Students: Part 1
J. Austin Buen-Gharib

J. Austin Buen-Gharib
My name is Austin Buen-Gharib, I’m a rising senior in bioengineering. I am also a pre-dental student in the honors college as well as the 2018-2019 President of the Engineering Honors Society Tau Beta Pi. I’m passionate about helping people, maximizing impact, and making a difference in the world through great ideas and innovation. I’m excited to be a part of this year’s CIP program with the Anesthesiology department under Dr. Hokuto Nishioka, MD who also happens to be the Medical Director of the OR. Please let me know if you have any questions and I’ll be happy to help!
J. Austin Buen-Gharib Blog
J. Austin Buen-Gharib Blog
Welcome to Week 1! Anesthesiology: No Pain, No Gain!
Confession time: This is my first ever blog post, so please bear with me for now! I imagine just like finishing up the first of week of clinical immersion, there is a bit of a learning curve as you transition, but just like anything, you just do the best you can with what you have! I want to point out that I’m very excited to be a part of the 5th year of the Clinical Immersion Program (CIP) at UIC working in an Anesthesiology rotation with Dr. Hokuto Nishioka, MD (and also Medical Director of the OR) as well as John Marsiglio (M2 inthe iMED program [innovation in medicine]) and another undergraduate student intern who is a CS/bioinformatics major on a pre-med track. I’ll admit, I’m a bit nervous maybe because last year’s anesthesiology group composed of Nick Green, Vijay Putherickal, and Joe Sauer (you can also read find their blogs under 2017) actually ended up with a provisional patent! For me, that would just be bonus!
I’m here mostly to learn and observe and try to help make a difference in healthcare. In general our goal in this program is to identify clinical needs and areas of improvement and brainstorm solutions and ultimately a design concept to address these issues while focusing on user centered design. In our first design session on Monday, we actually practiced improv with Byron to help prepare us for the challenges we might face working in a team in a clinical setting and I really enjoyed it! I thought it was a lot of fun and it really did have a purpose. We covered concepts like coming in with energy to be ready to make the most of the day, explaining our areas of expertise in a way that helps make our teammates feel comfortable, and positively responding to our teammates’ ideas to help facilitate innovation. We were also given several frameworks to help us make observations and record insights, for example the AEIOU system helps us keep in mind the Actions, Environment, Interactions, Objects, and Users around us.
Soaking in the Second Week with Storyboarding!
Even though the second week was a day shorter with the holiday, our group continued to work hard to soak in the clinical experience in the OR. As part of our weekly assignment, our task was to choose a process of interest, storyboard all of the relevant steps, and identify points of torture or areas of improvement. Although we were initially interested in further investigating the iShuddle initiative, we were unable to interview the Operations Director of the OR as she was on vacation. We did notice though that while the iShuddle time of return for the next patient was often written on a whiteboard in the front of the room, few nurses actually announced this time to the team suggesting a gap in communication. We postulated an automatic device or app that might help the team implement this system easier. In this case the innovation would help bridge the benefits in theory to practice in reality to provide measurable results. We also noticed several bulletin boards to help track the progress of the iShuddle and record first case delays which tend to have a domino effect. Unfortunately, we also learned that the person responsible for updating this board left a couple of months ago. Ideally, there would be a way to automatically update and display the progress and compare the hospital’s goals. I think this system would help the hospital be more accountable and efficient because as I’ve been told, when you record the appropriate measurements, it’s easier to view and understand the current status as well as make and monitor improvements.
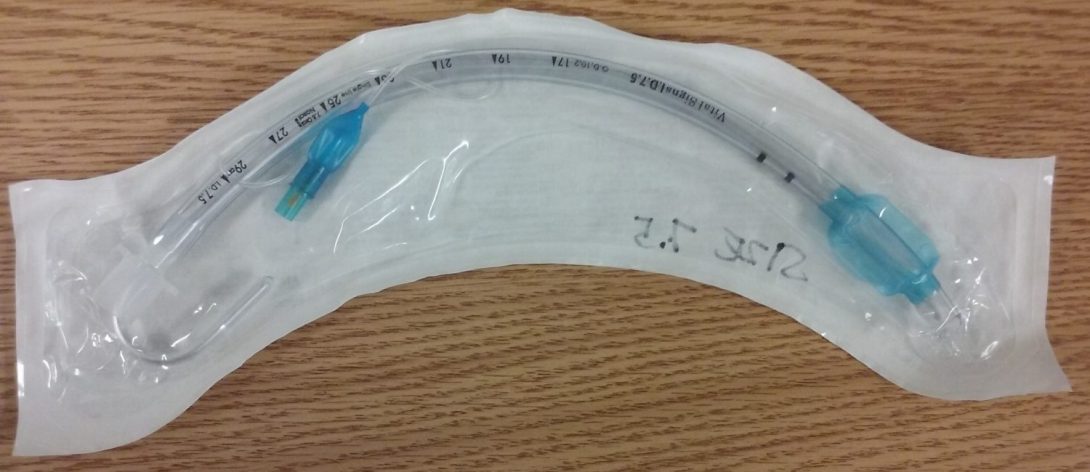
Our other storyboard idea which we will present on involves the process of intubating patients. Essentially, intubation is putting patients to sleep with general anesthesia (GA) to make surgery easier and more comfortable for both the patient and surgeon/medical team. Actually, the process of putting them to sleep is known as sedation and intubation is the placing a ventilation tube inside the patient to help them breathe during the operation as the aesthetics often cause paralysis of the muscles including the diaphragm which inhibits breathing. Often the tube goes through the patient’s mouth and down their airpipe (larynx/trachea), but in cases where they operate in or around the mouth or throat (oral surgery or tonsillectomies), the tube can be placed through a person’s nasal cavity. Intubation seems to be a pretty routine procedure for all patients that receive GA, but that does not always mean it is a smooth process. For starters, everybody is different, which can make visualizing a person’s vocal cords difficult, especially for pediatric, geriatric, and bariatric patients (or people with abnormal anatomy eg. a tumor in the neck). Anesthesiologists use a variety of tools (that I’m still getting acquainted with) in order to find, visualize, and open the airways. They use what they call a blade to peel back the patient’s esophagus and open the windpipe up for the ventilation tube. The actual process is shockingly blunt, often inducing blood with the potential of damaging tissue or possibly even knocking out teeth.
Before intubation, there is a bit of prep consisting of measuring the patient’s vitals such as their pulse and oxygen saturation with a pulse ox, blood pressure with a catheter or cuff (sphygmomanometer) , and ECG with a couple od placed leads. When the patient is deemed ready, the anesthesiologist begins sedating them with a gas mask. I’m not very familiar with a lot of the pharmacology and narcotics they use, but they favor nitrous oxide and sevoflurane, which might explain why some patients wake up feeling nauseous. After the patient is put to sleep, the anesthesiologist has a window of time to intubate the patients and hook up the ventilator. Usually the anesthesiology attendings assist the residents in this step as it can be a bit tricky to visualize the vocal cords and position the patient properly. Often the anesthesiologist must manually ventilate the patient in the meantime. Maybe a device to help position the patient’s neck and jaw would be helpful, if it doesn’t exist already. There is usually an extra camera tube called a laryngoscope which helps them get a better view. Once the tube is in place, the patient is ready for surgery and the anesthesiologist is responsible for monitoring their vitals during the procedure. Interestingly enough, although the patients are sound asleep, their bodies still provide a physiological response to the procedure, so the anesthesiologist uses a variety of drugs to help maintain the patient at relatively healthy levels.
While the process of sedation and intubation makes surgery much more manageable for both the patient and the surgeon/medical team, it’s fair to point out that it has inherent risks. For example, last week we attended an M&M – Morbidity and Mortality – meeting about a case in May where the ventilator wasn’t properly hooked up, so there was no oxygen flow to the patient! The bariatric patient became hypoxic and went into ventricular fibrillation. I think they were able to treat the patient in the ICU before she was discharged about a week later, but I believe that incident caused or exacerbated organ failure of almost 4 different systems, which sadly has a high mortality rate. One issue is that some of the UIC machines are older and do not have warning lock systems for when there is no gas flow. Some people thought that the problem was that the issue was almost too basic, it was easily overlooked. For some reason though, there was a lot of disagreement in the room about the correct standard of care, like different people have their own system. It was an interesting case study to observe and maybe it warrants looking into further.
In other news, we saw some more pretty interesting cases in the OR from a kidney transplant to a knee replacement to a cholecystectomy to cochlear implants to an amputation to a colostomy on a 3 week old with hirschsprung disease. It’s really interesting being in the OR, you never know what you’re going to see. We’re still on the lookout for more good and bad designs, maybe I can update the last entry with those. I feel like I’m learning a lot, my iMED partner John is really smart and able to fill in a lot of my questions and our attending mentor is super nice. Sometimes he’s a bit busy, so we have more flexibility seeing a variety of cases in the OR. That’s it for now, I’ll keep you posted! Thanks for reading! Hope you enjoyed!
Week 3: Evolution of Our Needs Statements RPMs
Photo Week 3
So our assignment this week was to develop 3 iterations of a needs statement in terms of the population, problem, and intended outcome as well as explain the rationale behind each change. I hope to keep this post short, sweet, and easy to read! I’ll also try to include the feedback from our presentation to give you a better of idea of where we are and where we’re heading.
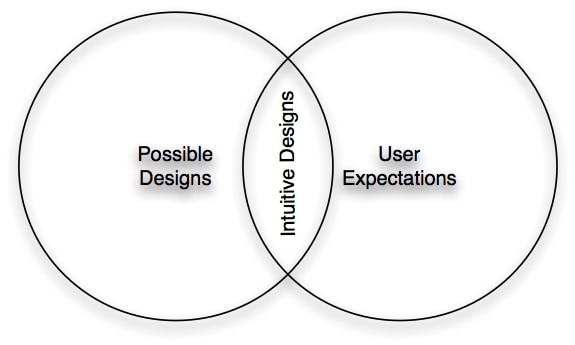
Our topic involves more of process improvement than actual medicine, but for big operations, even marginal improvements in efficiency can lead to drastically different results. In an effort to maximize impact we decided we want to continue to explore the iShuddle initiative which was recently implemented in February to help improve Turn Over Time (TOT) in the OR by announcing the end of cases, the next case type which has a corresponding time to set up which gives a predictable start time for the next case. Still delays are common in the OR and another goal of the iShuddle is to account for the different reasons that lead to the delays including patients, surgical instruments, or medical staff/teams.Unfortunately, there are several issues with the iShuddle most notably compliance because nurses already have long To Do lists, people don’t really want to blame each other, and lack of incentives to maximize efficiency and see more cases besides maybe finishing faster. Ultimately, it seems that the main issue involves the human element, but that’s where I believe user centered design is meant to account for all those factors and help make it easier for the users to implement (intuitive, adaptable, affordable).
My actual need statements involved more of the funneling in from the general hospital goal of providing quality healthcare to as many people as possible (at UIH we treat every patient that walks in the door, but as a state hospital that receives no endowment funds from the state, we must work not just harder, but also smarter and run a tighter ship).
Then I went on about how our mentor Dr. Nishioka shared literature with us on the importance of reducing TOT in the OR, not just time or money but also less stress (when on schedule) and a better experience for both the patients, surgeons, and medical staff. That’s the reason they started the iShuddle. It seems like a well intentioned system, but sometimes implementing systems requires evaluations every 2 weeks and personal/professional development reviews (as opposed to performance reviews ~ to stress the importance of branding) at least according to my mom who is a dentist and business owner.
So my 3rd iteration involved a system to better implement the iShuddle system in the OR, however a major issue with this train of thought is that it already contains an embedded solution which might limit our own creativity. Although we are currently brainstorming a solution related back to the iShuddle, there is an issue of scope.
But here is where I believe teamwork makes the dream work because my iMed partner John helped articulate a balance between a solution specific example and a overly generalized statement:
A way to keep staff on schedule with turn over time that also increases awarenessof why cases are running behind and promotes accountability.
(Future reasons to update: as we explore the iShuddle system more we may be aware of other issues it has besides compliance)
It’s still a work in progress, but I believe it’s a great start and I’m excited to see what’s next. To give you a taste for what’s next, we’re now discussing high specifications while we brainstorm solutions to this clinical need. Already we are considering some sort of Alexa compatible app, but we’ll see.
I just want to point out a couple more things really quickly. For personally, I’m still learning how to be a (better) innovator, designer, and engineer but I’m starting to see that innovation doesn’t have to involve reinventing the wheel, but also includes taking existing technology and applying it in different ways and for different problems.
I think one pneumonic to help understand and visualize this process is RPMs (Result, Purpose, and Map). Essentially the What, Why, and How of clinical needs. I’ve been told the most important question to answer and start with is why.
Also I think an important theme of engineering is quantitative data, in other words, if you can’t measure it, you can’t improve it. So in addition to our needs statement, I believe it might be beneficial to also work on ways to effectively collect more data, which would make evaluating other systems/innovations easier.
Definitely there is a psychological/motivational element to this issue as well and if I learned anything from this weekend’s seminar, it’s that our (Physical, emotional, mental) state is one of the biggest factors in our performance and ultimately our quality of life (and that there are ways to shift or hardwire our habits/thoughts/body to achieve a beautiful, peak state and maximize (the time in) our lives). I guess that’s my Tony Robbins plug… but thanks for reading, I hope you enjoyed it! Wish you all the best!
Week 4: High Specs? Check!
Photo Week 4
Wow! Time Flies (when you’re having fun)! We’re almost done believe it or not, but so far so good! I believe our group is in a good place, but now it’s time to start developing and refining our design concept. So last week we brainstormed what different really solutions might look like and this week we were tasked with identifying high specification that can help us evaluate each solution. We identified around 8 major factors to consider (I’ll go over them in just a bit) and then we categorized them into Must Haves (2), Moderately Important (2), and Other Considerations (4). We graded each solution as either 1,5, or 10 for each specification, then we took a weighted average to distinguish our best 3 ideas. (Funny enough the current system had the highest unweighted score! But that’s not exactly innovative enough for us)
Must Haves (2)
- Predicted impact on ToT (goal of the projection)
- Staff willingness to adopt (pitfall of current system)
Moderately Important (2)
- Ease of use for staff (minor iShuddle barrier, intuitiveness)
- Ease of implementation (hospital admin desire)
Other Considerations (4).
- Cost (always a factor at a state hospital)
- Time to implement (hospital admin desire)
- Adaptability (ability to be incorporated at UIH/other hospitals)
- Safety (all our ideas are relatively safe, but in healthcare this should always be a factor)
Week 5: Tackling Turnover Time with Technology
Week 5
As we wrap up the program, we spent the majority of last week conceptualizing our solution to address the clinical need we identified. Based on the high spec evaluations of our Crazy 8 brainstorming activity, we decided on developing a design concept for a web/mobile app that can help increase efficiency, reduce TOT (Turnover Time), and promote accountability. As we discussed the potential of the app, we tried to incorporate features that reflected our other observations in the OR. We ended up coming up with over 30 features and then we tried to categorize them into Must Haves, Moderately Important, and Bells and Whistles.
Although it is important as part of the next step in the iterative process to streamline our ideas in the interest of remaining intuitive, I also noticed a more general theme in the hospital. Our mentor noticed that our high spec criteria covered all of his general focuses in the OR except for being patient centered. Of course all of the design specs of our project is aimed to (in)directly benefit the patients as well as the medical staff and hospital administrators. I might have mentioned before but the effort to improve TOT is a long term of project of the hospital and they are still in the initial phases. I think it would definitely help this project (and therefore one of the focuses of our project is to) continue collecting data so we can really focus on the areas that need improvement. I think one of the more general goals/themes of our project is putting your best foot forward and always focusing on improvement because if you’re not getting better, you’re getting worse. Hopefully our project will help the hospital be more efficient and better able to help people. A great goal that really resonated with me is to create an OR environment we can be proud of and that we feel comfortable enough with to bring our own friends and family for care and treatment. And as one of the many UIH positive posters articulates CARE stands for Compassion, Accountability, Respect, and Excellence. Hopefully our project will help the hospital provide the best care possible and live out its mission by changing medicine for good.
This will be our last week in the program and we will most likely be busy finishing up our final presentation, report, and design concept, but I just want to say a quick thank you to everyone who helped make this program possible. I think it’s been a great learning expereince and it’s been a lot of fun along the way. Also thank you for reading! I hope you enjoyed it! Take care and wish you all the best!
Sincerely,
J. Austin Buen-Gharib
Week 6: Next Steps, Final Thoughts, and Many Thanks
So hopefully I can wrap up everything in this post. In our last week we ended up giving two presentations,one for Dr. Nishioka, some of his colleagues, and the office of process improvement; and a second one for the rest of our CIP team.
After our first presentation in the hospital, the doctors gave us great feedback but overall thought our work was “outstanding” (and definitely publishable ~ although I feel like that might require an additional testing phase). As far as next steps, they wondered if we would be interested in continuing our project to implementation and execution. While I believe it would be awesome to see a project through from design concept to use, I think there’s also a lot of red tape and it might be tough for us given that John and I are both returning to school soon. I think it could evolve into a great senior design/research capstone project but that’s a bit beyond the scope of this program. I think this project will likely be adopted by ITEA (Innovation Technology and Education in Anesthesia) which I believe is also overseen by Dr. Nishioka. I’m definitely interested to see if our idea would actually work and help out in the OR. It seems that Mass General or Boston Children’s Hospital might already be utilizing a similar idea, although for a slightly different clinical need. While we are still looking into this, I think that helps justify our idea as more feasible although it definitely needs further refining with a closer look at all the details, nuts, and bolts.
Overall I have to say that I really enjoyed this program. I learned so much and had a lot of fun. I feel much better heading into senior design because I now realize the design process is called a process for a reason. There are concrete steps that we focus on and in the end it all comes together (hopefully). I think this program’s focus on user centered design really resonated with me and I’ll make sure to take the lessons and experiences from here and apply them to all the problems I face in the future.
I also believe I met some really great people. I knew all the bioEs going in, but it was really nice to spend more time with them this summer. I appreciated meeting all the iMed students. They’re all so smart and I’m sure they can all become great doctors. I have to say (with all due respect) John was probably the best partner I could have asked for honestly. I was a bit worried about working in a 2 man team and how we’d divide up all the work, but if anything I think he may have carried the team more than me. I think we worked pretty well together and I hope we keep in touch.
A big thanks to all the OR staff for letting us be there in the first place and observe and bother them with all of our questions! There’s too many to name, but I wish them all the best!
And a very special thanks to our mentor Dr. Nishioka who really took us under his wing and showed us the ropes. His guidance and support are tremendously appreciated. I also want to personally thank him for all the lunches! I hope I deserved it!
Also I just want to thank everyone that makes the UIC CIP possible (you know who you are). I think it’s such a cool idea and I’m so grateful to be part of it. I want to continue to explore innovation especially in healthcare because those are my passions.
For any future CIP students, best of luck! I hope you work hard, have fun, and enjoy the process of engineering/design/innovation. Maybe I’ll come back and read your blogs some day!
Also thank you for reading my blog! I hope you enjoyed it! And if you have any questions, comments, concerns, or compliments please feel free to reach out to me. I’m always more than happy to help!
This has been Austin Buen-Gharib, thank you for your time, take care, and stay classy!
Over and out.
Ryan Dahlin

