
Mia Cirrincione
Medical Student (M2)
2024 Department of Plastic and Reconstructive Surgery
Pronouns: She/Her
Email:
Week 1. Sticking Points & Surgical Pouches
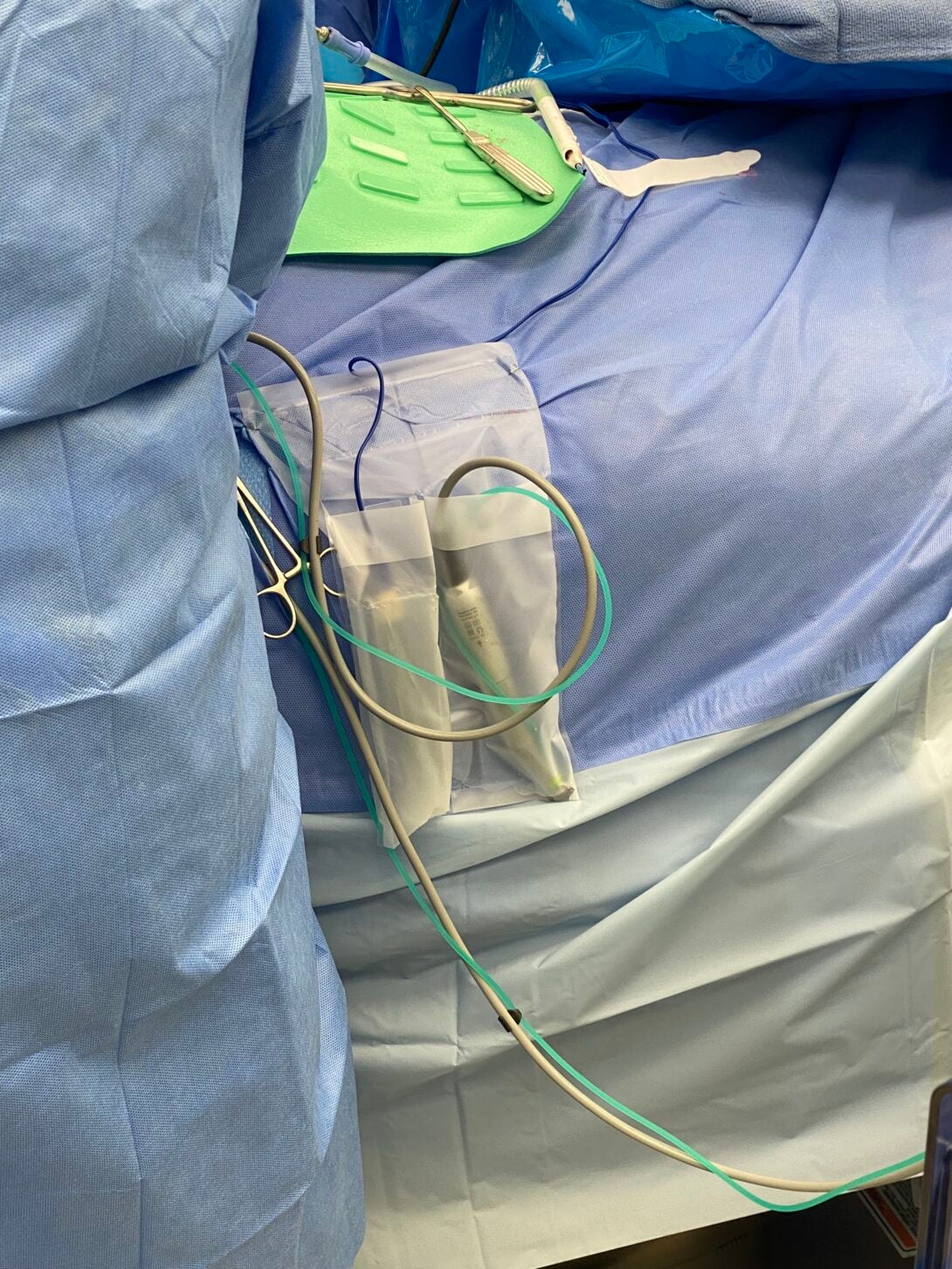
Surgical pouches are commonly used in the operating room to hold various sterile instruments during a procedure. Applying the AEIOU framework below demonstrates and characterizes their use:
Activities: Surgeons and OR staff interact with these pouches throughout countless procedures. Activities include unboxing the pouches, attaching them to the operating table, and ensuring they securely hold instruments throughout surgery. Many instruments with tubing or electrical wires are placed in these pouches to maintain organization. Issues can arise when the adhesive fails, which leads to the use of alternative methods like stapling. Specifically, during the procedure, surgeons may inadvertently catch their gowns on the adhesive of the pouches, leading to unintended pulling or dislodging of the pouch from its intended position.
Environments: The surgical environment of the OR demands strict adherence to sterility, while immersed in a room with many moving parts and people. Surgical pouches maintain organization and accessibility of instruments during procedures. When adhesive malfunctions, there is a risk of contamination if the instruments fall to the ground.
