
Jamie Rae Cuartero
Student Participant
Biomedical Engineering Undergraduate Senior, Cell & Tissue Engineering concentration
Gastroenterology Department
Pronouns: She/Her/Hers
Email:
Week 1: Good and Bad Designs
There was a lot to take in during my first week observing the GI endoscopy lab. I was especially attentive to the overall systematic flow of patients into and out of the lab. From the point of view of a patient, the process upon arrival is simple: Arrive, talk to nurse, change into patient gown and get an IV, talk to doctor, get rolled into the procedure room, go through the procedure, get rolled to post-procedure and receive a long-awaited meal (since patients must fast the previous day). However, it is a bit difficult to write out this process from the point of view of a fly on the wall since many things happen simultaneously. While the nurse is asking the patient questions in pre-procedure and documenting the information in a computer, doctors and technicians are prepping the procedure room to make sure they have the correct equipment for the colonoscopy, EUS, ERCP, or other procedure. During the procedure, the nurse continues to document information from the procedure while comforting the patient and labeling biopsy jars if necessary. After the procedure, the nurse rolls the patient to a post-procedure bay. The doctor moves to the central desk of the lab and uses a computer program to quickly label a diagram with pictures from the procedure and goes through a variety of drop-down menus to fill in the blanks to construct a report for the patient to take home. During this, the technicians clean the procedure room and set up for the next patient. By the time the technicians are ready, the doctor is probably already obtaining consent from the next patient, which means a nurse has already prepped that patient while the doctor was performing the previous procedure. The swift coordination and communication between all staff is essential to efficient patient care. It is streamlined by the use of comprehensive computer programs tailored to the GI department and a systematic circulation of patients throughout the lab’s layout: pre-procedure bays near the entrance, procedure rooms down the back hall, and post-procedure bays along the wall leading back to the patient entrance.
