
Anooshay Aamir
Student Participant
About
Introduction: I am a 4th-year undergraduate student, majoring in biomedical engineering with a concentration in neural engineering
Area of Research: Division of Cardiology | Department of Medicine | Heart Center University of Illinois
Mentor: Dr. Erik Wissner, Director of Cardiac Electrophysiology at UI Health
Contact: aaamir3@uic.edu
Week 1: Welcome to a week in the life of a BME intern!

This week was extremely exciting! We met with Dr. Erik Wissner, Director of Cardiac Electrophysiology at UI Health, who introduced us to the rest of the Cardiology department. On our first day at the clinic, we saw many patients and later in the week transitioned into different divisions of cardiology such as the echo lab, the electrophysiology lab, and the cath lab. I was able to experience the operation room where we observed surgeries such as a transesophageal echocardiogram (TEE), angiographies, thrombectomies, and ablations. Here are some of the designs we saw this week!
Good Design: Cryoballoon Ablation
Patients who have symptomatic paroxysmal atrial fibrillation and are unresponsive to medication need an alternative therapy. In comparison to antiarrhythmic drug therapy, catheter ablations such as cryoballoon are more effective in maintaining sinus rhythm.
At the clinic, we met a patient who will be going through this minimally invasive surgery soon. The cryoballoon procedure takes place in three steps. First, to reach the heart, a small incision in the groin area is made to insert the catheter. Next, the physician goes through thin tissue that separates the left and right side of the heart to reach the pulmonary veins with the cryoballoon. Second, the balloon is inflated and moved to the opening of the pulmonary vein. The purpose of this technique is to maintain contact with the opening of the pulmonary vein so the balloon is able to reach a colder temperature. Finally, when the cryoballoon is in position, the tissue is frozen, creating a scar where the balloon touches the opening of the pulmonary vein. This line of scar tissue stops the transmission of electrical signals that cause atrial fibrillation.
This surgery is not only safe but also effective such that the patient is least likely to need a repeated ablation or be hospitalized after the ablation due to complications. Furthermore, it helps eliminate the daily symptoms that the patient feels such as fatigue, sudden chest discomfort, and difficulty breathing.
Bad Design: Exercise Stress Test
The goal of the exercise stress test is to see how well a patient responds to their heart working at its maximum potential. The patient is instructed to walk on a treadmill where the speed is increased every three minutes. The electrical activity of the heart is recorded through an electrocardiogram. The ECG records the heart rate and rhythm, as well as the strength and timing of electrical signals as they pass through each part of the heart during rest and exercise.
This test has multiple flaws. After the patient has concluded their walk on the treadmill, the sonographer has under one minute to take images of the heart. The patient not only goes from a standing position to laying down on their bed but also has to do a 180 degree shift of their body so that the sonographer can access their chest. There are many different wires that are attached to the patient’s body that hinder their capability to move so fast. However, due to the sensitivity in time, the technician and the sonographer shifted the patient rapidly. This created visible stress and anxiety for the patient. In addition, due to heavy breathing after exercise and the sudden movement, there is a possibility for the images to be inconclusive.
After observing this procedure, we interviewed the technician to see how often there are errors during the ultrasound. She mentioned that if the images are unclear or harder to make conclusions with the physician requests for another test. Depending on the availability of the patient as well as the hospital, this can delay the diagnosis of the patient which may be detrimental to their health.
Week 2: Are you ready for a story time?
