Students: Part 2
Luke Pretzie

I am an Honors College student, I have a 3.9/4.0 GPA, I am founder and president of the IEEE Engineering, Medicine
and Biology Society at UIC, and I will be seeking an entry-level industry position come summer 2018.
The accomplishment I am most proud of is the chapter I helped and had much help creating and running. EMBS is one of the resources I have used most during my time at UIC. Its Chronus Mentorship Program has helped me connect with professionals from around the world and has allowed me to receive advice that I would not be able to ascertain from any other source. Its IEEE backing of more than 421,000 members from over 160 countries ensures that participants within student chapters have the resources necessary to exercise their creativity and problem solving skills. Most important to me was the opportunity it gave me to partake in a leadership position, empowering me with the soft skills that a university curriculum cannot provide.
In my free time, I enjoy simple, small things, such as long car rides, tasty food, niche music, scenic views, and a game of cards.
Luke Pretzie Blog
Luke Pretzie Blog
Week 1 Ophthalmology Observations – Sanitation in the OR
Luke Pretzie Blog

The operating room is a necessarily sterile place, and while observing I noticed that there are many procedures in place to ensure that the place remains sterile. There are the obvious observations, such as watching primary attendants, fellows, residents, technicians and others scrubbing and washing before and after each surgery. This you could gather from a medicine-themed television drama. Some things you don’t notice until you are in the environment. This includes the amount of material that gets thrown out. Gloves, surgical smocks, iodine, lactated Ringer’s solution, 0.9% sodium chloride solutions, hoses, overhead lamp handles, monitor coverings, you name it. Throwing out these items is necessary in terms of keeping the operating room clean, the number one priority of the hospital, but if there could be a way to sanitize the operating room without wasting so many materials, then who knows how many resources can be saved. More time in the OR will be needed before I can conclude whether or not this is possible.
Image Citation: Porter, R (2001). The Cambridge illustrated history of medicine. Cambridge University Press. pp. 376. ISBN 0-521-00252-4.
Week 1 Ophthalmology Observations – Retina Analysis Device
Luke Pretzie Blog

Working in the OR today, I was able to observe the use of a device known as the Clarity RetCam 3. This device is used to observe the retina of patients in a relatively non-invasive manner in order to aid surgeries or diagnose maladies. I noticed that this device has two major flaws. The most basic flaw to overcome is the resolution of the images. Given enough time, advances in optical and image processing technology will result in higher quality images. Another problem with a less intuitive solution is the means of operating the device. There are three different control schemes on the device. The first is the camera itself, which is held by the MD using at least one hand, often times two. The second is the keyboard of the machine, used to alter settings on the device or create new recordings. The third is a foot switch, whose function I am unaware of but which was used nonetheless. These three control schemes make the device very difficult to use, and often require two doctors in order to fully utilize the machine. One thing that immediately comes to mind in terms of making the machine more efficient to use is to add button controls to the device in order to make use of a keyboard less necessary. With time and research I am confident that an improved design can be discovered.
Image Citation: “Smartscope PRO.” Optomed. Extranet, 31 Aug. 2015. Web. 06 July 2017.
Week 2 Ophthalmology Observations – Making Teaching Easier
Luke Pretzie Blog

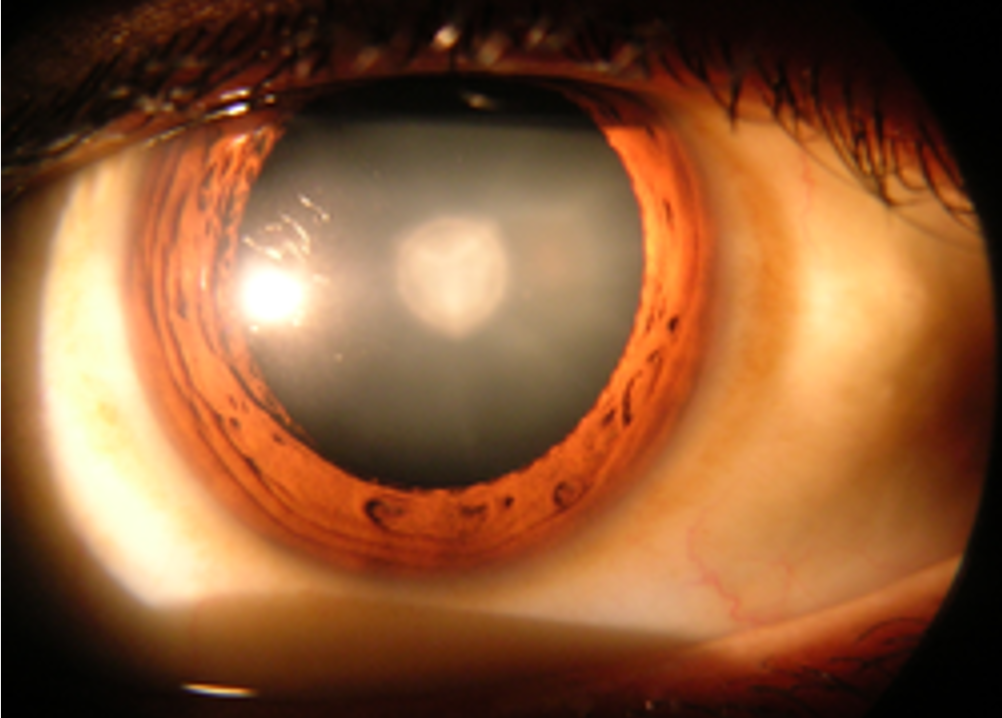
Regardless of what department of ophthalmology you are in – cornea, retina, glaucoma, you name it – you will find a device known as the slit lamp. The slit lamp has undergone few changes since its formal unveiling in the 1920s, which is precisely why Dr. Lim of the retina department suggested modifying the device such that images which she sees through the binocular scope of the slit lamp can be seen on a monitor on the wall. This would allow her to show her findings to residents, fellows, and family members.
This concept seems relatively easy to implement, but it brings forth many interesting design questions. The most obvious question is cost: If the cost of providing this technology is too high, then it will not be approved. The next natural question would be “How cheap of a camera system could we design that allows fine detail in the image to be seen without making the device too expensive”? The technology might not even be there yet. It goes to show how difficult it can be to properly implement ideas in any setting.
Week 2 Ophthalmology Observations – Unusual EMR Software
Luke Pretzie Blog
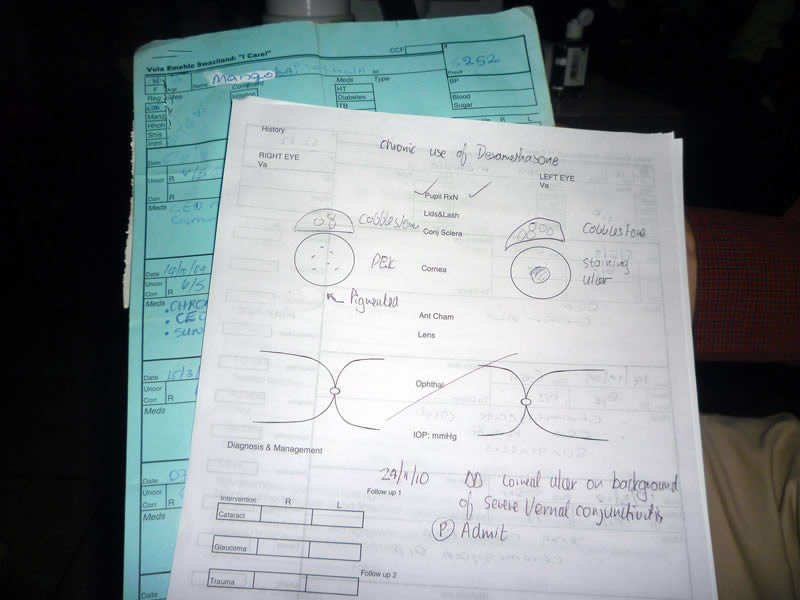
During my rotation in the pediatric ophthalmology clinic, I got a chance to speak with a research assistant about the EMR software, or Electronic Medical Record Software, that they use. The way ophthalmology uses EMR is strange. Most other clinics submit all information using a computer which they type information directly into, almost like a Word Document template. Ophthalmology has similar forms, but for the most part, they have physical copies which they scan and submit into the computer. The reason for doing this is that most ophthalmic notes have quick sketches of the eyes that the doctor makes to let other doctors know, for instance, where the location of a scratch on the cornea is in a qualitative way.
On top of this, there were complaints that the software was slow, and thus trying to access many different entries of a patient was difficult. There are other software systems which are faster and easier to use that other healthcare centers, such as Rush University Medical Center, already employ. Of course, they are more expensive. If a compromise between power and price can be found, then the ophthalmology software could almost certainly see a big upgrade.
Week 3 Ophthalmology Observations – IR In The Clinic
Luke Pretzie Blog
One of the suggestions made by an ophthalmologist we are working with is actively being worked on by resident students. This concept is the use of infrared light in the place of visible light for slit lamps. Slit lamps are devices which rely on reflecting visible light off the eye in order to make a diagnosis. The problem with this technique is that most people require dilating eye drops in order to get good images, which takes a long time and causes obnoxious wait times. The solution is to use infrared light in the place of visible light to make the images. This works because the eye cannot see the infrared light and therefore will not dilate, however the light can still be collected by a photo detector and processed to create useful images. Only time will tell how far this technology progresses.
Image Citation: “Eye Examination with the Slit Lamp”, Zeiss, p. 33
Week 3 Ophthalmology Observations – Gas Dissolution in Vitrectomies & Membranectomies
Luke Pretzie Blog

This week we spoke with Dr. Leiderman about coming up with an alternate gas to use during vitrectomy and/or membranectomy procedures. A vitrectomy is a procedure in which vitreous fluid is removed from the eye, and a membranectomy is a procedure in which layers of unhealthy retinal tissue are removed. During these procedures, a gaseous substance is gently pumped into the vitrea of the eye in order to apply constant pressure to the retina so that it can stay firmly affixed to the back of the eye. The body will constantly replenish vitreous fluid in the eye, eventually absorbing and secreting the gas, until what is left is an eye which appears to be functioning normally.
Dr. Leiderman was very generous to give us suggestions as what could be far-off solutions to problems which most clinicians are not considering at this time about the procedure. Certainly there are obvious constraints with the gas. For instance, it must be non-toxic to the body and highly non-reactive. Less obvious, however, is the fact that the gas currently being used is not environmentally friendly (Its production releases tens of thousands of times more greenhouse gases than gasoline combustion, however its niche applications make its global contribution minimal), it has poor refractive properties (a gaseous substance which mimics the refractive index of the vitreous fluid would allow patients to have maximum vision while waiting for the gas to be metabolized), and cannot have its volume adjusted after administration (whatever the patient gets, they are stuck with, unless they want to undergo another surgery). These potential solutions to problems which are only now being recognized is very far off, but it nevertheless makes for a good thought experiment regarding what we should be considering during our rotations.
Image Citation:
Luke Pretzie Blog
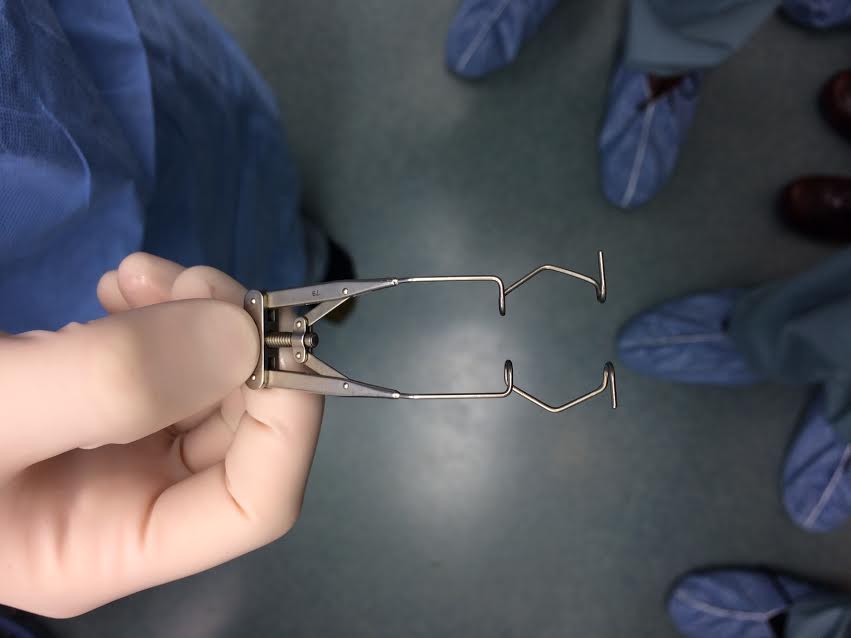
Dr. Yu approached us earlier this week asking us if we would consider redesigning the eye speculum, a device which is used to hold the eye open during certain procedures, such as cataract surgery and intravitreal injections. There already exist a few variations on the eye speculum, such as the pediatric eye speculum for younger patients. All speculum, however, suffer from two major design flaws. The first design flaw is the thickness of the prongs that hold the eye open: They constantly get in the surgeon’s way as he or she is performing procedures. The second flaw lies in the implementation of the speculum in the first place: they are typically difficult to insert and difficult to extract.
My group has already began researching the patents and design documents of eye speculum that have been used in the past and are currently being used now. We are hoping to have a basic design blueprint within the next few days.
Week 4 Ophthalmology Observations – Force Requirements For New Eye Speculum
Luke Pretzie Blog
In designing this new eye speculum, one of the biggest questions which was raised had to do with the force requirements. My group and myself have witnessed firsthand that some patients have a strong urge to blink in the middle of surgery. The speculum needs to be strong enough to withstand that force, but weak enough to be handled by the surgeon with ease.
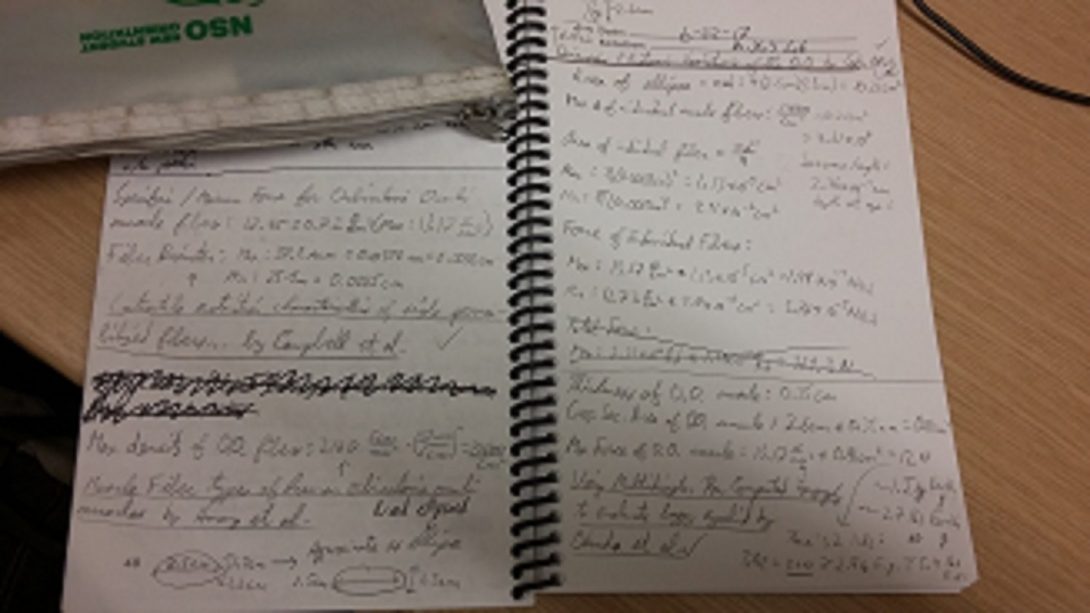
I tasked myself with determining the theoretical blink strength of a typical human eye. Using cited ophthalmology research papers I was able to determine the dimensions of the orbicularis oculi muscles (the muscles responsible for closing the eye) and the maximum force which could be generated by these muscles.
Using these calculations, I was able to determine that the maximum theoretical blink strength of a typical person is approximately 24 newtons. That is, if both eyelids were attached to a friction-less pulley system, the person would be able to lift 2.4 kilograms (5.4 pounds) off the ground by closing their eyes.
Eye speculum which require 24 newtons of force to close would obviously have to be tested on volunteers before they could be used clinically. Nonetheless, determining this criteria bring us one step closer to creating a new medical device.
Citations:
Luke Pretzie Blog

This week our group got a chance to see the laboratory that Dr. Yu and his students conduct research in. There are two main projects towards which they are currently directing their efforts: The first is an essay in the feasibility of 3D printing a Boston KPro prosthesis (which I will be sure to discuss in the following blog), and the use of virtual reality to diagnose visual field defects.
A visual field defect is a condition in which a person’s area of vision is decreased, typically due to damage of the optic nerve, the occipital lobe of the brain, or the eye itself. The resulting symptom of these defects ranges from tunnel vision to lack of central vision, and can even result in each eye only being able to receive the left or right side of an image.
By using a virtual reality driving simulation, these conditions can be built into the game such that anyone can understand what it feels like to have these conditions. While the impact of Dr. Yu’s virtual reality work is not yet fully realized and the project is still in its infancy, there lies potential in the application of this technology to educate the public on the symptoms of visual field defects.
Week 5 Ophthalmology Observations – Feasibility of 3D Printing Boston KPro
Luke Pretzie Blog
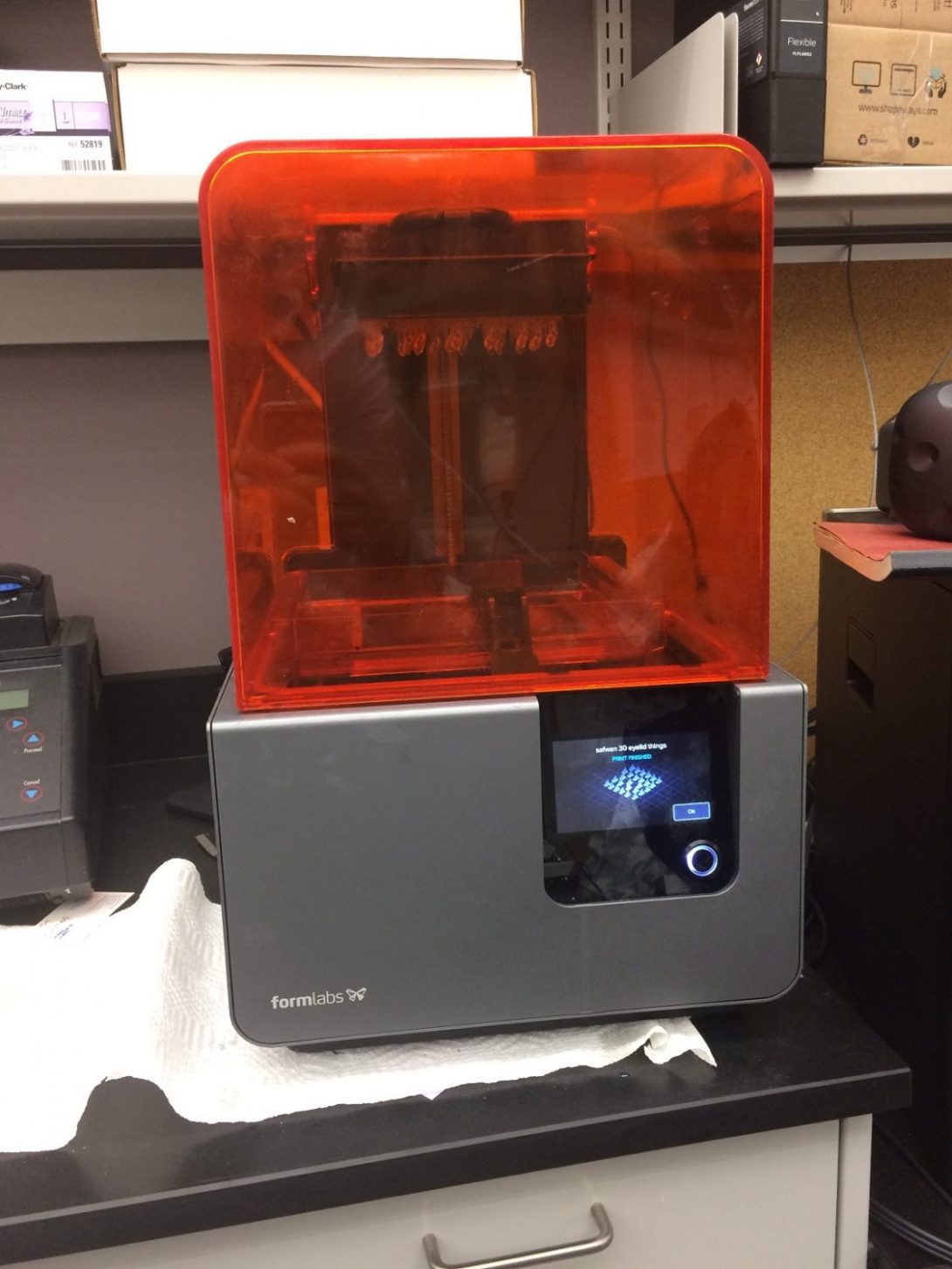
The Boston Keratoprosthesis, also known as the Boston KPro, is a device used to replace the cornea of a patient who is unable to accept a biological cornea transplant. This device is synthetic, and therefore must be made from biocompatible materials, such as polymethylmethacrylate and titanium. One of Dr. Yu’s areas of interest in research is the feasibility of using a 3D printer to mass-produce these devices with greater ease and less expense.
The 3D printer being used is the product of FormLabs, a company which is known not only for their printer technology, but also for their highly successful Kickstarter campaign which allowed them to innovate and grow their business. One of the many materials with which you can print from the FormLabs machine is a proprietary 3D ink which is biocompatible, hence Dr. Yu’s application of the device to the creation of synthetic corneal transplantation prostheses.
Currently, it is understood that the device can be produced using the 3D printer. The yield, however, is quite poor, with many of the prostheses having defects which makes them unusable. Dr. Yu’s intuition is that the manufacturing process is not suited for the creation of these devices. Time will tell if mass-produced 3D printed Boston KPros is viable.
Week 6 Ophthalmology Observations – Gathering Eye Dimensions Using Digital Photography
Luke Pretzie Blog
You can gather from reading the series of blogs I have written that many projects were assigned to the ophthalmology group. Doctors from all departments of ophthalmology were giving us advice about how to tackle the major problems in their disciplines. For a variety of reasons, we decided that the project we were going to focus on was the redesign of an eye speculum. If we had not chosen that project to focus on, we would have almost certainly chosen to work on our second choice of project: Facial recognition and distance software.
Dr. Setabutr from occuloplastics was the one who suggested we work on this project. Within the field of oculoplastics, it is common for practitioners to need to know the dimensions of the eye. In order for them to determine these dimensions, they typically use a small ruler and manually measure the dimensions of the eye and the area around the eye. This process is simple and typically yields accurate measurements, however it is a mundane and repetitive task which clinicians would prefer not to perform.
In an attempt to solve this problem, the ophthalmology team has considered researching and developing software which, when given an image of a human face, would calculate the distances and dimensions of they eyes. The most important aspect of this theoretical device, according to the practitioners, is that it has to be accurate to one millimeter in order for procedures to be successful. Meeting this criteria would make the device worth using.
After a sufficient amount of research, our team concluded the project would be too advanced for the six week duration of the program. In spite of this, we are still interested in collaborating with Dr. Setabutr in the future to create such software. Google recently unveiled a new platform known as Google Tango which allows a phone camera to approximate distances to and from objects. Integrating Google Tango with pre-existing facial recognition software might be enough to generate a feasible design.
Vijay Putherickal

Strong healthcare services professional seeking a Bachelor of Science (BS) focused in Bioengineering from University of Illinois at Chicago. Mainly skilled in AutoCAD, Pymol, Matlab, C, and C , and an experienced Certified Pharmacy Technician with a demonstrated history of working in the retail industry.
Vijay Putherickal Blog
Vijay Putherickal Blog
Starting the Journey
Vijay Putherickal Blog

Day 1 of the program was an introduction/orientation which briefed an overall picture of the program and its purposes. I was very excited to meet new people and share experiences with them. We had a short lecture discussing the process of designing human-centered devices. A good design can be described by answering three questions- is the design desirable? Is the design feasible? and is the design viable? if we can answer yes to all these questions, our product will make into the category of best designs. In order to make the concepts clear, we also reviewed a case study about infusion pumps. We had a guest speaker in the afternoon session who helped us to develop our professional skills and increased our confidence levels to perform successfully in the clinical environments.
On day 2, our team of anesthesiology met with our mentor Dr. Nishioka in UI hospital. Dr. Nishioka is one of the doctors who is very calm and welcoming. He loves to introduce new technologies to medical world which boosts patient care to its next level. Our team divided into groups of two which includes an IMED student and a BIOE student. We went to different surgical rooms to observe what is needed to be improved and took notes for further discussions. As a team, we brought up suggestions starting from the layout of the room to minor corrections which might help the user to perform their tasks efficiently. I am very excited to continue this academic journey with my colleagues and waiting to learn and explore more from this clinical atmosphere.
The World of Machines
Vijay Putherickal Blog
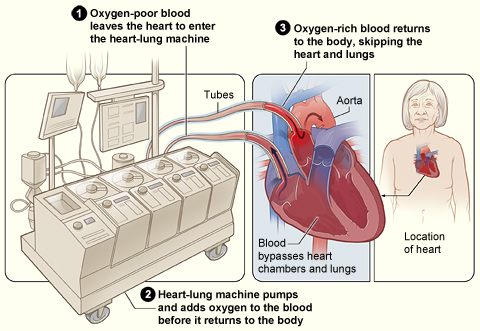
The devices and instruments medical professional use during surgeries can be very intense. As my journey of exploring clinical environment continues, our group have been exposed to several kinds of machines which perform miraculous works and aids medical professionals to help meet patient needs. So far, I have been exposed to heart-lung machine (aka “Pump”) which aids in purifying the non-oxygenated blood (removing CO2from the blood) and pumps oxygenated blood to the body, The Da Vinci machine which perform surgeries without making big cuts on the body. The robotic arms of this device are passed through small holes made by surgeons. Then, the technicians change the arm according to the surgeon’s commands. The surgeon control these robotic arms from a small booth like structure. Advanced anesthesiology machines show the concentration of anesthetic gases, heart rate, blood pressure, oxygen levels, and if patient is breathing with the aid of the machine or not. If the patient is breathing with the aid of the machine, then the anesthesiology machine would show output in green, and if the patient is breathing without any assistance, then the output is shown in blue. There are also small devices such as laryngoscope and fiber optics which help the anesthesiologist to check the airway of the patent. The devices mentioned above worth millions of dollars and even some of their disposable parts can cost between hundreds to thousands of dollars. As engineers, we can make generic parts to these disposable parts, which are more affordable for patient use.
One of the common observation which brought a lot of attention was the inefficient use of space and disorganized wires. In many surgical rooms, doctors and other attendees had hard time moving around the room. For major surgeries, the rooms will be crowded with individuals and complex equipments. The wires from these equipments are laid down, and anyone can trip down and fall if careless. Everyone should be cautious about the wires which are laying down and that is very inconvenient for everyone. We also visited the pre-op area, where the patients check in before the surgery. We saw some inefficiency in the flow which rushes the staff to perform their tasks quickly, and get the patients to their respective surgical rooms on time. As a group, we thought that this might create a lot of tension in patients since space of error is so big. The reasons behind this inefficient flow are many, and one them is that the patient might come later than the scheduled time. So, as a group we thought that if we can come up with an interactive schedule which tracks the patient and notifies the nurse or any technicians, that might help the staff to regularize the schedule little more conveniently.
Another problem which came to our notice is the schedule conflict and lack of sufficient staff for each surgery. According to hospital polices, there is a flow chart they refer for scheduling surgeries. Sometimes surgeons might tweak a lot more cases beyond the capacity, and the department is helpless to provide enough anesthesiologists and other professionals to assist in the surgery. There is also an issue with booking surgical rooms due to this surgical conflict, and the scheduling wing is unwantedly getting all the blames even though they did their best. A week worth of experience taught me a lot about hospital administration and its functions. Looking forward to learn more and as always going to have more fun times!
Does Sleepless Nights Make a Good Doctor?
Vijay Putherickal Blog

The new week started off with our group presentations including past week’s experiences and observations. Dr. Susan Starling gave us a presentation on how to be a successful observer, and gave us some tips on it. Later she talked about how to interview someone and the approach to it. Interviewing someone and getting all the information required is a very hard task, and if not careful, the interviewee might get offended/bothered with our questions. She also taught us that we should not make any direct questions (ie. Yes or no questions) which might end the conversation. Later in the day, we had an activity session where I interviewed my partner Joe and tried to gather some information about his “Perfect Day.” We wrapped up Monday’s session with a group activity where we had to write our observations and other important info. On a sticky note and stick to a white board provided to our teams. The main challenge in that activity was to arrange each observation and other info and to group them accordingly. Finally, we took a group photo of the whole clinical immersion team, which would be later used as a cover picture for summer 2017 clinical immersion activity book.
On Tuesday, our team started at 6:30 AM as usual in the anesthesiology conference room. No department meeting was scheduled for that day. Dr. Nishioka usually picks a topic for us to focus on each day. For Tuesday, our team was focusing on education. After we met with Dr. Nishioka, we went to the ICU with him to observe an ultrasound. After attending that, Dr. Nishioka introduced us two senior residents who oversaw the ICU that day. They gave us valuable information regarding the medical school life and what difficulties they had to go through over the past years to achieve their goal. Our aim was to find out if technology can help medical students to get to their goal more conveniently with better understanding of the material presented to them (ie. Interactive learning simulations). As we talked to them, we understood that the academics itself was not bothering them that much, but discomfort was on practical part. They lacked practical training and was very nervous if they are going to make any mistakes. Residents also told us that they did not get exposure to every department during their rotations and had situations where students switch to some other department in the later period due to lack of interest/passion. I got a chance to talk to some more residents on that day, and understood that most of them are adjusting to their discomforts since their expectations for medical school was very similar and they chose to go for it. As a team, we thought that we should have a better education curriculum. Medical students are the future doctors, and we don’t want them to make mistakes due to lack of knowledge. Many students tend to forget many of the important contents since they crunched the topics and memorized most of the contents for the sake of doing well on the upcoming exams. We should develop interactive learning assignments where they can visualize what they are learning and apply their knowledge in the scenarios simulated. Thus, there is a better chance of remembering the contents for longer time.
Wednesday was another day for closer observations. This time we went to surgical rooms individually than going in groups of two. We observed the procedure, took down some notes and tried to identify the roots of these problems. May of our observations were very similar to the ones brought up before. We also brainstormed some ideas which might be the solutions to these problems. Ideas are like stars, there are infinite of them, but the biggest and the brightest is better seen than the other ones.
The Role of Convenience in Designing
Vijay Putherickal Blog
This week started off with our group presentations as usual. Each group got to present what they observed and got a chance to say what problems they found throughout. This time there was a time restriction for the presenters, and the timer would ring after 15 mins and that included Q&A as well. Most of the groups were successful in presenting within their time limit and had a great time listening to the things needed to be improved. The interesting factor is that, some of the problems were overlapping throughout the department such as the problem regarding running wires. After our presentation, Dr. Kotche gave a small lecture on writing need statement. A need statement is composed of addressing three main things; problem, population and outcome. We don’t want to be so specific about the matter, but at the same time we don’t want to be too general either. A good need statement would have a balance of the three components. Usually the afternoon sessions are dedicated to activity session, and this time we were directed to writing more observations and started writing our needs statement based on our observations.
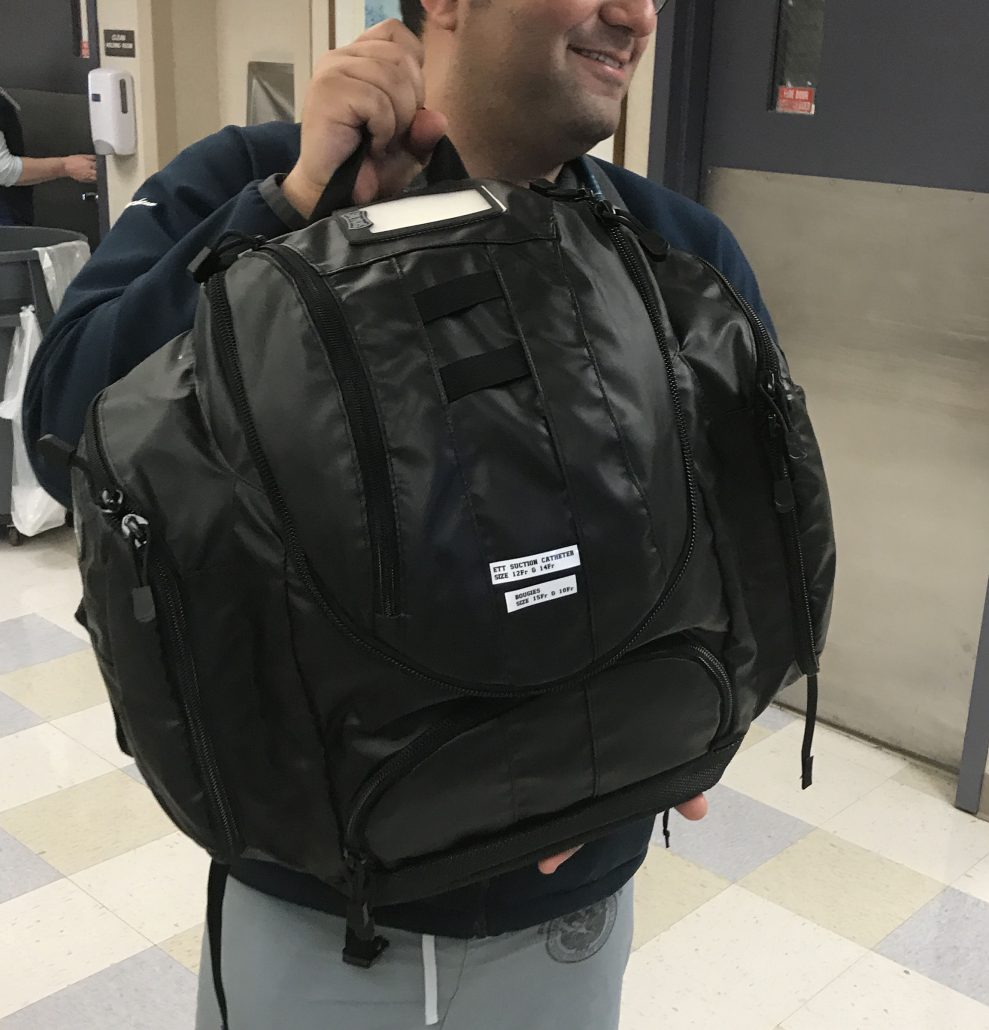
Adding to our observation list, we were introduced to old and current airway box. The design of this emergency airway box makes it difficult to operate. The main purpose of this emergency airway box is to help the caregiver to reach the place of emergency quick and start resuscitation as fast as he/she can, but the current design is very confusing and due to the lack of order, the caregiver can get confused and can have hard time finding the medicine or the equipment he/she is looking for. The other problem with this design is the size. After filling all the equipments and medicines, the bag looks very bulky and prevent the freedom of movement. The caregiver could not fit themselves into a small space due to this bulky bag, and restricts its usage to larger area. A new design for the emergency airway bag was suggested, and it’s on the process of getting clearance from different departments to make sure it’s safe to use.
Another problem which is going on in the hospital is reserving items. Some devices such as PDMs (Patient display monitor) are being reserved by different departments. PDM is something like an external hard drive which save a patient’s vitals until he/she is gone from the hospital. There are only sufficient PDMs for each bed and there are no extras if it goes missing. So, if some department reserve this PDM then that blocks a patient to get a bed in the critical units. The hospital cannot get extras due to its high cost, a PDM can cost from 10K-20K per unit. There should be a way to track these kinds of devices regularly, and make sure it is available in every unit so that each department can admit patients in need efficiently.
Our journey with the hospital crew is getting more interesting as the days are passing by, and every staff are welcoming and taking their time to talk to us. We are trying to interview as many hospital staffs and patients to understand their difficulties and always thinking a feasible solution that might help the situation.
Sharing is Caring
Vijay Putherickal Blog

