
Django Allegretti
2024 students
Neurosurgery
Pronouns: He/Him/His
Email:
Week 1: Complete Immersion (Good vs Bad Designs)
June 24th – June 28th
Complete Immersion
This week was quite a shock to the system to say the least. We began day one with a quick meeting with Dr. Mehta, and then headed straight to the neurosurgery operating rooms (OR). After donning scrubs for the first time, we were led into our first surgery, an anterior lumbar interbody fusion (ALIF). The sights, sounds, and smells of the OR commanded my full attention. We observed several complex surgeries that first day and I gained an immense respect for the skill and professionalism of the entire surgical team. As a former dancer, the scene reminded me of a work of choreography. Everyone was hyperattentive of each other and the task at hand, with the ability to improvise as the situation warranted.
On day two we attended rounds in the neuro intensive care unit (ICU) to start to develop an understanding of preoperative and postoperative challenges related to complex neurosurgery. Afterwards, two of us headed to the special care building (SCB) OR while the rest headed off to observe a series of CT angiograms. In the SCB OR I was able to observe two surgeries involving the insertion and maintenance of neurological nerve stimulators to treat pain. We witnessed a suborbital implantation and were told that this procedure is relatively rare due to few surgeons being willing to perform the operation, and limitations due to insurance approvals.
Throughout the week, our conversations with OR representatives of the various medical technology companies were invaluable to our understanding of the challenges of the surgeries we were witnessing. I spoke with representatives from Medtronic, Globus, Boston Scientific, and Stryker.
Days three and four had all of us back in the neurosurgery OR for the duration. I was able to observe the removal of a tumor on the pineal gland. This surgery required the coordination of the ear nose and throat (ENT) surgical team as well as the neurosurgery team. The ENT was required to control the endoscope, while the neurosurgeon removed as much of the tumor as possible. I was also able to observe more interbody fusions and am starting to gain a better understanding of the details and challenges of the procedure.
I truly understood the meaning of immersion this week. Whereas on day one I was overwhelmed with a sense of trepidation and apprehension, by Thursday I was able to calmy observe, take notes, and ask questions during complex and sometimes high stress procedures. This new state of mind allowed me to identify a good and bad design and evaluate based on the AEIOU user-centered design framework we discussed during the didactic meeting.
Bad Design: Anchor array for the infrared surgical navigation system
Activities: The surgeon is placing screws into the patient’s spine and the imaging technologist is controlling and monitoring the navigation system.
Environment: The IR navigation system is used during spine surgeries where screw placement is required.
Interactions: The surgeon is regularly directing the imaging tech to record a desired location for a screw and to change views of the system.
Objects: The IR system requires a four-pointed anchor array placed on the clamp attached to the patient that allows the navigation system to be overlayed on a reference O arm CT like X-ray. Each tool must also have a four-pointed array and needs to be registered along with the anchor array. The technologist and surgeon monitor screens depicting the tool and screw locations on the anatomical images. The system also requires an IR transceiver that is placed high above the patient’s head.
Users: The surgeons use the system to ensure accurate placement of the screws without the need for constant X-raying. The technologist must control the position of the IR transceiver and monitor the calibration of the system.
While this technology is overall very impressive, it has some limitations. One of which is the possible accidental movement of the anchor array. If the anchor array is moved, then the system believes the position of the body has moved and thus the placement of the screws could be incorrect, a very serious issue. There are many opportunities for the array to be accidentally moved and the only precaution against this is someone in the OR noticing that it has moved. The technologist also has the responsibility of repositioning the IR transceiver and thus is not always able to dedicate their attention to the position of the anchor array.
Good Design: Ceiling mounted arms with electrical outlets
Activities: Many devices require power and need to be plugged into 120 V AC outlets.
Environment: These devices are positioned around the operating table in the OR.
Interactions: Most devices are plugged in during setup by the nursing and tech surgical team, but some devices such as the O arm X-ray scanner may need to be moved in and out of the room and thus needs to be plugged in and unplugged by the X-ray tech.