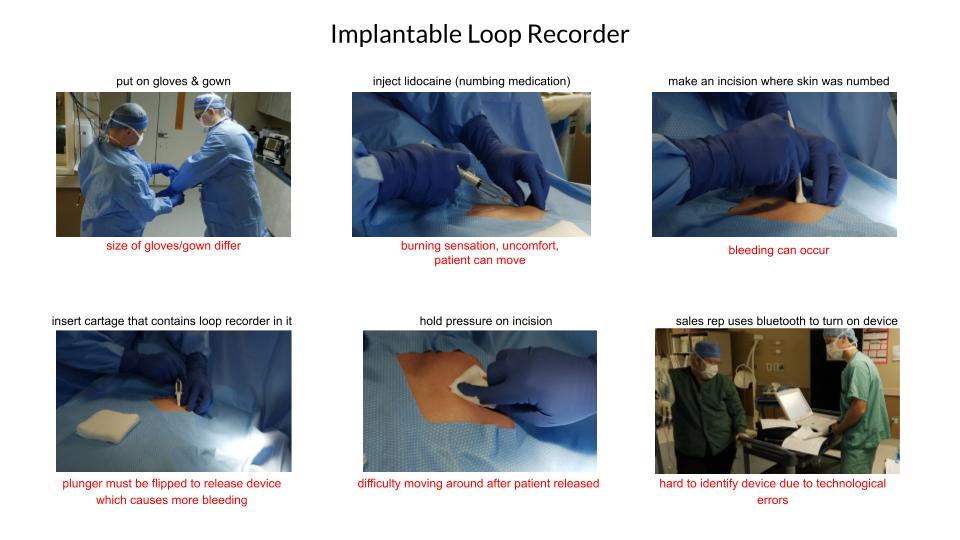
This week was all about getting comfortable! Now that we know our way around the cardiology department, it’s been fun to move around different divisions when a procedure is occurring. A simple procedure such an implantable loop recorder was fascinating. I created a storyboard to walk you all through each step. I also identified some problems that arise. Each step is listed in black and corresponds to some pain points in red.
Implantable loop recorders (ILR) are cardiac monitors placed under the skin of the chest purposed to monitor the heartbeat while daily activities are performed. This implantation takes place due to an abnormal heartbeat or an unexplained stroke or syncope. The device proves to be beneficial for diagnostic timing and follow up strategies for potential interventions.
The first ILR was produced in the 1990 known as BioMonitor 2 developed in Berlin, Germany. The advantage of this device lays in its memory management which is based on a SMART algorithm allowing for the storage of the first, longest, and the last episode of every arrhythmia. The second ILR was produced by Medtronic known as Reveal LINQ and has a weight of 2.5 g. It is the smallest ILR out of the four and has a duration of three years. The third was Reveal XT which was launched in the market first and had a separation between automatic recordings and activated patients. The last ILR is the Confirm Rx launched by St. Jude Medical which has a remote monitoring connected to a smartphone app.
The clinical application of this device is mainly for transient loss of consciousness, among others. However, even though ILR’s have such advantages, this study describes that they are underutilized in clinical practice. Sophisticated algorithms can detect atrial fibrillation episodes, but physicians are not using this device to see the possible effects on patient antiarrhythmic and those who need anticoagulant therapy management as much as they could. Therefore, a limitation present is the need to have further studies that identify all the potentialities of the tool to increase the use of ILR. A detailed evaluation, past medical history, and a diagnostic procedure tailored to the patient will not be replicable to an ILR, however, it may be an additional data point to evaluate a patient and justify possible interventions.
After seeing a live procedure of the implantable loop recorder as well as talking to the sales representative, it was valuable seeing how much technology has advanced. At one point, patients had to come in weekly or even daily so that doctors could monitor their heart. This device has truly changed the magnitude of data that can be collected when the patient is not in the hospital. It would be cool to improve this device further to maximize it’s potential for both patient and physician needs!
