
Richard Chiu
2023 Students
IMED, MS2
Department of Neurosurgery
Pronouns: He/Him/His
Email:
Week 1: A transition to a new environment and perspective
During this first week of the Clinical Immersion Program with Dr. Mehta, my teammates and I had the privilege of observing spine surgeries in the operating room and shadowing in the neurosurgery clinic. We were tasked with a simple goal: be a sponge and absorb as much information as we could about workflows, operations, and areas for improvement. Having just finished the first year of medical school, switching from a mindset of clinical reasoning to that of an innovator has proven to be more difficult than I expected. I found myself often thinking about indications, complications, and outcomes for procedures, rather than how devices and processes could be improved. This week of clinical immersion also marked the first time that I have ever stepped foot in the operating room, and getting used to the atmosphere, culture, and unspoken rules of this environment was yet another hurdle to overcome. Nonetheless, I was able to tackle this difficult transition by the end of the week and identify a few devices that I found to be either lacking in design or particularly well-engineered:
Good Design: O-Arm Surgical Imaging System
In the OR, my group observed three lumbar interbody fusion (LIF) procedures, two with a transforaminal approach, and one with an anterior approach. Towards the end of each procedure, the surgical team used an O-Arm Surgical Imaging System by Medtronic to intraoperatively generate a 3D rendering of the vertebrae and confirm proper placement of the pedicle screws and fusion cage. This device stood out to me as an incredible innovation for a few reasons, outlined as follows:
Activities: The O-Arm is operated by a technician, who moves the machine into place when the surgery team is ready to check placement of screws, cages, and other surgical equipment. They first cover the machine in a sterile plastic drape, position the machine correctly around the patient, and then activate the machine to record and render a 3D representation of the vertebrae. At the same time, everyone else in the operating room leaves the room to avoid radiation exposure. In this case, the design of the O-Arm to easily allow for a sterile drape to be placed around it, the mobility which allows for proper positioning of the device around a still patient, and the rendering ability of the machine to produce a 3D representation of vertebrae and surgical hardware makes this device incredibly effective and contributes to improved surgical outcomes.
Environment: The O-Arm is specifically intended to be used in the operating room for intraoperative imaging. The OR environment tends to contain multiple different large devices, machines, tools, and tables. Thus, the mobile and relatively compact design of the O-Arm lends itself to being used in the OR environment.
Interactions: The most relevant interaction between the O-Arm and its users comes in the form of large doses of radiation. However, this is avoided simply by moving out of the operating room while the O-Arm is imaging the patient.
Objects: The O-Arm system consists of the actual imaging apparatus and the attached monitor which displays the 3D rendering. A remote can rotate the rendering in three planes, allowing for easy visualization of hardware placement. In this way, the O-Arm is intuitive in its operation.
Users: The users of the O-Arm are (1) surgeons who use the 3D rendering to ensure proper placement of hardware, (2) technicians who operate the device, and (3) patients who are imaged by the device. The O-Arm serves all three of these user groups by providing an intuitive 3D rendering, having a compact and mobile design, and facilitating sterility.
As a final point, this device also simplifies the workflow of surgery and postoperative assessment. It allows for continuous localization, targeting, and proper placement of hardware during the procedure, rather than relying on a single preoperative image to guide the surgery. Prior to closing, it also allows for a final check of screw and cage placement, rather than having to close the patient first, send them to radiology, and then assess hardware placement. This makes it easier to make any adjustments without requiring the patient to undergo a second surgery.