Objects: The most important objects that judge the quality of the design are the power cables and their path from the device to an outlet.
Users: The users in this case are all of the occupants of the OR. Throughout a procedure the surgeons, nurses, techs, and medtech representatives all need to move around the room and inadvertently interact with the power cords.
The ceiling mounted arms containing power outlets are a good design because they allow outlets to be positioned above the devices that require power. Most importantly this design eliminates the need for cables to lay across the floor becoming a potential tripping hazard, as I witnessed in ORs that lacked this design feature.
Week 2: First Steps Toward Synthesis (Secondary Research)
During this second week in the OR, the shock had fully worn off and I was better able to take in my surroundings. The terminology was sinking in, and the act of observing an open spinal surgery began to feel routine. The ability for human beings to quickly adjust to novel surroundings always fascinates me.
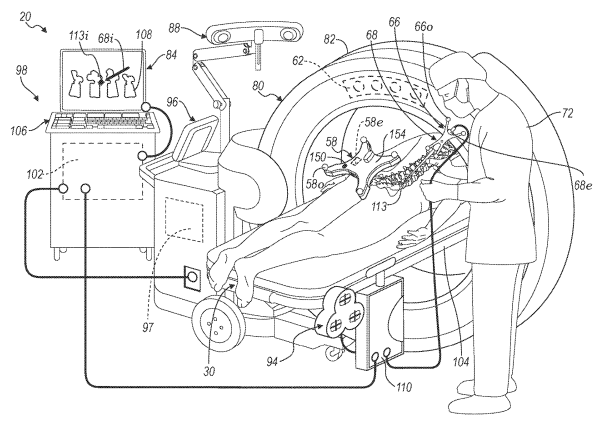
During a posterior spinal instrumentation surgery I was able to spend a significant amount of time learning about the optical surgical navigation system being employed to track pedicle screw placement. The system is called StealthStation and is produced by Medtronic. The system uses an infrared (IR) transceiver and reflective reference arrays mounted to a clamp on the patient, and any tools being used to overlay the position of the tools and pedicle screws on an O-arm x-ray scan. The system’s software allows an accurate estimation of penetration depth of the screws and screwdrivers.
I was able to locate the patent for this device, US 2024/0164846 A1 published on May 23, 2024 [1]. The detailed description of the device gave me a better understanding of the underlying science and engineering principles driving optical surgical navigation.
While this technology is very impressive to me, through observation and speaking with both the technology representatives and surgeons I identified a few potential sources for error. Open surgery is messy and often the reflective reference nodes get covered in blood, so the surgery has to be paused in order to clean them. The surgeons must continually orient the reference arrays connected to the surgical tools or risk the potential misplacement of a screw. Also, the reference array mounted to the patient clamp may inadvertently be moved causing the system to think the body has changed position.
This led me to search for research papers related to sources of error in optical surgical navigation. I found a paper on hidden errors using optical surgical navigation for deep brain stimulation implant surgery [2]. The researchers were able to quantify errors in the accuracy of the system directly related to the orientation angle of the clamp reference array to the IR transceiver. The quantified error was within the acceptable region stated by Medtronic, but they did show that there was significant variation related to orientation angle, and an ideal position of 90 degrees. From my primary research I observed that rarely was this ideal angle achieved. While the error from this source might not be a problem, when combined with the other potential sources of error I described earlier, the total decrease in accuracy could be a major source of miscalculation.
References:
[1] System and Method for Registration Between Coordinate Systems and Navigation of Selected Members, by V. D. Snyder et al. (2024, May 23).Pub. No. US 2024/0164846 A1
[2] Holland, Marshall T., et al. “Hidden Error in Optical Stereotactic Navigation Systems and Strategy to Maximize Accuracy.” Stereotactic and Functional Neurosurgery, vol. 99, no. 5, 2021, pp. 369–76.