Ryan Dahlin Blog
Ryan Dahlin Blog
Week 1 – Pulmonary Critical Care
Ryan Dahlin Blog

Our first week in Pulmonary Critical Care already has me and my Bioengineering partner, Celine, full of ideas for innovation and excited to return to the hospital each day. Our Tuesday-Friday schedule was aggressive with two separate rotations each day. We have already visited the ICU, pulmonary fellows clinic, pulmonary hypertension clinic, bronchoscopy and procedures, and the sleepy study lab. This medley of clinical environments seemed daunting at first, but I’ve come to realize how beneficial it has been to rotate through the different areas of a pulmonary medicine in such short order. It helped us obtain a fuller grasp of how lung disorders are diagnosed and managed.
There were several areas of potential improvement that we identified (some more feasible than others), but we found the contrast between two lung function tests in the pulmonary function lab particularly notable.
Good Design: Pulmonary Function Test Battery (pre and post bronchodilator)
Celine and I had the opportunity to play patient for this particular lung test, and found the process efficient, accurate, and incredibly user-friendly. Our technician was well trained and expertly guided us through a series of computer measured breathing maneuvers in a span of about 10 minutes. We each received a printed report at the end that communicated the results of our tests. The only area of improvement I could identify would be to include more patient-friendly graphics or explanations of the test results in the printout so that patients may better understand their lung function. The printout was clearly designed to be delivered to and interpreted by a physician.
Bad Design: 6 minute walk test
In this test a technician walked with a patient for a span of 6 minutes. During this time, their heart rate and oxygen saturation was measured every minute, and O2 delivery adjusted accordingly, if necessary. The total distance walked was also recorded. This particular test seemed to have a few flaws that I will now enumerate. Firstly, the hallway in which the test took place had several obstacles (chairs, beds, equipment, etc) as well as other patients and medical staff. This proved to be a hindrance to the tech/patient/monitor convoy and seemed to alter the test results. Secondly, one of the techs themselves needed a walker for mobility purposes. This also seemed to be a complicating factor. All in all, there seemed to be too many disruptions in the testing environment for it to be a true assessment of mobility and oxygen requirement. I think using a very small indoor track or specialized treadmill might be a more consistent way of performing this test.
We look forward to presenting our findings this next week and meeting with our mentors to see what other areas of pulmonary medicine are ripe for innovation.
Week 2 – Pulmonary Critical Care
Ryan Dahlin Blog

Having now had time to acclimate to our clinical sites and hours, our second week in pulmonary medicine was much less frantic. We devoted a good deal of our time to more fully flushing out problem areas in designs that we had already elected to improve. We chose, specifically, to focus on the process of patient education during Pulmonary Function Tests. The steps in this process and associated areas for improvement are outlined below.
1) Patient makes appointment for PFTs – They probably know that they are having lung issues at this point but may not fully understand what PFTs are and why they need them.
2) Patient performs PFTs with assistance from their Technician – Some technicians may explain details of their test results as they receive them. Most techs leave this complete up to the physician. Techs could potentially be trained to better educate their patients about PFTs as they are being performed.
3) Patient has two copies of their report physically handed to them to later give to their physician. We learned that it takes four days for the scanned copy of the report to appear in the physcian’s EHR system. We think this is the best area for innovation – a more patient oriented report/cover sheet could be the best tool for patient education after PFTs are completed.
4) Patient may or may not read their report and try and decipher the results on their own. The report itself is incredibly dense and difficult to read even with a medical education, so this is a major area of potential patient confusion/frustration.
5) Patient delivers their report to their Physician. Hopefully the reports have not been lost or damaged at this point, otherwise the patient/physician will have to wait the full four days until the scanned copies appear in the EHR.
6) Physician explains pertinent details of the report to the patient. This varies from physician to physician and patient to patient. Physicians may communicate different or more/less details of the report based on what medical conditions the patient may have.
7) Patient may or may not perform future research on their report/lung function numbers after their appointment.
Although each of the steps in the PFT process has room for potential improvement, we identified that there is no standardized step to insure adequate patient education (if they so desire). We aim to correct this so that patients can be better advocates for their own health moving forward. We believe a patient education cover sheet might be the best way to accomplish this and hope to work on designing one in the coming weeks.
Week 3 – Pulmonary Critical Care
Ryan Dahlin Blog
Week three in Pulmonary Critical Care once again provided new sources of inspiration. Two problems, one mechanical and one within the EHR system made themselves known.
The mechanical ventilators sometimes fail to allow adequate time for their patient to exhale their full lung volume before triggering another inhalation cycle. This leads to a buildup of trapped air volume and alveolar pressure in the patient that can lead to barotrauma within the lungs. Could there be a way for the ventilator to automatically test and correct for auto-peeping at a regular interval?
Secondly, many physicians and other health care workers have pointed out that the number of acronyms used in medical notes can be an issue. Some providers use acronyms specific to their field while others may come up with acronyms on the fly that are not commonly used. This causes inefficiency and confusion for other providers. Could a built in translator be incorporated?
Now, back to the theme of the week, which was needs statements.
We began with a general statement regarding pulmonary function tests and patient education in class:
1) How might we improve patient education regarding pulmonary function testing, to increase patient understanding of their lung function and disease state
Next, after talking to several providers we designed two additional statements – one with the provider in mind and one with the patient in mind.
2) How might we improve PFT reports to show patients the progress of their lung health and underlying condition?
3) How might we improve the layout of PFT reports for easier interpretation by providers?
Finally, we combined our two target users into a joint needs statement.
4) How might we improve the layout of PFT reports for easier interpretation by providers and more intuitive patient education regarding the progression of their lung health and disease states.
Week 4 – Pulmonary Critical Care
Ryan Dahlin Blog

