
Yesui Delgermunkh
4th Year Biomedical Engineering Student
Biomedical Engineering, Ophthalmology
Pronouns: She/Her
Email:
Week 6: Final Post
As my time in the ophthalmology clinic ends, I want to reflect on the invaluable lessons learned throughout the program. The interactions with patients, the insights gained from observing healthcare professionals, and the challenges faced in the clinical environment have collectively shaped my understanding of the complexities involved in providing quality care. Here are key lessons and recommendations for future Clinical Innovation Program (CIP) participants.
- One of the most significant insights was recognizing the need for ergonomic workstations for ophthalmologists. Long clinic hours often lead to physical strain and decreased productivity. An ergonomic setup can enhance comfort, reduce fatigue, and ultimately improve patient care by decreasing wait times.
- Observations revealed that extended wait times directly impact patient satisfaction. Patients expressed frustration, and this, in turn, affected staff morale. Efficient clinic operations are essential not only for patient care but also for maintaining a positive work environment for healthcare providers.
- The clinic’s reliance on technology, from the use of advanced surgical systems to electronic health records, underscored the need for seamless integration. The inefficiencies caused by constant log-ins and data retrieval during patient consultations can hinder productivity. Streamlining these processes is vital for improving patient flow and clinician efficiency.
- Engage with the technicians and patients to understand their experiences and challenges. Their feedback is invaluable in developing solutions that cater to their needs, particularly regarding discomfort during examinations. The doctors only see things from their perspective. Take the initiative to shadow everyone not just the doctor you are assigned to so you can get a better and thorough understanding of the clinic.
- Feasibility and viability are huge factors that sometimes we forget about because we’re too focused on the desirability Just because we need something does not mean it can be made, especially by a group of senior design students. Evaluating the practical aspects of implementing solutions was a crucial lesson. The realization that our initial proposals must consider available resources and existing constraints significantly refined our approach. In addition, the economic sustainability of proposed solutions is a key consideration. It can be difficult to see it all on a day-to-day basis, but it is important to constantly consider both the viability and feasibility.
Week 1: Good and Bad Designs

Our first week in the clinic has been primarily getting more comfortable in the environment. As someone who has worn glasses my entire life, it has been very interesting getting to see the eye doctor’s office from a different perspective.
Good design: One good design we saw was the handheld slit lamp. The slit lamp is the primary instrument used when examining the patients in the ophthalmology clinic. Unfortunately, it is a rather large instrument and is supported by and connected to a stationary platform. For patients who could not be moved to the chair, which we saw with patients in wheelchairs, a portable and handheld slit lamp was used.
A: Observing the use of handheld slit lamps for patients in wheelchairs.
E: Ophthalmology clinic with stationary and portable slit lamps.
I: Interactions patients in wheelchairs and doctors using handheld slit lamps.
O: Handheld slit lamp for examining patients. Stationary slit lamp.
U: Patients in the clinic. Ophthalmologists performing examinations. The observer (aka me).
The smaller version has all the main features as the original. However, some downsides are that they may have slightly lower quality optics compared to stationary models and typically offer fewer magnification options and simpler imaging capabilities. In addition, adjustments can be more limited compared to stationary models.
Bad design: On Tuesday, I had the opportunity to visit the operating room. The doctors used a device called the Constellation Vision System which was used to aid during the surgery. The CONSTELLATION® Vision system is an ophthalmic microsurgical system that can be used for both anterior (removal of cataracts) and posterior(vitreoretinal) ophthalmic surgeries.
A: Visiting the operating room. Witnessing a surgery involving the Constellation Vision System.
E: The operating room during surgery.
I: Interaction between the doctor and the Constellation Vision System using foot pedals. Doctor’s interactions with the scrub nurse to manually adjust device settings.
O: Constellation Vision System for ophthalmic surgeries. Foot pedals for controlling the Constellation Vision System.
U: Ophthalmologists performing surgeries. Scrub nurse assisting in the operating room.
In one surgery, while attempting to remove a fragment from the back of the eye, the doctors used a setting for fragmentation. Whether it was on or off was controlled by the foot pedals for the device. One major annoyance was that due to the nature of the fragment, it was very difficult to keep on the suction device. As such, fragmentation switched from on to off every time the fragment was grabbed and then dropped which occurred quite a bit. Similar to the idea of alert fatigue, after a few times, it became rather annoying. Alert fatigue is a phenomenon where individuals become desensitized to warning signals due to the excessive number of alerts they receive. This often leads to longer response times or even the complete disregard of alerts.