We wanted to see the need of an anesthesiologist in different departments. To do so, first we went to IR department to watch couple procedures which were done under anesthesia. As usual, our group splits into two groups to observe different procedures. Both procedures were complex and time consuming. One of the common problem we observed in these rooms are the lack of space and there are no live video projections which would help in observing. Giant X-Ray machines are placed in every rooms, and other standard equipments fills the room. Only bare amount of space is available for caregivers. We spent most of our day in the IR department to observe different types of procedures.
We visited OB another day to see how anesthesia is helping the procedures in labor rooms. It was interesting to see that the layout of the OB rooms is little different than normal OR. Here anesthesiologists are provided with omnicell which is a small shelf where they keep different drugs. The main difference from other drug shelves is that it is password locked and computer keeps the record of the amount of drugs dispensed. Due to this reason, even narcotics are allowed in these drawers when anesthesiologists need to access them. Most of the patients will be awake during the procedure, therefore observing the procedure is difficult. A crowd might make the patient nervous and that can impact the procedure, so only limited number of caregivers are allowed during the procedure unless there are some complications. We interviewed the residents from the OB anesthesia to understand their needs and concerns. Some suggestions they had was to have an automatic drug dispenser through IV. When the caregiver input the name and dosage of the drug, the computer should administer the drug to the patient. They also said that countries like Japan already have such technology in their hospitals. These rooms were not filled with all sorts of devices as a normal OR. Only limited devices were observed, and it looks like they designed the layout of the room little better.
We usually have a small meeting around 6:30 AM in the anesthesiology conference room. The meeting can vary from a full-size presentation to review of an academic journal. This week we had chance to listen to an awesome presentation about a field service conducted by UIH med students in Rwanda. They went there to teach about the usages of equipments such as ultrasound machines, ECG, etc. It was surprising to hear that even some of the medical professionals over there did not know how to use them. They had these costly equipments there, but no one knew how to use it. Another sad part was that, once these machines had some technical issues, no one knows to repair it, so they lock these machines in closets and these get permanently damaged after long time. Another unfortunate news I heard from them was the graduation rate from medical schools in Rwanda are very low, and most of these graduated doctors usually don’t serve in the country. They prefer to go abroad due to better quality of life. The people who stay there tend to have very little knowledge and their clinical skill applications tend to be riskier compared to the procedures performed by doctors in United States due to the lack of advanced technology.
We are coming closer to the end of this program, and I wish I had more time to observe and listen to these interesting things. I am sure that the upcoming three weeks would load me with even more information.
Flickering Ideas
Vijay Putherickal Blog

Another Monday have arrived. As usual we begin with the presentation, and this time we had to present our three needs statement along with at least three drafts. Making a needs statement require a lot of revisions, and to have a good need statement we should incorporate our population, problem and outcome clearly in the statement and we also have to make sure that they are not too general neither too specific. The three main problems we thought need attention are; caregiver identification by the patient, Promote learning atmosphere, and schedule conflicts. From these three, we must come to one important problem which we can find a feasible solution to in next two and a half weeks. It is a hard decision to make, but fortunately we didn’t have to choose it at that moment. We had a small presentation from Dr. Kim helping us to brainstorm ideas efficiently and to stay focused on the topic. Also, we had a brainstorming session in the afternoon which helped us to narrow down our three topics into two. We will be brainstorming more of these ideas with our mentor to come to a single problem that we will tackle down in the coming two and half weeks.
The next day, we went back to OB and in pre-op to see more procedures and this time we switched as well. So, the group who got a chance to visit OB last week would go to pre-op area to see nerve blocking technique. I went to OB this time hoping to observe a procedure. The OB rooms are very different from OR rooms. Here the patient is awake most of the times. So, the resident will have to get the consent from the patients to let us in to the rooms. Most of the patients were very nice to give consents and we got a chance to see the “Check status” first. The residents would go the rooms of respective patients to check their status and make sure that they are not receiving unnecessary medications. They do mini physical tests to see if patient can do these tasks or if they are uncomfortable doing it. According to these feedbacks they determine if everything is going well or not. Then we went to see an epidural and a spinal nerve block. This procedure seems to be very hard especially for a new resident. Ultrasound machines can aid this procedure to a level, but as we were talking to Dr. Galvan about this, she said even experienced doctors can have hard time since the body language of the patient can be tricky enough to make the procedure harder.
Next day, we get to see more procedures in the OR. We are specifically focused on the topics we chose and noting down many more observation regarding those two main topics we are covering. As we understand one problem better than the other, we can start proposing a solution which could improve the situation. We can also have a discussion sessions afterwards on why the proposed solutions would work and if there are multiple ideas, can choose the best solution to the problem. We are hoping to have a clearer picture of the solution by middle of this week and can start our rough drafts based of that. Even though this sound so much work intensive, we are enjoying this program a lot and I wish to do this every summer and find a solid solution to some of the chronic problems.
A Third Eye for Future Surgeons
Vijay Putherickal Blog

I can’t believe that it was our last monday session, and we are wrapping up the program. It was really amazing to see the ideas and design concepts every groups had, and I believe if we extend this program little further we may actually see some functional devices by the end of this program. As usual the evening session was very productive and helped us in developing ideas for the prototypes. The small accessories we got, helped us to create a gimmick of the actual scenario and helped us to discuss further what needs to be improved in the execution side. Since we are coming closer to the end of this program, we are more focused on one area which needs maximum attention.
Moving forward to create ideal solutions to the problem, we always tried to think from the user perspective. Our goal is to make OR learners experience much better without disturbing the surgeons and other clinicians involved in the procedure. Joe and Chris (IMED students) always gave guidelines in designing this learning atmosphere. They would make suggestions to make sure that learner is absorbing the maximum content without any confusion. For example, they suggested that the necessity of multiple camera views to make sure that the learner is fully aware of the region where the procedure is taking place rather that a single camera view which focuses on a smaller field. If we only had a single camera view, the learner would be confused about the exact location where this surgery is happening and would have to collect some background information prior to the surgery in order to gain a clearer picture of the procedure. We also discussed where this room have to be located, and should this footage be recorded for future references.
I am sure other groups are also doing their best to make an efficient and a feasible design. I wish everyone the very best and let all our designs help to create a better healthcare system.
Final Edits
Vijay Putherickal Blog

As the clinical days are coming to an end, we did more observations and brainstormed more feasible solutions to the problem we identified. Initially, we thought to do live streaming video as well as a projection of this video onto a mock patient, and the resident gets to do the same procedure to what the doctor does. The resident can also choose to do a test mode, where a software can analyze and compare how close the resident performed compared to the actual surgeon. This way residents can get feedback on how well they understood this procedure.
Another opportunity we got this week was that we got a chance to speak with Linda, who is a hospital designer. She gave us so many valuable advices and suggestions on how an ideal hospital should be designed. Something that got my attention was the statement about wires and tubes. She said we could avoid the problem with wires and tubes if the cable organizer is the last person involved in the design process. So, after all equipments are installed, the cable organizer gets to organize all the wires in the room, and nothing new can get tangled. She also brought up a great point on getting community involvement in the process of evolution to make our hospital to a greater hospital. By that way, the issue with funding can also be addressed.
Our last week is going to be very short and fast since we are off till Tuesday. On Wednesday, it would be the last chance to add something to presentation as well as to the paper. Thursday is going to be a presentation day in the anesthesiology department, and that would also be the last day in the clinical setting. Finally, Friday would be the last day of the program, and that includes final presentation from each group and wrapping up the program.
Jonathan Rasio

Originally from the small town of Villers-Le-Temple, Belgium, Jonathan studied biochemistry and mathematics at the University of Illinois at Urbana-Champaign. His research primarily involved engineering protein-shell microspheres as contrast for OCT and targeted to atherosclerotic lesions. Before starting medical school, he worked on tobacco studies at the Centers for Disease Control and Prevention and completed a brief stint on the Ebola response at the height of the epidemic. Jonathan looks forward to working as part of an interdisciplinary team on developing cost-effective medical devices through IMED. In his free time, he enjoys rock climbing and hiking.
Jonathan Rasio Blog
Jonathan Rasio Blog
Wednesday, May 31st
Jonathan Rasio Blog
On our first day in the hospital we were given an introduction to cardiology by the head of the department, Dr. Darbar. I chose to do my rotation in cardiology for a number of reasons. I spent time during undergrad doing research in a lab that focused, among other things, on developing a catheter-based OCT system. This technique could provide an image of the cross section of a vessel with high resolution information several millimeters deep. I thought about my grandfather who suffered from a heart attack a few decades ago and needed to have a bypass surgery, a complicated and risky procedure. It became very clear to me that technology in cardiology is developing rapidly and more and more procedures on the heart are prevented by early intervention (thanks to imaging) or treated by catheters inserted in the femoral or radial artery. Dr. Darbar highlighted some of his research on atrial fibrillation and the newest technologies used in electrophysiology, a sub-specialty of cardiology dedicated to treating conditions affecting normal heart rhythm. These technologies include an atrial mapping device that can map in high resolution the anatomy of the atria and its electrical circuits so that ablation can be done with high precision.
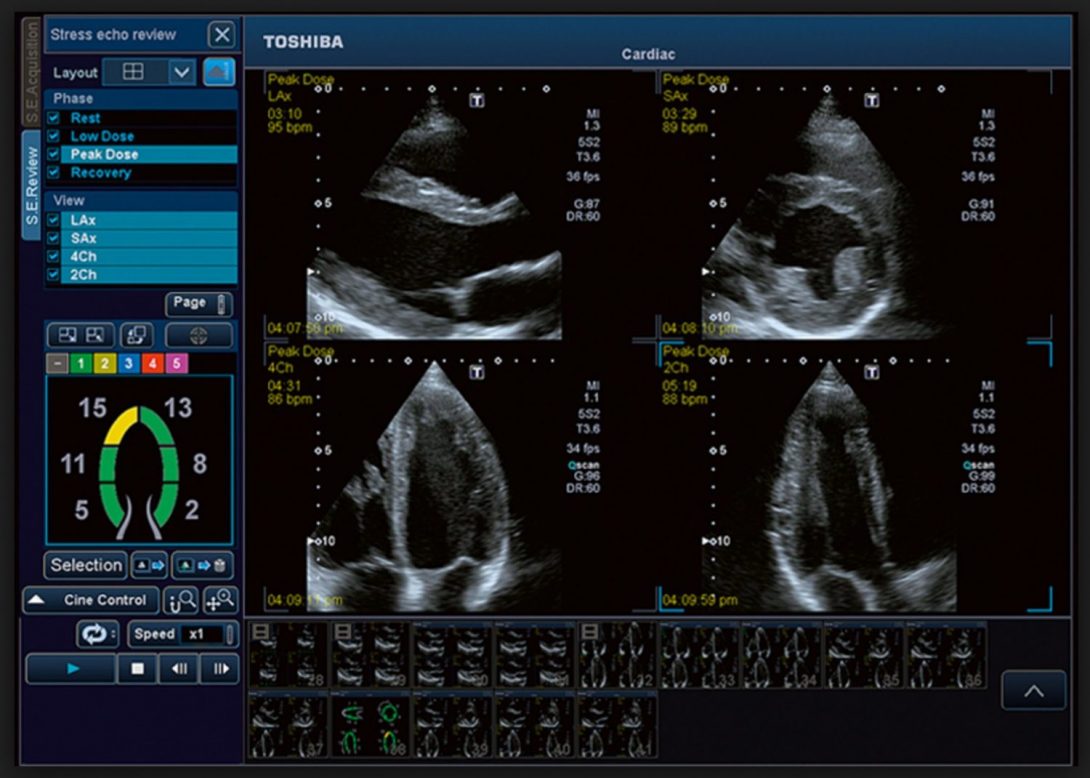
We then met with Dr. Gans in the echocardiography lab. We unfortunately did not have the opportunity to see the process of obtaining the echo on the patient. This is usually done by a technician and is routine. The technician places an ultrasound probe directly onto the chest of the patient and captures short videos of the heart at many different angles. Doppler images can also be obtained and show the direction of blood moving across the heart during systole and diastole. Dr. Gans was reading the echoes on a monitor and submitting a standardized note directly to the electronic medical record. Reading an echo study consists of looking at about 70-80 of these ultrasound videos at every imaginable angle to obtain an idea of the state of the heart and its valves. It can take anywhere from 2 minutes per echo for an simple study to 25 minutes per echo for a complicated study. He mentioned he typically reads echoes twice a week and gets through ~450 echoes per month.Echoes are ordered very regularly because they have cause almost zero harm to the patient and can reveal a large amount of information about the heart. Dr. Gans was able to assess the state of the atria, the mitral and tricuspid valves, the state of the ventricles, the volume of blood in the ventricles and atria, the quality of the interventricular septum and the pericardium, the ejection fraction (and thus contractility), the aortic and pulmonary valve, and much more. With regards to Doppler is was interesting to note that the software shows blood moving towards the probe as red and blood moving away from the probe as blue. This is in fact the reverse of the conventional red shift and blue shift for objects moving away and towards the probe, respectively. One cardiologist commented that this was the result of stupidity and nothing more… I cannot rationalize an explanation for why those colors might have been chosen, but everyone seems to have gotten used to it.
Friday, June 2nd
Jonathan Rasio Blog

The cath lab is the place of much innovation in cardiology. It is used to obtain imaging of the blood vessels of the heart such as the coronaries and tributaries, as well as repair blood vessels via catheters inserted into the femoral or radial artery. Unfortunately, because of Memorial Day weekend, many procedures were cancelled. This meant the cath lab was unused for many hours. This came off to me as rather wasteful given the very high cost of the equipment in the room. The operating table alone, which just pans in a circle and can go up and down, costs in the area of $250,000 to $350,000. The x-ray machine used for fluoroscopy can reach several million dollars. From a business perspective, this seems inefficient, not to mention that a team of highly skilled interventional cardiologist have little to do on those days. What surprised me was that the patient load for interventional cardiology procedures is actually increasing and more and more patients require stents and imaging procedures—I blame fast food restaurants.
I started thinking that there might be an easy way to develop a model that would predict the likelihood of a patient to cancel a procedure based on various variables such as previous record and demographics, as well as the procedure being performed. The program would then selectively overbook patients so that the cath lab is always used, similar to how the airline industry overbooks its flights. Shockingly, such a scheduling program does not yet seem to exist.
On Thursday and Friday, we got to observe a number of different procedures in the cath lab. Two of the three were rather short because the interventional cardiologist found no blockages in the arteries of the heart. This is very good news for the patient. In the third procedure, the interventional cardiologist found a number of blockages as a result of atherosclerosis necessitating placement of a couple of stents. The artery used for access is the subject of debate. Traditionally, the femoral artery is used. However, femoral access has worst outcomes, increased bleeding, and access site complications when compared to radial access. This is why UIC and most of Europe are almost entirely switched onto the radial approach. The femoral access site is still sterilized as a backup. The radial approach, however, has a high learning curve for physician trained on the femoral approach and is associated with a longer procedure and fluoroscopy time, with increased exposure to radiation. The radiation exposure is not much of an issue for the patient, but is concerning for the physician and staff who are exposed every day.
Another principle issue with the radial approach is comfort for the physician who has to access the right arm which sits 5 to 10 inches inferior to the femoral access site. To prep the arm of the patient for catheterization, a green plastic patient transfer board is inserted and secured underneath the mattress of the operating table on which the patient lies. The arm of the patient is then taped and secured to the board and the radial artery is available for catheterization. There then remains a moderate amount of real estate on the board adjacent to the legs to place instruments to control the catheter.
On the other hand :), when the physician has to access the left radial artery, he has to lean over the patient (who is often overweight or obese) to do the procedure. Although it may seem logical to simply do the procedure on the other side of the table, this is actually problematic because the physician would be turning his back to the monitors with the x-rays and vital information and the catheterization procedure would need to be performed with the physician’s left hand. Several different methods have been suggested to accommodate easier access to the left radial artery, each with their own problems.
Tuesday, June 6th
Jonathan Rasio Blog
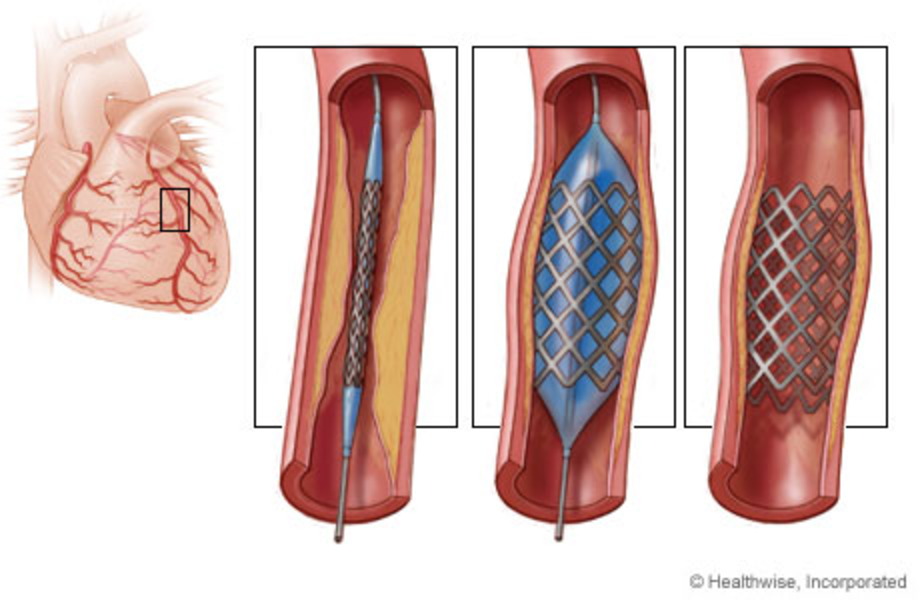
The heart muscle is supplied with blood by the right and left coronary arteries, which come off just superior to the aortic valve. The left coronary, also called the left main, gives off the left anterior descending (LAD) artery and the left circumflex (LCX). The LAD is the location of many blockages from atherosclerosis. This restricts oxygenated blood from reaching heart muscle and results in an infarction. This medical emergency is treated by an interventional cardiologist by expanding the artery with a stent.
We had the opportunity to scrub in for this procedure and got to see up close the many different types of catheters used during the procedure. One catheter is used to perform the angiogram where small amounts of contrast are released into the two coronaries and visualized by x-ray. This helps find the occlusions, which are clearly apparent. The imaging software has a large number of tools to precisely determine the degree of occlusion, but most often these are not used. Surgeons rely on experience to obtain ball-park estimates. This is where it really pays to spend time in a hospital before jumping in front of a computer to write code. Many tools exist in all these imaging software packages, but many don’t seem very useful.
After the angiogram is done, the image is saved on a different monitor and used as a guide. The x-ray is continuously used to detect the precise location of the various catheters. A different catheter containing the stent is then inserted into the radial artery. A stent is a small metallic meshwork tightly coiled around a small inflatable balloon. When the balloon is inflated with contrast (to visualize the location of the stent on x-ray so it can be placed precisely at the lesion), the stent is expanded and holds the artery open. It is worth noting that a stent can only be expanded and cannot collapse. Thus, it is crucial to not overshoot when inflating the balloon. A pressure monitor keeps track of the pressure of the balloon and a standard chart is used to determine the pressure needed for each stent size. When the balloon is inflated, blood flow is temporarily stopped which might result in some angina.
Given how often coronary angioplasties are performed, I was surprised to learn that stents are relatively new and date from the late 1980s. Since then, stents have been the subject of much innovation. One of the major complications from stents is the formation of a thrombus and so the market developed drug-eluting stents. An interesting and novel area of research is the use of bioresorbable stents. The vessel tends to heal itself after a few months, but the stent cannot be removed without a transplant. During this time, there is an increased risk of thrombosis and other possible complications including the formation of artifacts on CT scans. Bioresorbable stents are made of a polymer that gradually dissolves into a lactic acid, a normal metabolic product. Clinical studies are under way to determine if outcomes are actually improved.
Friday, June 9th
Jonathan Rasio Blog
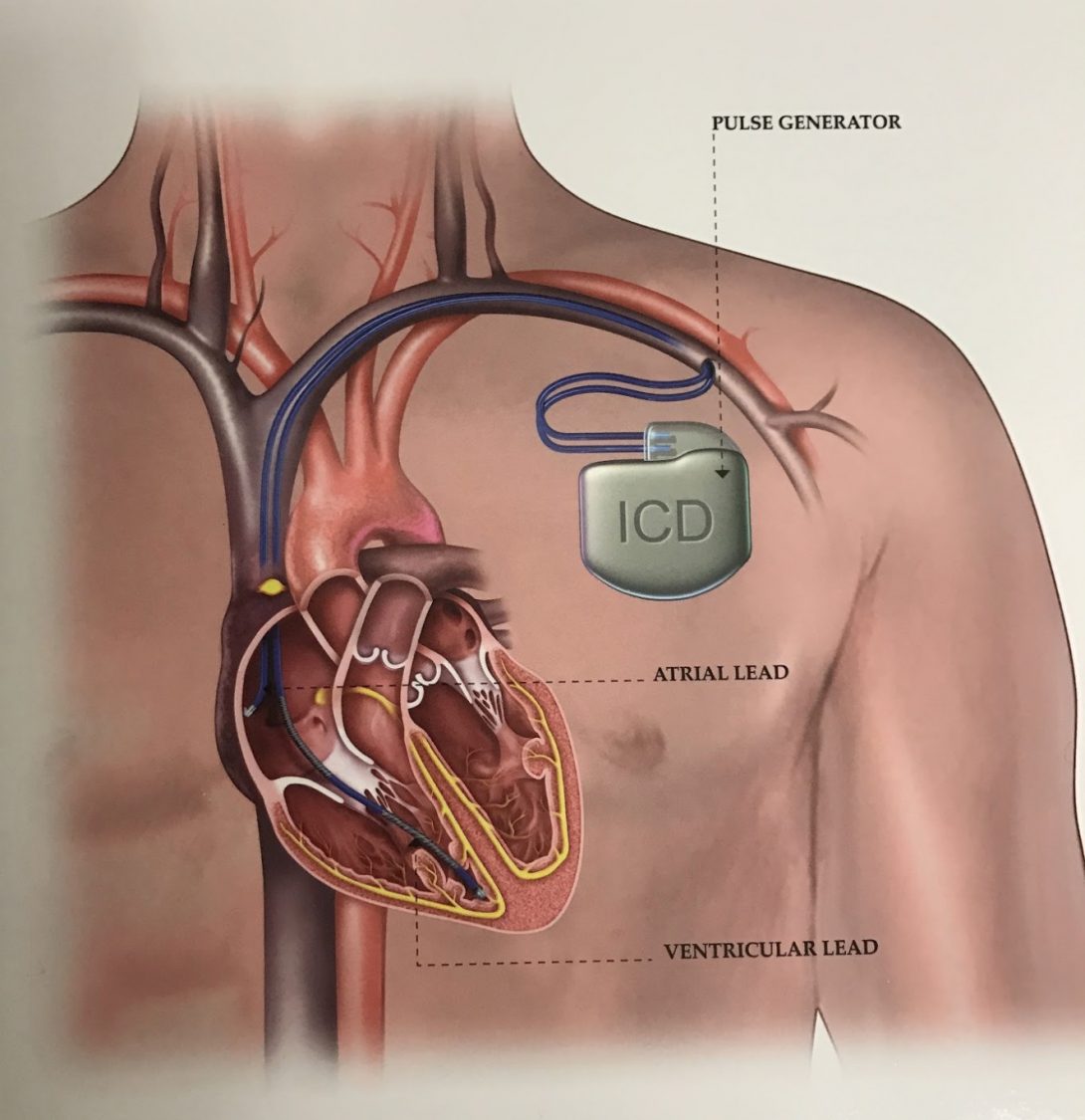
Cardiologist can often be divided into plumbers and electricians. The plumbers open up arteries and place stents while the electricians concern themselves with the electrical circuits in the heart. The electrophysiology lab is full of cutting-edge technology. One of the most common procedure performed is the implantation of a pacemaker (to control the pace of the heart) or an implantable cardioverter defibrillator (ICD) (to shock the heart out of arrhythmia). This week, we were able to see the implantation of an ICD, follow up with the patient in the hospital the next day, and then discuss remote monitoring with patients at the out-patient clinic.
The procedure for placing a permanent pacemaker/ICD has become streamlined given the large number of cases in the US. An incision is made over ~5cm on the chest inferior to the clavicle, cautery is used to stop bleeding, and the pectoralis major muscle is identified. The leads that monitor rhythm and shock the heart are placed into the subclavian vein and screwed into the heart muscle in either the right atria, right ventricle, or both. The ICD was then inserted deep to the muscle. Best practice is to tie the ICD to the pectoralis major with non-dissolvable sutures to prevent the device from migrating downwards overtime. This would otherwise requires another surgery to retrieve the device. During the procedure, the impedance of the leads is constantly monitored. This can tell you two things about the integrity of the leads. If the impedance suddenly goes up, the lead was probably fractured. If the impedance suddenly goes down, the insulation of the lead was compromised and a short circuit was created.
Interestingly, the left heart is not used because of risk of stroke. In the right heart, blood flows from the right atria to the right ventricle then through the pulmonary artery to the lungs. A clot formed along the leads would get stuck in the lung and result in a pulmonary embolism. In the left heart, blood flows from the left atria to the left ventricle then through the ascending aorta. Blood can then flow directly to the brain by way of the common carotid. While a pulmonary embolus can have a bad outcome for sure, a stroke can cause permanent and severe damage.
When we followed up with the patient the next day, I was amazed at the small size of the incision. While sutures were visible they weren’t very noticeable and the lesion will probably scar nicely. The ICD, however, could be seen edging through the chest and may be a little uncomfortable. Unfortunately, I did not have a chance to ask the patient. The purpose of following up was to change the dressing and check for infections. The patient was told not to lift his arms too high for a few months so that scar tissue has time to form around the leads in the heart. A brisk movement of the shoulder can cause the leads to be disconnected, which would require another surgery.
In the device clinic, a nurse practitioner was interrogating the pacemakers of patients. A “wand” is placed around the patients neck and sits on top of the pacemaker. This allows the provider to wirelessly obtain information about the device, such as the serial number, battery life, and EKGs of possible events. The battery life is usually <10 years and cannot be charged by induction. When the life of the battery reaches an end, the pacemaker has to be replaced. The provider can also make changes to the settings of the device. Each company of pacemakers has their own set of equipment.
Patients at the device clinic are also counseled about remote monitoring options. Patients who consent are sent a wireless recording device that plugs into a phone jack in their bedroom. This records information from the pacemaker when they sleep and sends it over to a secure server. The provider can then log into the company’s software and see information about their patient’s health. If alarms go off, the provider is contacted and they can call the patient to schedule an appointment or send an ambulance. Again, each company has their own software and it can be difficult to find what you need. It seems that there is need for a standardized monitoring platform. Unfortunately, it would be difficult to sign on profit-driven companies.
Tuesday, June 13th
Jonathan Rasio Blog
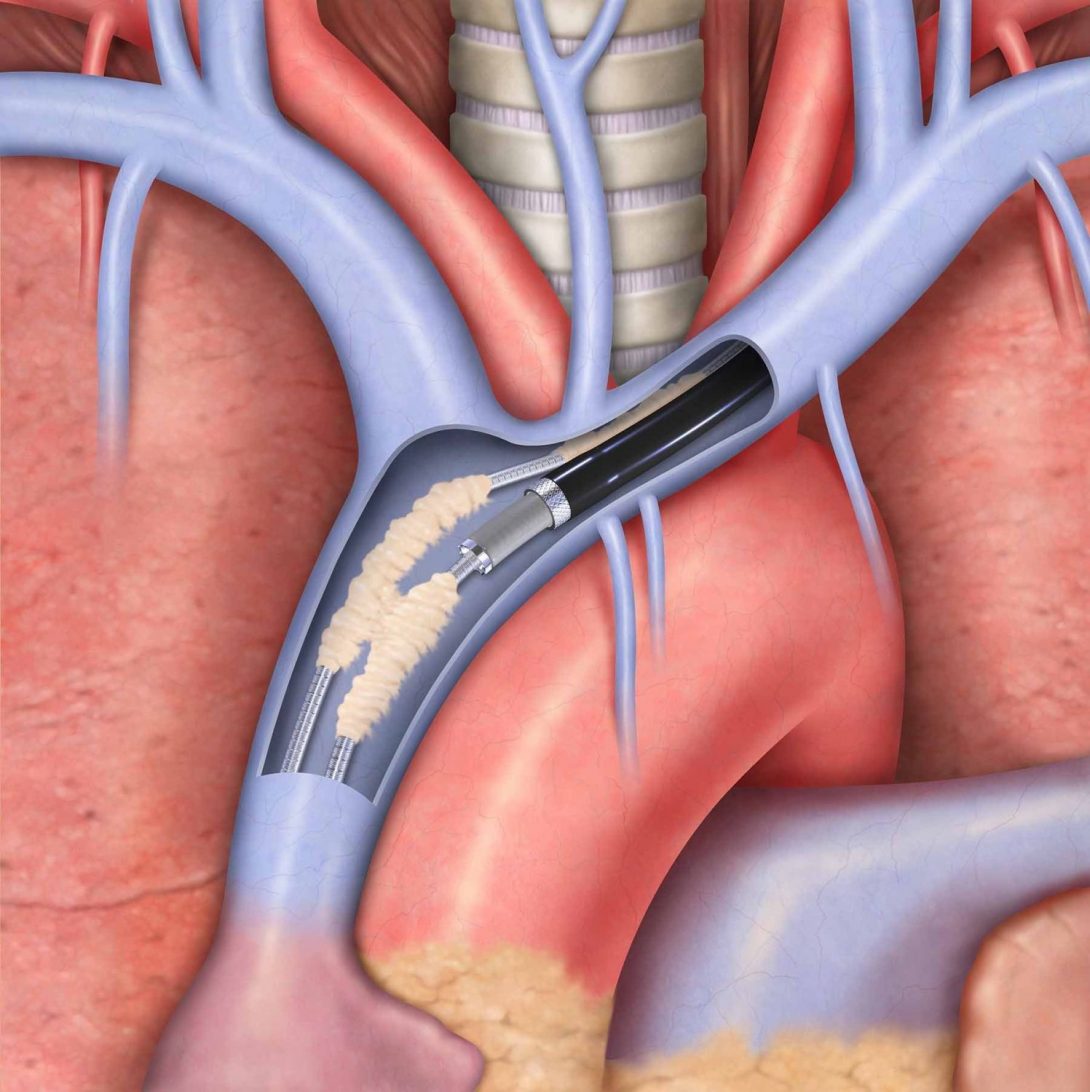
Recently, the FDA issued a recall of the St. Jude Medical Implantable Cardiac Defibrillator (ICD) and Cardiac Resynchronization Therapy Defibrillator (CRT-D). These devices are necessary to monitor the heart of some patients for dangerous or fast rhythms and then shock the heart if necessary. The recall was issued because of a significant defect in the battery of the devices causing them to run out before they could be replaced, which resulted in some deaths. The problem is that some 200,000 of these devices have already been implanted and will need to be serviced.
There are several reasons that a pacemaker needs to be removed. A recall is definitely a major reason. In addition, the pacemaker/leads can result in infections, the pacemaker may be out of battery and need to be replaced, and the leads may fracture or the insulation may become compromised. In any case, removing the leads from the heart wall is a difficult affair. Fibrous tissue builds up over time around the lead, anchoring the lead to the intima of the subclavian vein and endocardium. To remove the leads, the operator has to cut through this scar tissue in order to liberate the lead. There is a major risk during the procedure that the operator will accidentally puncture the subclavian. This would result in massive bleeding and death within minutes. A cardiothoracic surgeon is thus present for the procedure to immediately intervene if this unfortunate situation were to happen. The volume of lead extraction is such that UIC built a special operating room for this purpose: a hybrid operating room that can serve both as a minimally invasive catheterization lab and a cardiac operating room for open heart surgery.
The method for liberating a lead from scar tissue in the vessel and heart involves advancing a laser sheath around the lead. The company Spectranetics, who manufactures the laser, sent a technician to the OR to assist with any technical issues with the laser during the procedure. The necessity of a company technician in the OR seems to be a trend with many of the newer surgical and imaging technologies. The laser sheath is advanced along the lead slowly while the operator pulls on the lead to create tension. This helps avoid cutting through the subclavian vein. While the laser has helped a lot with regards to safety and time, this procedure is sometimes still performed mechanically where the scar tissue is cut manually. The mechanical technique takes much longer to perform and is much less successful. The cost, however, is about $2000 less for the non-laser extraction.
I was interested to later learn that operators who perform lead extractions tend to favor a different type of lead when installing an ICD. Most ICD leads are manufactured with either a single right ventricular coil or dual superior vena cava and right ventricular coils. The coils tend to result in the formation of more scar tissue and make extraction more difficult. Thus, single coil extractions are much simpler than dual coil extractions. The dual coil lead was initially preferred due to concerns over failure to defibrillate. In addition, the dual coil may also be slightly more efficient. However, the difference in clinical outcomes between single coil and dual coil ICD leads is still unclear. Hence, operators who perform ICD lead extraction now tend to install single coil leads over dual coil.
Wednesday, July 5th
Jonathan Rasio Blog
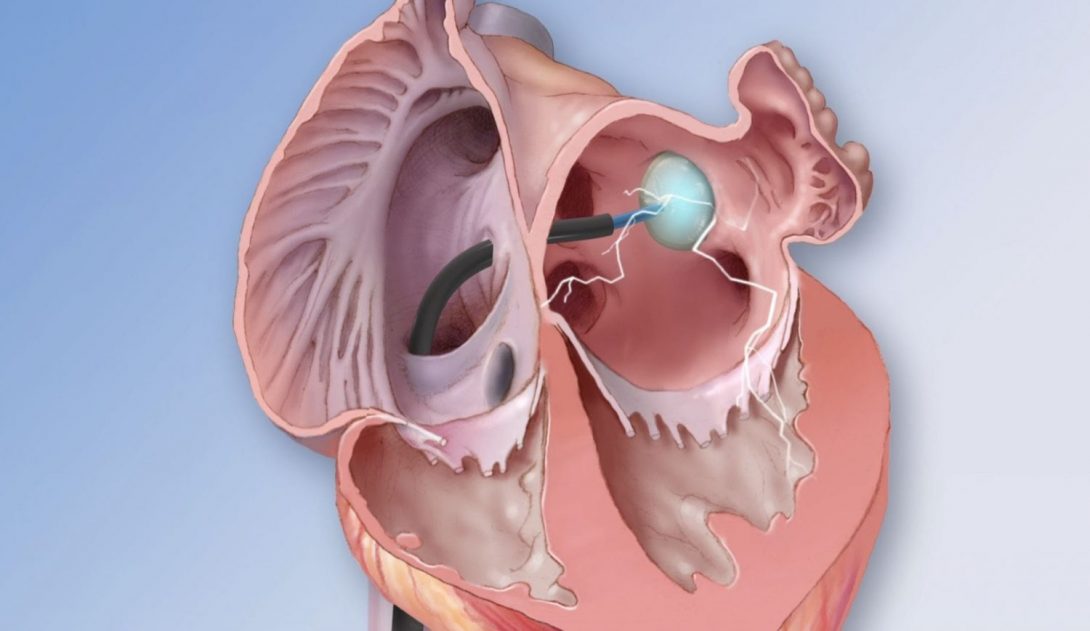
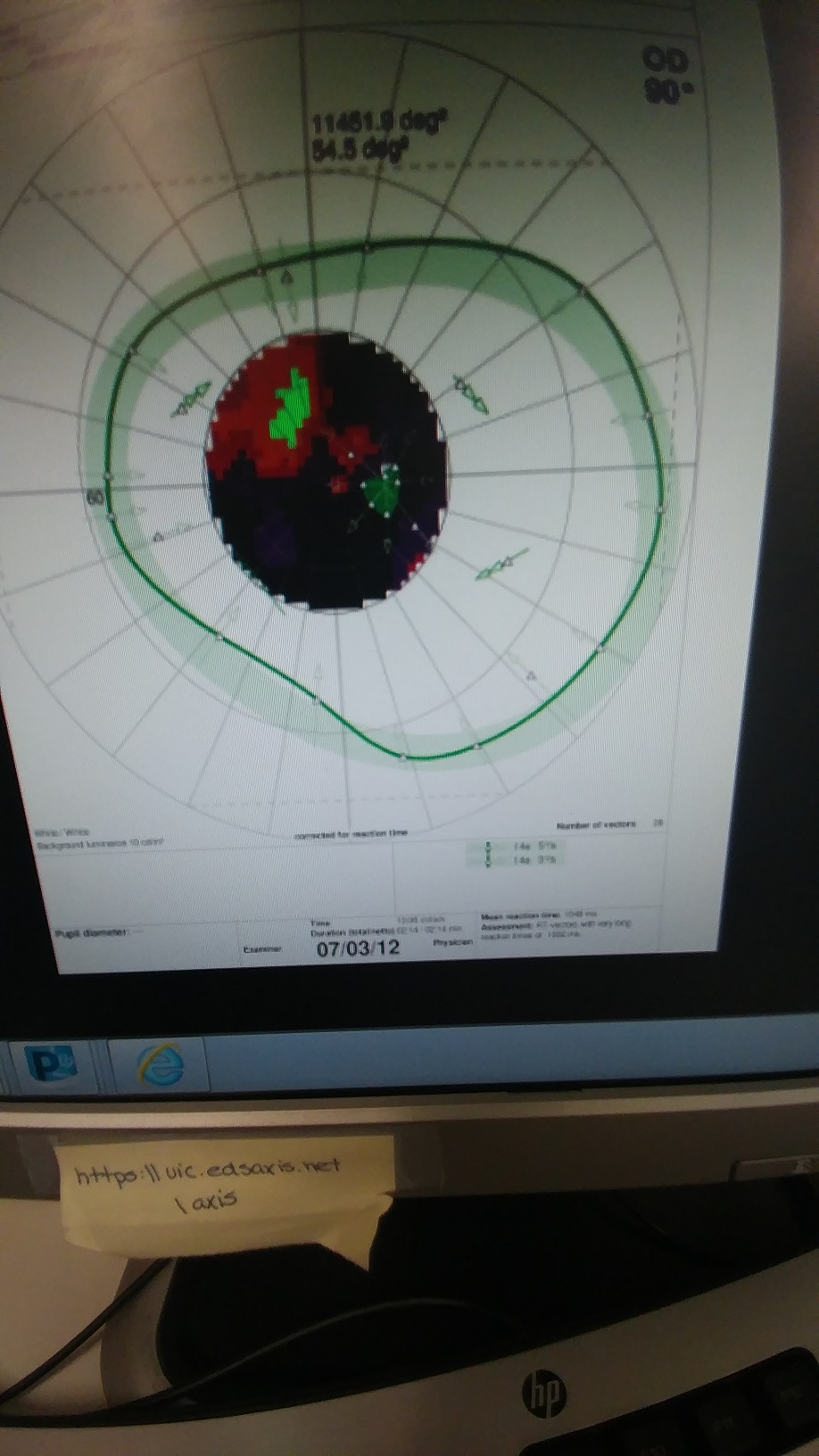
Ablations are a major component of electrophysiology. During the procedure, a catheter is introduced trans-septally to burn off a small section of the left atria and short-circuit the aberrant electrical signal in patients with atrial fibrillation, atrial flutter, or Wolff-Parkinson-White syndrome. We had the chance to observe several different ablation techniques and they each have their own advantages and disadvantages. Generally, a detailed electrical and anatomical map of the atria must first be generated. A special catheter containing a series of electrodes is introduced and moved across the entire atria, including sections of the pulmonary veins. The catheter is tracked magnetically and the “GPS” information is used to generate the anatomical map. At the same time, the electrodes capture the electrical activity of the atria to generate the electrical map. This is used to pinpoint the location needing ablation. The process of generating the map is complex and the software is complicated. Each ablation company employs representatives to cover a territory and have to assist in creating the map on all ablation procedures. However, it seems that doctors would rather be able to process the map themselves and not deal with hassle of coordinating with the different companies.
The actual ablation can be done using several types of energies. We observed ablations with RF energy, cryo energy, and lasers. RF ablation is the oldest technology and involves inducing an RF signal at the tip of the catheter for about 40 seconds to heat up and destroy a small dot of tissue. The utility of RF ablations is only as good as the operator’s ability to get one dot next to another dot. If there is a gap between two ablation dots, the aberrant electrical signal may still be generated. Precision is thus very important and the procedure is typically long. However, the technique is very useful in the sense that it provides the flexibility to burn off either a line in the atria, a very specific section (as would be needed in WPW), or isolate pulmonary veins.
Cryo and laser ablations have a different approach. The techniques seem to be much quicker and very effective. However, they are less precise and flexible in their applications. Typically, in patients with atrial fibrillation, the aberrant signal is generated at the pulmonary veins and so the outline of all four pulmonary veins is often ablated. In cryo and laser ablations, the catheter is introduced into the pulmonary vein and fluid is injected to blow up a balloon. The balloon temporarily occludes blood flow into the atria and places the balloon in full contact with the intima of the vein. In cryo, cold energy ablates the whole surface of the vein at once. On the other hand, in laser ablations, a laser covering a sector is moved circumferentially to ablate sections of the vein. Both techniques are significantly faster than RF. However, with the laser, the operator must take care to not ablate in a spiral as he goes around the vein. To avoid this, they typically finish each vein isolation by ablating at several locations along the z-axis. I was surprised to see the small sector size in the laser ablation. A larger sector would allow for a quicker ablation since fewer points would be needed to isolate the pulmonary veins. I was informed that such a catheter is currently being designed by Cryofocus and is being tested on animals with promising results.
Faster ablations are a huge deal for electrophysiology since ablation procedures can be very long and require a lot of staff, which is expensive and tiring (especially when wearing all that lead to protect against radiation). Atrial fibrillation is also becoming very prevalent and the market for ablation is expanding. Finding ways to reduce the EP lab time would allow for more procedure to be performed.
Shouvik Sarkar