Bad Design: A certain wheelchair design
A glaring example of a poor design was a specific wheelchair observed by my team in the neurosurgery clinic. A patient with multiple sclerosis, presenting with lower extremity weakness, was brought into the clinic by their partner in this wheelchair. During the visit, the physician needed to perform a physical examination of the legs, requiring that the footplates and leg rests of the wheelchair be moved aside. However, given the patient’s lower extremity weakness, it was difficult for them to do this on their own, thus requiring the assistance of their partner to do a seemingly simple task. Given that patients in wheelchairs are more likely to have lower extremity pathology, I found it puzzling why a wheelchair was designed in a way that made it difficult for a patient with limited control of their legs to free their legs for the purpose of physician examination. A more organized summary of points for improvement are as follows:
Activities: A wheelchair’s main purpose is facilitating movement, and in this regard, this design did not seem to have significant faults. However, it is also important that a patient in a wheelchair is able to easily manipulate different components of the wheelchair to allow them to have better control of their movement. This specific wheelchair design failed in this aspect, as it was difficult for a patient without full leg strength and control to move footplates and leg rests.
Environment: Wheelchairs are intended to operate in all environments. In this regard, the design of this wheelchair made it difficult to operate in the clinic during physical examination, and likely when the patient tries to stand up from the wheelchair.
Interactions: Regarding the footplate and the leg rests in particular, there are not many interactions to consider. However, there may potentially be long-term consequences involved with prolonged discomfort or repeated use of a design that is not ergonomic.
Objects: The objects of interest for this wheelchair are specifically the footplates and leg rests. A patient with limited lower extremity control would find it difficult to remove their legs off these components in order to move them to the side. To do this, they would have to pick up their leg with one arm, while leaning down and forward to push aside the footplate. Such as design is not ergonomic and not user friendly for patients who need a wheelchair. A possible solution may involve hand-operated levers that can move these components, and footplates that rotate downward towards the floor, rather than upward against the patient’s foot.
Users: The main user of a wheelchair is the individual who is sitting in it. Other users might include people who help push the wheelchair to assist with navigation, as well as physicians who might be performing a physical examination of the patient in the wheelchair. This specific wheelchair did not effectively serve its users, since it was difficult for the patient to move the elements of the wheelchair, thus making it difficult for the physician to perform a physical examination of the lower extremities.
Week 2: Continuing observations
During this week of clinical immersion, my team and I were introduced to the neuro ICU and continued to observe spine surgeries in the OR. We were tasked with making new observations and synthesizing the information from the last two weeks to further refine our findings. To this end, I continued trying to observe in the OR from the perspective of an innovator, aiming to identify processes or devices that worked well, and those that did not.
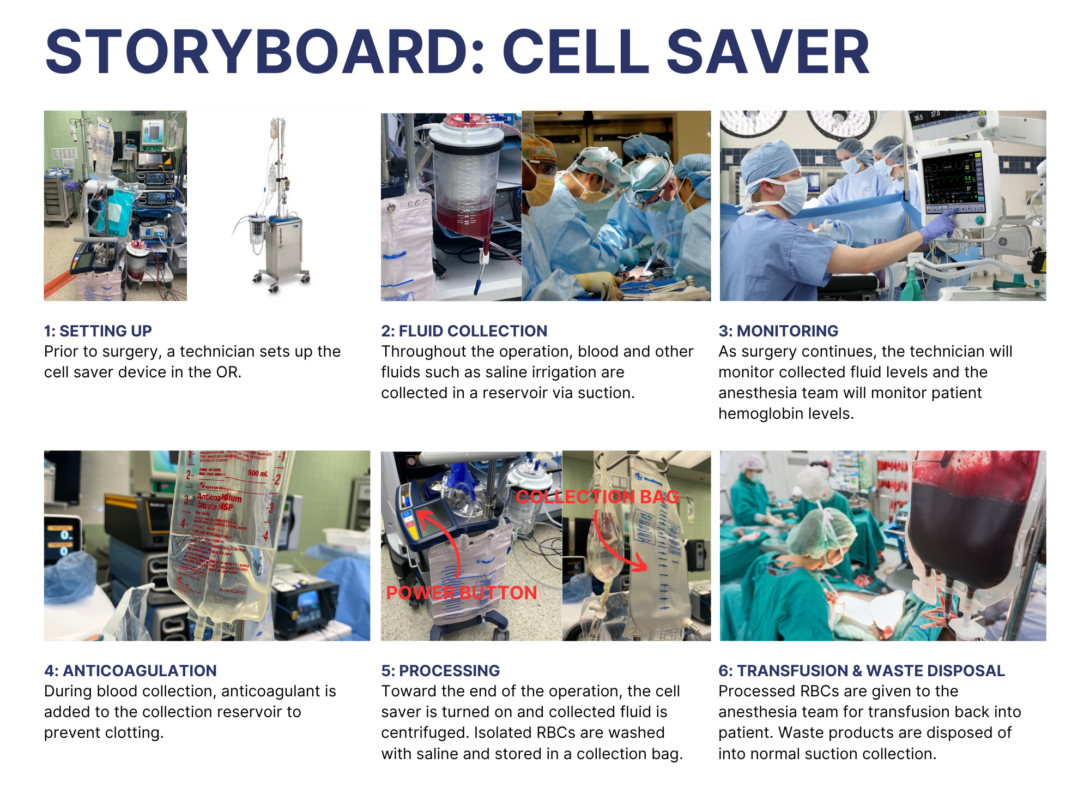
