X-NONE
X-NONE
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:”Table Normal”;
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-parent:””;
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin:0in;
mso-para-margin-bottom:.0001pt;
mso-pagination:widow-orphan;
font-size:12.0pt;
font-family:Calibri;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;}
Week 6 Blogs
Usman Akhter Blog

Unfortunately, I spent less time in clinic this week and didn’t take thorough notes, so I have no updates to add this week. We spent time researching our ideas on our own as a team and following up in clinic to get feedback from Dr. K and the rest of the Urology team.
Bekah Allen

Rising senior in the bioengineering program with a concentration in neural engineering. My rotation for this program will be in cardiology. With a basic understanding of the heart, I am very excited to see what I can learn from medical experts in this area, and how I can apply my knowledge of engineering principles to this project!
Bekah Allen Blog
Bekah Allen Blog
Immersion
Bekah Allen Blog
This week has started with a lot of unknowns but an overwhelming amount of excitement for everything that this six-week adventure in the cardiology unit would entail! Our very first day of the program started how it will every Monday (except it was Tuesday due to Memorial Day); an entire program meeting to first give a run down of the program, and then guide us through different concepts in these initial stages of design. Although we will be in our respective units mainly observing, this, in fact, is the first stage of the design process, and a very important one at that. This is why it’s called a needs assessment. Designing devices that no one needs or would be able to use would just be a waste of time and money. We discussed the importance of creating devices that are desirable, viable, feasible, as well as having a human-centered design. Human-centered design is a term that is used often but is one of the reasons I am so excited for this program. Understanding how products I may potentially develop will affect and integrate into the workflow for the end users such as doctors, nurses, technicians, clinicians, etc, will give insight I might not have had otherwise.
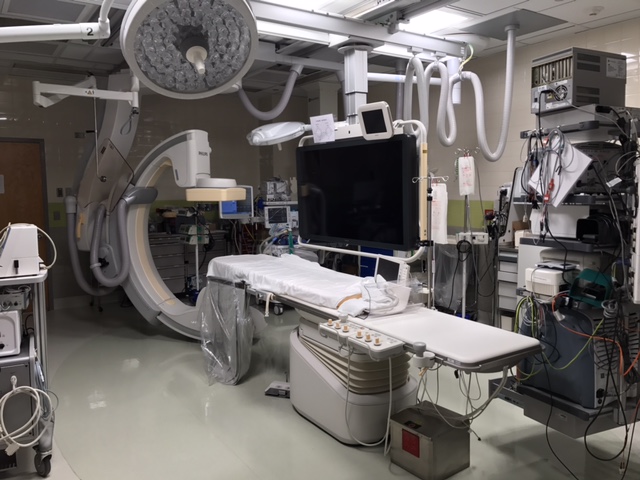
For our first week in the hospital setting, the focus was to observe and get a better understanding of the cardiology unit, not to find opportunities quite yet. Our first day in the hospital on Wednesday started with a meeting with the chief of cardiology, Dr. Darbar. He explained his background, as well as his take on the ever-changing trend in technology, which was an interesting perspective to hear. He spoke of how the technology for mainly imaging has advanced greatly compared to when he had done his training. But he could also tell where the current trend in technology advancements are heading for electrophysiology (EP). The next part of our day was spent with Dr. Gans in the echo lab.He seemed to appreciate the technology that was used currently for his job and seemed content with his current workflow. Which was obvious after spending a couple of hours with him; I’m not sure an autonomous robot would even be able to examine 75 different images of the heart, to accurately update a patient’s medical record faster than Dr. Gans was able to complete one (when we weren’t asking ten questions per minute). The last part of the day was spent in the cardiology fellows room, listening to the senior resident present multiple patients’ cases to Dr. Stamos, Director of General Cardiology Fellowship. We actually then got to go on their rounds with them to the various patients. This wrapped up the day for us, with a lot of things to take in and observations to review.
Day two came on Thursday, which was spent with Dr. Ardati, an interventional cardiologist. It was interesting to see the comparison of the two days, the first that appeared to have less obvious needs for innovation versus the second where there were immediate issues that were addressed for improvement. While this week was intended for mainly observation, it was hard to not immediately start brainstorming ideas.
Before we knew it, it was already Friday and the last day of our first week in the program. Because our mentor, Dr. Wissner, had been out of town teaching medicine in Iran, this was the first day we were able to meet him. Immediately talking to him, it was clear he was passionate about this field, and thus I am very excited to have him as a mentor. He mentioned how there was a large amount of bioengineering possibility in ablation and catheters; whether it’s non-invasive mapping systems, catheter design, navigation, etc. One quote that Dr. Wissner said that stuck out to me was “Ablation is a cure”. This was interesting to me because this isn’t always something that is possible or true in medicine. Dr. Wissner talked of one patient showcased on the hospital’s wall, who benefitted from both the cure of ablation and the engineering of non-invasive mapping systems. She was a patient with a heart condition that had worsened with pregnancy, and could not receive the standard procedure with fluoroscopy for the safety of the baby. Dr. Wissner was able to utilize a 3D mapping system to safely ablate the areas of the patient’s heart and cure the disease! We then got to meet with Dr. Shroff, an interventional cardiologist, who was just finishing up a stress test for a patient needing clearance for a kidney transplant. He also mentioned that interventional cardiology is growing because of a true collaboration between clinicians, engineers, and pharmacists. After just a few days in the cardiology unit, I could already tell how true this was. I cannot wait to learn more while in the cardiology rotation for the next six weeks and hopefully can be a part of the equation that will continue the innovation that is helping patients like the one Dr. Wissner treated!
Scrub Up
Bekah Allen Blog
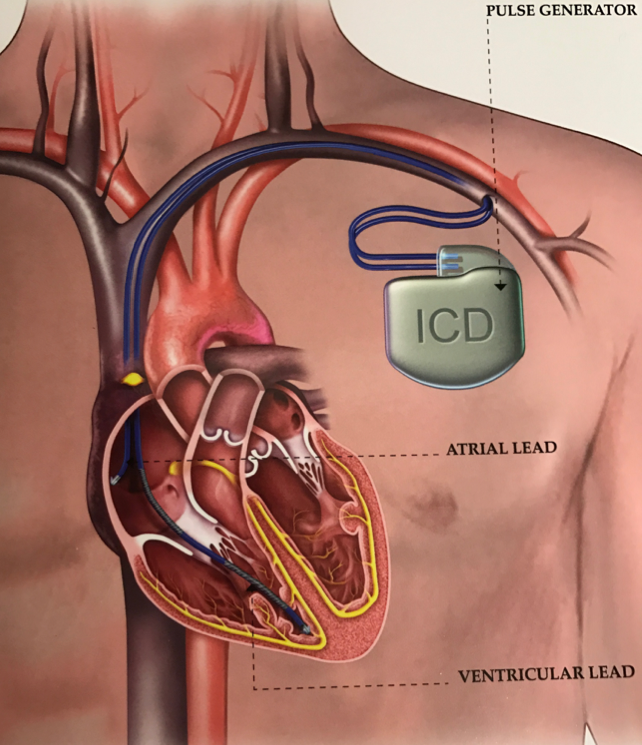
The first part of this week has been a bit of a different scene than last week. There have already been many more procedures for us to observe, and in almost all of them, we have been allowed to put on scrubs and the protective lead aprons to observe right from within the room. Each day has been something new, but each day I have an overwhelming appreciation for the doctors and staff on the cardiology unit for not only what they do for their patients, but also how kind and willing they have been to teach us.
On Tuesday, a patient had presented with shortness of breath, and so Dr. Adati performed a diagnostic cath procedure. After the procedure was completed, Dr. Adati was looking at the contrast dye images of the patient’s arteries using the imaging program called QCA (Qualitative Coronary Analysis). This program measured the arteries to be 8 mm, which are massive arteries, but I was shocked to find out that there were not even stents for that diameter for the length needed in this part of the artery. So if this patient were to need stents, they would literally not have an option which was unbelievable to me.
The next case Dr. Adati dealt with was an angiogram for evaluation for a kidney transplant. The patient’s FFR (fractional flow reserve (there is an abbreviation for everything in medicine)) was determined to be 0.86, where a perfect FFR would be 1. Dr. Adati wanted to check this narrowing using IVUS (intravascular ultrasound) to visualize the plaque. From this imaging, it was decided that the narrowing was not as significant as the angiogram showed and that they would just keep an eye on this for now. Dr. Adati mentioned how twenty years ago she would have just had to go to surgery because it had appeared as a left lesion, but because of the Boston Scientific IVUS, a more accurate, less invasive diagnosis was able to be made. Later on, the nurse put it best, “Thank God for cool technology”.
Our next day was spent entirely in the EP lab, and the first procedure was amazing to see from inside the room. Dr. Lazar performed an ICD (Implantable Cardioverter Defibrillator) procedure, that we were able to watch from the other side of the cath table on stools kindly provided by the nurse. Dr. Lazar was extremely informative before, during, and after the procedure, to the point that it should be its own separate blog post, but I will attempt to be succinct. Dr. Lazar received his B.S. in biophysics, so while he was able to test the IMED students on medical terms, he was also able to test us (the bioengineers) on some physics-based concepts. These included Fourier Frequency Transform, the complex version of Hilbert’s Transform, Laplace Transform, and impedance questions regarding the defibrillator’s leads. The medical devices and technology that were used today gave me such a respect for the relationship between the skill the doctor utilizes and the quality assurance the medical device provides. The ones specifically being used today were the ICD, an electrocauterization tool, the TEE (Transesophageal Electrocardiography), and the temporary pacing leads. Long story short, you could say I’m loving everything about this internship so far.
Fully Immersed-End of Week 2
Bekah Allen Blog
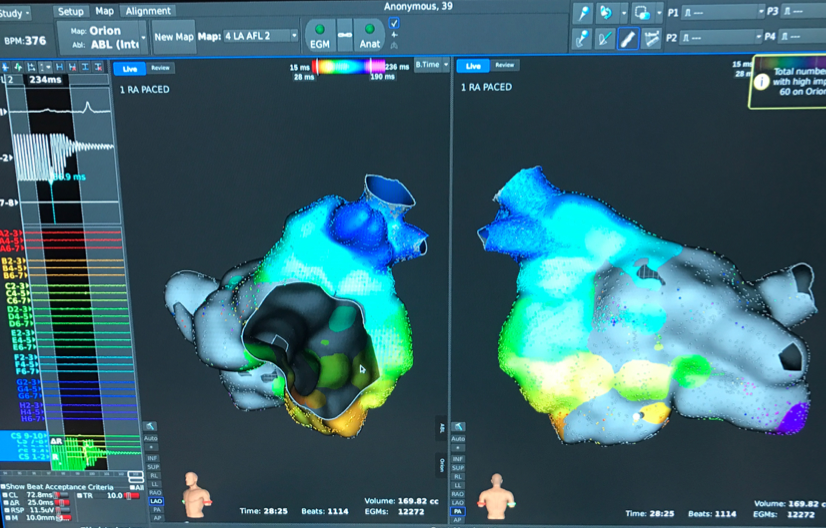
The beginning of Thursday was spent following up on the previous exciting day of cases. It was nice to be able to go on the rounds with Dr. Lazar to see the patients he had worked on the day before. Before he did this, he pulled up the x-ray of the patient who had the ICD put in to make sure there wasn’t a collapse in the wall of the lung since a very large needle had to be inserted in that vicinity to implant the ICD leads. While there might be room for improvement to make the doctor’s job easier, I think that just came down to the skill the fellow and doctor have worked to master while in such delicate areas. Another insight Dr. Lazar shared with us was the idea of using fractal mathematics for R wave variability as a possible predictor of disease. He also mentioned that this could be used for anesthesiologists as an indicator of pain, and the French has already patented a wearable device to help anesthesiologists monitor patients.
The second part of Thursday included an entire array of amazing medical tools and technology. While in the control room, I had the opportunity to talk with the Medtronic rep that was providing the medical equipment for an atherectomy. The first tool was a directional atherectomy system that grabbed atherosclerosis and coiled it back into the cone, this was followed by a drug coated balloon catheter that was designed to treat the disease inside the arteries. A mesh-type net was also placed distal to the area being treated as a backup in case any of the plaque that was being removed broke off instead of going back inside the atherectomy cone. This mesh was designed to prevent any embolism, and it actually had caught some of the plaque!
After this finished up, I was able to pop into the other room where the other two team members were watching an ablation that used Boston Scientific’s Rhythmia Mapping System. From what I saw this was an awesome development of technology that allowed Dr. Huang to successfully ablate the areas of the patient’s heart by utilizing this electromagnetic mapping system.
Friday once again came quickly and was spent in the remote monitoring clinic with two wonderful nurses, Rose and Berenice. They explained to us how life works for the patients after the devices we saw are implanted. Rose also mentioned how some of the older devices don’t have the remote monitoring capability, meaning these patients don’t have their episodes directly sent to the nurse’s computer. We were able to investigate the pros and cons of the user interface for the varying companies with the remote monitoring software on Rose’s computer, as well as be in the room for a patient’s device interrogation. Rose mentioned she had her favorite company’s program just because of the intuitive user interface, and looking these reports over is a big part of her job. After going between two different programs, it was clear why Rose might favor one over the other. Although unrealistic, my team member and I talked about how perfect it would be if the companies would work together to take the best parts of their software to make the best program for health professionals (as would be true for most companies in life). When in the in-person interrogation, a wand was placed over the patient’s device and uploaded to the companies program monitor, from there Berenice could retrieve all of the patient’s device data from up to a year. Berenice also mentioned that while information of the patient’s device will be sent to their secure network, the only time changes can actually be made to the patient’s device is while in the clinic due to the possibility of hacking a device to change its settings. Rose spoke of how some of her older patient’s don’t like the idea of the remote monitoring because they like the face to face interaction since they know they can trust her. This brought up her point that in this field, it is an art of medicine and science, it can’t all just be technology. Through this program, I continue to get a better understanding of this relationship, and the importance of how a medical device will be able not always replace, but enhance the skill that these nurses and doctors have already developed.
Musculoskeletal Distress-Beginning of Week 3
Bekah Allen Blog
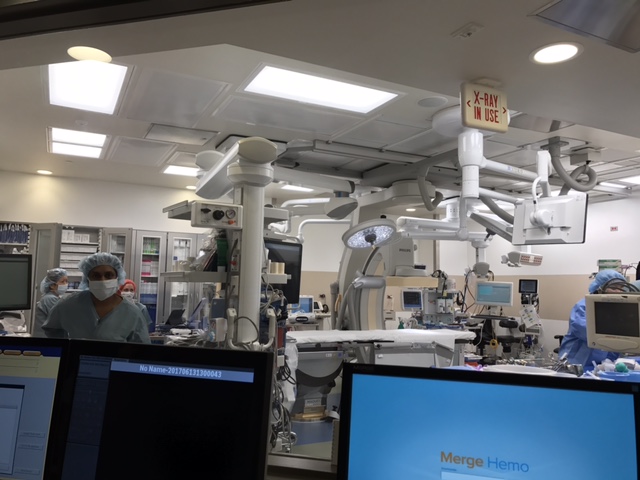
The beginning of this week has been spent with the EP doctors, and the difference in musculoskeletal stress has been noted. We’ve been told that for the interventional cardiology doctors, the longest one of their cases may take is around an hour and a half, and that’s if it is a really involved case. The EP cases last around 3-4 hours, and standing for that long with the lead apron on that I once thought was not so heavy became actually quite heavy. I mentioned earlier that the VA has an anti gravity lead shield but that it is never used because it is too cumbersome when the doctor turns since it doesn’t fit as seamlessly to the body as a vest does. This got me thinking that there should be an exoskeleton type lead shield that would redistribute the weight to the persons legs to reduce the strain on the doctors back. During our ideas meeting with Dr. Ardati, I found out this was already a thing where it is similar to the frame hiking backpacks have to take the weight off of your shoulders and redistribute it around the waist. However there are some other ideas I have about this, and will not give up there.
This week, while still fascinated in the medical jargon going on, I tried to filter some of this out and focus more on what I was observing that might be a work around or something to be improved. I have to mention though we got the opportunity to go into the brand-new, hybrid OR which was quite the honor. This OR had the capabilities for surgery, but also fluoroscopy capabilities, so we were able to observe two ICD lead removals.
One thing I noticed during the second case on Tuesday was that there was a long prep time that made me wonder why some of that couldn’t be done while the patient is awake. Some of these things included cleaning the patients chest, fitting her arms on the bed with the sheets, attaching sterile drapes, but none of these things stood out to me as needing the patient to be intubated for this part. There may be another reason that I’m not aware of but to limit the amount of time the patient has to be under anesthesia would seem to be a positive. Another work around observed in this case was that the arm pads that were supposed to latch on to the rail of the bed didn’t attach very smoothly and had an angle that made it look like it was just going to fall off of the bed. This actually did happen, and they ended up just leaving it off the bed, then wrapped the patients arms up by her side with blankets.
In the second case we saw in the OR, it was the same procedure but there was a delay because the correct piece of equipment was not in the room and it took a while to be able to figure out who was able to go down to the second floor to get it. I’m not sure where the miscommunication or error occurred, but maybe there is a better system to ensure the proper equipment is in the room at the start time. Both of these cases were to preform an ICD lead removal, which is a more complicated procedure than would be initially thought. This is because it is a very delicate process to remove the lead from the scarred walls of the heart. To remove the lead parallel to the walls of the heart, Spectranetics offers the only excimer laser for lead extraction. It does so by pulsing UV light energy to gently dissolve the tissue scarred in to the leads. While this technology is a brilliant invention, and safer than the traditional mechanical methods, I couldn’t help but hold my breath as the gravity of the situation required a surgeon to stand on call, and extreme care by Dr. Lazar as to not burst through the wall of the artery. Of course though, Dr. Lazar is an excellent doctor and successfully removed the leads in both cases.
On Wednesday morning, the loop recorder and pacemaker implant were both cancelled so instead we popped into one of the cath labs where a vascular procedure was being done. After the case, the doctor wanted to give us one piece of advice, and that was that communication is critical for success and the safety of the patient. I could definitely agree that the part about communication was very true, and could be applied to all areas of life. A miscommunication or rather lack of communication occurred between an intern and the doctor so that when the doctor was in doing his procedure he could no longer proceed with placing a stent that requires anti-coagulants after because there was a suspected transcranial bleed. Because this information was not passed along, he had to send her up to CT to be certain there wasn’t a bleed and then bring her back on another day to do the procedure. This obviously caused a whole lot of people’s time wasted, as well as equipment and space that was used for really no reason.
In the afternoon we spent our time in the outpatient clinic with Rose and Dr. Wissner. We were able to see the patients with both Rose and then dr. Wissner. The biggest issues Dr. Wissner addressed with us was getting the data, writing it down, communicating when there are language barriers, and no shows. Dr. Wissner said he is a fairly slow typer and so a lot of his time was spent entering in notes after seeing patients. The other thing Berenice said was that for each different remote monitoring website, for all the data that was uploaded from the patients device interrogation, each piece of information had to be manually entered into the patients medical record. This seemed so tedious especially since for each patient there was the same general information that was being transferred to their EMR regardless of the company. I’m not sure what would have to occur if it’s licensing but it would be way more convenient if the data could be automatically uploaded to the EMR after an interrogation.
Why’s Arise-End of Week 3
Bekah Allen Blog

In an effort to finish Week 3 with a focus more on needs, I made a point to ask myself why as I observed things being done. This strategy brought forth a couple of why’s that I think bring up a good assessment of a few needs. On Thursday, during an ICD procedure performed by Dr. Huang, he was dealing with a very large man which made Dr. Huang have to cut through much more tissue to get to the pectoral pocket, meaning it would require a lot of lidocaine. However, the size of this man seems to be about the average size of the patients seen for the procedures in the cath lab or EP lab over the span of these three weeks. So the question that was brought up is why was the cath table designed to be so narrow? Obviously optimizing space is ideal, but most of the times the patient’s arms have to be tucked in to their side by using an inserted plastic arm guard. Otherwise, there is no space left on the table for the patient’s arms to comfortably rest. And this patient was not the first to have the clear arm guards, it is something used consistently so the arms are wrapped in to the body. Another question was raised during ICD procedures where the blue sterile drape is covering the entire body, including the face. This has to be done for sterility issues, but each time the blue drape has to have a hole ripped through it for it to then be hung to an infusion pump. During these procedures, the patient is awake, and just lightly sedated so many of them complain of this drape over their face saying they can’t breathe with that on. So a make shift tent of sorts has to be made to allow for air flow, which is a very obvious work around with room for innovation.
The next question came while on EP consult rounds with Dr. Huang. For patients with a new ICD, it takes around 1 month for the leads to heal into the tissue of the heart. So during this time, the patient is not to raise their arm above their head because this could actually detach the leads from their heart, which would require another procedure. The patient is instructed to wear an arm sling while sleeping incase they were to raise their arm unknowingly, but my team and I were thinking that there might be a more full proof way to ensure the arm doesn’t raise above the head. Another thing noticed while on rounds was the number of people who went on the rounds. It was the size of a small class, and not to mention most of the rooms were split rooms which halved the amount of space there was to talk to the patient. With 10 different doctors, fellows, or residents, and then three of us (which only one of us would go in for each patient), I would venture to say it was a bit overwhelming for the patient. Granted, patient’s know to expect to have this type of experience while receiving treatment at a teaching institution, I wondered if there was a way to reduce some of the people by use of video or other technology. This week has been another beneficial week of getting insight to some opportunities for innovation that I might not have thought of without observing in this setting.
White Coat Hypertension-Week 4
Bekah Allen Blog
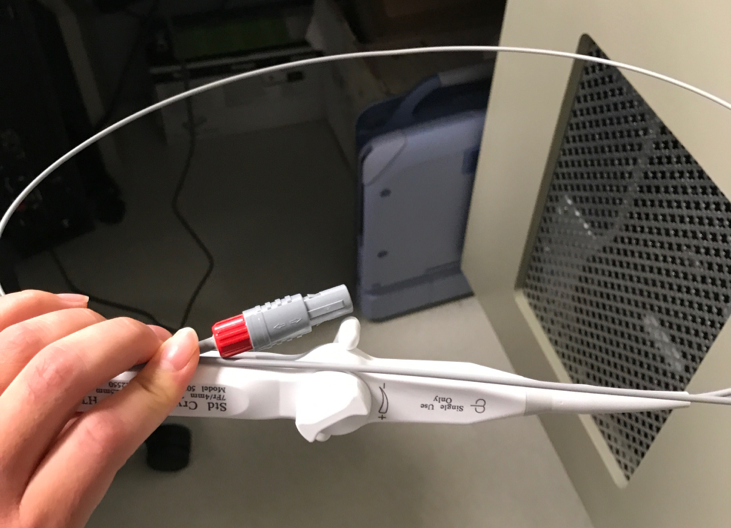
We spent the first day of week 4 with a new doctor we had not yet spent time with, Dr. Stancu. In the first case she performed an accessory pathway ablation, and used St. Jude’s mapping system. If I were to be partial, it seemed that one system had a simpler user interface after observing the two from the control room. However, there is always a rep from the company who runs the program but from an outsider perspective I know there would be one I would want to use more. During this procedure, one of the ablation catheters had touched a table outside of the sterile field, so they could no longer use it. Luckily for us, we were then able to try it out, observing how the catheter tip bent at various small or large bends depending on which way the dial was pushed. All of us agreed that this system was not intuitive, and we felt could very easily get confused as the catheter tip is rotated during a procedure. You also have to use a little bit of force while manipulating the dial to get the catheter to bend, which I would assume would put a bit of strain on the doctor’s hand during a two to three hour procedure.
The next day we met with Dr. Wissner to plan our schedule for the rest of the week, and then met with Dr. Ardati to show him our prototype of the design we made for him. We wanted to receive feedback on our physical concept before we made one in SolidWorks. After this, we observed another tilt test, but for a patient whose case was a little more complicated because of various diseases. One thing I found interesting was this thing Dr. Wissner called “White coat hypertension”. I thought this was funny because it seems to usually be true that your blood pressure is always higher when you’re at a doctor’s office or when the doctor walks in. So in this case where the doctor’s are trying to observe the patient’s blood pressure while doing the tilt test, it would be important that the patient is in a quiet room with very little stimuli. Dr. Wissner also mentioned that there are the 24 hour BP cuffs, which might be something useful in cases like these. Later on in the day, we went on EP consult rounds with Dr. Huang and followed up with the patient who had the tilt test. Because of the results, and the absent seizure they observed during the procedure, they were going to have to follow up with neuro to see if his problems are stemming from his brain.
Mishaps-End of Week 4
Bekah Allen Blog
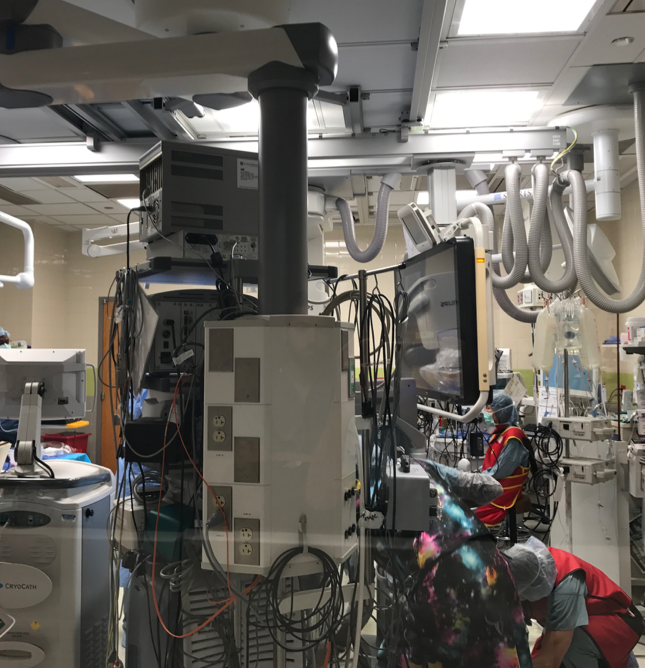
For our last two days spent back in the EP lab, I thought I would bring up a few small mishaps observed that I believe stem from a few central themes. On Thursday, a patient scheduled for a cardioversion had to cancel because she had thought she was supposed to stop a medication that apparently was needed, thus canceling the procedure. The next issue came in the EP lab, when it seemed that one system had been set up for an ablation with a specific catheter, when the doctor in fact wanted a different catheter, which required a different system. This was a relatively simple fix, but caused waste of time and equipment, and frustration for the nurse who was told the wrong catheter to grab. During this procedure, the other EKG lines were also not showing up on the monitor, which took around 45 minutes to fix the issue. This made sense it took this long to trouble shoot considering the massive tower of systems that had cords running in every direction. Another thing I noticed during the procedure, was that the lights went off at least three times due to the fellow stepping on a foot pedal that controlled the lights. While it seems it might be convenient to have the foot pedal so close in case they want to turn off lights to see an image more clearly, it also seems a bit dangerous to be able to accidentally turn them off while something like an incision might be happening. I believe these issues all stemmed from two main themes: communication and organization. These might not initially be thought of for an area for a medical device or innovation, but they are two themes that are too important in all aspects to be successful in life.
Friday might have been my favorite day this week because we got to watch one of my favorite procedures, a pacemaker implant, with our mentor Dr. Wissner. But one of the Boston Scientific reps was there to help with the procedure who has been doing this for 20 plus years. I loved getting to hear about the evolution of pacemakers and ICDs that she has witnessed. Pacemakers used to have to be implanted through open heart surgery, and the generator, which was about the size of two hockey pucks, would sit above your stomach rather than in the pectoral pocket. It used to also be literal pads that were placed on the outside of your heart, and the lead shields used were so heavy and stiff that she said you could hardly bend over. From all the innovation that has happened in the past twenty years, I can’t wait to see where it will be another twenty years from now!
Last Clinic Week
Bekah Allen Blog