Week 3: Searching for Opportunities (Needs Statement Iterations)

This week started with an extended meeting with Dr. Mehta where we discussed our current areas of interest. Although we were all feeling a bit frustrated that we hadn’t found a clear direction, Dr. Mehta explained that it was important that we were still searching and a bit confused. I can see now how jumping to a specific need too early could stunt our ability to remain open minded with several weeks of observation still ahead of us. With this attitude in mind, and our recent lessons during the didactic sessions about forming needs statements, I attempted throughout the week to remain patient and heighten my attention to the smaller details of the goings on in the OR.
I was still interested in the complex systems such as the surgical navigation systems and microscope arrays, but now I was noticing the delays in beginning a procedure because they had to wait on an O-arm to arrive, or a miscommunication about the draping required for a particular procedure. Observing in this vein led me to a significant source of potential danger and time loss, the disorganization of cables and tubing. The tubing required for anesthesia, cables for neurophysiology monitoring, tubing for suction, and large power cables for the myriad devices and their monitors arranged around the operating table can create a nightmare of tangles beneath on the OR floor. I observed an x-ray technician almost fall onto a patient because they tripped on an unseen cable as they were rolling the C-arm toward the bed.
Through secondary research I came to understand that this is a very common problem in ORs around the country and there are many proposed solutions to solve what some researchers call “spaghetti syndrome” [1]. I found several simple solutions such as power banks mounted to devices, ceiling mounted outlets, cable fixing tools attached to devices [2], and plastic sheaths that are taped to the ground. However, in my experience these solutions are rarely implemented due to the inefficacy of their design. Other solutions involve redesigning the OR to have power banks attached to large ceiling mounted arms or designing recesses in the floor of the OR to facilitate cable and tubing organization, however, these solutions are incredibly expensive and not practical. These observations and secondary research led me to develop the population and opportunity for my first needs statement: OR workers need a better method for cable management.
Now for the opportunity, or the “so what?” The CDC reports that slips, trips, and falls (STF) are a significant source of hospital worker injury. STPs are 90% more likely to occur in a hospital setting than in the average workplace, and account for 25% of hospital injuries. While tripping is not the only cause of STPs in a hospital setting, the CDC reports that it is a top 10 reason for STPs. The Bureau of Labor Statistics reported the rate of injury to hospital workers to be 38.2 per 10,000 employees, in 2009, with 50% of these injuries considered “severe” [3]. This research led me to my outcome: to decrease the risk of injury and reduce cost to the hospital.
Combining all three elements of the POO (population, opportunity, outcome) model, I arrived at my first needs statement: OR workers need a better method for cable management to decrease the risk of injury and reduce cost to the hospital. This needs statement comes with a total addressable market (TAM) estimate of $2.608 million per year in the United States. This quantity comes from multiplying the previously mentioned STP rate of 0.382% by 10% of the number of total hospital workers, 6,564,224 in the US, as reported by the Bureau of Labor Statistics in 2019 [4] and estimating that 10% of hospital workers work in the OR. This quantity was multiplied by the average cost of a workplace injury $1,040, as reported by The National Safety Council [5]. This estimate of cost does not account for the effects of employees of the hospital being unable to work.
This TAM was relatively low and could be improved by increasing the scope of my needs statement. By considering that almost all hospital staff may be required to enter an OR at some point, the population could be changed from “OR workers” to “hospital workers”: Hospital workers need a better method for cable management to decrease the risk of injury and reduce cost to the hospital. This increases the TAM estimate to $26.08 per year in the United States.
So far, I have only included “a better method cable management”, but this opportunity is limited and almost provides a solution. If this is changed to simply “need a reduction in tripping hazards” the needs statement becomes: Hospital workers need a reduction in tripping hazards to decrease the risk of injury and reduce cost to the hospital. Now the potential solution space is much larger and accounts for solutions such as wireless technology and battery systems.
References:
[1] Jay Haynes, Kelly Bowers, Richard Young, Trudy Sanders, Karen E. Schultz; Managing
Spaghetti Syndrome in Critical Care With a Novel Device: A Nursing Perspective. Crit Care Nurse 1 December 2015; 35 (6): 38–45.