One of the cases that we observed was a Jehovah’s Witness who was undergoing a corpectomy followed by a cervical discectomy and fusion. Given the patient’s religious beliefs and the potential risk for significant blood loss, a cell saver autologous transfusion device was used to recycle blood lost during the surgery back into the patient’s circulation. This device struck me as particularly effective. It is relatively simple to operate, intuitive in design, and opens the possibility for transfusion for those that are religiously or otherwise opposed to allogeneic transfusion. Even still, some pain points exist in the process of performing autologous transfusion. To help contextualize these points for possible improvement, I created the above storyboard outlining the general steps of how a cell saver is used during a surgical operation.
Pain Points
1: Setting Up
- The presence of the cell saver and associated personnel needed to operate the device adds to OR crowding, which may especially be a problem when large apparatuses such as intraoperative imaging (i.e. C-Arm or O-Arm) or endoscopic equipment are also present in the room.
3: Monitoring
- The technician is only able to provide a rough estimate of RBC output given the amount of fluid that has been collected in the reservoir. During the procedure that I observed, this was done via a rough calculation of subtracting the amount of anticoagulant and an approximation of other fluids from the total reservoir volume.
5: Processing
- From activation of the cell saver device to the RBC transfusion bag being given to anesthesia, the processing step took around 10-15 minutes based on the single operation that I observed. Although this may be variable depending on multiple factors, this raised the question of whether transfusable blood could be prepared in an emergency situation where blood is being lost at a fast rate.
For a more comprehensive assessment of the utility of cell saver transfusion, I turned to the literature to examine the safety, efficiency, and relative costs of this method compared to allogeneic transfusions. In a review article by Frank et al., the authors provide an overview of relevant literature and important points regarding the use of autologous blood transfusion. They contend that use of a cell saver can provide numerous benefits, including provision of higher red blood cell quality, enhanced cost effectiveness compared to banked RBCs, and reduced exposure to allogeneic RBCs. However, it is stated that despite these benefits, clinical outcomes such as mortality, re-operation for bleeding, infections, and length-of-stay were uninfluenced by the use of cell salvage techniques. In terms of efficiency, the authors estimate that a modest 57% of shed blood is recovered using a cell saver. Variation exists based on surgical practices, but these findings suggest that there may be room for improvement or standardization in the practice of salvaging red blood cells. Finally, the authors discuss the perceived drawbacks of cell salvage. In cancer surgery, autologous transfusion introduces the possibility of reinfusing cancer cells into the bloodstream, which some have hypothesized could increase risk for distant metastasis or cancer recurrence following surgery. However, it was found that there was in fact no difference in cancer recurrence or development of metastasis between cancer patients undergoing surgery with either autologous or allogeneic transfusion. Similarly, although the authors discuss the possibility of bacterial contamination with cell salvage methods, they found that compared to operations using allogeneic transfusions, the risk of contaminated blood is minimal when appropriate measures are implemented, such as use of leukoreduction filters. Once again, this finding suggests a potential opportunity for standardization of practices to prevent negative outcomes.