Check out the review article for more info: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6373656/
Watch the procedure live: https://www.youtube.com/watch?v=E_jYMuw_05A
Week 3: Where I saw a chaotic surgery
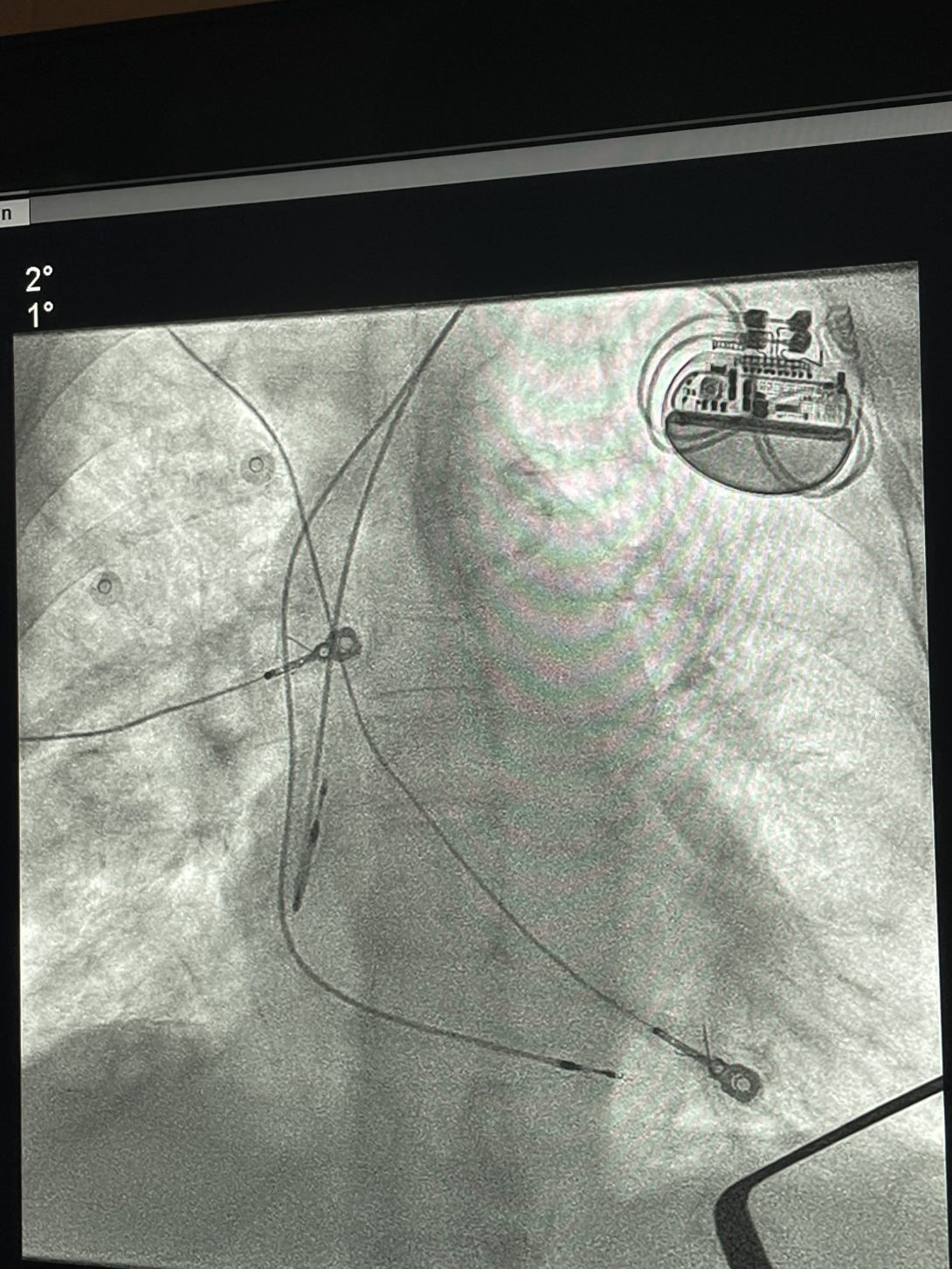
What started off as a regular pacemaker placement procedure turned into a long and eventful day. This week we saw many new procedures, among one was a pacemaker implant. Usually, these procedures take about thirty minutes to an hour. However, things did not go as planned. When the aged patient had other severe conditions such as COPD and came in unstable, it was tough for the anesthesiologists to make decisions regarding sedation. At one point of the surgery, everyone was instructed to leave the room and the surgery had to restart. It was chaotic, stressful, and a bit nerve-wrecking to be standing in the room while the nurses, doctors, and technicians worked together to bring the patient comfort.
This scenario got me thinking more about pacemakers. The surgery was successful but this week focus was identifying needs in Cardiology. Depending on how well the pacemaker works for the patient, they’ll come back in about 6-10 years to replace the battery. A pacemaker has two components. The first part is the pulse generator which houses a battery and controls the electrical signals sent to the heart. The second part are the leads (electrodes) that are placed in one or more chambers to adjust the heart rate. While these electrodes remain in your heart, the battery must be replaced. The replacement may cause infection related complications that can be detrimental to the patient’s overall health.