I must quickly say how fast this program has gone and cannot believe we’re already to the last week of clinic. With that being said, I’ve been trying to take in every last bit as much as I can. To recap, the first two days of this week has been spent back in the cath lab. It’s interesting to note that our first introduction to cardiology procedures was in the cath lab, and now here we are again in our last week. The difference four weeks has made in my understanding and knowledge of the fluoroscopy images is amazing! In the first week it seemed like the catheter was just being floated through this beating space, and the contrast dye was just being pushed through with no issues. Now I have a handle on which artery the catheter is being threaded through and can find the lesions as the fluoroscopy captures the contrast.
In the first case we saw in the cath lab, the patient had a lesion in his LAD but was also pre-kidney failure and had a creatinine level of 4. Because of this, Dr. Shroff would not stent him because contrast dye is hard on the kidneys. Dr. Shroff wanted to emphasize these types of lessons to his fellows, that they just don’t do cases with a creatinine of 4. For Dr. Shroff, he weighs the importance of the procedure he would do versus being on hemodialysis later on down the road. The decrease in quality of life is something that is taken heavily into consideration before Dr. Shroff would blast him with contrast. So for this patient, he said they will wait to improve the patient’s kidney function and then place the stent.
On Tuesday, we were back in the cath lab with Dr. Vidovich, who is excellent at choosing stent length and how much to expand them, which is something I can appreciate now that I can see the fluoroscopy images and understand what is happening. It is really amazing how far a procedure like that has come, and how easily Dr. Vidovich was able to successfully stent a lesion. We observed Dr. Vidovich do five procedures throughout the day, and each one was extremely useful for our team to observe all the possible challenges and constraints of the designs we are prototyping. Equally as important was getting input and feedback from the nurses and technologists on what they thought of our ideas and how they thought it might be integrated to the work flow. Thinking through a problem and then designing at this level that is so hands on and ground level, where we have gotten to test things in its clinical setting has been an unbelievably beneficial experience.
One Last Ablation
Bekah Allen Blog

Our last two days were spent back in the EP lab. On Thursday, Dr. Wissner and Dr. Huang performed a laser balloon ablation for atrial fibrillation using CardioFocus catheters. Some of the ideas our group had talked about after watching a balloon ablation, were actually mentioned as one of the new versions of a CardioFocus catheter soon to come. While watching this procedure, we also talked to one of the nurses sitting in the control room about when he completely tore his pectoral muscle off while trying to transfer a 400 lb woman who was having a heart attack in her car. While this is not the usual situation, it brings up a major issue that nurses face with patient transfer. The nurse talked of one company who invented the HoverMatt, which revolutionizes patient transfer. It’s essentially like an air hockey table air mattress which allows the patient to basically float on air, making lateral patient transfer much easier. This is design makes patient transfer safer for both the patient and caregiver, which was something else important to consider for some of our designs.
The next day stayed true to the typical length of EP procedures, while we watched a three hour ablation for supraventricular tachycardia. This ablation used Boston Scientific’s Rhythmia mapping system, and while the ablation systems are quite advanced software, the two bioengineers talked to us of possible project ideas that used the data set from the mapping system and Matlab. This got me thinking of some of the different ways we could represent the ablation data with MATLAB. This was the only case for the day so the rest of the day was spent prototyping and meeting with our mentor. He wanted to get our feedback on the program, and what we thought of the cardiology department as a rotation. Personally, I could not have been happier to have been placed with cardiology. The amount of innovation that has happened, and that will happen in interventional cardiology and electrophysiology is inspiring. Not to mention everything I have learned from a medical standpoint in cardiology is something that I also cherish, as is not a typical opportunity for bioengineering students. From just reading the description of the cardiology unit when doing our preference ranking before the program started to now having a good understanding of what cardiologist do on a day to day basis. Additionally, everyone in the cardiology department who has allowed us a look in to their work to learn and observe have all been so kind and helpful. The willingness to talk and explain to our team has made our time observing and innovating as productive as I could have possibly hoped. I must say, the cardiology department has been an excellent addition to this Clinical Immersion Program.
Darius Ansari
I’m Darius, a bioengineering student with an interest in instrumentation, ophthalmology (retina), and brain-computer interface. My career goal is to improve healthcare for patients with neurological/visual deficits either through medical device design or by attending medical school and practicing medicine.
This blog details the most interesting parts of selected days in the Ophthalmology department, taking place in the Illinois Eye and Ear Infirmary, Lions of Illinois Eye Research Institute (LIERI), and the College of Medicine Research Building.
Darius Ansari Blog
Darius Ansari Blog
Week 1 – Ophthalmology Clinic
Darius Ansari Blog
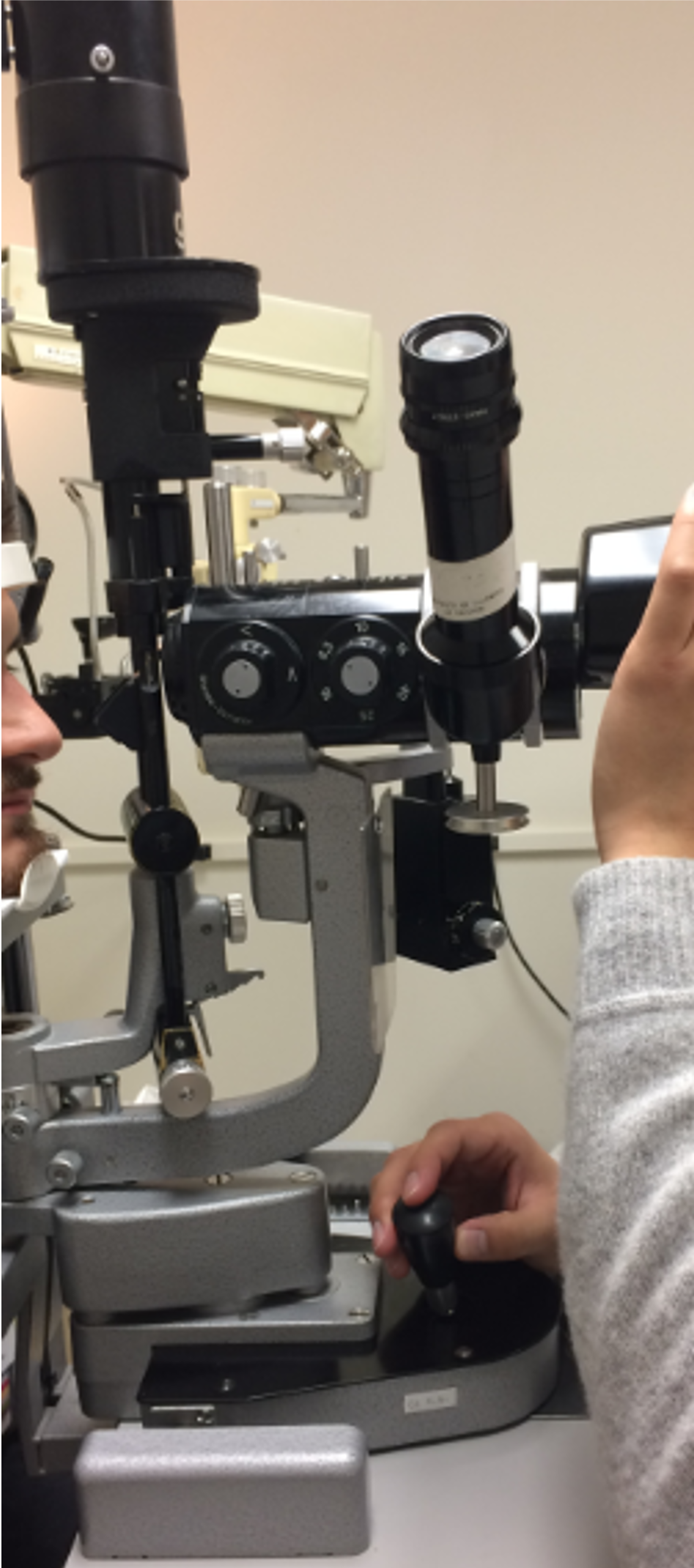
We began our day in the Ophthalmology department at the cornea clinic. Meeting with patients is always the most appealing parts of being in the hospital because we are able to observe medical technology directly during its use. To begin, we observed Dr. Sugar operate the slit lamp and the ophthalmoscope during routine visits with his patients. Many of these patients had undergone a recent cornea operation and were performing a postoperative follow-up, and others were present for routine visits.
One of the most critical visualization capabilities provided by the slit lamp biomicroscope technology is the ability to perceive depth of the anterior chamber of the eye. This information is useful in assessing the shape and other information from the cornea. The instrument itself is sophisticated (as shown in the photo) and requires specific height/orientation in order to operate most effectively. As such, the position of the biomicroscope relative to the physician’s seat can cause discomfort for both the patient and user. There appears to be potential in improving these comfort/ease of use aspects in a few of the devices found in the examination room.
I spent the rest of the day with Dr. Mieler in the retina clinic around similar devices. The ophthalmoscope is a convenient instrument to help the physician view the retina, and can be combined with Optical Coherence Tomography (OCT) to greatly inform the physician of the patient’s health in this critical visual field. This is one of the features of the ophthalmologist profession, as some have said; being able to directly view the target organ noninvasively is unique to the study of the eye, much in thanks to imaging technology and simpler optics-based instruments.
Introduction to the Operating Room
Darius Ansari Blog

After having spent the first day in the Ophthalmology department observing patient visits into the clinic, it was satisfying to see the operations that were prescribed to so many.
The day began in the operating room with a vitrectomy and membranectomy that took more than an hour to complete. Most operations on the retina are of particular relevance due to their extensive use of imaging equipment and/or specialized lenses to view the target. In other words, there are greater opportunities to identify improvements for this technology.
The Retcam3 (pictured) is one such example of a useful yet operationally burdensome device. A surgeon must secure the camera at a highly specific location above the eye (in order to view the retina), control the focus/zoom with a footpedal, and in some cases, perform the operation simultaneously. This complexity and physical labor can draw attention away from the procedure at hand, and some sort of design to make this control process less demanding may be rewarding to some degree. Later, a fellow performing a separate retina operation suggested that one of the light pipes used in surgery could see greater use if certain adaptations were made. Being in the hospital environment for even just one day can be enough to make observations about what can be improved upon, due to the sheer volume of people and machines.
We also observed some cornea surgeries, primarily cataract removal. Compared to the previously described retina operations, most of the cornea work was quick, the primary exception being the cornea transplant.
In all cases, the surgical teams were extremely kind and willing to accept us into the room to observe. I look forward to returning to the operating room.
Week 2 – Pediatrics
Darius Ansari Blog

I have always been impressed by a hospital’s ability to maintain their pediatric department in such a way that it no longer seems like a hospital; at least to the children. The pediatric ophthlamology clinic is no exception, although it seems that all of the young patients are quickly reminded where they are as soon as the doctor attempts to use a tonometer.
I began the day observing children with ages ranging from early infancy to teens. Many observational technologies common to each clinic were present (slit lamp, ophthalmoscope, etc.) and some are pictured. The unique aspect of pediatrics is not the complexity of the instruments used, but the difficult task in obtaining measurements from children. Most children that we saw reacted negatively to bright lights in their eyes and puffs of air, which are necessary to inform the physician with basic physiological state. I was unable to observe many workarounds; in many cases, the physician would resort to indirect ophthalmoscopy as opposed to using the slit lamp with an external lens to view the retina, or would have to settle for intraocular pressure measurements taken while holding open the patient’s eyes.
In terms of conditions, many of the patients were at the ophthalmologist for similar reasons: some had a prior operation (such as congenital cataract removal) and were visiting for a routine post-operative checkup, others were in for a general visual checkup, and some were evaluating their options to correct their strabismus. The attending physician is confident that bioengineers can develop a new treatment for strabismus, as the current strategy of altering the mechanical advantage of eye muscles such as the recti has a success rate of approximately 75%. I haven’t given the idea much personal thought yet, but a novel treatment would certainly involve some sort of electrode to alter muscle tone.
Overall, pediatric ophthalmology faces challenges in obtaining reliable measurements of visual acuity (macular function), intraocular pressure, eye motility, and surely many others. Although I didn’t find pediatrics to be the most interesting/engaging clinic in the ophthalmology department, the attending physicians and the entire pediatrics department did an excellent job in allowing me to observe patient care and in explaining their thought processes.
Imaging and Walk-ins
Darius Ansari Blog

The last day of week 2 was spent in the general eye clinic (GEC) and the eye imaging room. Located on the third floor of the eye and ear infirmary, the imaging room is a playground of optical coherence tomography (OCT) machines (pictured) and other related equipment such as fundus (back of the eye) cameras. I observed the technician taking corneal thickness measurements from one patient and OCT images from another; not much time (~8 min) was necessary with each. After acquiring images/other data, the technician can submit the results for the ophthalmologist to view.
The GEC is unique because it is run primarily by residents; the residents split the load of walk-in patients by spending two days each week specifically meeting with them. Although it may not seem like a big deal, these patients are generally more taxing on the physicians because they are almost always new patients (so there would be little/no prior familiarity), have a wide variety of eye conditions, and the patients are present in high volume. During my day visit, most of the patients were present with some sort of an infection or conjunctivitis, rather than illnesses that one would consider to be more dangerous.
Ophthalmologists in the GEC must be prepared to address any concern and perform an examination for a multitude of diverse conditions such as glaucoma. For this reason, the technology present in each room is similar to that of the other rooms I have described in previous posts: indirect ophthalmoscope, slit lamp, tonometer, etc. After the resident examines the patient, they consult an attending physician to examine the patient as well to ascertain their opinion. I enjoyed my time in the GEC since I was able to observe many cases in rapid succession.
Lasers and Intraocular Lighting
Darius Ansari Blog

We returned to the operating room today to observe some procedures with Dr. Leiderman. I’m always grateful to be invited to the operating room, as it is crowded already without the extra four students. Dr. Leiderman takes time during and after surgeries to explain to us what exactly was happening.
All of today’s surgeries involved a vitrectomy, and most additionally had a membranectomy or laser treatment. Vitrectomy is performed by placing three cannula on the surface of the eye to reach the vitreous, or inner gel. Using a vacuum-like instrument, the vitreous is removed so that the surgeon can access the retina which lies delicately at the back of the eye. There, the surgeon can perform a membranectomy, which can involve removing unhealthy tissue from the retina.
Because the surgery takes place within the eye through tiny cannula, a sophisticated lighting system is necessary in order for the physicians to operate. In addition to the microscope through which the surgeons look to view the eye, an external lens is necessary to focus light on the surface of interest, in this case the retina. To actually illuminate the inner eye, the surgeon must either use one of his hands to hold a light pipe, or they may use a device called a chandelier which can be secured to the cannula and held by a piece of tape (thus freeing up a hand). However, a chandelier can only be used once per operation and so a new one must be obtained for each procedure, adding to the waste produced by each surgery.
Printing Prosthetics
Darius Ansari Blog
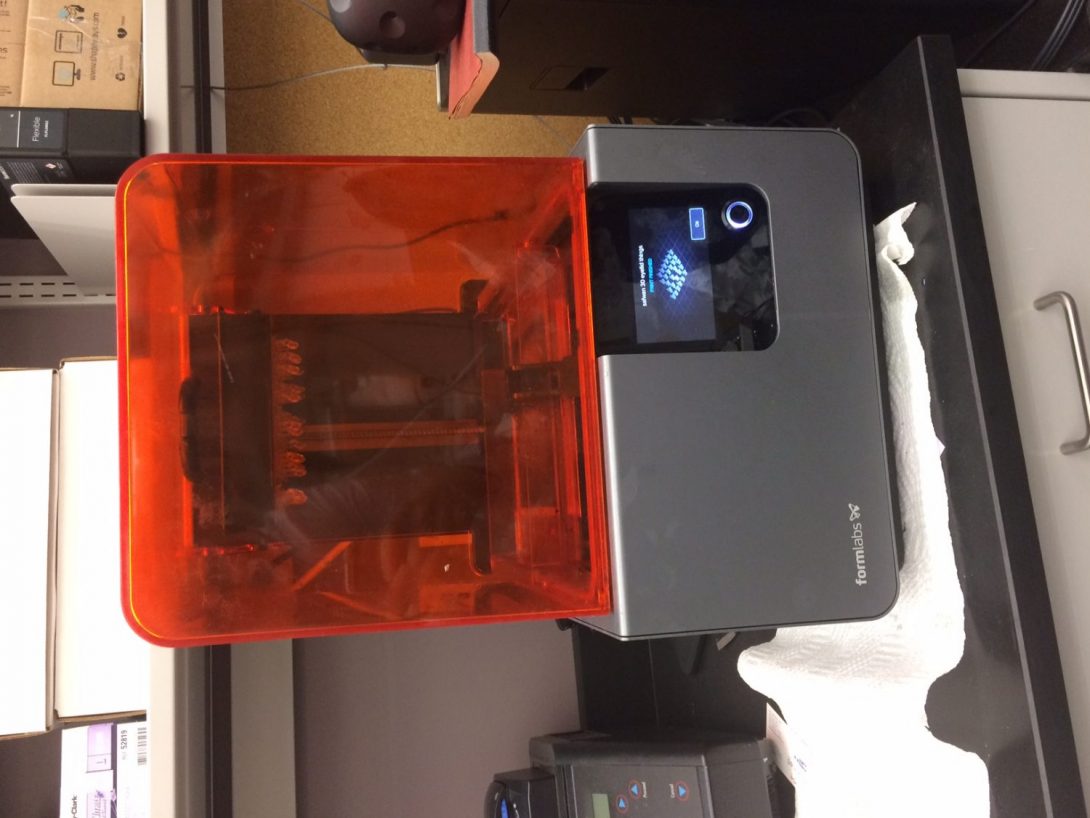
Spending the entire Thursday in Dr. Yu’s lab was an incredibly fun and interesting experience. Despite the fact that Dr. Yu spends a lot of time in both the operating room and the clinic, he still manages to host a number of engineering projects in his lab at COMRB.
Perhaps most notably, we got to observe the 3D printer (pictured) in action, which was particularly fascinating due to its extremely high resolution (and correspondingly high printing time) and capability of creating extremely small products suitable for implementation in the eye via surgery. Dr. Yu and his research team are currently working on an improved keratoprosthesis based on the Boston design. Specifically, they seek to build upon the Boston K-Pro by making it foldable: this would allow surgeons to make a smaller incision to implement the prosthetic and hopefully would lead to better outcomes for patients. Currently, Dr. Yu’s model has been tested in rabbits after having been drafted as a concept approximately a year ago–a pretty impressive timeline.
Another project concerns patients with visual field deficits, such as those that may be obtained after suffering from a stroke. Dr. Yu has a virtual reality headset, along with a steering wheel and footpad controller to go along with a driving game. I got to test out the equipment by placing tape over my glasses (to simulate a visual field deficit) and trying to drive; needless to say, I was fortunate that I was crashing a car in a video game rather than in real life.
Learning about the process by which Dr. Yu has brought these projects to their current form is relevant to the aims of the program. For the prosthesis project, Dr. Yu described the entire story, which starts with the history of cataract removal. In cataract surgery, after the cataract is removed, a new lens is placed in the eye. In the early days, this lens was rigid and required a large incision, which was subsequently replaced by a foldable lens. This observation inspired the foldable prosthesis of Dr. Yu’s lab, and the process that he is taking to bring the idea to the market is an example of the possible path forward. I look forward to returning to the lab.
VA Hospital
Darius Ansari Blog