I was also able to observe multiple procedures performed in the GI lab. The process is generally the same across different procedures. The scope is inserted into the patient through the rectum, mouth, or nose, and the GI tract is inspected for polyps, inflammation, or any abnormalities. A technician, Kevin Johnson, explained that scopes vary in diameter and camera orientation and how they may be chosen and operated for specific procedures and patients. Each scope has tradeoffs as some are stiffer, which increases the risk of perforating the walls of the GI tract, but less stiff scopes are more susceptible to looping around in a bend in the colon instead of continuing down a turn. Dr. Trivedi also informed us that about 40% of GI doctors file for long term disability for hand and wrist problems due to the weight and repeated movements to maneuver the scope and its multiple knobs and buttons. Aside from the instruments, the procedure room also posed various ergonomic challenges as monitors are too high up for some doctors so they must look high up and away from the patient to see the camera. Wires and tubing pose trip risks, and limited space make moving around the room slow and difficult.
Good Design:
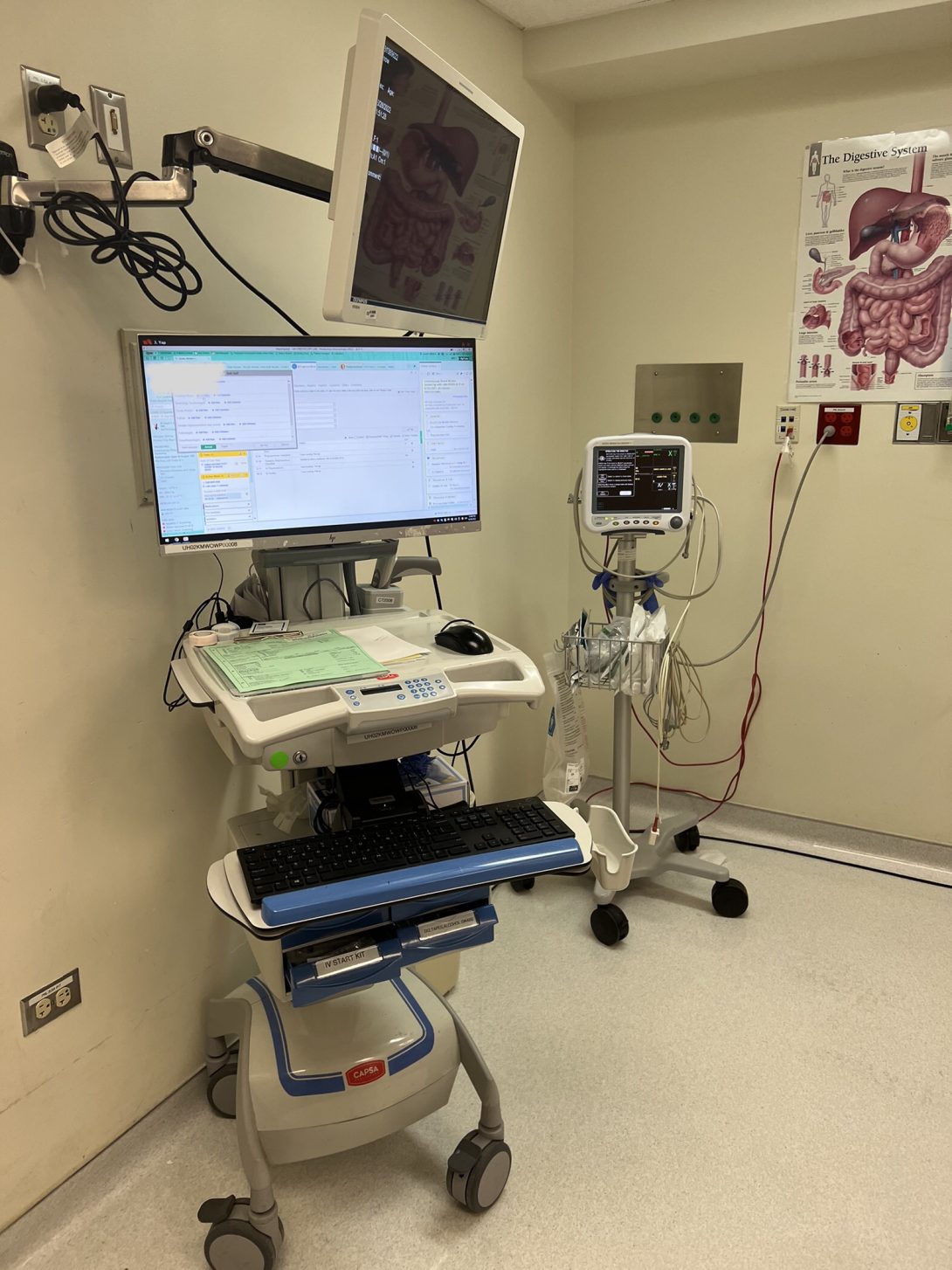
With most of the patients in the endoscopy lab being outpatients, there’s a lot of movement between bays. Given the small space in the endoscopy lab, there is not a computer in every patient bay. Instead, computers are mounted on carts that the nurses can roll from bay to bay. The carts have multiple tiers of platforms and compartments that the nurse can place the patient’s clipboard and IV bag. Each cart also has drawers of supplies that the nurses need such as an IV start kit, needles & syringes, and medication labels. This compact cart design eliminates extra walking back and forth across the room for supplies in an already busy environment.
Bad Design:
As stated earlier, the procedure room poses ergonomic challenges for the doctors. One that multiple doctors mentioned was the monitor positioning. The monitors where the scope video is displayed is mounted on the wall or ceiling and are too high for comfort and practicality. The doctors must crane their necks upwards during the procedure which causes strain and discomfort over time. It is also suboptimal in terms of practicality since the doctor has to look away from the patient and scope in their hands during the procedure. During ERCPs, another screen for X-ray images is needed, but it is mounted far from the scope video monitor which adds another extra movement for the doctor.