Iteration 1: Cardiologists treating patients with pacemakers who need a replacement of battery need to identify a method to decrease infection related complications during replacement surgery
- Population: Cardiologists treating patients with pacemakers who need a replacement of battery
- Opportunity: Reduce additional surgeries post implant or increase battery life of pacemaker to more than 10 years
- Outcome: Decrease infection related complications
This iteration was the first thing that came to mind. However, it has some flaws. The population is too broad, perhaps, it should focus specifically on electrophysiologists since they do pacemaker implants. In addition, the scope of this scenario is extremely high. The opportunity is unrealistic since this is a need that has been present for many years. However, this need statement was a good way to practice how to identify problems present in the field. This problem is extremely serious in the cardiology field as one of the literatures mentioned that a patient underwent pacemaker replacement seven times in thirty-three years due to battery exhaustion or inadequacy.
Iteration 2: Electrophysiologists replacing pacemaker battery need to identify a method to decrease infection related complications such as endocarditis.
- Population: Electrophysiologists replacing pacemaker battery
- Opportunity: Identifying a method
- Outcome: Decrease infection related complications such as endocarditis
This iteration is an improved version of the first iteration. The population is more specific since electrophysiologists are the only ones treating pacemaker patients. The outcome also becomes specific through an example. However, endocarditis is not the only infection related complication. Pneumonia, sepsis, and other types of infections also include the list. Lastly, the opportunity remains extremely broad. A “method” is too broad of a solution.
Iteration 3: Electrophysiologists replacing pacemaker battery need to identify pre-infection symptoms that reduce infection related complications post replacement surgery.
- Population: Electrophysiologists replacing pacemaker battery
- Opportunity: Identify pre-infection symptoms
- Outcome: Reduce infection related complications post replacement surgery
The method is not too specific in this case since a need statement should not be solution based. It’s hard as an engineer not to think of solutions when identifying problems. The first thing that came to mind is introducing wireless chargers for the pacemakers to avoid getting a replacement surgery. However, most of the literature suggests that even an iPhone can cause magnetic interference when placed very close to implantable cardiac devices from some brands. This perhaps becomes a conflict of interest when thinking about inventing a wireless battery for the pacemaker. An argument can be made that the scope of this iteration is too broad, however, a larger scope also opens a better understanding of what is present in the literature today and can create a model for what needs to be targeted.
Week 4: When fluoro became a problem for my back
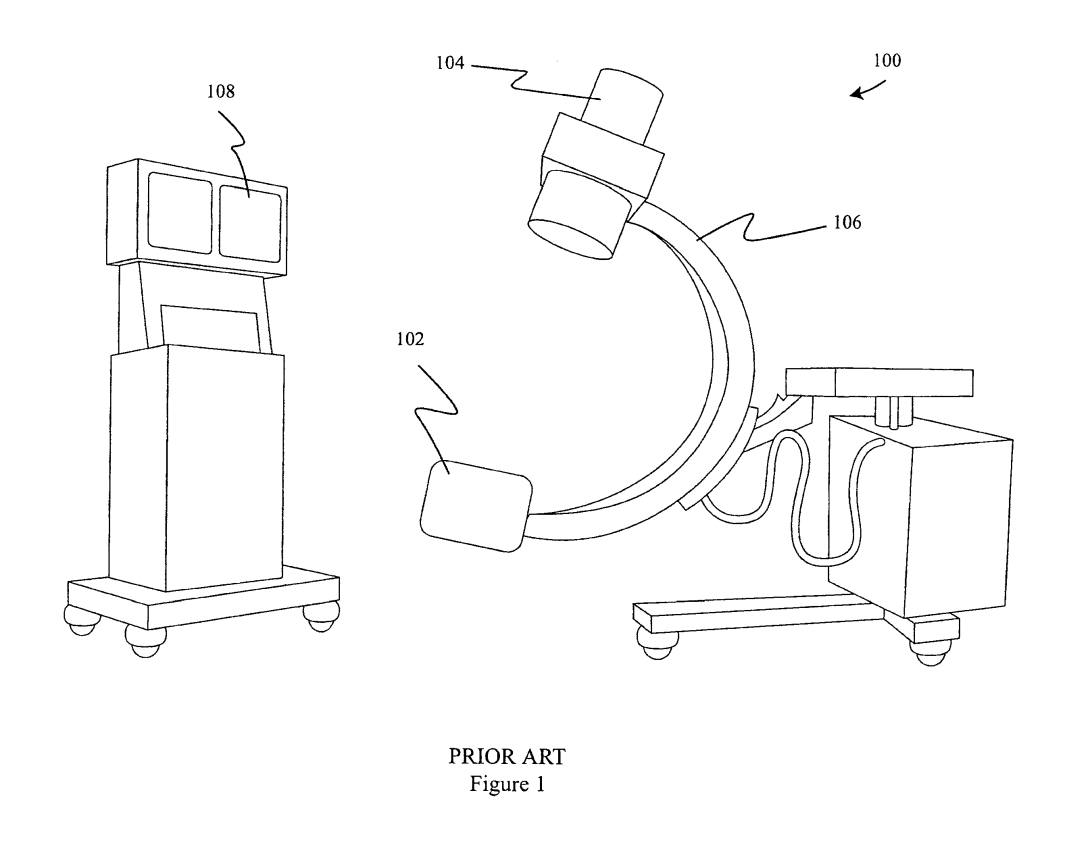
We tied up loose ends this week by rewatching procedures to establish a better understanding such as the Atrial Fibrillation Ablation with Cryoballoon. We also saw interventions such as a pacemaker replacement, a stent placement, and a bypass study. All of these procedures had one thing in common: radiation. Cardiology uses fluoroscopy in all, if not most, of their procedures. Fluoroscopy is a real time x-ray imaging technique used as a medical diagnostic tool to collect information regarding the movement or functionality of the organs. Since most of the procedures are catheter-based interventions, there has been an increase in the use of fluoroscopy. This invention is amazing; however, it poses threat to the patient and the physician due to the radiation.