I am a senior bioengineering student who has a sincere interest in regenerative medicine. I am very excited to be in the crossroads of engineering and medicine through clinical immersion. From this experience, I hope to develop a knack of bioinstrumentation development.
Shouvik Sarkar Blog
Shouvik Sarkar Blog
5/31- Rotation Commencement
Shouvik Sarkar Blog

On the first morning of our clinical rotation, the four of us were told to meet at the radiology admittance center, where outpatients can sign in to get services performed. Medical professionals escort patients into the specific branch of radiology that can provide help. In our nonpatient scenario, we were escorted by Dr. Bui to the interventional radiology lab, an area that houses several medical professionals and students. The first thing that captured my attention in this area was the size (or lack thereof). The hallways are severely cramped, especially with the addition of four clinical immersion participants. I reckon the medical professionals are perpetually careful to prevent collisions.
The first procedure we witnessed was a paracentesis, which involves draining excess fluid in the abdominal cavity. The fluid buildup, known as ascites, is relatively simple to remove by using ultrasound when the fluid is not loculated, or divided into small cavities. I noticed that the fluid was collected in a Baxter-manufactured jar so that it can be tested. Next, we observed the placement of a nephroureterostomy tube in a patient so that her kidney stones can be removed. This is a pre-surgery procedure done to guide a urologist to the kidney stone(s) for a quick and straightforward operation. One memorable issue I witnessed during this procedure was the interference due to the radiographic imaging equipment. Dr. Bui kept bumping into the unit, and this can pose a safety risk to both the doctor and patient.
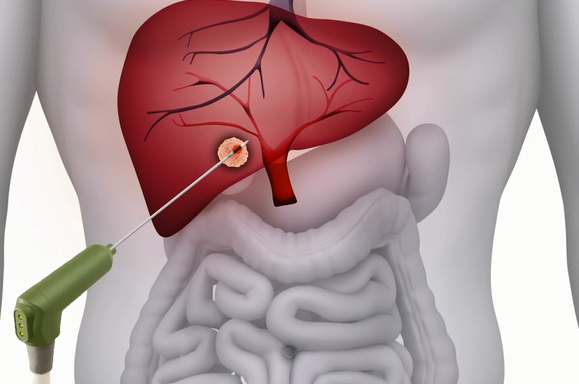
Another procedure we saw today was an ultrasound-guided renal biopsy. This procedure requires a special type of needle that can pierce through renal tissue and capture blocks. An image of this device is shown; it requires two hands to operate because of the “pumping” function. The trigger must be cocked so it has the potential to pierce through tissue. Albeit intuitive, this device is difficult to use when one hand is occupied. An image of this device is shown below:
6/2- Week 1 Conclusion
Shouvik Sarkar Blog
Thursday was an early day for all of us, as we attended a multidisciplinary tumor conference at 7am. Although this meeting was more medicine-related than engineering, I learned several new radiology terms. Ablation, or tissue removal, can be used in conjunction with radiology to heat certain nerves and thus interrupt pain signals to the brain. Some other terms I learned are fibroid and solitary adrenal metastasis. In attendance at this meeting was the Vice President for research at the University of Illinois system. We were told that he also has a background in engineering, so it might be worthwhile to discuss potential improvements to medical devices in the future.
As for procedures, we witnessed chemoembolization for carcinoma in the liver. In addition to this, we also witnessed more biopsies; however, they were in different organs. Thus, the tip of the needle used in the procedure was slightly different from the one that was used in the renal biopsy. Dr. Bui told us that the reason for this is the difference in morphology between the tissues. At this point, we were also introduced to the unique identifying property of these needles- their gauge size. The gauge size is synonymous to the diameter of the needle, and it makes sense why different tissues may require differing gauges. A few other procedures we witnessed were the conversion of a nephroureterostomy tube to ureteral stent and gastrostomy tube placement using ultrasound.
Another clinical issue that was identified relates to scheduling and orders. A stable, interventional radiology patient was under the assumption that her order for a thyroid biopsy was placed and that she’d have the procedure done on Friday, but the system did not let the schedulers know that she needed genomics done with this order. In the order-placing GUI, there is no differentiation between a simple biopsy and a biopsy with genomics, so confusion is impending.
During our downtime, I explored the interventional radiology department to get a better sense of the rooms. The layout of the operating rooms is advantageous to the patient and healthcare provider due to the isolation. These rooms are between the major hallway of the hospital and the doctors’ desks. This allows patients enter the room through the outside hallway, and doctors can see the patient’s medical history on the computer (located adjacent to the OR). A sketch of this layout is shown below.
6/7- Week 2 (Biopsies and Embolization)
Shouvik Sarkar Blog
Many clinical practices were observed during the second week of clinical rotations. We witnessed a liver biopsy and learned about several other methods of tissue retrieval. Three major ways of obtaining hepatic tissue exist- transjugular liver biopsy, percutaneous biopsy, and operation. The transjugular method is what interventional radiology uses to obtain samples and requires incising the neck. The percutaneous liver biopsy can be done in two ways- ultrasound guided to determine where the liver lies and landmark to approximate the anatomical placement of the liver- and requires a slightly more invasive procedure. Lastly, the operative procedure involves surgical removal of hepatic tissue and therefore is the most invasive for testing cytotoxicity. In addition, Dr. Bui showed us images of epithelioid hemangioendothelioma, a rare type of tumor that has relapsed in the patient in question.
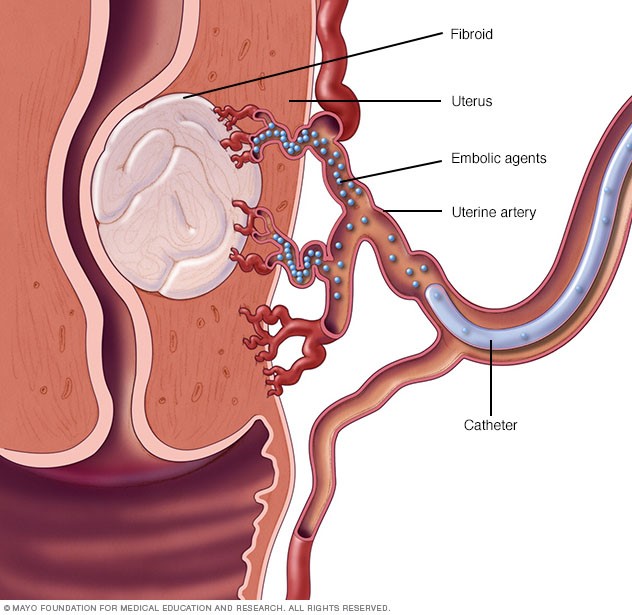
The following day was an eye-opener in which we saw a variety of cases ranging from uterine fibroids to dialysis catheter insertions. A woman was admitted due to adenomyosis, a condition in which endometrial tissue grows in the uterine wall. To combat this discomfort and prevent further tissue growth, embolization (creation of artificial clot) was performed. Bilateral uterine embolization is the placement of synthetic materials to block and therefore constrict blood flow to tumors in the uterus. This method is less invasive than open surgery and an effective way to prevent unwanted tissue growth. Dr. Lipnik performed the procedure by first inserting a femoral catheter and then injecting a drug comprised of 500-micron beads to close off the capillaries. Following the procedure, the team of doctors tested the effectiveness of the closure by injecting a dye and viewing its flow under fluoroscopy.
I’m curious as to how we can improve the process of drug delivery to treat oncologic cases. Currently, the process is relatively straightforward for physicians and patients, as local anesthesia is used to numb the area around the incision for the outpatient procedure. However, the design of the beads can be better in my opinion. Per the attending physician, the drug is designed to stay in the capillaries for a lifetime, but they can be dislodged or travel farther into the vessel. Also, there could be ways to target malignant tumors using specific drug delivery through the beads. A studytesting the efficacy for drug-eluting beads in liver embolization was performed in which significant cytotoxic effects were observed by increasing the concentration of doxorubicin. Although fibroids are benign, reliable drug-administering beads can be used to fight malignant complications.
6/9- Week 2 (Devices)
Shouvik Sarkar Blog
It’s amazing how interventional radiologists can treat seemingly major complications through a simple incision distant from the affected organ. Obviously, none of this would be possible without state-of-the-art medical devices.
Each operating room in the interventional radiology branch is fitted with large and expensive radiographic imagery equipment. However, even these fancy machines are responsible for complications. For example, miscues in communication may occur as nurses serve as the middlemen between doctors and the fluoroscopy machine. This is done to prevent contamination and maintain a clean work environment. Doctors can ask the RNs to take a burst of images, and the settings must often be calibrated for each specific case. Unless the physician performing the procedure is crystal clear with directions, there may be problems in imaging. In addition, the GUI for the fluoroscopy machines was acting up, and I overheard a nurse say that Siemens must look at the problem the next time they provide service.
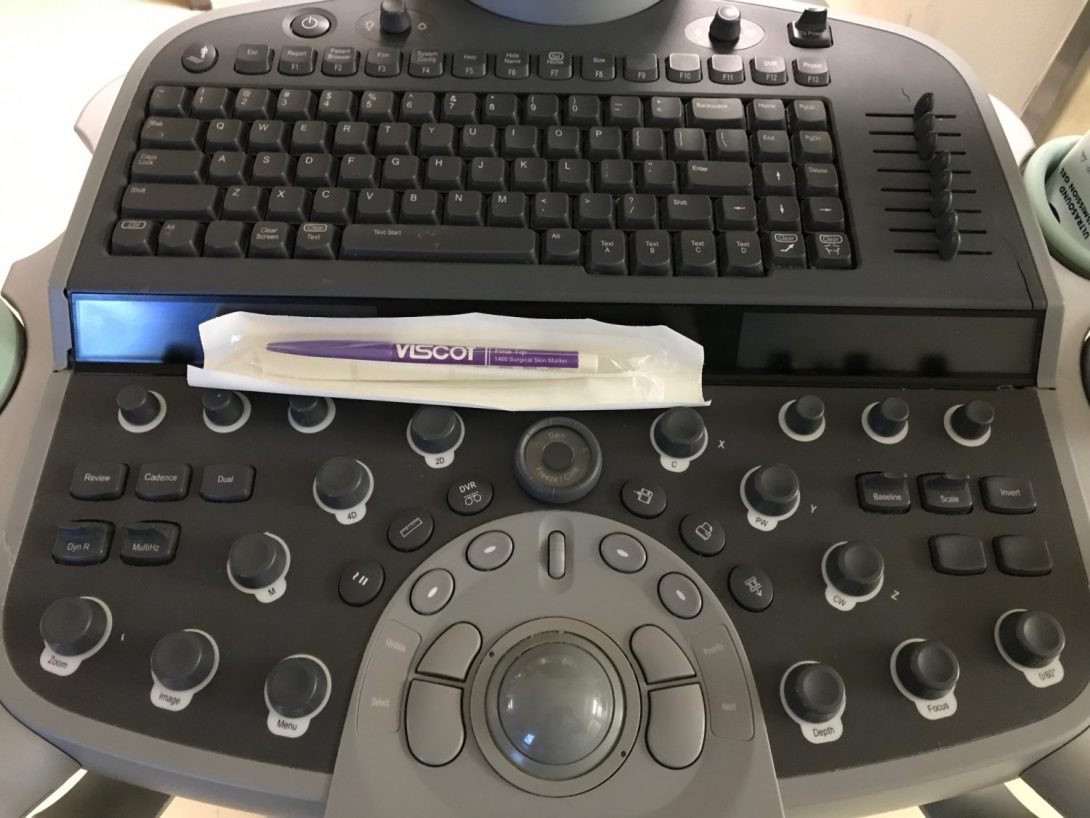
Another ubiquitous machine in IR is the ultrasound imager. This is predominantly used as a landmark device that helps guide physicians to the correct incision area. For instance, this machine is used to help show where abdominal fluid is located in the case of ascites so that paracentesis can be performed. Despite its vast uses, the ultrasound machine has a few shortcomings. First, its limited gray scale makes it difficult for doctors to see exactly where their needle is located despite its echogenicity. Also, I’ve noticed that nurses prepare the machine before every patient using a baggy plastic wrap over the entire display/interface, making it a struggle to press the correct button and consequently increasing the chances of a mistake. I suppose a tighter and easier-to-use wrap can be designed to fit the machine (based on its size specifications).
(Pictured- Ultrasound Machine Buttons)
6/14- Week 3 (Radioembolization)
Shouvik Sarkar Blog

Week 3 of shadowing introduced us to several new procedures including oncologic treatment as well as novel devices. An interesting case we witnessed was radioembolization of a hepatic tumor, which utilizes radioactive decay inside the body to prevent uncontrolled growth. To this end, an isotope of Yttrium, Y-90, was injected intravascularly to not only thrombus the tumor but also to pathologically deter the metastatic tissue from reproducing. The isotope has a half-life of approximately 64 hours, so it is relatively stable for use in patients. The decay is given by the following process:
Y90->B Zr90
This is different from chemoembolization since that disperses cancer-demoting agents in chemical form (hence “chemo”). Radioembolization similarly incorporates embolization (formation of an embolus, or blood clot) but by using a different form of drug: Y-90. Due to the radioactive nature of the drug, a health physicist and her isolation cube (pictured) were in attendance during the procedure to ensure the safety of health professionals.
Although I was under the impression that using radioactive decay is a surefire way to destroy tumors, I continued to be skeptical. A question I had for Dr. Gaba was regarding the [safe] handling of the radioactive material. Throughout the course of our time in IR, I’ve noticed that nurses and most doctors take utmost precaution around radiation by increasing distance, decreasing exposure time, and wearing lead vests. How is it possible that a health physicist and a fancy cube can keep everyone in the room safe? The solution (minimizing Y-90 exposure) is far from perfect and can be improved. A tubing system that doesn’t require doctors to touch the radioactive material is an effective technique, but the additional attendance of a physicist can translate to extra time and money. Nonetheless, the process of checking out, in which our radiation levels were tested before we left the operating room, was neat.
6/16- Week 3 (Carotid Case)
Shouvik Sarkar Blog
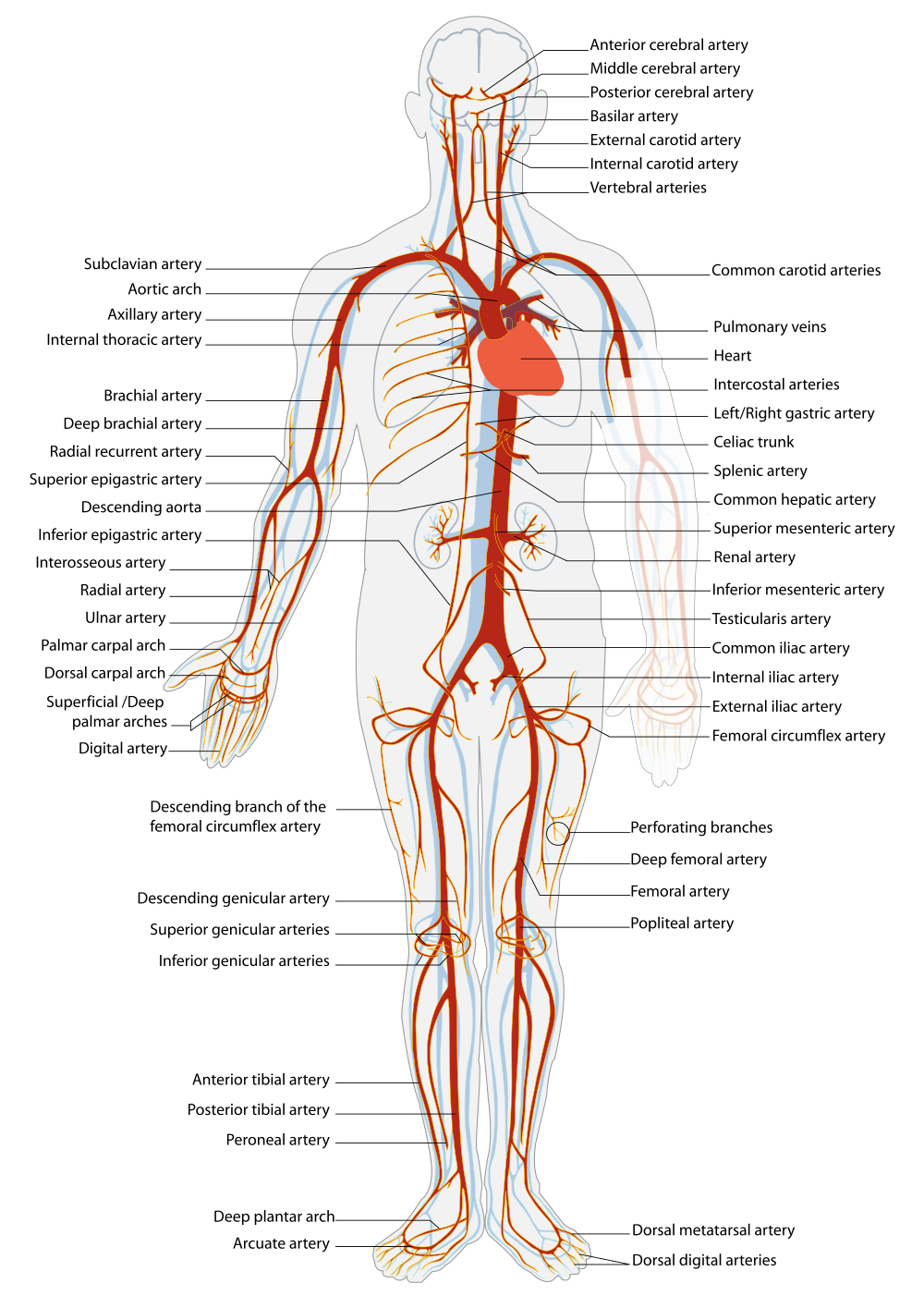
The latter half of week three provided us with a glimpse of one of the most interesting cases in our rotation. A man with a large tumor in his neck was at risk of a carotid blowout. Since the carotid arteries provide oxygenated blood to both the head and neck, a blowout will surely be fatal. According to Dr. Bui, the best solution to this problem is to deploy a stent to prevent the tumor from constricting the vessel. To this end, catheters were inserted through the femoral artery and driven upstream to the aorta. At the aortic arch, the angle to get into the carotid was extremely minute, and due to the degrees of freedom limitation of the catheter as well as scarring from repeated trials, the operation had to be stopped. Nonetheless, this was a fascinating case to illustrate the cyclical nature of the arteriovenous system (pictured). It’s amazing to me how a catheter inserted in the femoral artery can theoretically make its way through the iliac into the aortic arch and subsequently into the carotid.
The second half of the day consisted of a discussion of interventional devices such as the fast lidocaine injector. Lidocaine, in addition to treating arrhythmia, is used by radiologists to numb the skin around where an incision is to be made. This allows them to perform somewhat invasive procedures (eg. chest port insertion) without the need for complete sedation. The fast lidocaine injector does exactly what its name suggests, but it comes with a major drawback: since the injection is hurried, air can travel percutaneously in addition to the drug posing a hazard to a patient. Regardless, physicians use this tool when performing relatively noninvasive procedures near joints. In addition, we were able to play with different types of catheters.
6/20- Week 4 (Microwave Ablation)
Shouvik Sarkar Blog
The fourth week of clinical immersion introduced us to a novel form of therapy used to combat tumors. Arguably the most modern method observed throughout the program, microwave ablation was used to ablate hepatocellular tissue. A probe was inserted percutaneously to access the liver using CT-guidance. Due to the heightened dose of radiation emitted by the CT machine, most health professionals stand outside the operating room during the scan. One slight issue I noticed, despite being somewhat unrelated to interventional radiology, was the anesthesiologist’s need to constantly enter the CT room to perform sedation-related tasks. For example, the radiologist wanted apnea for a few of the runs, and the anesthesiologist often found herself in the room adjusting breathing settings while the CT machine was initializing. Long-term health may be compromised with lengthened exposure to ionizing radiation, so it’d be a wise choice to wear lead or have a type of anesthesia machine that can be controlled from an external environment.
Administration of the microwaves was safely done with the guidance of a representative from the manufacturer. Erin, a rep from NeuWave Medical, helped Dr. Gaba decide exactly which product to use and the duration of the radiation dose. The microwaves are supposed to destroy cancerous tissue that may or may not be malignant. Once the locations of the hepatic tumors were pinpointed using a needle and CT, the microwaves were administered for a few minutes (modeled using the image).
Since the patient was under general anesthesia (unlike most radiologic procedures), he was not able to view the procedure. We were told that upon waking up, the patient would experience a pain analogous to a punch in the gut, a minuscule price to pay for a high success rate of tumor ablation.
(Image Source- http://www.neuwavemedical.com/images/PRthumbnail.png)
6/22- Week 4 (Bovine Thrombin)
Shouvik Sarkar Blog

During the weekly tumor board, we were able to witness the challenges of medicine with respect to its interdisciplinary nature. A case that was originally diagnosed as metastatic lung cancer that had spread to the liver to become hepatocellular carcinoma (HCC) by radiologists was determined by pathologists to be hepatocellular adenoma. Such a misdiagnosis can lead to ineffective therapy and unwanted progression of disease. Radiologists were predominantly looking at the behavior of the tumor as opposed to the morphology of cells, and this clearly pointed to carcinoma. For example, simply looking at the cellular proliferation would point to carcinoma due to the increased mitosis compared to adenoma. On the other hand, path was looking at markers such as beta-catenin to analyze carcinogenesis. Regardless, this snafu was not extremely concerning since the life-limiting factor in this patient was the lung cancer.
While looking at cases with Dr. Bui using the picture archiving and communication system (PACS), a thrombosis case caught my attention. In this scenario, a patient suffered a ballooning of a blood vessel, colloquially known as an aneurysm, in his leg. Due to the weakened blood vessel wall, the size of the balloon was rapidly increasing and thus heightening the risk of a catastrophic rupture. Apparently, the therapy in this case was to use bovine thrombin to create a clot and prevent blood from expanding the balloon. The outcome of this strange case was extremely positive, as doctors were able to thrombose within minutes.
6/28- Week 5 (Varicose Veins Sclerotherapy)
Shouvik Sarkar Blog
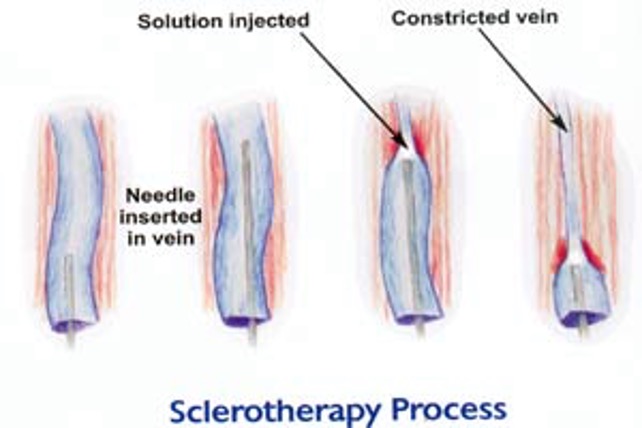
The beginning of this week again provided students with the opportunity to view unique cases. One fascinating case that the BIOE students watched was a varicose veins sclerotherapy. Sclerotherapy is a procedure that eliminates varicose veins, which form when the valves within veins fail by allowing blood to flow bidirectionally. This causes blood to pool, increasing the vessel diameter and occasionally resulting in discomfort. The sclerotherapy was administered using a laser to collapse the vessel. Like other procedures, all the materials required for this intervention were placed in the operating room by nurses; however, the laser administration was not tested (or turned on for that matter). Following the administration of the lidocaine/epinephrine buffer in the vein (precursor to laser therapy), the clinicians attempted to power the laser supply. Unsurprisingly, there were technical difficulties, as the nurse who had used the power supply previously tried to tinker with the fuse and consequently reassembled it incorrectly. It took the nurses approximately twenty valuable minutes to fix the power supply before the procedure could safely resume. Nonetheless, seeing the laser was eye-opening. Everyone in the OR had to wear special eyewear to protect their retinas.
In addition, a patient was admitted for a TIPS revision. The original TIPS had complications bypassing the liver, and thus the stent length had been increased. However, there was thrombosis that was occurring at the start of the shunt. The attending physician inserted thrombolytic material to the beginning of the shunt to allow blood flow. Lastly, we witnessed another uterine fibroid embolization. We were told that the catheter used to inject embospheres had suffered a kink and thus had to be replaced during the procedure. Problems like these are very important to the bioengineering students, as they will be the ones at the forefront position to improve devices.
6/30- Week 5 (UreSil Presentation)
Shouvik Sarkar Blog
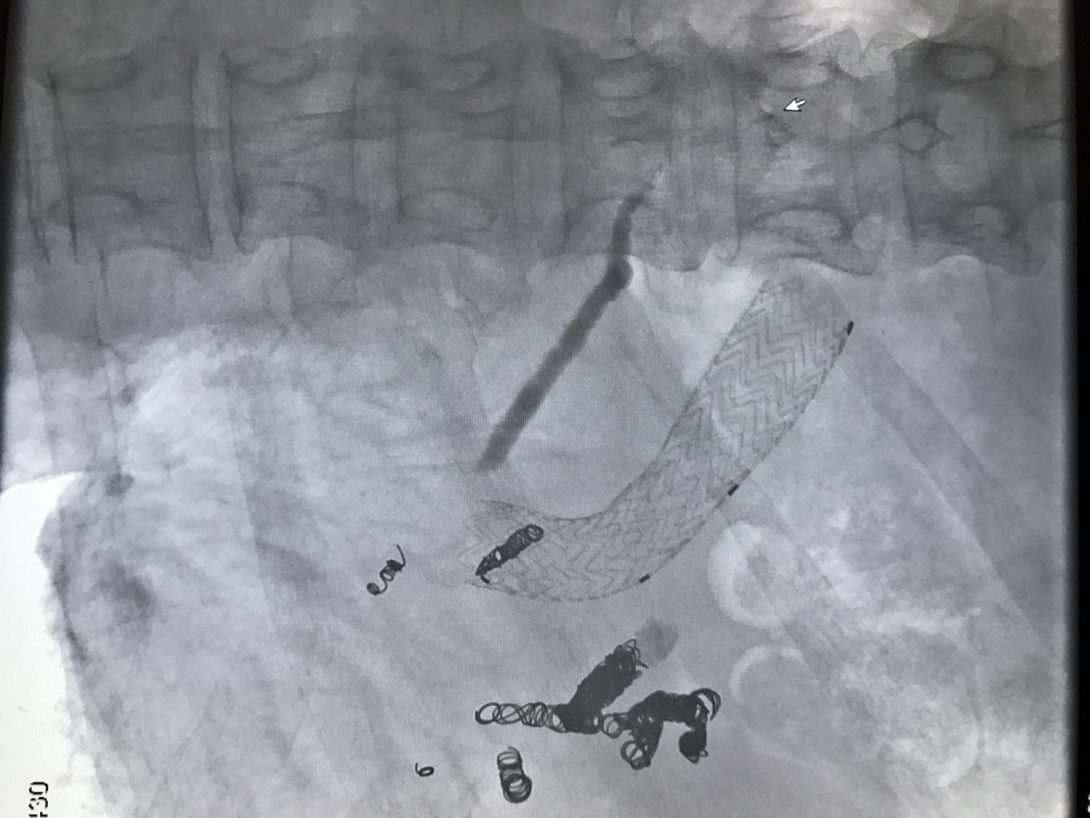
At this week’s IDP meeting, doctors discussed potential cholecystectomy and hepatectomy for a few patients. In addition, I learned about a splenorenal shunt, an abnormal collateral communication between the splenic vein and left renal vein, resulting in portal hypertension. Also, I learned about the bleeding risks of vastin, a drug that decreases cholesterol/triglyceride (statin) to prevent atherosclerosis from progressing.
As far as cases go, we saw a mesenteric angiogram, uterine fibroid embolization, and an IVC filter removal. The angiogram allows radiologists to understand the anatomy of a person’s arteriovenous system, allowing for effective therapy in the future. In this case, the patient had a malignancy in the liver which physicians had strategized to target with Y-90 radiotherapy; however, the angiogram revealed that a capillary that leads to the stomach must be blocked off to prevent Y-90 from reaching there.
Furthermore, we witnessed a hepatic artery embolization that was performed to treat an aneurysm. Another patient was seen in the emergency room, as he had suffered renal bleeding and was in extreme pain. One observation noted from this case was that it took Dr. Bui a few minutes to find the emergency medicine physician assigned to that patient, as if the ER is not already one of the most chaotic places in a hospital. Another fascinating case was the recanalization of the Fallopian tubes, which was done to re-enable reproductive function in a young patient. In addition, a TIPS reduction (pictured) was performed to treat encephalopathy resulting from too much bypassed blood. The attending used two stents- one smaller than the other- to limit the volume of blood that was bypassing the liver.
Lastly, we had the chance to speak to a UreSil vendor who brought in drainage bags, nephrostomy/biliary drainage accessories, and catheters. Not only are vendor meetings uber-helpful for learning how the devices work, the hands-on aspect provides keeps everyone engaged.
7/6- Conclusion (Thanks!)
Shouvik Sarkar Blog

Today marks the end of our tenure shadowing in the interventional radiology department. Throughout the past six weeks, countless hours were spent not only immersing in the clinical environment to learn about tools/procedures but also to learn more about the lifestyles of physicians.
First and foremost, interventional radiology is a perfect branch of medicine to shadow because it allows both bioengineering students and medical students to share knowledge and effectively mull a novel product. One of the most fascinating (albeit tedious) procedures that we witnessed during our rotation was the placement of TIPS (transjugular intrahepatic portosystemic shunt) to direct blood flow from the portal vein to the hepatic vein to consequently bypass the liver, which is barely efficacious in Hepatitis C/Nash Syndrome patients. To supplement our learning of this procedure, physicians invited us to view how they combat complications of TIPS, which may cause encephalopathy due to unfiltered blood reaching the brain. Another interesting procedure we enjoyed viewing was the embolization of uterine fibroids (performed femorally) and capillaries supplying blood to tumors in the liver (performed percutaneously). Both procedures highlight targeted therapy to fight metastasis, an important topic in the future of medicine. In addition, we even saw one example of radioembolization using Yttrium-90, another form of extremely targeted medicine. More recurrent procedures like paracenteses and declots were also very fascinating to view due to the patient satisfaction following the procedure.
Essentially, interventional radiology is based on principles of flow- physicians either attempt to increase blood flow through vessels and decrease flow through a others using different types of instruments (eg. stents and embolization coils). The field is very interdisciplinary in nature and thus requires physicians to thoroughly understand a slew of anatomy/physiology. For example, they need to know the vascular system inside-out in addition to the physiology of the liver in a TIPS procedure. Although the procedures may generally appear blunt, they are far from antiquated. In fact, their intuitiveness and effectiveness help interventional radiology become one of the fastest-growing fields of medicine. Overall, I am very pleased to have chosen this as my rotation, as patient outcomes are frequently positive and radiologists rarely see life-threatening cases.
The purpose of this program was to use observations and apply insights to finally develop ideas for device modification or completely novel devices. To this end, we looked at stents, as they are ubiquitous in the field. Stents currently exist in non-covered (nitinol) and covered (PTFE) forms but are prone to restenosis, a condition in which a blood vessel narrows due to the aggregation of inflammatory cells that may lead to the proliferation of smooth muscle. The issue with present stents is that they are not capable of notifying the patient/physician about restenosis, so the condition may go unnoticed until it is too late. Therefore, our idea is to create a “smart” stent that is not only capable of notifying interested parties as soon as restenosis occurs using a micro sensor but also to prevent constriction using a scraper. Obviously, this ambitious project will require loads of time and research outside clinical immersion.
On behalf of my group members, I’d like to thank the entire interventional radiology team of physicians for graciously allowing us to shadow them for four weeks. Specifically, thank you to Dr. Bui (mentor), Dr. Lipnik, Dr. Gaba, Dr. Ray, and Dr. Lokken for taking time to ensure our understanding. In addition, I’d like to thank Dr. Kotche, Dr. Felder, Susan, and Kimberly for spearheading the program.
Joseph Sauer