In week 4 of our pulmonary critical care rotation, we began shifting gears from observation to narrowing in our final project goals. We had already previously established our goal of improving the quality of pulmonary function test reporting and education. Now, we began to define what criteria would be essential to measure in order to assess whether we had accomplished this goal.
We defined these criteria in the form of four high level specifications – was our design 1) Intuitive, 2)Appealing, 3) Easy to implement, and 4) Effective?
1) Intuitive – Was our approach to the layout of PFT reports both easier for physicians to rapidly interpret and simple enough for patients to better understand their lung function?
2) Appealing – Was the layout of our new report visually appealing, and arranged in such a manner as to catch the eye and encourage patient engagement?
3) Easy to implement – Were the changes we proposed simple and inexpensive enough to be implemented on a wide scale with minimal difficulties in transitioning from the old report?
4) Effective – Does our both report reduce physician analysis time and increase patient understanding?
We hope to keep these criteria in mind as we move forward with the next stages in our project – brainstorming and designing our solution.
Week 5 – Pulmonary Critical Care
Ryan Dahlin Blog

For our 5thweek rotating through UIC Pulmonary Critical Care, our focus continued to shift towards product design and rapid prototype creation. We spent less time in our various clinics and more time asking focused questions related to our needs statement and potential solutions. In the end, we decided the best way to improve the delivery of PFT reports was a three-pronged approach.
1) Design a cover sheet for the PFT report that was more visually appealing, only listed essential PFT numbers, and contained explanations for patients – we have a working sample of our cover sheet at this point.
2) Develop a tactile lung model learning tool to help physicians explain to patients some of the most common lung conditions. We have a series of three syringe and balloon models that simulate different lung states patients often have – mainly restrictive lung disease, normal lungs, and hyperinflated COPD lungs.
3) Improve the quality of the 6 minute walk test by advocating for the purchase of a sonar equipped self paced treadmill to replace the chaos of performing the test in the busy hallway.
We plan on continuing to develop and improve on our ideas in the next week.
John Jarka

I am a bioengineering student, with passions for improving patients’ hospital experience, and improve quality of life during recovery and post recovery. I was fortunate to be placed in my preferred department of neurosurgery. I will use my time there to learn more about the technology surrounding the treatment of the nervous system and the interactions patients have with this technology. I will apply my new experiences with these devices and patients to further my work with prosthetic and assistive devices, as well as aide in developing my understanding of brain computer interfaces.
John Jarka Blog
John Jarka Blog
Week 1: Introductions and Intubations
John Jarka Blog
My time in the department of neurosurgery started as a blur. My first day began with rounds in the NSICU with Dr. Arshi. His deeply rooted passion for innovation and education became obvious after a short time, and I felt lucky to have landed with such a perfect teacher and guide for my first day. As my eyes and ears began to focus through the passing nurses, residents, and their jargon, I gathered details about my surroundings. The ICU is a rather uninviting place. The chimes and blips of instruments cut from every room and fill the hallways with the torrent of their noises to create an alarm that seemed to always be going off. Most patients were in varying levels of comatose and required devices to assist them in breathing and/or secretion control. Their condition and surrounding tangles of instrumentation created an atmosphere of desperation, and I feel that this likely causes patients and their visiting family anxiety.
After finishing rounding with Dr. Arshi, I left to meet my program mentor, Dr. Mehta, outside the operating room. While I was waiting, I studied the surrounding staff and tried to understand their rhythm. People passed quickly, ducking in and out of rooms, delivering supplies or lending aid. Carts of surgical kits were stacked along most walls of the extra wide hallways, but their seemed to always be staff carrying tools into started procedures. I assume this means the surgeon needing more than expected is not all that uncommon. In general, the OR felt more systematic than the ICU. The planned, methodical atmosphere matched the type of work being done, as much as the unpredictable atmosphere of the ICU matched its own. Dr. Mehta arrived, and we stepped into his OR. The staff outside the sterile field talked casually, while those inside prepared their tools and themselves silently. This divide in demeanor continued through the operation. Towards the later part of the operation, Dr. Mehta used a surgical microscope as he worked, and its partnered screen allowed for myself and three other students to comfortably view the surgery, as if we were leaning over his shoulder.
I was back in the ICU with Dr. Arshi the next morning. I had asked about the mechanism of the assisted breathing devices most of the patients seemed to have. After explaining it, he added that most of the patients are actually capable of breathing on their own, but they have been intubated or have undergone a tracheostomy because they are unable to keep their saliva from going down their trachea. This was as depressing as it was shocking, and I felt a new type of empathy for the patients who suffered through the risks and discomforts of these treatments.
My week ended with Dr. Mehta and one of his students, Dr. Theiss, in the outpatient clinic. Most of my personal experiences in the hospital have taken place in this area, and it felt familiar. The calm, scented air seemed strange after my time in the ICU and OR. The pace of things was still fast, but lower stakes were definitely reflected in the mood of the staff. Things were mostly relaxed, but tensions seemed to always rise when patients talked about their health insurance provider. Patients had missed treatment because they were dropped from their insurance, and others worried what treatments they could afford under their current plan.
Reflecting on my week, I tried to imagine myself as a patient and then medical student. As a teaching hospital, UIC has an obligation to the needs of both. As a patient, I would be horrified to have to choose between the options of tracheal intubation or a traechostomy. Invasive surgery weighted against the discomfort and dangers of intubation would not be an easy choice. Both procedures offer a serious risk of infection, and intubation leads to days or weeks of constant discomfort and/or sedation. Both of these procedures and devices presented the most impactful opportunity for innovation I found this week, and pertained to the needs of the patient. Whereas the use of the surgical microscope as an instrument for both surgery and education was the most innovative solution I found, and it greatly improved the educational experience for students in the OR.
Week 2: Storyboard of the OR
John Jarka Blog