[2] Azizoglu, Hatice, and Fatma ETİ ASLAN. “Evaluation of the Effectiveness of ‘Cable Fixing Tool’ in Ensuring and Maintaining Patient and Employee Safety in the Operating Room.” Perioperative Care and Operating Room Management, vol. 33, 2023, pp. 100355-
[3] Center for Disease Control: https://www.cdc.gov/niosh/docs/2011-123/default.html (visited July 12, 2024).
[4] Bureau of Labor Statistics: https://www.bls.gov/opub/ted/2020/number-of-hospitals-and-hospital-employment-in-each-state-in-2019.htm (visited July 12, 2024).
[5] National Safety Council: https://injuryfacts.nsc.org/work/costs/work-injury-costs/ (visited July 12, 2024).
Week 4: Narrowing Down Leads (Revising Needs Statements)

This week offered another full slate of complex spine surgeries as well as multiple endoscopic brain tumor resections. I was able to witness two iterations of the newly FDA approved TOPs system surgery, an alternative to fusion in order to achieve decompression. I was also able to witness the implementation of a new optical surgical navigation tool produced by Augmedics. This employed similar IR based optical navigation technology to Medtronic’s StealthStation, but mounts the IR camera on an augmented reality (AR) headset. The headset eliminates the need for surgeons to continually check a monitor and allows surgeons to view a holographic image overlay of the patient’s O-arm 3D X-ray, including the ability to monitor the depth of an inserted tool by simply tilting their head. I observed the successful use of this system to perform a kyphoplasty to treat a form of scoliosis. I was also able to get a look at the Surgical Innovation Training Laboratory (SITL) located in the basement of the neurology research building. The SITL is an American College of Surgeons Level-1 comprehensive institute and houses some of the most advanced surgical robotic systems currently available. It is extremely exciting to be able to witness the cutting edge of surgical techniques and device development and implementation.
One of my key takeaways from this past week’s workshop based didactic session came from receiving feedback about my needs statements from team members from other clinics. It allowed me to truly realize how important it is to correctly word the needs statement in order to convey your intended need without providing additional context. While my own team is steeped in the context, other teams may have a contextual bias completely different from my own based on their recent experiences. Taking what I have learned I can improve my needs statement from the previous week: Hospital workers need a reduction in tripping hazards to decrease the risk of injury and reduce cost to the hospital.
While the population still feels appropriate, the opportunity now appears to me too broad, and the outcome too vague. The opportunity of reducing all tripping hazards could refer to trash on the floor or overcrowding of the OR, while changing the opportunity to tripping hazards arising from medical devices allows for my intended solution space of reducing the risk of tripping due to cables and tubing. While this limiting of scope necessarily decreases the viability of the eventual solution, it increases the feasibility as the solution space is better defined. The current outcome is a bit too unspecific and unfocused. Reducing cost to the hospital is not the only outcome of injuries to hospital workers due to tripping. Tripping in the OR could endanger patient safety or damage equipment. Also, the challenges to scheduling caused by employees needing to miss work such as increased pay to other workers or postponement of procedures could have a significant financial impact on hospitals. The challenge is to find an expression of the desired outcome that encompasses all of these challenges while remaining quantifiable. This change in outcome could be to reduce the financial impact of employee injuries. However, I am not satisfied that this change increases the clarity of the outcome. My revised needs statement is: Hospital staff need a reduction in tripping hazards arising from medical devices in order to reduce the financial impact of employee injuries.
My observations in the OR over this past week have led me to develop a new needs statement. Surgeons require an intuitive suction device that can manage tissue clogging in order to reduce lost time during procedures. On multiple occasions I observed the need for scrub nurses to take a suction tip clogged with soft tissue and manually force saline through the suction tip with a large syringe in order to clear it. During some procedures the scrub nurse had to perform this action upwards of 10 times. While the surgeons were able to switch to a secondary suction tip, the time lost during exchange and the waste of time for the scrub nurse was not insignificant. After speaking with Dr. Mehta about this issue, he confirmed that it was a constant and somewhat frustrating problem and that an intuitive solution would be useful. There are several products on the market or in development, with the most common being the Chicago Tip. This device allows the surgeon to manually force out the tissue with a slider, however Dr. Mehta does not feel the device suits his needs. This implies that there is likely room for improvement.