Another issue was that the doctor had to ask whether fragmentation was on or off every time she moved or stopped for some time. This was an overarching issue with the various settings of the device – the doctor continuously had to ask the scrub nurse what the pressure was, if the infusions were on, etc. and then have it changed manually. This delays the scrub nurse in fulfilling other duties they may have, as they have to stop and take time to change it manually while the doctor waits for the next instrument they asked for. I wonder if it would be possible to have the machine decipher the doctor’s commands using AI, similar to voice-to-text.
Overall, the opportunity to be with different doctors throughout their days has been a wonderful learning experience and everyday, I feel more and more comfortable with the general environment as well as asking more questions.
Week 2: Secondary Research and Patents
In ophthalmology, the surgeons often remain seated for precision, stability, and comfort. Eye surgeries require extraordinary accuracy so being seated with the arms stabilized by a support aids in minimizing hand tremors and enhancing control over the delicate structures of the eye. Any minor movement or error during these surgeries could cause complications. In addition, the operating microscopes used require alignment with the surgeon’s eyes. This means the surgeon typically cannot move or look away from the scope throughout the surgery. As a result, the surgeon needs to use foot pedals for everything else they need to control during the surgery. This can be as simple as adjusting their seat’s position or controlling surgical instruments and devices.
One of the major uses of these foot pedals that we observed in the OR was during vitrectomies. The foot pedals are typically multifunctional, allowing the surgeon to perform several tasks without looking away from the surgical field or using their hands. One of the main functions is controlling the vitrector, a device used to cut and remove the vitreous gel; utilizing the foot pedal, the surgeon can modulate the suction and cutting speed. The foot pedals can also be used for changing the intensity and focus of the lights, maintaining intraocular pressure and volume, and adjusting the focus, zoom, and position of the microscope.
Although there are many types of foot pedals for ophthalmology, two commonly used ones are the conventional foot-pedal control and the dual-linear foot-pedal control. The conventional foot-pedal control operates in a single plane (pitch), managing only the ultrasound power. In this system, phacoemulsification starts after achieving full vacuum pressure, with the foot pedal solely modulating the phaco power. This setup uses a gravity infusion system with an infusion bottle height of 70-80 cm, offering simplified control for the surgeon who needs to manage just one variable.
In contrast, the dual-linear foot-pedal control functions in two planes (pitch and yaw). This allows the surgeon to independently control both the ultrasound power (pitch) and vacuum (yaw), providing three-dimensional control over the surgical process. This dual control facilitates more precise movements, such as increasing vacuum pressure to move the nucleus towards the phaco tip and then applying moderate vacuum pressure for emulsification. The dual-linear system also features adaptive fluidics, which automatically monitors and adjusts vacuum flow rate and infusion pressure, with a lower infusion bottle height of 65 cm. This enhanced control can improve the efficiency and safety of ultrasound energy delivery.
The study by Kim, Seong, and Rho aimed to compare the safety and efficacy of dual-linear versus conventional foot-pedal control in cataract surgery (1). With a cohort of 94 patients or 188 eyes, each patient underwent cataract surgery in both eyes, one with the dual-linear (study group) and the other with the conventional foot-pedal control (control group). The researchers analyzed the phacoemulsification parameters such as average phaco power (the amount of ultrasound energy used to break up the cataract) and effective phaco time (the total time the ultrasound is actively used during the procedure), and surgical complications. They found that the average phaco power and effective phaco time (EPT) were higher in the dual-linear group. Despite this, safety outcomes, including endothelial cell loss, central corneal thickness, and surgical complications, were comparable between the two groups. The dual-linear system’s ability to independently modulate vacuum and ultrasound power potentially offers improved surgical precision and safety compared to the conventional foot-pedal control, though both systems showed similar safety profiles in the study.
Although overall ophthalmological foot pedals have a variety of great mechanisms, as we saw last week and again this week, they still do not encompass everything the surgeon needs to do. The surgeon still needs to be in communication with the scrub nurses to change the settings on the vision system when switching to a different method. Miscommunication with the nurse could lead to medical errors that could’ve been avoided if the surgeon had direct control of the machines.
Patent 11617682 for an ophthalmological foot pedal device with force feedback describes a pedal designed to enhance the precision and control of foot pedal devices used by ophthalmic surgeons during surgery (2). The foot pedal device includes a movable member whose movements are registered by a sensor and processed by a computer. The device provides force feedback, such as resistance or stopping force, in response to specific surgical parameters or conditions detected by the surgical console. By offering resistance when certain thresholds are reached or when non-optimal values are detected, the device aids in maintaining precision and accuracy. The force feedback mechanism can be configured to provide varying levels of resistance depending on the specific needs of the procedure, ensuring that surgeons can make fine adjustments with greater confidence and stability. The device’s ability to adapt to different operators through calibration further enhances its usability and effectiveness in delicate ophthalmic surgeries. Improvements to the foot pedal design can lead to a decreased chance of error and overall a better surgical experience for the doctor, nurse, and patient.