In addition, observing the pre-procedure nurses and talking to Dr. Trivedi, it is evident that patient preparedness and compliance was one of the biggest factors dictating the ease of flow of procedures on a given day. The patient eating solid food the day before or the morning of the procedure would obstruct the doctor’s view through the scope during the procedure. Certain substances such as milk products necessitate having a conversation with the anesthesiologist since it could react negatively with the medications. If the patient did not finish all of the prescribed prep liquid the day before, there would be an abundance of bile in the digestive tract that would make it difficult for the doctor to see polyps or inflammation on the tract walls. Not only does patient noncompliance decrease the efficacy of the procedures, but it can also give rise to a huge scheduling disaster for the charge nurse. Procedures are delayed, the procedure list must be rearranged so doctors, nurses, and patients must be informed, and all this is happening while new patients are coming in (or not showing up, which is also disruptive), which leads to needing to make more phone calls, arranging transportation, etc. Long story short, noncompliance very easily cascades into a monstrous scheduling disaster. This bad design is not necessarily a tangible device, but rather is an issue regarding an insufficient communication with patients which could stem from miscommunication due to a loud environment in the lab during phone calls, language discrepancies, or lack of reminders for the patient.
Week 2: Storyboard
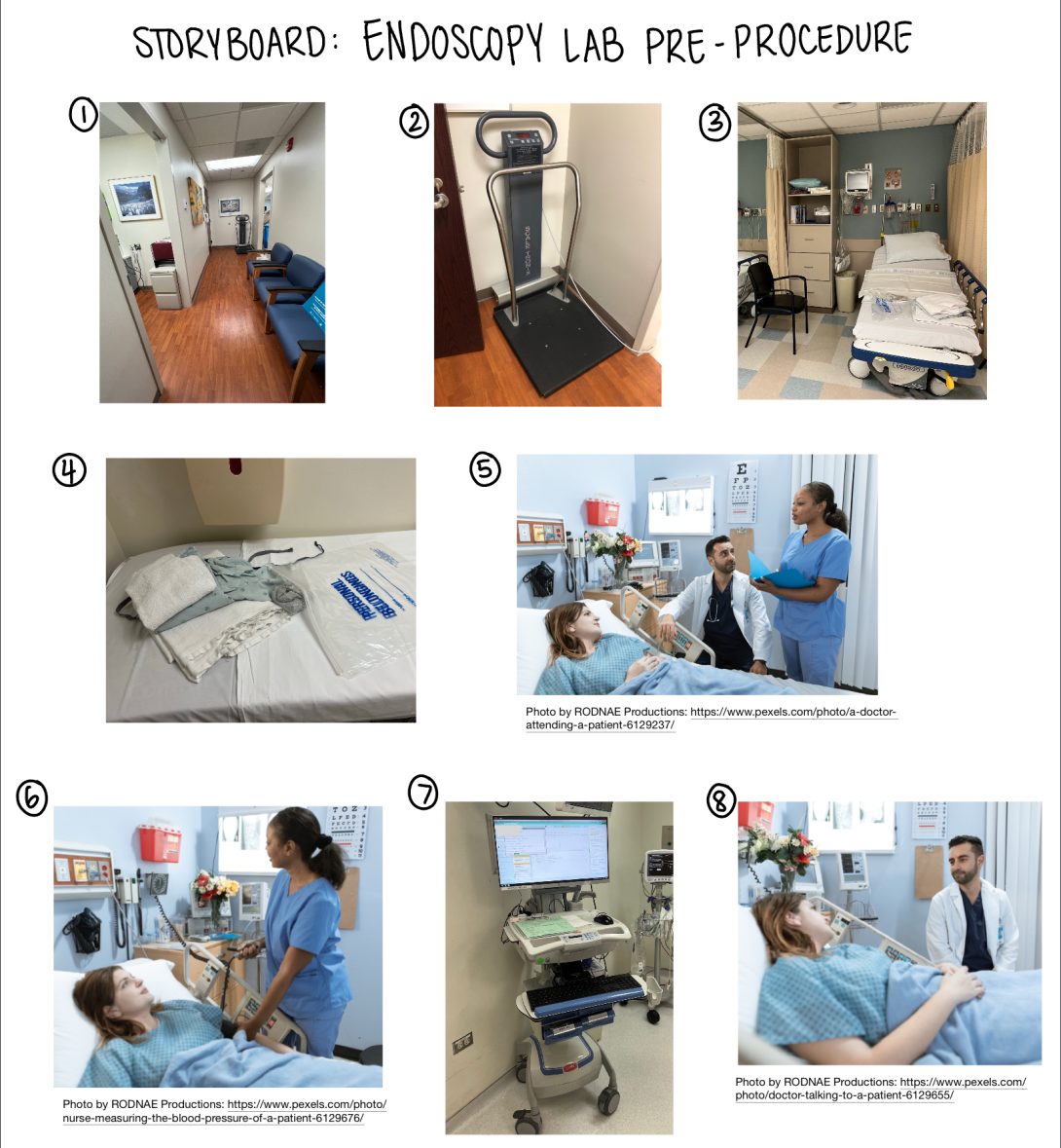
As I mentioned in the previous blog post, there are many simultaneous processes that happen in the endoscopy lab. Of course, there are the routine colonoscopies and endoscopies, but one of the tasks that I closely observed was the pre-procedure process that the nurses perform with every outpatient. The process is described below with pain points identified below each step. The corresponding pictorial storyboard is shown above.
