
Michelle Alemu
2023 students
Email:
Week 1: Welcome to Urology!
Good Design – Cystoscope
Activities:
The flexible, single-use cystoscope allowed the physician to observe the patient’s bladder through a monitor. To do this, the patient’s legs are placed inside stirrups to access the urethra. After wiping the area with iodine, a gel is applied to numb the area, and a solution is applied to fill the bladder. The resident then performs three steps with the cystoscope: moving the scope upward, shifting left and right, and finally inspecting the entrance where the scope has entered the bladder. The procedure took less than 15 minutes, and the patient learned the test results immediately.
Environment:
The cystoscope is utilized in the outpatient clinic due to its flexibility, which allows the patient to be numbed at the urethra.
Interactions:
As the resident begins to use the cystoscope, the procedure details are made clear to the patient to ensure they understand precisely what is happening. The patient is directed to look at the monitor displaying the live camera inside the cystoscopy as the resident completes the procedure.
Objects:
A monitor is beside the patient connected to the cystoscope, and a tray was previously filled with instruments needed for the procedure.
Users:
A resident controls the cystoscope by applying slight pressure to a button to move it up or down. The cystoscope bends when the button is moved up or down. The patient may feel the cystoscope enter the urethra.
Additional points: Single-use cystoscopes avoid the step of cleaning or the potential risk of infection, which could occur with reusable cystoscopes. In 2021, the FDA expressed a concern about “reprocessing urological endoscopes,” which include reusable cystoscopes, due to “infections and contamination issues,” implying that patients receiving the operation using single-use cystoscopes may have fewer concerns (FDA). The single-use cystoscope does not need to be cleaned because it is already sterile.
Bad Design – Cord Covers
Activities:
Cord coverings are a temporary solution for safeguarding healthcare staff from the numerous cables that link medical devices to the wall. The cord cover functions similarly to tape and is applied over many wires during surgery to keep them together. With its vivid orange color, the cord cover may improve staff awareness and potentially prevent falls by grouping the wires together.
Environment:
Cord covers can be found in the operating room (OR) since various medical devices are used within urology procedures, such as the DaVinci surgical robot, which has multiple components.
Interactions:
Often, cord coverings must be removed following surgery, which creates a possibility for employees to get carts caught or trip over the same cables that previously had cord covers before the subsequent surgery. Furthermore, when the tape is put in during the procedure, just a small part of the cable is covered, which suggests individuals may still stumble if they are not paying attention or feel the bump of the wires as they walk on the cable cover.
Objects:
The OR was filled with devices such as the DaVinci surgical robot with its surgical arms, imaging carts, and surgeon console. In addition, anesthesia devices, medical waste containers, and all the wires connecting medical devices to the wall.
Users:
Users would be nurses who repeatedly place these coverings over cords and rip them off after surgeries.
Source:
https://www.fda.gov/news-events/press-announcements/fda-investigating-reports-infections-associated-reprocessed-urological-endoscopes