This week we were in the operating room again, except with Dr. Yu at the Jesse Brown VA hospital.
All of the surgeries performed were cataract removals, except the patients had denser cataracts than those we had seen previously at at the University of Illinois hospital. In order to phacoemulsify (break down) these cataracts, the operating surgeons employ a technique in which the lens is divided into four pieces with the active instrument (the phaco). Once grooves are formed to divide up the cataract in this way, the aspirator is used to remove the damaged lens, and the operation proceeds as normal with the implantation of an intraocular lens implant.
While observing the surgery, we noticed that the eye speculum (the device holding open the eye) would get in the way of at least one of the instruments of the surgeon. Dr. Yu confirmed this to us in a conversation we shared. During cataract removals, access to the superior lateral portion of the eye is critical, as the physician sits at one end of the patient’s head throughout the procedure. We got to work attempting to design a speculum that addresses this obstruction problem while still maintaining a wide/reliable enough eyelid separation.
Addressing Surgical Instrument Obstruction
Darius Ansari Blog
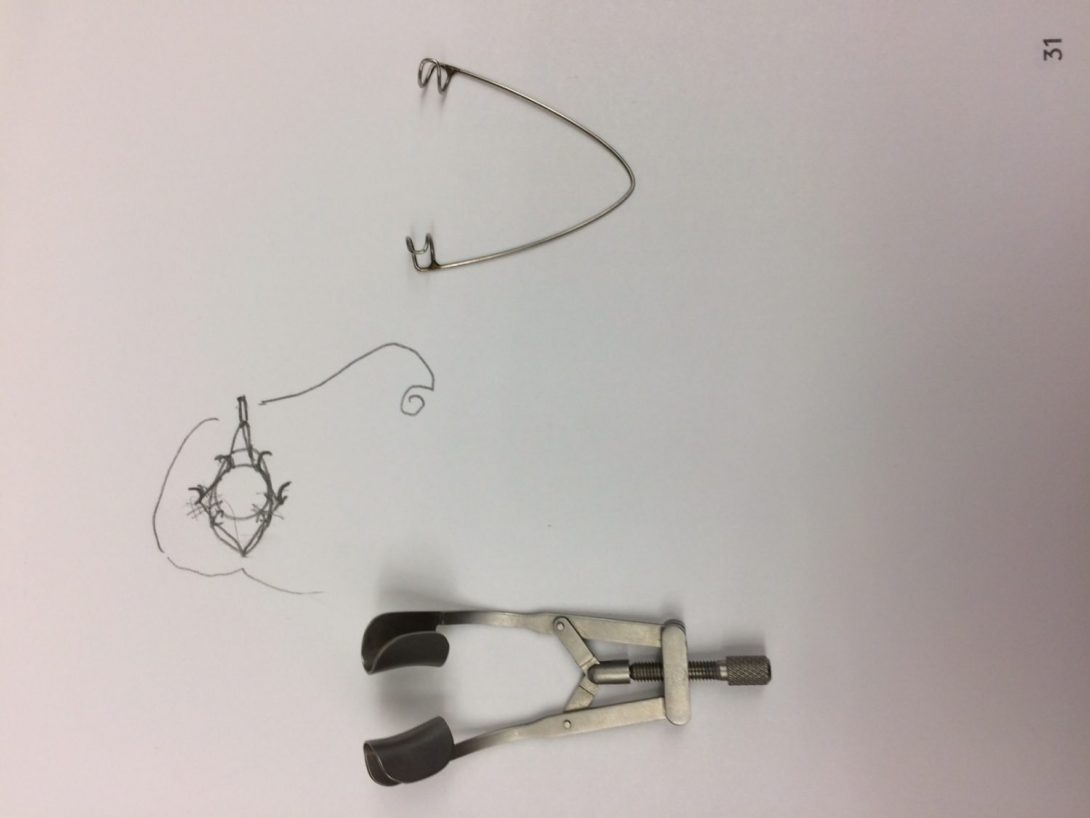
On Thursday and Friday we spent some more time with Dr. Yu in his laboratory in COMRB and in the Lions of Illinois Eye Research Institute. We were fortunate to witness an implantation of the keratoprosthesis into a rabbit preceded by a cataract removal. A particular speculum is used to hold open the eyes of the rabbit, which is pictured above next to a rat eye speculum.
As described in the previous blog post at the VA hospital, the eye speculum is used in every eye operation and a variety of designs exist. In essence, the speculum is placed between the eyelids and applies forces to provide prolonged separation. Although the function is simple and the device design is easily understandable, it often reduces the physician’s access/flexibility to operate on the eye. From watching videos of cataract removals performed by various ophthalmologists, it is apparent that the problem is more widespread than we had initially thought.
Brainstorming ways in which we can reduce the speculum’s obstruction of surgical tools has proven challenging, as the part of the device that provides its entire function is the same part that tends to get in the way of the surgeon. Nonetheless, we formulated some preliminary ideas, such as a design with the speculum handle on the medial end of the eye rather than the lateral. Changing the position/number of the speculum attachment points to the eyelid results in changes to the amount of eye surface exposed, and so any design implementing this idea may require prototype testing to determine whether or not the eye surface area is sufficient for surgeries such as cataract removals.
In the coming week, in addition to the normal clinical observations that we make, I would like to interview a variety of ophthalmologists in the department to try to understand whether or not they find the current speculum design to be problematic. On Wednesday, when we return to the operating room, I’ll make a particular effort to see if I can notice the obstruction (or lack thereof) myself; I hypothesize that ophthalmologists that have been doing the same procedures for years may not notice the speculum problems as they have become used to its position on the eyelids.
Mauricio Borda

Mauricio received his B.A. in Psychology and B.S. in Biology from Florida International University. He is board certified as a behavior analyst and worked in the field for over five years in Miami and San Francisco before starting medical school. His research interests include aging, neurodegenerative diseases, and robotics. His plan is to improve healthcare in underserved communities by utilizing the latest technology to maximize efficiency and lower cost. During his free time, he likes exploring cities, meeting new people, reading the latest astronomical research, riding his bike, hiking, and expanding his vinyl collection.
Mauricio Borda Blog
Mauricio Borda Blog
Understanding Your Environment
Mauricio Borda Blog
The hospital is a complex environment consisting of interactions between staff, patients, and machines. In this complexity, there are bound to be many opportunities to improve efficiency. I have been assigned the cardiology unit for the clinical immersion program Most of our time has been spent in the catheterization laboratory and a room dedicated to reading echocardiograms.
The catheterization laboratory, or cath lab for short, is used to access the heart via catheters. Before this technology, physicians had to open the chest wall, a much more invasive procedure. The insertion of the catheter can vary depending on the hospital. Most hospitals in the United States use the femoral artery due to its size and ease of insertion. At UIH and in much of Europe, the radial artery is used as the point of insertion. The advantages include less risk of bleeding, faster recovery time, and more cost effective. Disadvantages include a large learning curve for the physicians, higher radiation exposure, and longer procedure times. When developing a product, I must think outside the scope of the hospital I am observing to see if it is a useful application to other institutions. Other hospitals may also have work arounds that may help with coming up with a product.
Echocardiograms, or echoes for short, use ultrasound to image the heart including the chambers, valves, and aorta. Doppler is also used to see the flow of blood. Here’s a fun fact, red-shifted flow is rendered blue and blue-shifted flow is rendered red and that has become the standard, why would they do this? No clue. Echoes are great because they pose virtually no risks since sound is used.
The patient interactions were great. The physician explained the situation to the patients and any questions they had were answered. I am looking forward to interviewing patients later in this program to see what they like and don’t like about the setting and procedures. I also decided to brush up on my heart anatomy to get more from this experience. That’s a basic rundown of the environment I will be in for the next few weeks.
Psychology of Medical Innovation
Mauricio Borda Blog
My background as a psychologist gives me a unique perspective on the clinical immersion experience. I tend to be aware of human behavior and why people do what they do. When innovators attempt to make a medical device, they focus on the medical and engineering aspects of the design. I would argue that psychology is equally as important. Today we went to the remote monitoring clinic which allows you to monitor patients with pacemakers and defibrillators remotely. The pacemaker or defibrillator sends the data via radio frequencies to a hub connected to a landline, this then sends the data to the electronic medical record. That means that if the patient were to go on vacation, they would have to bring the hub with them and connect it to a landline there. Wouldn’t it be wonderful to have an app that can accomplish the same thing? Yes it would! Except, many people prefer the landline approach. This is due to the psychology involved with the patient population using the product. Many of these individuals tend to be older and some are not comfortable using/don’t own a smartphone. The two options are to either make the process more seamless or to adapt to the patient population and use older technology. After all, patient compliance is vital.
Another example is about physician behavior rather than patient behavior. Why do interventional cardiologists and surgeons have to stand during a procedure? Sitting would be more comfortable and sitting is the norm in large hospitals in Germany where many procedures are done daily. Standing for long periods of time with the added weight of lead can have adverse effects like varicose veins and back pain. Some mention maneuverability issues, some say it’s a preference. I suspect it is tradition and social stigma associated with sitting. We must make it okay for physicians to care about their own health as well. Look at this product for instance:
https://www.youtube.com/watch?v=XPQPn3udKQ4
It would be the perfect compromise between comfort, maneuverability, and health. Unfortunately, it is not widely adopted because of the psychology surrounding the clinical setting. Although I do not agree with the mindset, it is important to take these cultural practices into mind when designing a medical device.
In both cases, there are great ideas out there but if the target users are not comfortable using them, then it is not a good product. We must remember to take the time to understand the user’s environment if we wish to see our ideas come to fruition.
What Kind Of Doctor Do You Want To Be?
Mauricio Borda Blog

As a medical student, I always get asked which kind of doctor I wish to be. Normally that implies that they are interested in knowing which specialty I am pursuing. But there may be a better way to respond to that question. Yes, specialty is important, but equally as important is how you will practice medicine. During this program we have interacted with many cardiologists and their styles are extremely different. I have noted 3 great qualities including eagerness to teach, open to innovation, and knowledgeable about their field. I will discuss them below:
Eagerness to Teach
Some of the cardiologists we have followed really enjoy teaching. This is evident by the time they take to explain concepts and procedures to both the students and the patients. They are avid listeners and do a great job answering questions. They also ask us questions to test our comprehension. The nurses also did an amazing job teaching us about remote monitoring. I really appreciate that they take the time to do this and wish to emulate this quality once I begin practicing.
Open to Innovation
Some of the doctors we saw were content with how things were run and did not see the need to change much about their workflow. Others are constantly conducting needs assessments without noticing it and have pinpointed areas that need improvement. Even more impressive is that they have ideas on how these shortcomings can be improved. I hope the IMED program instills this sense of innovation into the medical students so that the medical field can progress even faster.
Knowledgeable About Field
Many of the people we have met are passionate about cardiology. You can tell that they took the extra steps to understand the details of what they are doing and why they are doing it. People trust them with their lives and they step up to the plate. It has motivated me to brush up on my heart physiology and anatomy.
This experience has been incredible and I have learned so much. Looking forward to seeing new things this week.
Standardization
Mauricio Borda Blog

There seems to be a common trend in biotech companies and more generally in tech companies that is causing consumers inconveniences. The problem arises from competition. Apple is the epitome of this phenomenon. They want people to only use apple products, so they made an ecosystem that makes using their products a seamless experience. The downside is that some other devices have better capabilities than apple products and there’s an incompatibility issue. For example, apple will not adopt USB-C, a universal port and has kept the lightning port in order to have a monopoly on the chargers and cables.
We witnessed a similar scenario in the remote monitoring clinic. The three big companies making pacemakers and ICD’s are Boston Scientific, Medtronic, and Abbott (formally St. Jude). In order to change the settings on the device, they must place a wand over the skin to connect with the device. This is fine if the patient knows which device they have. If they do not, three separate wands connected to what looks like a laptop in the 80’s must be hauled in. This is because only the wand made by the pacemaker company is compatible. To make things worse, all the data transmitted from the device gets sent to an online module for that specific company as well. This means the you must have three tabs open on your browser in order to see all your patient information. If these systems were standardized instead, then workflow would be much more efficient.
Visitor Comfort
Mauricio Borda Blog

We were doing rounds and checking on the patients. There was one woman that had to stay overnight and was being tended to by her daughter. The daughter was on an armchair next to the hospital bed but it only reclined a few degrees making it very uncomfortable to sleep in. You can tell she tried to make it comfortable by stacking blankets underneath. When we entered the room, the daughter made it clear that she had not been able to sleep and asked when her mother would be discharged. This got me thinking. How much thought is put into the comfort of the people visiting?
When you visit a loved one in the hospital, it is already a negative experience because you know they are not feeling well. But then you are subjecting yourself to more discomfort by not having a good place to sleep and not having access to entertainment aside from the few channels on cable. At least install a chromecast or have a smart TV. All rooms should also have a chair that converts into a bed.
Another problem is privacy. There are many shared rooms separated by a thin curtain. Private rooms are much more comfortable and allow you to feel more comfortable disclosing more information with your doctor. This is because you will not be worried about the stranger next to you hearing about your history.
We should always try to remember all the users when innovating. I suspect that visitors are usually not put into the planning stages when designing hospital layouts. They should be.
Self-Risk For Innovation
Mauricio Borda Blog
We stood next to the operator as he unpacked the catheter from its packaging. “Have you heard of the person who did the first heart catheterization?”, he remarked. We did not. He proceeded to tell us the story of Werner Forssmann. And now I will relay the story to you, because it is pretty damn cool. Werner Forssmann lived in the era where urinary catheters were gaining popularity and he had the idea of using a catheter to access the heart through blood vessels. After not getting permission from the hospital to try the procedure, he decided to try it on himself to prove it could be done. He applied local anesthetic on himself, inserted the catheter into his arm, and pushed it into his heart. He ran up to the room with the x ray and got the x ray film depicting the image featured on this blog post. Amazing. He later got fired by the hospital when they got word of what he did. But this turned out to be the birth of cardiac catheterization as we know it. This innovation was so great and made such an impact that he received a nobel prize.
There have only been a handful of humans that have done self-experimentation in order to innovate. Barry Marshall proved that H. pylori, a bacterium, is directly responsible for stomach ulcers. Previously it was thought to be caused by stress and ingesting acidic food. To prove he was right, Barry Marshall grew the bacteria and swallowed the contents of the petri dish. A few days later he had damage to his stomach and the biopsy showed colonization. Antibiotics cured him and others in a later double-blind study. He also received the nobel prize. Leonid Rogozov had acute appendicitis while in Antarctica. Flying back to another continent was not possible due to the weather conditions and he was the only doctor on base. He cut himself open and operating on himself. He got two assistants to help hold up a mirror while he operated. He did not get a nobel prize, but he did get to live appendicitis-free and had the best conversation-starter on the planet.
This goes to show that sometimes you have to take risks and go against the status-quo in order to innovate and change the world. They inspire me and others in the medical field to try and push the envelope.
Wireless Operating Room
Mauricio Borda Blog
I was shocked by the number of cords in the operating room. Many devices are stacked atop each other like a totem pole, waiting to be used. This leads to many disconnected cables dangling in the air. One device is chosen and the stack is wheeled into position. It seems inefficient. Later, they had to do an ultrasound to see the chambers of the heart. So they wheeled in yet another machine. I asked the operator what the cable connected to the ultrasound transducer was for and he told me it was for power and to communicate with screen. He informed me that there are new models that are wireless and connect to the large screen in operating rooms.
We have seen it many times in an average consumer market, the next big thing is making things cordless. Wireless charging is gaining popularity and eventually we will have induction charging built into the walls or transmitting energy and recharging your device as you walk around the room. Unfortunately, in the operating room, older technology is sometimes used. For instance, the device that is used to connect to the pacemakers are very bulky. When I asked them why all the bulk was needed, she responded that there had to be room in the box for a built in ink printer. If you are printing from an electronic device, that means there must be a better method to accomplish the task. Printing something on paper is highly inefficient.
A wireless operating room will result in less clutter and hopefully more focus on the procedure itself.
Redesigning A Human Heart
Mauricio Borda Blog
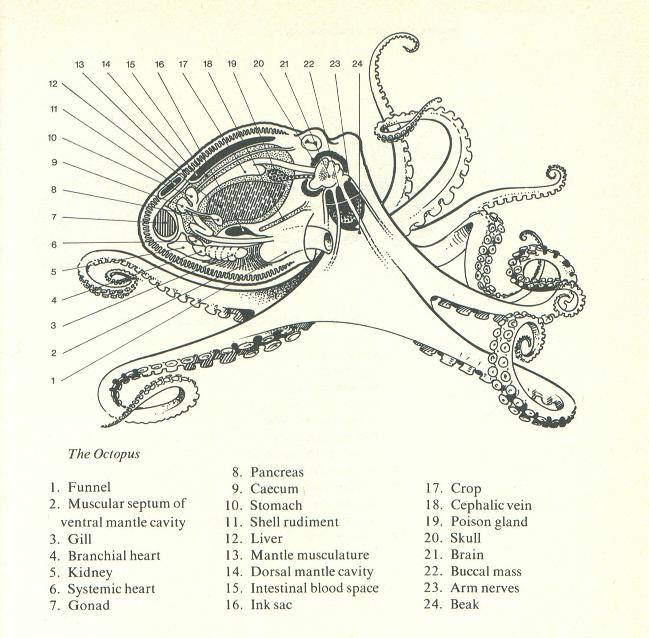
In the Clinical Immersion Program, we are encouraged to think freely and to welcome outlandish ideas. I used this as inspiration to answer the following question: If technology were not an issue, how would we solved heart disease? One of the physicians I encountered suggested redesigning the heart itself. I thought this was an interesting idea. It is conceivable that in the future we will be able to 3D print organs and coat them with our cells to avoid transplant rejection. While it may be tempting to recreate the current design of the heart, we have the option of creating something more efficient. Let’s look at other organisms for inspiration.
Most fish have one atrium and one ventricle, the blood goes through the heart, gets pumped out and gets oxygenated by the gill capillaries, then it travels systemically and returns to the heart. This seems very efficient and would be worth taking into consideration for our optimal heart. Octopuses (or octopodes if you want to seem smart) have three hearts. One is an organ heart in the center and the other two help pump blood from the gills. This gives us the option of designing a human with multiple hearts if it improves efficiency. Amphibians have three-chambered hearts but the oxygenated and deoxygenated blood get mixed making this circulatory system less efficient.
Another factor we should consider is coronary arteries which provide oxygen to the heart muscle itself. They are the first vessels to branch from the aorta and are susceptible to plaque buildup. Seems inefficient to have a massive amount of blood going through the heart and having no diffusion take place.
The ideal circulatory system in my opinion would involve two hearts containing two chambers each, like a fish heart, and each capable of pumping the blood throughout the body independently. The reason for having two is a failsafe mechanism similar to the kidneys. The chambers will also have diffusion capabilities on the inside of the chambers to avoid the need for coronary arteries. I am sure there are some flaws to my design but that is the beauty of innovation. You begin the design process assuming there are no boundaries and you tweak the design to accommodate for limitations and feasibility.
Importance of Feedback
Mauricio Borda Blog

Feedback is the reason Amazon is successful and why people trust strangers in their homes with Airbnb. Feedback has also been shown to be very essential during this program. An example of this was when we were designing our prototype. We had an idea for an innovation in the catheterization lab that could potentially change workflow. After the cases were done for the day, we United with all the hospital staff that works in the lab to see what their perspectives were on new innovation. This was a very valuable experience because new issues that we did not consider surfaced. For example, they realized that in order for our product to be feasible, we needed to take into account the worst-case scenarios. If the patient has a code during the procedure, it is important to be able to switch to the protocol without hindrance.
Other issues with our design such as space in the lab surfaced and we took this feedback and redesigned our product. Our mentor in the program did an excellent job when listening to our feedback. He would summarize our feedback and would encourage us to inform him of areas of improvement rather than just compliment the program.
Our final piece of feedback so far has been during the 3D printing process, the person in charge of printing or prototype gave us cost and time estimates and suggested we redesign our product to make it more efficient or to consider using acrylic with laser cutting rather than 3D printing unless necessary. Innovation is 50% making and 50% listening and that’s something I never considered before this program.
My Perception Of Cardiology
Mauricio Borda Blog

The concept of cardiology has changed tremendously since the beginning of the program. Over the last 6 weeks I have gotten a realistic approach as to what cardiology entails. I was under the impression that most procedures of the heart required either open heart surgery or intense medication. I was not aware that catheterization played such a major role in many procedures. This was much less invasive than I expected and it fascinated me to know how much is possible through access via the vessels.
Cardiology is more approachable than I expected also. During our time in this program, we began seeing the same procedures being repeated on other patients. Although some may think that this will get repetitive quickly, it is important to remember if there is a lot of anatomical variation and that each person has a unique situation and adjustments may have to be made based on allergies or other unforeseen circumstances. I was also under the impression that cardiologists were all sleep deprived and had serious personalities but what I’ve noticed is that all of them are very passionate about their field and surprisingly approachable.
I am excited to see what the clinical immersion program and cardiology unit will collaborate to produce in the future. This was the first year that this specialty was added and it has been nothing but a positive experience. The heart is an amazing organ and it has been a privilege to witness the skilled hospital staff in action and to see patients in a state of vulnerability. I have learned so much and will strive to continue the teaching culture that I witnessed in the hospital.
Christopher Deeble

Chris grew up in the suburbs of Sacramento, California and has always been an avid fan of inventing. His other hobbies include cooking, skiing, tennis, and traveling. As an undergraduate, he studied bioengineering at UC Berkeley. His research experiences include microfluidic research (for point of care diagnostic testing) and Alzheimer’s disease research. As a part of his gap year before medical school, he applied his engineering skills to help his parents start an orchard. As a part of the IMED program, he hopes to learn more about how to how to apply engineering principles toward developing solutions that will improve patient care.
Christopher Deeble Blog
Christopher Deeble Blog
The first days in Anesthesiology
Christopher Deeble Blog

The clinical immersion program is headed by Dr. Miiri Kotche (from the bioengineering department) and is designed to provide students an opportunity to perform a needs assessment in clinical departments of choice. Those pieces of information can then be used to generate innovative solutions to problems in those fields. The first two days of the program had the students become situated with each other and their departments of choice. My department of choice was Anesthesiology because it is a field that is very technical in nature and I saw many great opportunities for innovation.
It was during the first day’s workshop in the innovation center that I met my group members Joe, Nick, and Vijay. Joe is a fellow rising M2 (second year medical student), and Nick and Vijay are rising fourth year bioengineering students. This variety is crucial to our program because it will provide us different viewpoints on the issues that we will encounter. I look forward to working with them and seeing what unique ideas they will come up with.
The second day of the program was the first day in the hospital setting. Anesthesiology predominantly is involved with operations, so our first task was to become familiar with the operating room and associated spaces. Although the first day had us start at 8 am, we decided to change the start time to 6:30 am since that is the typical start of a day for an Anesthesiologist. During this first day we met our mentor Dr. Nishioka, his Anesthesiology colleagues, and many staff members working in the OR. Our primary goal this first day in the OR was to in general observe how everything worked. A few of my observations were centered on the use of medical instruments, organization of the rooms, and the flow of staff, patients, and supplies.
Picture: Anesthesia machine and supporting equipment
Topic to think about
Christopher Deeble Blog
For the last two days of the week, Dr. Nishioka had our team focus on some specific aspects of Anesthesiology and how the operating room works. We started by observing patients and staff in the preop area. One point of interest was the busyness at the start of the day, but then the relative slowness after the surgeries started. Some questions we thought of during this time were the following: 1) Is there a way to spread out the busyness? 2) How can many teams of providers see the patients without causing congestion to the area, potentially causing anxiety to the patients, or disrupting the workflow of others? 3) How to keep track of beds during this time?
Our next goal was to focus on the machines that Anesthesiologists use on a regular basis. I was amazed to find how many machines they encounter each day. And the physics, chemistry, and engineering behind all these machines can be quite complex. An important question that arose was how to know if the machines are accurate? And to what level is this significant? Further, Anesthesiologists must use all this technology in the operating room in addition to the manual procedures that are still required. One resident I talked with said it would be great if there were a way to easily control the machines from across the room so that he wouldn’t be so restricted to one area. In addition to learning more about what Anesthesiologists do, we also had the chance to go to meetings and lectures to learn more about the behind the scenes work and science of this field. Through all of this, I learned that there are many different ways innovation can be applied to Anesthesiology, and I’m sure I will encounter many more in the weeks to come.
Picture: Anesthesiology supply cart
Some other details
Christopher Deeble Blog