Week 5: Breaking down processes (Storyboard development)
Week 5 was our last full week in the OR and I was determined to make the most of it. I was able to observe another TOPs surgery using surgical navigation. I was able to speak more to the medical reps and learned that some representatives have a purely commission-based salary, which incentivizes their desire to sell new technologies to the surgeons. Also,
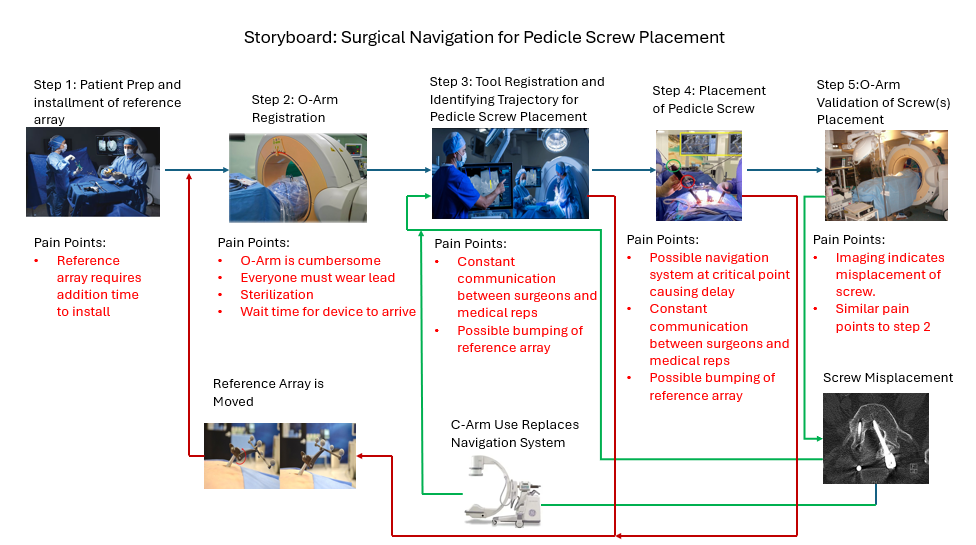
I was able to view another surgery using the Augmedics system, this time a L1-L2 OLIF (oblique lateral interbody fusion). The Augmedics system is a headset based augmented reality surgical navigation system designed for a number of surgical applications. I observed that while the IR reference array is able to be sterilized in the Medtronic StealthStation navigation system, the Augmedics arrays are single use and discarded after use. While this offers more assurance of sterility, it produces much more waste and cost to the hospital. While the Augmedics system has several advantages, it still suffers from some of the limitations of other optical surgical navigation technologies. I have created a storyboard for the process of performing a pedicle screw placement using surgical navigation, in this case the Medtronic StealthStation, highlighting issues with the reference array that affect both Medtronic and Augmedics systems.
Steps involved in using a surgical navigation system for pedicle screw placement:
Step 1: The patient is prepared for surgery as normal. After incision and the placement of the retractor blades, a infrared (IR) reflective array is attached to the retractor blade.
Pain Points: The reference array requires addition time to install, delaying the procedure.
Step 2: The O-arm x-ray imaging device is brought into the OR and used to register the location of the reference array to a 3D X-ray image of the patient.
Pain points: The O-arm is extremely large and cumbersome. It also requires everyone in the room to be wearing lead, or else leave the room. The O-arm must be sterilized by covering it with new draping before each use. Due to the expense of the O-arm, there are few available in the OR, and thus sometimes the wait for one to arrive can delay surgery.
Step 3: The tools are registered with the navigation system and the surgeon begins to identify their desired trajectory and depth for placing the pedicle screw.