Week 2: The Story of a Prostate Biopsy
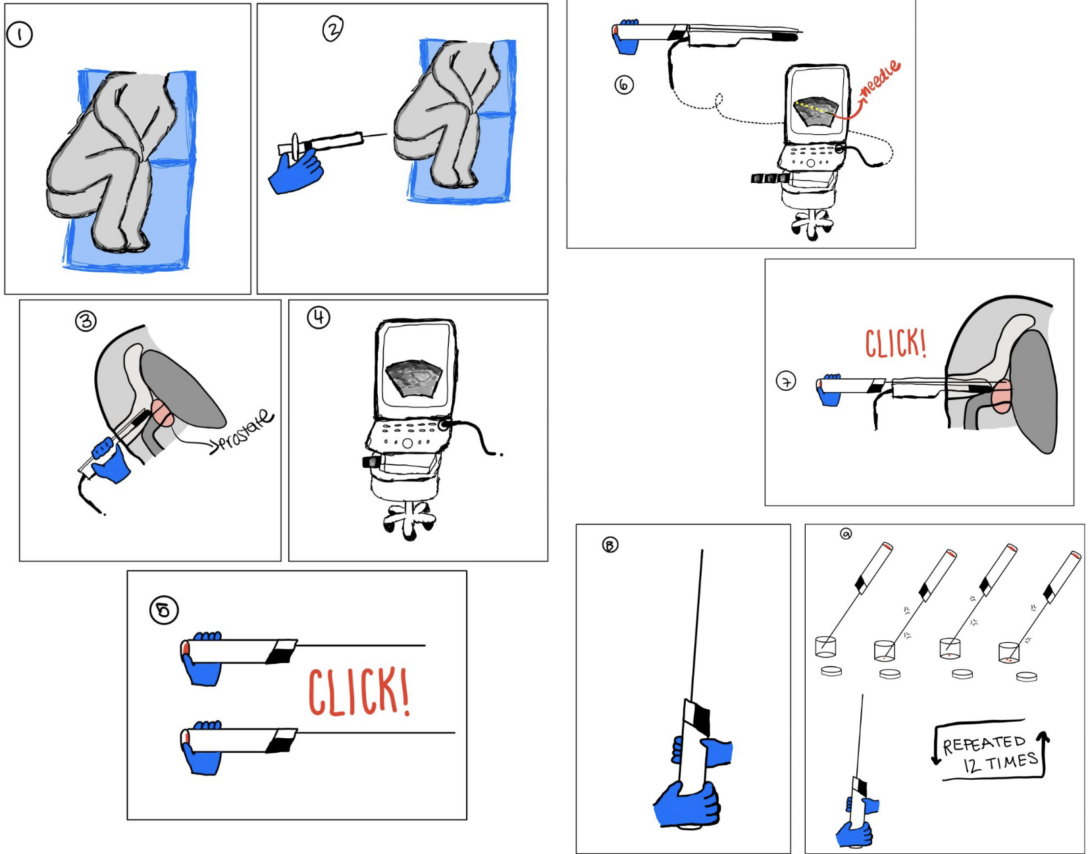
Week 2 consisted of alternating between the clinic and the operating room and witnessing new procedures, such as vasovasostomy, prostate biopsy, and shock wave lithotripsy, that we had not seen the previous week. Because of the numerous steps required during the biopsy, I focused my storyboard on the prostate biopsy procedure.
- The patient is instructed to lie on his side, knees to their chest, with his back facing the resident and ultrasound monitor.
- Pain Points:
- The patient could feel uncomfortable lying on his side instead of hi back during the procedure.
- Pain Points:
- The resident then places numbing gel using a needle into the patient’s anus.
- Pain Points:
- The patient might feel discomfort when the gel is placed.
- Pain Points:
- The resident inserts an ultrasound probe into the rectum with a lubricant gel.
- Pain Points:
- The patient’s fear may increase making it more challenging for them to relax and harder for the resident to place the ultrasound probe.
- Pain Points:
- An ultrasound monitor was used to take photos of the prostate, and the resident placed numbing medication on the prostate.
- Pain Points:
- The patient could feel uncomfortable as the resident looks for the prostate with the ultrasound probe and administers numbing medication for the prostate.
- Pain Points:
- The resident clicks the needle device to inform the patient of the sound the needle makes when the sample is collected from the prostate.
- Pain Points:
- Patients may become more frightened by hearing the clicking sound and seeing the length of the needle used.
- Pain Points:
- The needle device slides into the ultrasound probe’s guide wire, verifying the patient’s prostate with the ultrasound monitor.
- Pain Points:
- The patient could be worried about the sample collection and the clicking sound from the needle device.
- The patient may have issues staying still because of anxiety about the procedure.
- Pain Points:
- The sample is taken from the prostate when the resident clicks the button on the needle.
- Pain Points:
- The patient can have blood coming out of the rectum, which could drip on the floor when the needle is removed from the guide wire.
- The patient could move during the procedure but must remain still for biopsy collection.
- If the patient is not in the correct position, the resident could have difficulty collecting samples because the needle must align with the ultrasound monitor’s angled line.
- Pain Points:
- The resident hands the needle-like device to the nurse to transfer the sample into a container for testing.
- Pain Point:
- Patients become nervous as they cannot see the procedure and may get worried seeing the needle with the sample.
- Pain Point:
- The nurse taps the needle on the side of the container and then returns the device to the resident, and this procedure is repeated 12 times.
- Pain points:
- If the resident does not aim the needle correctly or the nurse does not get enough of the sample on the needle into the container, the sample will need to be retaken.
- The patient experiences the procedure for longer and is put in an uncomfortable position.
- After the procedure, the patient can get a fever and must go to the emergency room. In addition, the patient could experience blood in the urine.
- If the resident does not aim the needle correctly or the nurse does not get enough of the sample on the needle into the container, the sample will need to be retaken.