- Patient gets called from waiting room into lab entrance hall
- Patients get frustrated when later arrivals get called in before them
- Introductions between nurse and patient. Patient is weighed and asked if fasting, prep liquid and Covid-19 test were completed
- Missing Covid-19 test necessitates a rapid swap test, which creates a 15-20 minute delay
- Unfinished prep liquid or ingestion of solid food/nonclear liquids lead to poor procedure efficacy, delays, or rescheduling
- The nurse brings the patient to the pre-procedure bay
- The bays are small
- Environment is usually loud
- Computer carts or hospital beds make walkways more narrow
- Patient gets changed and puts belongings in bag
- Nurse asks more questions about metal in body, current medications, and allergies.
- Language barriers can make it difficult/slow to communicate
- Use of blood thinner medications make the procedure riskier
- Vitals are taken and IV is inserted
- In special cases, patients’ veins are very hard to find
- Nurse documents the patient information into their computer
- Limited computer availability in the lab
- Doctor gets consent from patient
- Language barriers can make it difficult/slow to communicate
A pain point in this process that I witnessed many times is the need to delay or reschedule a procedure. As doctors and many nurses have mentioned, one of the biggest factors impacting the lab schedule and the effectiveness of a procedure is patient preparedness. Before a patient comes in for a colonoscopy, they are instructed to be on a high fiber diet at least a week prior and a clear liquid diet the day before their procedure. In addition, they must complete a split-dose preparation liquid: one dose the previous day and one dose 6 hours before the procedure. What I have witnessed in the lab, and what many doctors and nurses sigh in disappointment about, is that so many patients eat food within 24 hours before their procedure. It is problematic because solid foods and nonclear liquids obstruct the scope’s view of the walls of the colon, which is the entire goal of a colonoscopy. Patients also forget to complete their prep liquid, which leads to amounts of bile in the colon that also obstructs view of the walls. Although patients are sent home with instructions and nurses make call reminders a few weeks before the procedure, noncompliance is still present. Given that the time between consultation and the procedure could be 5 months or even longer, it is understandable that patients forget.
In a research article from 2021 titled “Impact of Automated Time-released Reminders on Patient Preparedness for Colonoscopy,” Nayor et. al. explore the use of automated and personalized text message or email reminders in order to increase preparedness quality. In the experiment, colonoscopy patients were enrolled in automated reminders that instructed patients when to start a certain diet, when to take a dose of their prep liquid, and even when to arrive at the procedure site. These reminders were tailored to each of the patients according to their scheduled procedure date and time, as well as to the type of preparation they were prescribed. There were also attached links that brought the user to a personalized website that outlines the timeline of the procedure and provides more detailed instructions. Compared to patients not enrolled in the automated reminders, the data showed that there was a 7.7% increase of adequate preparation quality and a significant decrease of 1.8% in colonoscopy cancellations. In addition, patient satisfaction was evident as patients involved reported feelings of reassurance and care because of the reminders and check-ins.
Nayor J, Feng A, Qazi T, Hurwitz S, Saltzman J. Impact of Automated Time-released Reminders on Patient Preparedness for Colonoscopy. Journal of Clinical Gastroenterology. 2019; 53 (10): e456-e462. doi: 10.1097/MCG.0000000000001211.