Joseph Sauer is a registered patent attorney and holds inactive memberships with the Illinois and District of Columbia bars. Joseph graduated from Wheaton College with B.A. in psychology (2003) and B.S. in Biology (2006). He earned J.D. at Marquette University Law School (2006) and M.S. in Biotechnology at Johns Hopkins University in Baltimore, Maryland (2010). Following completion of M.S. at Johns Hopkins, Joseph served as a psychiatric counselor at MedStar Union Memorial Hospital in Baltimore under Dr. Claude Smith. This experience proved transformative and Joseph decided to forego further training in the law in favor of medical school. While applying to medical school Joseph held teaching assistantships at the Harvard University Extension School in Physics and General Chemistry and served as a senior laboratory teaching fellow at Harvard College in Chemistry and Chemical Biology. In 2015, Joseph received a Certificate of Distinction in Teaching from the Bok Center, Department of Chemistry and Chemical Biology. His research experience includes studying stapled peptide synthesis at the Verdine Laboratory, Harvard Department of Stem Cell and Regenerative Biology. Joseph is interested in cellular metabolism, drug development, biomedical devices and serving patients directly in clinical practice.
Joseph Sauer Blog
Joseph Sauer Blog
Getting situated in anesthesiology
Joseph Sauer Blog

The opening two days of our clinical immersion program (Tuesday, May 30-Wednesday, May 31, 2017) were used to introduce us to the program (Tuesday) and then ease us into the clinical environment (Wednesday). Introduction to the program involved meeting instructional staff, meeting our student colleagues from BIOE/IMED, thinking about the need to use care in interdisciplinary communication, and reviewing deliverables for the program. Chief among these deliverables are this blog assignment and weekly presentations.
The main goal of the clinical immersion program is to gain experience in using clinical observation to develop a needs assessment. I am optimistic that we will take these initial steps with a longer view for questions of feasibility, cost, and other downstream elements in the process of innovation. After all, this does seem to be what our readings in Biodesign seem to suggest – i.e., that one should identify problems and formulate needs assessments based in view of questions of feasibility, cost, and other factors.1
Interestingly, although IMED students know each other reasonably well because of our work together in medical school and attending IMED lunch presentations on clinical innovation, the BIOE students seemed somewhat less acquainted with one another. Nevertheless, everyone seems to be working together quite well and I do think it has to do with the idea that we focus on communicating well and welcoming the input of others.
Our clinical mentor is Dr. Nishioka. IMED students recognize Dr. Nishioka right away because he visited the Class of 2020 during our first week to show us a Google Glass demo – e.g., that this technology could potentially allow the study of clinical medicine from afar.2
Dr. Nishioka has suggested six (6) areas for potential needs assessment:
1) Patient care
2) Patient satisfaction
3) Value based care (i.e., best outcomes in view of limited resources)
4) Supply chain management (i.e., improving how materials move from one area to another in the safest way)
5) Employee engagement
6) Maximizing revenue (i.e., financial efficiency)
References
- Zenios, S. A.; Makower, J.; Yock, P. G.Biodesign: the process of innovating medical technologies; Cambridge University Press: Cambridge, UK; New York, 2010; .
- AnonymousUIC Anesthesiology Department well represented at Society of Obstetric Anesthesia and Perinatology Annual Meeting. http://chicago.medicine.uic.edu/departments___programs/departments/anesthesiology/news_and_events/(accessed June 3, 2017).
Observing, learning and the limited space in operating rooms
Joseph Sauer Blog

Since this is our first week in the IMED/BIOE program, our first full days on the Anesthesiology unit were Thursday, June 1stand Friday, June 2nd, 2017. Hours on the unit usually begin around 6:00 am and finish about 2:30-3:00 pm depending upon what we are learning or studying on a given day. While we tend to arrive on the unit around 6:00 am, we don’t meet with Dr. Nishioka until around 6:30 am because we have to collect a fresh set of scrubs, store our belongings, and gather ourselves for the day ahead. I mention this just to give the reader an idea of how a day will actually function. Perhaps I should add that the drive time to reach campus is outstanding around 5:00 am. On a personal note, while I almost exclusively rely upon the Metra train to reach Chicago during regular academic terms (then taking the Pink Line over to campus), because no trains leave early enough to reach campus at 6:30 am, I will drive to campus for the summer.
When we observe procedures on the unit, we typically split into 2-person groups with one IMED student pairing with one BIOE student. Vijay (BIOE) and I started on Wednesday (May 31) by observing a triple bypass – which is quite a complex procedure. Subsequently, Vijay and I have been thinking that this has skewed our perception so that other procedures seem mild in comparison. The demands on operating room (OR) space, chord management, and staging of sterile tools is quite different (at least in terms of magnitude of supply and equipment) for complex procedures in comparison to less demanding procedures. In regard to needs assessment, this might suggest making ORs specifically capable of accommodating more demanding procedures in particular regard to power supply, device placement, and cable / tube management about the operating field.
Thursday, Chris (BIOE) and I observed a kidney transplant. While the kidney was largely prepared for removal from the donor using a da Vinci Surgical System (i.e., laproscopically), once it had been removed, its preparation was finalized by a surgeon on a small operating table. During this latter portion of the procedure, residents and medical students had difficulty observing the field. This reminded me of the need to ensure that procedures that take place on small operation fields (without endo/laproscope) are broadcast to ensure that learners are able to follow the procedure.
Friday, Vijay (BIOE) and I observed the removal of a tumor from the maxillary sinus. Again, because the operating field was so small, it reminded me of the need to make a small operating field easily visible for people who are not in sterile garments or enabled to stand near the operating table because of the strong limitations on space about the table. Since we have observed the difficulty with which a small operation field can be viewed by learners, we tend to think that this is almost certainly an area that may be a proper subject of a problem and needs statement. IMED students know well that during our M1 year, it was often difficult to observe dissections and various parts of teachbacks (i.e., a time when an M1 student who has performed a dissection teaches the dissection and anatomy one’s classmates who were not part of the dissecting team for a given laboratory session).
Of course, one might think that a technology like Google Glass would offer a potential solution to the difficulty of viewing a dissection (in medical school) or operation (on a clinical unit). However, as Dr. Nishioka shared with us this week, the camera on Google Glass is fixed so that it projects directly out from the eyewear as if one were viewing an object that along a line of sight that is orthogonal with respect to the lens of the eyewear. In practice, one finds often, one views a structure or object that is slightly below this – as if a surgeon were using a bifocal to observe a structure. Accordingly, even a promising technology like Google Glass doesn’t seem to offer a viable solution for a great many scenarios where learners want to observe the detail in a small dissection or operating field.
Week 2, Innovation in the realm of graduate medical education
Joseph Sauer Blog
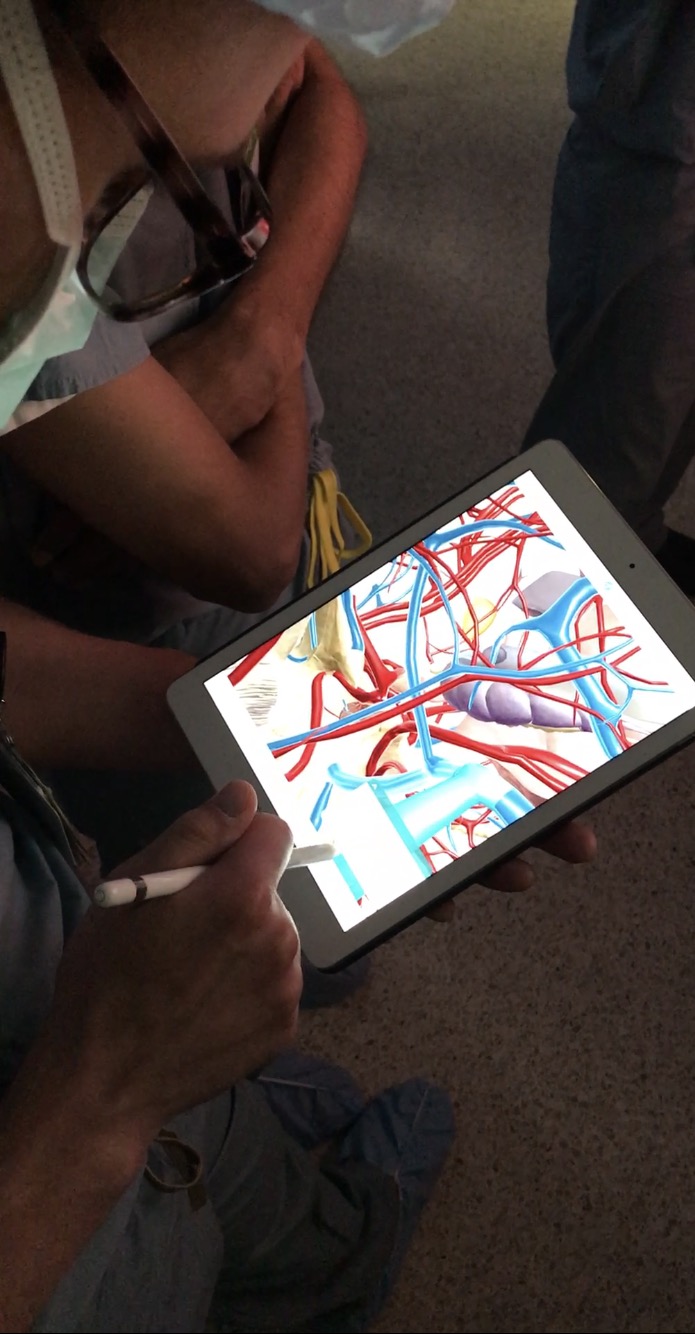
Early this week (Tuesday, June 6, 2017), we examined issues associated with the medical education. Dr. Nishioka summarized that residency usually involves two (2) fundamental elements: (a) clinical work; and (b) more formal education (i.e., texts and exams). Dr. Nishioka raised the question of why residency programs are themselves accredited and why graduates of accredited programs need to pass a board exam for their various specialties. One might perceive these educational requirements as constituting a two-step validation process to ensure the quality of board-certified physicians in a given area of practice.
In regard to clinical experience, residents shared with us that end-of-life discussions are often difficult but that one usually grows through having these discussions with patients and their families. Residents encouraged us to choose the ICU for a clinical rotation. The ICU is said to be like detective work where anesthetists think about hemodynamics quite often. Residents also encouraged us to select the Emergency Department (ED) for a rotation because this is often where patients present. Residency, they tell us, is where one transitions from not having true responsibility for patient care to having responsibility for patient care.
As mentioned briefly in last week’s posts, I tend to think that observing small surgery fields is a common issue for graduate medical education because students need to follow the nuanced details of a surgical or other procedure in an environment where space is strongly limited.
Wednesday morning (June 7, 2017), we began the day with a case study involving an 8-year-old boy who had a difficult recovery following a tonsillectomy. The reason the patient (a hypothetical) returned to the ED was that he had bleeding and pulmonary edema (swelling of the airway). Residents tended to consider this patient as being an easier case than younger patients with lesser communication skills, but the complication of an airway that is itself bleeding illustrates the need for good technique when video-assisted intubation is not practical (i.e., because blood will occlude the camera).
Also this week, I observed several Electroconvulsive therapy (ECT) sessions. Although I had previously worked on a psychiatry floor while considering whether to apply to medical school, I had never observed one of these procedures. I had read accounts of patients thrashing about but when an anesthesiologist is present, the patient can receive a muscle relaxant and this inhibits the muscular contractions in large measure. This reduces the risk of harm to the patient but of course requires an anesthesiologist to monitor vitals, maintain respiration, administer medications and ensure proper recovery along with other staff. Interestingly, the efficacy of the muscle relaxant is checked (often more than once) by using the Babinski reflex (stroking the bottom of the foot to elicit a dorsally reflexive movement of the foot / toes).
Still involving the brain, I sat in on a neurosurgery this week. Getting back to the topic of education and innovation in this realm, it is important to note how eagerly the residents study. Here is a telling image of how a resident can study near the operating room to better comprehend the details of a procedure. The app shown is Visible Body, which is a personal favorite for reviewing anatomy and for which I volunteer as a beta tester. As education become increasingly interactive from an earlier stage (e.g., in the form of anatomy applications like Visible Body), this may help to alleviate some of the steep learning curves for medical students and residents.
The redesigned emergency airway kit
Joseph Sauer Blog
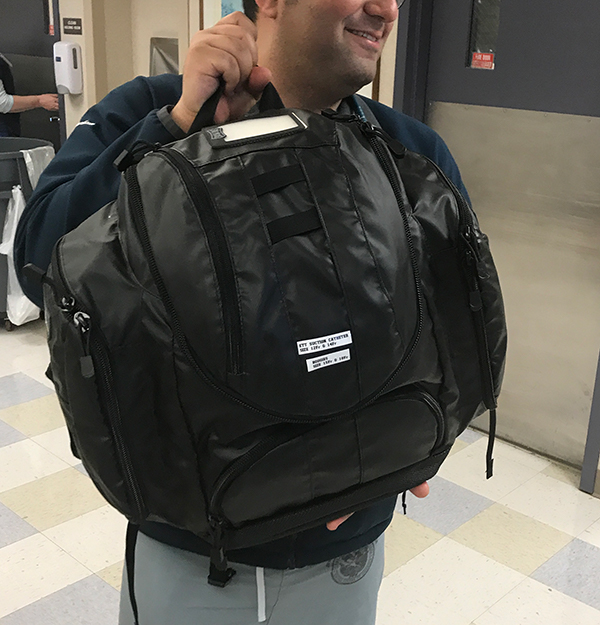
Thursday (June 8, 2017) we observed an emergency intubation. This was coincidental because earlier in the day we reviewed the redesign of the emergency intubation kit (aka: emergency airway kit) for the unit. This kit used to be stored in what looked like an old tackle box for fishing – but in a bright orange color and having clear lettering on it. When the old kit opened, it also opened like a tackle box to have three (3) levels upon which supplies were situated before the user.
(this kit is no longer in service but is used only as a comparison with the updated, redesigned kit)
In contrast, the redesigned kit is housed in a nylon backpack. Although this backpack does bear labels (indicating what is kept in its several compartments, see below), it is not clearly labeled to tell a user what this backpack stores in general (e.g., “emergency airway kit”) in the event that there is any doubt what it includes (which admittedly should be a rare coincidence).
The backpack is actually heavier than the original tackle kit, and while it can be transported on a user’s back, it can be difficult to deploy in an ED or other site of use because of the need to have a broad, flat surface upon which the kit can be deployed.
Moreover, when the backpack is opened, one finds that within the backpack, there are other nylon bags or compartments – which also need to be unzipped in order to retrieve items (e.g., MAC blade, medications, etc.). Most of the storage capacity of this backpack is occupied by one bright yellow roll-out nylon/plastic storage surface that houses most of the kit’s essential supplies – but which requires a broad surface upon which the kit can be unrolled.
Here is the updated emergency airway kit when in use:
The bright yellow material draped over the top of this mobile shelf is the nylon/plastic storage surface that is itself stored within the main compartment of the nylon backpack (seen here sitting on the floor to the left of the mobile shelf unit) but which can be unrolled as one can see in this image (above). Altogether, this means that one has to unzip the backpack, then unroll this yellow nylon/plastic material, and finally one must unzip the lesser compartments on the nylon/plastic surface. All of this must happen before a user can access even the first tool – and some tools like the MAC blade have to be set up and checked before use.
Although we admire several of its properties, this bag captured our attention because we are not fully certain that it is preferable to the original tackle box design. On balance, we acknowledge that the original tackle box lacked the ability to amply re-supply a user after an initial emergency event whereas the backpack has lesser pockets stocked with additional blades, biohazard disposal bags, syringes, plungers, etc. – so the additional weight of the backpack does add value to the pack. Nevertheless, at least this writer would like to see a pack that is easier to deploy and use. One option that comes to mind immediately is a kit that is optionally capable of being hanged from a hook or loop (or other improvement) that allows a user to deploy this inner kit much like a garment bag.
https://www.tumi.com/p/tri-fold-carry-on-garment-bag-022137D2#
The advantage of such a design is that can deployed to a hanging position (optionally) so as to take up minimal horizontal space but where it uses mostly unused vertical space. As between horizontal and vertical space in an operating room or emergency department, there seems to be more untapped vertical space in these environments (although I have not quantified this inclination). Of course, if a user preferred to deploy such a system onto a more horizontal surface, this would still be possible. One way to think about a system like this is that it gives the user the option to hang it – but one can still use this on a horizontal surface.
One of my student colleagues mentioned the use of Velcro rather than a zipper to access the main or lesser compartments of such a bag — which seems like it might be a good idea.
Interestingly, the garment bag (shown immediately above, also below) is actually a bag that unfolds from what initially looks and operates like a laptop bag:
https://www.tumi.com/p/tri-fold-carry-on-garment-bag-022137D2#
Importantly, when I asked a resident who had just finished using the redesigned emergency airway kit if it would be preferable for the roll-out kit to be deployable to a vertical position to utilize vertical rather than horizontal space, the resident indicated that indeed, this would be desirable but was concerned that there might not be a suitable place to situate the kit in a vertical position (i.e., there might not be a suitable hanger neraby). Nevertheless, I tend to think that adding a hook or other means of hanging the most fundamental part of this kit would at least enable this kit to be vertically positioned where space and other equipment allow for this — and where conditions do not allow for this, it can be deployed horizontally.
Anesthesia as a ropes course
Joseph Sauer Blog
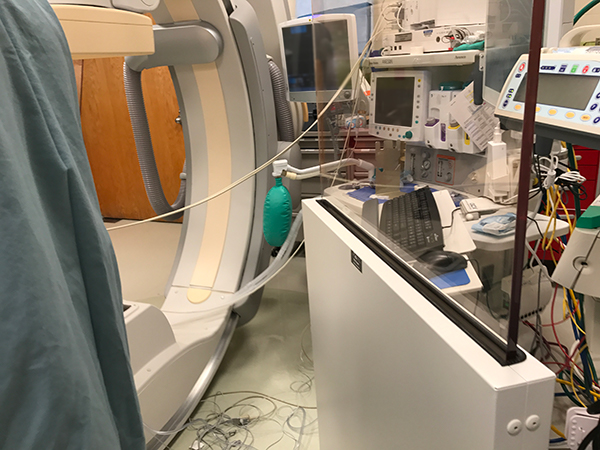
Early this week, we studied the work of anesthesiologists “off-site” – which is to say away from the operating rooms where one is most likely to find an anesthesiologist hard at work. These so-called off-site locations in the hospital include the interventional radiology, gastroenterology, cardiology catheter, and other suites. Often, the work areas in these off-site locations are situated so that the anesthesiology equipment is moved to a dedicated part of the room so that anesthesiologists must arrange their wires and tubes from the equipment to the patient (and around other equipment) – which can create something like to a ropes course when a practitioner needs to move quickly between the anesthesia machine, nearby supplies, and the patient.
We have been encouraged not to focus on the wires and tubes because this problem is so pervasive in the field and immediate solutions (e.g., using wireless connectivity) are conceivable only to a limited extent at this time without redesigning either the entire operating room (or other off-site suite), anesthesia machine – or both. Nevertheless, the wires and tubes represent a true issue for practitioners. In fact, Morgan and Mikhail’s Clinical Anesthesiology (5thEd.) teaches that the single greatest source of injury to patients involving anesthesia machines is attributable to misconnects or disconnects.1 So it is difficult not to think about the way that tubes and wires are situated in these quite special treatment environments.
One way that tubes and wires might be easier to keep track of is to bundle them and one way to make it easy to keep track of bundled wires and tubes is to color-code them.
- Butterworth, J. F.; Mackey, D. C.; Wasnick, J. D.; Morgan, G. E.; Mikhail, M. S.Morgan & Mikhail’s clinical anesthesiology; McGraw-Hill: New York, 2013.
Managing supply stocks and cabinets
Joseph Sauer Blog

Later this week, we met with the group of individuals who track supply and usage of equipment at the hospital. Areas for growth include managing supply in a way that allows the hospital to ensure that stocks of perishable items are used well ahead of expiry dates. As things are, all perishable items are checked for expiry date prior to use and expired products are discarded. Ideally, however, supply could be managed in a way that ensures that perishable stocks are used well ahead of their expiry dates so that the hospital would need to discard expired stocks much less frequently. The issue seems to originate with the local areas in which stocks are stored and managed. Although the hospital is proud that expired stocks are not used in treatment, it recognizes that there is an opportunity to reduce losses due to expiry.
In terms of the local environments where supplies are managed, there doesn’t seem to be a uniform policy on managing supplies (e.g., reviewing to avoid unintentional product expiration). In one OR, we found that supplies were conveniently situated, but that users could not easily determine what supplies were behind which supply area unless one were to unlock and remove a metal door that covered the supply cabinets. This kind of setup is certainly secure, but difficult for ease of supply management and access for use.
When we asked technicians (who were accessing these cabinets and using supplies from these areas) whether these supplies would be easier to manage if the cabinets had transparent doors, the technicians indicated that this would be preferable to the metal, opaque doors that are currently in use.
In another OR, we found a cabinet for storing supplies that did have a set of translucent (presumably glass) doors – so visualizing supplies was easy (although not necessarily for the purpose of determining expiry date).
However, this cabinet was not well designed to house the variety of plastic containers in which supplies were situated – so the doors failed to fully close and required a piece of Velcro to hold them in place when the cabinet was essentially closed. During the course of a procedure, sometimes the doors would be ineffectively shut and would remain open.
On a separate (more pervasive) note, it is also interesting that the hospital is not part of a hospital network. This means that it presumably relinquishes leverage when determining per unit prices on stocks that may be ordered in massive bulk quantities (e.g., as between a plurality of hospitals that are part of a care network). After all, this kind of thinking has been a major driver of integrating care networks over the past few decades.
The hospital also seems to inexplicably lose scrubs, sheets and blankets. We wondered if perhaps it might be time to start RFID tagging these items to ensure that people leaving the hospital don’t take these items with them. This seems to be a constant, minor source of financial drain for the hospital.
On Friday, Nicholas and I visited the OB/GYN clinic and observed an epidural placement. After this session, Nicholas and I wondered if perhaps there isn’t a better way to design an apparatus for epidural placement.
Problems are an untapped resource
Joseph Sauer Blog

Week 4 (June 20-23, Tuesday – Friday) began with a lecture from an Anesthesiology staff physician on the infant airway – i.e., that it can be difficult because it has ~15x more airway resistance than that of adults and a more compliant chest wall. Care for an infant patient needs to be thoughtfully developed in view of the special needs that an infant patient has.
This week, we wanted to more directly find opportunity for innovation in the hospital, so we started to ask more direct questions — more interviewing. We began by observing a vasculature procedure where the surgeon was interested in a clip to secure one end of vasculature onto a device for boring through tissue because this was an issue he frequently encountered.
We have noticed that while interviews can be structured, that we get a lot of insight when asking practitioners what their problems are quite candidly. Practitioners (and other employees) often have a major problem they can identify immediately because this problem bothers them so frequently. This was the case with a member of an ophthalmology surgical team. When asked what his greatest issue was, he discussed the difficulty of manipulating one of his devices, holding a patient’s eyelid open with one hand, and also adjusting a light source. We think this is a good example of how easy it can be to get to the real question that devils someone’s everyday work experience. Most people know what bothers them each day. If they think a solution can be crafted — or that there is any chance you might be able to do this for them — they are more than willing to tell you about the worst part of their work experience.
Other times, you cannot question a practitioner directly (e.g., because there isn’t one around, or when they are preoccupied by rendering care); Chris likened the experience of finding insight into clinical or technological problems in the hospital to the experience of fishing — i.e., there is a lot of waiting, punctuated by moments (sometimes a few minutes) of activity (or insight, in the case of looking for issues in a workplace).
On rare occasion, someone will share an issue to which they believe there is absolutely no solution. I don’t challenge their belief that there isn’t a solution — but I tend to believe that there almost certainly is a solution. For most problems, there is a solution — and if there isn’t, I don’t see what the benefit of assuming that there isn’t would do for anyone.
More commonly, we find that practitioners or other employees can immediately point to an issue they experience that causes them tremendous frustration in the workplace but they rarely take the next step to craft a solution. While hospitals, management and administration are often immediately interested in the solutions (and IP) that their employees generate, how interested are they in the problems of their employees?
Central Sterile: Efficient and still looking for improvement
Joseph Sauer Blog
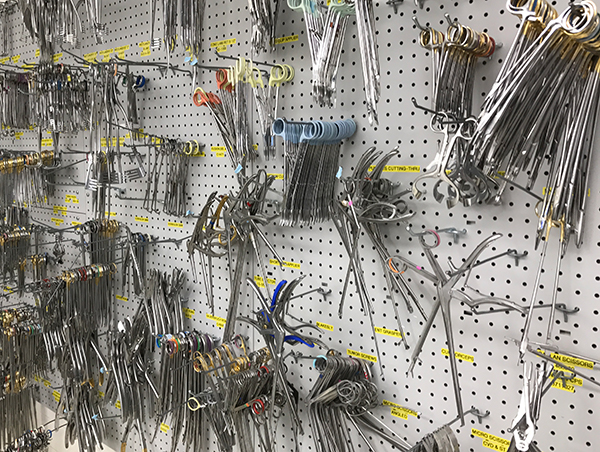
On Friday, we visited Central Sterile (CS). CS is a place that receives supplies that are shipped to the hospital and which processes all equipment that moves to or from operating rooms (and other hospital care environments). We were impressed by CS and its leadership. It seems that CS has done an immense amount of studying its processes for efficiency. We were told that at some point the loading dock from which CS receives its supplies was used as a set for the TV series “ER.”
Improvements in efficiency for CS moving surgical equipment to various ORs and other treatment areas seem to involve bundling surgical kits into larger sterile boxes that can be sanitized or moved more easily together. Since a hip surgery can use 8-20 surgical trays (kits), moving supplies en mass within larger sterile boxes can help to organize and save time.
Here is an example of a sterile cube for sterilizing a plurality of surgical kits together. After sterilization, these kits can be moved to a site of use together.
CS is efficient — e.g., its supplies are automatically restocked and they have thoughtful processes for handling surgical kits that are not used. However, there are areas for improvement and much of this may be had by re-positioning CS in the hospital. Perhaps oddly, “Central Sterile” is not central at all in its location — but relegated to an obscure basement area that neither interfaces directly with the loading docks (one level above CS) nor the surgical center (several floors above CS).
Communication in practice
Joseph Sauer Blog

Communication is lauded in theory but sometimes overlooked in practice. I will spare you the mindless “communication is so good” discussion and just get to an example:
The tape has been annotated with the word “CLEAN”— but are these IV pumps clean or do they need to be cleaned? That depends on whether the reader (or for that matter the writer) intended the word “clean” as an adjective or an imperative. If an adjective, then these pumps are indeed clean and ready for use. However, if this is an imperative then these pumps need to be cleaned.
Fortunately, as I came to learn, this is the practice for letting techs know that these pumps are actually clean (i.e., they have been cleaned in the past and may now be used). However, this practice may not be clear to visiting staff (e.g., during an overnight transplant case).
Hospitals need to streamline communication so that there are predictable inputs and outputs. Color-coding clean vs. dirty might not be a bad idea — but what about individuals who are visually impaired in the detection of certain colors? Perhaps a color icon system would work better. Such a system could be applied to scrub receptacles, waste bins, blanket receptacles, etc. – but ideally, the practice would allow easy determination of whether an item (or in this case a set of items) is clean or not clean for reusable equipment subject to cleaning.
Aakash Shah

Aakash Shah Blog
Aakash Shah Blog
Coordinated Chaos
Aakash Shah Blog

The first day of my Pulmonology & Critical Care rotation forced me to hit the ground running. After a brief orientation with Dr. Dudek, we were immediately led to endoscopy lab on the 2ndfloor of the hospital to observe a bronchoscopy in which they were also taking a biopsy to send to the pathology department. A bronchoscopy is where the patient’s nostril, trachea, and vocal folds are all anesthetized. Subsequently, a long black tube with a camera at the distal end is sent through the nasal pathway, down the larynx, through the vocal folds, and into the trachea. At the carina, the point where the trachea bifurcates, each lobe of the long is assessed to formulate a diagnosis. Then the physician and technician pass a long metal wire with forceps attached to the distal end into the tube to obtain several small tissue samples from the alveoli. The physician had to first see the forceps appear on the camera and then switch monitors to see where the forceps were via X-Ray.
What surprised me the most is how cramped the room itself was. In one room there was an X-Ray machine with an adjoining monitor, a computer cart, a monitor for the endoscopy camera, and the cart with equipment for the endoscopy camera. The room itself had one attending, one fellow, one resident, one technician, and one nurse. Each one had a particular role, but had versatile abilities, helpful in adjusting to the needs of that individual procedure.
With that being said, there were wires all over the ground and it seemed as if the core crew was boxed into a small operating space and there was very little space to maneuver the large machine. Each individual had their own small workaround, except the attending who was moving from one side to the other to monitor the entire situation.
After all this, I need to watch a few more bronchoscopies to truly determine common pain points in the workflow for the team.
Dissemination
Aakash Shah Blog

After observing my first set of rounds in the medical intensive care unit, the MICU, I realized that the purpose of rounding was to disseminate information from multiple sources to make that information common knowledge. For example, the lead intern would present the case to highlight significant facts about a case with nurses, pharmacists, and other health professionals confirming or adding any other useful information. This is the first act of dissemination as the case is now widely understood, albeit on a superficial level, by the relevant medical team.
The second act of dissemination is more in terms of medical knowledge from the attending physician who then uses the case as a teaching opportunity. The attending disseminates information from their experience to teach the fellows, residents, pharmacists, nurses, and students.
The duality of dissemination during rounds allows the entire team to be on the same page in terms of background information, but also on the same page for the agreed upon plan of action. While actively listening, I initially thought rounding was inefficient, and parts of it are, but when I saw the true purpose of rounds – the dissemination of information – I realized just how efficient the practice is at teaching.
P.S. I did not want to take any pictures of rounds because there were patients in the rooms, so I have attached a stock photo instead.
Cancellations
Aakash Shah Blog

Aakash Shah Blog

A few days ago, I got the privilege to observe a Spanish-speaking patient communicate with a non-Spanish speaking physician. It was quite interesting to see how through a quick call to the translation services; the physician could communicate with a patient in a real-time manner.
The setup was very simple, the translator was accessible via speaker phone. So the physician would ask a question, the translator would repeat it in Spanish, the patient would respond in Spanish, and the translator would repeat the answer in English. From the basic Spanish that I know, the translator was very fast and quite accurate in translation, even some of the more technical terms.
However, once the Spanish-speaking attending came into the room and conducted his own patient history and exam, we realized that there was a lot of information the patient had not told us, whether that be because the translator was present, she felt uncomfortable, or some other reason.
Therefore, at the end of the day, it is hard to replace the human connection, especially the nonverbal bond that is built between two native speakers. The trust established cannot be emulated through a translator.
Delirium
Aakash Shah Blog

Over the past few weeks, we have spent a couple days each week in the MICU – medical intensive care unit. While there are many aspects of the MICU to discuss, the most prominent problem I heard from the residents is ICU delirium. In layman’s terms, delirium is when the patients are in and out of clarity and overall do not really understand where they are. Upon further investigation, I realized that ICU delirium is very common in the hospital setting due to patients being exposed to a new environment, constantly woken up, prescribed benzodiazepines, and having very irregular sleep/wake cycles. Most notably, delirium is associated with an increased mortality rate and is thus, a severe problem that should be addressed.
So I did some background reading about ways to either prevent delirium or at least delay the onset in order to minimize the symptoms. The first solution came from a resident – which was to give each patient earbuds in order to dull the sound, especially when they are trying to sleep. One observation I made during my time in the MICU is the number of sounds there were – from mechanical ventilators, IV pump signals, nurses opening and closing doors, residents talking, hospital phones ringing. However, while each sound on it’s own is not a lot of noise, when they are all summed up, there is a symphony of beeping and muffled conversations. Another observation I made was that the doors for the individual patient rooms were typically left open, presumably so the staff could easily enter and exit a patient’s room. However, this allows a lot of unnecessary noise to enter the patient’s room. Understandably, patients have difficulty sleeping in this environment.
While reading a few publications, I came across several more solutions which I will discuss briefly. The first intervention is called, awakening and breathing coordination which sought to reduce coma times and also helped in reducing the time patients spent on a mechanical ventilator. The next intervention was to stop prescribing benzodiazepines – which in theory should be a relatively easy fix. The last intervention was to increase the amount of exercise patients got via physical therapy.
These interventions when grouped together can significantly decrease the amount of time an average patient is spending in the ICU, but this topic warrants a separate discussion.
Patient Education
Aakash Shah Blog

One of the most important aspects of being a physician/nurse/pharmacist/staff in an outpatient clinic is being able to explain complex diseases and drugs to patients who have limited understanding of the human body. Several times, I have had the privilege of watching and listening to a clinician explaining the disease has been very interesting because you can see the light bulb turning on in the patient as they slowly begin to understand what is happening inside their heart vessels. Even more interesting is seeing how the medication works to help alleviate the symptoms the patient has been experiencing.
However, throughout this whole process, the clinician is the one doing all of the talking while the patient nods along. To me, this is an example of passive learning with most diligent patients writing only a few notes. One possible improvement to check how much the patient actually understands would be to have the patient summarize what the clinician just described because then the clinician will see how much the patient knows.
Most importantly, the team of clinicians can discuss different aspects; such as the physician discussing the diagnosis, the nurse discussing insurance, and the pharmacist discussing the drug regimen. By breaking it down, the patient has a greater chance of retaining all of the valuable information.
With one simple question, the clinician can assess how much learning took place so that they can help the patient understand what is the pathophysiology of the disease/syndrome/etc. Research shows that when patients understand the diagnosis and prognosis, the more likely they will stick to the prescribed drug regimen, physical therapy, etc., thus leading to overall better health outcomes.
Sound
Aakash Shah Blog
The idea of using sound to notify our brains that something requires our attention is an archaic concept deeply rooted in biological origins. Babies cry to get the attention of their mothers, our ears perk at the sound of danger in moments of crisis, and our hands grab our phones at the sound of a ringtone. In similar manners, healthcare devices and monitors use sound to alert relevant healthcare professionals. However, when there are a plethora of machines in the room, the sounds drown each other out, especially when some machines use similar sounds to report that everything is normal. For example, cardiac EKG monitors beep every 5-10 seconds to report that the readings are normal.
This led me to observe how the nurses and residents that spend so much time in the MICU often do not realize that some sounds are even going off because their brains have learned to tune them out. One quick example was that they did not realize the phone was ringing until the third ring.
One solution would be to reduce the number of signals so the sounds ring at slower frequencies and longer time intervals. There are also some machines that do not need to be heard and should be simply muted. Finally, the patient should be provided ear plugs or headphones so that sound stimuli is reduced and they can get better rest.
All in all, I found it interesting how there were so many sounds in the MICU and that no one seemed to pay any attention to nearly 90% of them. There seems room for improvement in this area of medical device technology.
Multiple Hands
Aakash Shah Blog
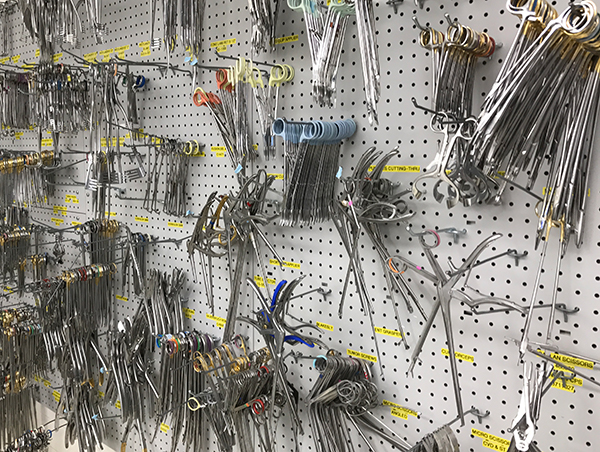
By this point, I have seen numerous procedures, and one common theme is the number of hands required to effectively complete a surgery. In almost all situations, there were at least two people needed, if not three. Usually, the person doing the main portion of the procedure will be busy in handling the instrument. The technician/nurse is responsible for the administration of the anesthetic and also for documenting the procedure. Sometimes there is a medical student or resident, trying to learn. The attending stands near to assure that the procedure goes smoothly. Again, this is just a rough depiction, the number of people required really depends on the procedure being completed.
Often times, one person may be suctioning, but then needs to take care of something else (like getting the lidocaine ready) and another person takes over the job. In a sort of silent, yet fluid way, everyone understands how to help and cover for their partners. It is this sort of nonverbal communication that separates a good team from a great team. From my vantage point, there is a positive correlation between greater fluidity and number of hours working together. The more comfortable the team is with one another, the smoother the procedure tends to go.
So what exactly am I trying to say?
There is importance in keeping the same teams together, in order to increase fluidity and at the end of the day, increase patient comfort, safety, and satisfaction. The goal of healthcare is first and foremost to help the patient, and whatever small steps we can take to make that happen, is something that we should all consider.
A Need for Innovation
Aakash Shah Blog