X-ray can be described in two ways: beam and scattered. X-ray beam occurs when the physicians’ hand or body part is placed direct under the x-ray while the fluoroscope is operating. X-ray scattering occurs when electrons in the patients’ tissue strike and deflect back to the sides at angles that are not parallel to the incident beam. The intensity of scattered x-ray is lower, however, can be harmful after accumulated for months and years of exposure. A radiation apron or lead is worn by all personnel present in the operation room when fluoroscopy is operation. For the past four weeks, we’ve stood in our lead aprons for hours during a procedure. These aprons are heavy and uncomfortable. They result into fatigue and back pain. Also, the apron only protects some body parts such as the chest, leg, and neck. It’s desirable to create a complete radiation protective device that eliminates heavy radiation protection garment in addition to protecting all parts of the body such as the hands and arms.
A patent has been created for such device that attaches to the C-arm of a fluoroscope, shielding and collimating the X-ray beam between the X-ray source and the patient and between the patient and the image intensifier. This protects the operator from inadvertently being exposed directly from the X-ray beam and eliminates a significant number of scattered X-rays. I thought it was interesting that this protective device also comes with a blanket-like radiation shield that covers he patient in the area surrounding where the X-ray beam enters the body. It also has a feature to be connected to the C-arm. In addition, it would be interesting to develop a controller that calculates the proper distance that is shielded from each angle of position. This may be part of the design, but the patent is not opposed to distance sensors. A comparison on which feature would be more accurate and beneficial should be conducted prior to the final product. There is a mention of using computer algorithms to determine the distance and angulation of the radiation shield. Through my observations in the operation room, this would require an additional technical staff which would make the workflow less efficient.
There are definitely limitations to this design given that it introduces another equipment in a room filled with multiple others. However, it is valuable to the overall experience of being in the room since it provides safety efficiently.
Week 5: Run to the finale!

While deciding between our final project, we thought of two things: passion & scope. In the last five weeks, we have encountered many needs. During our first week at the clinic, we ran into a patient who had irregular heartbeat. Since then, the word ablation has come up every week.
A cardiac ablation is described as the scarring of tissue in the heart to block irregular electrical signals. There are two methods of ablation to treat atrial fibrillation: burn or freeze.
The cryoballoon ablation is fascinating as it completes the ablation in four freezes in comparison to the radio frequency catheter that takes hours to complete. During this procedure, the physician freezes the tissue surrounding the pulmonary vein. It seems super simple. However, after seeing this procedure, it was hard to believe that something as small as a balloon could do so much to repair an irregular heartbeat.