This week I had the opportunity to observe a case, in its entirety, from the perspective of the surgery team. I decided this would make an excellent procedure to storyboard for this weeks exercise.
Things begin when the patient is wheeled into the room, on their bed, from the prep room. One nurse consoled the nervous patient as the other began laying out drapes and preparing the instrumentation. The patient was then asked a series of questions, for identity confirmation, before being anaesthetized and intubated. Because of the area of operation, the patients head was shaved following intubation, and the scalp was then cleaned with several times with a soapy mixture, alcohol, and iodine. The patients head was then rested on what the staff called a “horse shoe”.
This device created a 5-10 minute delay in the procedure. It is difficult to assemble and falls apart often. It is a couple of pads attached to a metal frame, which supports the patient’s head during surgery.
“Horse Shoe”
Perspective from bottom
Ultimately, the staff resorted to wrapping the fixture in gauze to hold the pads on, which is something they said they do often.
Cleaning ended with an Iodine laced sticker being placed across the entire scalp. The mid-line and incision line were marked with a pen and covering sheets were stapled in place around the area of operation. I overheard the staff discussing the occasional patient getting unwanted ear or nipple piercings. An unintended consequence of using surgical staples to hold the sheets in place against the patient. Curiously, the second layer of sheets, and scum bag, were held in place by an adhesive strip on the bottom side of the material, then stapled as well. I wonder if one style of fixation would be enough. The patient’s ID and needed operation was then confirmed a second time by one the surgeons, as a nurse read the patient’s name and operation aloud. The surgeon then proceeded to operate.
During the operation I noticed chances for improvement. The staff didn’t have enough saline to fully submerse the bone flap being replaced and needed to get more from a neighboring OR. Additionally, one of the patient’s IV drips had completely ran out before the attending anesthesiologist had noticed, and blood splattered the sheets and floor where the scumbag had failed to catch escaping fluid.
The operation finished without medical complication. Following completion of the operation, the patient was removed from anesthesia and gently woke up. The patient was then lifted by the surgical staff from the operating table to a new bed that wheeled her into the recovery room.
Week 3: Staff Needs
John Jarka Blog
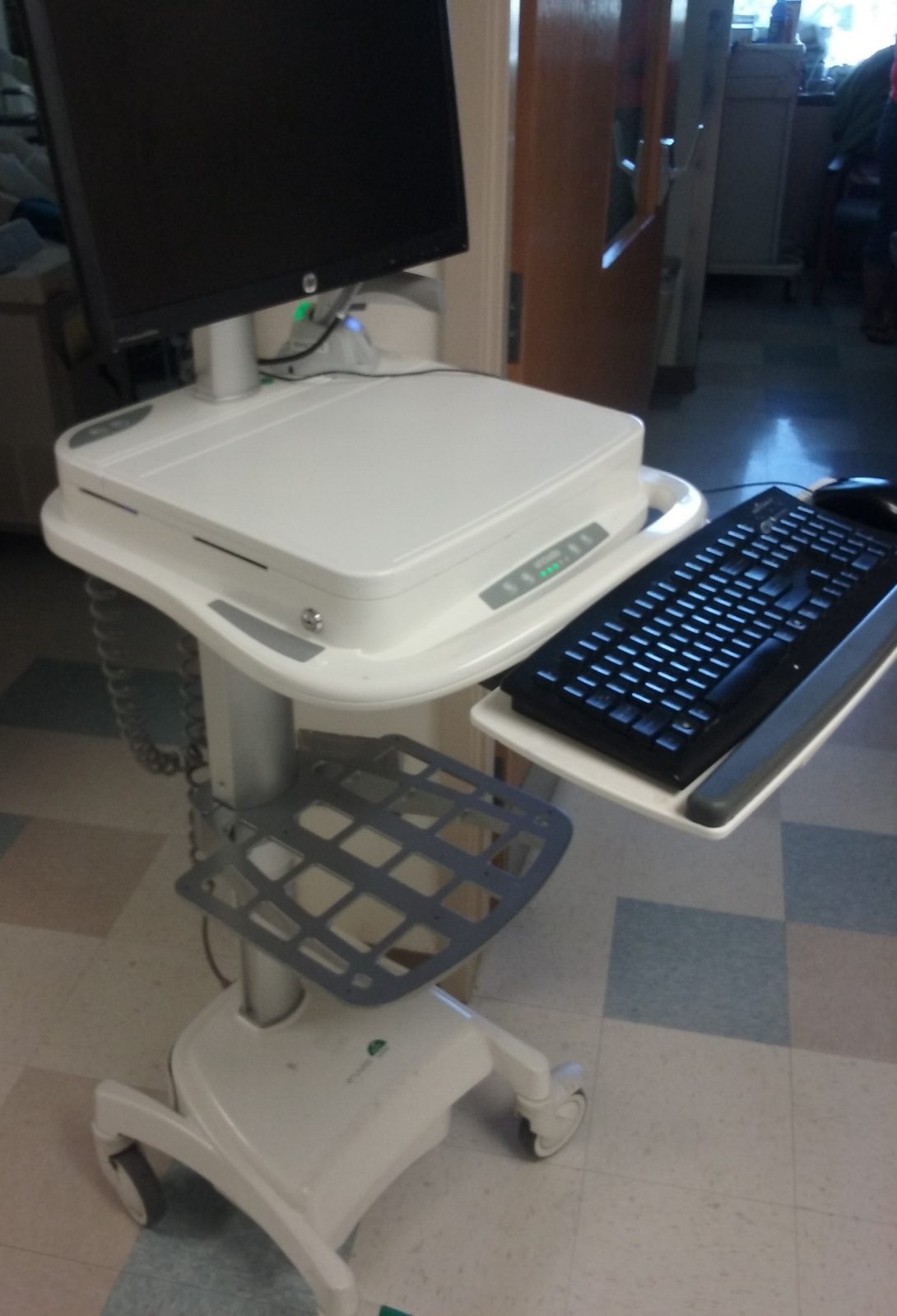
This week was focused on forming and improving need statements. I chose to focus on an issue that affects the staff rounding in the ICU. They use PCs built into push carts, called EMR carts or PC carts, during their rounds to pull up patient records and put in orders for patient treatments. These carts are bulky, dirty, and expensive. My initial statement began as:
“Reduce hallway congestion by reducing the size of the PC carts.”
After interviewing several members of the staff about how they feel about the carts, I was surprised to hear that a lot of them actually liked the larger size of the carts. The increased size gives plenty of space for a table top area for writing, and it also allows for a larger viewing screen and a full keyboard. All of these things would be difficult to accommodate on a smaller model, but not impossible. I revised the statement to:
“Maintaining the current functionality of the PC carts, reduce the the size of aesthetic or non-major components of the cart to allow for improved flow of staff through the ICU hallway.”
I ignored what the staff likes about the carts for a moment, and considered the issue of staff flow through the hallway. On several occasions, in a single morning, staff members detoured around our rounding team to get to their patients or other destinations. This is a big issue in a department that can see rapid patient decline in minutes or even an instant. So the focus then becomes preserving the current characteristics of the carts that the staff likes, while still reducing their hallway footprint.
As an aside, the carts wheels are designed with deep, narrow slits that seem to trap grime from the floor. There seems no easy way to clean them, and with a price point of ~$6,000 this should not be a concern for a device designed for a hospital. However, this design feature may be out of the scope of this need statement. I am thinking of pursuing a redesign of these carts, and now see that several need statements will be needed to do so.
Week 4: Brainstorming
John Jarka Blog
This week was used to brainstorm solutions to a problem afflicting patients of the NSICU. The development of pressure sores is a common issue in the NSICU, which often leads to infections and severe patient discomfort. According to the staff at the hospital, the current solutions to this problem include periodic rotation of the patient, special air mattresses to rotate pressure points, and disposable bedding pads.
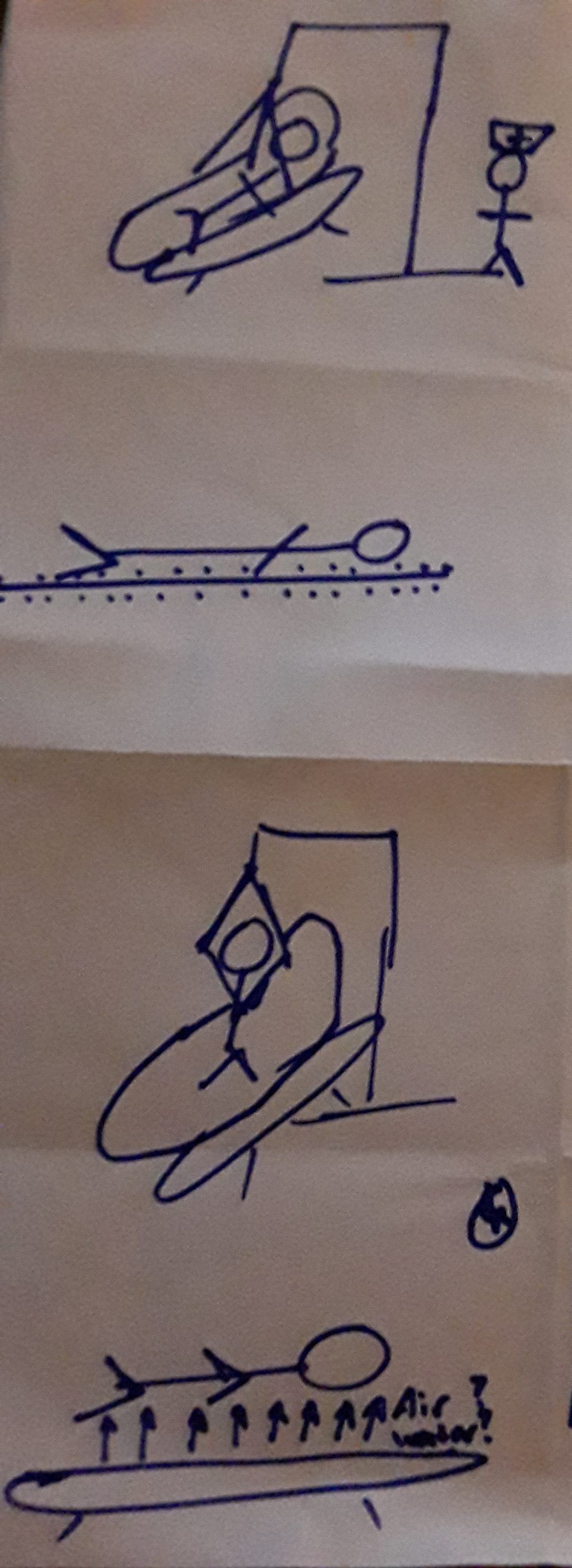
During class this week, we settled on a needs statement. We also learned and practiced several methods for brainstorming ideas and sifting through them (including rapid sketching of ideas, as shown in the image above). Following this exercise, our team decided to pursue several possible solutions. I kept them in mind as we continued our time in the clinic. As well as our need statement: “Prevent the development of pressure sores on unconscious patients”.
It was difficult identifying more criteria for narrowing down to a single solution, and I will be using my remaining time in the clinic to use primary research to narrow down to our team’s solution.
Week 5: Wrapping Up
John Jarka Blog
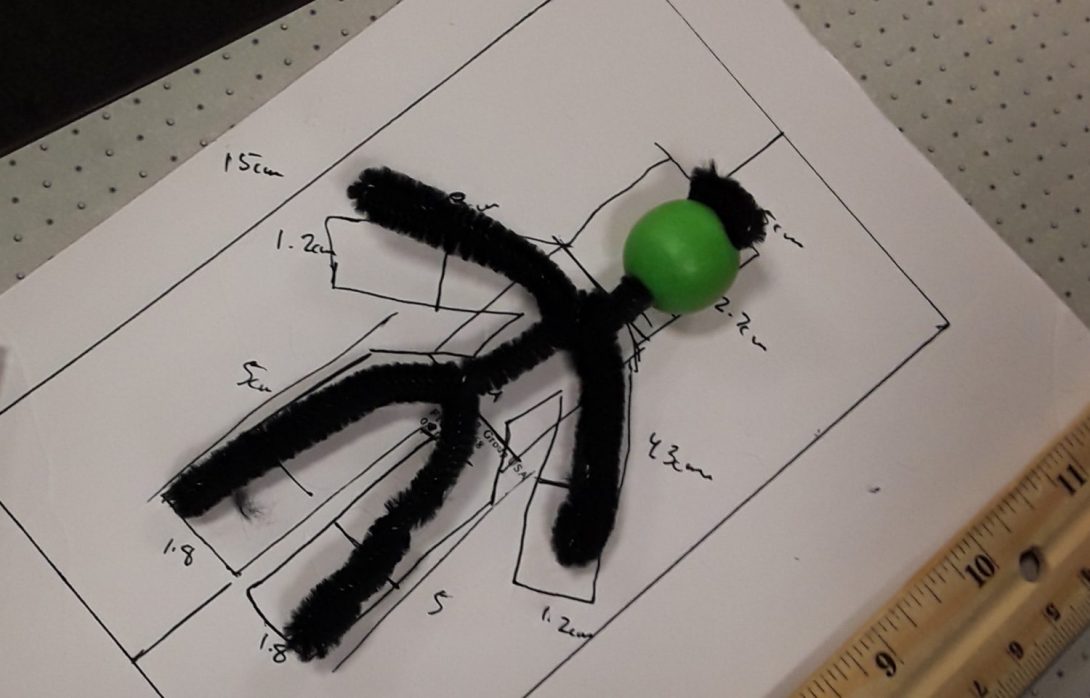
This last week has been my last for prototype refinement. Class time was spent making some very rough prototypes (evidence shown above as a pipe cleaner body analog). With presentations coming up soon, the week int he clinic was spent inquiring with the staff about our proposed device and adjusting from their feedback. Additionally, I spent a great deal of time doing my own secondary research, outside of the clinic, then parsing the differences between staff anecdotes and the literature.
I was a bit sentimental this last week, the hospital has come to feel like home. Its people and their pace are enthralling, and I will miss the days spent listening to their stories and learning through their demonstrations and lectures. Upon the conclusion of this program, I will look for ways of staying involved with the medical campus. Not only do I think it will be beneficial for my professional development, but I have come to really enjoy medicine and the people who practice it.
Aseel Kishtaini

Hello!
My name is Aseel and I’m in my senior year of Bioengineering. I started off as a pre-health student, however with a little of engineering exposure and research, I got fascinated by Biomedical engineering and the impact one can make on the future of medicine with such a background. Advancing in my studies has also helped me focus my learning on medical device development, hence I added mechanical engineering as a minor; in order to learn more about the mechanics of devices. I have also been actively participating within engineering societies to develop prostheses, in which I got to learn about the stages of device development and design requirements. However, I believe that being in a clinical environment and being close to the users of medical devices is an essential experience for every student in order to be familiar with the technology and the methods used n today’s medical institution and find possible improvements that can save lives or make them a little easier!
Aseel Kishtaini Blog
Aseel Kishtaini Blog
Week 1
Aseel Kishtaini Blog

Our experience in the first week of the immersion program in the cardiology department went by in a blur. The first few hours were a little overwhelming with all the procedures and medical vocabulary and abbreviations as well as the struggle of not getting in the way of nurses and doctors. However, we quickly adjusted and were able to record our observations and ask the important questions. I would like to believe that we successfully observed many different procedures and interactions, that we were able to identify a few problems within the clinical setting as well as appreciate the role of bioengineering in simplifying and advancing surgical procedures.
During our time in the clinic we came across a number of problems and complains from the clinical staff that can serve as our focus and an area of potential improvement.
Bad Design:
Problem1: Echo Readings
On our first day we got introduced to Dr. Nazir and Dr. Palm who were in charge of the Echocardiogram readings and procedure for that day. During our time with them we came to understand how difficult it was to read the Echo reports for overweight and obese patients due to bad image qualities compared to fit patients. Dr. Nazir commented that fit patients had a better chance of an accurate diagnosis, and that sometimes with poor image qualities the Doctor would have to ask for another Echo exam or make assumptions.
A = Echo Readings
E = Doctor’s office
I = Doctor with the echo reports
O = Bad image qualities due to obesity
U = Doctor
Problem 2: TEE probe
Another problem that we got exposed to on our first day in the clinic, that was also related to the Echocardiogram is inserting the echo probe into the patient in order to get the necessary images. The cardiovascular ultrasound system includes a 4D transducer for transesophageal echocardiography (TEE). The Echo probe can quickly visualize the different chambers of the heart and the valves, it can detect backflow across the valves and can also provide quantitative data including the ventricular pump function, myocardial deformation and mitral valve morphology. As you can see: this seems like a great diagnostic device and an easy procedure. However, we happened to observe to Echo readings, where the doctors had a lot of trouble inserting the probe into the patient. On our first case, Dr Palm, a fellow, tried a couple of times to insert the Glide into the esophagus however it she wasn’t successful, that’s when Dr Nizar interfered and tried herself for a few minutes and still couldn’t insert the probe. The doctors tried a couple of workarounds and tricks, such as having different positions of the chin and the chest, asking the patient (who was a little bit too sedated to corporate) to swallow to help slide the probe into the esophagus, they also tried removing the mouth piece and the nurse held the patient’s tongue out to open up some space for the probe to go in. However; nothing worked, and since the patient was on blood thinners the doctors did not want to risk a rupture in the esophagus, so after about 15 minutes of trying, they called the procedure off. In the other procedure, who was performed by Dr Palm and another attending, they spent around 10-15 minutes trying to insert the probe, but they had more success. Overall, we as a group believe that this is a very important design to focus on in order to make sure that the patient gets the exam they paid for, and save them from potential problems, such as esophageal rupture, as well as reduce procedure time.
A = Echo Exam
E = EP lab, which also happened to be over crowded with open drawers and wires everywhere, which can be hazardous.
I = Doctor trying to insert the echo probe into the patient’s esophagus with the help of the nurses to adjust the patient into different positions.
O = Transesophageal echocardiography probe
U = Doctor
Good Design:
We have of course also come across many fascinating and smart designs.
Design 1: Atrial Flutter Ablation Mapping system
During our time in the electrophysiology (EP) lab we observed an atrial flutter ablation procedure which was performed by Dr. Wissner with the help of two Boston Scientific representatives. The program that was developed by Boston scientific allows the doctor to map the entire atrium by just inserting a catheter with 20 electrodes into the groin area and up to the atrium. The mapping is very fast and accurate, which provides the doctor a full visual of the heart. The program also detects electric current in the atrium and can clearly show when the ablation is successful. Another catheter with fewer electrode and a cooling mechanism is also inserted through the groin into the atrium, and is used to create the ablation and stop looping of electricity in the atrium which causes the atrial flutter. The location of the ablation is clearly represented in the map of the atria as red dots, in which the doctor can keep track of his procedure and see what points he might be missing for a complete ablation. This was a great example to see the impact of bioengineering in the medical field, that it allowed to completely transform a surgery and make it much simpler and less invasive.
A = Atrial Flutter Ablation
E = EP lab
I = Doctor and Boston Scientific Bioengineers
O = Atrial Flutter Ablation Mapping system
U = Doctor
Week 2
Aseel Kishtaini Blog