Today, while in the Pulmonary Hypertension clinic, a patient that required continuous oxygen flow was complaining of how inconvenient it is to move the machine in her home which generates oxygen from the air, especially if she is on a different floor of the house.
So a little background: she requires more oxygen when she is moving (i.e. climbing stairs) and less oxygen when she is sitting down. She has the machine placed on one floor and has a very long tube that basically follows her all over the house as she moves so that she can get her oxygen.
The main problem occurs when she wants to move to a different floor, she puts the oxygen up to 5L/min, but when she reaches the floor and wants to move normally she only needs 2L/min of oxygen. However, she cannot change the oxygen setting remotely and has to go back down the stairs (which requires her 5L/min of oxygen)! As one can see, the lack of remote control of oxygen flow can lead to a wastage of oxygen, depending on what type of activity the user is trying to do.
This user experience seems like a prime opportunity for an innovator to create a device that allows an user to control the oxygen flow via an app on their smartphone or even a remote. It seems very intuitive, but the reason this simple problem has not been solved is largely to due to lack of knowledge.
The next steps would be to see the demand of such a device in order to persuade an innovator to actually build the product.
Aakash Shah Blog

This will likely be my final blog post and I firstly want to thank any readers who took time out of their day to read and ponder the thoughts I’ve had during this program. Spending time with healthcare professionals and patients is a great privilege and a huge opportunity to learn for me; something I will never take for granted. Additionally, I would like to thank all of the attendings, fellows, residents, nurses, medical assistants, pharmacists, technicians and fellow students who took time to explain something or to even talk to me. Without their friendliness and kindness, I never would have had the chance to observe medicine from an innovation standpoint.
This opportunity is not something I will take for granted and regardless of the tangible outcomes of the program, I will take the intangible skills I have learned with me and constantly question the status quo in order to see how I can improve the world around me. I started knowing very little about Pulmonary and Critical Care and though I’m far from an expert on the subject, I am proud to say that I have learned much more than I could have imagined.
Last but not least, I would like to thank the Clinical Immersion Faculty for guiding us through the design and innovation process. They showed us how to make an idea into reality and that is one of the most powerful teaching lessons I have learned. My fellow teammates were inspiring and it was encouraging to see others who had the same interests as me. A multidisciplinary team allowed me to see different perspectives and gave me a chance to see how others think.
If anyone has any questions or comments, please do not hesitate to contact me at ashah200@uic.edu. I would love to hear your thoughts and see the same issue from a different vantage point.
Sariya Siddiqui

I joined the Innovation Medicine program to to learn about the different parts of medical innovation by collaborating with individuals across disciplines. I studied math and computer science as an undergraduate, and then obtained a Master’s degree in education technology, focusing on medical education. With these skills, I would love to contribute to the fields of medical device innovation as well as medical education technologies.
Sariya Siddiqui Blog
Sariya Siddiqui Blog
Week 1 – Interventions for IR
Sariya Siddiqui Blog
Interventional radiology is medicine practiced percutaneously through small holes in the skin. There are two main components of all IR procedures: devices used for imaging and visualization, and the devices entered into the patient’s body to accomplish a certain goal. Both of these components cause certain limitations. We looked specifically at devices entered into the body during the first half of this week.
A variety of stents, catheters, needles and other small devices have been developed to help IR doctors to get to and manipulate different parts of the body. Each procedure requires a unique set of devices, each having evolved greatly over the years, making IR a truly remarkable field in terms of innovation. Of course, the devices need to create and fit through a small hole, which creates certain limitations, but also leaves room for imaginative solutions. Two devices we looked at were nephrostomy tubes and filters (pictured). The nephrostomy tube contains a pigtail loop with a fitted string connected to the beginning and end of the tube. The tension on the string can be relaxed at the proximal end of the tube, allowing the tube to be straightened and inserted into the collecting system of the kidney through a small hole. When the string is tensed once again, the loop reforms, and the device is secured in place. The function of the tube is affected by the number of holes in the pigtail
loop, limiting the amount of fluid drainage accomplished by the device. The filter, also shown above, is used to prevent clotting in the IVC. It is placed in the IVC, and when the hook is pulled, the filter assumes a compact shape which allows it to be pulled into and out of the IVC during placement and removal. Filters have gone undergone remarkable evolution over the years.
Week 1 – Tips for TIPS
Sariya Siddiqui Blog
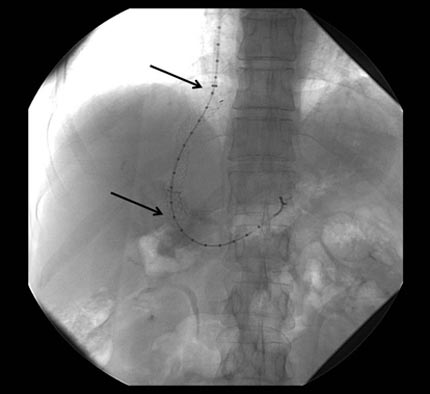
Image
Week 2 - Post 1 - Hemodialysis
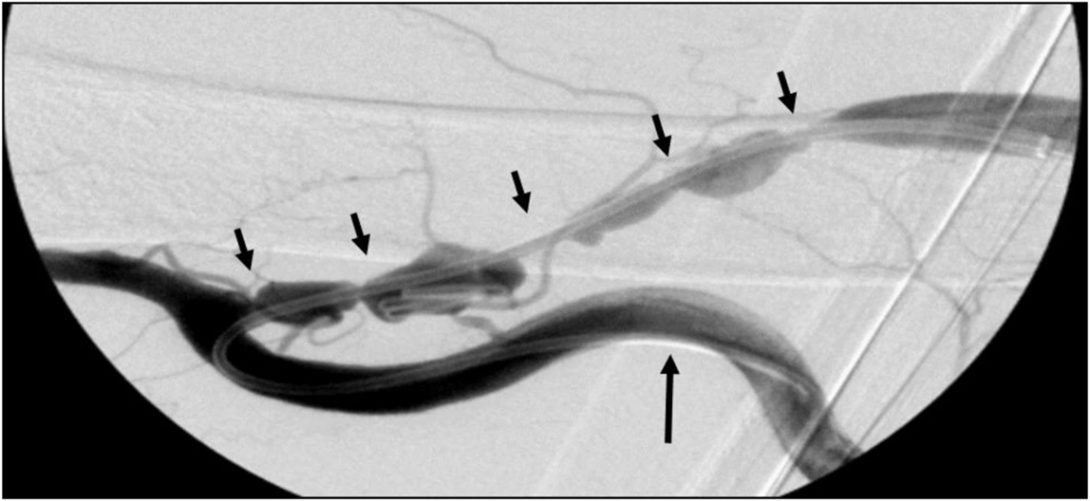
This week, we saw multiple patients on hemodialysis, a procedure used to treat kidney failure. IR physicians provide three ways of venous access for hemodialysis: fistulas, grafts, and catheters. Fistulas are surgical connections between an artery and a vein. They allow increased blood flow into a vein, allowing the vessel to mature and adapt to the greater volume of flow needed for dialysis needles. Grafts similarly connect a patient’s artery and vein, but are made of external tubing. Finally, catheters are usually used for emergency dialysis procedures, and have two lumens — an arterial and venous. Both tubes are inserted into a vein, the arterial bringing blood from the patient to the dialysis machine and the venous returning the blood back into the vein. Interestingly, the distance between the insertion of the two tubes into the vein needed to prevent cross-flow between the blood currents is very small, and most catheters simply have a staggered tip with one tube protruding a few mm further into the vein.
Each method of hemodialysis has strengths and weaknesses. Fistulas, when possible, are the “gold standard” of dialysis. This is because they do not require introduction of foreign material into the patient’s body. However, fistulas take over a month to mature, making them a poor choice for patients in need of urgent care. Maturation of grafts is a little quicker, at about 3 weeks. However, grafts tend to clog up with clots and stenose, as the body recognizes the tubing as foreign material. (Note: Fistulas also become stenosed over time, though generally at a slower rate than grafts.) Finally, catheters do not need to mature, and therefore are used to provide emergency venous access for dialysis. However, they are most likely to be clogged and become infected.
Stenosis of hemodialysis fistulas and grafts is a big problem. There is no way of telling whether a patient’s fistula or graft is blocked until the patient either begins exhibiting symptoms (pain, weakness, etc.) or happens to have some imaging done for another reason. It can be very difficult to open up the passageway once its blocked. We saw two patients who had to come in for multiple procedures (stenting, angioplasty, etc.) on different occasions, before it was determined that nothing was keeping their fistulas/grafts open long-term, and they ended up getting catheters to maintain their dialysis. It would be interesting if there was a way to monitor flow or blockage in these fistulas and grafts, so that stenosis could be detected earlier on, and procedures like stenting and angioplasty would have a higher success rate.
Week 2 – Post 2 – Operations and Work Flow
Sariya Siddiqui Blog

Preparation time prior to operating room procedures is lengthy on all fronts. Prepping the patient for the procedure — including transport and anesthesia — takes well over an hour each time. While we did not observe the details of prepping the operating room from the point of view from nurses and technicians, we did see some of the inefficacies on the side of physicians. Before entering the operating room, all physicians (and nurses) where shoe covers, head covers, face masks, and eye protection. Since these are all ideally changed between rooms, this process takes a significant amount of time. Moreover, if the procedure involves fluoroscopic guidance, each individual must don a lead suit. These suits are heavy, and are cumbersome to put on and take off the hangers. They also take at least a minute to put on each time. Many doctors (fellows and residents) joked about the suits causing them back and shoulder pain, which we learned from experience is a reality.
We also noticed some inefficacies in the operating room. For example, almost all fluoroscopically-guided procedures utilize small tubes of contrast, that are injected through catheters to view the surrounding blood vessels. One person (usually the medical student and sometimes a fellow) is occupied with emptying and refilling these syringes. It would be interesting if there was be a multi-dose storing syringe that could be refilled just once or twice during a procedure, to free up one of operators’ hands.
Another inefficacy is in storing fluoroscopic images. The doctor’s hands are usually preoccupied with holding catheters, wires, needles, and anything else being used for the procedure. The foot pedal he uses starts the fluoroscopy machine. However, every time a fluoroscopy image needs to be saved (about once every minute or even more frequently, while its being used), the doctor tells either a PA, nurse, or student to do so. This adds additional yelling over the many noises of the operating room, and because PA’s and nurses are moving around, causes some confusion. It would be nice if the software used for fluoroscopy viewing took voice commands directly from the physician.
Week 3 – Post 1 – All About TIPS
Sariya Siddiqui Blog
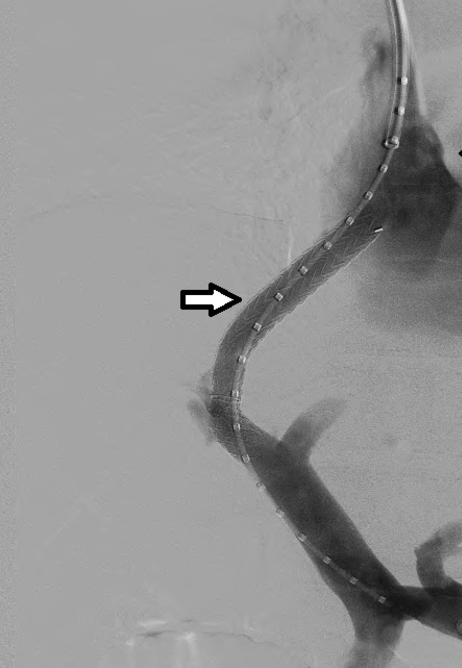
Over the last few weeks, we’ve seen multiple transjugular intrahepatic portosystemic shunt (TIPS) procedures. This procedure is done to bypass the liver in portal hypertensive patients with liver cirrhosis, to reduce complications of the hypertension such as bleeding from esophageal and gastric varices. By connecting the portal vein (draining blood from the bowels) to a branch of the hepatic vein within the liver, the blockage sites within the liver are bypassed.
At the start of the TIPS procedure, a patient’s portal blood pressure is checked. This value will be revisited post-procedure to ensure a decrease in portal pressure. The TIPS procedure is conducted transjugularly, or through the internal jugular vein. A catheter is guided through the venous system into the hepatic vein, and contrast is injected to ensure that the physician has reached the right position. The need for contrast can cause problems in some cases, as patients with a low GFR (glomerular filtration rate) due to kidney failure cannot handle a large amount of contrast. In cases where contrast agents are not used, the fluoroscopic image can be hard to read.
The next step of the TIPS procedure is usually the most difficult. Since the portal vein is not accessed percutaneously, it is found by repeatedly poking the liver in a direction predicted to be that of the portal vein. CO2 is injected into the liver parenchyma to visualize the vasculature around the catheter. If the right position has not been reached, the catheter has to be pulled back and the process repeated. This guesswork can take hours (we saw a TIPS procedure take almost 5 hrs!).
Finally, when a passage from the hepatic branch to the portal vein is identified, a stent is deployed to create and hold open a shunt. To do this, a marked catheter (with radio-opaque markings), is inserted to measure the length of the shunt, and a stent of the right size is deployed. The stent needs to be the right size; if it is too long, it can enter the right atrium and cause complications such as arrhythmia, tricuspid valve injury, or atrial septal injury. This is especially important since a stent cannot be moved once it is deployed!
One complication we saw was hepatic encephalopathy post-TIPS. This can occur if too much blood is shunted away from the liver. Since the liver filters blood it receives from the bowel, excessive shunting can result in excess toxins reaching organs like the brain. In order to solve this problem, two additional stents were deployed within the original stent, one the same size as the original, and another shorter and smaller in diameter. By placing these next to each other, a functionally narrower passageway is created (see first diagram below). This problem can also be solved by taking a single stent of the same size as the original that is balloon-expandable, and only partially expanding the stent, so a portion of it remains narrow (second diagram). Finally, a stent that has a diameter gradient can also be used (third diagram).
Another potential complication, as with deployment of any stent, is clotting or stenosis of the stent. The stent normally used for TIPS is covered with a PTFE cortex to prevent bile (a thrombogenic substance) from clotting blood. It also has a portion that is uncovered, which is inserted into the portal vein to anchor the stent; this uncovered part prevents clotting within the portal vein. Despite these measures, however, stents do eventually stenose, and angioplasty or drug releasing catheters may be needed to open up the shunt.
Week 3 – Post 2 – Oil Pipes to IVC Filters
Sariya Siddiqui Blog
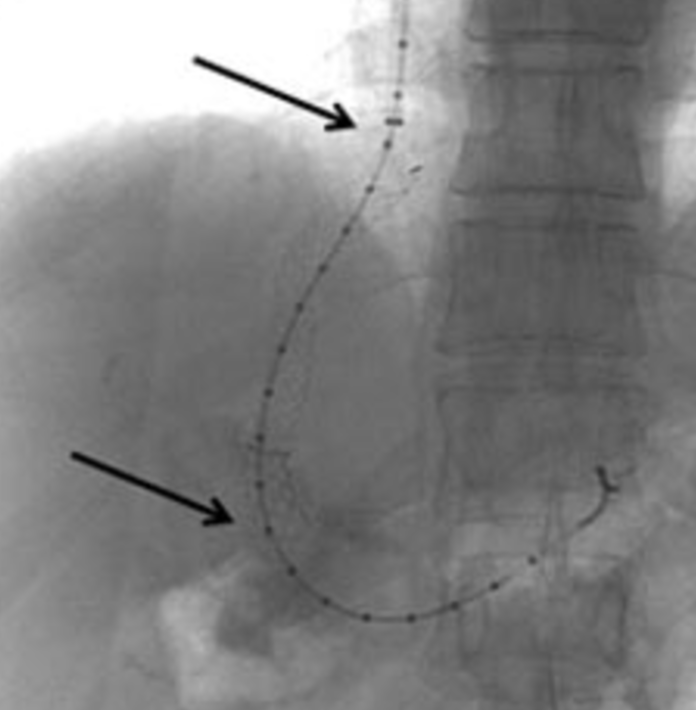
Image
Week 4 – Post 1 – Stents
Sariya Siddiqui Blog

At the end of last week, a representative from a stent-creating company came in to assist with a stent placement. The patient had advanced head and neck cancer, and his tumor was surrounding his internal carotid artery, with a fistula covering one side of the vessel, leaving a millimeter or so between his artery and the outside world. Because a carotid blowout would cause instantaneous death, the IR physicians decided to stent the artery, to prevent massive blood loss in case of fistula invasion in case of vessel rupture. The procedure was tricky, as the path to the internal carotid from the femoral artery is tortuous (once the catheter reaches the the aorta, it must make a sharp turn to enter the common carotid artery). Other entry points (such as the right radial artery) would have provided a less tortuous path but would not have allowed placement of a large enough stent.
The case itself was interesting, but the company representative was also kind enough to show us a variety of the other stents they sell. Stents have evolved a lot over time, and each design has different benefits and drawbacks.
. .
The stent to the left is the Wallstent, an early version of stents that was flexible (
beneficial for deployment and tracking through sharp turns in vasculature), but elongated length as it was compressed. This change in size was problematic, as it resulted in imprecise deployment. The next stent, second from left, is less flexible, but provides more radial force to hold open a vessel. It also has small anchors on the edges which help prevent migration. The third stent, similar to the one used in the carotid stenting procedure we saw, is a flexible stent that does not elongate when compressed. It is made of Nitinol, a metal alloy of nickel and titanium, that has shape memory (so it returns to its original shape upon cessation of external force) and superelasticity. This stent is available in both covered and uncovered varieties; the covered was used for the carotid stenting procedure, as the goal was to prevent blood loss in case of vessel damage. Finally, the stent to the right is a TIPS stent. The uncovered portion is inserted into the portal vein for anchoring; it is uncovered to minimize turbulence and clotting of blood within the vein. The covered portion creates a shunt through the liver parenchymal; it is covered to protect the blood from the thrombogenic bile present in the liver.
One drawback of stents we didn’t talk much about with the representative, but we’ve seen numerous times in the past few weeks, and discussed with some of the IR docs, is restenosis after stenting procedures. Overtime, neointimal hyperplasia (growth of muscle cells from the vessel intima into the lumen of the stent) causes a decrease in diameter of the stent. This is usually not detected until follow-up imaging is conducted, or if the patient exhibits weakness or pain in the area distal to the stent. It would be interesting to study restenosis rates in stents made of different materials, to see whether some materials may delay this process.
Speaking of blockage of stents, clotting within stents can also be a problem. We saw a patient this week with multiple clots in his TIPS stent, as well as a clot at the juncture of the stent with the portal vein. The patient’s stent was extended, and in order to dissolve the clots, a drug-infusing catheter was inserted and left overnight. Here’s what he looked like:
.
Week 4 – Post 2 – Interventional Oncology
Sariya Siddiqui Blog

Interventional radiologists treat many oncology cases through minimally-invasive, targeted therapies. Some of these procedures, that we’ve seen over the last couple weeks, are listed below:
- Chemoembolization
- TACE (transarterial chemoembolization) is the delivery of chemotherapeutic agents through embolic microspheres to the site of a cancerous tumor, usually in the liver. The embolic microspheres occlude the blood vessel supplying the tumor, and chemotherapeutic agents are released from the spheres to slowly kill the tumor. Interestingly, most of the blood supply of regular liver tissue comes from the portal vein, whereas most cancerous tumors receive their blood supply from branches of the hepatic artery. So, to optimize specificity of the embolization to tumor tissue, the embolic microspheres are delivered through the femoral artery up the aorta into celiac and then to the branch of the hepatic artery supplying the majority of the tumor. The process of finding the right branch to embolize can be lengthy. The catheter is threaded through each potential branch, contrast is injected, and the imaging is analyzed to determine how much of the tumor is covered by supply from that vessel. If the blood vessel is determined not to supply that tumor, the catheter is back-tracked and inserted into another hepatic branch, and the process is repeated. Ideally, the embolic agents are delivered to the smallest branch of the hepatic artery that supplies the largest area of tumor tissue.
- Radioembolization
- Radioembolization is another type of cancer treatment utilizing embolic microspheres. Unlike chemoembolization, radioembolization is the delivery of radioactive particles (generally yttrium-90) instead of chemotherapeutic agents. Yttrium-90 decays to release beta particles, which damage tumor cells.
- Because the embolic spheres used for radioembolization are radioactive, and therefore harmful to human tissue, care must be taken to ensure that the physicians and nurses are not in contact with the spheres. For this reason, a complex setup involving sterile lead-casing and sterile vials is used to prep the embolic agents (shown below).
- Radiofrequency Ablation
- Oncologic radiofrequency ablation is the ablation of tumor cells through heat generated from radiofrequency currents. A needle is inserted into the liver percutaneously and targeted to the spot of the tumor using CT-guidance. Because the heat can damage skin and tissue outside the liver when the needle is inserted, there is an internal cooling system on the device that only leaves a small active tip heated.
HCC or Adenoma: Physician Communication
Every Thursday, we attend a liver board conference, a group of inter-specialty physicians (and sometimes a couple engineers) who come together to discuss interesting liver cases. One of this week’s cases was especially interesting. A middle-aged man was referred to UIC oncology from an outside facility after being diagnosed with metastatic lung cancer. One of his scans uncovered a small lesion in his liver, which the interventional radiologists thought may be a lung cancer metastasis or possibly a separate liver cancer (hepatocellular carcinoma). To verify, a biopsy was taken and sent to UIC pathology. According to pathology’s checklist for diagnosis, the lesion was declared benign. The man continued chemotherapy for his lung cancer, which he was responding very well to, and IR ordered 6-month follow-up imaging for the liver lesion. Six months later, the man returned, and the liver tumor had spread across the entire liver. It was no longer treatable, and the man was given a few months to live.
During the liver conference, pathology was called in to discuss the measures they used to diagnose the patient. It appeared that each of their criteria are not absolute, but accurate to a certain percentage. However, the IR physicians were not familiar with this, and thought that if they had known previously that the pathology diagnosis was not absolute, they may have ordered an earlier follow-up, since the patient’s history revealed all the risk factors associated with HCC (hepatocellular carcinoma). This incident reveals a need for better communication between physicians — perhaps more opportunities for physicians of different fields to interact and get to know the basics of other specialties they interact with, so that they can make the best decisions for patients’ care.
Shana Snarrenberg
Shana Snarrenberg
I am a Bioengineering student on the neural engineering track. I am heavily involved in the Biomedical Engineering Society and I also enjoy my research involving EEG. Outside of school you’ll most likely find me outdoors or climbing.
Shana Snarrenberg
Shana Snarrenberg Blog
Day 1 – Clinic Observation
Shana Snarrenberg Blog
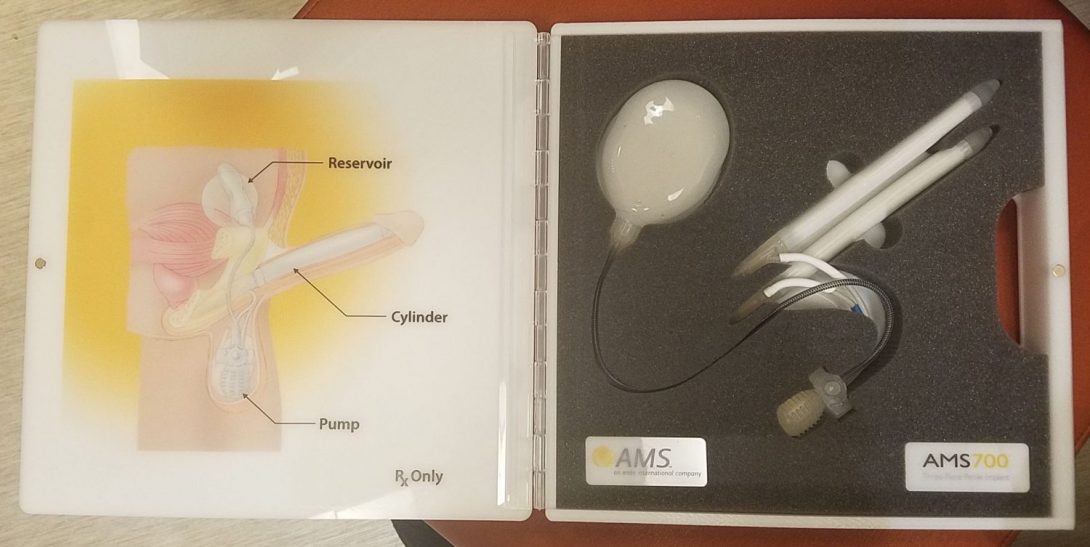
On our first day in the clinic on Wednesday, May 31, we were hit with a challenge right at the start of our morning. We arrived at 1220 S. Wood, the Mile Square Health Center, at 9am to meet Dr. Niederberger but we were told that he was not in clinic on Tuesdays. However, Dr. Nikita Abhyankar was very helpful and invited us to stay and observe with herself and another resident, Dr. Ryan Dobbs. Dr. Kocjancic was the attending physician in clinic that day and he was also welcoming of our presence. Despite the initial confusion, we were able to spend the rest of the day observing patient interviews and clinical procedures.
One of the first patients that morning came in with a malfunction of an implanted device, precisely a bioengineering problem. The patient had received an inflatable penile prosthetic (IPP) following a prostatectomy due to prostate cancer. He came in to clinic because the tubes of the prosthetic were not filling properly. The prosthetic consists of a pump that sits inside of the scrotum which fills two tubes inside of the penis from a reservoir sitting in the abdominal cavity. The user activates the pump by pressing on it through the skin and then deflates the prosthetic by pressing a button located above the pump. Dr. Dobbs gave me the statistic that 25% of implanted prosthetics need some sort of mechanical part replacement over the course of 10 years. Dr. Abhyankar also noted that it is not uncommon for infections or malfunctions to occur, however, IPPs are preferable to a simple malleable prosthetic because of the close resemblance to normal function.
Later a female patient came in with concerns about needing dialysis. During this patient interview, it was clear that there was somewhat of a language barrier although the patient declined the offer for an interpreter. The doctor interviewed the patient to try and understand the reason for her visit which was initially unclear. She was scheduled to have surgery soon with a different service to have a lymph node removed and the doctor performing that surgery referred her to urology because of concerns about her right kidney function. This patient had been through a lot: she had colon cancer and as a result had a colostomy, chemo therapy, and radiation. Damage to the bladder nerves when removing areas of colon ore the rectum can occur and cause incontinence and so she has to catheterize herself four times a day to void urine. She had a swollen lymph node in her lower abdomen which the other doctor was planning to remove and I believe she was in the urology clinic to determine if it would make sense to also remove her right kidney at that time. The visit was fast paced and at some points it seemed like there were some missed connections during conversation; ultimately the patient’s concerns were addressed and she expressed relief at not needing dialysis and having normal kidney function taken up by her healthy left kidney.
Overall, it was an exciting first day of getting to observe the workflow in the clinic of doctors, nurses, and medical assistants. Everyone was very helpful and patient with answering my questions. It was a fast-paced environment with lots of room to learn.
Day 3 – OR Observation w/ Dr. Garvey
Shana Snarrenberg Blog