Interactions: Interactions with faulty pouches affect the entire surgical team. In these situations, nurses need to address issues promptly to avoid delays or contamination risks. The adhesive malfunction can disrupt the flow of activities, requiring immediate attention and adjustments during critical phases of surgery.
Objects: Surgical pouches are designed to securely hold and organize instruments, ensuring they remain accessible and sterile throughout procedures. Malfunctioning adhesive impacts reliability. Other objects like magnetic mats (shown in green) are used to hold instruments. The mats are placed on a sterile tray or on the patient’s abdomen. In a maxillofacial surgery that uses drills, the surgeon explained it is not advised to place the drill on the magnetic mat. The magnet in the mat can actually initiate the drill’s motor, which is a safety hazard for all involved. In this scenario, the surgical pouches may be the closest and hence most convenient place to store this sterile tool.
Users: Surgeons, nurses, and surgical technicians are primary users of surgical pouches. There are constant handoffs of tools and sharing of resources throughout the procedure. Seamless interactions between users improves the procedure’s efficiency and effectiveness, by minimizing any delays or errors.
Initially perceived as excellent design, the usability of surgical pouches was questioned when the surgeon who uses them daily expressed dissatisfaction. This highlights the importance of user feedback in product development. User experiences, such as pouches catching on surgical gowns and their adhesive failing, provide valuable insights that may not be evident from observation alone. Incorporating regular user feedback into the design process can lead to improvements that better meet the needs and expectations of medical professionals, and ultimately enhance the efficiency and safety of surgical procedures for patients.
The AEIOU framework provides a structured approach to understanding the complexities associated with items like surgical pouches. By analyzing activities, environments, interactions, objects, and users, one can more clearly identify specific issues and strengths. This method captures critical data and can help facilitate iterative improvements to enhance surgical outcomes through better tools and equipment.
Week 2. The Art of De-Epithelialization
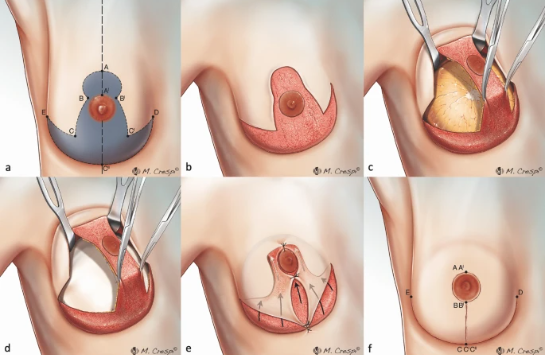
De-epithelialization is a technique that thins out the epidermis layer of the skin to resurface defects in a cavity or to implant a flap pedicle subcutaneously, preserving the subdermal plexus to support the vascularity of the flap.
From our observations in the OR, de-epithelialization is time consuming and requires more advanced skill than other techniques. According to Mabrouw & Wafa (2023), de-epithelialization is commonly used in breast reduction procedures. On the other hand, during our time of observation we saw the technique implemented in a variety of anatomical application for various spinal closure flaps.
The tools used in de-epithelialization are scissors and a scalpel. While there is another tool on the market, its indicated use is in breast procedures and it has not widely been adopted as standard operating procedure. The proprietary v-shaped blade allows for strips of epithelium to be removed in a more streamlined fashion.
Cordova, A., Rossi, M., Roggio, T. et al. The wide base bipedicled (WIBB) flap in nipple-sparing skin-reducing mastectomy. Sci Rep 14, 9226 (2024).
Aboul Wafa, Ahmed Mabrouk MBBCH, MSc, MD. Extended Superior Dermoglandular Pedicle Approach: A Versatile Technique for a Variety of Breast Deformities. Plastic & Reconstructive Surgery-Global Open 11(11):p e5430, November 2023.
Week 3. The Need for Speed
Primary Observation:
- A: Thin out the epidermis layer of the skin to resurface defects in a cavity or to implant a flap pedicle, preserving vascularity of the flap.
- E: OR, patient general anesthesia, private practice vs academic
- I: Time-consuming, advanced surgical technique
- O: Scissors, scalpel (manual)
- U: Plastic & Reconstructive Surgeons, Residents
Secondary Observation: average 15.5 min per manual de-epithelialization, physically taxing repetitive motion, uniform tension is critical in performing smooth dissection (Murphy, 2011)
Needs Statement: Plastic Surgeons performing de-epithelialization are required to perform a technically demanding and precise depth dissection for vasculature preservation, while there is a need to reduce overall procedure time, surgeon injury rate from repetitive movement, operative costs, and flap revision rate.
Second Iteration of the needs statement was created to define the outcome. The following statement hones in on the outcome that was deemed most important from interviews in the OR and literature review.
Needs Statement: Plastic Surgeons performing de-epithelialization are required to perform a technically demanding and precise depth dissection for vasculature preservation, and there is a need to reduce overall procedure time and consequent operative costs.