Although week two of the program was a short week, we got to see many new and very interesting procedures. We were able to scrub-in to most of the procedures and were much more comfortable with the terminology and asking questions.
We got more information about cardiac cauterization and talked to DR. Shroff about the advancement in technology and its role in saving the patient’s life. He mentioned an important service by the Chicago Fire department: where the ambulance is equipped with a LifeNet system that would send the patient’s EKGs to all close by hospitals. A dispatcher would then direct the ambulance to the closest Emergency room prepared with a heart attack center. The doctors would also get the EKGs by text message so they have the time to look over and assess the case before the arrival of the patient.
With Dr. Wissner, who is also our mentor, we got to scrub in into three procedures; one of them was a pacemaker procedure, and we learned about the placement of the leads and thresholds tests performed to set the accuracy and effectiveness of the device. The other two were ablation procedures done mainly through the advancement technology and biomedical engineering. As the atria were completely mapped and had an image for the electrical activity was present at all times to determine the progress of the procedure. Dr. Wissner got to use a newly developed balloon catheter; equipped with a camera, and a 360 degrees rotating laser for the ablation. The pulmonary vain isolation ablation procedure was one of the most fascinating and we got to learn a lot about the different programs and systems developed by engineering to make surgeries more efficient and less invasive.
However, for our storyboard assignment we decided to go with our week one problem: The Transesophageal electrocardiogram (TEE). Week two we got two see two more procedures that went a little more smoothly, however there were still some complications. Therefore, here is a rundown of the procedure:
Step 1: Doctor requires a TEE for diagnostic purposes
Pain points:
- Some patients might be over the weight specifications to go through the procedure.
- Some patients might not understand the importance of this specific procedure, given they have done another kind of electrocardiogram.
Step 2: Patient has to fast for 24 hours
Pain points:
- 24 hours are a very long time to fast and many patients fast for about 12-6 hours instead.
- Some patients have medications to take which are required to be taken with food
Step 3: Doctor reviews records and obtains consent
Pain points:
- In emergency situations, records are not easy to find
- Some patients have allergies to medications and anesthetics used in the procedure
- Patient might be unconscious and the procedure is needed to be performed immediately for another lifesaving procedure.
Step 4: Setting up the procedure
Pain points:
- Monitoring equipment might take time to set up and attach to patient
- Some patients are in critical conditions and are intubated or need extra measures; which means adjustments and workarounds are needed.
Step 5: Applying anesthetic: oral
Pain Points:
- Patient might have allergic reactions to anesthetic
- Time required for the throat to be numb enough and minimal gag reflex.
Step 6: Inserting probe
Pain Points:
- Requires specific directions that might be hard to follow and should be adjusted for each patient.
- It requires experience to know the limits of the esophagus and how gentle they should push against the pharynx
Step 7: Taking good images
Pain Points:
- Quality of images is different for each patient and getting some angles and images is challenging
- Controlling the probe at the mouth and at the knob with one hand is uncomfortable due to the size of the probe.
- Another physician is needed at the computer/device to take the images
Step 8: Reading the Echo and making a decision
Pain Points:
- The doctor who reviews the TEE images is not the same one who took the pictures, so difference in experience and perspective plays a role in diagnosis and use of the images.
- The physician needs to make some assumptions for their conclusion of the test due to the bad image quality.
Although The TEE is a great diagnostic test that is essential for many procedures, small improvements can be made to increase efficiency and accessibility.
Week 3
Aseel Kishtaini Blog
Needs Statement:
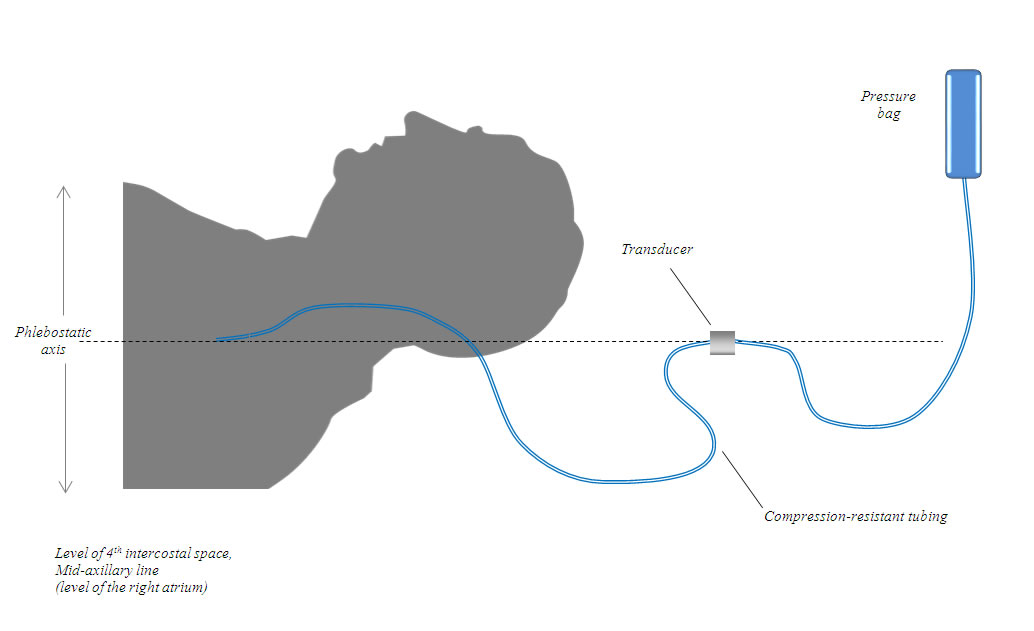
A potential problem that we observed and investigated on our third week of the program is the alignment of the physiological pressure transducer and the right atrium during catheterization procedures. During our time in the clinic we noticed that the nurses have to bring in a ruler and measure the patient’s and the transducer location to make sure they are leveled. We talked to one of the nurses about the problem and she said that they need to make sure the transducer is leveled and have to check multiple times, in which thy bring in a ruler and measure the patient’s axillary line and compare it to the height of the transducer. We believe that an easier and a readily available alignment mechanism would be helpful and more efficient.
Needs statement: is a brief summary that addresses a specific problem and provides a rationale
“A way to address the alignment of pressure transducer and the mix-axillary line for patients to ensure accurate measurements and quick setup”
“A way to address the alignment of the physiological pressure transducer and the mix-axillary line for patients undergoing procedures to ensure accurate central venous pressure measurements and quick setup”
– Adding physiological pressure transducer to make sure that the statement is specific to vitals in intensive procedures.
vs
– Making the population more specific as well, as the transducer is needed only during procedures
– Adding venous pressure measurements to make sure we are addressing one specific problem.
“A way to address the alignment of the physiological pressure transducer and the mix-axillary line in supine patients to ensure accurate central venous pressure measurements and quick setup for procedures”
– The setup for our problem is specific to supine patients
“A way to address the alignment of the physiological pressure transducer and the mix-axillary line in supine patients in intensive procedures to ensure accurate central venous pressure measurements and quick setup”
– The setup is specific and needed only during intensive care procedures
Week 4:
Aseel Kishtaini Blog
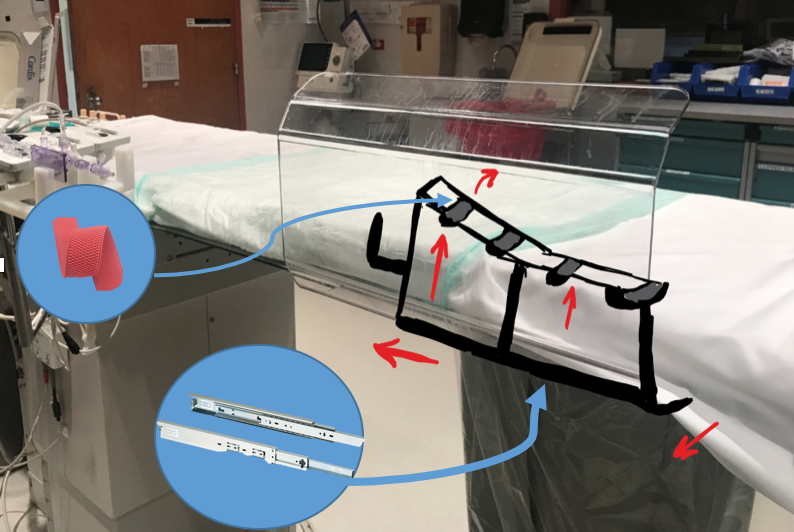
Our week four consisted of a lot of interviews and brainstorming about our final project. Talking to doctors and nurses helped us switch gears into a more prominent problem in the operation room during percutaneous coronary intervention procedures. We came to understand that although accessing the heart through the left radial can be safer for the patient and a less complicated procedure, most physicians avoid it and try to go for right radial or femoral access. The problem with accessing the artery through the left arm, is that most operation rooms are set in a specific way which doesn’t allow for changing the layout of the operating table or the equipment, as well as the fact that most physicians are not used to the new layout which they think would require more training. Also leaning over the body of the patient would put the doctor in the range of more radiation, which makes it more undesirable.
So our suggestion is to develop a left arm elevator that would raise the arm and cross it over the body so that the doctors can access the left radial more easily without changing the setup of the room and the position of the doctor. Our most recent iteration of the needs statement for this problem is “Optimizing accessibility of left radial artery in order to expedite patient recovery, decrease doctors’ radiation intake, and reduce physician fatigue”. And the design specifications for our design include:
- Comfort
- Since the patient is going to be immobile for long periods of time, the arm has to be cushioned well and not create any pressure points that would affect the procedure.
- Our design can be mechanically adjusted to match the needs of the doctor and patient; height wise as well as position.
- Safe
- Design has to be safe enough and have locking mechanisms for different positions so that it doesn’t move the arm during the procedure.
- Intuitive
- Design is going to be easily manipulated and adjusted mechanically.
- Mobile
- Attachable design that can be added/removed any time to any bed.
- Feasible
- Cost effective: no need for new equipment (operating tables) or changing the setup
- health benefits: our research and interviews has also showed that going through the left radial would save on operation time as well as recovery time, and has less complications.
- Adaptable
- Using slider attachments that can fit various beds
- Adjustable
- The design has to be adjustable to fit different patient sizes and body shapes.
Week 5: Prototyping
Aseel Kishtaini Blog
On the fifth week of the program we have focused mostly on interviewing the doctors and the staff in the cardiology department and getting feedback on our ideas for the final project. We have run the ideas and the rough design by two attending physicians to make sure that our design specifications are accurate and needed. Both doctors were very supportive of the idea and had a lot of feedback including the importance of such a design in making left heart catheterization procedures more accessible for doctors; thus reducing procedure time and risks. We have also worked on iterating and focusing our needs statement and worked on our prototype.
Our current needs statement is “Optimizing left radial artery accessibility in catheterization patients in order to expedite patient recovery, decrease doctors’ radiation intake, and reduce physician fatigue”. We proposed to design an adjustable arm rest that can be attached to any operation table, and is used to lift the left arm and slightly cross it over to the right side for better reach and accessibility.
We worked together to come up with more specific design requirements and goals to make the arm rest as functional and beneficial as possible. We came up with the following ideas:
- The design includes lockable rails that are attached to the bottom of the operation table. These rails would allow the nurses to position and adjust the arm rest for wider and taller patients.
- The arm rest can be elevated up to 30 cm which covers all patient shapes and sizes and can also be used for patients suffering of congestive heart failure and have to sit up during the procedures.
- The arm rest is made up of two parts, one to support above the elbow and another part to support the forearm and keep it in place.
- The arm rest is made up of the same material as the hospital beds to provide comfort for the patient.
- It has to be cleanable and can be used in sterile procedures.
- Must be radiolucent and not interfere with fluoroscopy.
- Use lockable flexible joints such as ball and socket so it can be easily adjustable according to the physicians and patient’s needs, and can be locked for stability and safety
- The arm rest also contains a band that exposes the wrist by holding the palm down providing better accessibility and stability.
Etc.
We have been coming up with more ideas and specifications as we model the design in SolidWorks, hoping to see how the different parts fit together and be able to provide a visual of the proposed model and build a prototype by the last week.
Young Jun Lee