Pain points: This process requires constant communication with medical representatives which can sometimes lead to errors. The reference array could be bumped out of position, leading to a whole new registration process, including the use of the O-arm.
Step 4: The pedicle screw is placed by the surgeon. If multiple screws are being placed, then the process returns to step 3.
Pain points: This again requires constant communication between the medical rep and the surgeon. Again, the array could be bumped leading to a new registration process. The system may experience a malfunction which leads to delays in the procedure.
Step 5: The O-arm is brought in to validate the correct placement of the screw(s).
Pain points: The imaging may indicate that the screw was misplaced. This is a serious concern and requires the removal and replacement of the screw. At this point the surgeon will decide whether to begin the navigation process over from step 3, or to rely on constant C-arm x-ray images while performing a similar process and ignoring the use of navigation entirely.
References:
Colombo, Paola Enrica et al. “Medtronic O-arm: Image quality and radiation dose assessment in 3D imaging.” (2010).
Huang, Xinle, et al. “Unilateral Biportal Endoscopic Lumbar Interbody Fusion Assisted by Intraoperative O-Arm Total Navigation for Lumbar Degenerative Disease: A Retrospective Study.” Frontiers in Surgery, vol. 9, 2022, pp. 1026952–1026952.
Crawford, N., Johnson, N. & Theodore, N. Ensuring navigation integrity using robotics in spine surgery. J Robotic Surg 14, 177–183 (2020).
La Rocca, G., Mazzucchi, E., Pignotti, F. et al. Navigated, percutaneous, three-step technique for lumbar and sacral screw placement: a novel, minimally invasive, and maximally safe strategy. J Orthop Traumatol 24, 32 (2023).
Medtronic. “Spinal Surgical Navigation: StealthStation S8 Surgical Navigation System”.Accessed August 1, 2024. https://www.medtronic.com/us-en/healthcare-professionals/products/neurological/surgical-navigation-systems/stealthstation/stealthstation-s8.html
Week 6: Lessons learned from CIP (Conclusion)
My time in the neurosurgery operating room with the clinical immersion program has been an academic highlight for me, and an experience I will never forget. I have gained a new perspective on surgery, medical professionals, medical device development, and patient care. I am so grateful to Dr. Mehta, Dr. Felder, Dr. Browne, and all of the residents, nurses, medical students, and other medical professionals who helped to provide such a rewarding experience. The program offered innumerable lessons from the mundane to the profound.
From the clinic or in this case primarily the neurosurgery OR:
- Remaining calm in stressful situations is critical to positive outcomes for patients.
- Every effort must be made to ensure that a procedure goes smoothly before the procedure begins, because complications will inherently arise.
- While a complex neurological surgery may seem like it requires a relatively rote approach, there is quite a bit of deviation in approach and technique between surgeons
From Program:
- The development of new medical devices is a long and complex process that requires thorough planning and comprehensive research
- User centered design practices are key to producing a solution that will be meaningful to the medical professionals and patients for whom the solution is intended to help.
- Medical innovation is an interdisciplinary process that requires input from many diverse fields and backgrounds in order to be successful.
From Stakeholders:
- Different types of medical professionals offer important pieces of the puzzle, and not everyone has all the information. In fact some OR workers may have different motivations and thus have a different perspective on a particular procedure.
- There are many solutions to problems faced in the OR being developed, however many of them do not directly consider the user experience, in this case the surgeon or nurse.
Advice for future participants:
- Asking questions is absolutely vital in order to extract as much value as possible from the experience. While the OR can be an intimidating experience, most medical professionals will be happy to answer any of your questions, and possibly inclined to reach out to you with further information if they believe you are invested. Ofcourse, the timing and place of any interview should be carefully considered.
- It’s ok to be overwhelmed for a while, weeks even. Being placed in an environment with mostly people who are more accustomed to the space and actions can make you feel that you don’t belong, but it’s important to remember that you are there to learn as much as possible.