[1] Kim, H., Seong, J., & Rho, C. (2024). Comparison between early clinical results of dual-linear and conventional foot-pedal control in phacoemulsification. Journal of Clinical Medicine, 13(3), 693. https://doi.org/10.3390/jcm13030693
[2] Ophthalmic surgery foot pedal device having force feedback. Justia. (2019, May 10). https://patents.justia.com/patent/20190350757
Week 3: Need Statements
On one of the clinic days, the patient we saw at around 8:10 am had been there since 6:30 am. Multiple patients throughout the last few weeks have complained about wait times, with patients stating they had been waiting over an hour without even being called to see the technicians. Not only are the patients complaining, but the staff are frequently frustrated and the doctors are constantly worrying about being too “behind.”
To see multiple patients without too much time spent in between, doctors rotate between 3 rooms usually. As such, they constantly have to log on to the computers each time they go into a new room, pull up the charts, read it, look at the images, etc. all while the patient is in the room. This takes up a lot of valuable time that could be used with the patients and speed up the process.
At the University of Florida, the first visit to the ophthalmologist can be very comprehensive, taking one and a half hours, possibly longer for specialized testing or complex issues (1). The visit starts with an in-depth medical history and filling out forms, available online. Visual acuity, refraction, eye muscle coordination, pupil response, and peripheral vision will be tested. A slit lamp exam and intraocular pressure check are performed, and most exams include eye dilation to examine the internal health of your eyes. Additional tests may be conducted based on initial findings. After the exam, the ophthalmologist will discuss the results and answer questions. This is typically repeated between techs, residents, and attending physicians possibly repeating the same steps.
With long wait times, patient satisfaction decreases quickly, “In a survey of ophthalmology patients, those who were “not completely satisfied” waited twice as long as those who were “completely satisfied.” Length of waiting time had the most impact on the overall satisfaction score.” (2).
Enhancing productivity overall in the clinic results in happy patients and a better work environment for the physicians, techs, and others involved.
NS1: Ophthalmologists need ergonomic workstations to enhance productivity during long hours of patient care and surgeries.
- P: Ophthalmologists
- O: Need ergonomic workstations
- O: Enhance productivity
One commercial product currently on the market is the Ergotron CareFit Slim 2.0 (3). According to the manufacturer’s website, it features a sturdy platform that supports large all-in-one computers and monitors up to 27 inches and 20 lbs. Its ergonomic design accommodates clinicians of all heights, offering simple height adjustment for full sit-to-stand functionality. The lean design fits tightly against walls to save space when not in use, and it is easily customizable with a broad range of accessories for specific workflows. At OfficeDepot, it can be purchased for $2398.04.
The number of ophthalmology clinics in the United States is approximately 1,715 (4). As such, let’s approximate and say that each clinic needs at least 3 workspaces at a time. The TAM is at least 12.3M (1,715*3*2,398.04).
NS2: Ophthalmologists need ergonomic workstations to minimize physical strain during long hours of patient care and surgeries.
- P: Ophthalmologists
- O: Need ergonomic workstations
- O: Minimize physical strain
- Rationale for change: Starting your workday with a setup that feels tailor-made for your comfort can make everyone happier. Addressing ergonomic issues from the get-go isn’t just about immediate relief—it’s a proactive approach to safeguarding your long-term health. By maintaining natural body positions and making personalized adjustments, ergonomic solutions not only enhance comfort but also sustain your mobility over time. Whether it’s adjusting your chair height or finding the perfect keyboard angle, these small changes can make a big difference in how you feel throughout the day. It’s about investing in your well-being, ensuring that every moment at your workstation supports your specific needs and keeps you feeling your best, day after day.
NS3: Ophthalmologists need ergonomic workstations to enhance collaboration during long hours of patient care and surgeries.
- P: Ophthalmologists
- O: Need ergonomic workstations
- O: Enhance collaboration
- Rationale for change: Imagine a workspace where comfort meets collaboration effortlessly. Ergonomically designed flexible spaces not only adapt to your work style but also make team projects a breeze. Picture easily reconfigurable setups that encourage seamless teamwork, where every adjustment is a step towards a more comfortable and productive environment. Shared resources like adjustable tables ensure that everyone can find their ideal setup, promoting a sense of unity and efficiency among team members. In such a workspace, ergonomic design isn’t just about comfort—it’s about creating an environment where collaboration thrives, making every day at work a little more enjoyable and productive for everyone involved.