For the first two days of this week in clinic, we focused on a few more general issues. The first was medical education. We had the chance to talk with a few residents and with Dr. Nishioka about their feelings and thoughts about the medical education process in the USA. The topics we focused on were the learning process (self driven or structured), the types of knowledge to learn, and standardization (such as evaluations, work hours, and examinations). The next topic we focused on was scheduling the OR. This was to evaluate how to maximize efficiency and decrease the burden on the clinical staff. We would like to dive deeper into this topic by further examining how the typical flowchart of scheduling breaks down.
The other experience I had during the first half of the week was observing and talking with an orthopedic surgeon. Interestingly, orthopedic surgeons work with a vast amount of medical instruments. And by talking with him, I found that innovation in this field may not be creating more devices, but by condensing the needed amounts.
Picture: Notice how cumbersome is it for the surgeon to take an X-ray with the setup of this machine in this room.
More specific to Anesthesiology
Christopher Deeble Blog

For the latter part of the week, we focused on problems more specific to Anesthesiology. Our first assignment was to evaluate the use of an emergency airway box, which is a device that contains all the necessary equipment and medications to provide a patient with an emergency airway. I enjoyed this one because we were able to learn about the background, the prior process, the updated process, and then view it in action. I always believe that some solid theory and then a real world application help me to best understand a situation. Although I wasn’t able to use the device yet myself, I have a better idea of what is going on.
The next focus was again on equipment, but this time in the OR. I had a brief talk with one of the OR nurses about what could be improved. Even with all the innovation out there, there is still opportunity for improvement. In particular, we talked about problems encountered using the IV poles, and the use of wired power. Also during this time, I noticed just how many wires and tubes Anesthesiologists use. I remember seeing an Anesthesiologist holding around 10 wires and tubes from one patient. Does it have to be this way? I’m not sure, but I’m curious to find out.
Note: In selected picture, notice how many cords and wires the Anesthesiologist is holding in his hand. These are all connected to the patient in some way, but go to a variety of machines located in a variety of directions.
Check out the machines
Christopher Deeble Blog

For the first 2 days of this week, I focused mostly on the design and layout of machines and rooms. One topic that was brought up was how to optimized the delivery of patient administered medication so that it would be safer and less bulky. Next, I visited the IR (interventional radiology) suite to see how their rooms are organized and how they conduct procedures. The rooms were very reminiscent of the OR, except everything was very cramped. I’d say they have even bigger space and organization issues than the OR. Also, IR room organization is complicated by the fact that there are very large and permanent X-ray machines in each room. This also directly affects the Anesthesiologists because they must place their machines further away from the procedure bed compared to the OR. Thus the tubes and wires are even longer in this place. Finally, I noticed that the Anesthesiologists have to often move between the procedure room and the control room (room with computers and protective glass to prevent X-ray exposure) to make adjustments and log data.
The next day, I sought to address one of the main problems that Anesthesiologists and nurses talk about – wires and tubes. A few of the nurses in the OR recount the previous clinical immersion team also focusing on this problem, however there was no follow up and no solution has been implemented. Thus, I focused on what was needed in the OR, how the setup procedure was conducted, and looked at how the rooms were organized for the procedures. My main conclusion was that there was little planning before the surgery started in terms of needed equipment and room organization. Some of my thoughts were that IV poles could be consolidated, unused machines could be removed from the room, and outlets could be more optimally placed. Although the planning stage would take some time from 1-2 people before the surgery, I believe this will offset the time lost due to inconveniences that occur during the entire surgery – inconveniences that also directly and indirectly affect many people.
While I encountered these problems, my next steps are to explore what else has been developed in other hospitals. Even this hospital has an improved OR room called the hybrid room. I want to visit that room to analyze its layout, and see if there are improvements here that will address the problems I have mentioned before.
Note: the selected picture shows one of the IR procedure rooms. Notice how large the X-ray machine is (this one has 2 axes), and also how much equipment is in the room vs. the limited space.
More machines and behind the scenes
Christopher Deeble Blog

During the latter part of the week, I focused on more details about the machines I encountered, as well as some ways that the hospital works. While in the preop area (location before surgery), my group and I noticed that there occasionally was a shortage of computers to log patient data. Further, the computers then went unused for the remainder of the day once many of the patients went to the surgeries. And finally, we noticed the many of the computers had lag in the loading of different parts of the program. The conclusion from these observations was that this computer problem was causing serious delays and also user frustration among the staff. Next, I focused on a common procedure in Anesthesiology – the nerve block. This procedure utilizes many machines and devices to ensure that the physician administers the local anesthetic in the correct location. Some of my observations are as follows: the ultrasound machine to locate the vessels and nerves had limited with persons of a particular body habitus; the administration of the anesthetic seemed to cause the patient much discomfort; maintaining the position of an epidural catheter proved difficult for long durations. Addressing any of these issues would improve patient care and satisfaction, especially by reducing the needed procedure time and pain caused.
My group and I also had the chance to have a meeting with two business managers from the hospital (OR and supply). They had lots of important insights into potential improvements. In particular, they highlighted addressing expired products that remain in storage, and the wasted vials and products during surgeries. Thus I can envision some changes to hospital policy, and maybe a tracking device to help with organization and use of supplies. Interestingly, the managers have collected data on these, and analysis of such data may be very enlightening.
Note: the selected picture shows the current technology used to keep epidural catheters in place. Since the device is attached to the skin (and not a fixed structure such as fascia or bone), there is a somewhat high rate of dislodgment.
Plenty to Consider
Christopher Deeble Blog

The start of this week was similar to previous weeks. However our group’s mentality was a bit different because we have now become very familiar with our department, and are now considering potential concepts to address the needs we encounter. We entered with week with two main focuses: patient identification and resident training. Thus we looked in more detail into the underlying process of how these problems arise. And we discussed with our mentor, Dr. Nishioka about different ideas to solve these problems. Through this, we narrowed our focus even more to consider just resident education – as this seemed the most feasible given our circumstances. Dr. Nishioka brought up some important points to consider for this: 1) how to bill patients in the teaching setting; and 2) the observation that residents prefer real procedures to simulations. Thus when we enter the selection phase of the design process, we will definitely need to consider these real-world problems with adoption and implementation. Further, I would like to spend some time talking with residents to see what their viewpoint on this is. Then I will hopefully have the perspective from both the higher ups and the ones in the trenches.
Yet even with this specific need, the Anesthesiology department never ceases to provide with new ideas. I decided to keep track of these issues and limitations too, since they too have a great significance, and I have feeling that one day I will have the chance to work on them as well. In particular, I encountered the following: problems interfacing machines with the EMR, refinement of Anesthesiology techniques (such as spinal and epidural blocks), practicing Anesthesiology on infants and young children, and applying current imaging technology to all body types. Addressing these problems will improve patient safety, improve efficacy, and reduce fatigue of the providers. I am excited about these findings because I see great potential for improvement, as well as the use of technology for simple and elegant solutions that will ultimately help the patients we serve.
Engineering Inspiration
Christopher Deeble Blog

For the latter part of this week, I took a special focus on medical devices and workflow improvements. It’s been a while since I’ve engineered something, and I think that part of me is giving me a lot of inspiration recently. The findings that I will write about in this blog are very technical, but nevertheless will provide great improvements to Anesthesiology and medicine. One such device would be a blood loss / blood volume monitor. This would help reduce the variability of providing fluids during surgery, and avoid the costly mistakes of fluid loss or fluid overload. Next I recall a conversation with an Ophthalmologist who said he had a machine that required three hands to operate – however he currently only has two to use. Thus I think there is a simple design fix that can combine two controls into one, or allow utilize another mode of control (such as eye tracking or voice command). Another instance of an improvement would be the selection of veins for grafting. I noticed that the surgeon had to test the flow of the vein in real-time during the procedure. However this took some time, and the patient was required to be under anesthesia in the OR for this to occur. I wonder if there is a way to test it out ahead of time, and provide the surgeon with a way to select the best regions before making major incisions. The key insight here is that veins are often somewhat superficial (especially the vein being harvested here: the great saphenous vein). I believe this would greatly reduce the complication risks associated with surgery.
When focusing on workflow, I turned my attention again to length of time for routine procedures, and the handling of OR supplies. This week I noticed that some Anesthesiology procedures such as nerve blocks or starting IVs could be very quick, or take a very long time. I think this is due to the variation of the anatomy of each patient, the ability to locate the anatomical landmarks, the experience of the physicians, some luck. Thus I can envision more refined medical devices that allow the physician to more easily perform his job. An example would be a blood vessel finder that allowed the physician to clearly locate the vessel and provide him with instant feedback to where his needle currently is located. Now while these devices already exist, but I believe they can be even better. Also, I envision a multi-function machine in the future that is standard in each room. This will address the current problem of machine shortages (or not having them in the right place at the right time). Next, we had an insightful talk with the manager of central supply. The coordination of the supplies for the OR and the hospital is truly amazing, and requires clockwork-like precision. The biggest problems that were brought up were the amount of inventory available at any one given time, and the turnover time. However another issue I noticed was the huge amount of different surgical supplies. Some trays had hundreds of different tools. I believe that this very large variety is a cause for much of the delays and shortages of supplies. I wonder if there is a way to streamline what is needed. Perhaps we can redesign how procedures are performed based on the tools needed.
Supplies
Christopher Deeble Blog

For the first part of the 5th week, we continued to analyze the stocking of anesthesia supplies in the OR. We often heard from resident anesthesiologists that certain supplies and equipment are commonly missing. To investigate further, we decided to shadow the anesthesia techs around the hospital from an entire shift, starting at 5 am. From this experience, we learned the great variation and great number of supplies that exist just for anesthesia. Further, we learned about the amount of work and planning that goes into successful stocking of the OR. We found that a shortage of staff was one of the main problems, as well as the distribution of staff throughout the day. This created role confusion and a lack of communication. In addition, we noticed other subtleties that could be improved as well. We found that a shortage of equipment was a common problem. IV poles and monitors were often left in different wings of the hospital. While recover of these supplies was the job of the anesthesiology residents, we found that some often did not return them back, thus creating a shortage in the OR. Further, certain machines were in great demand, such as glidescopes; we counted only around 8 for the 19 OR rooms. Therefore it was common for staff to look in many rooms and borrow the glidescopes for their own cases. Overall I think a good mapping of all the supplies and machines in the OR will help us better understand what is going on, and lend to possible solutions to fix the problems that we encountered.
Hospital Design
Christopher Deeble Blog

On the last day of the 5th week, we had the privilege to talk with a hospital designer. This meeting was motivated from our observations of the hospital from prior weeks. We noticed that there were bottlenecks in the workflow due to space constraints, as well as supply problems due to the organization of the hospital. Thus we wanted to talk with an expert to learn more about how hospitals are designed, and also thoughts on renovation. We learned some interesting insights from this talk. One was that updated and modern hospitals have the potential to draw many patients; it’s not just now good the doctors are. With this in mind, it is important to walk through a hospital and try to imagine what the patients see, and what they may think and feel. Some things to consider may be noise and lighting. For overall hospital design, the following characteristics are important for the longevity of the hospital: durability, adaptability, and flexibility. Next, when redesigning/renovating a hospital, a master plan and a budget are key. However, it is often times easier to start from scratch and build a new hospital. This may be due to the shift in the preferred layout in the last few decades. Older wards were designed with the staff in the middle of all the patient beds, and locate monitors and sounds directly in each room; thus privacy was more limited. However now a more common design is to organize the staff and patient areas such that the patients have a more comfortable experience; a change, for example, would be to have a central command area that handled of all the alarms, and thus patients wouldn’t have to hear all those sounds. I some aspects I like this change because I can see the improvement and focus on patient care; however I still have a nostalgic attachment to the old hospital style. I look forward to seeing in a few decades which design is the best after all.
End of a Chapter… Start of a Journey
Christopher Deeble Blog
My experience was that the six-week Clinical Immersion Program passed by very quickly. I think this perception is a good thing, because it means I had a very enjoyable time. I have many memorable experiences and I really enjoyed working with my group. We were able to shadow many different staff in the hospital and learn a lot about how things work. This gave us many opportunities to see different issues that arose, and this helped us develop our needs statements and narrow down possible projects to work on. The main one we decided to focus on was learning opportunities in the OR. We concluded that the OR space is very cramped, and the field of view to learn is limited. Although we skipped a few critical steps for the design process, we decided that a quick and cheap prototype would be something fun and productive to demonstrate our idea. We created a video system that better captures critical views from a surgery (or procedure), and demonstrated is effectiveness in a mock surgical setting. While the scope of this course was to gather observations and create needs statements, this is no doubt a significant part of the process. I appreciate the length of time given for us to really analyze and discuss the problems we encountered throughout the six weeks. I believe it gives us a great basis of understanding of Anesthesiology, as well as a great number of directions for future projects. And while the six weeks have come to a close, I believe my group and I will continue to pursue our ideas much further and create many projects in the years to come. I want to give my great thanks and appreciation to the clinical immersion staff for arranging and preparing everything. The amount of work must be great, and I am so thankful for this opportunity. Further, I would like to thank my group members as well as the UIH Anesthesiology department for their kind and thoughtful mentorship of us this summer.
Goodbye to the 2017 Clinical Immersion Program, and hello to many greats things to come in the future.
Susan Doh

Susan’s curiosity in the intersection of technology and medicine began during her undergraduate studies at the University of Chicago while she was studying biology and conducting research in immunology. At this time, she also become fascinated in the field of synthetic biology and co-founded and led the University of Chicago’s first team to participate in the 2013 International Genetically Engineered Machines (iGEM) contest held in Toronto. After graduating in 2014, she followed her passion in biotechnology at the National Institutes of Health as a research fellow in cellular cancer immunotherapy. Currently her goals in IMED are to broaden her knowledge of other technological fields and learn about their applicability to medicine and public health. Ultimately, she hopes to develop a capstone project that supplies innovative healthcare solutions and bridges together technology and community service.
Susan Doh Blog
Susan Doh Blog
General Ophthalmology Clinic
Susan Doh Blog
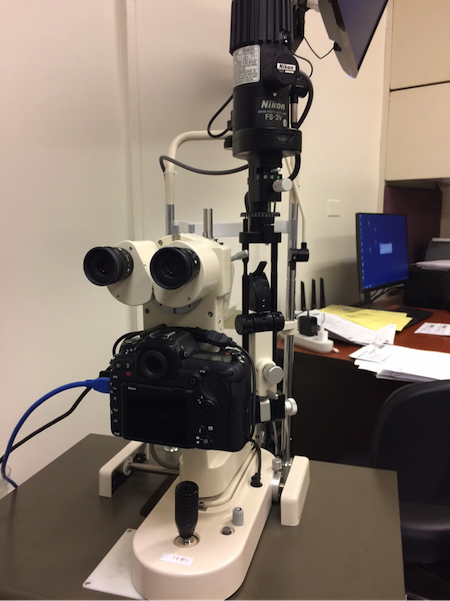
Ophthalmology is a specialty that blends the old and the new and the simple with the complex; as a result, there are many opportunities for innovation. Ophthalmologists undergo training in both surgical techniques and primary-care like bedside manner and patient interaction. In addition, the tools used in ophthalmology clinics can be quite divergent in their technological scope: for example, the opthalmoscope utilizes microscope technology that has been relatively constant and known for many years while the an Optic Coherence Tomography gives precise quantitative measurements of the retina not previously possible. Moreover, Ophthalmic surgies can utilize rather basic surgical tools (forceps, calipers, needle, and thread) or advanced surgical microscopes. As a result, physicians of this speciality may be scantly available in rural areas where acess to these resources and ability to undergo this type of training is not possible. As a result, a number of patients seen in the opthalmology clinic were from rural Illinois. In contrast, optometrists are more commo and can be great mediators for remote patients.
Everyday clinical practice involves use of a slit lamp which together with an adjustable chair on which the patient sits helps the ophthalmologist visualize the subtle layers of the anterior compartment of the eye (pupils, lens, cornea).
One potential for improvement is the ergonomics of the ophthalmologist’s chair for many ophthalmologists suffer from pinched cervical nerves. In addition, the optics of the scope can make it difficult for training and even experienced ophthalmologist determine depth perception with the light source is shining on the patient’s eye head-on. Depth perception during an exam is important for differentiating the different layers of the eye (cornea, haze of stroma, aqueous humor-an optically empty area) and is useful clinically for when one wants to determine the depth/location of an ulcer, for example. In addition, for extremely tall or short patients, the adjustment of the chair can be more customizable to accommodate for these patients.
Neuro-Ophthalmology
Susan Doh Blog
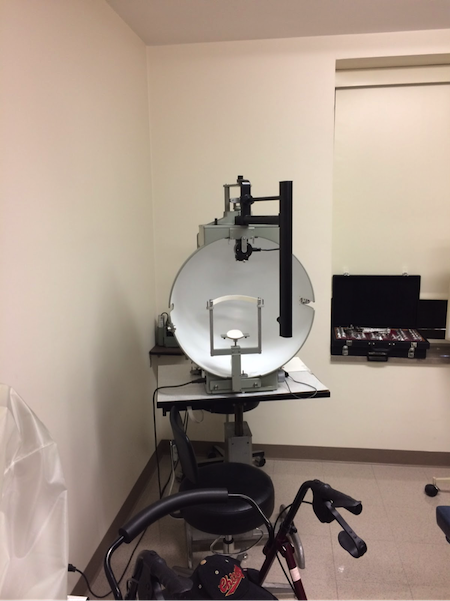
Neuro-Ophthalmolgy is a subspecialty of opthalmology that does not require the surgical techniques of general ophthalmology and commonly treats patients with visual complications from neurological conditions: e.g., pituitary tumors that impinge on the optic chiasm. As a result, some neuro-ophthalmologists train as neurologists first then ophthalmologists or vice versa; those with the former training find it a more difficult learning curve to operate the ophthalmoscope and distinguish the subtle parts/changes in the eye but have better training in reading MRI. Currently, this discrepancy is addressed through practice. Nevertheless, there is potential for the development of new educational tools to improve and speed up the learning process of using slit lamp biomicrosopes.
Neuro-ophthalmologists also utlize various machines that general ophthalmologists may not. For example, a pupillography utilizes IR light to visualize and measure pupil size, which is important for conditions such as Horner’s syndrome.
Frequently, neuro-ophthalmologists rely on measurements from visual field testing, which can measured and analyzed by different machines and software. The Humphrey visual field is most commonly used to test central vision.
http://www.glaucoma.org/treatment/what-is-a-visual-field-test.php
The Goldmann software shows hand-drawn visual field measurements as taken by the radiology technician. In contrast, the Octopus is completely computerized.
Most neuro-ophthalmology involves diagnosing and the state of the optic nerves. Fundus photography gives a qualitative visualization of optic nerve, from which one can observe the optic disc, optic cup, and vessels.
http://eyewiki.aao.org/Optic_Nerve_and_Retinal_Nerve_Fiber_Imaging
OCT (Optical Coherence Tomography) also visualizes the optic disc, cup and nerve but gives gives quantitative measurements of retinal nerve fiber layer thickness.
http://eyewiki.aao.org/Optic_Nerve_and_Retinal_Nerve_Fiber_Imaging
http://www.eyes.arizona.edu/Teaching/MedStudents/FundOph.html#IV.InstrumentSettings
Patient Education
Susan Doh Blog
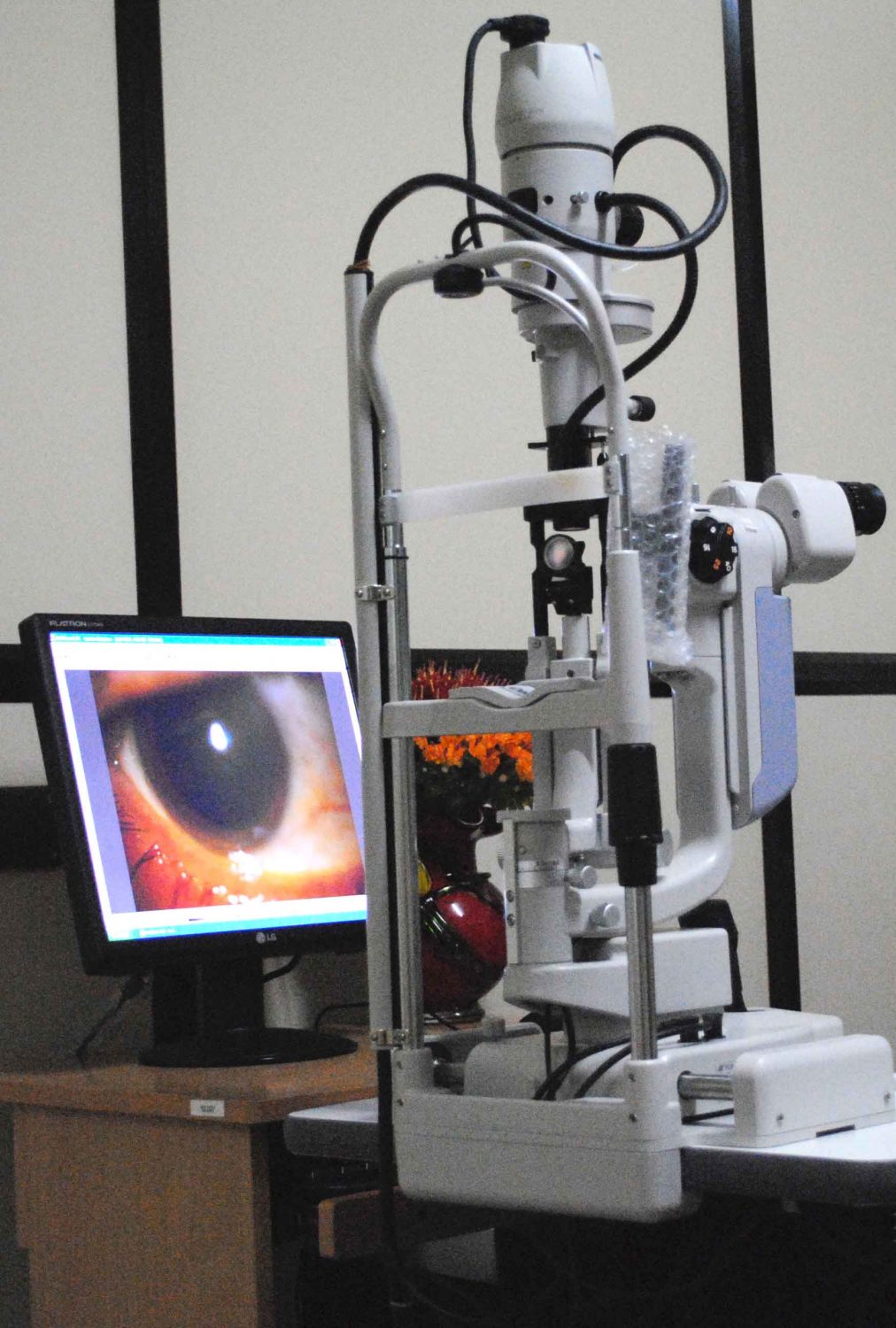
Ophthalmology could benefit from increased use of visual aids to educate patients and improve patient care. Currently, the use of a photographic biomicroscope is not widely adopted in general ophthalmologic practice over the clinical slit lamp biomiscroscope. In certain research clinics of the Eye and Ear Center, the photographic biomicroscope is used to document visual findings from the slit lamp from patients that participate in clinical trials but is also a powerful tool in patient education. Photographs of the patient’s eyes taken seconds before are displayed on a monitor and referenced by the physician to illustrate the patients’ conditions. For example, one patient with eye irritation was shown a picture of her eye with a red ring of irritation around her contact lens to illustrate the potential cause of her red eye due to the steep curvature of her contact lens. In addition, while most clinical exam rooms have posters of anatomical diagrams of the eye, these are neither referenced by physicians in their daily clinical practice nor useful for patients who lack a profound understanding of the anatomy of the eye. Simpler diagrams of the anterior segment or one-pager infographics of common conditions such as Fuch’s dystrophy may greatly aid patients’ understandings of their conditions. A consistent practice across pharmacies and clinics for ophthalmic medications is the use of the same colored caps to represent certain medications. This eases the burden on patients who must take multiple different eye drops of confusing names at different doses and also eases the work for physicians who have to reference only the color of the medication bottle to get instant recognition from patients of the medication. In contrast, a complex discussion the risks and benefits of certain medications over others and whether to increase or decrease dosing of medications are not so easily addressed through color-coding. Posters of specific medications, including their risks and benefits, what symptoms to look for when having to titrate the dosing up versus down, and their mechanism of actions in a simple, graphic format can help patients understand these complex discussions with their doctors better.
An Ophthalmologist’s Toolbox
Susan Doh Blog
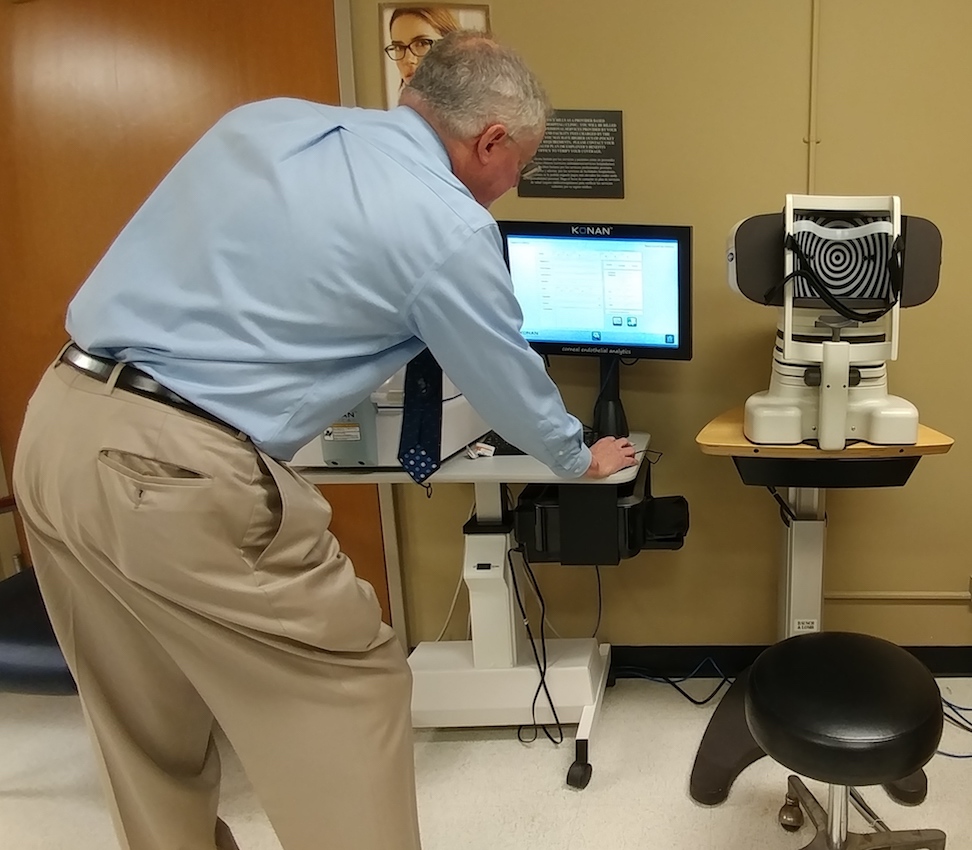
Various tools are that range from simple to very complex are used to measure and treat conditions of the eye. For example, the simplest form of temporary relief from a condition before the patient’s consult to oculoplastics for permanent surgical correction was a piece of tape used to prevent the curling in of the patient’s lower lid to prevent further irritation of her cornea. More common tools used for virtually every patient in the cornea service are the tonometer and pachymeter, which measure intraocular pressure and corneal thickness, respectively.
Before these tools are used, physicians apply numbing drops since the wands of these tools must be applied directly on the surface of the eye to obtain exact measurements. Adults are able to tolerate the measurement process well. However, for pediatric patients, especially fussy ones, obtaining these measurements are a greater struggle. Once pediatric patients begin to cry, their intraocular pressures increase, confounding the measurements of the tonometer, and often pediatric ophthalmologists must wait until the patient is under general anesthesia for a procedure for more reliable results. However, the advent of a new type of tonometer such as the “ICare” Tonometer which has been recently been adopted by physicians may help address this measurement error for certain pediatric patients because it does not require prolonged direct contact with the eye.
In oculoplastics, the Hertel Exophthalmometer is a commonly used simple instrument to measure the bulging of the eye from the lateral orbital rim to the corneal apex, which is important in the case of Graves’ disease or Thyroid Eye Disease. In the future, one could imagine software that measures the bulging of the eyes and drooping of the lids through photographs.
The most recent and often last resort treatment for defective corneas in adults is an artificial cornea replacement called Boston Keratoprosthesis (KPro). The replacement cornea consists of a corneal graft sandwhich between layers of metal plates, in which the “button-hole” configuration aids oxygen and nutrient flow. The Boston KPro is also used to treat pediatric patients with the congenital condition known as Peter’s anamoly in which the anterior segment of the eye has insufficiently developed and is favored over standard corneal transplants which would have to be done multiple times throughout the patients’ entire lifetimes. Currently, the technology has its complications such as bleeding, infections, and increased intraocular pressure (IOP). In addition, the KPro prevents the measurement of IOP by standard tonometers. As such, the Boston KPro is an emerging treatment form that many ophthalmologists are working into their clinical practice and can be improved upon for patients in which standard corneal transplants are not possible.
Technology in Ophthalmological Graduate Medical Education
Susan Doh Blog