On Friday, June 2, Ben and I observed three procedures with Dr. Garvey. Usman was in a different OR with Dr. Abern observing robotic surgeries with the DaVinci machine. The first two procedures we observed were shockwave lithography treatment of kidney stones using a device manufactured by Storz. Although the same device was used, the procedures were slightly different because of the location and size of the kidney stone.
Shockwave Lithography
Case #1: 41 YO m
The patient presented with a ~9mm kidney stone in the renal pelvis. A stent was placed with one end in the renal pelvis and the other end in the bladder following these steps:
- A cystoscope is inserted through the urethra to locate the renal pelvis.
- A guide wire is inserted through the cystoscope.
- The stent is threaded onto the guide wire.
- The pusher which is either a closed or open-ended catheter is threaded onto the wire to push the stent into place.
Dr. Garvey explained that stents are sized to the patient by height for length and the gauge is standard unless they encounter a need for a different gauge size during the procedure. This patient was sized to a 6 French x 26 cm stent. After placing the stent, the scope and wire were removed from the patient and the X-ray technician stepped in to set up the lithography machine. The maximum number of shocks to the kidney was 2500 shocks and 3000 for the bladder. The X-ray tech explained that more shocks could damage the organs and cause a hematoma.
During the time that the X-ray tech was monitoring the lithography machine, Dr. Garvey answered all of my questions about different types of kidney stones and he explained that 60 ~ 80% of stones are calcium composites and the rest can be one of a few different substances. Uric acid stones are the only type that can be treated medicinally by alkalinizing the urine and dissolving them. He also explained that stones less than four millimeters in size are considered clinically insignificant stones and are not treated.
Case #2: 65 YO m
The patient presented with a ~7mm stone in one of his calyces, an offshoot of the renal pelvis, but the exact location was unknown because the stone was less dense and therefore harder to locate. This patient did not receive a stent because of the smaller size of the stone and instead they temporarily placed a catheter during the procedure which was removed before he left the OR. A contrast agent was injected into one end of the catheter to reach the renal pelvis in order to more accurately locate which calyx the stone was in. Because of the smaller size, this patient received only 2000 shocks as opposed to the maximum.
The machine
Orchiectomy
We also observed an orchiectomy, removal of a testicle, performed on a 36 year old male. Dr. Garvey informed us that testicular cancer occurs in males aged 18 – 35 and with any mass on the testicle, it can be hard to confirm malignancy by biopsy so he plays it safe by removing it because the chance of a testicular tumor being benign is less than five percent. This was the first open surgery I have ever observed so it was very exciting to see. Dr. Talamini performed the surgery with Dr. Garvey coaching her from the other side of the table and occasionally lending a helping hand. Their main tools were a scalpel, cauterizer, and hemostats. They had to take care to avoid a large nerve running through the lower abdomen where the incision was made. Dr. Garvey commented that the patient had a great anatomy because he was fit and lean which made it easier to locate what they were looking for: a tract which leads directly to the testicle. They cut away tissue that they didn’t want to remove and essentially pulled the testicle from the scrotum through the incision in the lower abdomen, cool!
The OR was an exciting place to observe! I also stopped by a different OR where they were finishing up a robotic prostatectomy and I noticed that there was a very different culture in that OR. When I asked Dr. Talamini about why she chose to do a residency in urology, she mentioned that she enjoyed the problems and procedures but that she also liked the people and that Dr. Garvey was a good example of someone she likes to learn from and I understand based on the environment in his OR. Through talking with him, I might have identified a potential problem for us to address: a fully dissolvable stent.
Week 2 – Clinic
Shana Snarrenberg Blog
We observed in the clinic for the first two days this week, this time with Dr. Abern.
Dr. Abern specializes in cancer treatment and so the cases we saw were patients with prostate cancer or bladder cancer for the most part. I was in the room for one difficult conversation with a patient where the patient was being informed for the first time that he definitely has bladder cancer and the tumor is so large that his entire bladder needed to be removed. The patient took it quite well considering the prognosis and Dr. Abhyankar delivered the news in a professional and empathetic manner. She had a rapport with the patient from previous visits leading up to the diagnosis and she was able to leverage that to speak frankly with the patient but with a caring tone.
I was able to observe clinic visits with two elderly patients as well which was interesting for me because I am interested in interacting with the elderly. One patient was an 86 year old man suffering from severe dementia; It was not possible for any of the staff to speak with him or to discuss the procedure with him. He was having trouble with recurring kidney stones and they needed to take a fresh urine sample and thus had to change his catheter which was placed abdominally. The nurse prepped the patient in his wheel chair by moving his clothing out of the way and then tucking in some absorbent material in case of spills. The patient was in distress and kept calling for a nurse. When the nurse removed the catheter, he started screaming, “OW OW OW” and saying “they’re hurting me, they’re hurting me, nurse, nurse, nurse”. It was sad to observe but the fact of the matter was that the staff needed to get through the procedure in the patient’s interest and there was no way to have him understand what needed to happen. The staff did their part to try and work as quickly as possible to minimize his discomfort and the nurse who brought him to the clinic from the nursing home was massaging his shoulders and talking to him to help calm him down. The other elderly patient was also in his 80’s but ambulatory and also completely lucid. He had to wear a condom catheter and urine collection bag and the previous pain he was having was gone. He wanted to not have to wear the collection bag and had hopes of having another surgery like his previous artificial urinary sphincter. Dr. Abern came in to consult on possible options for him. Afterwards, to obtain a urine sample, the nurse practitioner helped him to change his catheter and urine collection bag and at that time, we realized that the bag was rather cumbersome and not completely intuitive to place, a potential problem for us to focus on. Nadine, the nurse practitioner, kindly gave us a sample to take home.
Week 3 – Clinic w/ Dr. Garvey
Shana Snarrenberg Blog
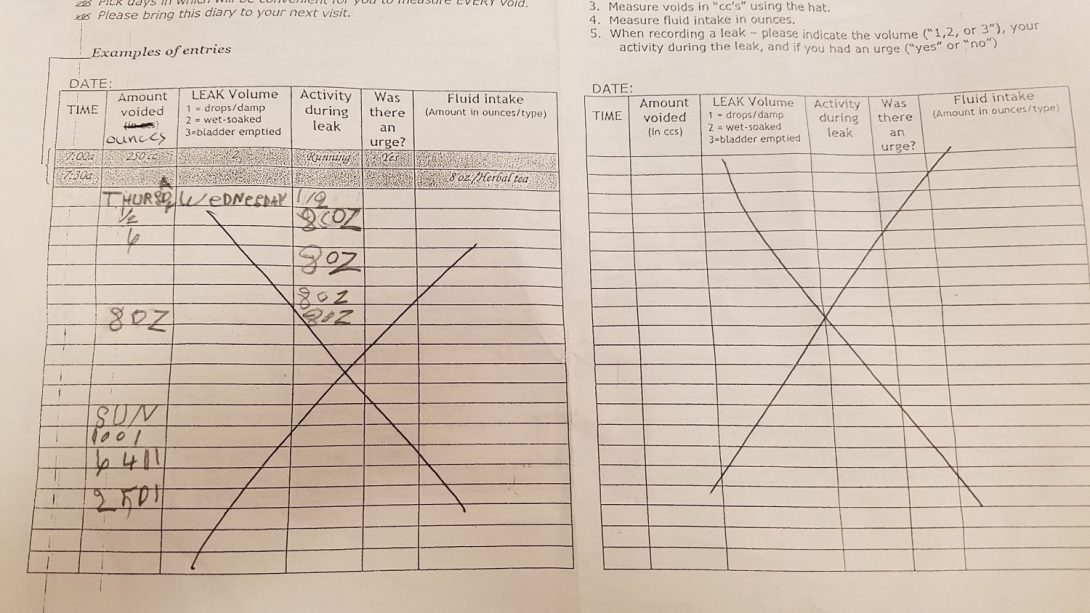
This week I had the opportunity of observing in clinic with Dr. Garvey. First of all, it was interesting to observe the difference in clinic operations with and without residents. Dr. Kocjancic and Dr. Abern have residents in their clinic and sometimes a nurse practitioner as well who see the patients before the doctor. The residents also often give a verbal summary of the patient case before the doctor enters the room. Dr. Garvey does not have residents in his clinic so he reads the patient’s chart, sees the patient, and also orders the prescriptions and labs. Usually when there are residents, they complete the ordering at the end of the patient’s visit. Dr. Garvey had up to three patients at different stages in their visit at a time in exam rooms one through three. He had to manage his time and adjust his ongoing mental task list according to how the visit were progressing and what patients were in for. He communicated frequently with the nurse and medical assistants on staff to coordinate patient visits. However, one medical assistant agreed that the clinic seemed more relaxed with less working bodies present and he said it was especially more relaxed if they were able to get into a good flow like today.
I had the chance to ask Dr. Garvey some questions about potential problems and we discussed 1) the issue of using CDs for viewing scans from other providers, 2) patient error when giving urine samples, and 3) patient errors on voiding diaries.
1) The reason for using CDs to deliver imaging results from one provider to another is apparently a consequence of electronic medical records (EMR) not having the ability to transmit that type of information because of software incompatibility. Dr. Garvey explained that there are many types of EMR software and none of them can exchange information which makes it difficult to deliver images. Written reports can be faxed in but images on CDs have to be delivered in person by the patient taking up the patient and provider’s time.
2) Dr. Garvey had to explain the process of giving a urine sample almost ten times this morning. The key point was that after cleaning the genitals, the patient needs to empty their bladder almost completely into the toilet before collecting a sample in order to avoid bacteria commonly found in the urethra ending up in the sample. Sometimes the patients don’t understand this and they pee directly into the cup resulting in an inaccurate lab result. I asked if it would be helpful to have posters but Dr. Garvey said that in his private practice days, there were posters all around his practice, even huge ones in the bathroom and they would still encounter the same patient error.
3) I had previously taken a look at the voiding diary template which gets handed out to patients and thought that it might be sort of confusing because the boxes to write in are smaller than most people’s handwriting. The pages are filled with a lot of ink seemingly to save space but the doctors and residents handing out this sheet often cross off large portions that they don’t need the patient to use. Dr. Garvey said this wasn’t much of a hassle for him but that there could definitely be a more optimal layout both for the patient and the doctor. The featured photo is an example of a patient’s incorrect use of the voiding diary. I suggested that with all this space, one half page could be a full day’s example to help the patient better understand what information is desired and to record it properly. I plan to ask the other doctors as well about this issue to see which sections they tend to use and which they can do without.
Week 4 – Voiding Diary
Shana Snarrenberg Blog
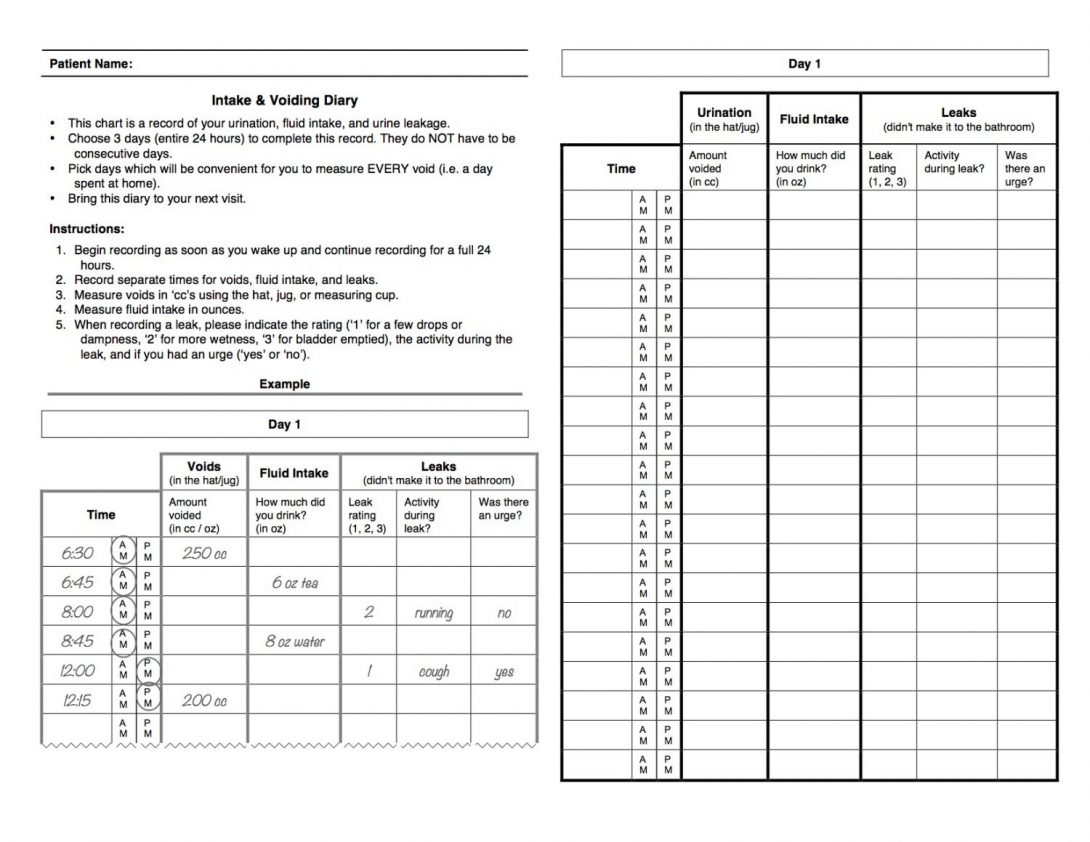
This week, as the Urology team, we discussed our potential options for the problem statement to address. One of the potential problem statements has to do with improving the voiding diary provided to patients to track their urination throughout a 24 hour period. Compliance is low because the patients have a difficult time understanding how to use the current form. Patients often don’t record all their voiding for the entire day and if they do, the times are unclear. Most doctors don’t use a large portion of the form for recording leaking and fluid intake. The form also has sections for recording voiding, leaking, and fluid intake all next to each other without clear distinctions between the three types of occurrences which is confusing. For example, when a patient experiences a leak, it would be impossible to record voiding volume or when a patient drinks a beverage, there should be no need to record anything about leaking. Nadine, the nurse practitioner, also made a suggestion to have AM/PM printed on the form for the patient to circle so that it would be clearer when the entry was made. I implemented these changes and made a new form template which she said she would check with the doctors about and then begin using. The featured photo is the new voiding diary template that I created.
Another issue that she told me about is that patients have difficulty understanding how to complete the Litholink 24 hour urine collection test. She herself had never seen the kit or instructions provided to the patient because she orders the kit, and then the lab sends the kit directly to the patient. I was able to find this information online and I plan to type up a streamlined set of instructions that the Urology clinic can provide to the patient to prep them on what to expect.
Dr. Garvey thought that the 24 hour urine collection test sent to the lab was not a major issue for patient compliance and instead he wanted to see improvements with the Uroflow test. He said that patients have a hard time understanding that they need to arrive for their appointment with a full bladder with a normal urge to urinate. Instead they often arrive too full which affects results, or not full enough. When they arrive not full enough, they often impatiently drink a lot of fluids very quickly and then still have poor results on the test and then potentially even have accidents on their way home. He mentioned that a take-home test that a previous IPD group had been working on has a lot of potential to improve the situation. If patients could take home a kit, they could conveniently use it when they happen to have an urge while sitting at home.
On a separate note, I assisted today for a super pubic tube (SPT) change on a nursing home patient. The patient was non-mobile and on a stretcher and under 60 years old which is young for being in a nursing home. She was not receiving adequate care in the nursing home for her SPT which was leaking due to spasms and so she had a lot of moisture in the area. I was helping to lift her stomach as she was also overweight and the smell was very intense. Apparently she also has a cystocele on her bladder that can be felt through her vagina which should have been taken care of in October but still hadn’t been resolved leaving her with a second urine leak through her vagina. It was concerning to see a patient neglected in such a way. The patient was very nice and compliant with the procedure but had no autonomy to manage her own care. She also could not remember if the tube had been changed and claimed it hadn’t but Nadine discovered that it had been changed. I’m not sure what the solution to this patients issues with care were; It seems like the problem is a systemic problem with public and possibly private nursing homes.
Week 4 – Voiding Diary cont.
Shana Snarrenberg Blog
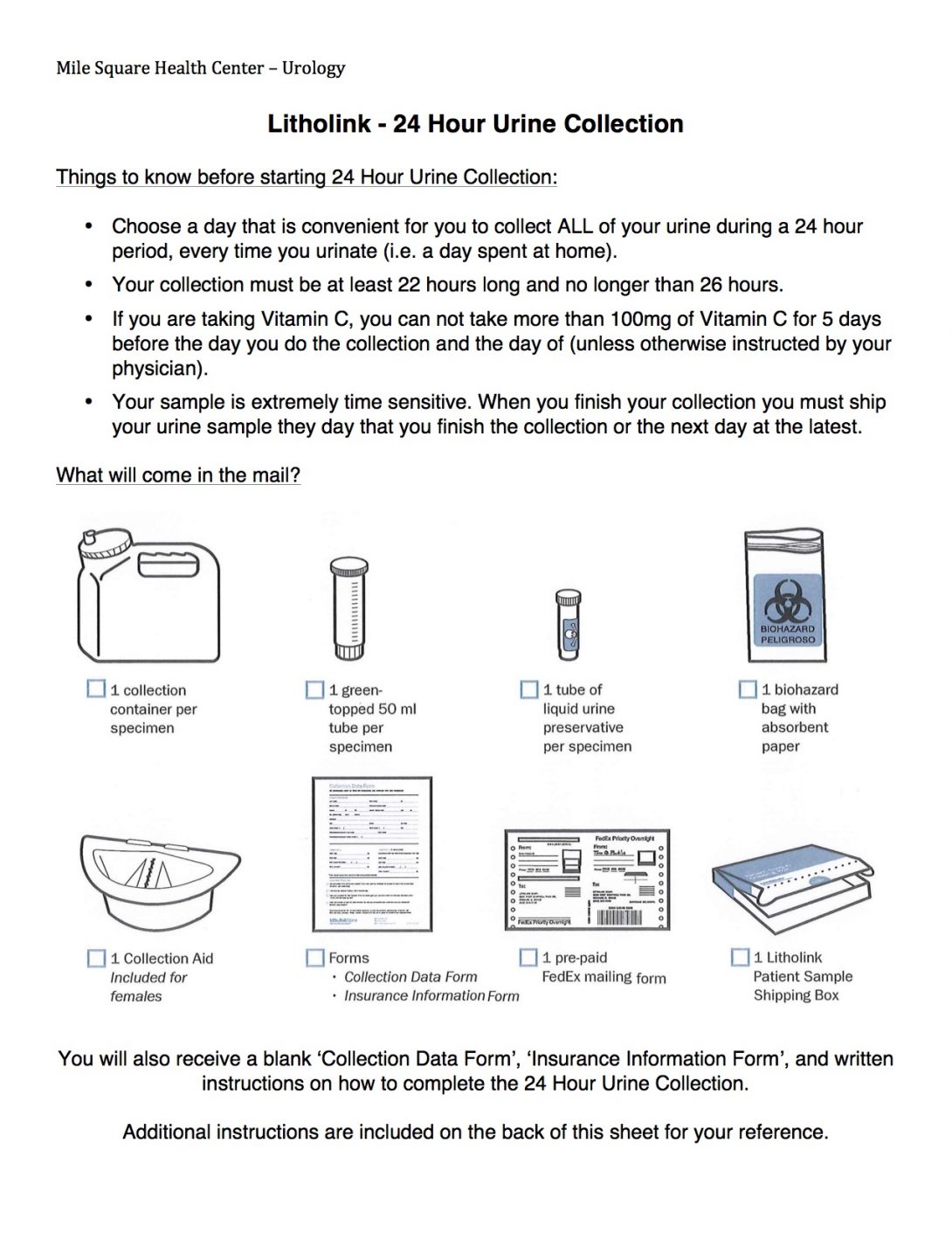
Nadine checked with Dr. Garvey about the updated voiding diary and he gave her the ok so they already began printing off the new version. I decided to make an instruction sheet for the Litholink 24 hour urine collection test as well. Although Dr. Garvey didn’t see much of an issue with compliance on this test, he did say that anything to help patients understand the process better would be welcomed. Nadine felt that the patients were very confused about the test and needed clearer instructions and she asked me to make a set of instructions that were more user friendly. The featured image is a first draft of a set of instructions which I think is more user friendly and I plan to discuss with her on how to improve them even more.
Week 5 – Problem Statements / Patient Education
Shana Snarrenberg Blog
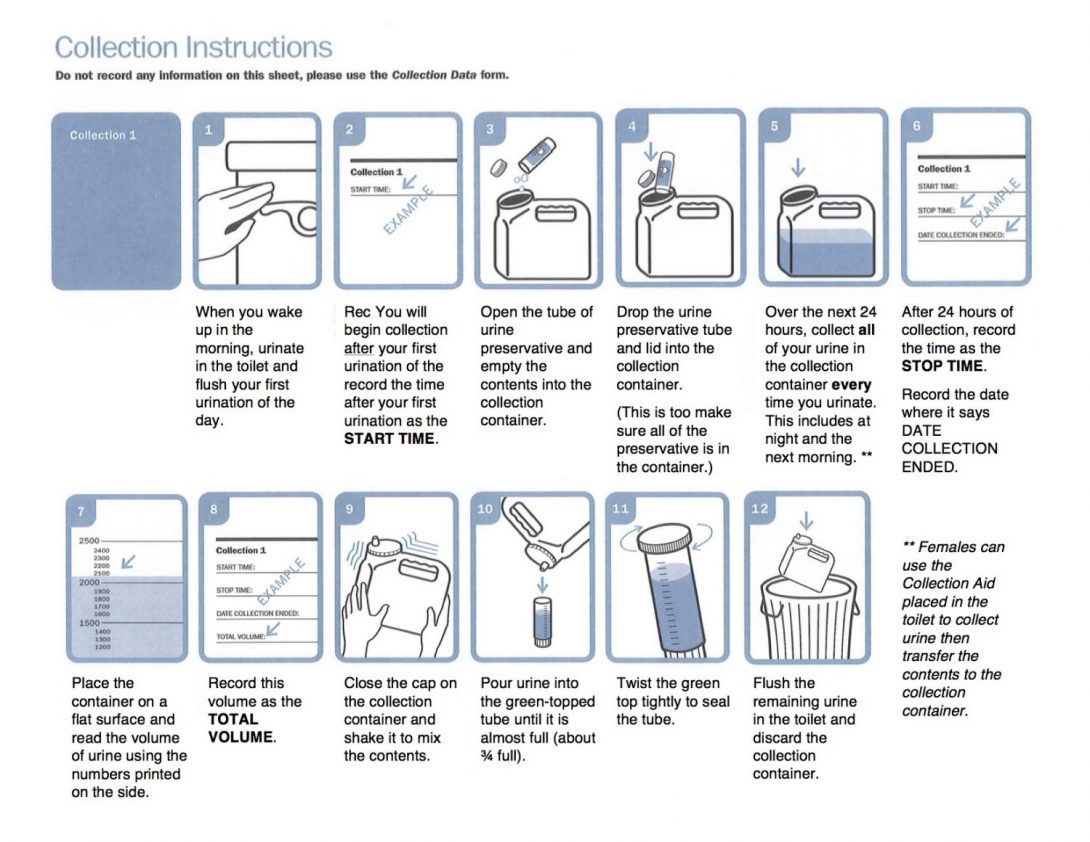
I talked with Nadine, the nurse practitioner, today about the Litholink 24 hour urine collection instructions I created for her last week and got some feedback. She felt like the instructions were too wordy and they would not be useful for her patient population. I agreed that it was very wordy and I made her a new version with more pictures. I decided to just take the relevant parts of the existing instructions and stitch them together and replace the text with an easier to read font and text size. She was happy with the result and plans to give patients this sheet with the lab order sheet that the patients get when they are instructed to complete the Litholink collection.
Another patient education handout that she wanted improved was the pelvic floor exercises handout for men. This sheet was a bad copy of a text-only document which wasn’t that helpful to her patients. Today she demonstrated for me the three exercises that she asks her patients to do: a pelvic lift while laying down, knee lifts while sitting, and also stopping urine flow during urination. She told me a funny story about a patient who took her words literally when she explained the last exercise and told the patient he needed to hold his urine. The patient came back three months later for a check-up complaining that his leaking had not improved and he was holding his urine as instructed. It turned out that he was literally holding his penis to stop the flow instead of using his muscles.
I also presented our problem statement and solution to Nadine. The problem statement we decided on was “To improve consistency of urodynamic testing results.” Part of the solution we are interested in is to come up with a take-home uroflow test which would allow patients to complete the test at home when they have a full bladder and the urge to urinate. Dr. Garvey was explaining that patients often come in with a bladder that is too full or not full enough and the test has to be repeated. Our current design consists of a funnel made out of a soft material such as silicone which would fit onto a tube that contains a flow sensor as well as a chip to store the collected data. Physicians would then be able to download data from the device. So far in my research of flow meters, it seems like most affordable meters are designed for flow rates of 1 – 30 L/min like this one available on Adafruit. Urine flow rate peaks at 1.8 L/min with lower rates for patients with BPH or strictures which is what the test is intended to detect. Flow meters that are designed for lower flow rates for rates such as urine flow tend to be in the three digit range price wise. This is something we need to look further into. Below is a sketch of our design.
Another issue related to urodynamic testing is with the catheter used in bladder pressure tests. The catheter has no way of staying put in the urethra and vagina and often falls out. Nadine says that she has to tape the heck out of the catheter for it to stay. Otherwise, when the patient begins to urinate, the tape will get wet and the adhesive will stop working. The catheter does not have a balloon on it, most likely because that pressure inside the urethra would affect test results. Nadine said that previous groups of students had looked at this problem without coming up with any results. She also explained that it was a nation-wide problem. I’d like to look more into this problem because of how pervasive it seems to be. She told me that there will be urodynamic testing on Friday afternoon so I plan to visit with her then to observe the procedure.
Marta Turowski

Marta Turowski
I have recently completed my Bachelors Degree at Northwestern University. I finished with a major in Cognitive Science along with a double minor in Science & Human Culture and Global Health. I am currently pursuing a dual MD/MBA degree at UIC. My interests lie primarily in the cross-section of patient care, technology, and business.
Marta Turowski Blog
Marta Turowski Blog
Week 1 – Post 1
Marta Turowski Blog

Interventional radiology (IR) is a highly interesting specialty for the clinical immersion program as it is an ideal example of the constant evolution of technology in medicine. Our mentor, Dr. Bui, explained, “If an interventional radiologist is doing something exactly the same more than a few times, something is wrong… they should always be trying to evolve, to discover a faster way, or a way that makes patients have better outcomes”. This concept is inspirational because it provides evidence that it is not physicians stuck in their old ways that create limitations, but it is the technologies that they are provided with that limit their horizons. With this in mind, I have found new motivation to push myself to help provide physicians with a small improvement in their devices, in order so they can make great strides in patient care.
The main concept behind IR is being able to complete a procedure in the most minimally invasive way possible. Usually, this means that procedures are completed through a tiny incision in which catheters, stents, and other small devices can be guided through. Guidance of these devices takes great skill as the only means of seeing their paths comes from imaging devices such as X-rays, MRI, ultrasound machines, and CT scans. This poses the first great limitation that IR currently faces: the issue of visibility. Currently, there is a trade-off between real-time imaging with low quality images, such as ultrasound, and high quality imaging, that can only provide static information, such as CT scans. Creating a device that can give the best of both imaging techniques, high visual quality with real-time ability, would revolutionize the field. It would make procedures faster, safer, and potentially could allow physicians to do tasks currently deemed impossible.
Becoming familiar with the cramped, fast-paced, and energetic atmosphere of the IR department has been exciting. Every procedure is different, requiring a new set of devices as well as a completely different approach. I look forward to the next couple weeks so that I can delve deeper into understanding both the workflows, devices, and processes of the many different procedures that occur in IR.
Week 1 – Post 2
Marta Turowski Blog
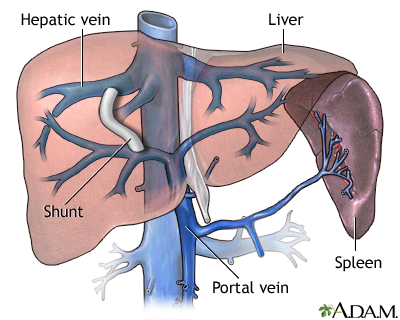
TIPS – transjugular intrahepatic portosystemic shunt
One of the first large procedures we were able to observe was a TIPS placement. This procedure is used to treat portal hypertension. In order to avoid creating more strain on the liver, the TIPS procedure allows the blood of the body to bypass the liver. This is done by placing a shunt made of a mesh-like cage that provides stability to the structure, covered in a thin envelope that provides penetration of the blood into other unintended areas of the body.
The issue with this system is that it can sometimes cause too much blood to reach the heart. When this occurs, the heart is overwhelmed by the return input and can actually cause the body to go into cardiac failure. To counteract this issue, a secondary and tertiary shunt can be placed within the original shunt in order to slow down blood flow to the heart. This essentially creates a “tube within a tube” effect that slows flow. Some issues that were presented with this “fix” is that it is complicated and takes many steps. It is also difficult to control how much flow is actually reduced by. It would be wonderful to figure out a way in which to do this in a simpler manner. For example, in gastric procedures, balloons can be placed and altered over time by inflation and deflation. This changes the amount of available space in the stomach. Similarly, this idea could be applied to the TIPS shunt to alter flow in a more precise way within an artery or a vein. Another potential approach would be to create a valve system that could be narrowed to alter the entry or exit of the shunt, essentially creating the same effect. I hope to explore this idea further in the weeks to come and discuss the potential solutions that may prove to be effective in solving this issue.
Procedure board
A central aspect of the IR environment is the procedure board. It is centrally located, creating a natural space for people to gravitate to. It is also essential to communicating to all staff members the overview of the current happenings of the department and what will happen over the next few hours. It contains an overwhelming amount of information from room numbers, to staff members names, to procedure details.
A glaring issue to me is that this board is still a simple white board with magnetic stickers placed on it that are updated by hand. Across from this board hangs an electronic version of this board that is linked to the hospitals electronic medical records (EMR). While this board is helpful, because of the information it provides and because it is automatically updated by the hospital’s EMR, it has limited flexibility. Essentially, this electronic board is not able to be fully customized in the way staff members are accustomed to. Dr. Bui insists that a new board would have to be able to be modified so simply that it could be done by the swipe of a hand. He describes something best summarized as a giant touchscreen. I believe updating the current electronic board to meet the customization needs of the department could improve patient safety and department efficiency.
Week 2 – Post 1
Marta Turowski Blog
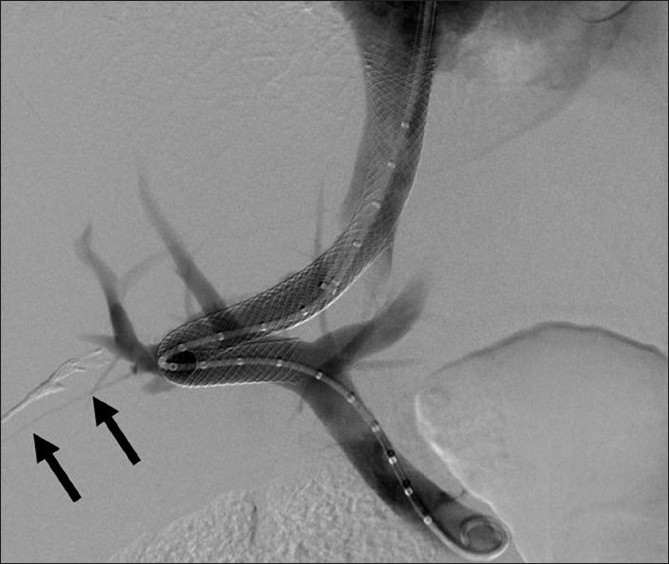
TIPS Update
After discussing the potential solutions for over-shunting blood to the heart after a successful TIPS procedure, Dr. Bui informed us that a new shunt has just come on the market! This shunt helps alleviate the previously described problem as it is a size 8 when it is placed. If the flow rate is deemed too little, it can be permanently stretched and locked into a size 10 by inflation of a balloon within it.
While this is an exciting development as it confirms the issue that we discussed as being worthy of finding a solution, this new device does not fulfill all the necessary criteria. First, the change in size is permanent. There is no means to reduce the size once the shunt has been stretched to the larger 10 size. Moreover, the shunt only has two distinct sizes. A more valuable improvement would be a shunt that can be altered to be a variety of sizes. Additionally, this ideal shunt would be easily adjustable many times and would not be locked in a certain size once manipulated.
Another interesting aspect of the procedure we got to observe this time was the measuring of the necessary length of the stent. While the uncovered mesh portion of the stent is standard, the length of the covered portion is variable. This is determined by first placing a marking pigtail catheter that not only helps determined needed length for the shunt that is to be placed, but it also provides the ability to inject contrast. A similar device is a marked wire that has the disadvantage that it does not allow for one to inject contrast. These two devices are good examples of how a simple addition to a devices ability can revolutionize its purpose.
Week 2 – Post 2
Marta Turowski Blog
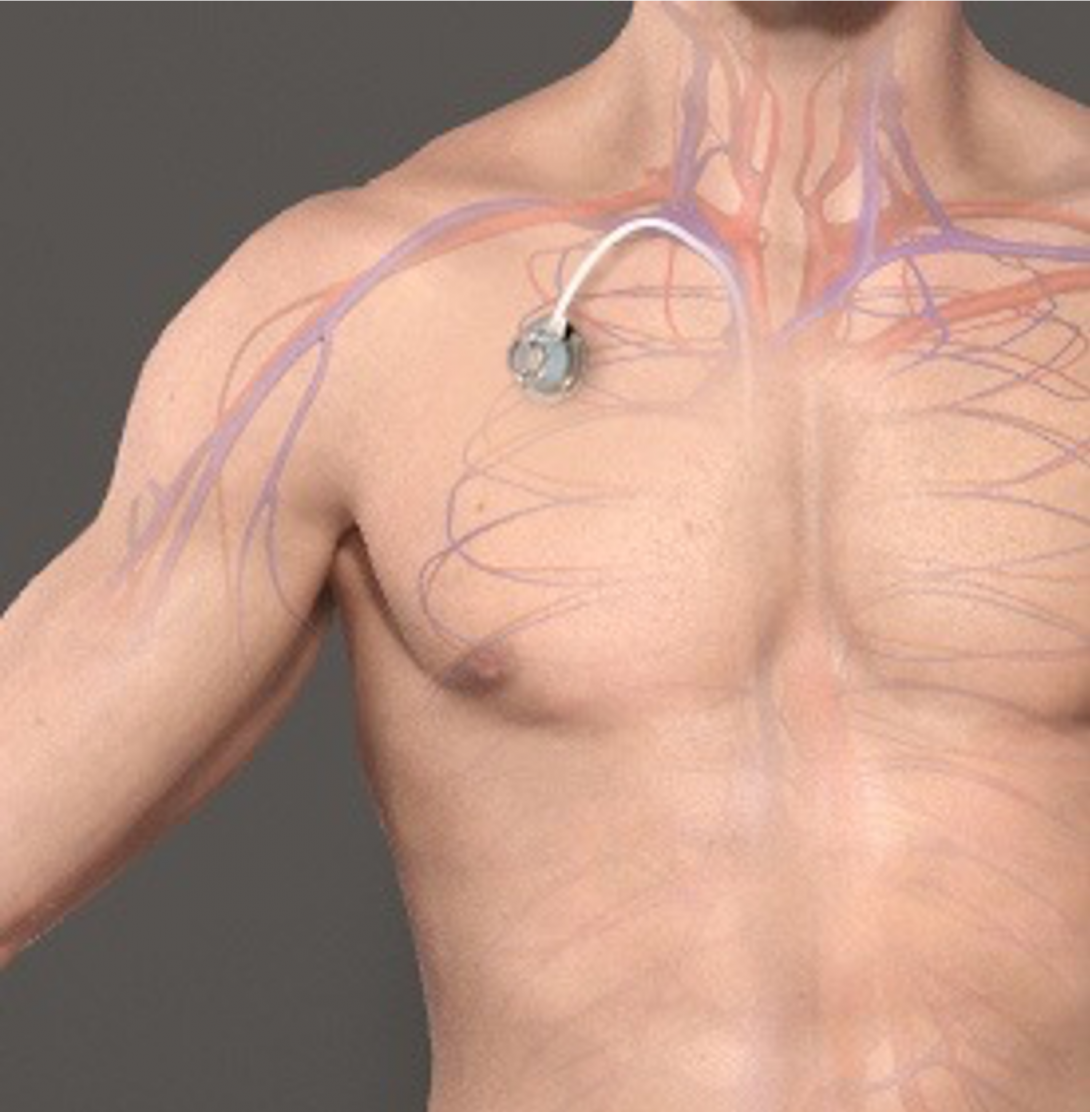
Chest port
Today we witnessed a very routine procedure for the IR department that had fascinating medical device applications. When putting a chest port into a patient, a special port is placed under the skin that leads to the inferior vena cava. This provides the ability for physicians to administer drugs that can potentially harm small vessels straight to a large vessel in a less invasive way.
What was most fascinating about this was the material which the port is made of. The septum technology that is palpated by a clinician is where drugs are later injected. It is specifically backed with a hard material so that the administrator does not pierce through to gentle organs below the chest port. The septum itself is made of a fascinating, highly resilient material that essentially reseals itself so that the integrity of the structure is not compromised over time as it is used. This is accomplished by using a special needle that is called a non-coring needle. Typical needles are coring, which means that the center is hollow and leaves a puncture hole in whatever material it pierces. The special non-coring needles have their holes on the side of their shaft so that they can still administer drugs, but do not leave a hole in the septum. This leaves the septum functional for hundreds of uses and decreases the likelihood of infection. This device is an amazing example of thoughtful design that takes into account the need for repetitive use and safety of the patient.
Week 3 – Post 1
Marta Turowski Blog
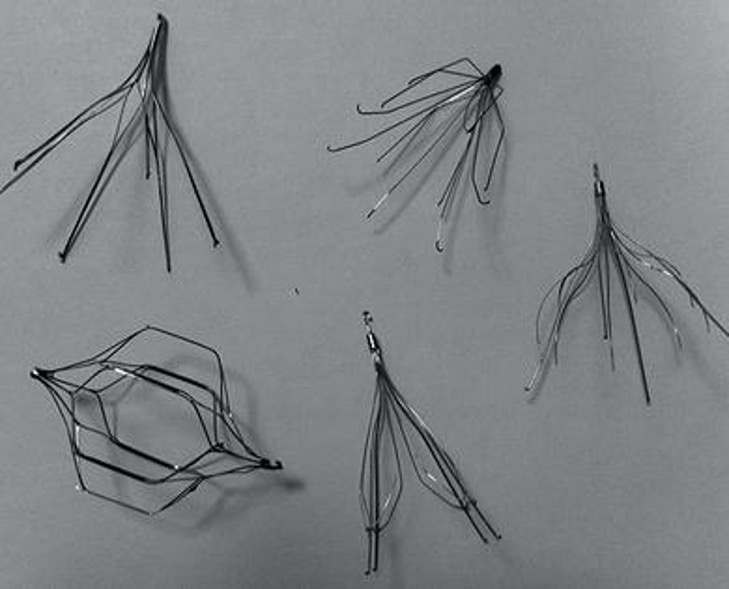
Inferior Vena Cava (IVC) Filter
After having several opportunities to watch an IVC filter placement, our group has finally had the opportunity to learn more about the device and the procedure. Essentially, the device is placed in the inferior vena cava in the attempt to block blood clots from migrating from the periphery of the body to the heart. These clots are caught in the filter’s delicate design and are then naturally desolved by the body. The filter is typically kept in the body for some time and then is expected to be removed after a patient is no longer in a situation that they are in a high level threat for having blood clots. While this seems like an elegant solution that has greatly improved with time, there are still many major flaws with the design of the device. Some of these issues include, but are not limited to:
- The device has hooks on its feet that help anchor it in the blood vessel and keep it upright. These sharp hooks can hurt the sides of the vena cava and make it difficult to remove the device. Actually, the hooks are so sharp that they can penetrate straight thorough the sides of the blood vessel, creating a potentially very serious situation for a patient.
- The device is capable of migrating within the blood vessel far from its intended location. This too can be dangerous for the patient as the device is placed precisely for best clinical outcomes. This migration also leaves the blood vessel vulnerable to more likely injury by the sharp anchoring hooks.
- The device shape has been changed and updated many times, but it is still not ideal. It does not catch all of the clots that clinicians would like it to. The trick in this is that it should not catch all clots, but only the ones large enough to cause serious issues for a patient. The design of the filter should also cause minimal change to the flow of blood past it, as this can affect efficacy of the heart.
- The device can become clogged with clots and not let any blood through. The clogging is at such a fast rate the body can not break down the clots quickly enough.
Week 3 – Post 2
Marta Turowski Blog
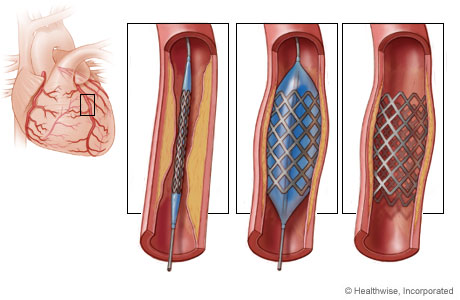
Stents
Similar to inferior vena caval filters, stents have gone through many generations of their design. Their placement is essential to maintaining a vessels functionality by keeping it open. A problem that typically occurs is that they can begin to stenose or close. When this happens, the patient is at risk for receiving less blood where they need to. This is a potentially dangerous situation. Speaking with some of the clinicians, they suggested a device that can electronically alert physicians when a stent is becoming occluded. This may mean that it can report a narrowing of the device or a change in flow. While change in flow may be an easier measure to detect, this is an indirect measurement of the actual problem that needs to be monitored. Flow rate is also altered frequently due to simple things such as a patient’s level of activity. Therefore, it would create many false readings. Due to these issues, finding a way to measure the narrowing of a stent would be preferential.
Something worthy of consideration is the need to replace batteries if this sort of device was electronically operated. This problem could be potentially solved with piezoelectrically powered devices. Devices integrated with this are just coming on the market. For example, the new generations of pacemakers that are now available.
Week 4 – Post 1
Marta Turowski Blog
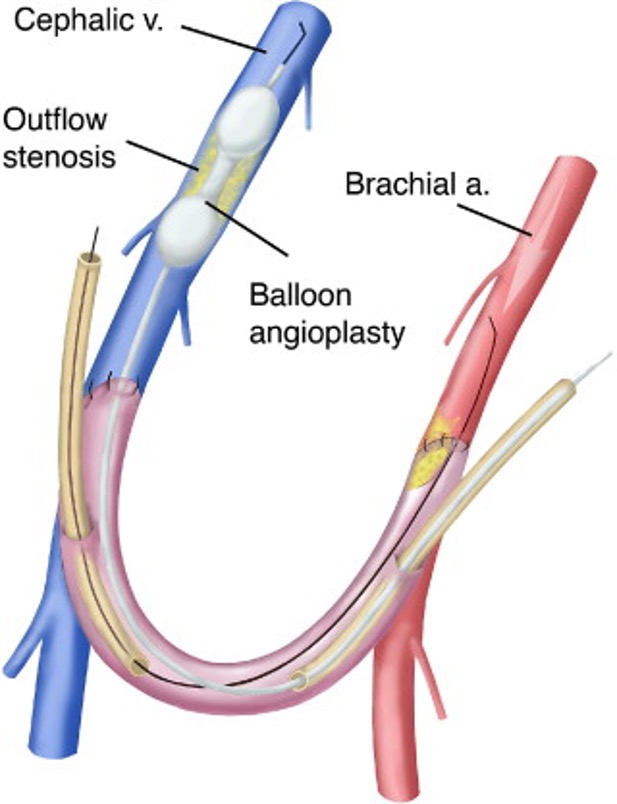
Dialysis Fistulas
A dialysis fistula is a connection between an artery and a vein that is made surgically that improves the ability of a patient to receive dialysis. They can be made with a graft made of foreign material or they can be made with a patient’s own natural vessels.
An issue with all foreign object placement in blood vessels is that over time, the body attempts to remove this object. Since actual removal is impossible, the body tries to find a way to block this foreign object off. Typically, in the case of fistulas, this means that the vessel begins to clot off the area where the graft has been placed. To fix this issue, physicians have a variety of mechanisms to try to declot a fistula. One method to do this is performing an angioplasty. This is a procedure that uses a balloon to clear a vessel of debris. What I found particularly interesting was the differences in possible balloons that could be used for this procedure. There are compliant and noncompliant balloons that are inflated by a special device called an insufflator. This device is cumbersome to use and requires a significant amount of manual force by the user to actually inflate a balloon. Compliant balloons are similar to classic birthday balloons that can continuously increase in size as more air or pressure is added. Non-compliant balloons blow up to a certain size and remain at that size. Further addition of air merely increases the pressure of the balloon and makes it harder, but does not increase its size. The helps make sure a vessel is not over-stretched or burst.
The angioplasty procedure is currently sufficient to improving unclogging of vessels, but it is not ideal. Perhaps the balloon’s design could be improved to better clear blood vessels. Also, it is a consideration to think about other uses of the balloons. Maybe these balloons could be used to remove IVC filters. For example, by inflation of the balloon in the filter could help dislodge a filter and maybe could be wide enough to be used to pull the filter out of a vessel.
Week 4 – Post 2
Marta Turowski Blog