Frank, S.M., Sikorski, R.A., Konig, G. et al. Clinical Utility of Autologous Salvaged Blood: a Review. J Gastrointest Surg 24, 464–472 (2020). https://doi.org/10.1007/s11605-019-04374-y
Week 3: Identifying needs in neurosurgery
The last three weeks of clinical immersion have made one thing clear: surgery, in many ways, has already been incredibly optimized. As I observed in the operating room, I was surrounded by high-tech equipment, efficient surgical tools, and advanced imaging modalities. Moreover, company representatives, some of whom work for multi-billion-dollar companies, constantly offered new devices for surgeons to try. I increasingly felt out of place — I was a mere second-year medical student attempting to innovate within a space that industry giants operated in. To top it off, I was reminded that there are surgeons, some with decades of experience under their belt, who also have engineering expertise and are already developing innovations related to the surgical implements they use every day. With this in mind, I began focusing more on processes and devices adjacent to surgery itself, rather than surgical tools which have already been well-engineered.
During this past week of observation in the OR, I witnessed one such process that seemed particularly prone to error and inaccuracy. The procedure was a percutaneous T12-L2 fusion which utilized a StealthStation Surgical Navigation System by Medtronic. Part of using this system is obtaining the initial imaging which consists of first affixing the passive reference array to the patient, and then using the O-Arm to obtain imaging of the bony anatomy relative to the array. Throughout the remainder of the procedure, the passive array must be kept perfectly still, or else the navigation will be offset and screw placement could be displaced, potentially injuring important structures within or surrounding the spine such as nerves and major arteries. Moreover, the StealthStation system has no way of automatically detecting if the passive array were to be moved, and this would only be detected when the surgeons realize there is a mismatch between the navigation imaging and their own tactile feedback (i.e. the StealthStation shows that an instrument is hitting bone, when the surgeon feels only soft tissue) or at the end of a surgical step when intraoperative imaging is used to confirm placement of surgical hardware (i.e. C-Arm confirming placement of pedicle screw within the pedicle). Witnessing this difficulty in the OR led me to develop my first iteration of a needs statement:
Neurosurgeons performing surgery using the StealthStation Surgical Navigation System require that the passive array is perfectly affixed throughout the surgery and need to improve the accuracy and reliability of surgical navigation.
- Population: Neurosurgeons performing surgery using the StealthStation Surgical Navigation System
- Opportunity: Passive array requiring perfect fixation throughout surgery
- Outcome: Improve accuracy and reliability of surgical navigation
Reflecting on this needs statement, I realized that it was not only the passive array that had issues, but also the arrays attached to instruments that allow them to be detected by the StealthStation sensors. The arrays are large, potentially obstructing proper grip on the part of the surgeon and posing ergonomic issues. Moreover, the arrays may move due to mallet use or rotation of the instrument, which could create difficulties in detection by the StealthStation system. This led to the second iteration of my needs statement, slightly altering the opportunity that is being addressed:
Neurosurgeons performing surgery using the StealthStation Surgical Navigation System require that arrays are properly affixed to the patient or instruments throughout the procedure and need to improve the accuracy and reliability of surgical navigation.