Due to the eye’s small size, many ophthalmic surgeries require fine motor skills that must be honed to prevent even minor mishaps that can result in damage to delicate structures such as the cornea and retina. Even surgeries external to the eye such as eye muscle surgery, which are not as small in scale as vitreoretinal surgery, require great care: exertion of too much force when dissecting away the layers of the eye can result in unintentional abrasions, complicating recovery for the patient. As such, residents learning these techniques practice using EyeSi, an ophthalmic surgical simulator that provides several modules aimed at training specific skills and teaching surgical procedures while providing immediate, quantitative feedback.
The student first selects a module, grabs the correct tool, and views the “patient’s” eye through the microscope to begin the procedure. The left foot pedal adjusts the focus and position of the microscope, while the right foot pedal controls the aspiration of the vitrectomy cutter. As a result, the simulator mimics the set-up and controls of a real operation table.
During the module, the student can use real-time cues to aid their approach of the tools inside the eye to the target. For example, shown below in the lower right-hand side of the screen is the depth of the tool relative to the cornea above and iris below. This informs the student so that he or she is careful not to touch either one and remain within the boundaries of the anterior chamber of the eye.
Once the goal is achieved, the module ends and the student receives a score out of 100 along with a detailed breakdown of how well he or she did in such categories as instrument handling, microscope handling, and tissue treatment.
In addition, residents largely utilize the wet lab microscopes in the surgical training lab to train with physical specimens that resemble the real human eye most closely and no doubt are necessary for all components of building muscle memory—feeling the subtle changes in resistance and texture of the different layers of the sclera and cornea, for example. This of course takes time, but to speed up the learning process, one could imagine a special type of surgical tool students could use during practice on eye tissue that combines the properties of the simulated tools of EyeSi and the traditional metal forceps, aspirators, and cannula. For example, one could imagine surgical tool used for microsurgeries of the eye that would give real-time feedback in the form of pressure or other measurements and provide warning signals when the student applies wrong or bad technique on the physical specimen. This would allow the ophthalmologic residents of the future to practice surgical procedures in the safety of the lab with the advantages of both EyeSi and practice using physical specimens, thus improving resident education and surgical safety for patients.
Naomi Faulk

Hi all! I am a rising bioengineering senior. I enjoy (and draw inspiration from) music, the Lord of the Rings trilogy, cookie dough ice cream and cats. Despite the many prospects of majors I have tried, I found that studying bioengineering has increased my scope of impact more than any other major. I plan to go on to medical school after completing my BS in BioE. I hope this experience, along with my major, will help me in my future career to identify where the present systems are lacking and bridge the gap between the medical needs of patients and biomedical resources.
Naomi Faulk Blog
Naomi Faulk Blog
Intro to Pulmonary Critical Care: Communication is Key
Naomi Faulk Blog

We began our first day in the Pulmonary Critical Care unit. In a small room, lined with computers side-by-side, we were introduced to some of the fellows, residents and attending doctors we would be working with for the next 6 weeks. This workspace, I noticed, is where communication from doctor to doctor happened, conversations were fast and full of information, part of me was amazed to see them in a matter of minutes, discuss several different patients and procedures without taking note or even getting confused.
Our fellow discussed a bronchoscopy that we were going to watch him do and after a brief introduction, we were ready to go. We stepped into a standard hospital size room, with a cart holding the equipment and a computer screen on one side, a portable x-ray (c-arm) with it’s screen on the other and a procedure bed in the middle, and a screen hanging above the foot of the bed. We waited for 15 minutes while the patient was being prepped for the procedure in another room, which was not what I expected. During this time, the bronchoscope technician ran back and forth from a GI procedure room to the patients’ room back to the pulmonary procedure room. He then walked the partially anesthetized patient to the room, where she was given more anesthesia and the procedure began. The tech assisted the doctor as a long, flexible scope with a digital camera on it was inserted into the patients lungs. The video was shown on the screen in front of the doctor, as shown in the picture above, while a second doctor watched the x-ray images from a screen on the other side of the room. Midway through the procedure, the doctor at the x-ray could not see the other screen displaying the scope’s camera and so the tech moved the screen, this is something I felt took time and compromised sterility, I felt it could be easily solved by adding an additional screen, or splitting the available screen. Impressively, the procedure was completed quickly almost under 30 minutes.
We watched 2 similar procedures later that day in the medical ICU where the all the same equipment was transported by cart to the patient’s bedside, I found this to be convenient for both the patient’s comfort and the doctors time. The final procedure was a tracheostomy, for a patient who had been living on a ventilator. The doctors had originally planned to perform a percutaneous endoscopic gastrostomy (PEG) at the same time, but made the “cardinal mistake of checking the patient’s history,” one doctor joked, and because the patient had a recent stomach bleed, decided against it in the best interest of the patient. The doctor did not intentionally discover this, but happened to read the patients history minutes before the PEG was scheduled.
A common theme among the doctors, residents, nurses and techs was that they were all juggling multiple engagements, quickly moving from tasks and spaces. While retentiveness, organization and a sort of balance are expected in this field, the amount of business and stress led to some confusing moments of miscommunication, which I felt could be problematic. I noticed during the first procedure, when the doctor in passing told the tech to set up for a transbronchial biopsy which he had no idea about until moments before getting the patient. This seemed like a familiar form of communication between the team, which works if the doctor happens to “catch” the tech in time (or vice versa) however if not, this leaves room for a lack in communication which can cause confusion, wasted time, and/or additional stress. I observed a small example of this during the first bronchoscopy when the doctor brought a tube for blood collection in, and because of the lack of communication with the nurse, when she arrived, she experienced confusion and even asked us what the purpose of it was. As the procedure started, the team lost a little bit of time in figuring out who’s tube was what. A similar “in the nick of time” communication happened during the last procedure, which helped me to see the familiarity in the system, and possible room for change.
The Clinics (The rest of Week 1)
Naomi Faulk Blog

Pulmonary Hypertension Clinic
Walking into the clinic is very different than walking into a hospital. At first, the rooms and hallways give a warmer vibe, I realized the beige/yellowish colors on the walls and many windows allow natural light to fill the room. Additionally the clinic is less crowded than the hospital, and decreasing patient/doctor traffic, this changed the mood completely.
We spent Thursday morning in the pulmonary hypertension clinic located in the UIC outpatient care center. We began in the fellow’s room similar to the one at the hospital; a small room, lined with computers, where the doctors overviewed patients. Unlike the hospital, the clinic operates around a certain pattern. The patient begins with the medical assistant, who takes their vitals and relays this back to the fellow (or nurse practitioner) via bulletin board, who is in the meantime reviewing the patients history and test. Then the fellow sees the patient and conducts the appointment. After the fellow has gather all information they present the case to the attending and review the patients chest exams (X-ray, CT-scan, echocardiogram, etc.) as well as diagnosis together. Finally the doctor visits the patient, checking the same things the fellow has, as well as asking similar follow up questions, and determines the plan of care with the patient.
We were given the opportunity to observe the fellow and doctor during to the appointments and I remember feeling a bit odd at first, like our presence was intrusive. However almost all of the patients were welcoming and kind, we got lots of “good luck’’’s and thank you’s (even though we were the grateful ones!). It was interesting to learn about pulmonary arterial hypertension (PAH) from so many angles of different patients. Because it is a very specific, uncommon condition, I was surprised to see so many patients at the clinic with PAH and also saddened to see that many of them dealt with several other chronic health problems in addition to that. During one visit, the doctor suspected PAH and wanted to conduct a procedure (probably a right heart catheterization) to confirm so that he could begin treatment and slow down the progressive PAH, however the patient admitted that she did not want the procedure right away, she had gone through several other surgeries that year as was overrun. Although the doctor suggested otherwise, the action of care can only go as far as the patient wants, and I realized the patients who take initiative in caring for their health are generally healthier, however as they begin to juggle more complications, it just gets harder to persist with the same amount of fervency.
Although I find the frenetic pace of the Medical ICU is more my style, the clinic was very straight forward, and allowed more patient interaction, which was a nice break.
The Sleep Clinic
Friday afternoon, we did a rotation to the Sleep clinic, which is about a 15 minute walk from the hospital. The sleep clinic resembled the previous one in structure and ambience, however it was unlike any clinical setting I have been in before. Each room had a large hotel-style bed, covered with homey blankets, monitored with a surveillance camera, an intercom, and sensors for the patients to monitor their vitals, as shown below:
(ECG, EKG, EMG, CEMG)
These rooms were used to study sleep apnea, narcolepsy, insomnia, hypersomnia, and many other sleep disorders. There are many layers to a diagnosis of a sleep disorder such as sleep apnea, I found that a big part of the doctors job is understanding what is normal for the patient and what may not be but the patient accepts as normal. Below is a sample self exam called the Epworth Sleepiness Scale, used to gage sleep abnormalities a patient may overlook when asked about “how tired” they’ve been.
While this is no where near a final diagnosis of anything, I encourage you to out yourself in the patients place or try it for fun. 0-10 is a pretty normal score, while it is higher for teenagers, high scores can mean a number of things and I would not suggest jumping to any conclusions.
Each case we followed here was different and interesting, the fellows here were great, demonstrative teachers and I really enjoyed learning about sleep medicine, I am excited to spend more time here.
Levels of Redundancies (Week 2)
Naomi Faulk Blog