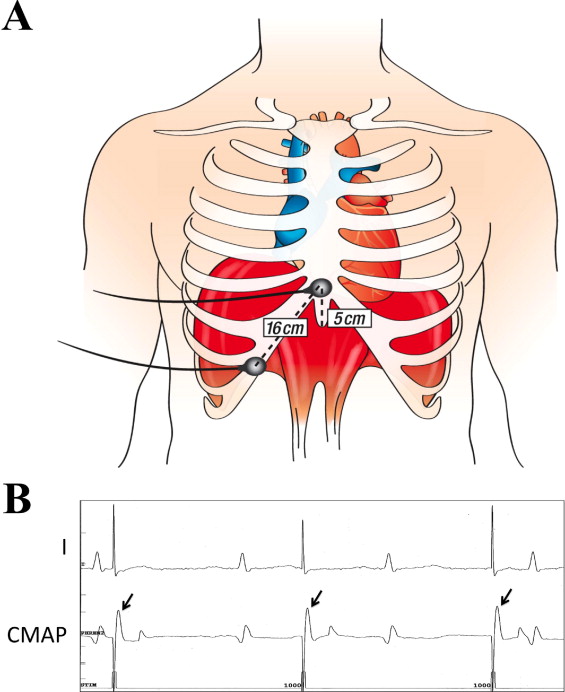
After the freeze, the physician mimicked what happened inside of the body to us. While the balloon was expanding, a thick layer of ice surrounded it. This demonstration was valuable but unrealistic as it eliminated all the complications that occur inside the body. While rethinking about the procedure, I thought about the parts of the procedure where the physician was unable to talk to us because he had to solely focus on the movement of the patient’s hiccups. You must be thinking, why hiccups? During the ablation, when it was time to ablate the left side of the heart, there came danger to the phrenic nerve.
The phrenic nerve originates from the spinal nerves in the neck and is important for breathing since it provides motor control of the diaphragm. It lies near the area of the ablation and damages to the phrenic nerve can cause shortness of breath in patient for up to a year. A method to assess the functionality of the phrenic nerve and prevent damage is to pace the phrenic nerve to stimulate the diaphragm, hence the hiccups! When the hiccups faint or completely stop, there is damage to the phrenic nerve.
Let’s think of an analogy. You’re at the intersection of Michigan Avenue and State Street. The hiccups are when the light turns orange and you’re confused if you should speed up or stop. If you speed up, there is a potential risk for an accident due to the traffic from the opposite side. If you stop and the person behind you fails to stop, you may find yourself in a rear-end collision. The hiccups do not provide a prevention of the damage, they simply act as a warning sign. Ideally, you’d want to prevent the damage of the phrenic nerve through a method that acts as a green light when it’s safe to continue ablating without the risk of any damage. Another method to eliminate the damage is placing an EKG electrode over the diaphragm to indirectly measure the phrenic nerve function. However, this is yet another example of an orange light. The dislodging of the catheter could be a reason for losing an EKG signal. Stopping the ablation due to a false alarm could be cumbersome for everyone involved and would make the procedure less efficient. Therefore, a green light solution must be generated.
While diving deeper into this issue, I found that about 75,000 cardiac ablations occur in a year and that 1.1% – 6.6% of those result into phrenic nerve injuries. Although there is no specific product involved as the EKG is a diagnostic tool used for many other procedures, the total cost of an EKG machine is approximately $1000. Through this information, I was able to calculate the total addressable market which is the # of units/ year multiplied by the cost of product. In our case, the # of units/year are the number of ablation patients per year and the cost of product is per use.
Here are the final measures:
# of impacted lives = 75,000
# of units/year = 825 – 4950 (based off of 1.1% – 6.6%)
Cost of product = $1000
TAM = $825,000 – $7,950,000
Week 6: The final proposal
Where time went is an overwhelming thought but where we are now is a product of the last six weeks. I present to you my final proposal!
Atrial fibrillation is characterized by rapid, irregular beats from the atria (>400/min). Think of it like a choir: the singers lose synchronization with the pianist. The atria and ventricles are our singers and pianists. This abnormal heart rhythm arises from the pulmonary veins. The best noninvasive therapy consists of an inflatable balloon inserted through a catheter known as a cryoballoon. As described last week, a cryoballoon ablation freezes tissue surrounding the pulmonary veins to break aberrant electrical signals causing irregular atrial beats. Although this method is successful, about 4.2% of patients have damage to their phrenic nerve due to the proximity of the cold front from the ablation.