Young Jun Lee
Young Jun Lee Blog
Young Jun Lee Blog
Week 1 Notes – Urology – Young Jun Lee
Young Jun Lee Blog

Over the course of the first week, the urology group was able to rotate through the clinic, the operating room, and the waiting area. We tried to apply our AEIOU (Activities, Environment, Interaction, Object, and Users) framework to understand the situation clearly.
Furthermore, Urology Lab meeting at the Innovation Center clarified our goals for the summer, to make clear user centered needs statements, needs specifications, and to conceptualizeand prototypea validated, solution driven approach to a problem. (and the endless feedback to improve everything in the path).
Each team member (Jude, Lara, and I) brought up problems we saw in our visits throughout the week, and weighted them based on multiple factors i.e.
- Patient Impact – Does this problem life-changing or a minor nuisance?
- Doctor Impact – Does this problem significantly impact physician activity?
- White Space – Does this problem have other players in the field?
- Personal Interest – Does this problem interest you personally?
- Market Opportunity – Does this problem impact a wide audience?
Lara brought up an issue that she saw while in clinic, where patients were not preparing for their prostate biopsy correctly. We took a stab at the problem, using the AEIOU framework.
- Activities – Prostate Biopsy Preparation non-compliance
- Environment – Patient’s Home
- Interactions – Physician Patient Interaction / miscommunication about directions
- Objects – Instructions on how to prep for prostate biopsy
- Users – Patients who do not understand the instructions correctly
We discussed the outcomes – the clinic delay, patient delay, infection risk, and physician time wasted as well as how they can be measured.
Then we moved to phrasing them in “A better way …. as measured by ….” and find the appropriate scope. Some examples were
- A better way to follow up with the patient before procedure as measured by frequency of delayed prep
- A better way to make sure the patients are able to get the medication
- A better way to standardize prep
- A better way to make prep unnecessary
- A better way to make biopsy unnecessary
In this step, we had to differentiate the problems into different groups, whether they were patient-behavior types, patient-physician interaction types, or physician-technology issues. While there are rooms for improvement in insurance, healthcare delivery, and society level, we wanted to focus on patient-focused problems.
In order to look deeper into why patients had issues complying with prostate biopsy preparation, we had to learn what goes into a prostate biopsy preparation, and what parts the patients are most likely to make an error.
With five weeks left, the group will need to constantly think in an innovative mindset, and this exercise has prepared us to define the patient need more precisely.
Photo Credit: Young Jun Lee
Week 2 Notes – Urology – Young Jun Lee
Young Jun Lee Blog
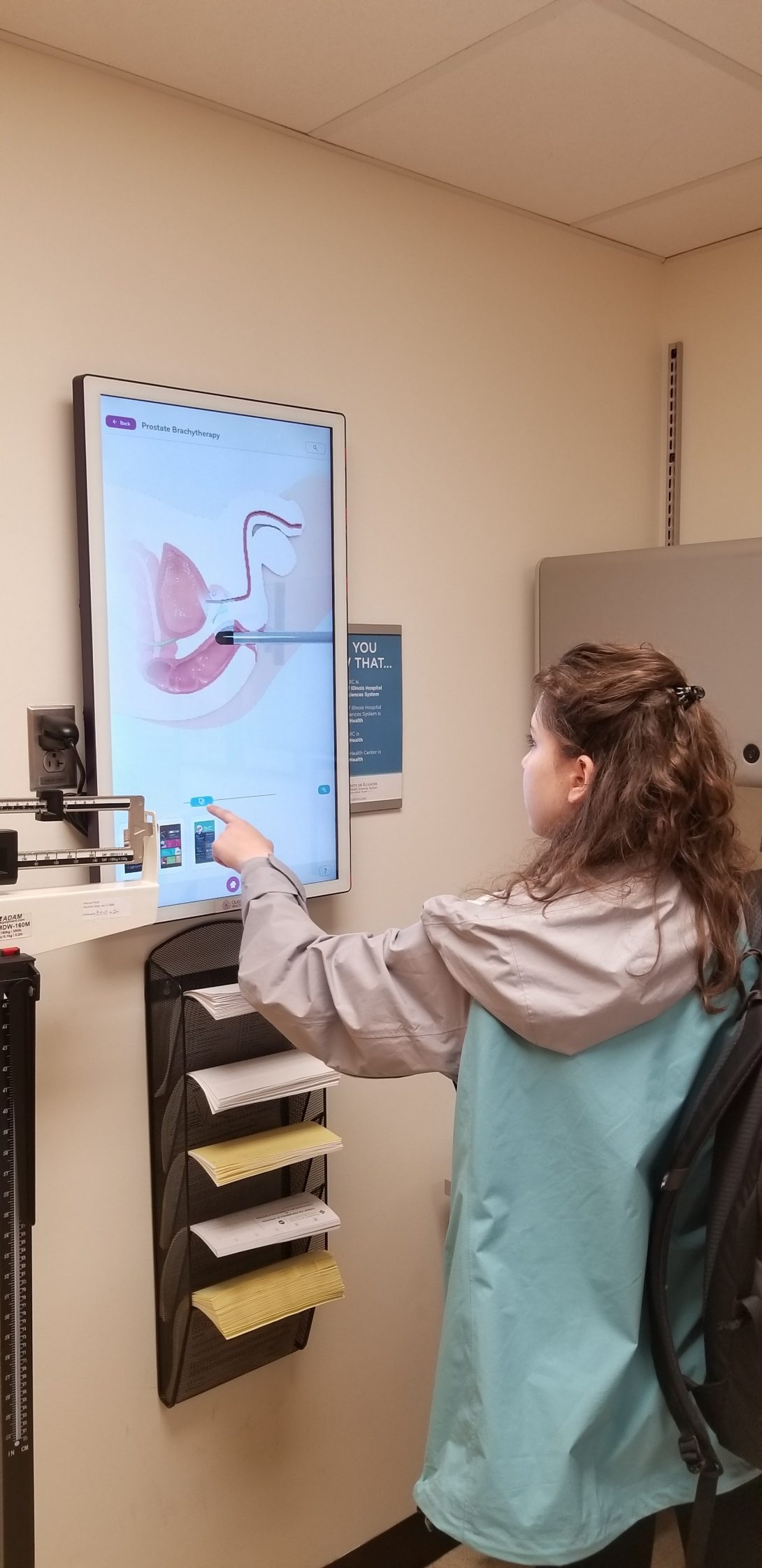
This week, we made more observations in the clinic and during the morning rounds with the urology department in surgical ICU. (Featured Image shows Lara interact with the touchscreen monitor showing different procedure/anatomy in the clinic, so the physician can communicate better with the patient)
Then we discussed our observationswith each other and compiled a list of potential problems. From there, with help of Whitney (PGY-4), we derived a list ofneeds statements. These statements did not suggest any solutions on purpose, and we attempted to make multiple needs statement for each observation, because we did not want the scope to be too narrow or too large.
Next, we compiled a decision matrixby coming up with reasons why each problem is important. They were:
- Patient Impact,
- Physician Impact,
- Market Size,
- White Space,
- Personal Interest, and
- Feasibility (within the Clinical Immersion Program).
Each category was given a score of 1-3, where greater number equated with a bigger reason towards picking a problem (i.e. an innovative NG tube could potentially have a wide market, but there are already saturated market for innovations to prevent NG tube blockage).
Finally, we presented the triaged problems from the decision matrix to the Urology Lab meeting. We received many feedback from the Innovation Center with experts from different field (physician, bioengineering PhD, designer, intellectual property, business management), and will improve upon the problem list.
Week 3 Notes – Urology – Young Jun Lee
Young Jun Lee Blog
After presenting our story of a 50 year old man who went through the prostate biopsy, I decided to spend more time looking at people who were going through the prostate biopsy.
Prostate cancer is quite common, with 1.1 million new cases in the the world (~50,000 in US) per year (World Cancer Report 2014), and although prostate biopsy does not mean prostate cancer, it is the gold standard for diagnosing prostate cancer, and over 1 million prostate biopsies are done per year in the US.
After we worked on the storyboard, I wanted to focus on all the stakeholders in the process. We imagined where the pain points were for the patient, but wanted to verify and validate these.
I filtered the clinic patients to see who was coming by for prostate biopsy, and met Mr. D. Mr. D, who came in with his wife, had gone through prostate biopsy, and had learned he had a positive test. Further imaging demonstrated that the cancer had not metastasized, and he came in to discuss possible options, between surgery, and radiotherapy.
After a lengthy discussion of benefits and risks of these options, the patient chose surgery, and I watched them with our point person for scheduling surgery. This person discussed preparation for surgery, with pamphlets that described the process in depth. When I interviewed them, the patients told me that making the decision between radiotherapy and surgery was the most difficult portion of the whole ordeal.
That’s when I realized our previous needs statement, which had focused on prostate biopsy preparation might be too narrow in its scope. Of course there are pain points in prostate biopsy, including pain, and hematuria (blood in urine), hematospermia (blood in sperm), but patients view the problem differently.
My needs statement was thus revised to focus on the patient: A better way to deliver/communicate the news of prostate cancer to the patient, and navigate them through the intricacies of healthcare to receive proper care, and provide support in times of need.
It was difficult to quantify this information, but I met a nurse practitioner at the hematology oncology clinic who was tackling this exact issue, by asking patients for their need for support, and screening them with social workers should a need ever rise. They have access to patient health outcome as well, so they plan on publishing their paper on this, which will help us understand their impact.
We then spent time at a cancer support group meeting, listening to each patient’s experience as they have gone through the chemotherapy, surgery, radiation, and so forth. The meeting was organized by an external nonprofit community organization, and their location is free for all cancer patients, and have many wellness activities.
I plan to do more research to see whether there will be benefit/market space in connecting men with prostate cancer to these non-profits.
Week 4 Notes – Urology – Young Jun Lee
Young Jun Lee Blog

Last week, I developed the ideas for prostate cancer further, and the visit to the Gilda’s Club Chicago made me become aware of other support that is available to men.
This week, we took the problems that our team have developed separately, and decided to pick on an problem that we would dedicate the rest of our time.
Our focus ultimately turned to how we can mitigate the gap between clinics for a new patient. When a patient is referred from a primary care physician (PCP) (who’s not in University of Illinois Health) to University of Illinois Health (UIH), medical assistants (MA) try to figure out who the PCP for the patient is and what data needs to be sent to the urology clinic before the physician can examine them. If the referring clinic does not provide this information (i.e. imaging, labs), the urologists will have difficulty in figuring out the best treatment method.
This problem, however, is dependent on the clinic.
In one UIH clinic, I measured on 7/18/2018 that 1 of 6 of the new patients from outside UIH had difficulty bringing in their information, and the MAs spent about an hour per shift to track them down. (while seeing 34 total patients in the clinic for whole day). The MAs estimated that this was an issue about once or twice per month.
In another UIH clinic, this problem happened almost every clinic (or once per week), due to the lower socioeconomic status of the patient population, who have less continuity of care. The MAs have difficulty locating the PCP, and patients have lower health literacy, leading to visits where the patients do not understand their reason for their visit. Some patients will come from the Emergency Department, and the MAs will spend time tracking the patients’ medical history.
However, our primary research with physicians, nurse practitioners, and medical assistants suggest that this is a problem that does need to be addressed.
Then using our brainstorming ideas from the Innovation Center, we looked at possible solutions, and then researched other current solutions. This helped us decide how our solution would solve different portion of the problem, or to solve it in a unique way that the current solutions do not address.
Furthermore, we worked with our residents to understand the most relevant medical information regarding patient health in Urology. Many patients with diabetes are now more aware of A1C values, and we want to bring important numbers more available to the patients.
Week 5 Notes – Urology – Young Jun Lee
Last week we brainstormed ideas for our problem of inefficient data sharing across clinics. This week we worked on prototyping on our need: “Inefficient sharing of patient tests between different healthcare delivery systems results in delay of care, redundant testing, and additional expenses.”
We divided our brainstormed ideas to different process of data sharing. In the Innovation Center, we used some of the material provided to create a device that a patient could carry, and looked into the specifications on its strengths and weaknesses.
We also thought of an idea that would facilitate the physician once the data is received, and looked into the possibility of the idea. The idea would look for what the physician do when the batch of patient medical records is handed to them, before they see the patient.
I also went to visit the Medical Records department to learn how they were uploaded once they were given. Medical Assistants were printing the pdf that is generated through the e-Fax, then the physician would use paper copy, then the paperwork would be sent to medical records, where a room full of people were uploading them into the right patient file.
While the excess of paper might be not as effective of a scope as the needs statement, it is a layer that could be improved to potentially see more patients on a reliable manner.
Then we discussed value proposition, the economic viability, as a sort of a thought experiment.
Michael Lukas