Week 3: Needs Statements
By this week, I had gotten pretty familiar with the colonoscopies and endoscopies procedures, which actually made my goal of crafting a needs statement harder because like how some doctors have explained things, I often just told myself “that’s just how it’s done.” So, I tried to take a step back and just observe. Observe any inconveniences, no matter how small. During procedures, it is very easy to get fixated on the scope video on the screen and live out The Magic School Bus exploring the pink walls of the digestive system. However, peeling away from the screen and watching what doctors do with their hands throughout the procedure has led me to finding my needs statements for this week.
Before I present my needs statements, I must outline the process by which a biopsy is taken. Initially, the doctor’s left hand is holding the scope control body, which consists of knobs to control the scope tip and buttons to control air, water, and suction. Their right hand holds the shaft of the scope to apply torque and feed it into the patient’s orifice. Once the doctor finds an area or polyp that they want to take a biopsy of, they ask the technician for a tool to perform the excision (forceps or a snare). These tools take the form of a long wire with the forceps/snare at one end and a plunger at the other end that opens or closes the tool. The technician holds the plunger while the doctor lets go of the scope shaft and uses their right hand to insert the tool into a port in the scope body and feeds it through until it exits out of the tip of the scope. Once it is fully through, the doctor grabs the scope shaft again to reposition the scope to the area of interest. The doctor directs the technician to open and close the forceps/snare on the tissue. If using forceps, when the tool has a hold of the tissue, the doctor lets go of the scope shaft again and tugs on the wire to pull the sample off of the rest of the tissue. Then, the doctor and tech pull the forceps out of the port. The sample is aggressively shaken off into a biopsy cup by the technician. Once the technician confirms that all of the tissue has been released, they rinse the forceps in sterile water and the process is repeated to obtain the next biopsy sample. If using a snare instead of forceps, the doctor simply suctions the excised tissue which will be collected from a trap in the suction tubing.
The problem I observed is that the patient’s breathing and the peristaltic motion of the digestive tract shifts the position of the scope throughout the procedure. It creeps out of the patient’s orifice when the doctor lets go of the shaft to feed the tool into the port, which necessitates repositioning of the scope before taking a biopsy. This scope movement happens throughout the entire procedure, but especially when the doctor lets go of the shaft. This can get frustrating when the polyp or area of interest is in an awkward position with respect to the scope camera. Based on my observations, feeding the tool through the length of the scope can take 7-30 seconds. The following are three iterations of needs statements that I crafted, each one increasingly more effective than the last.
Needs statements:
- GI doctors experience wait time between biopsies and need more efficient tool handoffs.
- Population: GI doctors
- Specifies that the doctors are in the GI department since that is where endoscopies are performed
- Opportunity: Wait time between biopsies
- Implies that the problem is the amount of time between each biopsy
- Outcome: More efficient tool handoffs
- This points toward a solution that would improve the handing of tools from the tech to the doctor, but neglects solutions that could intervene at different points in the process. Also, “efficient” is not explicitly measurable in this situation
- Population: GI doctors
- GI doctors experience scope movement during tool handoff and need decreased time between biopsies.
- Population: GI doctors
- Opportunity: scope movement during tool handoff
- I changed this to “scope movement” instead of “wait time” to clarify that the problem is not necessarily the amount of time it takes for the tech to hand the tool to the doctor, but that the scope moves out of position while waiting
- Outcome: decreased time between biopsies
- Time is a measurable quantity. However, “biopsies” is vague since the word refers to the entire process of taking a biopsy
- GI doctors performing endoscopies experience unwanted scope movement during biopsies and need to decrease the time between tissue excisions.