In the MICU – Tuesday Morning Rounds
Walking into the MICU that morning, my first thought was that someone died, why else would there be 20 doctors, nurses and pharmacists in the hallway? This was rounds. Rounds are like this: There are two teams of maybe 5-7 residents and interns, one team worked the floor over night and therefore has all the new patients, the other team came in around 6 am to do “pre-rounds” for their patients. There are 2 fellows who oversee both teams and an attending doctor who is scheduled to lead rounds that week. There is also a couple of pharmD students with their leading pharmacist and nurses near by. Everyone is holding a packet of information on all the patients and their vitals. The whole group moves together from door to door “rounding” the floor. A resident or intern will present the patients case to the attending while others listen and take notes, the attending then sort of quizzes the group on what they think should be done, and everyone sort of puts their medical knowledge together to create a plan of action, kind of like a Grey’s Anatomy episode. Then the attending and as many of the residents that can fit, go into the room, check the patient again, and update the patient of their health and decide how to move forward moving forward.
Rounds; part of the team is in the patient’s room at this point
This takes about 2 hours for the entire floor. The last half hour, everyone meets in the fellow’s room (no there are not enough chairs or space for everyone) and goes over every patient again, this time looking at x-rays, CT-scans and other tests. After this the doctor leaves, the teams split up and again review patients and their next steps (updating dosages, planning procedures/surgeries, etc.)
The “fellow’s room” – after rounds
To me, rounds were the coolest thing. Even though I spent most of the morning trying to decode their medical jargon, which sounded like a completely different language, I admired the way each member of the team came together, using their background to help the patient. It was like watching some kind of sports’ game, each part of the team needed each other; the residents needed the nurses, who only have about 1 or 2 patients, to understand each patient’s condition and then worked with the attending to come up with a plan, helping him see every patient faster, while the pharmacists assisted with drugs and dosage decisions, as well as giving important information on their side effects. Finally the nurses were updated on patient treatment and pulled the show together. Every patient felt like a mystery and every solution a miracle.
Many parts of the round process felt repetitive, like the attending and residents asking the same questions, or the team reviewing the same person for the 3rd time, but the attending, Dr. Dudek, explained it like this, “There are multiple levels of redundancies which we need.” Going over and over the patients is the only way the doctors can be sure they aren’t missing anything and is a seemingly extensive but necessary process to prevent error.
One question bothered me, why do rounds at 8 am?
Rounds begin when the doctor arrives at 8am, therefore the interns must be there at 6:30 am to do pre-rounds, meaning the nurses and technician have to start checking vitals and run test at 4:30am to be ready for the residents. This means that not only are patients disturbed by the constant MICU alarms, they are also woken up in the middle of the night for these tests and again in the early morning for the doctor. This causes the patients agitation and stress, and overall loss of sleep, which effects even a healthy person. So why rounds at 8 am? It’s because making interns work longer than 28 hour shifts is illegal, and since the overnight team arrived the day before at 6:30am for the pre-rounds, legally they have to leave at 11am the next morning. Our readings have been focused on teaching us to design things “user-centered”. When I apply this to the hospital, or more specifically the MICU, I think we can make them “user-centered” by scheduling rounds considering the patients. Here is an area I think should be looked at systematically, along with the loud noises and constant MICU alarms, to be revised which has potential to benefit the patients experience and health tremendously.
What Everyone hates…
Naomi Faulk Blog
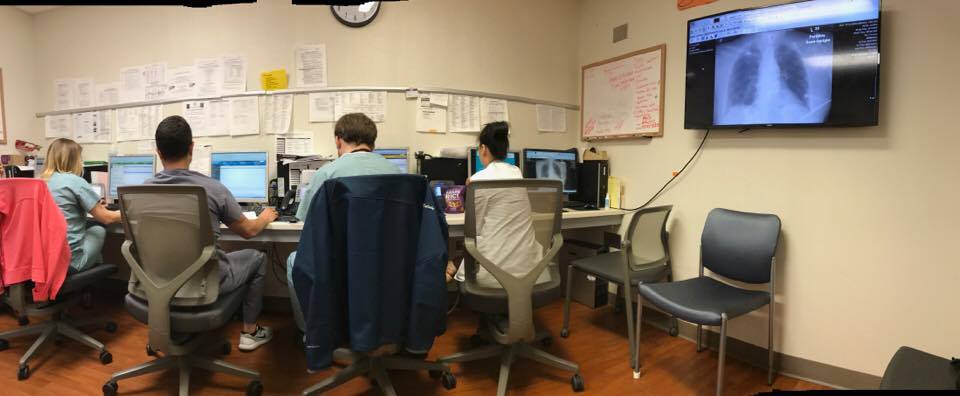
Paper Work
- Medical scribes are people hired to transcribe the patients information for the physician, giving them more time. Medical scribes can be an extra expense that a hospital/clinic cannot afford.
- Speech recognition software such as Dragon will type as the physician speaks. However this software is commonly mistaken and fixing error can be just as time consuming as with out the program
Naomi Faulk Blog
This Tuesday’s rounds in the MICU ended early which gave us a chance to sit down with the residents and hear about the hospital from their perspective. I realized that this was an unique opportunity to kind of address the problems they run into daily, after all they have been in the hospital much longer than we and are part of the users that we are designing for. With a few simple questions, we began an informal group interview and by the end of it my notepad was full of complaints and criticisms.
Here are some of the major things we were hearing:
- Large medical devices are being stored in the ICU hallways. They feel this makes the ICU clustered and compromises the device’s sterility while there are better rooms they feel they should be stored in.
- MICU Delirium. This is a serious disturbance in mental abilities that results in confused thinking and reduced awareness of their environment (Mayo Clinic) and causes stress on the patients as well as the staff, making it harder to care for the and can (should be) minimized.
- Cerner. This is the system that the hospital uses for all things electronic, there were many complaints about it, including the new 12-character password which took up time when logging in.
- Missing supplies. There are floor-specific supplies for each unit, however when a patient from one unit is being treated on a different floor, physicians are supposed to retrieve supplies from the patient’s original floor. However, because of time and convenience many doctors will just take supplies from the floor their on which causes a shortage of supplies for that unit.
- More computer space. Things (paperwork) could go a lot faster if residents had two computer screens or a larger screen where they could have two windows up at the same time
During these conversations I found myself feeling overwhelmed by the systematic hospital issues. It was hard to narrow in on something we can actually help with, all of these problems felt out of my reach. Consequently, I began to move away from looking at the giant system of problems and go back to our observations. Although the residents, hospital staff and other “users” have a string of complaints, sometimes it’s the details that go unnoticed or are overlooked, that cause the issues they see.
Because of the advancement of technology as well as the societal, cultural and environmental changes over the years, sometimes the way things have been is no longer the most efficient way to do things. These past few weeks I recognize the nature of teaching from student to intern to resident to fellow and to attending is to follow and mimic techniques, habits, etc., exactly as they’re taught. For this reason, I feel extremely lucky to have such an opportunity, where I am able to come in, without a medical background, and replace various “that’s just how it is” with procedural questions.
A Teaching Institution – Week 3 Wrap Up
Naomi Faulk Blog
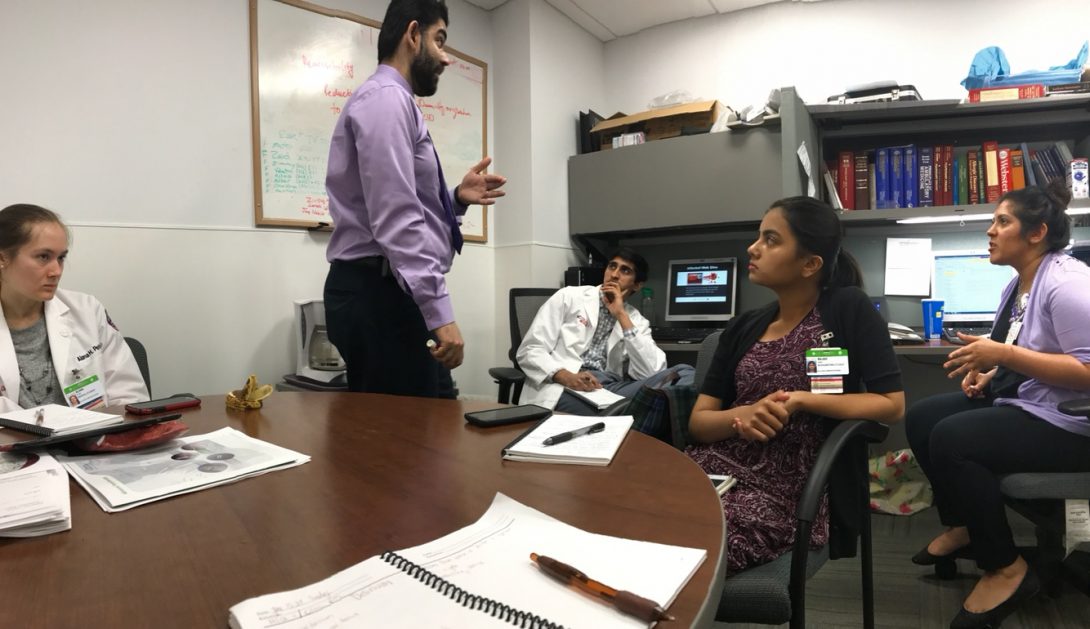
Going into the clinic makes me nervous. There’s nothing particular about that clinic or its doctors as it is seeing patients. Every time we walk into a patients room, the doctor opens the door first and says something like “I have some students who are here to learn is it ok for them to join us?” and I cringe hoping they say yes but also hoping that they’d feel comfortable enough to say no. My nerves are completely unsupported since every time each patient has responded yes, often times they respond with an, of course!
At the sleep clinic on Friday, after observing last Friday, one of the fellows had us split into groups and actually ask the patients about their medical history and symptoms alone, to then give him a sort of debrief to make the appointments faster. I was so anxious, observing appointments was one thing but actually interacting with the patients was a lot of pressure. I was worried I’d forget what to ask, or respond in the wrong way, making a patient feel uncomfortable. I also worried that a patient would question who I was and why I was there, I had already stumbled into awkward explanations of why a bioengineer was in the hospital and didn’t want that to effect their responses. However, to my surprise the patients were all very welcoming to my questions and besides a patient who refused to see anyone but the doctor because she had been waiting for so long, the other group had the same experience. Here I realized the value of this opportunity being in a university setting instead of a private practice. From the first day, almost everyone we’ve met has taught us something, many doctors go out of their way to draw us diagrams, teach us equations and even interact with the patients to put ourselves in their shoes. Last week the doctor had us listen to a patient’s breathing to allow us to see the process he goes through when diagnosing, this worried me again since I had never held a stethoscope before and I wondered if the patient would mind, but he was so supportive of us learning that he too encouraged us.
“This is a teaching institution,” we constantly hear in the hospital, “Everyone has to start somewhere.”
Overall, this week flew bye, I cannot believe we are more than half way through the program and are supposed to be designing something. This experience has become way more hands on than I ever expected, and I am so thankful for all the doctors, residents, nurses, technicians and patients who helped cultivate this experience. The teaching I’ve observed in the hospital (not just to us, but also doctor to fellow to resident to student) creates a beautiful environment unique to what I’ve experienced in school or at work, it’s challenging (since you can get questioned on anything at anytime) but motivating and makes me excited to join the medical process.
What’s an EBUS and my thoughts (Week 4)
Naomi Faulk Blog
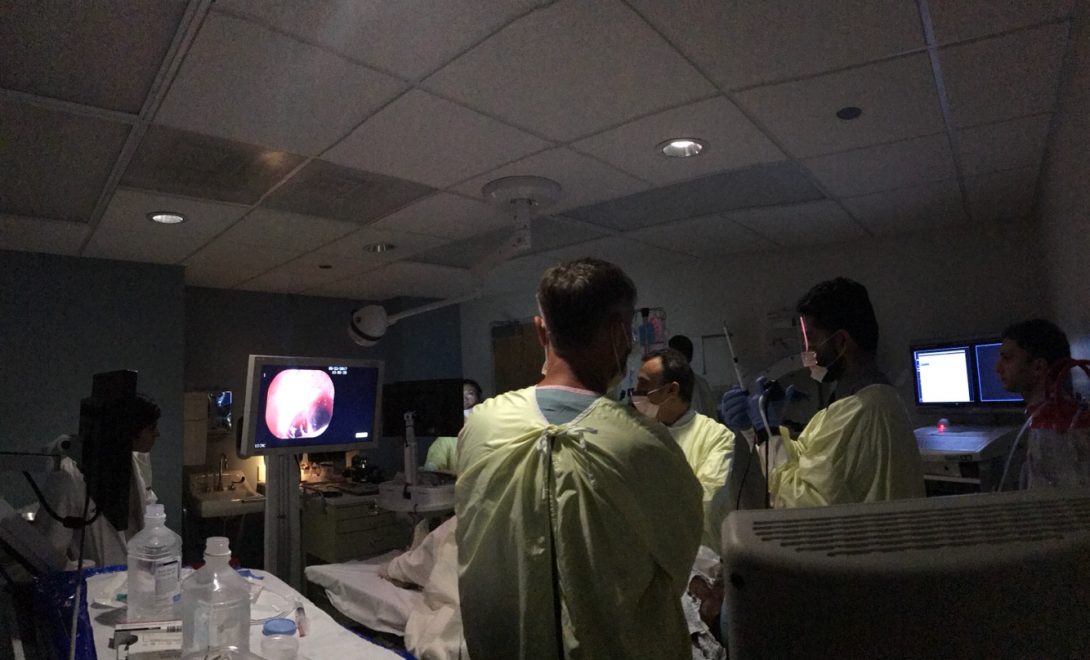
Yesterday we observed an Endobronchial Ultrasound (EBUS) for the first time. The process was very similar to the many bronchoscopies and transbronchial biopsies we’ve seen but slightly different mostly because of the ultrasound and needle aspiration.
An EBUS procedure allows the doctor to insert a needle into the lungs, or in this case a mass in the lungs, guided by an ultrasound to collect fluid/tissue samples for biopsy. This was so cool to me because conventionally a doctor would have to make an incision to biopsy which could take weeks to get back from the lab, however with the EBUS scope and in-room pathologist, there is no need to cut because it goes through the bronchoscope and in the mouth, and the doctor can see a real time image of the lungs or mass accompanied by an ultrasound, allowing the pathologist to evaluate them immediately, requesting any additional samples right then and there. The safer, quicker and superior technology of EBUS over mediastinoscopy (conventional diagnostic surgery requiring an incision above the neck to access the chest) motivates me to look at current invasive procedures and surgeries and think, is there a future for surgeries that won’t need stitches or leave scars?
Just like in the previous procedures, the patient was moderately sedated with lidocaine. Although at the start of this particular EBUS the doctors realized the patient was actually not sedated enough and so they stopped (after starting) and gave him more drugs. I think having an anesthesiologist during the procedure could have helped to prevent this but since this was a minor delay and is the only instance we’ve witnessed out of many other ok anesthetizing, I can see why one is not a requirement.
In a small procedure room (same room for the bronchoscopies) we fit a technician and his cart, a nurse and her cart, 4 doctors (a pathologist and her cart, 2 fellows and their attending), and 5 observers (us plus a medical student) along with all the machines and instruments in the room a you can kind of see in the picture below:
Here are some needs noticed during the procedure:
- Ways to allow the doctor to see both the screen of the ultrasound and the bronchoscope camera’s screen. Similar to the problem during the transbronchial biopsy (when the physician could not see both the x-ray and bronchoscope screens and consequently had to move them during the procedure), it was impossible for the the fellow to see both screen and when looking at the EBUS screen, had to turn his head completely making it hard to coordinate the bronchoscope in his hand simultaneously.
- A bronchoscope controller with more than 1 axis of rotation. Below is a picture (found on the internet) of the bronchoscope controller that the doctors use, it allows them to curl the scope up/forward or down/backward (green arrow), however is the doctor wanted to turn to the left or right (red arrow) to see maybe a mass on the left lung wall, then he would have to turn his entire arm in an awkward and slightly difficult manner. vs I think a video game controller style stick would not only give them an easy access because of the two axis but it would also be more familiar.
- A way or system to determine patient sedation or discomfort for minor procedures that don’t require an anesthesiologist .
- Design a better structure for the space (or a new and larger room completely) to fit all machines while allow all persons access to the patient and see the screens for educational purposes as well.
- This:
The state of Delirium
Naomi Faulk Blog

This week ended much slower than the others, leaving us with more downtime that we choose to use investigating the MICU. While I love observing procedures, I found these times to also be very beneficial. We had time to discuss problems and questions with different residents and fellows, and one of the things we began to focus on was delirium.
My hospital exposure before this program is very limited so I had no background knowledge of the medical term delirium. The residents explained to us that in the MICU patients who stayed for more than a day were at risk to becoming extremely confused because they would loose track of time and consciousness, this was especially the case the longer they stayed, they called this delirium.
A quick google search explains delirium as a medical term for patients who enter a severe state of confusion due to temporary brain failure. About 2 out of every 3 patients who come into the ICU will develop delirium and this percentage is higher for older patients, patients on benzodiazepines or breathing tubes. I also learned that there are many small interventions that seem to make a big impact in preventing delirium such as regulating the patients sleep/wake cycles and re-orientating the patients with family member/friend contact or even pictures. These seemed like easy and low cost solutions to a problem that not puts stress on the nurses and doctors, but increases the length of stay in the ICU, costing the hospital more money and decreasing the patients overall health, comfort and chances of survival. Which begs the question, why haven’t any of these solutions been implemented?
Looking back at my observations of the MICU, this problem made a lot of sense. There are constant noises and alarms going off in and out of the patients room and hallways and almost all of the rooms are open, in fact many of the patients doors are glass. While delirium sound like a quick fix by simply avoiding disturbance to the patients sleep at night, with alarms that are needed to alert the nurses, vitals at 4am and medical supervision, how could they prioritize the patients sleep over their medical care?
“Scrubbing in”
Naomi Faulk Blog
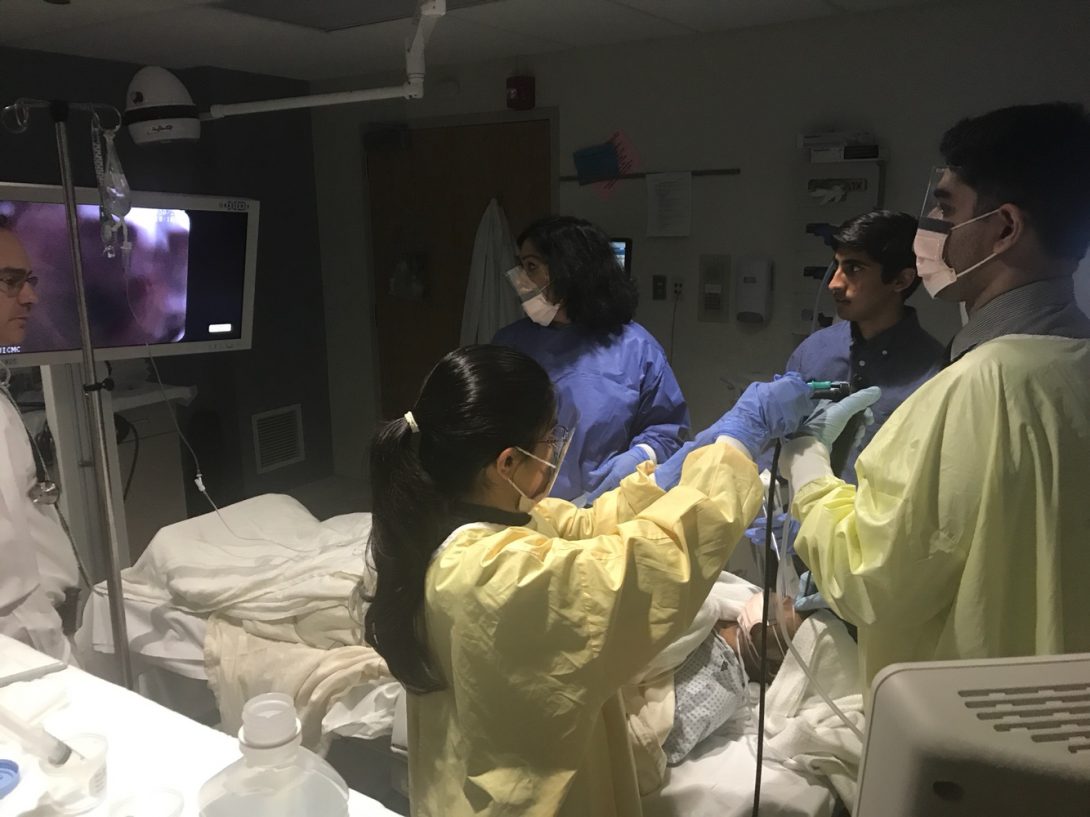
Not actually, but when the doctor asked if one of us could assist with a bronchoscopy on Friday, we felt like an intern from Grey’s Anatomy being offered the chance to “scrub in”.
On Friday two BAL Bronchoscopies were scheduled, however the primary bronchoscopy technician was gone for the holiday weekend. Because we’ve seen so many of these procedures done and were already going to be in the room, the doctor offered us the chance to assist in the place of the technician. While our assistance wasn’t as substantial as our excitement would lead you to believe, we the chance to work with the doctors as a team. I realized that as a bioengineer this was truly an amazing opportunity, we would never in our career get this close to the usage of the technology we design while interacting with not just the patients but the physicians, who are the users.
This was definitely one of the more exciting days, even looking back at my note book I did not write much down given all that was going on we didn’t get the chance too, luckily my colleagues and I got some great photos out of it.
Najah and Aakash getting ready for the first bronchoscopy! Najah preparing the Lidocaine to inject into the bronchoscope!
Hopes & Fears: The End
Naomi Faulk Blog
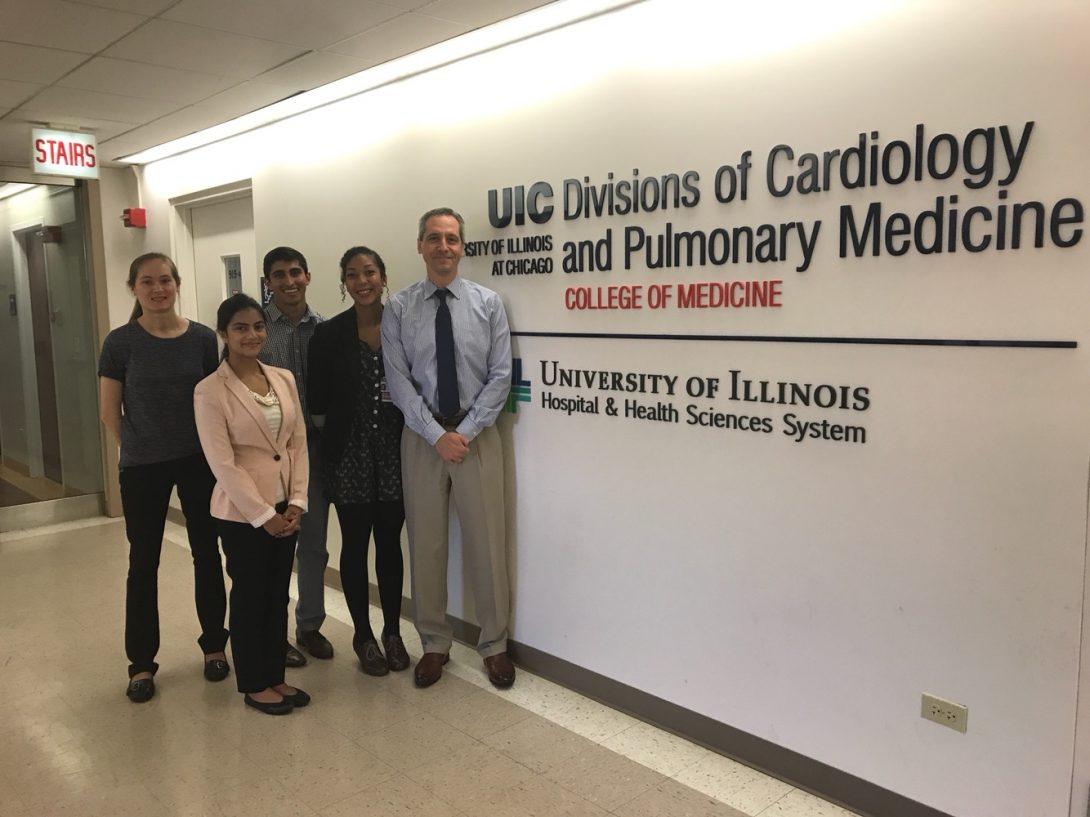
I’d like to begin this final blog thanking my clinical mentor Dr. Steven Dudek and the many other doctors from the pulmonary and sleep units, who took time during many difficult, busy days and procedures to teach us. You have given us an incredible opportunity to not only observe what you do but also to understand why and experience medical technology and the hospital systems as you do. I’d also like to thank those of you reading now, who have journeyed with me from not knowing what a bronchoscopy even was to assisting in one.
My understanding of both general health care and specific pulmonary challenges has grown so much in such a little time and as this program comes to an end, my hope is that my pursuit of the problems would not end here. My team and I plan to incorporate some of our solutions with involved faculty into research trials at the hospital and clinic. We hope to continue to learn about the problems at hand and continue to work together to solve them. Because I have seen the many problems doctors and hospitals have to deal with, I fear that our project won’t receive necessary funding or priority to move forward. But I will continue to hope that this program, my experience and these blogs will carry on to be a small part of a bigger solution.
Benjamin Follman

Benjamin Follman
Benjamin Follman Blog
Benjamin Follman Blog
Week 1 – Clinic
Benjamin Follman Blog
At times, the clinic ran like a well-oiled machine, and everyone moved around in an organized chaos in which my role was to not get in anyone’s way. Although I felt a bit like a protagonist in a Camus novel, I made numerous observations of potential areas of improvement. The clinic frequently acted like an assembly line – operating as efficiently as it could within limits set by forces not directly in control of the health care team. Nonetheless, those parameters provide opportunities for improvement.
Unpredictable patient visit lengths and patient no-show rates resulted in both long wait times for some patients while at other times, doctors and nurses would be waiting for extended periods of time for other patients to show up. I wondered if this dichotomy could be at least partially resolved by scheduling based on estimated length of the visit and whether a given patient had a history of late appointments.
Another limiting factor to time efficiency was in communication and administrative. A surprising number of patients did not know they had been scheduled for a test while others required a follow up with another provider which for one reason or another did not occur. These types of errors result in inefficiency consuming the time of both the patients and the providers, but more importantly can have effects on patient outcomes.
I also observed cystoscopy which appeared to be uncomfortable to the patient. As the cystoscopy went on, I questioned the necessity of the relatively large radius of the scope. Cameras have been getting significantly smaller while also having better resolution. If this technology could be implemented in cystoscopes the way it has been in phones, it could be done faster with less discomfort. There would be other challenges in this such as irrigation and lighting, but I also have sketched some ideas on how those could be handled and improved as well.
Week 1 – Operating Room
Benjamin Follman Blog
I tried to focus my observations in the OR similar to the clinic – by focusing on inefficiencies. One of the main things which was very readily apparent was the extensive layout of equipment which seemed to be precisely placed in order to get everything to the surgeons as soon as they ask for it. Nonetheless, there was still not always the correct equipment present. I tried to get an idea of what type of equipment was used and look for opportunities for consolidation of equipment. Unfortunately, my limited knowledge base prevents me from identifying and appreciating nuances that might make the difference between something being extraneous or not extraneous. The issue of having the correct equipment was handled very well at the University hospital’s OR where the nurse and OR technician had access to an equipment list not just by procedure but which attending physician would be performing it, thereby allowing the list to be catered to which attending surgeon was operating.
The preparation for surgery took as long as some of the procedures themselves. It is very clear how the healthcare sector of the economy has fallen victim to Baumol’s cost disease, as it would seem that productivity is not just limited to the time of the surgery itself but also by how quickly tasks like laying out instruments and preparing the operating room for the next patient take. There were many large machines that were being moved in and out. For example, the lithotripter was moved into the room and back out of the room, and there were discussions involving how to schedule patients based on when the machine was available.
There were also significant ergonomic issues as taped sheets were being used as arm rests during microsurgery. Adjusting the equipment to fit the needs of the case and the surgical team was a fairly time consuming and cumbersome process. As previously mentioned, these preparatory measures were rate-limiting, so to speak, in the operating room. A lot of time was spent trying to adjust the operating area to account for the height differences, lighting, ensuring all of the monitors could be seen by the people who need to see them, etc.
Week 2 – Clinic
Benjamin Follman Blog
The clinic once again was significantly limited by language barriers. Patient-doctor interactions take place through a translator and therefore are twice as long as the conversation needs to happen twice, once in each language. Furthermore, the accuracy of the translator becomes vital in this scenario, as frequently the doctor is discussing life changing operations with the patient through this translator. For example, what type of penis implant would be given for erectile dysfunction or the different options a patient would have after a bladder removal.
After a discussion with Dr. Niederberger, I tried to refocus my efforts towards identifying problems as identifying solutions. Although it is part of my nature to view things through the lens of, “if this could be done this other way,” I was consciously making an effort from this point on to view things with the perspective of “what problems exist.” Frequent problems I overheard in the clinic involved logistics, especially regarding patient transportation and scheduling. Also, one or two sperm samples from patients were often insufficient to understand why infertility problems were present.
One of the doctors, after being informed of what I was present for, was quick to offer suggestions. The first one being the orchometer (pictured) was an archaic and inaccurate way to determine the size of a testicle. He also suggested he wished the ultrasound machine could be as portable as the orchometer. However, the clinic generally did not have many issues regarding a lack of equipment in the proper places.
Week 3
Benjamin Follman Blog