I’m a rising senior undergraduate bioengineer.
Michael Lukas Blog
Michael Lukas Blog
Week 1 – Learning Curve (6/25 – 6/29)
Michael Lukas Blog

Orthopaedics is the branch of medicine that addresses and treats deformities of bones and muscles, and I am grateful to be placed in this department at UI Health for the 2018 Clinical Immersion Program (CIP). During this internship, I will be mentored by the renowned orthopaedic surgeon, Dr. Gonzalez, and work with a rising second year medical student to observe the clinical environment, identify problems, and conceptualize solutions. The purpose of this public blog is to document my clinical experiences and answer weekly prompts, both of which I may reflect upon later.
On Monday, the CIP faculty clarified our objective of developing a user-centered design approach, and established a framework for making successful clinical observations. The framework consists of five observable artifacts: Activities, Environment, Interactions, Objects, and Users (A E I O U). We were also given notebooks for documentation and received a teambuilding exercise from guest speaker, Byron Stewart. Our prompt for this week is to utilize the A E I O U framework and identify “good” and “bad” designs within the clinic.
On Tuesday, my colleague, Rown, and I arrived at the Illinois Bone and Joint Institute (IBJI) off Michigan Avenue in Chicago. I commuted to the building on foot from Union Station, and to reach the office, I had to pass through a revolving door and then a security gate to get onto an elevator. I also noticed two nearby parking lots/garages. Although the clinic was easily accessible for me, I wonder if commuting barriers could deter handicapped patients from visiting a clinic. Nonetheless, most of Dr. Gonzalez’s patients at the IBJI clinic were visiting because of hand related issues, so I don’t imagine mobility being a major concern, unlike for the patients at UI Health. Upon arrival, I introduced myself to the secretary, and she escorted me to Dr. Gonzalez’s office. I had apparently arrived before Dr. Gonzalez and his resident, but I had the chance to meet another orthopeadic surgeon, who mistook me as a new resident. The doctor expressed great respect for Dr. Gonzalez for his skills as a physician. I observed the clinical environment while I waited. The clinic itself was aesthetically pleasing and was directly connected to a physical therapy facility. In the office were four desks with desktops, stacks of (somewhat) organized papers and folders, and windows with an amazing view of Millennium Park. I would later find out that this office is where Dr. Gonzalez resides to fill out paperwork when he’s not attending to patients.
Dr. Gonzalez’s resident arrived soon after and surveyed a list of 20 incoming patients that a nurse had placed on his desk. While reviewing the list, the resident distinguished new patients from returning patients. New patients would almost certainly require an X-ray or MRI to determine a treatment plan, while returning patients came in for check-ups following a previously prescribed treatment. We visited the first patient once Dr. Gonzalez arrived. There were about eight patient rooms, and each room was only big enough to hold approximately six people. In each room were two chairs, an exam table, a countertop, and a bottle of hand sanitizer that was frequently used by the doctors. On the outside of the room, clinicians used signal flags that were installed on the wall next to the door. Some of the flags were labelled “INJECTION” or “X-RAY”. For example, if a physician needs a new X-ray from a patient, they would put up the “X-RAY” flag near the room, and a nurse or technician would escort that patient to the X-ray machine. X-rays and MRIs were evaluated on a monitor in the hallway, but required doctors to log in before every use with a password, which seemed to be a bit of a nuisance for them.
Dr. Gonzalez examined his patients quickly and effectively. He performed physical examinations, using his hands to assess flexibility and pain sensation. He would feel for tension around the joints and ask the patients if they feel any pain when he moves their extremities in certain directions. Many times, he would order for the patient to get an X-ray or MRI so that he may have a better look at fractures or joint deformities. Common issues seemed to involve hand fractures, rheumatoid arthritis, and jammed fingers. Once he fully assessed the patient’s condition, he would consult with the patient possible treatments such as seeking physical therapy, getting a steroid injection, or surgery. On occasion, he would also advise the patient to wear a device that would stabilize movement around the joint like a brace, splint, or buddy tape. The clinic also provided other services such as removing casts and sutures. I was surprised by the strong relationships Dr. Gonzalez formed with his patients. He clearly respects his patients, always giving his honest opinion in a kind manner. After the examination, he would sometimes inquire about the personal life of the patient and discuss various subjects such as the quality of pizza parlors. I was also impressed by his Spanish-speaking ability that he showcased when interacting with some other patients. Although his father says that he speaks Spanish like a “gringo”, Dr. Gonzalez proved how much of an asset being bilingual can be. I learned a lot on the first clinical day, but would have the opportunity to compare the IBJI clinic with the one at UI Health the following day.
I arrived early to the orthopaedics clinic at UI Health on Wednesday. I parked at a parking garage near the hospital, took a large elevator to the second floor of the hospital, and walked across a bridge that connects the hospital to the clinic. When I entered the waiting room, I noticed there were more chairs than the one at IBJI. The secretary showed me to the “Attending Physicians” room, which acted as the central hub for doctors to hang out in between patient examinations. The room was shaped and functioned like a narrow hallway, with two doors on both ends of the room and half a dozen rolling stools and computers lining both sides of the walls. The room was just wide enough for three people to stand shoulder-to-shoulder. In the center of the room was a monitor that displayed X-rays and MRIs, but unlike the one at IBJI, it did not require doctors to login with a password every time it’s used. There were usually two attending physicians using the room at a time, with a team of medical students and residents reporting patient information to them. Residents were constantly using the computers in the room, either reading a patient’s history, or submitting a summary of a patient’s visit.
Week 2 – Holiday (7/2 – 7/6)
Michael Lukas Blog
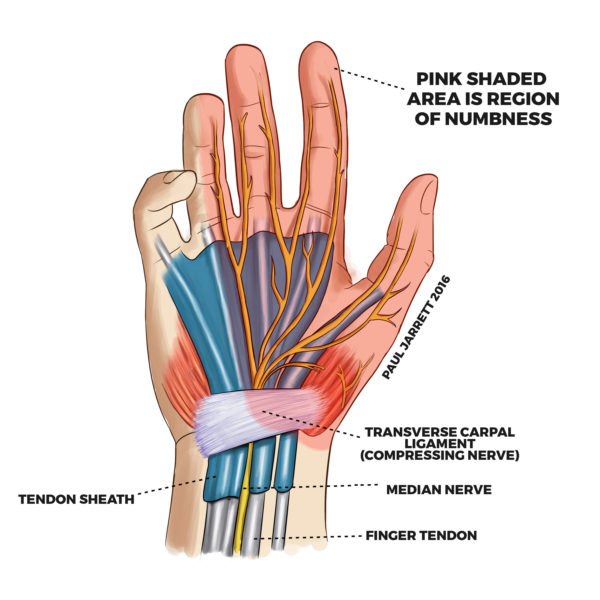
This week’s prompt was to identify a step-by-step process and create a storyboard for it. We were able to stick with three patients and observe their entire visit from when they checked in to when they scheduled a follow-up. The storyboard we’re presenting on Monday is heavily influenced by what we observed from the first patient.
Dr. Mejia introduced us to the medical assistant (MA), Claudia, working the front desk. Claudia introduced us to the plethora of problems she noticed in the clinic that could be improved. One was the “world of disconnect” between MAs and Residents. Another was the poor quality user interface of the Cerner electronic health records (EHR) system that was currently being used in the clinic. She believed that tablets and an improved EHR system would improve the “flow” of the clinic. After thanking Claudia for her insights, we went to observe the process of one patient’s visit.
The first patient we observed was a 30-40 year old woman with carpal tunnel in both wrists, with more severe symptoms in the right wrist. She first checked in at the front desk, which was indicated by a notification icon that appeared next to her name on the MAs schedule. It was the first time the patient visited this clinic, so the MA printed out a referral by the primary physician with details of her medical history (Chief Complaint, Symptoms, History of Illness). She then took the printed out record, called for the patient in the waiting room, and escorted her to an available examination room. The MA placed the medical note in a bin outside the door and raised the green flag before entering the room. When the MA and patient were in the room, the MA asked a few questions to fill out an intake form for the clinic. Once finished, the MA leaves and a medical student, who reviewed the note in the hallway, enters to assess the patient. The patient was first asked a series of questions to understand the reason for the visit. The medical student then performed a physical examination to measure the pain of the injury. During the examination, the medical student took notes with a pen on the margins of the document itself. After the examination’s completion, the medical student leaves the room and summarizes what she learned to a resident. The resident then takes a look at the patient’s medical note and asks the medical student a few questions about past treatments and medical tests. Once the resident is informed of the patient’s reason for the visit, he enters the patient’s room with the medical student. This time, the resident asks the patient questions and physically exams the patient while the medical student continues to take notes. Afterwards, the two clinicians leave the room again and seek out the attending physician. The attending is then debriefed patient information by the resident. The attending enters the room with the resident and medical student and gives the patient her third examination. The attending discusses with the patient all the possible treatment plans. In this case, the patient agreed to wear a wrist brace at night and take vitamins for the next two months. The attending, resident, and medical student leave the room as the patient waits to get her brace fitted. When done, the patient heads back to the front desk to schedule a follow-up appointment. Much later in the day, the resident dictates to a transcriber on a phone information about the patient’s visit to create a new clinical note. Dictation takes residents about 3-4 minutes per patient. The MA, however, inputs all her patients’ information for the clinical intake form into the Cerner HER system at the end of the day.
The next two patients we observed underwent similar processes, except both of them needed an X-ray of their joints in the nearby radiology department. The third patient also had his cast removed by a cast saw used by another resident. I promise to go into this in further detail at a later time. But for now, I look forward to learning more about our next week’s prompt.
Week 3 – Necessities (7/9 – 7/13)
Michael Lukas Blog
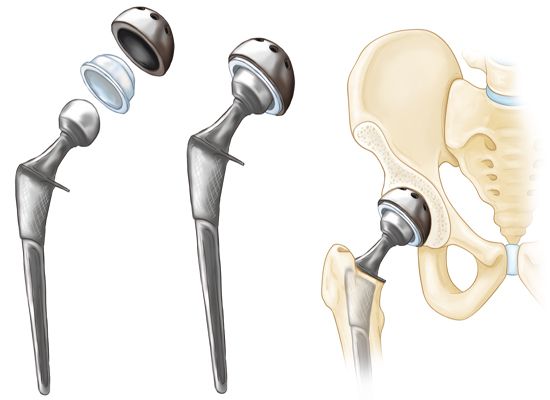
This week’s prompt was to come up with a “needs statement” within our department. We have to identify certain things that can be improved upon using our observations. Luckily, this was our first week in the operating room (OR). While in the OR, we were able to witness multiple orthopaedic surgeries: two total hip arthroplasties (one being a revision), two trigger finger releases, a tendon and muscle repair of the forearm, a carpal tunnel release, and a scaphoid fracture repair.
An important detail about the OR is that the entire floor is sterile. To walk around you have to wear scrubs that you get from a vending-machine by swiping your iCard. At the end of the day, you return your scrubs by depositing them in a different but similar machine. Before leaving the locker room, we put on shoe caps and a hair net. Before entering any of the actual operating rooms, we cleanse our hands with hand sanitizer and put on a face mask. Some of the face masks have a plastic shield attached to it to protect our eyes from any blood that may squirt out.
Anyways, back to the prompt. Last Thursday, in the OR, we watched a revision surgery of a left hip implant.
Revision surgery is an operation that corrects for the failure of a previous implant. Failure can occur from infection, (recurrent) dislocation, fracture, wear, loosening, and negative metal reactions. Going under the knife (again) will always have risks involved: infection, heart problems, blood clots, kidney failure, ect. The operation is not only costly to patients but also to the hospital. In an article from 2003 stated that, on average, the hospital loses over $5,000 per revision surgery. And to the patient, the process can be time consuming, as it could take months for a patient to recover and return to work.
Last week, a resident explained to a patient why an implant can fail. The factors are:
1) Surgical Skill/Implant Used – Which are factors that are controlled by surgeons and the hospital, by individuals other than the patient
2) Patient’s Post-Op Behavior – Is the patient following the physicians recommendations? (Like going to physical therapy) These are factors based on the decisions of the patient.
3) Genetics – These are factors that are not controlled, the surgery could have been perfect, the patient could be doing everything they’re supposed to, but they still do not recover. The resident said “some bodies don’t like surgery”.
First Needs Statement: Design a better, longer-lasting endoprosthesis and/or develop an improved surgical technique for hip (or joint) replacements.
First off, this would be the most ideal problem to solve be it universally affects all individuals receiving an implant. However, it would also probably be very difficult for us to come up with a feasible solution in the next three weeks.
The first ever hip replacement was in 1940, a proximal femoral replacement with a fixed vitallium head. Since then, there has been dramatic improvements in the design of hip implants. For example in, earlier renditions of hip implants sported metal-on-metal components, which reported having high rates of failure (6.2% within 5 years). The implants were later improved in their design by using metal-on-plastic components instead, decreasing the failure rates (1.7%).
As for surgical techniques, there are multiple approaches to performing a hip replacement. The approaches differ in the way the hip joint is accessed, where the incisions are made and what muscles get cut. Different approaches will correlate to different rates of dislocation, repair of the joint capsule, and healing of certain muscles. Surgeons determine the best approach by evaluating the conditions and body-type of the patient.
There are also different tools used depending on the preference of the surgeon, such as using either bone cement (PMMA) or screws to fixate the acetabulum cup.
Second Needs Statement: Remind and motivate patients to practice healthy behaviors (before and) after total joint replacement surgeries.
Activities include: attending physical therapy, quitting smoking, keeping the wound dry, sticking to a diet, and performing light exercises daily
This needs statement is probably the most feasible one for us to tackle. An idea that comes to mind is a smartphone app that gives off frequent notifications reminding and motivating individuals to follow their physicians advice. If we do go for this needs statement, then we may need to read up on post-surgery practices and obstacles, as well as how to make a smart phone app, with of course, a user-friendly interface.
Third Needs Statement: Find a better way to screen out patients who are likely to not (or have difficulty to) recover from a hip-replacement surgery.
This is probably the most vague and difficult needs statement to follow. It only applies to individuals whose bodies don’t recover well after surgery. Surgeons already currently evaluate patients to see if they are healthy enough for surgery using diagnostic tests like X-rays, MRIs, EKGs, and blood and urine tests. I guess a more concrete evaluation is to analyze the patient’s DNA to determine if they have the genes necessary for recovery. One article from 2016 states that the MG53 protein has been found to help wound healing and decrease the recovery time following surgery. I’m not sure if we could realistically use this information in this internship, but perhaps in the future, gene expression and protein production may play a bigger role in orthopeadic implantation.
Overall, I predict we will focus on something more on the lines of the second needs statement, but either way, I look forward to next week’s workshop and visit to the exciting OR.
Week 4 – Time To Get Physical (Therapy) – (7/16 – 7/20)
Michael Lukas Blog