- Pain points:
Prostate cancer is a leading cancer among men and requires a biopsy to determine whether a patient has the cancer. Before an individual can receive a biopsy, PSA (“prostatic-specific antigen”), DRE (“abnormal digital rectal exam”), or “clinical suspicion of prostate cancer” can be used as a ticket to get a prostate biopsy. But, these pre-biopsy exams (DRE and PSA) have led to patients receiving “unnecessary biopsies”(Streicher et al., 2019). In contrast, mpMRI (“multi-parametric MRI”) can be used as a critical factor for a patient to get a prostate biopsy, can be used when collecting a biopsy sample, and is a non-invasive exam (Streicher et al., 2019). TRUS (“transrectal ultrasound guided biopsy”) is primarily used as the method for a prostate biopsy, with 6-24 samples taken laterally (Streicher et al., 2019). However, TRUS is not the only prostate sampling method, “targeted prostate biopsy” such as “direct MRI-guided (in-bore) biopsy” and “cognitive fusion biopsy” can use mpMRI to locate “suspicious lesions” in the prostate and could be more successful than the current biopsy method (Streicher et al., 2019). The current prostate biopsy procedure can be significantly improved by implementing the combination of mpMRI and targeted prostate biopsy, which are better at detecting prostate cancer than TRUS.
Source: Streicher, J., Meyerson, B. L., Karivedu, V., & Sidana, A. (2019). A review of optimal prostate biopsy: Indications and techniques. Therapeutic Advances in Urology, 11, 175628721987007. https://doi.org/10.1177/1756287219870074
Week 3: Need Statements
Week 3 primarily focused on observing various clinic and OR procedures using a cystoscope, ureteroscope, and DaVinci surgical robot. This week’s procedures were familiar, so I gained insight into various ways from a fellow, resident, and attending urologist. Although I could distinguish these slight variations, I decided to brainstorm on a need statement related to a problem during a DaVinci procedure. The issue was related to the blood suction being challenging for the surgical assistant to move during robotic surgery. In addition, I learned that this complication was affecting the fellow and the surgeon, who relied on the assistant to move the suction.
Iteration 1: Urology fellows adjusting the suction position during robotic surgery require a new solution for a less tedious and more efficient way to maneuver the suction for the urological surgeon.
- Population: Urology fellows (OR)
- Opportunity: Adjusting the position of the suction
- Outcome: A less tedious and more efficient way to maneuver the suction
In specific instances, the surgeon will ask the urologist fellow or an assistant to move the blood suction for more significant movements, which could be challenging for the surgeon to do alone. In addition, shifting the suction based on the surgeon’s request can be challenging for the fellow and could take time, as the fellow relies on a monitor, not the surgeon’s console. When delving into more research about suction, I found that the surgeon depends on the fellow, as “effective bleeding control requires the surgeon and the surgical assistant to coordinate their actions during the procedure” (Barragan et al., 2022).
Iteration 2:Urologic robotic surgeons require a new method for guiding the blood suction to be more effective when necessary in robotic-assisted surgery and eliminate the need for an assistant.
- Population: Urologic robotic surgeons (OR)
- Opportunity: Guiding the blood suction
- Outcome: be more effective and eliminate the need for an assistant
Ultimately, the population became more focused on the surgeon as they relied on suction to complete the surgery. In addition, the outcome was slightly altered as the need for an assistant can lead to wasted time for the surgeon who needs the suction to be moved in a specific direction.
Iteration 3:Urologic robotic surgeons utilizing a blood suction for robotic-assisted surgery require a new solution to make suctioning easier, more efficient to maneuver, and fully independent.
- Population: Urologic robotic surgeons (OR)
- Opportunity: Utilizing a blood suction for robotic-assisted surgery
- Outcome: Suctioning easier, more efficient to maneuver, and fully independent
The outcome was altered again because it could be more focused. In regards to being fully independent, this indicates that the fellow would not need to play a role in the suction. The suction requires the surgeon to move it by themselves, which can be difficult, so a more accessible and efficient process is critical to making the surgery go smoothly.
Source:
Barragan, J. A., Yang, J., Yu, D., & Wachs, J. P. (2022). A neurotechnological aid for semi-autonomous suction in robotic-assisted surgery. Scientific Reports, 12(1). https://doi.org/10.1038/s41598-022-08063-w
Week 4: Examining Patents
As the week began, I intended to look for new challenges and possibly develop a new need statement. However, after speaking with the urology surgical assistant last week, I reassessed my previous need statement. The highlighted aspects were the assistant’s difficulties moving the suction laterally and the surgeon losing one surgical arm for the suction device. To address these concerns, I decided to update my prior need statement.