On Monday the Urology team discussed many of the areas for potential improvement as a team, focusing in on patient education and compliance. The Urology team also began to formulate ideas for problem statements. A radical cystectomy was observed in the operating room in which a part of the ileum was fashioned into a pseudo-bladder of sorts.
OR room turnover and patient prep remained as time consuming tasks. Surgery start times were often delayed for one reason or another, and height differences between the attending, resident, OR tech and nurses continued to prove challenging. Some of the surgeries took 4-5 hours to complete and ensuring the comfort of the surgical team may help an operation move more smoothly, although it can be difficult in long procedures.
Further issues with translating services were observed. A sign language interpreter was needed, and therefore was unable to be reached via phone. Another issue was that American Sign Language does not have the same diction and syntax of spoken English. Therefore, trying to communicate via typing on a computer screen proved to be futile, and the patient was rescheduled with a note that a physical translator would be needed.
Due to some ideas that were already being pondered by the urology team, a patient education group was also set up to address some of the issues that had been observed. It has been very productive up to this point, and hopefully will be able to address some of the needs witnessed over the past few weeks independent of the clinical immersion program.
Week 4 Part 1
Benjamin Follman Blog
This week the observer witnessed more examples of scheduling inefficiencies where half of the morning patients did not show up while in the afternoon every patient showed up leading to long wait times. Furthermore, the afternoon was booked with a large number of new patients with significantly longer visit times. The most common cause of extended appointment visits remained translation which remained a challenge in time, comprehension, and accuracy. One doctor commented, “I need a translator for the translator.” Furthermore, there were many examples of issues of transferring patient and lab data between providers. In one instance, a patient was referred due to abnormal blood work, and when the provider faxed over the patient’s chart, they left out the bloodwork which led to the referral.
Dr. Garvey mentioned interstitial cystitis for which very few patients were familiar, but were frequently referred for. Many patients are incorrectly being referred for cases of prostatitis by other physicians for cases of interstitial cystitis.
There were also further examples of language barriers as a patient who could only speak mandarin was given a copy of the International Prostate Symptom Score, a likert scale used to assess symptoms that could be related to the prostate, while being unable to read it.
The Operating Room continued to be an area for potential improvement, as people were frequently cramped while little vertical space was being employed.
Since patient compliance has continued to be a potential area for improvement, one of the projects identified as a potential need to be addressed was the voiding diary, due to its low compliance rate. Shana took great initiative and developed a very good and redesigned voiding diary for use in the clinic making it simpler with a larger format.
The observer has also begun working on an independent project which he is choosing not to disclose for reasons of potential intellectual property.
Nicholas Green

Rising Senior in Bioengineering. Concentration Area is Cell and Tissue.
Nicholas Green Blog
Nicholas Green Blog
The First of Many!
Nicholas Green Blog
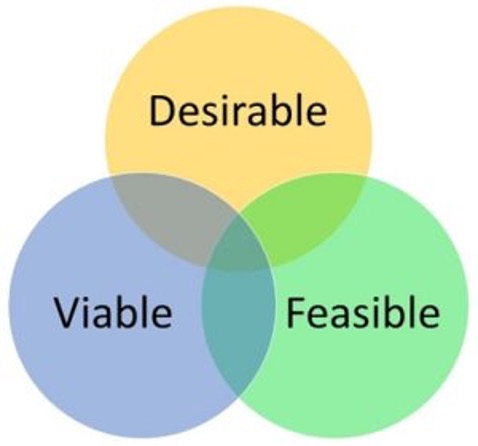
It has only been two days and I already feel like I’ve been exposed to so much! I’m not sure about the other participants, but this is my first time working in a clinical setting and it is completely different than anything I have ever been a part of. Well before I get too deep into that portion of the experience I should talk about the Tuesday workshop.
The first half of Tuesday was all about Human-Centered Design. This means creating a device that is desirable, feasible, and viable because if any of these three components are missing the device won’t make it into being anything more than a concept. If no one wants the device you have no market, if the device is impossible to create it doesn’t matter how great of an idea it is, and if the device doesn’t have a purpose it will never go into creation. The main thing that we discussed that ties into these ideas is that every user will have different ways of defining those three criterion and will have different needs. By using Human-Centered Design practices you are able to work with people who will actually be using this device in real world situations and their feedback is crucial to making an effective device. The various clinicians that you have testing the device also provides a way to identify usability and issues earlier in the process so they can be addressed before the device goes into real world applications.
Then Wednesday came around and showed me a whole new way of seeing and thinking about clinical issues. Sure you can read a textbook and theoretically solve given problems, but are you able to go into an operating room and observe things that can be improved? Are you able to think about the layout of a room, the devices that are being used, and the employees and how they are working in the space? These were all things that were noticed or brought up between the two operations I observed and speaking with our mentor Dr. Nishioka! I am really excited to continue to make observations and discuss ideas as this program continues!
The Da Vinci Code
Nicholas Green Blog

Thursday and Friday were really intense days! After morning meetings we started viewing at 7am in the pre-op area and most of the start surgeries begin at 7:30am. The clinicians, nurses especially, were SO BUSY but it didn’t phase them at all! A big focus so far has not only been the technology side of engineering but also processes and how just improving those can drastically improve the efficiency and effectiveness of a unit.
When talking to the clinicians it seems that one of the issues is making sure people are in the right place at the right time. Examples of this could be the patient being late or the various clinicians being delayed from their previous patient. Most of the clinicians all pointed to this being one of the most challenging aspects of operating room efficiency and wondered potential ways technology could be used to cut down on these issues. While we were still thinking over different options we were moved into the next phase of the day: being in an operating room and observing the technology being used and the way the space is set up.
Now for me this was completely different from anything I had seen. Between Thursday and Friday three of the surgeries I observed used a Da Vinci surgical machine. This basically puts the surgeon in a position where he is controlling robotic arms to perform surgeries while a few other clinicians are near the body to provide different viewing angles and support as necessary. This for me has been one of the craziest things to wrap my mind around! When you think about how far technology has come in the medical field there may not be a better example than this machine and all of the different capabilities it has. It has attachments to cauterize, grab, cut, clip, and on top of all of that it takes video for everyone to see whats going on!
This is what made my first week with the Anesthesiology department so amazing! I get to see the anesthesiology aspect of prepping for surgery and being there with the patient every step of the way, and all of the technology on that side such as the monitoring devices and infusion pumps, but I also get to see the surgical side of things. So far the technology has been a little overwhelming as I am moving into things that I have never seen before, but the opportunity to work with these amazing clinicians who are always willing to answer questions has really made this an enjoyable and educational experience so far!
What is Your Perfect Day, the Art of an Interview
Nicholas Green Blog

Our second week started off with presentations from each group in the program. It was really interesting to be able to compare what our mentor has us do on a daily basis compared to what other groups do. After the presentations we had a short lecture and the thing that stuck out from it to me was how important the questions asked are in an interview. All of the different aspects that go into making the other person feel comfortable and not biasing their response. We then went through an exercise that not only allowed us to practice our interviewing skills, but also to learn more about the people in this program. The interview was based around what your perfect day would be and everyone prepared their own questions for their partner. The main thing I learned from this is that responses then lead to further questions. I started the interview with four questions but then by the end had about twelve things answered. This can only happen if you go in with an open mind and allow the interviewee to be comfortable.
This experience has already been useful for me in the two days since. Last week I was still feeling sort of out of place and thought that if I asked a question I would be distracting the clinicians. The workshop Monday also brought up how important timing of questions is. I used these skills to talk to five clinicians about a few different topics ranging from the current educational system for doctors to the operation of the Da Vinci machine. Gaining different perspectives on these topics really allows me to see things in multiple ways and adjust my thinking. For example when talking about the medical education system I have only seen it from the perspective of family members, all of whom are still in medical school. The clinicians who I talked to have actually experienced whether or not the different exams, courses, and rotations really are helpful when it comes to actually practicing medicine. One person felt that there was an unnecessary amount of standardized tests while someone else felt that is the only way to truly test if people are studying all of the topics. One thing that everyone seemed to agree on is that the introduction of humanities on the MCAT is beneficial to the medical system. Although knowledge is extremely important, being able to communicate and interact with people is also very important to treating a patient. This really tied the first three days of this week together. It goes back to making the other person comfortable and allowing them to open up and accept that you really do have their best interests in mind.
Airway Emergency
Nicholas Green Blog
Thursday started out with being introduced to the emergency airway bag. We saw the evolution from what looked like a fishing tackle box to the current bag model. This change is a project under one of the residents as a way to make carrying the bag around easier and making it easier to get to the emergent equipment faster to help the patient as quickly as possible. We then went to see the actual bag instead of just pictures and see if there were any changes we thought would be beneficial with fresh eyes. To see all of that life saving equipment in one bag was almost hard to believe and it made me see why you want it to be as convenient and mobile as possible. A couple hours later we got a call from the resident in charge of the bag that there was an urgent airway situation in the ED. We hurried down to see the bag in action and saw how quick the resident was able to access the tools necessary to visualize and open the airway, one point airway bag!
Friday was all about patient transport. We followed a patient from ICU to OR and back to ICU to observe the whole process. Once transported from the ICU they have to switch the patient to an OR bed due to different features between them and the ICU beds. This includes switching out some equipment and tubing for the patient that can cause a slight delay, but the clinicians handle it all with precision. While in the OR the nurses were asking us why bioengineering students are in these operating rooms (something that has happened often so far in this program). When we told them about observing to see about possible improvements they had tons of ideas! It came to the point where one of them said that if we get rich using these ideas we better not forget who told them to us!
To finish off Friday we got to watch a double nerve block before surgery. As someone who has zero anatomy background it was truly amazing to watch the doctor be able to recognize the difference between all of the inner workings of the human body simply using an ultrasound machine. The patient was very grateful for what the doctors were doing and it was a great way to end the week seeing a procedure for the first time.
The Connection
Nicholas Green Blog

As you might expect there has been a lot of, “Why are there bioengineering students in the OR?” through these first 3 weeks. This week has been a little bit different so far. On Tuesday we were observing the Interventional Radiology portion of anesthesiology. While we were in this area we met a PhD Bioengineer who was working the nuclear medicine portion of a procedure. It was very interesting to talk to her and learn the path that she took from getting an industrial engineering degree in a foreign country to coming here and getting a PhD in bioengineering, and then getting a certification to be able to do actual procedures with nuclear medicine. We were conversing about the possibilities in the field before moving to the next portion of the day, but it was a completely different experience than anything from the first two weeks.
An interesting topic that has popped up throughout this week is off-site anesthesia. While the first two weeks we were only exposed to OR operations, we have spent a lot of time this week on different units observing the anesthesia. It is a very different dynamic as the anesthesia equipment very much seems like an afterthought in these rooms. This was a common issue that has arisen while off-site, the anesthesiologist has a very difficult job to be able to both control the anesthesia machine and do their patient work (IV’s, tubes, etc.) due to the way the rooms are set up. There was a point where the anesthesiologist in one of the rooms had to climb over the wires and tubes, through an x-ray machine opening (it was off), and then get over to the other side to adjust something on the patient.
Today (Thursday 6/15) we got to visit another off site location, OB. While we didn’t see any cases due to it being a slow day, there was still a lot to observe in this area. One thing that was brought up was how they have the Omnicell (medication releasing machine) right in the operating room. This added a layer of convenience not only for the clinicians, but also for the patient as it allows medication to be accessed instantly for faster administration. An idea that was brought up with these is self-administering Omnicells as a way to increase speed and convenience further, while also eliminating the chance of controlled substances being taken out when unnecessary.
As a final note, for me it has gotten to the point where I feel like I know what is going on and who most of the people are! Since we are getting into the middle of the program it feels like everything is starting to come together!
Another Day, Another Department
Nicholas Green Blog
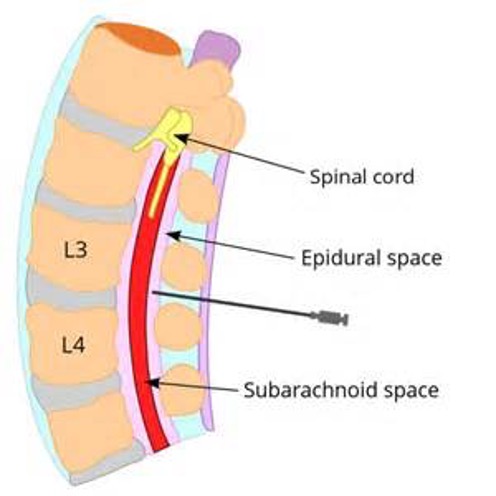
Most of Friday was spent on the OB unit focusing on the anesthesia side of things. To start the day we were introduced to a new attending and resident before we had a morning meeting. The attending gave us an article that was related to one of the patients for the day as a way to understand the different nuances that different patients can bring to the table. It is truly amazing to see all of the different things that go through the doctor’s mind while they are deciding what treatment path to take with each individual patient.
Once we got back up to the unit we spent the rest of the day watching two procedures. The first wasn’t much different than others that I had seen in the OR setting, except that they didn’t want to do a complete sleep anesthesia. The goal was to just get moderate sedation so that the patient would be breathing on their own, but wouldn’t feel any pain of the procedure. The attending told us that this might be the most difficult type of anesthesia because it is a very fine line between awake, moderate sedation, and completely out. After the procedure was over we went to see a brand new procedure!
The new procedure was an epidural for a pregnant patient! It was a completely different type of anesthesia as the point isn’t actually to sedate the patient, just to set a numbness level for comfort. The concept is to get into the correct layer, but you can’t go too far or too short. The clinicians were very careful to make sure they hit the perfect spot, even asking the patient if she could tell them whether it felt like they were in the center of her back. It was amazing to see the change in comfort for the patient from the time they started the procedure until it was over. One observation I made was how helpful it would be for the patient and clinicians if there was a better way to find that perfect spot as it took a little while due to the caution being taken.
Overall it was another amazing and educating day/week! I can’t believe we are more than halfway done… where has the time gone!
Brainstorms are in the Forecast
Nicholas Green Blog

Monday’s session was all about brainstorming from our 3 topics for needs statements down to 1 topic for the final presentation. Right away we were able to narrow our choices down to 2 that we felt were the most feasible. We did a brief wordstorm to generate some ideas around those statements and brought this into a meeting on Tuesday with Dr. Nishioka. We met and discussed the ideas for about an hour and were able to narrow it down to one topic, but I’m not spilling that here! You’ll just have to keep tuning in to see!
Tuesday was also my first experience with a pediatric case. This showed me two things, first, I am very fortunate to have had a very healthy life growing up, and second, while these kids aren’t that lucky they do have all of these physicians who are working extremely hard to try and give them as normal a life as possible. To me this is one of the most noble jobs imaginable and has to be extremely draining to work with everyday. This experience was completely different than seeing any of the other procedures to this point.
What I didn’t mention is that Tuesday was actually the longest day we have worked in the hospital (hours wise) but seemed to go by the fastest between our brainstorming and the pediatric procedure. Overall, it was the day that to this point has been the most memorable.
Wednesday had a lot to live up to, and while it may not have been as memorable as Tuesday it still brought a lot to the experience table. We started the day by listening to a conference about the topic of staggering surgeries, which is currently a very hot topic in healthcare. The issue being that attending physicians need to be in the OR during critical portions of the procedure, but these portions are not defined which can lead to issues for the attending.
After this we saw one procedure with a quick break for lunch. Before leaving for the day we did a little more brainstorming so that going into the homestretch of this program we have a strong foundation for the project. We are really looking forward to putting together the final ideation to build the paper and presentation together!
Here is to a strong end to this week, and a deeper appreciation that has stemmed from it!
The Supply Chain
Nicholas Green Blog

The end of the week was very different from anything else we have done to this point. Thursday was a slow day in the OR but we did get to talk to some of the residents about everything from our program to their plans for the future. It was a big end of the week because Friday was the day that the PGY4s graduated. They were talking about the different hospitals they were going to begin working with and for some the fellowships that they would be joining. They were all excited to be moving on to their new endeavors and into the next step of being a doctor.
Then we had a crazy day on Friday, starting off by going to visit Central Sterile in the basement of the hospital. In just the hour and a half we were there they told us we were in both the cleanest and dirtiest rooms in the entire hospital. We got to see everything from the dirty used trays coming in one door to them being cleaned and sterilized before being packed to be ready for use. It was an extremely interesting opportunity as an engineering student, and truly amazing to see how much work goes on behind the scenes of the hospital. These people are taking blood covered tools and sterilizing them within 3-5 hours to be clean enough to perform another surgery! That’s CRAZY! When we got back to the anesthesiology department they were having a retirement party for one of the secretaries so we went in and talked to more of the people from the department. It was a very lively experience as it was the last day for the PGY4s and everyone seemed really happy for them.
We finished the day with some conversation about the final project for this program, how are we already working on the final project??? Time really does fly when you’re having fun!
How Did We Get Here?
Nicholas Green Blog
It seems like just yesterday we were all walking into the innovation center for the first time, new faces and faces that I had seen for up to three years. Now I know this isn’t my last blog, but this week really feels like we are winding down with the program. When I think back to the first day and meeting two new people who were going to be in my group I never would’ve thought that we would get as far as designing an actual product and hopefully finishing a prototype. In fact, I didn’t really think any of the groups would get to the point we are at now!
I had heard from the previous year of this program that they got up to needs statements and then it was pretty much over, and even though I knew it was six weeks on one unit versus being divided into two units I still didn’t think we would get this far. Just to point out a few examples: The cardiology group has a SolidWorks design of something that their mentor wants to try and implement, Ophthalmology is talking about working on software to give precise measurements of the eye, and our group (Anesthesiology) is trying to provide a better learning experience to medical students and residents while reducing the clutter in small operating fields (current rough sketch as feature image).
Now I know that there are no guarantees, but I also know that everyone who is participating in this program is very capable of taking these ideas to the next level. So as we brace for this final week, and the stress that may come with it, I just want to wish everyone the best with finishing up this program and the projects that go along with it!
We The Ducklings
Nicholas Green Blog

Amid rumors that this might be our last blog I felt that I should give a shout-out to the group that has made this such a wonderful experience! Our group consists of four students (the ducklings) and an amazing group in anesthesiology, spearheaded by Dr. Nishioka. Ever since our first day in the clinic the lady who sits at the front desk in the anesthesiology suite has called us the ducklings, for our tendency to fall into a single file line behind Dr. Nishioka. Even now if it is only one or two of us there is usually a, “There go some of the ducklings”, or “Where are the other ducklings?”
My fellow ducklings are some of the most driven people that I have ever met. No presentation goes without a group chat and dedicated time to complete, no observation is left as just an observation, and no conversation ends quickly. We have had countless times where a topic will pop up in the morning and we will discuss it during lunch, or something will happen in the afternoon and we talk outside the hospital for some time at the end of the day. The one thing that really stands out above the rest though? Well that has to be the desire to improve patient outcomes and satisfaction. We have looked at everything from scheduling to supplies to the equipment used in the ORs and the one thing we always come back to? How can this improve the outcome of the patient. To me that is the best thing about this group. No one is taking this opportunity for granted and we want to help as many people as possible.
So to my fellow ducklings, and the department that has shaped this program, I say thank you! Thank you for making this six weeks something that is truly memorable and makes me feel as though we can all definitely have an impact on the lives of others!
(Before writing this I thought we had a group picture… but I can’t find one so ducks in a row it is!!!)
The Last Hurrah
Nicholas Green Blog

I’d be lying if I said that I wasn’t thoroughly impressed with where all of the groups ended up. The final presentations were amazing! Who would’ve thought six weeks ago that people would have developed actual prototypes to solve REAL clinical issues? This internship was an awesome experience and I couldn’t thank my teammates, mentor, and the faculty who run this program enough.
I hope that each group continues to refine their ideas and that we can develop some of these amazing issues as we all enter our future endeavors. Just to have gotten to concept generation in six weeks is an amazing accomplishment and proves the talent that was in this group. So to my fellow innovators, let’s keep pushing the envelope with needs identification and providing the best care possible in the clinical setting! It was awesome to meet all of you, work with you, and more importantly learn from each of you! The main goal was to gain various perspectives in what goes into creating a valuable device and I can honestly say that I have learned something from each and every one of you!
Have a great rest of your summer and keep finding those problems!!!
Maxwell Mckeough

I am a rising senior, pursuing a bioengineering degree. I began college as a pre-med neuroscience major, but transferred to the college of engineering before Sophomore year. I was an active member in EWH for the first version of the laminar flow hood project, and am currently one of the team managers for the second version. I am also proud to be EWH’s treasurer, and look forward to doing good work with the organization going forward. I hope to go into industry after I graduate, and perhaps in the future pursue graduate work with signals processing or regenerative medicine. As a person with autism I work on professional development seminars for special education instructors on the use of technology to improve outcomes for autistic students. I have a personal fascination with workflows, and am constantly striving to improve my efficiency and efficacy. I have many hobbies (and try to engage in new activities frequently), but my most consistent interests are speculative evolution, science fiction, fantasy, strategy video and board games, walking, philosophy, and creative writing.
Maxwell Mckeough Blog
Maxwell Mckeough Blog
Blog 1 (June 1)
Maxwell Mckeough Blog

Well, a whole lot has happened in a brief period of time. We started yesterday at the Echo Lab, where we had the opportunity to learn about the hardware and software associated with ultrasound. Dr. Gans demonstrated his years of experience with some seriously impressive scan readings, and a greatly appreciated patience for our long string of questioning.
After a few hours of Q&A, we headed to lunch followed by General Cardiology rounds. We followed Dr. Stamos to different patient rooms, and had the opportunity to observe all manner of field technology and techniques employed by the hospital physicians, and to once more bombard the professionals with curiosity.
Today had us with Dr. Ardati in the Catheter Lab, where he gave us a fantastic rundown of the lab’s equipment, and some technical challenges facing the field. We also got to see some of the monitoring equipment in action, and some really gratifying technical information on its operation.
Both the Echo and Catheter labs seem to be quite technology-intensive, and I really look forward to spending some more time in them performing observations.
Blog 2 (June 4)
Maxwell Mckeough Blog
Friday was quite interesting.
We met in the morning with Dr. Wissner, who will be our mentor going forward. He was very curious about our backgrounds and hopes for the program. After a bit of discussion in his office, we headed down to the Electrophysiology lab, where he gave us a rundown of the equipment that he frequently employs; and he provided us with some information that not only did I not know, but never would have thought to think about.
Apparently the companies that provide medical technology have to send their own technicians to provide operations and logistical assistance during many procedures.
After that, we parted ways with Dr. Wissner for the day, and went to the catheterization lab with Dr. Schroff. We were able to observe two procedures, and we gathered a lot of valuable information. The staff were incredibly patient with our questions, whether we queried about impacts of new techniques to patient outcomes, or mid-operation changes to the room setup. The catheterization process is really something to observe, and we were fortunate enough to also bear witness to room preparation. Jonathon and Mauricio had the chance to scrub up, and observe from inside the operations room while Bekah and I remained in the control room making notes about control procedures and computer interfaces.
Blog 3 (June 8)
Maxwell Mckeough Blog

As you can see from the featured image (apologies for my dour expression), this week has found the team scrubbed up and inside the procedure rooms.
Tuesday saw my first time wearing the protective lead gowns in the catheter lab (and gaining a finer appreciation for those who wear them on the daily), and having the opportunity to observe a catheterization up close.
Wednesday was spent in the EP lab, viewing some seriously interesting procedures. We saw an open-incision procedure for inserting an ICD, we saw a tilt-table test, and we saw a temporary pace maker implantation. The EP lab has an awe inspiring assortment of high-tech equipment, and even with just one day of observation, it’s clear that a great deal of innovation is set to take off in the forseeable future.
Today we had the chance to follow Dr. Lazar on rounds, and meet with some of the patients whose procedures we had witnessed. Seeing recovery was quite valuable from an innovation perspective, as there seem to be myriad opportunities to improve patient’s comfort after a procedure (even if the requisite solutions are non-obvious). We also observed an ablation, and I cannot say that I have ever witnessed a more beautiful piece of software than the 3D mapping system that was employed.
Blog 4 (June 11)
Maxwell Mckeough Blog