This week, we were tasked to identify criteria and specifications for our project. On Monday, we decided that physical and occupational therapy might be a good place to search for project ideas, so this week, we visited and observed the routines of two different physical therapy clinics.
The first clinic we visited was at IBJI. The occupational therapist (OT) we observed was meeting with post-op patients with various hand related injuries. There was an interesting machine called “fluidotherapy” that uses flowing hot air to massage the hand as the patient performs hand exercises. The OT also used other devices to work on wrist/hand control, flexibility, and strength. One was a “PowerWeb” that the patient pushes into as hard as they can for ten seconds, another was a washer on a metal 3D maze that exercises the wrist, and there was a clip-based activity where patients use their thumb, index, and middle finger to open plastic cloth clips onto a thin pole.
At the clinic at UI Health, we were able to observe another OT. This clinic used different devices. They used putty that the patient molds for a few minutes, it used a ball with a gyroscope to increase wrist strength, one exercise had the patient rotate a tennis ball around the edge of an upside-down frisbee to work on wrist control, and they used a clamp to pick up wooden kegs from a board and place them back. There are a lot of instruments used in OT, but there is definitely room for improvement.
Some of the specifications we identified was: safety, effectiveness, cost, intuitiveness, motivation. All of these specifications should be accounted for when designing a new OT device.
Week 5 – Still Alive (7/23 – 7/27)
Michael Lukas Blog
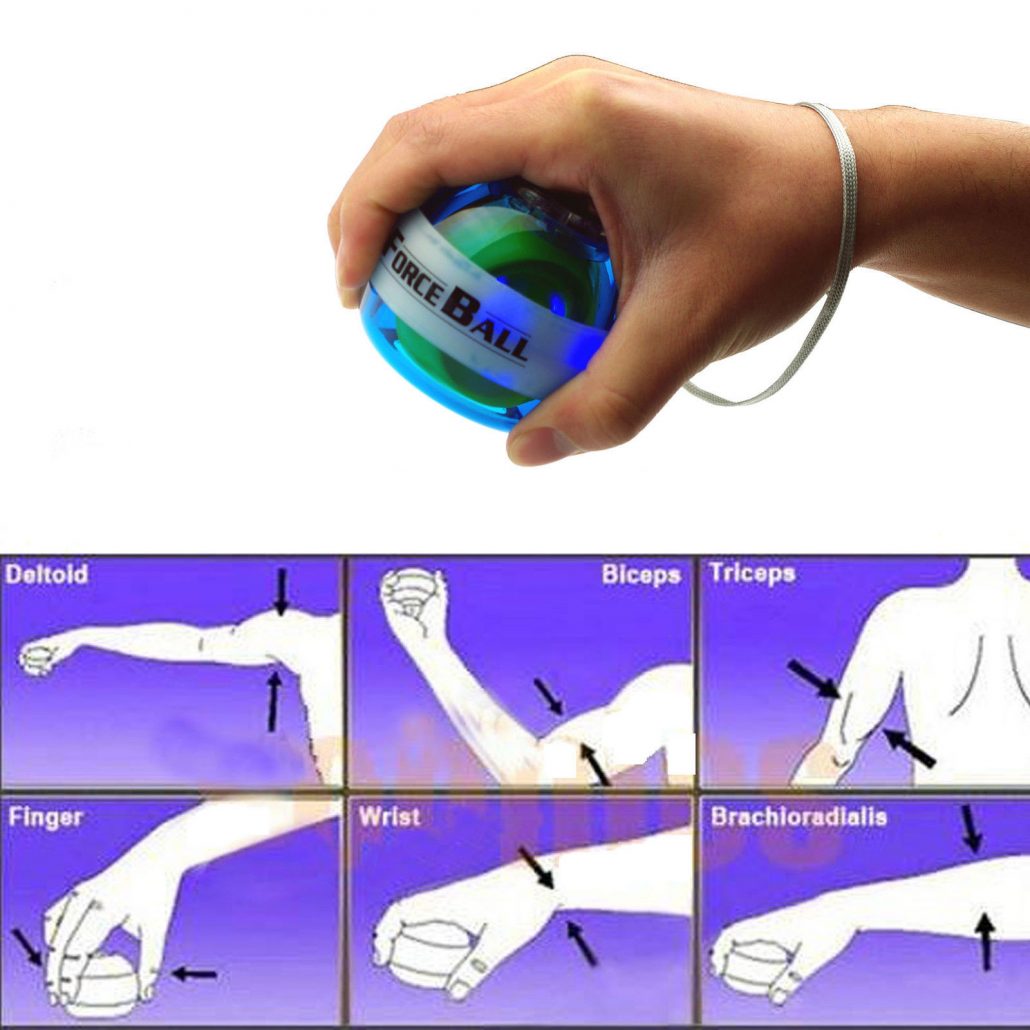
On Monday, we decided to pursue the design of a self-starting, handheld, gyroscopic ball that would be used to strengthen the wrist in occupational therapy. Currently, gyroscopic balls are baseball sized hollow plastic spheres that contain a gyroscope on the inside. When a gyroscope spins, it resists lateral motion. Users build wrist strength by rotating their wrists with the ball in hand while the gyroscope is spinning. However, most gyroscopic balls require the user to either quickly pull a string or wind the gyroscope back and slingshot it (autostart) to get the gyroscope spinning. The string is wound across the gyroscope much like a yo-yo. It was clear in our observations that the start-up process of the ball requires a lot of dexterity and control of the hands, something that occupational therapy (OT) patients may not have. So to make the ball more practical for OT patients, we propose designing an electrically motorized gyroscope that can be controlled with simple pushes of some buttons. This design would make it easier for patients to utilize the weight-bearing strength exercises without the difficulty of winding a string, pinching the string, and pulling quickly. The is also room for enhancements and features, such as the ball reading the speed and resistive force on a small LED screen, or having the ball vibrate every time an OT patient is supposed to perform their hand exercises.
During the rest of the week, we were able to observe more pre and post-op patients at the IBJI and UI Health clinics. Therapy is a conservative treatment for many joint problems. But health insurance companies also require that it be trialed for a few weeks before they agree to a surgery. Only after the patient shows no improvement after conservative treatments will the insurance subsidize an operation. There was one patient with severe hand pain an strongly believed therapy wasn’t going to help. Regardless, she still had to try OT before she could undergo surgery. Other conservative treatments include anti-inflammatory medications and cortisone injections.
In the OR this week, we observed four procedures. Two left TKAs, a right knee antibiotic spacer exchange, and a right patellar tendon reconstruction with an Achilles allograft. In the first TKA, the vendor brought endoprosthetic components that were larger than Dr. Gonzalez’s preference. To adjust for the setback, Dr. Gonzalez had to sacrifice some of the bone cement to make the acetabular cup fit. Overall though, the rest of the operation went smoothly. In the second TKA, I noticed the sutures used differ in thickness and function. Some sutures have antibiotic properties. All the sutures though are sterilized and packaged. The outside of the package is not sterile, so a nurse has to open the package while the surgical tech grabs the wound up suture. There are also other packaged tools that a nurse has to open for the surgical technician. The surgical tech is responsible for counting the number of suture needles and gauze used to make sure nothing is left in the patient’s before closing the incision. The third operation was intended to be a revision implantation surgery following an infection. However, the infection did not go away after the previous antibiotic spacer, so the old one was removed and a new one was implanted. An antibiotic spacer is made up of bone cement loaded with antibiotics and shaped like a prosthesis. It is a temporary implant because it is not meant to bear loading and can wear. Antibiotic spacers are typically used for 6-8 weeks before replacing them with metal and plastic prosthetics. The final operation was a new one for me. The patient tore his patellar tendon, which is actually a ligament that connects the patella to the tibia. The patellar tendon was reconstructed using the Achilles tendon of a cadaver (allograft). The resident surgeon drilled three holes into the graft and patellar tendon and sutured them together. After suturing them together, the surgeon flexed the knee with his arms to measure the function of the newly grafted tendon. It performed well. The wound was closed and the patient was taken to recovery.
Week 6 – Final Post (7/30 – 8/3)
Michael Lukas Blog

This is the final week of CIP. It was a pleasure working with Rown and Dr. Gonzalez. On Monday we worked on our presentation and report. Tuesday was our last day at IBJI. We asked OT how she felt about our project idea. She said she liked it. On Thursday we exchanged farewells with the med students, residents, and Dr. Gonzalez. It was a real honor to be a part of this immersive program.