- Population: Neurosurgeons performing surgery using the StealthStation Surgical Navigation System
- Opportunity: Arrays requiring proper fixation throughout the procedure
- Outcome: Improve accuracy and reliability of surgical navigation
This second iteration of a needs statement more accurately captured the issues related to the StealthStation arrays, but the scope of the relevant population still needed additional refinement. In particular, the specific use of StealthStation that I observed seems to be primarily for percutaneous spine surgeries, since intraoperative CT imaging is best used to visualize bony anatomy. When used for soft tissue surgery, such as brain surgeries, a different process involving the overlaying of preoperative MRI is used. Thus, the final iteration of my needs statement is as follows:
Neurosurgeons performing percutaneous spine surgery using the StealthStation Surgical Navigation System require that arrays are properly affixed to the patient or instruments throughout the procedure and need to improve the accuracy and reliability of surgical navigation.
- Population: Neurosurgeons performing percutaneous spine surgery using the StealthStation Surgical Navigation System
- Opportunity: Arrays requiring proper fixation throughout the procedure
- Outcome: Improve accuracy and reliability of surgical navigation
Ultimately, crafting these needs statements was good practice for honing in on specific problems within a defined scope. As I continue clinical immersion in neurosurgery, I plan to identify additional needs that could be the focus of my team’s innovation project.
Week 4: Pondering pain points, patents, and possibilities
In this week of clinical immersion, my group and I were largely left to our own devices. Our clinical advisor was out of the country, and we were responsible for finding our own activities that would contribute to our exploration of needs in neurosurgery. This largely consisted of joining rounds in the neuro ICU and attempting to find cases in the OR that we could observe. We were also tasked with synthesizing the observations, research, and interviews we have conducted in the last four weeks to further explore the feasibility of addressing the needs that we have identified. With this focus on feasibility, much of my research focused on two areas that seem the most approachable from the perspective of a student inexperienced in the actual practice of neurosurgery: patient positioning during cranial surgeries and array fixation when using the StealthStation Surgical Navigation System. The following research will focus on the latter.
From last week, the latest iteration of my needs statement for StealthStation navigation arrays was: Neurosurgeons performing percutaneous spine surgery using the StealthStation Surgical Navigation System require that arrays are properly affixed to the patient or instruments throughout the procedure and need to improve the accuracy and reliability of surgical navigation. For this week’s task, I have opted to focus the scope of this needs statement on just the passive reference array, rather than the instrument arrays. Upon reflection, I also chose to change the measured outcome to something more quantifiable, namely reducing the frequency of navigation-related surgical delays. I focused on preventing surgical delays rather than reducing navigation-related complications since the literature suggests that use of intraoperative computer-assisted navigation in pedicle screw placement is not associated with any difference in complication rates, but is associated with an increase in operative time by over 40 minutes [1]. Thus, the working needs statement I will be focusing on for this week is: Neurosurgeons performing percutaneous spine surgery using the StealthStation Surgical Navigation System require that reference arrays are properly affixed to the patient throughout the procedure and need to reduce the frequency of navigation-related surgical delays.
This focus on time delays related to the use of intraoperative navigation raises the question: is the increased operative time related solely to the setup and use of navigation systems, or do device errors meaningfully contribute to surgical delays? Unfortunately, I was unable to find an answer to this question in the literature; however, from my own observations and interviews with stakeholders knowledgeable with intraoperative navigation, it seems that device errors are quite common and do contribute significantly to delays. Namely, undetected movement of the reference array can result in all surgical navigation being displaced, resulting in improper placement of surgical hardware and requiring adjustments that prolong the surgery. Additionally, the navigation system that I observed in the OR had no method of detecting this movement, meaning that any displacement of the reference array had to be seen by a member of the surgical team and manually corrected. Seeing this as a potential space for innovation, I decided to investigate solutions that have already been developed and implemented.