The phrenic nerve controls the diaphragm which is the large dome-shaped muscle between the abdomen and chest. This is valuable to our breathing and injuries cause shortness of breath, recurrent pneumonia, difficulty weaning from mechanical ventilation, and other symptoms.
Through our observations and secondary research, we were able to identify a need. Electrophysiologists who perform cryoballoon ablation for atrial fibrillation need to avoid damage to the phrenic nerve to reduce incidence of postoperative dyspnea.
The phrenic nerve is monitored during the ablation by fluoroscopy, pacing of the diaphragm, and common monitoring program (CMAP) through an EKG. The phrenic nerve pacing induces diaphragm contraction which leads to hiccups. This movement can be seen on fluoroscopy as well as underneath the patient sheet. The pacing is done through a diagnostic catheter in the superior vena cava. This catheter can be provided by many companies such as Stryker. In addition, the CMAP is a supplemental method that is recorded with surface electrodes. The signals are assessed in case of phrenic nerve threat. A progressive amplitude drop >30% indicates phrenic nerve damage. Although these solutions exist, they are extremely limiting. For instance, the hiccup method is not reliable since a stop in hiccup is a confirmed damage. There is no way to see a “decrease” in hiccups since they stop abruptly. Furthermore, the fluoroscopy shows the movement of the patient hiccuping. There is no indication that the patient is about to stop hiccuping. The most reliable way of preventing damage is through the CMAP. However, a loss of signal does not necessarily mean that the ablation is close to the phrenic nerve. Due to the difference in anatomy of patients, a catheter displacement is a possible reason behind a decrease in signal. Therefore, if a physician stops the ablation due to a false signal, restarting the process could lead to additional usage of the EP lab as well as time of the physician and staff that could be allocated elsewhere.
The success of this proposal depends largely on the market summary and landscape. The market analysis identifies the number of impacted lives and the competitiveness. As part of viability, the total addressable market (TAM) is calculated which is defined as the maximum size of opportunity for a particular product or solution. This estimate is valuable for the validation of our need and a critical part of substantiating a project as worth continuing longitudinally. According to the FIRE and ICE study, more than 250,000 patients in more than 50 countries worldwide have been treated with cryoballoon. This serves as the number of patients who have a possibility for getting phrenic nerve injury. Although the incidence rate of phrenic nerve injuries is 4.2%, it is important to consider all the major stakeholders. The second part of the TAM consists of the total cost of the product. In this case, there is no specific product being targeted, however, many additional services are utilized. The service cost of EKG is estimated to be $1500 per patient. The total addressable market accounts for 250,000 patients multiplied by the total cost of $1500 which is 375 million dollars. In comparison to a coronary sinus catheter used to pace the patient, the CMAP monitoring is more expensive. However, it is also a better measure of the injury. There is a gap between these two processes since pacing is less efficient and less expensive whereas the CMAP monitoring is more efficient and more expensive. The needs statement can be fulfilled by a more efficient system that detects the distance of the ablation from the phrenic nerve. This would increase both the efficiency and the cost. Due to the magnitude of the total addressable market, this need is extremely valuable and worth the cost.
As our physician described, if the phrenic nerve was not close to the ablation site or if we created a potential solution to avoid the nerve, he could “sip an espresso” while he ablates. Today’s research and technology only monitors the phrenic nerve. There are no reliable preventative techniques for its damage. Our group will be creating a prototype in a form of sensor that detects the proximity of the phrenic nerve to the ablation site.
Other potential projects that we saw during our time in Cardiology was air bubble embolization during cardiac catheterization. Moreover, we saw the difficulty that shorter physicians had accessing the left radial artery during these procedures. Something we felt for six weeks on our backs was lead aprons that were important for protection from fluoroscopy but led to a lot of back pain. It would be interesting for other groups to take on these projects.
I’d like to sincerely express gratitude to my mentor, Dr. Erik Wissner, for his guidance during immersion. We would be unable to experience Cardiology without his flexibility and willingness to hear our crazy solutions. A huge shoutout to the staff of the Electrophysiology and Cath lab for being welcoming and letting us explore the different procedures. We also appreciate the fellows, attendings, and medical students who were a part of our learning experience. Lastly, thank you to Dr. Browne and Dr. Felder for choosing me to experience immersion. This internship has introduced a new perspective of engineering and I could not be more thankful.