The Process of the Lead Apron
So far, I have described many devices used within the IR department, but have said little about the efficiency of the processes. One area that I find extremely cumbersome is what I will call “the process of the lead apron”. Lead aprons are necessary coverings that members of the clinical staff have to wear during most IR procedures. They help limit the amount of harmful radiation exposure that clinicians are exposed to. While their use is essential to the safety and health of everyone, there are many aspects of their use that may be reevaluated in order to improve efficiency and or health.
Some of the considerations include:
1. Lead aprons currently only cover the core are of a person’s body. There are head pieces available, but few members of the staff wear them. The portions of someone’s body that are uncovered are exposed to very harmful radiation and their exposure could potentially be minimized by better designed aprons or with more strict regulations on what is required of clinicians during procedures.
2. Lead aprons are extremely heavy and uncomfortable. Perhaps there are some designs that would better distribute the amount of weight that is concentrated on one area of a wearer’s body. There are already some variations available such as ones that only hang off someone’s shoulders versus ones that hang off the shoulders and the waist.
3. The process of putting on a lead apron is very tedious and slow. The aprons are all hung on two rods, which makes it difficult for more than one person to access their lead at a time. They are packed together and are on non-removable hangers. All of these things combined, slows down the already sluggish process of removing and putting on lead aprons. Usually these aprons have both velcro and buckles for both parts of the apron. It would be good to look into better mechanisms of closure of the aprons so that this part of the process could be sped up.
4. There seems to be a constant struggle of trying to find “your” lead. People have unique radiation sensors they clip on their lead that is later used to measure the amount of radiation exposure that a person has experienced. It is important to maintain safe levels in staff. Often, people swap lead and then do not swap out sensors, causing inaccurate sensor readings. By better labeling lead or having people be responsible for purchasing their own lead could save people from this safety hazard and from the constant struggle of finding the lead with their sensor.
Generally, clinicians make the best out of a frustrating process. I believe some improvements in both the design of the lead, the storage of the lead, and the processes around lead could improve safety and efficiency alike.
Week 5 – Post 1
Marta Turowski Blog

Paracentesis
One of the most common procedures done in IR is paracentesis. This is the draining of a body cavity of built up fluid. Usually, this is done with a pigtail catheter. At the very start of our rotation our group had a discussion about some of the short comings of the process. We discussed the fact that the collection bottles are glass and can potentially be dropped and broken. They are also not as efficient in collecting fluid as possible and are sometimes difficult to discern when they are full. Furthermore, we saw that the bottles can lead to dripping of fluid and potentially spreading infectious substances at both the valves and the actual site where the hose connects to the patient.
It was exciting to see the innovation thoughts we had were shared by others as this week a device representative came to visit the office and discussed their new line of paracentesis devices. These devices were made of a new soft plastic material that could avoid the need to solidify the collected fluid as is usually done now for waste control measures. They also eliminate the fear that the bottles will shatter if dropped. Additionally, the bottles are pressurized to promote rapid fluid collection and even have an accordion plastic indicator that shows when the pressure is “used up” within the system and is no longer very effective. Finally, the valves on both ends of the tubing system were improved in this new model to prevent dripping. It was very rewarding to see that the experts in the field thought similarly about the shortcomings of the device as our group. It served as a good example that we are capable of coming up with powerful, useful solutions.
Week 5 – Post 2
Marta Turowski Blog
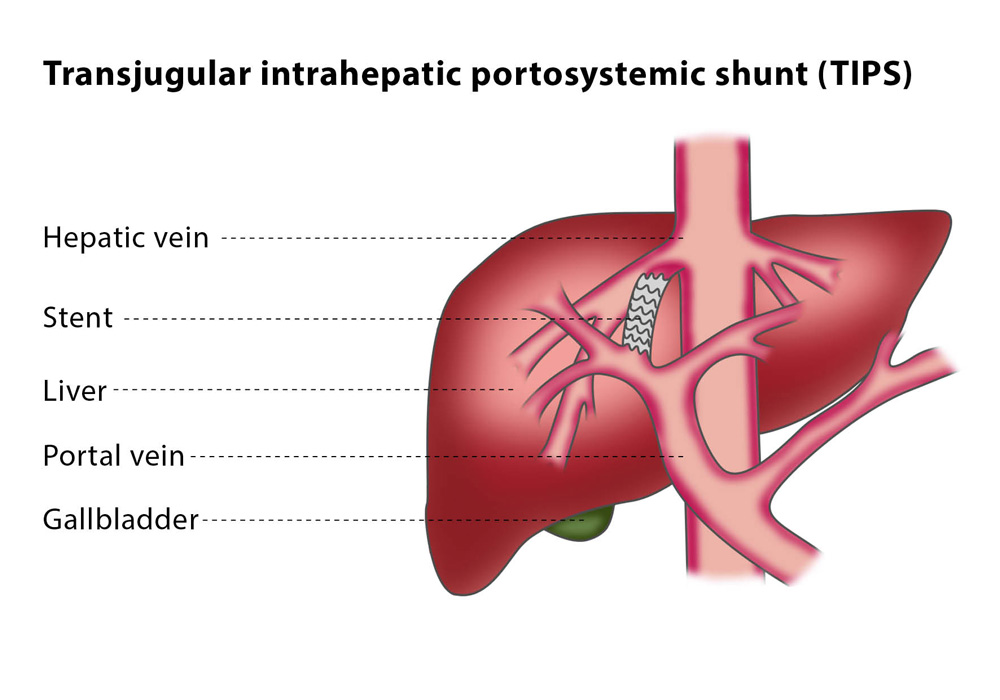
TIPS – Part 3
This week we saw a complication that can possibly happen with a TIPS procedure and it spurred interest in a new type of stent that could be created. Sometimes, patients that receive TIPS procedures get too much blood shunted past the liver and it can cause major problems for the body. For example, a patient can have encephalopathy or experience right heart failure due to a TIPS. In order to combat these issues, the stent placed for a TIPS procedure has to be narrowed. One of the attendings explained to us several methods for narrowing the stent. After hearing all of the methods, it became clear that all of them are essentially “workarounds” in that there could be a simpler device created to serve their purpose. For example, one of the methods is opening a stent partially on both of its ends to wedge it within the original stent. This is difficult to do and can still slip out of the original stent. Another method involves deploying two stents, one small and one large. The small one pushes against the large stent narrowing its diameter.
A stent with a thick lining could serve this purpose in a simpler manner. It would be easier to deploy. Something that is important to consider is that whenever placing a stent within a stent there is a chance of it slipping past and dislodging from its original location. Therefore, the new stent design would need a method to grip the interior or sides of the stent so that this problem could be avoided. This is an interesting stent problem that would be valuable to look into.
Mike Yamakawa

Mike Yamakawa
Mike graduated from Johns Hopkins University with a degree in Biophysics in 2014. In college, he engaged in various technology projects, including a fellowship to evaluate didactic methods in biophysics using an open-source Java viewer of macromolecular structures. Through another grant, he also studied the effectiveness of third-generation ventricular assist devices as a destination treatment for heart failure, alongside an evaluation of an adjusted eligibility criteria for heart transplantation. Technology in education and healthcare is one of his growing passions. Before attending medical school, he took two years off to intern at a start-up pharmaceutical company in Baltimore – an opportunity that allowed him to gain a perspective of medicine in an industrial and business context. Alongside nine other members of the company, he aided in achieving FDA approval for a life-saving pediatric orphan drug in the hepatology space. His goal is to graduate with an M.D/M.B.A to work as a clinician-entrepreneur.
Mike Yamakawa Blog
Mike Yamakawa Blog
Keeping an Eye on clinical needs
Mike Yamakawa Blog
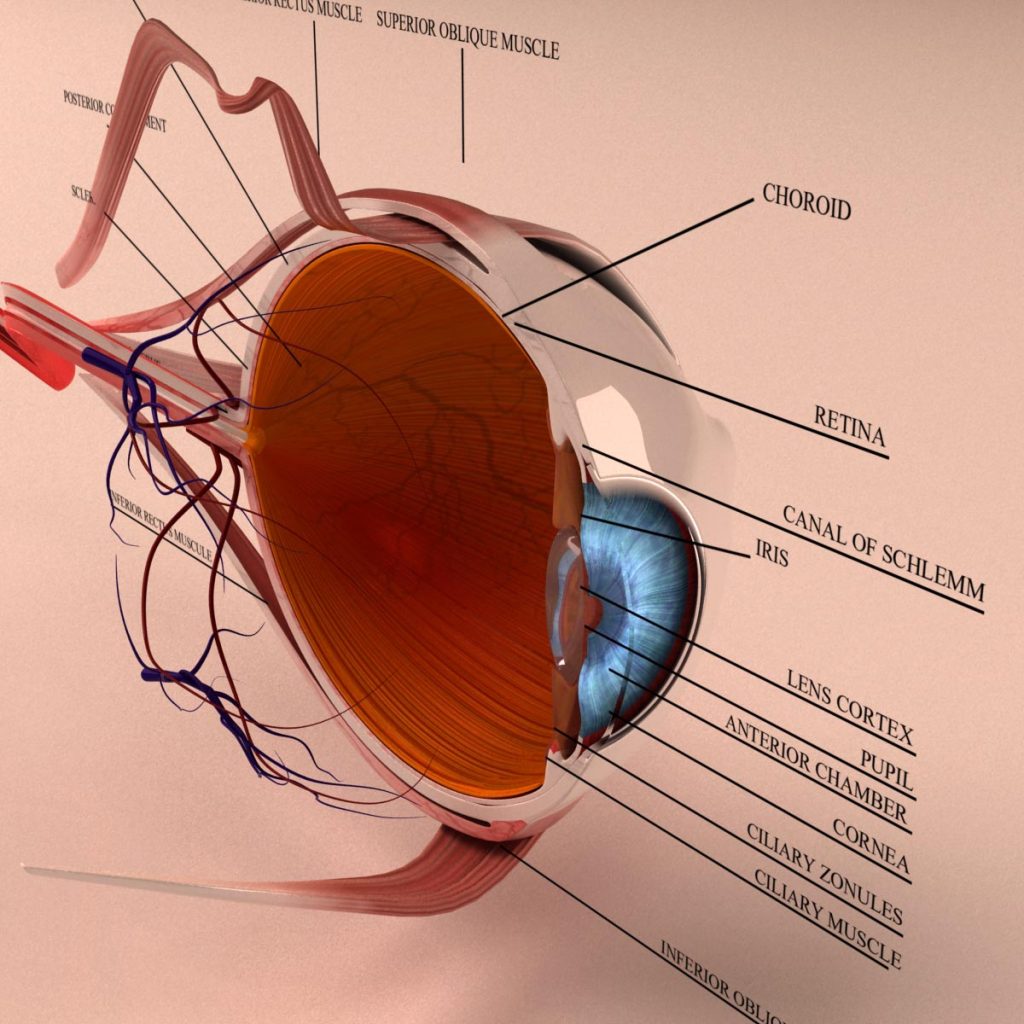
First blog post here… I would say that warrants a quick introduction about why I chose Ophthalmology before we proceed. Prior to medical school, ophthalmology to me meant LASIK and free eye drop samples– nothing much more than that. While many of my friends set their career direction towards this field, I never understood how one can be fascinated by what seemed to be an uncomplicated organ (it’s just an eyeball, right?).
Enter anatomy. Fourth nerve palsy, orbital fractures, hydrocephalus-induced papilledema, foveal-shift caused by retinal detachment… The eye is literally multi-layered and faceted, bridging our outside world through a carefully constructed apparatus that translate light into signals that travels through the optic nerve into other elaborate designs in our brain. Ophthalmology (proud to say I can finally spell this without spellcheck) is meticulously concerned with not only the eye, but its inputs and outputs, and we have many man-made apparatuses that help visualize and measure these things. A complicated puzzle can be born from such a simple-looking structure– this is what got me interested in ophthalmology.
Anyways, I think the best way to get my clinical observations and eye-deas (too cornea?) across is to write posts in list form. These are the four main areas of need that I would like to assess during my rotation in the clinic:
- Eye care technology: This includes slit lamps, topographers, tomographers, hand held pediatric microscopes, light diffuser, anti-VEGF therapy etc. All of these are used to not only visualize the surface and inner compartments of the eye, but also test visual acuity and eye muscle function.
- Patient Education: From what I’ve observed, there is a slight disconnect in information exchange between the physician and patient as seen in other fields, mostly because of the technical component of medicine that is hard to communicate in lay terms. However, there are solutions to bridging this disconnect to make information as accessible as possible for patients. Concurrently, due to UIC’s demographic, there are also Spanish speaking patients who are difficult to explain things to for obvious reasons– but there are certainly some ways around this as well.
- Ergonomics: This is a big topic in ophthalmology because many residents and attendings are complaining of back pains and cervical nerve pinches resulting from poor posture in practice. The design of the slit lamp and other image technologies require physicians to bend forward and strain their neck to look through– while there may be a technical component to the lack of adaptation in design (perhaps a limit in length for which the device works optimally), there may be a few “add-ons” that can help physician reduce some strain.
- Patient Flow: In any clinic, this is an important thing to talk about, both for patient satisfaction and business. The Pediatrics eye clinic at UIC has a show rate of about 60%, down to 40% on particularly bad days. This creates scheduling problems and increased waiting times for patients. Furthermore, CERNER, the EMR system used by UIC does not have a good interface for ophthalmology cases.
Innovation =/ technology
Mike Yamakawa Blog
Today, I want to focus a bit on patient education and patient flow, two areas in ophthalmology that seem to be replete with shortcomings.
Patient education:
The orientation of the eyeball is a bit difficult to understand, let alone the physics behind optics. If the inferior oblique muscle is not functioning, in which direction is the eye overcompensated? If the lens is flatter, do you see further or closer? These are things that ophthalmologist have to routinely explain to their patients, who may often leave the office still confused about their own condition. Admittedly, even I was a bit lost when Dr. Azar– my mentor during my rotation through the pediatric ophthalmology department– was explaining why a patient’s eye was esophoric and exophoric (eyeball deviated in or out) depending on the distance at which he was focusing.
To add to this, almost half of the patients we saw in clinic were non-English speaking (mostly Hispanic). Despite this, there were no tools used in the office to augment patient education– no visuals or translation assistance. There seems to be a wide room for innovation in this regard.
Patient flow:
We were done with the our A.M patients at 3 P.M– over three hours behind schedule. The doctors had skipped lunch and seemed to share the same frustration that patients in the waiting room were displaying. Parents’ phones were running out of battery and the kids had exhausted all use of the magazines in the rack. Today was a particularly bad day, according to Dr. Azar. But this inconsistency is rooted in the unpredictability of patient behavior. The show rate in this specific clinic hovers around an average of 60%. This of course means that on some days, like today, the show rate can rise to 80%, and on others it can be a quiet 30%. This is, for obvious reasons, a nightmare for scheduling.
Furthermore, scheduling is further complicated by the diversity of tasks needed to be done during appointments– some patients may need to have their eye dilated (adding an idle half an hour to their outpatient stay), others do not; some may be post-op follow ups for a quick look at the eye, while others may be first-time patients who have an underlying genetic condition like Duane syndrome that requires some additional diagnostic steps. Either way, the nature of the appointment, which may not be known until the doctor actually sees the patient, dictates how long it is, making scheduling difficult to operate rigidly.
Glaucoma and Oculoplastics!
Mike Yamakawa Blog

I know I’m going against the rules, but I’ve decided to work on a small project this weekend. I’m designing a poster that will be placed in each of the seven clinical offices owned by the Glaucoma unit, which will help patients identify one of many eye drops they need to keep track of. The over 50 eye drops used by ophthalmologists look the same, and labels can be hard to read. There’s very little we can do about that… and the pharmaceutical companies responsible for their designs are under tight regulations. What we can do though– and this seems to be a general theme in clinical innovation in relatively low budget settings– is to empower patients with better tools to take control of their own healthcare. A poster that aesthetically (maybe chromatically) categorized each of the bottles seem to be an easy, cheap solution. (Sorry, Clinical Immersion directors, this will be my only project during this program I swear).
Glaucoma is a condition in which the fluid pressure within the eyeball gets very high– it can be very common amongst diabetic patients. Patients are therefore plentiful in the Chicago area, and more often than not, the clinic is packed with patients. This makes patient flow, yet again, a very relevant issue for needs assessment. However, today I want to talk more about the equipment and technologies ophthalmologists use to diagnose and treat diseases of the eye. I’ll be reflecting on my experiences in the glaucoma unit and oculoplastics. First thing I noticed about Glaucoma was that there was at least one anatomical model of the eye in each office. They certainly weren’t just decorative; Dr. Goldmann, the second year resident I had the pleasure of shadowing, used them regularly to explain the underlying physiology and treatment techniques to help patients understand their condition. This is compared to other ophthalomology departments, which lacked them. Quick research showed that these models can cost as much as $100-250. Perhaps there are cheaper ways to manufacture them?
In a short interview with Dr. Goldmann, along with cursory conversations with others, it became clear to me that the slit lamp that every ophthalmologist learn to use is– for now– in its most evolved state. I asked each doctor I had spoken with if there was one thing that they could think of that could improve the slit lamp. All of them replied no. There was a unanimous agreement that a camera be installed in the slit lamp for photographs or for other viewers to see on a separate screen. That’s all a matter of whether the state would fund such a thing, though. There’s only one in the entire ophthalmology department (specifically in the clinical trials offices).
While the scope itself may not be problematic, that’s not to say that the position of the slit lamp is optimal. Far from it, actually. Cervical nerve pinches and backaches are a real problem amongst ophthalmologists, who strain their spine to look through the scope. I even noticed that since there was so little space between the patient and doctor when looking through it, Dr. Goldmann– a relatively tall woman– had to adjust her legs to the sides and twist her torso around to look through. There’s something very unnatural about this stance.
Oculoplastics is a bit different from other ophthalmology subspecialties– they deal with everything but the eyeball. So that means, eyelid, orbit, eyelashes, tear ducts and whatnot. The first thing they do with many patients is take a high resolution photo with a common DSLR camera for documentation. Afterwards, in the office, they make multiple distance measurements like the palpebral fissure (how much the eye is open) and MRD (distance between the pupil and top of eyelid). Physicians reflect on their own experiences and intuition to estimate these values without a ruler, and often times, I realize, the measurements are different from doctor to doctor.
Oh, also, they still use CD-ROMS to share radiological images within the department. Like… what.
A little on vitrectomies
Mike Yamakawa Blog
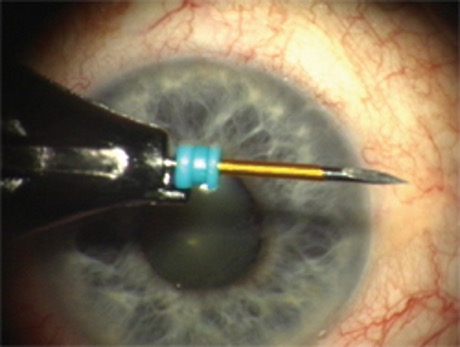
One of many great things about the doctors involved in Clinical Immersion is that they’re incredibly enthusiastic about innovation– always suggesting ideas and pointing out inefficiencies in their own clinic. This week was more about understanding current ideas of innovation and research brewing within ophthalmology. We visited the department labs and even attended an ophthalmology alumni conference on Friday. Free food included!
Dr. Liederman, a retina specialist, took us to the OR on Wednesday. We observed two vitrectomies, a procedure that helps mend a detached retina. They do this by infusing gas or oil into the fluid-filled eyeball, while taking the fluid (“vitreous humor”) out. The gas eventually pushes the retina back against the posterior wall of the eye, allowing it to reattach and heal. To begin the operation, three or four cannuli are inserted into the eyeball; these are four openings that allow for the insertion of other surgical instruments, including a fiber optic light source, forceps, oil/air injection equipment etc. Since an operation of the retina requires equipment to go through the humour, I can’t really think (at the moment) of more minimally invasive strategies than using cannuli– it’s a rather elegant way to perform sutureless surgeries on the eye. However, there is something to say about the endo-illumination options during vitreoretinal surgeries.
There are multiple factors to consider when discussing endoillumination. For example: 1. angle of illumination, 2. light source, 3. phototoxicity.
Generally, retinal surgeons has forceps in his dominant hand, while holding a focused illumination in the other. This allows him to control the direction of light towards the working area view. The most common means of illumination involves a light pipe, which allows the heat to stay behind at the light source and conveys the light to the posterior chamber of the eye through fiber optics. However, phototoxicity can still occur via thermal, or even photochemical, damage (this happens when thermal deposition is higher than the rate of thermal dissipation). More commonly, the light source has shifted from halogen or metal halides to xenon, which has a higher intensity. This was to address the reduced transmission of light after the advent of light pipes.
Surgeons recently have enjoyed the use of wide-angle illumination, which allows for a greater illuminated field of vision– this is done with a conical tip that delivers the light from fiber optics uniformly in all directions. However, this “diffuse” illumination technique can prove to be less effective in viewing a viscous fluid like the vitreous. When Dr. Liedermen needs his other hand for a delicate operation, he would typically forgo the use of focal fiber optics and use what they call a “chandelier,” or diffuse illumination to free his hand.
A variety of instruments are currently available to supposedly help out surgeons with illumination, including illuminated forceps and picks. However, there is a tradeoff with these instruments. They can fail to provide enough or emit too much illumination; the light may not be illuminating the right locations; and an unforeseen consequence could also be shadow generated by the instrument itself. Some available fiber optic devices use dual fibers to eliminate shadows by shining light from two directions.
Dr. Liederman also performed a few cataract removals, sort of out of convenience since he was already working with the patients’ eye. Cataract surgeries, the most-performed surgery today, have evolved drastically in the past few decades, but innovation in this area seem to have stagnated– the only reason being that its already incredibly safe, cheap, and effective…So there’s no reason for pharmaceuticals or academic institutions to spend money on a fully evolved product. Today, surgeons use a technique called phacoemulsification, during which an ultrasonic wave is emitted by a handpick equipment, breaking down the lens material. The pieces are then aspirated with a tool called vitrectomy cutter. This has its needle opening on the side, an innovative measure to allow surgeons to see the aspiration occurring in the vitreous.
Back to the vitrectomy… again, the eye is filled with either gas or oil to help reattach the retina to the posterior wall of the eye. (Its worth mentioning that vitrectomy is performed for other cases as well, including diabetic retinopathy, macular holes etc.) There are two gases approved by the FDA for this purpose– C3F8 and SF6. Eventually, the gas is absorbed by the eye, only to be replaced by aqueous humor that your eye constantly produces.
Dr. Liederman posed a simple, yet important question: What makes a “good” gas for this procedure?
After a slow start, we began to brainstorm a confluence of factors that contribute to “gas innovation.” It should be a gas that’s obviously not toxic to the eye. It should also be able to be absorbed by the eye, as the eye fills with natural fluid again. It should have a good shelf life for storage, and should not be corrosive to existing equipment.
What could make a “better” gas than what we have right now? Currently, the infused gas makes the patient’s vision very poor, at least until all of it is reabsorbed– the reason being the gases we use has a different refractive index than vitreous humor (n~1.33, since humor is basically water). So perhaps finding a gas that not only checks off the aforementioned parameters for a “good” gas as well as has a refractive index comparable to water (not sure if that even exists) can be an even “better” gas. If that doesn’t exist, possibly some dissolvable medium that helps change the refractive index temporarily.
Another option is to use silicon oil. It is long-acting, quicker to recovery, doesn’t expand or compress by ambient air pressure, and doesn’t require patients to keep their head face-down an hour after surgery (a measure to keep the gas bubble to the posterior of the eye). However, the oil is not naturally reabsorbed by the body, so a second surgery is needed to remove the oil.
Pasta con tonno
Mike Yamakawa Blog

Dr. D’Amico’s long awaited presentation about advances in retinal detachment management began with a slide of a Sicilian pasta con tonno dish. Pasta con tonno means tuna pasta in Italian. “Just look at it for a moment,” he said. “Its relevance will come to you in a bit.” Our team was invited to the 41st annual Ophthalmology Alumni conferences, and we– merely nascent Ophthalmology “immersers”– sat amongst the experts and internationally renowned professors of the field. And among even this accomplished group, Dr. D’Amico was, judging by the loud applause and testimony of others, a big shot ophthalmologist.
He talked about trends in detachment surgery, a procedure that can actually come in many forms including laser therapy, scleral “buckling,” vitrectomy, and pneumatic retinopexy. Apparently some surgeons have a preference for one or the other. Data also suggests similar success rates between techniques. He mentioned several other things that I didn’t nearly have enough foundational knowledge to understand. I thought perhaps I can figure out what the pasta meant at least… but I couldn’t even make the slightest connection between it and the rest of his presentation. The dish kind of looked like an eye if I blurred my vision a bit? But I was sure Dr. D’Amico had not intended that to be the hidden message. He explained eventually. But, in spirit of the way he executed his presentation, I’ll bring it back at the end. For now, let’s get to specifics of my week.
Thursdays for us are reserved for research lab. One of Dr. Yu’s main projects is designing a new corneal prosthetic, more colloquially known as the KPro. Corneal prosthetics, as you can imagine, are an alternative treatment option for diseases not amenable to corneal transplants. There are a few models already available, and several thousand operations have already been done with the device.
Interestingly, in the design process of this prosthetic, innovators ran into a certain dilemma: the prosthetic must be host-tissue friendly (as in any other implantation device) so that the surrounding corneal tissue can grow into it, vascularize, and secure the device. Simultaneously, the material must have low affinity for the host tissue in some portions to prevent migration of tissue over the central optical region (your field of vision!). To accommodate this dual requirement, the prosthetic had to be designed into several different detachable pieces. There are several other factors that innovators, like Dr. Yu, can consider in its advancement, including reducing ocular structural distortion and optimizing anterior optical curvature to match with a patient’s specific condition.
I’m sure the ophthalmology team has mentioned the OCT (optical coherence tomography) in some form for every blog post due to its ubiquity in the field, but we learned about something astounding – at least to me – that can supplant fluorescein angiography (the current gold standard) to visualize vasculature in the eye: OCT angiography. It can capture images of the capillary flow in the retina and choroid in a matter of a few seconds. Here’s the astounding thing about this method: It does not require dye– instead it uses the motion of red blood cells as contrast. It compares the differences in backscattered OCT signal intensity between sequential scans to construct a map of blood flow. This is a non-invasive and super quick, and only recently made possible thanks to algorithms that help optimize motion detection by OCT.
So what does pasta have to do with anything here?
If Dr. D’Amico were to ask us to cook that very dish we saw on the slide today, we would not be able to. The dish is something that his grandparents had prepared for him during his childhood– a meticulously designed concoction, with hand-picked, mercury-less tuna, organic semolina and pesticide-free tomatoes from the local market, which no longer exists. We wouldn’t be able to get those exact ingredients. And perhaps our generation has a subtly different way of cooking pastas. We even have our own way of collecting our preferred ingredients– making our purchases over the web, for instance. It is futile to adapt to anachronistic methods, when our world today has prepared for us the ingredients and tools we need to get things done a new way. In a similar vein, the way we manage retinal detachment or take angiograms is very different from the way we used to do it a decade ago. Knowledge has changed. New tech has been introduced. Perception of certain surgeries and techniques have evolved. Physicians and innovators must poise for rapid turnovers in the way things are done in medicine. And that’s how Dr. D’Amico brought the presentation to a full circle. It was beautifully done. Hopefully I was able to accomplish something similar here.
Eye’ll be back
Mike Yamakawa Blog
“Please make sure you do not move your head during the procedure, O.K.?” Dr. Liederman asked as he set up the microscope. “O.K.” The patient nodded.
One point of caution during eye surgery is head movement during critical moments– for example, when the surgeon has both of his surgical tools through the cannuli in the eye. An accidental grazing of the retina can cause irreparable damage to the patient’s vision. Naturally, the surgeon reminds the patients– who are fully awake during the procedure– to keep his head still on multiple occasions.
So there Dr. Liederman was, both of his forceps and fiber optic illumination tools in the cannuli, removing retinal scarring of an elderly Japanese patient one small peel at a time. Dr. Liederman reminds his patient once more. “Mr. Mizuka*, please make sure you don’t move your head, okay?” The patient nodded, “O.K doctor.” Dr. Liederman’s entire body froze. The nod had almost made him rip some of the healthy retinal tissue off.
In this particular case, there was a cultural barrier– a particularly interesting one for me because I have my own innate behavioral proclivities as a Japanese American. Nodding is a very common gesture in Japan; in fact, you’d see waves of undulating heads at restaurants where customers are conversing. For Mr. Mizuka, nodding towards Dr. Liederman in response was a sign of respect. To Dr. Liederman, it was possibly the end of the man’s vision. Of course, accidental movements are not limited to these cases. Some times, patients fall asleep and jerk around unconsciously. Another patient we saw had right facial palsy. It’s quite frightening that such small movements can threaten the success of surgery, in the worst case taking away man’s vision.
One sure way to prevent such event is to develop a head restraint– sort of like what they have for neurosurgeries. However, those restraints were not designed for ophthalmology– most likely, they would get in the way of an eye surgeon’s hand or tools. Perhaps there is something discussion to be had in this realm?
Anyways, this is my last blog post. Well, at least on this site. It’s been an eye-opening (started with a pun in June, why not end with one…) experience in ophthalmology, and I hope to continue working with the department to pursue some of these curiosities I have posted. Shout out to Dr. Kotche, Dr. Yu, Dr. Liederman, Dr. Sugar, other physicians at the Eye and Ear Infirmary, and my team for a wonderful and edifying six weeks.
Alvi Yasmin

Alvi Yasmin
I am a Bio engineering undergraduate student at UIC. I will be a senior from fall 2017. My concentration area is Bioinformatics. I want to pursue my career in the field of medical device industries.
Alvi Yasmin Blog
Alvi Yasmin Blog
A journey to new exposures, challenges and discoveries!
Alvi Yasmin Blog

05/31/2017
On wednesday morning, I woke up a little bit earlier than I needed to be because of the exciting anticipation of the day ahead of me. Also, I wanted to reach there on time. Once I got there around 8 am, I saw my fellow teammates in the waiting room, waiting for our mentor, Dr. Bui, to take us to his room. As we were waiting, we were observing the waiting area and thinking about the things like human-centered design methodology that we talked about in the clinical immersion workshop on Tuesday morning at the Innovation Center. We were seeing if the waiting room was user friendly enough. Was it boring or Was it able to provide entertainment to engage the patients? The waiting room had several things to save patients from boredom. They had engaging arrangements for patients of all ages. It was kind of funny how we were just talking about this on tuesday and was able to relate to it the next day. Thank god for the TV news. Before even starting the day, I learned a lot about the world, especially about the Trump’s infamous tweet!
Around 8:50 am, a nurse came and directed us to Dr. Bui’s office. We introduced ourselves to Dr. Bui. He was really nice and friendly. Right away he told us to get scrubs and changed into them. I was like Yes! Scubs! So official! (of course, in my mind). After putting on the scrubs, my work mode was on. He told us to put on shoe cover, masks and caps because we were going to an OR to observe Paracentesis procedure. The procedure was guided by ultrasound because the doctor needs to see the abdomen in real time. Basically, this procedure is done to remove fluid called ascites. Ascites builds up in the abdomen for different reasons such as liver disease or portal hypertension. In the operating table, there were one syringe, needle to take out the fluid, bottles to collect the fluid. Depending on patients, the amount of fluid withdrawn from the body may vary. We observed this same procedure twice on two different patient. Three vials of fluid was collected from one patient and a huge bottle of fluid was collected from another patient. This was a pretty interesting procedure.
After that, we observed nephroureterostomy tube (aka nephrostomy tube) for stone access procedure. This procedure is done before planned surgical PCNL the next day. This procedure is so coool!!!! I had no idea that you need to get this procedure done by IR before getting your kidney removed. You learn something new everyday! This day, I felt like I was learning something new very hour! I was just really enjoying learning new concepts and procedures. Oh, almost forgot to mention, before they performed any procedure, they do this time out thing to make sure the correct patient, procedure and everything. Anyways, this procedure creates an external drainage for renal collecting system. For this procedure, Ultrasound, previous CT scan and X-ray were used. The nephroureterostomy tube was inserted around the kidney stone and advanced into the bladder. This procedure minimizes the injury to the kidney. Several ways kidney can be removed. Shock wave couldn’t be used in this case because stones were large. That’s why it was important to insert the nephroureterostomy tube to remove the large stones from the kidney the next day. I noticed in most procedures, they use smaller needles to pierce through the skin/membrane rather than a scissor to prevent big holes in the patient’s body. In this procedure, a directional wire and directional catheter was used. The guide wire is very important to navigate the catheter to the right place. The catheter goes over the wire in order to slide over and inserted to the directed site. In this case, it was kind of difficult to put the guidewire around the stone due to the anatomy of the patient. But, the procedure was successful at the end. It was really fascinating. Also, Any procedure involving X-ray always required us to put on lead apron for protection. So, we did have lead apron on. Honestly, this thing weighs more than me ?
After Lunch, we looked at another case where the patient needed to Renal Biopsy procedure to be done. It was completely different than the other two procedures. I was exposed to the Biopsy needle for the first time. In this procedure, the doctor basically extracted tissue from the renal. It was a small needle. He injected the needle 4 times to collect the amount of tissue samples needed. I was curious why did he use small needle when it took him 4 tries to get enough sample rather than using a big needle and get all the samples at once? Thinking to myself, maybe they don’t have bigger needles. I asked Dr. Bui about it. He explained that smaller needles are better when it comes to biopsy because then he can get samples from 3 different places reducing the sampling error. Bigger needles = higher sampling error. He performed another Kidney Biopsy where he used 18 gage needle. It was interesting to learn about the importance of using different sizes of needles. In Dr. Bui’s office, he went over some concepts such as Seldinger Technique and like when IR was innovated. The background information that he provided was extremely helpful to understand the procedures.
Later that day, we went to see two clinic patients. Dr. Bui was informed that one of the patient’s percutaneous drainage catheter has a leak. That’s why Dr. Bui and we went to check up on that because that doesn’t occur often. Dr. Bui had a feeling thing that there might not a leak. When we went there, the doctor realized the issue wasn’t the leak. The catheter wasn’t capped right or it could be defective. Another patient was in 7th floor. We took the stairs. Oh man, that was a good work out! ( After 5th floor, I was dying. That’s how you know I am not fit…) When we entered the patient’s room, we noticed there was coal in the room. Later, we discovered that it was to prevent room from smelling. Anyways, for this patient, the doctor attempted US guided bedside abdominal drainage. On our way back from there, we were discussing about the features of the abdominal drainage tube. This tube has a loop where it has couple of holes (see the picture provided). The holes are basically designed in the loop so that nothing gets clogged up. One thing Dr. Bui mentioned that the tube isn’t optimal because it cannot drain everything. I think we asked why there aren’t more holes on the tube’s pigtail. He said “because too many holes cause it to lose its integrity”. Yah, that makes sense!
Overall, day 1 at the IR department was just mind blowing. One thing I have to mention, medical terms were a big challenge for me. Thanks to my M2 teammates for helping me out with that. But, I really enjoyed learning so many new things!!!! This is just the beginning of my journey to discover new things! I am excited and looking forward to working and gaining more knowledge from everyone involved in this program!
Tumor Tales.
Alvi Yasmin Blog
06/01 & 06/02
Thursday was another interesting day at the hospital, with lots of different procedures. Around 6:45ish in the morning, I showed up and changed into scrubs quickly. In the IR office, Dr. Bui, the fellows, the residents sat down to discuss about the patients and when and which procedures need to be done on them and who would be attending which case for the day. We showed up early morning to be part of this meeting and get a sense of the workflow of the department. Right after the meeting ended, we followed the team to a conference room, where we got to witness a multidisciplinary tumor board meeting. In the meeting, couple of PhDs and couple of experts in different medical specialties were present to discuss about complex patients’ cases and approaches to treat them. It was pretty interesting to see the importance of teamwork in the medical field.
After the tumor board meeting, we joined a fellow who was about to start the chemoembolization procedure for hepatocellular carcinoma. This procedure was really fascinating; like I always hear about chemo for cancer and stuff but I never had the chance to witness anything like this. That’s why I was really excited. Anyways, the doctor first started with an angiogram to locate the blood vessel that is the closest to the liver tumor. There were 3 tumors in the liver. It was a challenge to deliver the chemo medicine to the tumor that was the furthest to the blood vessel. Basically, the doctor used a catheter to deliver the drug to the targeted tumors. I noticed that it was quite a challenge to get the guidewire to the correct location of the desired blood vessel. It took a while, but the procedure was successfully done. During the procedure, I noticed the injector was being used gave warning to “disconnect the patient from the injector”. This issue was addressed by the operator of the injector.
Next, another cool and challenging procedure just blew my mind away. This was the most interesting one of the day. This procedure is known as the transjugular Intrahepatic portosystemic shunt (TIPS) placement. This procedure is important to reduce pressure in the portal vein. Basically, a mesh like shunt is placed through the liver to connect the hepatic vein to the portal vein. This procedure lasted for 5 hours. The difficulty was finding the right vein to connect the shunt to. There’s so many branches of the vein. That’s why finding the right vein using the guidewire was quite a challenge. After standing for 2 hours straight in the OR, we got tired of standing. Our feet started to hurt. So, we left the OR. I seriously don’t understand how do they have so much patience and energy! Oh my goodness, props to them!
Since we left after a while, we couldn’t see the end of the procedure. However, we got to see the Superior Vena Cava intravascular mass biopsy. The procedure was similar to the liver/kidney biopsy we saw before. This time, the samples were taken from the tumor in the blood vessel. Dr. Bui mentioned that it was kind of risky because while performing the procedure, if the tumor moves down/moves at all, the patient might even die. But, he was able to do this without any problems. He is just awesome! He told us to check out the biopsy needle and we were playing around with it to see its mechanism. It was pretty cool to learn how the biopsy needle works!
Learning how Biopsy needle works.
Later that day, we observed the attempted procedure of declotting of LUE AVF and the placement of chest tube on another patient. Then, the day ended with debriefing with Dr. Bui. It was quite a long day. We were there for 9 and 1/2 hours, but it was definitely worth the learning.
On friday, we came around 9 am-ish. Dr. Bui had a meeting till 10. We tagged along a fellow. We observed another paracentesis procedure. When Dr. Bui came back we went to see a clinic patient. This patient was supposed to get a Thyroid nodule biopsy that morning, but wasn’t able to due to unspecific order of the test. So, what happened was the hospital’s scheduling system’s order for test wasn’t specific. They didn’t specify it was a thyroid biopsy with genetic testing. That’s why they will have to come back again. There is a room for improvement in the thyroid biopsy scheduling process.
There was a patient who came back after removing kidney stone. Dr. Bui noticed that there were still some stones left behind to be removed. We observed the procedure of removing the nephroureterostomy tube and placing a ureteral stent. Then, we saw another tumor related biopsy. It was the Neck mass biopsy. The doctor used a different biopsy needle compared to the ones we have seen before. The needle and the device was smaller than the other biopsy needles. (see the picture below)
Neck Mass Biopsy Needle
It was interesting to see the different sizes of needles used for different biopsies. Also, the technique of storing the sample was different compared to the kidney/liver/SVC intravascular mass biopsies.
Another day passed by very quickly, involving bunch of exciting things! Just loving it this experience already!
Fascinating Filter
Alvi Yasmin Blog