This research led me to patent “US20150327948A1” titled “Navigation System for and Method of Tracking the Position of a Work Target,” assigned to Stryker European Operations Holding LLC [2]. This device corresponds to Stryker’s SpineMask tracker, which is an alternative to MedTronic’s reference array. The SpineMask is a noninvasive method of providing real-time navigation of surgical instruments relative to patient anatomy and contains features that address some of the issues associated with the reference array. Namely, the patent describes this device as having the ability to “[compensate] for the deformations sensed in [the device].” Additionally, it is claimed that if deformity is detected, the device is able to maintain accurate navigation by excluding deformed tracking points so that recalibration is not necessary. This suggests that this tracker is able to automatically detect movement of the tracker and prevent displacement of surgical navigation, which is a major pain point with the StealthStation system. However, it remains unclear whether these claims hold true in actual practice, as well as what amount of deformity is able to be corrected for by the device.
[1] Wagner, S. C., Morrissey, P. B., Kaye, I. D., Sebastian, A., Butler, J. S., & Kepler, C. K. (2018). Intraoperative pedicle screw navigation does not significantly affect complication rates after spine surgery. Journal of Clinical Neuroscience, 47, 198–201. https://doi.org/10.1016/j.jocn.2017.09.024
[2] Schoepp, H., Breisacher, J., & Kaltenbrunn, J. (2020). Navigation System for and Method of Tracking the Position of a Work Target.
Week 5: All about the money
This week, my team and I continued to observe in the OR to iterate on our needs statements and explore the desirability, feasibility, and viability of the problems we were looking to address. Given the importance of market forces and profit in the success of medical device sales, we were also tasked with estimating a total addressable market (TAM) for a medical device of interest related to our needs statements. For the sake of continuity, I chose to focus again on the reference frames for the StealthStation used during computer-assisted spine surgeries; however, my team and I will pursue a different problem for our final project proposal. This final project will focus on locating the source of bleeding during endoscopic spine surgeries, which is a problem that we have been considering on and off since our first weeks of clinical immersion.
Last week, my needs statement for the problem of surgical navigation arrays was “Neurosurgeons performing percutaneous spine surgery using the StealthStation Surgical Navigation System require that reference arrays are properly affixed to the patient throughout the procedure and need to reduce the frequency of navigation-related surgical delays.” Given the importance of scoping when estimating TAM, I wanted to revise the population based on what I observed in the OR this past week. I realized that the StealthStation was used not only for percutaneous spine surgeries, but also for many open surgeries to aid in pedicle screw placement. Thus, the final iteration of this needs statement is: Neurosurgeons performing spine surgery involving pedicle screw placement using the StealthStation Surgical Navigation System require that reference arrays are properly affixed to the patient throughout the procedure and need to reduce the frequency of navigation-related surgical delays.
To start estimating the TAM, I wanted to first determine the number of total spine surgeries in the United States involving the placement of pedicle screws, followed by determining the percentage of these surgeries that use computer-assisted intraoperative navigation. By far, the largest contributor to spine surgeries requiring pedicle screw placement is spinal fusion procedures. Based on information from the Agency for Healthcare Research and Quality (AHRQ), there were an estimated 455,000 spinal fusion surgeries performed in the U.S. in 2018, representing the most costly operating room procedure with hospital stays for spinal fusions costing a total of $14.1 billion [1]. To determine the percentage of these spinal fusions that used intraoperative navigation, I turned to the literature – one study estimated that over 10% of all fusions used some kind of computer-assisted navigation in 2017 [2]. These estimates suggest that approximately 45,500 spine surgeries annually in the U.S. use some kind of computer-assisted navigation, an estimate that does not even include other less common spine surgeries that may involve pedicle screw placement.
At this point, a number of issues make TAM estimation quite difficult. Firstly, most reference frames for surgical navigation are reusable, meaning that simply multiplying the cost of a single reference frame by the number of annual surgeries would not provide an accurate estimate of directly addressable market. Moreover, based on a thorough internet search, a per-unit cost for new reference frames is not publicly available. An accurate TAM would have to instead be based on per-use cost of the reference frame or number of new reference frames sold annually, which are both impossible to reliably calculate based on publicly available information. Instead, I opted to use a conservative estimate of $100 based on the sale of used reference frames on various sites. Using this estimate, the TAM for this needs statement is $4.55 million, which also does not factor in secondary costs and savings such as reduced complications and time savings associated with addressing this problem. Moreover, the market for surgical navigation devices for spin surgery may have expanded since 2017 as the technology continues to improve and more surgeons adopt these technologies in their own practice. Based on these reasons, it is possible that the TAM is actually much greater than what I have estimated in this post.