Total Addressable Market: Current device on market $512. 100,000 Annual Breast Reconstructions in US. Assumption of single-use product. $51.2 M
Week 4. Iterative Needs Statement
Needs Statement: Surgeons performing de-epithelialization are required to perform a technically demanding and precise depth dissection for vasculature preservation, and there is a need to reduce overall procedure time and consequent operative costs.
Week 5. Storyboard
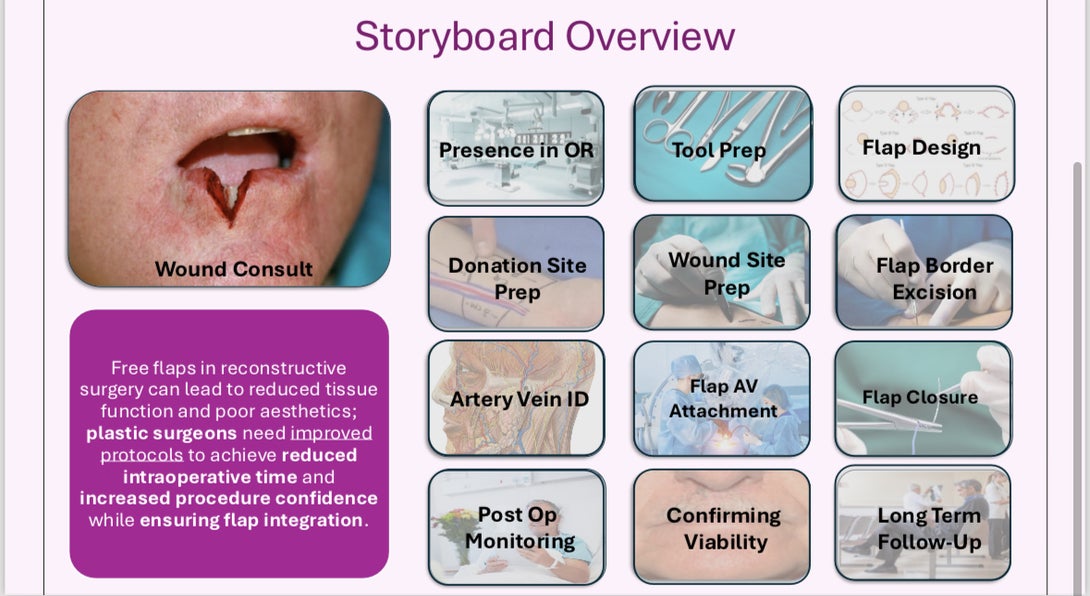
Flaps
Week 5. Part 2 Intraoperative Details
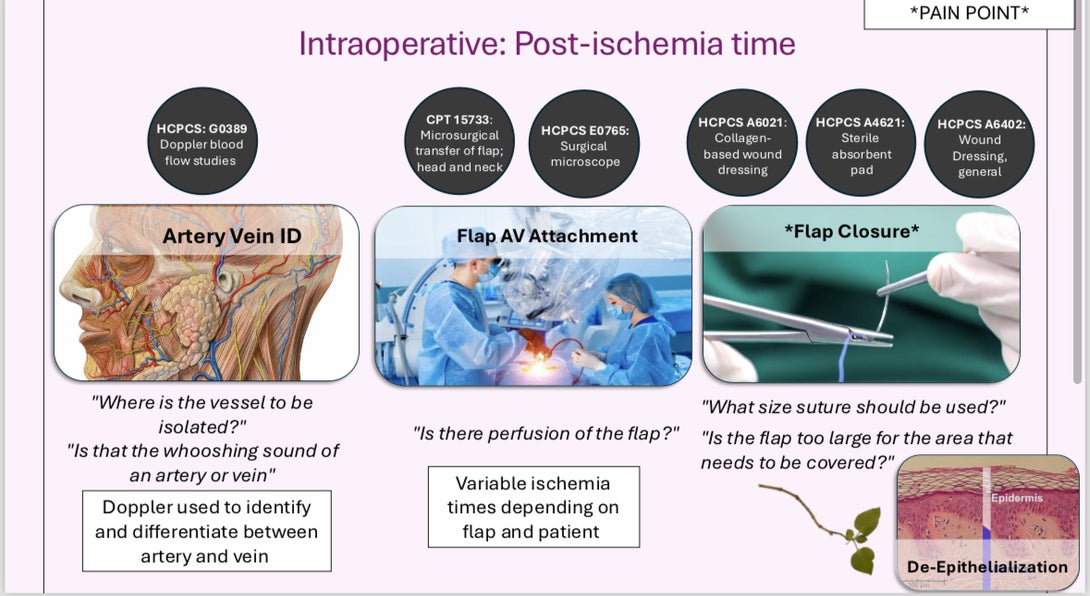
.
Week 6. "OR-ganizing My Thoughts: Conclusion of CIP
……