- Population: GI doctors performing endoscopies
- I added “performing endoscopies” to scope into the activity that the needs statement addresses
- Opportunity: unwanted scope movement during biopsies
- Addition of the word “unwanted” clarifies that the scope movement is not beneficial and sometimes detrimental for the procedure. I also used “biopsies” instead of “tool handoff” since movement occurs throughout multiple steps of the process, not just when the doctor lets go during tool handoff
- Outcome: decrease the time between tissue excisions
- specifying “between tissue excisions” helps clarify that the time to be measured encapsulates all the steps from the moment the sample is cut out including feeding the tool in, taking the tool out, and releasing the tissue into the biopsy cup. This widens the amount of places in the process that a possible solution can intervene
- Population: GI doctors performing endoscopies
Week 4: Patents
This week in the endoscopy lab, we continued to observe more scoping procedures and paid attention to details relating to our group’s needs statements. We asked doctors about their opinions on the ergonomics of the scope control and found mixed opinions, usually dependent on their hand size. It turns out that their scopes were designed for people with bigger hands. I also talked to some fellows and nurses about the validity of my needs statement from last week. Minimizing scope movement does have potential to shave minutes off of procedure time. Their lab does not have any means to minimize that movement other than medication that slows down the patient’s digestive tract, the dexterous scoping skills of the doctor and the speed of which techs can open packaging and hand tools to the doctors.
After receiving some insight, I have tweaked my needs statement: Gastroenterologists need to minimize unwanted scope movement between polypectomy excisions in order to decrease unnecessary procedure time. I replaced “biopsy” with “polypectomy” since that is where the scope movement problem is most bothersome. The new outcome, “decrease unnecessary procedure time,” does a better job of showing the clinical value of addressing the unwanted scope movement.
When crafting this statement, I recognized that minimizing unwanted scope movement can be approached in many ways. One related patent I found is for a “Polyp retrieval assembly with separable web member” (US Patent 5486182) by inventors Naomi L. Nakao and Peter J. Wilk. The device described is essentially a cauterizing snare loop with an attached net.
As with most patents, the first claim lists the components that the device is comprised of. The following claims explain the components’ relative attachments to each other. This instrument is made up of a tubular sheath that houses a contractible cauterization loop made of conductive material which is connected to a conductive wire that extends through the sheath. The end of the wire has an electrical connector that couples to an electrical source. On the loop, there is a flexible web member that forms a pocket whose opening is defined by the circumference of the loop. The web is detachable for the major part of the loop’s circumference excluding at the distal tip. Claim 10 describes the use of the instrument. The cauterization loop and attached web is opened by sliding it out of the sheath tip. The loop is maneuvered around a piece of tissue to be cut. While closing the loop (by sliding it back into the sheath) to cut the tissue, an electrical current is sent through the cauterizing loop. Also, the web detaches from the cauterization loop except at the distal tip so that the loop is safely inside the sheath and the web is closed but remains outside and attached to the sheath.
The device satisfies my needs statement by eliminating the chance of losing the polyp after a snare excision. Multiple times I have witnessed an excised polyp drift out of view into the depths of the colon before it can be suctioned out. Searching for lost polyps adds potential minutes to the procedure. The device also reduces the amount of separate tools needed to excise and collect a polyp, thus minimizing the amount of time that unwanted scope movement can occur. When the polyp is too large to be suctioned, another tool called a roth net is necessary to surround and close upon it to capture it. In between each separate tool, the doctor must retract the previous tool and feed the next one through the scope’s tool channel. Doing this requires the doctor to let go of the scope’s insertion tube. The longer the doctor isn’t holding the insertion tube, the farther the scope tip can move out of position and the farther away a loose polyp can travel.
Link to patent: https://patents.google.com/patent/US5486182A/eninventor=naomi+nakao&oq=naomi+nakao&page=3
Week 5: Total Addressable Market
This week in the endoscopy lab was filled with more colonoscopies and upper endoscopies. Since our team has chosen to focus on scope ergonomics as the topic for our final proposal, we paid close attention to how the doctors interact with the scopes. We found that doctors have differing habits when using a scope. Some might use a second hand to turn the smaller dial while others don’t. This can be due to small hand size as the smaller dial is difficult to reach, but it is also attributable to personal preference since those with larger hands did that too. Upon further questioning, some doctors have trouble handling the scopes. Those who wore a size medium or small glove reported some inconvenience such as heavy weight of the scope or strain while reaching for the dials or buttons. Those who wore large or XL did not report any notable problems with the exception of tennis elbow in their right elbow due to the repeated motion of feeding the scope into the patient and applying torque to it.