As usual, we began our Tuesday morning around 8 am. We started off with a liver biopsy procedure. Previously, we have seen liver biopsies. But, this time, the liver biopsy was performed using a different approach. Previously, we observed percutaneous liver biopsy, meaning the tissue samples were taken out of the liver by puncturing a hole on the skin right above the biopsy site (liver) using a biopsy needle with ultrasound guidance. However, this time, we observed Transjugular liver biopsy. Dr. Bui explained to us that there are three different ways to do liver biopsy. One approach is the percutaneous way with image guidance (ultrasound) or landmark (eye balling and guessing where the liver is). Another way is the transjugular liver biopsy using the transjugular pathway to access into the liver. The third way was open cut surgery. He said it’s very rare that physician use the open cut surgery method to do biopsy. It’s only done when the patient is already having open cut surgery for something else. He also mentioned that transjugular liver biopsy is the best one out of the three because it exhibits the lowest risk. If something goes wrong during transjugular procedure and the vessel bleeds, the blood goes back into the system. We noticed that the procedure for transjugular liver biopsy is really different than percutaneous liver biopsy because of the difference in pathway. Since the procedure itself is quite different, the needle for transjugular liver biopsy is a lot of different than the percutaneous liver biopsy needle. The needle used in transjugular is inserted using a curved sheath with a stiffening and guiding metal cannula and the sheath is inserted through the transjugular artery into the liver to collect tissue samples.
Transjugular Liver Biopsy Needle Percutaneous Liver Biopsy Needle
Another interesting procedure we observed is TIPS. Last week, same procedure took about 5 hours to complete, however, this time it only took about 2 and 1/2 hour. This could be due to anatomy of the patient or the physician’s skill. This procedure was to create a new connection using metal stent which has two parts-2 cm of the stent is uncovered and the rest is covered with a net-like cloth. The tunnel is between the hepatic vein and portal through the liver. I noticed that the physician used a marking catheter that has a pigtail in order to determine the length of the stent. The length that they measured is basically the length of the covered part of the stent, not the entire stent. I looked the packaging of the stent. It shows that the uncovered part of the stent is always 2 cm long, while the covered part of the stent is varied depending on the patient’s anatomy. After finding the portal vein, the physician inserted a stent that was 8 cm long (covered part). The marking catheter was inserted again to check if the placement of the stent was appropriate. They noticed the stent needs to be shorter. So, later, they used a 5 cm long stent. Basically, the uncovered part of the stent is placed into the portal vein and the rest covered part is the channel from the end of portal to hepatic vein. It was pretty cool to see how the stent was released into the liver.
Another case that I found really fascinating was the placement of Inferior Vena Cava filter. Basically, a catheter is inserted into a vein and advanced through the IVC in the abdomen. A IVC filter is attached to a catheter which is pushed over the guide wire and once the IVC is placed on the correct position, the filter is released. The filter is then expands and gets attached to the walls of IVC. When I saw the release of the filter, i was blown away by the amazing design of this filter. Later on, when we talked to Dr. bui and Dr. Gaba, we found out that the filter does an okay job. It’s not the best.Dr. Bui said “it’s not as filtering as you would think it to be”. They both mentioned that the filter is able to block big clots, not small clots. Dr. Gaba stated that the filter can penetrate the blood vessel because it has sharp hook like ends. Also, the actual filter itself can get clogged. There is a room for improvement. But, they said it does a good job at blocking the large clots. So, it’s alright. It was interesting to learn about the advantages and disadvantages of the IVC filter.
IVC filter after releasing
Project Embolism
Alvi Yasmin Blog

Another day started with case discussions among the residents, fellows and the physicians. Right after the discussion, we followed Dr. Lipnik to an OR to observe bilateral uterine artery embolization procedure. I was wondering why the patient needs to get the procedure. The physician explained that the patient was bleeding a lot during menstruation due to uterine adenomyosis disease. Adenomyosis occurs when extra tissues grow within and into the walls of uterus. This extra tissues causes excessive bleeding. He said embolization is not the greatest procedure to treat this. The patient has 50:50 chance to get treated entirely. For this procedure, there were 2 surgery tool tables. First, I didn’t understand why they needed two surgery tables. This was my first time seeing that. Later on, I realized in one surgery tool tables, they put the drugs for embolization and in another table, they put the all the other equipment. The procedure called bilateral uterine artery embolization because the the embolic agents were distributed in both sides of the uterus. The physician inserted small bead-like embolic agent into the artery with contrast. The bead like agents are called embospheres. They mix the embospheres with contrast in order to see where the spheres are going. The embospheres are so small like 500 microns. Basically, the embospheres goes into the arteries and then advances into the capillaries and then blocks the end of the capillaries. Capillaries provide nutrients and supplies blood to the extra tissues inside the wall of the uterus. By blocking the capillaries, the physician is able to block blood supply/flow to the tissues, which helps to prevent the tissues from growing. I thought this procedure was super cool because I could see the embospheres and where they going. The application of the embospheres within the body was super fascinating to learn about.
Two surgery tool tables The embospheres mixed with contrastDuring the procedure, I noticed a work-around that caught my attention. The physician needed CO2 to insert into the patients body. So, a tube coming from the CO2 cylinder needed to stay on the surgery tool table. So, the physician used a fabric bandage to put it around the tube in order to make sure it doesn’t fall off the table (as shown in the pic below).
Bandage used to stick the tube onto the table
Later that day, we have been to couple of procedures where catheter was placed inside the body for different purposes. For one patient, the physician inserted a trifusion catheter for chemo therapy purpose. I saw the catheter has 3 inputs. Each inputs is used for different things. One input is to draw blood and other two inputs were to give two different drugs. Using Ultrasound and fluoroscopy, this procedure was executed. The catheter can stay inside for weeks or even months. We also saw the procedure of tunneling the dialysis catheter through the subcutaneous tissue on the chest wall for dialysis purpose. This catheter had two inputs for in flow and out flow of blood. Also, Dr. Bui mentioned this catheter is cuffed closer to the inputs, meaning it has adhesive section on the catheter in order to hold the catheter in place. That was pretty interesting. Also, the cuff section helps during removal as well.
After that, we saw a percutaneous renal biopsy. Even though we saw this procedure before. But, this time I got a chance to talk to the cytologist. When I asked him what’s the minimum amount of tissue sample do you need to do the testing, he responded that they need minimum of 15 glomeruli you need. But, he aims for 20 glumeruli just to be safe. Glumerli are the tiny units in the kidney where blood is cleaned. After that, Dr. Bui went through some concepts with us such as why delivering chemo through a chest port more ideal than delivering it through the IV way.
On Thursday, we went to the multidisciplinary tumor board meeting. In the meeting, they talked about different patients with complex issues. They talked about this liver mass biopsy patient’s treatment options. Basically, the doctors couldn’t see the mass in the CT image. But, there is a mass. When everyone heard about the case, one of the physicians suggested to repeat MRI at the end of the June to access for internal growth of the mass. They also talked about couple of other cases; all the cases were interesting and complicated. Later that day, we observed a hepatic artery embolization procedure. The purpose of the procedure was to insert oil based contrast in the hepatic artery so that they can see the masses/tumors a lot better and clearly. This helps a lot when they come to treat the patient later because this procedure is basically marking the masses for the latter doctor to treat the mass.
At the end of the day, we were able to see the placement of chest port procedure on a patient. We had been hearing about chest port a lot. So, it was nice to see the procedure in person. The chest port has a reservoir compartment with a septum attached on the top. The septum is like sealing membrane, where needle is inserted each time there is a need for delivering any drug. Also, a catheter is attached to the port, which helps to deliver/spread the drug into the body. We saw how the physician inserts the chest port entirely under the skin in the chest. This procedure is the most infection resistant compared to the catheters. That’s why chest port is an ideal approach to deliver drugs inside the body.
Chest portFor the rest of the day, we went over couple of cool devices in Dr. Bui’s office. Every single device was so different and unique. It was fun and enlightening. I really enjoyed learning about the devices, their applications, advantages and disadvantages of each device. It was just a perfect end to a perfect day!
Radioactive Particles!
Alvi Yasmin Blog

One of the coolest thing about interventional radiology is that it covers a wide range of procedures and clinical problems, covering a wide ranges of area, from the neck to the abdominopelvic cavity. That’s why there’s always something new to learn while shadowing. On Tuesday, I was lucky to witness another interesting procedure called radioembolization of liver tumor. The patient has tumor in the liver. In order to thrombus and kill the tumor, embospheres contained with radioactive isotope Yttrium-90 (Y-90) were injected through the hepatic artery, since this artery supplies blood the most to the tumor. These bead-like spheres are about 30 microns. These spheres block the artery, causing to block the blood supply to the tumor. Once they are at the site of the tumor, these emits high dose of radioactive beta particle and delivers it to the tumor. These beta particles cause the DNA strand of the tumor cells to break, meaning the cancer cells cannot replicate anymore, which causes these cells to die. Because these embospheres contained radioactive particles, they were handled very carefully. A health physicist had to come for the procedure, who brought the embospheres with her. When it was time for the insertion of the particles inside the body, it was placed in a container inside a small square glass shield. Basically, the doctor didn’t touch the medicine. There was a catheter, whose one end was attached to the shield and another end was inside the patient’s body. Using a separate catheter, pressure was introduced to the container inside the shield, which caused the spheres to move up the another catheter that goes into the body. The procedure was really interesting. I also noticed the health physicist was carrying a radiation scanner. she was scanning the room. When we got out of the OR, she scanned all of us to see if there was high radiation. That was different compared to the all the procedures we have seen so far.
Radioembolization Set-up for delivering Radiation scanning deviceI remember asking Dr. Gaba if the catheters they used for the procedure was specially made to deliver radioactive particles. He said, “no, they are like the regular catheters”. He said they don’t really use special catheters for these particles because they never really exhibit huge risks unless there’s a leak in the catheter. But, later he mentioned there is deterministic risk and stochastic risk associated with radiation exposure. If there was a beta shield catheter for radioactive particle embospeheres, it would be awesome because the beta shield catheter can protect anyone in the OR from the stochastic risks. The idea of inventing beta shield catheter sounds great me!
Another procedure called mesenteric angiogram was done on the same day. The patient’s bowel is bleeding. So, they were doing the mesenteric angiogram to determine the source of bleeding in gastrointestinal tract. Since fluoroscopy takes images within few seconds, they were having trouble seeing the source of bleeding. The bleeding wasn’t occurring continuously. That’s why the images taken in seconds weren’t helpful at all. They kept taking images until they find the GI bleed. Unfortunately, they couldn’t due to the fast fluoroscopy images. If they could take images continuously for 15 minutes, it would be easier for them to determine the GI bleed.
Device Talks!
Alvi Yasmin Blog
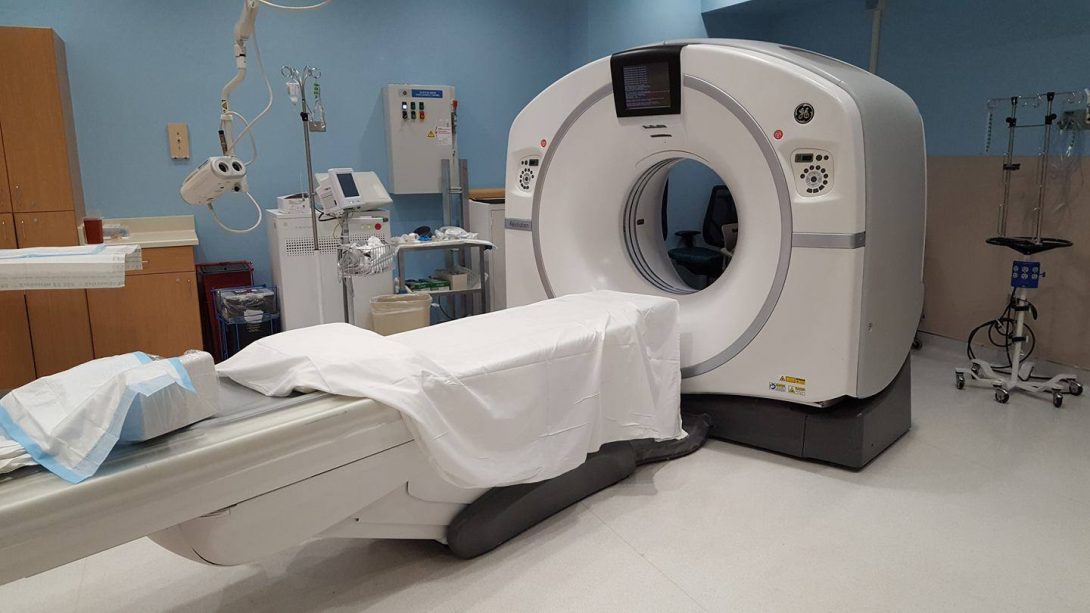
Almost all Interventional radiology procedures rely on CT scan images. But, you know what’s funny? We haven’t went to the CT scan room until this week. We always see CT scan images on the computer and observe how doctors analyze these pictures to determine the disease or the treatment before going into any procedures, however, We never got to see how these images are taken until now. Also, this was our first time seeing a CT guided lung biopsy. There was a control room outside the procedural room with CT scanner. The patient had a tumor on the surface of his lung. Lung biopsies can be challenging because you don’t want to puncture the lung by accident, causing air leak and lung to collapse. In this case, it was less risky because the tumor wasn’t inside the lung. It was on the surface of the lung. I noticed that every time the physician needed to scan the body to see if their needle is at the right position, they would take 5 images in each run. One of the things that bothered me the most was that every time the physician needed to see the images, he would have to come out of the procedural room and come to the control room where there is a monitor displaying the images. I thought that made the procedure extremely slow and risky. Imagine you are making something out of clay in one room, but the picture of the object you are making is on a different room. You would have to go back and forth between the rooms in order to make the accurate design. That would make you slow and less precious right? That’s how I felt about this CT guided lung biopsy. The doctor had to come to the control room multiple times during the procedure. After seeing the images, he would go inside the CT scanner room and fix the direction and the angle of the needle going into the patient’s lung. He would have to remember in what angle/direction the needle should be inserted in after seeing the image. I was like “how did he do that without having the images in front of him?”. They are experienced doctors. So, they do it very smoothly. But, honestly, I thought the lack of real time image in front of the doctor made this procedure slow and a bit risky. I actually asked the doctors why don’t they just include these screens with CT scan images inside the CT scanner room? He said you are right. It would be ideal. But, this is an old CT room. That’s why they don’t have it. But, the new CT scanner rooms do have screens.
In this week, we were lucky enough to meet two awesome medical device sales representatives. One lady was from cook medical Inc. Another lady was from gore medical. Both of them were so friendly and enthusiasts about teaching us about their devices. The lady from cook medical came to educate the physical assistants and nurses on their new device called Retracta detachable embolization coils, which is used for artery and venous embolization. It was so cool. The tiny detachable coils has synthetic fibers. The design itself was great. It is also retractable. She taught us how to place and retrieve the Detachable coils using catheter. After that, she pulled out couple of filters that are used for vena cava. She let me use the placement and retrieval device to deploy the filter and retrieve it as well. I was so happy that she let me do it. She showed us two different filters, which are tulip and celect. Both are for vena cava. They are just different versions of ivc filter. She told us the advantages and disadvantages of each filter.
Tulip (left) and Celect (right)She mentioned the cone-shaped design concept of the filter came from oil pipes. Celect is newer version of ivc filter. The tulip filter’s design wasn’t effective enough because it would tilt inside the vessel pretty often. When it tilts, it makes it difficult to remove from the vessel and cannot filter properly, which makes it a short term filter. That’s why they came up with the new filter called celect, which is much better than the tulip filter. Its improved design helps to prevent itself from clogging. Also, she mentioned that celect is not made out of nitinol, which makes it better because the legs of the filter won’t fracture. It was really an informative discussion about devices.
The next day, Dr. Gaba was nice enough to bring us a box of different devices from his office so that we can look at them. We noticed couple of cool filters, stents and closure clips. One of the things that drew our attention was this uncovered stent because when you squeeze the stent, the stent’s length and diameter both changes. The stent basically elongates each time you press on it. We asked him about the stent. He said it is called wall stent and used for TIPS procedure. He continued to say, “we don’t really use that anymore because we use covered stents for TIPS now, which is so much better than wall stent”. The covered stent is basically a metal stent covered with PTFE material. He asked us why do you think covered stent is better than wall stent for TIPS? Then, he said, “Since wall stent elongates, it is not precious enough.” Covered stent don’t elongates. So, it can be placed on the desire spot accurately. These stents are placed in the liver. Liver produces bile. They are thrombogenic, meaning they promote clots. Covered stent does a very good job of preventing bile from entering into the artery, prevents blood clots. That’s why covered stents are widely used nowadays for TIPS procedure. However, these covered stents aren’t the best stent. Over time, they may clog. That’s why Dr. Gaba was mentioning that it would be cool to have stents that are self-reporting in future. The stents that are able to report if it’s narrowing or clogging. It was really fun to talk about these devices and their advantages and disadvantages.
Liver Cancer Treatments
Alvi Yasmin Blog
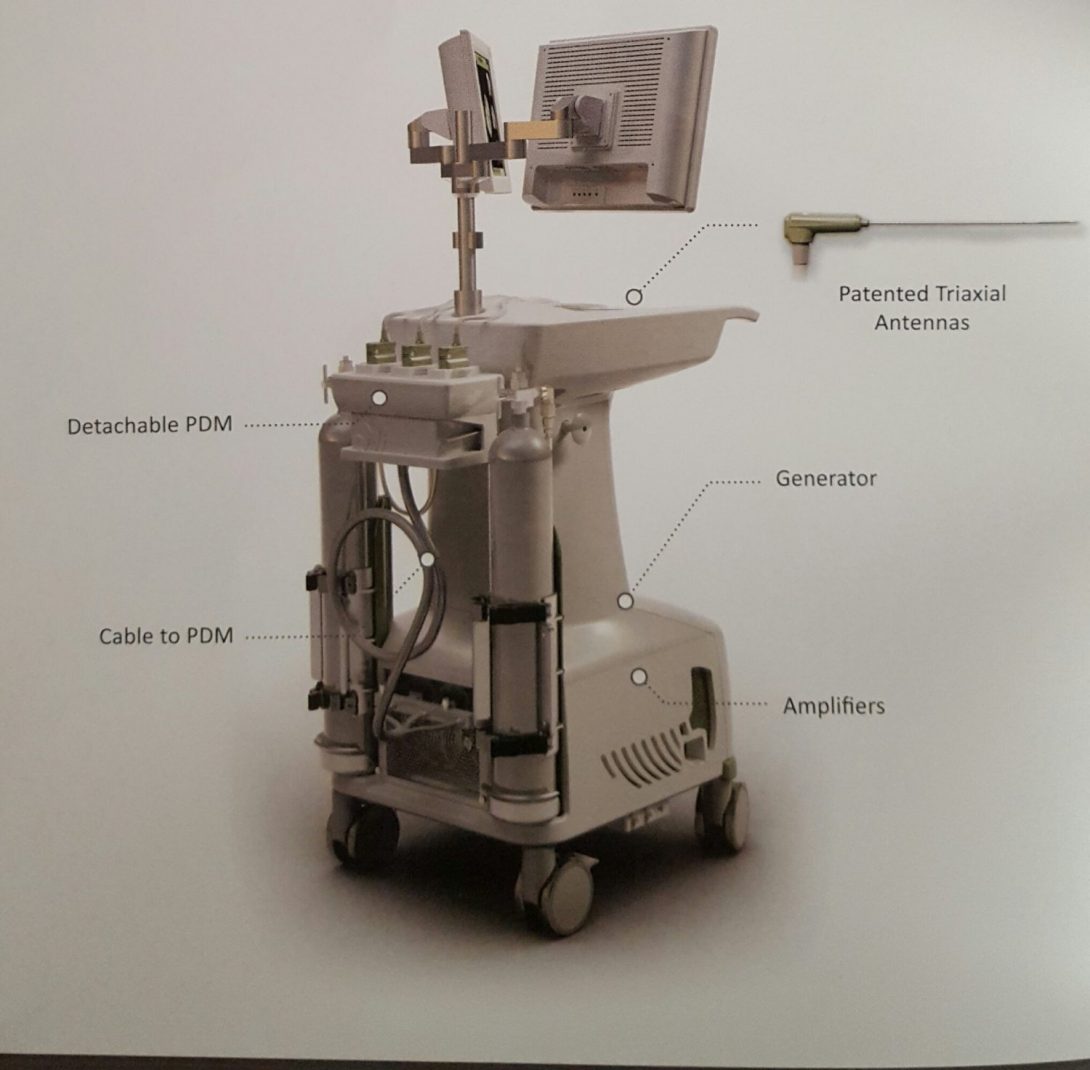
Liver cancer is a very common cancer. It is the third most common cause of cancer related death worldwide. Over the past few weeks, we have seen multiple ways to treat liver cancer in IR using different methods, skills and technologies. One of the most common procedures to treat liver cancer that we have observed was the transarterial chemoembolization (TACE). Today, one of the liver cancer patient was treated using TACE. In this procedure, the doctor basically uses catheter that delivers embolization beads into the blood vessels in the liver. These beads are infused with chemotherapy medicine. Basically, the beads block the blood vessel to prevent blood flow to the tumor. Then, the chemo agents are released from the beads, which then kills the tumor over time. Today, when the doctor was done inserting the catheter into the blood vessel, he noticed that the chemotherapy embolization beads haven’t arrived yet. That’s a problem. The patient has catheter inside of him already but the chemo wasn’t ready. The doctor came out of the OR room to call the people who are supposed to send the beads by 10:20 am. When he called them, he found out that the order of chemo wasn’t placed until today in the morning. However, apparently, IR department ordered it yesterday. There was some miscommunication. According to Chemo people, it was ordered in the morning and they were going to send it by 11:30 am. After knowing, the procedure has already started, the chemo people decided to send it by 11:10 am. Because of this miscommunication, the procedure got delayed. Other procedures were pushed back. It caused inconvenience for everyone.
Previously, we have seen other ways to treat liver cancer such as radioembolization where radioactive particles are inserted to kill the tumor cells. Today, we saw a completely new procedure to treat liver cancer. This procedure is called ablation. This procedure uses heat to destroy the tumor cells. The device that is used to tailor ablations is called the neuwave medical ablation system. This system has multi-probes (3 probes in total). For this case, they called the neuwave medical inc. representative to assist with this device during the procedure. I was talking to the rep. She said this device is pretty new to the market. It’s a 4 year old company. This device is really effective at covering large, multiple tumors. Before this they had single probe system. Also, radio-frequency ablations were more common than microwave frequency waves. The patient had about 3 tumors in his liver. So, this device was ideal for the procedure. The benefit of having multi probes is that if there are 3 tumors in an organ, all of them can be destroyed simultaneously by placing 3 different probes at the different spots of the tumor. Also, if the tumor is huge, the 3 probes can be activated simultaneously, which creates high, consistent temperature and large confluent ablations. This is possible because all the probes are connected to a single generator, which produces in-phase waves. Also, the procedure with this device is much faster than single probe system. In single problem system, repositioning of the single probe and ablating multiple times in order to cover the tumor completely make the procedure longer. Basically, one end of the probe is attached to the generator and the other end of the probe is inserted into the liver (at the site of the liver tumor). Then, current with microwaves frequency is passed through the probe to the body, which generates heat that kills the tumor cells. Before they used to use current with radiowave frequency. But, microwave ablation is much safer and effective at ablating than radiowave frequency ablation. I asked her what is the maximum frequency a doctor is allowed to apply? She said there is specific FDA regulations for it. For example, doctor cannot apply 65 watt frequency for more than 10 minutes. It has to be for 10 minutes or less. The max frequency that can be used is about 145 watt frequency for certain amount of minutes. So, they are really restricted on how much they can apply for how long. It shows that because of FDA regulations, there is limitation in freedom of using the product you developed the way you want. So, when developing a product, you have to be aware of the fact that your freedom of using the product the way you want might be limited by the regulations imposed by the FDA.
Things Got a bit Heated…
Alvi Yasmin Blog

As usual, on Thursday, we joined the multidisciplinary liver tumor board meeting. These tumor board meetings have been always engaging with interesting cases. This is where the specialties from different departments come in to discuss the treatment options for complex cases and agree on the best route to treat the patients with complex liver diseases. One of the cases particularly made this week’s tumor board really interesting. So, this patient has lung cancer and possible liver cancer. The patient came in first with lung cancer issues. He had additional problems. Then, the IR physicians looked at the CT, MRI images of the patient. They noticed he has tumors in his liver as well. When they noticed tumors in the images of the liver, they thought it is hepatocellular carcinoma (HCC), which is a type of liver cancer. So, they performed a liver biopsy procedure on him to make sure it is what they think. They sent the samples to the pathology department so they can examine the samples of liver tumor tissues more closely. One of the pathologists came to the meeting to discuss about their finding and their insights. So, the pathologist pulled up a slide with the images of the microscopic view of the tissue samples. By looking at the cellular structure of the samples, they determined that the tumor is benign. She said they believe it is hepatocellular Adenoma (HCA) based on the samples. HCA is a very rare kind of liver tumor. The IR physicians were like what? It was kind of clear to them that it is HCC. The pathologist was like maybe you guys didn’t get enough samples. She was implying that there could’ve been some sampling issue. Things got heated a little bit in the room. There were some disagreement between the results from the pathology and imaging. The lady from pathology kept explaining about HCA. She was saying HCA can turn into HCC in future. It’s not certain but could happen. She was suggesting to “act upon it soon”. But, IR physicians don’t treat tumors that are benign. They would treat it if it was HCC for sure. There were some arguments on how to go about this issue. Patient had lung cancer. But, when the pathologists examined the lung tumor samples, they found the tumor to be benign as well. That was kind of weird. I think later on, they decided to do another biopsy to see the result again. It was really interesting to see that pathology results can differ from the MRI images. Also, the way everyone provided input to the discussion by giving their opinion was really impressive.
TIPS has come full circle!
Alvi Yasmin Blog
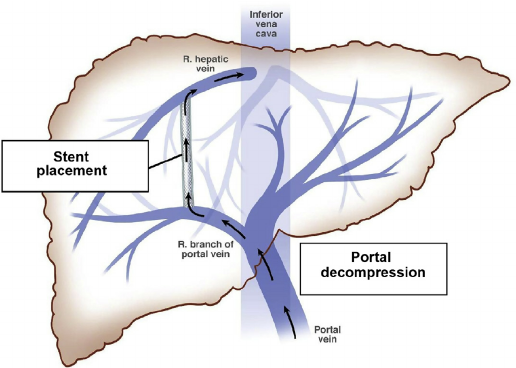
Transjugular intrahepatic portosystemic stent is typically known by its abbreviation, TIPS. It would be a shame if I forget the full form of TIPS by the end of this program or ever in my life. TIPS has been the one of the most common procedures we have witnessed in the IR rotation. We started off our first few days with couple of TIPS placement procedures and we ended our clinical days with TIPS revision and TIPS reduction procedures. It’s like TIPS has come full circle. We got to see the entire cycle of TIPS over the past few weeks of our time in the IR rotation. TIPS placement is done on patients with cirrhosis and portal hypertension. Thrombosed portal vein causes portal hypertension, meaning there is an increase in blood pressure in the portal vein. In order to create optimal pressure in the vein, a stent is placed between the portal vein and hepatic vein to reroute the portal vein blood flow into the hepatic vein. The stent allows normal blood flow, reducing the pressure in the portal vein. For the past 4 weeks, we saw many TIPS placement, where the physicians would place stent between the hepatic vein and portal vein to create the channel for proper blood flow. The stents have two parts: covered with PTFE and uncovered bare metal part. The uncovered part of the stent goes into the portal vein and the covered part is positioned in such way so that it starts from the front end of the portal to the hepatic vein all the way. We have seen TIPS placement procedure at least once a week. Then, this week, a patient came in for TIPS revision. This is another interesting part of the TIPS cycle. Even though we have seen multiple TIPS placement, this was our first time seeing a TIPS revision case. The patient had her TIPS placement procedure done in the middle of the June. She came in for a follow-up visit last week. The physicians noticed there isn’t any blood flow in the channel created using stent. The stent isn’t functioning properly. The physician couldn’t recognize the main reason of this issue from the images. So, TIPS revision procedure was important to investigate and plan accordingly.When they were able to access inside the vein, they measured the pressure. It was really high. Then, they decided to extend the stent in the hepatic side of the channel. Even after extending the stent, there wasn’t much blood flow. It was because of the blood clots in the channel and the portal vein, causing blood flow to impede. Then, they decided on doing a portal vein lysis procedure on her the next day. This procedure was quite interesting because we haven’t seen anything like that before. The physician placed a lysis catheter (shown in the picture below) in the thrombosis vein so that it can administer a thrombolytic agent called TPA directly into the clot. The lysis catheter was kept inside to deliver TPA continuously over the night.
The lysis catheter was really cool because it has bunch of holes at the end of the catheter, which is placed into the clot. All the small holes on the catheter allows TPA to enter into the thrombosis vein, aiding with dissolving the clots. Then, the next day, they brought the patient down again to see if the lytic agent worked or not. It turned to be really effective. Even though the clots were mostly dissolved, the stent still weren’t able to function properly. Then, the physician ended up extending the stent in the both ends of the stent. They placed 3 stents in total inside the original stent, overlapping one another.
When they extended the stent at the portal vein, they placed a uncovered stent. They place uncovered portion at the portal vein to allow blood flow from the collateral veins to the portal. The extended side of the hepatic vein was covered. I was really mesmerized when I saw placement of 3 stents inside one. One of the questions I remember asking was that “Doesn’t insertion of 3 stents overlapping with other stent causes thrombosis of the stent?” The physician said, “no”. He said when they place the stent, they place it against the wall of the original stent, leaving no space in between the stents. Another problem he mentioned is that overlapping the stents to extend may cause them to slip off from one another, which could be life-threatening. This was a really interesting TIPS revision case. The patient had to go through a lot. However, after extending the stent, the result was just beautiful. It was so satisfying to see the stent working properly at the end.
Another part of the TIPS cycle that we were able to witness was the TIPS reduction procedure. TIPS reduction is done on a patient when there is too much blood flow in the channel between hepatic vein and portal vein using stent. Too much blood flow can be toxic for the body. That’s why narrowing the stent is the ideal treatment approach. So, TIPS reduction is really important to limit excessive blood flow through the stent. As shown in the picture below, the physician inserted a small bare metal stent in the middle of the original stent. Then, he deployed another stent, which has the same size as the original stent. Also, it was covered as the original stent. Once the covered stent was deployed in the stent, the small bare metal stent was expanded to its nominal diameter. Since bare metal stent is stiffer, it can push the covered stent inside, reducing the diameter of the covered stent. This decreases the blood flow and reduces the portal vein pressure. Honestly, this method of reducing the diameter of the stent seems like not the best option. By deploying a stent with thicker wall (smaller in diameter) can solve the exact problem without having to deal with 2 different stents at the risk of slipping out of one another, which can be unsafe. By observing all these procedures, we figured that the stent has to be malleable in order for it to be fit in the artery. Also, the stent should be covered with the kind of material that doesn’t cause it to slip out from the other stent. Firmer interior grip would be ideal for the issue. Stents are so important for many procedures in the field of IR. There is a definite need for improvements in stents. I am glad that we got to see from placing the stent to revising and reducing of the stent in this short time period. It feels so good to learn so much from this experience. I cannot believe it’s coming to an end. Looking forward to ending the week with more interesting cases and more learning opportunities.
Can’t believe its over…
Alvi Yasmin Blog

The clinical days are coming to an end. So, throughout the week, I was hoping to see as many new procedures as possible. Thank god I was able to wrap it up with some cool new procedures. One of the procedures among all really caught my eyes because it was unique. It was the varicose vein endovenous laser ablation. The patient had varicose vein pain because her left leg veins were dilated (not the usual). Her varicose veins were kind of swollen and had a bluish color. Dr. Bui inserted a catheter into the varicose vein in the left leg so that the laser fiber can be advanced through it. For some reason, when the guidewire and marking catheter was being inserted, the patient was in pain, which is unusual. The procedure was guided using Ultrasound machine. Once the laser was inside, the ultrasound machine was used to check if the position was accurate. Then, the laser was turned on and the laser energy burns the lining within the vein, which causes it to shrink and thrombus the vein. As the laser was burning the vein walls, Dr. Bui was pulling down the laser fiber so that it burns everything as it makes its way down. This makes sure that all of the varicose vein is covered. This procedure closes the vein. I asked if it is life-threatening to close up a vein. He said not really. It is just one vein and since it was varicose, it wasn’t able to supply blood to the heart anyways. It was cool to see the light of the laser moving down the vein from outside the skin. Another problem that appeared to happen was that the tech couldn’t turn on the laser ablation machine. There was some problem with the machine or she didn’t know how to use the machine. So, they called for another tech to fix the problem. But, after about 15 minutes, she was able to fix the problem. Someone might have taken apart the parts of the socket that should be plugged to the machine and haven’t put it back the right way. This caused a delay in the procedure. It created inconvenience for everyone. So, it is important to put the machine back as it should be after the procedures are done.
End of the Laser fiberLastly, I would like to thank the clinical immersion faculty for giving me the opportunity to be part of this program. Shadowing the IR physicians and exposure to the clinical setting was one of the best experiences I have had in my life. I found my experience to be beyond any expectations. I am beyond grateful to have experienced and learned so much in such way. I would also like to thank our mentor Dr. Bui and other IR physicians for spending their valuable time teaching us. It was fun looking at everything in the hospital from an engineering standpoint. Also, everyone’s kindness and friendliness attitude in the clinical setting really made this experience invaluable, unforgettable and memorable. This is something I would never take for granted. I feel blessed to be part of this program because this is something an engineering student like me probably won’t get the chance of experiencing. I honestly can say I learned more than I would learn from pages of a book. I can’t believe it’s over… I will definitely miss this. This is one unique experience that I will cherish for a long time.
Thanks to everyone who has been reading my blogs since the day one! Hopefully, you also were able to learn new things by reading my wonderful experiences in these blogs 🙂