We spent Friday in the Remote Device Monitoring clinic. We followed the attending Nurse Practitioners on their patient interactions, and had some first hand experience with the devices that monitor ICD and Pacemaker performance.
We also had a chance to see the at-home devices that transmit patient data to the clinicians, and finally got up-close-and-personal with an ICD (the implantation of which we witnessed earlier in the week).
Blog 5 (June 15)
Maxwell Mckeough Blog
Tuesday was really something special.
Doctor Lazar was performing pacemaker lead extractions, which is more complicated than it might sound on first brush. As pacemaker leads sit in the heart, they become ingrained with the surrounding tissue. If they fracture or become infected, they cannot be simply pulled out.
Instead, the clinicians get to use lasers.
The procedure goes roughly as follows: a catheter with an Ultraviolet laser on the end gets threaded into the heart, cutting through overgrown tissue and freeing the leads.
Of all the buzzwords that get engineers excited, laser is probably the biggest. It’s simultaneously great for the state of technology, and sad for us that there don’t seem to be improvements waiting to be made to the laser procedure.
Blog 6 (June 21)
Maxwell Mckeough Blog
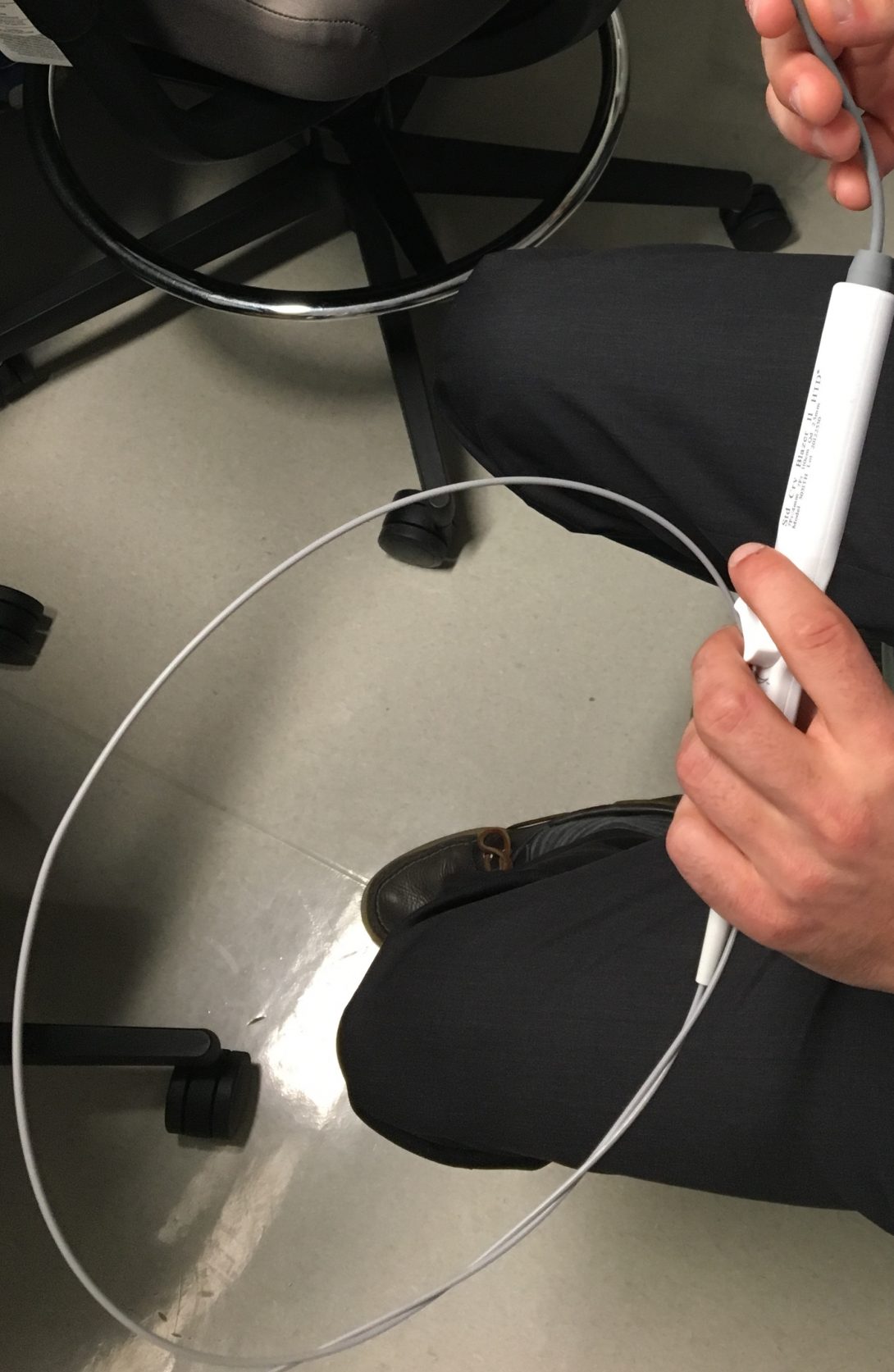
Yesterday we had the chance to observe an EP procedure we’ve seen before, but with some new perspectives.
We bore witness to a catheter ablation, although this procedure was conducted using hardware from St. Jude, rather than Boston Scientific. The differences in interface were quite noticeable, although staff seemed equally as comfortable with both. New to this viewing entirely was the chance to examine an actual catheter up close.
It’s a very neat piece of technology. Although the example we worked with was not plugged in, its mechanical functions were fairly clever. There seems to be some sort of pulley and wire system that operates from the turn dial to control the ablation tip. I can’t help but feel that, given the resistance the turn dial puts up to being operated, there’s probably a great deal of hand-strain after prolonged use.
Blog 7 (June 25)
Maxwell Mckeough Blog

Rather than a description of a days work in the clinic, I would like to treat this blog as a reflection on larger themes.
As I sit at my desk, my window is open and the sounds of Halsted street are pouring in. I just finished up the last of my work on my team’s rough draft for our final paper. It has thus far been easy to view the program day by day, analyzing data in discrete packets. The paper forced me to consider the whole of the experience in aggregate.
For all the different procedures, clinicians, patients, and circumstances, we keep returning to several central themes. Common problems or observations, things that pervade the whole of the clinical experience. Underlying all of these though, I am struck by the idea of constraint.
There’s a trap I think that all bioengineering students can easily fall into: the idea that the clinic is perfect. Every idea we have can be implemented. Every item is used to it’s full capacity. Every clinician is not a human being, but a flawless machine. The patients’ problems are all entirely homogeneous. I think we view the clinic as a petri dish in a lab. Everything can be easily changed when something new and better comes along. Every problem is the same in every situation.
But it isn’t true.
Going beyond the minute detail, and viewing the big picture of what we’ve seen (which is something new for me, I love the trees but hate the forest), the clinic is a melting pot of constraint.
Structure, practice, tradition, resource limitation. These are all things that can act as obstacles to new ideas and inventions. There is a transition cost. There is a limit to human ability.
Accidents, lifestyle, phenotype, patient history. These are all things that throw spanners into the cogs. There willbe unexpected complications. There willbe situations that demand more than a device can offer.
Having worked as a part of EWH, I have been used to the idea of space, cost, and time constraints for several years. There is something different though, about this idea that I don’t have the power to impose perfection as an engineer. It’s an interesting challenge, to face these new constraints of both order and chaos. A challenge that I look forward to facing as I draw nearer to the conclusion of collegiate career and the start of my professional life.
Blog 8 (July 6)
Maxwell Mckeough Blog

As the program draws to a close, I thought I’d immortalize in the blog some of the truly monumental experiences from the last 6 weeks.
The first day in clinic, when we met Dr. Gans in the echo lab for the first time was very interesting. Although it would end up being only one of two times that we dealt with echoes, it was a good way to begin mixing with the world of cardiology, and the technology that underlies it.
Similarly, our first catheterization case (and later the first cath case that saw us donning lead gowns) was a memorable first step into what would become a primary focus of our observations for innovation.
Seeing the Boston Scientific ablation equipment was simply fantastic, and I still can’t get over the programming that underlies it. I’ve spent several nights lying awake trying to piece together how it must interpret data for its mapping visualization.
These are the great firsts, but then there are some obvious experiences from arenas that we were experienced in. The laser lead removals, holding a demonstration pacemaker, and seeing cardiac stents with our own eyes instead of through the fluoro unit.
These last 6 weeks have been a learning experience that I think have had a very positive impact on my future activity as an engineer. It’s really something special to see the procedures first hand, and meet the people who use the devices that we will one day be a part of designing.
Alana Peters

Alana Peters
Alana Peters Blog
Alana Peters Blog
Day 1 in the Clinic
Alana Peters Blog
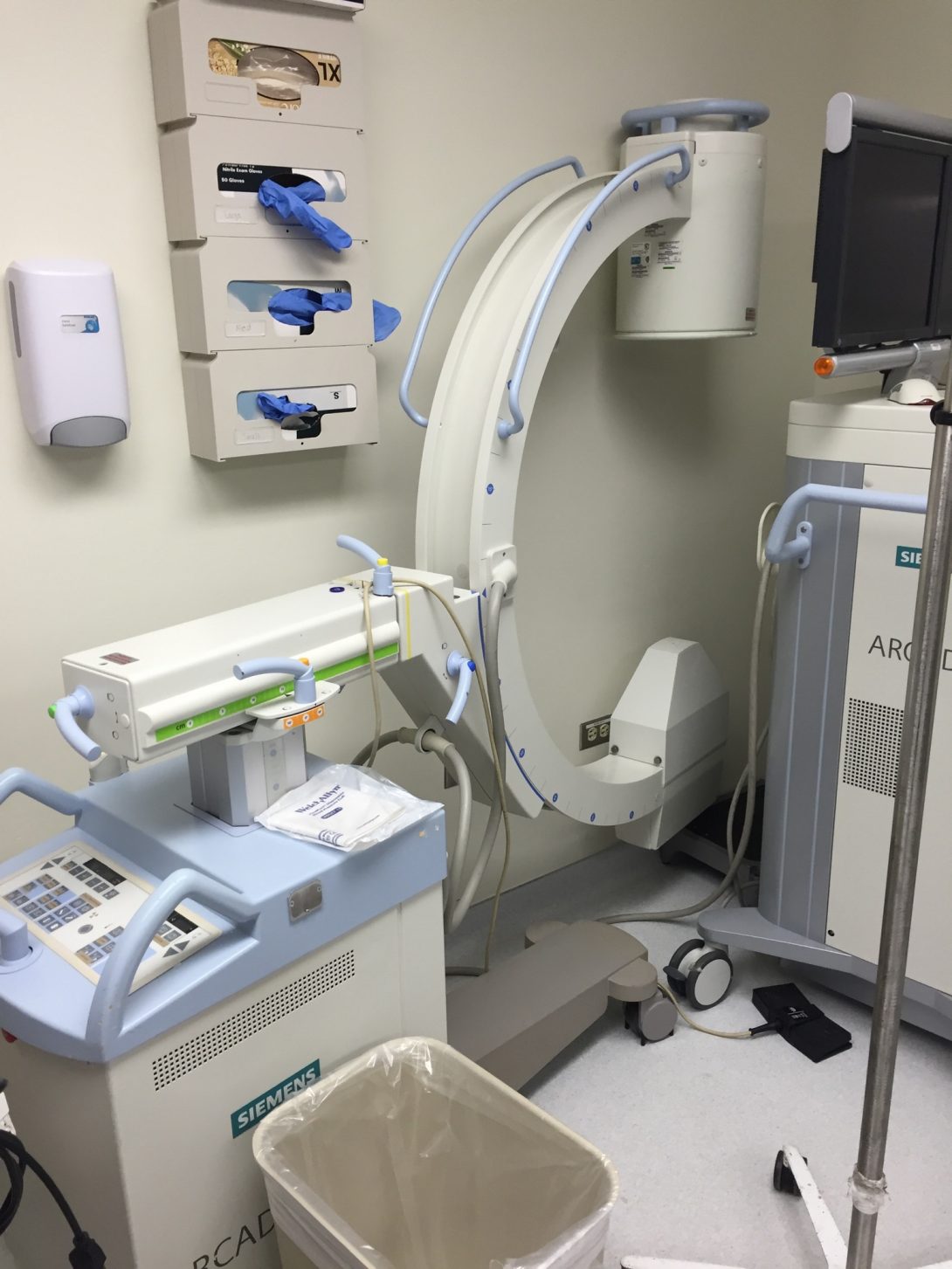
On our first day of clinic (5/31), we had a meeting with Dr. Dudek, who explained where we would go on what days and which providers we should observe and ask questions of. In the morning, we spent time with the fellows and observed a bronchoscopy. It took place in one of the endoscopy labs; the room was cramped and had a lot of equipment including an x-ray machine with a moveable C arm. (see picture) The x-ray machine was used to help the doctors visualize the location of the scope.
One of the fellows, Dr. Paul Lederer, took us under his wing for the afternoon and we went with him to the ICU. He is an excellent educator and has a seemingly endless supply of witty jokes. We observed a tracheotomy done by him and another fellow; before the procedure he explained to us exactly what he would do in each step of the procedure, which made it a great learning experience. Too bad he is moving to Texas soon and won’t be around much longer to educate UIC students.
In between seeing cases, we hung out in a break room with some of the residents and fellows, and I asked them what they’d like to see changed or if they had come across any needs in their work environment. I was surprised by how many people had laundry lists of issues they were ready to rattle off. Going into this summer I had expected that most of the needs identification would come from observing, but in fact that hasn’t been the case so far. I haven’t identified a ton of needs from observing (but I have learned a TON of clinical knowledge); rather, I have been able to identify needs mostly from asking the residents and other healthcare providers as they are quick to point out what the needs are.
One of the areas for improvement that came up is the number of lights, alarms and other noises in the ICU. This indirectly increases the incidence of delirium in patients, because delirium is exacerbated by disrupted sleep/wake cycles, and the ICU environment does not enable patients to maintain proper sleep cycles. Below is an article that helps explain this concept. Anyway, that’s all for now. Thanks for reading.
Sleep Clinic
Alana Peters Blog

Friday (6/2) afternoon we walked to the sleep center, which was a longer walk than we anticipated from the rest of the hospital/medical school. We saw patients with Dr. Najjar who had a wide range of sleep ailments, and then saw a woman fitted for a CPAP machine. There were number of neat things I learned about that I’d like to explore more in subsequent visits. Specifically, I would like to watch an overnight sleep study and be able to see the entire process unfold, and learn more about the different aspects of the patient’s sleep quality that are measured, and how these measurements are obtained.
We saw four patients in the clinic; two had sleep apnea, one had narcolepsy, and one had severe insomnia. After the appointment, one of the sleep apnea patients was fitted for a CPAP machine. It seemed like there were about 20 different options for machines in stock, with the differences mostly being in the face pieces. The rooms in the sleep clinic look very different than typical medical exam rooms; they have large beds that look like something you’d find in a hotel. (see picture). Patients are examined in the rooms during the day, and then every night patients undergo sleep testing in the rooms. Thus, they are designed to be as similar as possible to a patient’s bedroom at home.
I’m guessing most of the areas for improvement in the sleep clinic would come up during actual sleep testing, which I haven’t observed yet. However, Dr. Najjar did mention some issues he had with the computer software; he said it was time consuming to navigate patient records and the layout was clumsy. I’m hoping to identify more needs in future visits; but today I at least learned a lot about narcolepsy and the medications used to treat it.
ICU observations
Alana Peters Blog
I (and the other students in the pulmonary/critical care group) spend a fair amount of time in the ICU. The people who work in the ICU, especially the residents, have given us a lot of ideas for things they want to see improved. I have also noticed a few things. For example, during rounds, a large team of physicians, students, residents, nurses, and pharmacists (sometimes ~20 people) congregates outside the room of each patient to discuss the case before going in the room. The rooms aren’t anywhere big enough for everyone to go in, and also the hallways are sort of narrow and the spaces outside the rooms can be awkwardly shaped. This makes it hard for everyone to hear the person who is talking during rounds. The majority of times, I wasn’t able to hear what the speaker was saying, or I could only make out certain phrases; I had to focus very intensively to try to hear the essential information. If there was a way to improve the acoustics in the spaces outside the rooms, I think that would help the healthcare providers communicate, and would help the students have better learning experiences.
Typically, after we finish rounding on the patients, we will go into a small conference room to look at scans. During this time, I (and the other students) usually get a hold of a packet with information about each patient seen during rounds. This information helps us piece together the things we see and learn from them, although if it was easier to hear the people talking during rounds, we would probably get a better understanding. I also noticed that the room in which we view scans only has one medium-sized monitor on the wall. When 20 people cram into the room, and some people have to stand because there aren’t enough seats, it can hard for everyone to see the monitor. I think this could easily be fixed by putting another monitor on the wall.
Dr. Dudek, the physician who is supervising us for the summer, described to us how ventilators damage patients’ lungs. Ventilators use positive pressure to make patients breathe, whereas people usually use negative pressure, which can cause injury. Another big issue this causes is infections; when patients have tubes going into their airways, pathogens can bypass many of the body’s normal defense mechanisms and infect the patients. One of the biggest drivers of quality improvement in the ICU is infections transmitted in the hospital. If there was a way to better filter the air these patients breathe, the rate of infections might drop. Hopefully this is something our group can look into as the summer goes on.
I’m required to upload a picture with each blog post, so here is a picture of a bulletin board in the ICU with information about quality over time.
More time in the sleep clinic
Alana Peters Blog

Friday afternoon our group was in the sleep center. This was a really fun day for me, probably the best day I’ve had in clinical immersion so far. I got to ask the patients a lot of questions, and see some of them before the doctor saw them, almost as if I was doing a rotation. It was a very empowering experience and it reminded me that, even though I forgot a lot of things I learned this past year, I still learned so much that I can apply to treating patients.
One of the neat things about Friday afternoon was that I got to spend a lot of time with the patients and hear about all of their medical conditions. Some of the patients we saw had very complex medical histories, and the fellows and attendings are very constrained as far as how much time they can spend with each patient. Since I’m in the unique position of being a student (and not needing to get paid by an insurance company), I had the freedom to spend more time with the patients and hear about more of their issues than someone farther along in their training.
A few physicians have expressed frustration at not being able to spend more time with patients. Dr. Dudek told our group earlier in the week about how he is allotted 20 minutes per patient, and that includes time for both seeing the patient and doing paperwork. He said that he is required as part of his job to see a certain volume of patients, and that a lot of times the amount of time he gets with them isn’t sufficient to hear all of their complaints. Additionally, he described how the electronic medical record system is not designed for optimal patient care; it is designed to facilitate billing as much as possible. This means that he has to deal with a system that is not particularly user friendly for the physicians, requiring him to spend more time at the computer and less time with patients. Nearly all of the physicians I have gotten to work with are only able to spend a limited amount of time with patients, and I have observed that they have to be very strategic about what questions they ask in order to elicit the necessary information within the time constraints. One of the patients told me after seeing the doctor that she was worried she had annoyed him, because she started talking extensively about medical problems that weren’t relevant to her chief complaint, and he (as politely as he could) had to cut her off. I explained to her that she probably didn’t annoy him, but that he just had to get through the appointment in a limited amount of time because that was what was required of him by his employer.
It is unfortunate that physicians working for a large hospital don’t have more input into how much time they can spend with each patient. I think one thing that would allow physicians to spend more time with patients is if they could spend less time doing paperwork. This would probably be accomplished by a more user-friendly medical record system, or by hiring other people to do it (which might not be feasible because of the cost it would add).
There were a few other issues that came up in the sleep clinic, but I can write about those next week.
Things I have learned
Alana Peters Blog
I have really enjoyed the first three weeks of clinical immersion. I feel like I am getting a lot out of the program, especially when it comes to medical knowledge and skills. The goal of the program is for us to come up with ways to improve on issues we encounter, through devices or other interventions. I have had to try very hard to stay focused on this goal, because by default I usually focus on the patients and their medical situation rather than what is going on around them. I have gotten to see so many patients with rare and unusual cases that it is hard to look around the room and pay attention to what is going on with the technology. In between seeing patients it is easy for me to default to reading about certain medical conditions I observed, rather than brainstorming ideas of how to improve the technology. Thankfully, the other students in my group have helped keep me on track with this.
I think it’s probably a good thing I enjoy seeing patients and learning medical skills so much, since my training will involve doing that for extended periods of time. One thing I have definitely gotten better at is reading x-rays and CT scans, especially scans of the torso. The fellows in the pulmonary clinic have been very good teachers to us, and have walked us through the scans of many patients. While I’m not sure how this skill will help me in clinical immersion or in my IMED capstone project, it is a useful skill to have for licensing exams and a medical career. The pulmonary fellows have also gone out of their way to teach us about other topics–pulmonary hypertension, sepsis, lupus, and several other conditions. The picture attached features Dr. Asharul Usmani teaching us and several residents about pulmonary hypertension…I swear I learned something even if I look spaced out.
I have also really enjoyed seeing the ways in which the physicians interact with the patients. Some of the physicians are really exceptional in this regard, like Dr. Roberto Machado, whom I have gotten to see patients with a few times. Some of the physicians are more average when it comes to people skills. In each encounter, I try to learn something about how to treat patients. I think this is an important skill for me to develop because I would like to make patients feel as comfortable as possible, and also because good doctor patient relationships usually lead to higher rates of compliance with treatment plans.
Things We Are Working On
Alana Peters Blog
After the first three weeks spent in clinical immersion, our group has identified a few issues that we would like to address. We probably won’t be able to tackle all of them this summer, but hopefully we can make some progress at least.
One area of need we have identified is the need for better patient education regarding the use of inhalers. Improper inhaler use is a huge problem. A lot of patients don’t know how to properly use their inhalers, and a lot of patients have multiple inhalers they mix up and take at the wrong frequencies. Additionally, control inhalers don’t always yield immediate results, and because of this a lot of patients quit the medication because they don’t see immediate effects. This UpToDate article covers a lot of the issues nicely, and explains that proper patient education and a good physician-patient relationship are important in minimizing inhaler noncompliance.
https://www.uptodate.com/contents/enhancing-patient-adherence-to-asthma-therapy
Another issue we would like to address is the high rate of patients not showing up to their appointments. On any given day, 10-50% of patients will not show up. The doctors usually compensate for this by scheduling more patients than they can realistically see, and still usually they are running late. A lot of factors contribute to patients not showing up. Some patients lack transportation, some patients have trouble getting time off from work, and some patients have a hard time keeping track of when their appointments are. Earlier this year, UIH launched a service called PRONTO, which partners with Lyft to provide rides home for people receiving inpatient care. Ideally, there would be a way to expand this service and provide rides for people with outpatient appointments. When patients miss their appointments,the hospital loses money, so this would be in the best interest of the hospital as well. Providing patients with rides to their appointments wouldn’t eliminate all the causes of no-shows, but it would eliminate transportation concerns and also increase patient accountability.
ICU Delirium
Alana Peters Blog

On Friday our group met with Dr. Dudek to run some ideas by him, and it turned out to be a helpful meeting. He helped us identify which of our ideas were the most promising, as well as express his support for our ideas. We were very happy about how supportive he seemed, since having faculty support will make it much easier to actually implement one or more of our ideas in a patient care setting.
Our group has narrowed our focus down to two issues we intend to work on to hopefully get actual solutions implemented. One of the issues we are working on is minimizing delirium in ICU patients. Delirium is a problem throughout the hospital but especially in the ICU. The most commonly affected patients are elderly. Typically delirium stems from patients not knowing where they are, and it can be exacerbated by disrupted sleep/wake cycles. As a result, most of the interventions we are working attempt to either help orient the patients to their situation, or to regulate their sleep cycle properly.
When we met with Dr. Dudek, he told us about someone he worked with in the public health department, Dr. Anthony Faiola, who tried to implement a system in the ICU that would enable patients to FaceTime their relatives. Apparently the project did not get adequate funding, but this is something we plan to look into because it sounds like it would be helpful to keep the patients oriented. When it comes to solutions we could actually implement, we are hoping to focus on interventions that are free or low cost, because this way we could realistically implement them in one or two rooms and observe the outcomes of the patients in those rooms versus the others. I’m not sure how much I should write on this blog about our ideas, since anyone can read it, but we have compiled a list of ~10 interventions we think could address this problem, and we are hoping to implement at least a few of them by the end of the summer.