Aside from our time in the lab, we spent our Monday lecture learning about viability, which has to do with the marketability of engineering endeavors. With that comes the concept of Total Addressable Market (TAM). TAM is the revenue opportunity available to a product/service if 100% of the market share was achieved. In order to calculate that, the following equation is used:
TAM = # of units/year * cost
To exercise this calculation, I have chosen to continue with my needs statement from last week, which is “Gastroenterologists need to minimize unwanted scope movement between polypectomy excisions in order to decrease unnecessary procedure time”
Without an actual solution finalized yet, it is impossible to have a perfect estimate for the cost to be used in the equation. Instead, I will use the cost of a snare, which is often used to perform polypectomies. Most snares cost around $20 each.
To estimate the number of units per year, I have segmented the population from total U.S. patients having a colonoscopy done to the amount of those patients who had a resulting polypectomy performed on them. As colonoscopies are recommended for everyone at age 45, over 15 million colonoscopies in the US are performed each year. Of that 15 million, polyps are found in about 43% percent of them. Even if the polyp does not look cancerous, a polypectomy is usually still performed. Since a single snare is used for each patient (even if they have multiple polyps), the number of units per year is the number of patients who are found to have polyps per year: 15 million * 0.43 = 6,450,000 snares used per year.
Using the two values found above, the calculation for TAM is as follows:
TAM = 6450000 * 20 = 129,000,000
Week 6: Final Reflections
When I first walked into the Endoscopy Lab at UIH, I remember being too nervous and excited to even know what to expect. Then, I remember being amazed by the thoroughness of the technology and processes that have been cleverly develpoed to optimize patient care. As a patient, it’s easy to take things as they are in a hospital and just let the healthcare professionals do their job. On the other hand, as a student in the Clinical Immersion Program, I got to see the minute details of how things are done up close and in depth. The chance to see medical devices in use from this perspective is a rare one and allowed me to grow my skills as an engineer.
In a class I have taken, our professor stated that projects are likely to have greater success if the engineers and stakeholders undergo communication. The Clinical Immersion Program (CIP) provided exactly that. It opened up space for questions and conversations with the users of medical devices, giving me an important perspective on the current challenges that exist in the endoscopy lab. The nature of gastroenterology procedures as being heavily reliant on medical devices and the dexterous skill of doctors, technicians, and nurses made it quite interesting to observe and provided multiple topics to explore. Although our final proposal was centered on scope ergonomics, we also got to investigate opportunities for innovation in performing biopsies, polypectomies, and increasing patient preparedness.
Something important I learned is that medical technology that is in need of innovation is not inherently “bad.” They don’t always present themselves as blatant problems waiting to be fixed. Rather, opportunities to innovate are hidden in everyday practices and masked by workarounds and acceptance of traditional ways. Once you get past superficial observations, you can recognize the numerous opportunities to somehow make something more efficient or convenient. As an engineering student, getting to practice the process of identifying needs was a valuable experience. I learned how to observe closely and ask the right questions to find needs that might not have crossed my mind otherwise.
A piece of advice I would give to future CIP students is don’t be afraid of asking questions. It’s something I’ve heard repeatedly throughout all of my years in school, but as a BME student, it is easy to feel out of place in a clinical environment. It is difficult to know when to ask and when not to interrupt. However, know that UIH is a teaching hospital. Every person I have asked a question to has been happy to answer. Additionally, talk to more than just the doctor. Talk to the nurses, technicians, medical assistants, and really anyone else who works there. Every person has a unique perspective and offers helpful insight.
Finally, I’d like to thank everyone who played a part in making the past six weeks possible! It was engaging, insightful, and also really fun. Thank you to Dr. Mutlu for allowing us to enter and explore the GI department. Additionally, thank you to everyone in the GI department for meeting us with welcoming and kindness. Thank you to Dr. Felder and Dr. Browne for making this program possible and teaching and guiding us every week. Finally, thank you to my group members Lana Khadra, Klaudio Haxhillari, and Jeremy Yuan for your teamwork and insight throughout the program.