Need statement: Urological robotic surgeons who manage blood suction in robotic-assisted surgery want a solution that eliminates mobility concerns with suction in difficult-to-reach places that require an assistant and reduces the number of healthcare workers who hold the instrument.
The need statement has been revised to be more focused and to clarify the outcome, which was lacking the previous week. I decided to learn more about the patent because the ROSI (“Remotely Controlled Suction/Irrigation for Surgery”) was frequently used in the operating room. The ROSI’s intended purpose is to allow the suction to be controlled remotely by the surgeon and adjusted by the surgical arm.
The ROSI device is said to feature a hard tip and a flexible body, allowing for adjustable movement in the surgical environment. The surgeon can operate the device inside the surgery port by holding a stiff suction tip with the surgical arm. The surgeon can operate the rigid/”distal tip” using a “remote controller,” such as a foot pedal. The ROSI is flexible until the tip, and it can suction a variety of fluids.
The ROSI device is designed to be independent for the surgeon, with no need for an assistant; nevertheless, the device does allow the surgeon to move the suction and perform certain functions via the foot pedal. The surgeon still relies on the assistant to direct the suction in practice. For example, the surgeon may encounter difficulties adjusting suction with the surgical robot for more significant moves, forcing the assistant to operate the device outside the surgical port themselves, which is not intended. When the surgeon uses the ROSI as intended, the user loses the capacity to use all three surgical arms, which may disrupt the surgeon’s flow. The outcome of improving device mobility for the user and minimizing healthcare staff must still be met, indicating that there is still a requirement within the operating room.
Douglas, G. (May 13th, 2011). Google Patents – EP2709686A2 – Remotely controlled suction/irrigation for surgery. https://patents.google.com/patent/EP2709686A2/en
Week 5: Total Addressable Market (TAM)
With one more week until our final presentation, we started to narrow down our need statements. After conversing with our mentor and interviewing a fellow, it became more apparent for us to focus on patient positioning during the prostate biopsy. I witnessed this procedure multiple times, but patients repeatedly seemed uncomfortable throughout the procedure. This observation remained the same even with more experienced urologists (attending, fellow, and resident) completing this procedure.
Patients experiencing pain during a prostate biopsy are not new, with various research articles focusing on understanding patient pain points (Nazir, 2014). Researchers have focused on pain from ultrasound probe insertion, biopsy needle pinching the prostate, and comparing patient positioning of lithotomy versus lateral decubitus (Lodeta & Lodeta, 2012; Nazir, 2014; Song & Ko, 2017). Instead of focusing on patient positioning or the biopsy needle, I decided to look at the ultrasound probe used during this process.
Need Statement: Elderly patients undergoing a TRUS (“transrectal ultrasound scan”) prostate biopsy who feel uncomfortable during the procedure need a less painful solution when the ultrasound probe is inserted.
The ultrasound probe is sold separately from the monitor itself, and the device is reusable, suggesting that a clinic would not need to purchase this device repeatedly; instead, use a covering to reuse the device. According to Universal Diagnostic Solutions, the ultrasound probe or “transducers” can last up to “5-7 years” if taken care of properly. Now that we understand the background information for the ultrasound probe, we can examine the TAM (Total Addressable Market) for this device. Every year, 1 million patients receive a prostate biopsy in the US (Schmeusser et al., 2022). Patients are charged $270-$529 with a calculated average TRUS price per use = $400 for using the TRUS system (Laviana et al., 2015; Venderink et al., 2017). Transrectal ultrasonography would account for 19.2% of the average prostate biopsy cost ($2755/$529 = 19.2% = average cost per patient divided by TRUS cost) (Venderink et al., 2017). However, the prostate biopsy cost does vary based on the hospital and location; for example, UI Health charges $9012 (w/o insurance and before discounts), which would be approximately $1732 for using the TRUS ($9012*.192 = $1732). The ultrasound system (TRUS) accounts for the monitor, printer, and ultrasound probe. The ultrasound probe by itself could be estimated to account for ¼ of the total price as the probe is often less expensive than the ultrasound monitor and printer (USC Ultrasound). Based on the following values, the ultrasound probe cost would be estimated at $100 per use.