[1] Agency for Healthcare Research and Quality. (2021, November). Costs for spine fusions. Agency for Healthcare Research and Quality. https://www.ahrq.gov/data/infographics/spine-fusions.html
[2] Sharma, M., Uddin, S. A., Hanna, G., Ugiliweneza, B., Kim, T. T., Johnson, J. P., Boakye, M., & Drazin, D. (2022). Trends and long-term health care utilization of computer-assisted neuronavigation in spine fusions: An exact matched analysis of national administrative database. World Neurosurgery, 166, e850–e858. https://doi.org/10.1016/j.wneu.2022.07.116
Week 6: Conclusion and reflection
This week of clinical immersion marked our final week of the CIP program. My group and I observed for the last time in the operating room to work out some final details about endoscopic spine surgery and delivered our final project proposal on the topic of bleeding detection during endoscopic spine surgery. This entire experience in CIP has been enlightening for me, both from the perspective of a medical student and as a student innovator. Not only was it my first time observing in the operating room, but it was also the first time that I identified a clinical need through iterations of observation, interview, and research. I grappled with the concepts of desirability, feasibility, and viability in the context of medical device design, and I move forward in my career with this knowledge to hopefully develop medical technology to better serve my future patients. As I look back on this experience, I reflected on lessons learned from the OR, the program, and from the stakeholders that I worked with:
Lesson 1: Innovation comes slowly
During my first week in the OR, I began trying to identify problems that my team and I could work on as our project proposal for CIP. I distinctly remember feeling worried that I was unable to find a feasible problem to work on, despite having only been in the OR for two full days. Looking back, I am not sure what I was expecting – innovation comes slowly. I first had to become accustomed to the OR environment and workflow before I could truly understand the processes that I hoped to innovate. In the end, my team and I did not determine our final project idea until the final day of Week 5, which goes to show that the process of identifying needs often requires weeks of observation.
Lesson 2: Inexperience can be an advantage
During my first session observing in the OR, I remember thinking that all the surgeons and nursing staff were so knowledgeable and well-versed in their respective roles. I thought to myself, “with all of these experienced staff, what could possibly be left for mere students to improve upon?” I am sure that given the intimidating nature of the environment, this thought may cross the mind of many student innovators stepping foot in the OR. What I did not realize was that experience can often introduce bias into the analysis of processes, and inexperience may make innovation easier. A surgeon who has performed a certain procedure for thirty years may have become blind to pain points because of their experience, whereas a naïve student innovator will see these pain points and question why they have not been improved upon. In this way, inexperience may be an advantage when innovating upon inefficiencies that have become the norm.
To future CIP students, I encourage you to keep these lessons in mind as you observe in the OR and clinics to identify problems and clinical needs of your own. In addition, I also want to offer the following advice:
- Don’t force it – You may be tempted, as I was, to settle for a problem you observed early in CIP and run with it. I encourage you to keep an open mind until you must pick a final project; you never know what clinical needs you may find!
- Don’t be afraid to ask questions – Surgical staff were far more approachable than I initially thought. When they are not busy, I encourage you to ask your questions to members of the surgical team; they are incredibly helpful! I found vendor reps to be especially knowledgeable about specific devices if you have questions about them.
- You get what you put in – Many aspects of CIP are self-driven, including the amount of time you want to spend observing in the OR. I encourage future CIP students to put in as much effort as you can in observing and thinking about clinical problems – it will pay off in the end!