TAM = individuals impacted yearly * cost of individual product per use = 1 M * [¼ *$400]= 100 M
Sources:
Karen. (2022, May 20). How Much Does an Ultrasound Machine Cost – 11 Factors to Consider. USC Ultrasound. https://www.uscultrasound.com/ultrasound-machine-cost/
Laviana, A. A., Ilg, A. M., Veruttipong, D., Tan, H.-J., Burke, M. A., Niedzwiecki, D. R., Kupelian, P. A., King, C. R., Steinberg, M. L., Kundavaram, C. R., Kamrava, M., Kaplan, A. L., Moriarity, A. K., Hsu, W., Margolis, D. J., Hu, J. C., & Saigal, C. S. (2015). Utilizing time-driven activity-based costing to understand the short- and long-term costs of treating localized, low-risk prostate cancer. Cancer, 122(3), 447–455. https://doi.org/10.1002/cncr.29743
Lodeta, B., & Lodeta, M. (2012). Prostate biopsy in the left lateral Decubitus position is less painful than prostate biopsy in the lithotomy position: A randomized controlled trial. Korean Journal of Urology, 53(2), 87. https://doi.org/10.4111/kju.2012.53.2.87
Nazir, B. (2014). Pain during transrectal ultrasound-guided prostate biopsy and the role of periprostatic nerve block: What radiologists should know. Korean Journal of Radiology, 15(5), 543. https://doi.org/10.3348/kjr.2014.15.5.543
Song, P. H., & Ko, Y. H. (2017). Lateral decubitus position vs. lithotomy position: Which is the best way to minimize patient’s pain perception during transrectal prostate biopsy? International Braz j Urol, 43(3), 462–469. https://doi.org/10.1590/s1677-5538.ibju.2015.0479
Ultrasound Portables. How Long Does A Portable Ultrasound Machine Last? https://www.ultrasoundportables.com/ultrasound-latest-news/how-long-does-a-portable-ultrasound-machine-last
Venderink, W., Govers, T. M., de Rooij, M., Fütterer, J. J., & Sedelaar, J. P. (2017). Cost-effectiveness comparison of imaging-guided prostate biopsy techniques: Systematic transrectal ultrasound, direct in-bore MRI, and image fusion. American Journal of Roentgenology, 208(5), 1058–1063. https://doi.org/10.2214/ajr.16.17322
Week 6: It's a wrap!
We have finally reached the final week of the Clinical Immersion Program. I can not believe that six weeks have passed, and I learned so much about myself and solidified my future ambitions in the medical field. Throughout the past six weeks, I witnessed various urological procedures completed in the outpatient clinic and the operating room (OR) and recognized needs in these different environments with my group.
Within the clinic and the OR, the environment continuously adapted to changes in the daily schedule. Patients may not have arrived at their appointment, or medical equipment may have malfunctioned. Ultimately, I learned to shift my day to cater to these changed plans. When clinic procedures spread throughout the day, we created questions to ask the medical staff (attending urologist, residents, nurses, and fellows) about procedures we had witnessed. Similarly, if we learned that there were no procedures in the clinic, we would head to the operating room for the day. I learned the importance of adapting to unforeseen changes.
As we approached the middle of the program, the procedures in the clinic started to become familiar. Although seeing a procedure multiple times was repetitive, I noticed how various urologists approached it and how these approaches influenced the results. Also, specific needs became more apparent to me. Lastly, I asked for the schedule after Monday workshops so my team could plan the week. Access to the procedures beforehand allowed me to research and understand each step before entering the operating room and clinic. In turn, it would be easier for me to come up with questions during the procedure.
For future CIP students, I advise watching procedures online before heading to the OR, asking for the schedule beforehand, and enjoying the process. Watching surgeries in the operating room for the first time can be nerve-racking, so I recommend reviewing the most common procedures online through YouTube to get a feel of what they will look like in the OR. In addition, make sure to eat a meal and drink water beforehand. Next, request the weekly schedule from the medical staff or the physician you are shadowing at the start of the week. The schedule will allow you to research the procedure beforehand and plan your week appropriately. Finally, this program focuses on looking for needs in a specific medical department, so each day you are in the operating room or clinic, be diligent when writing your notes. Make sure to review your notes from previous weeks. Sometimes you can skip an important detail which may become a need statement later in the program. Six weeks will fly by, so make the most of your time by keeping your eyes open and staying curious.
Acknowledgments:
Thank you to Dr. Anthony Felder, Dr. Micheal Browne, and Dr. Miiri Kotche for helping me and the team stay engaged with content, guiding us each week, and providing critical feedback during our weekly presentations.
Thank you to Dr.Simone Crivellaro, Dr. Micheal Young, Dr. Daniel Garvey, Dr. Rabun Jones, Dr. Luca Morgantini, Dr. Juan Torres-Anguiano, Dr. Julian Pacheco and all the staff at the urology department at UI Health for allowing us to shadow their procedures in the operating room and the clinic, taking the time to answer our questions about different techniques, and advising our group through the program.