[1] What to expect at your appointment for adults UF Department of Ophthalmology. (n.d.). https://eye.ufl.edu/patient-care/what-to-expect-at-your-appointment/
[2] Williams, R. D. (2020, October 30). How long would you wait?. American Academy of Ophthalmology. https://www.aao.org/eyenet/article/how-long-would-you-wait
[3] CareFit slim medical computer cart on Wheels. Ergotron. (n.d.). https://www.ergotron.com/en-us/products/product-details/c50-3500/
[4] (2024, May). Eye Surgery Clinics in the US. OD4159. Retrieved from IBISWorld database.
Week 4: More Need Statements
Revised NS: Ophthalmologists need ergonomic workstations to enhance productivity during long clinic hours to decrease patient wait times.
My original needs statement did not have a measurable outcome. We narrow our solution space by updating it to add “to decrease patient wait times” and specifying the need statement for the clinic.
Let’s break this down to the three components of IDEO (desirability, feasibility, and viability).
- Desirability: Desirability focuses on the solution’s appeal to the end users: ophthalmologists and their patients. Ergonomic workstations here can be desirable to ophthalmologists as they cut out repetitive and unnecessary steps they may have had to do. It helps to streamline the process of seeing patients in the clinic. Overall, enhanced productivity can lead to a more efficient work environment, positively affecting the morale and job satisfaction of the entire clinic staff. Adding the measurable outcome of decreasing patient wait times makes the statement more compelling. Patients will benefit from shorter wait times, leading to higher satisfaction and a better overall experience.
- Feasibility: Feasibility evaluates whether the solution can be realistically implemented given the available resources and constraints. Specifying the need for the clinic narrows down the application scope, making it more practical to design and implement workstations tailored for clinical use. In addition, it can help with integrating the technology already in use in the clinic to further enhance productivity, which aligns well with the needs of ophthalmologists for efficient patient care.
- Viability: Viability concerns the economic sustainability of the solution over the long term. Decreasing patient wait times can lead to higher patient throughput, potentially increasing the clinic’s revenue. Improved patient satisfaction due to shorter wait times can lead to higher patient retention rates and attract new patients through positive word-of-mouth, contributing to the clinic’s financial stability. The initial investment in ergonomic workstations could be justified by long-term financial gains. Furthermore, enhancing productivity during long clinic hours means more efficient use of time and resources, reducing operational costs in the long run.
—
In the last 2 weeks, I have been seeing a lot more pediatric patients in the clinics. Pediatric patients, especially those who are under the age of 10 struggle heavily with the bright lights needed during a regular ophthalmology clinic visit. Although this does not only occur in pediatrics, I’ve seen it more often recently as we have been seeing more pediatric patients. For one patient, in particular, the doctor had to check their eyes with an ultrasound rather than the indirect ophthalmoscope. The doctor saw that the patient may have a retinal detachment but because he could not look at the patient’s retina, he could not be 100% sure.
According to research, ultrasounds provide images with lower resolution, making it difficult to detect fine details and subtle pathologies. It also requires a skilled operator to obtain and interpret images correctly, leading to potential inconsistencies in diagnostic accuracy. Additionally, ultrasound offers a two-dimensional image, limiting the ability to fully assess the three-dimensional structure of the retina and vitreous body. This limitation can make it challenging to detect and accurately characterize certain retinal conditions, such as subtle retinal tears or early-stage macular diseases.
New NS: Patients who are sensitive to direct light require alternative retinal examination methods to accurately diagnose and monitor retinal conditions without causing discomfort or distress.
Week 5: Storyboard
NS: Ophthalmologists need ergonomic workstations to enhance productivity during long clinic hours to decrease patient wait times.
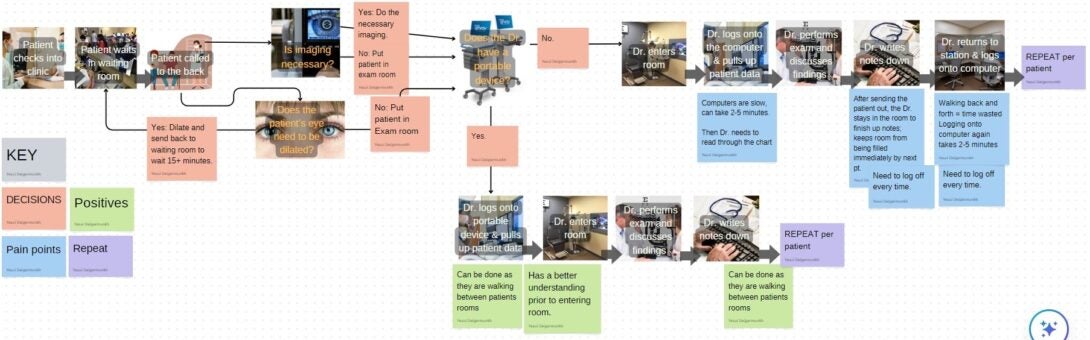
This week, we created storyboards for our needs statement, a critical step in the project planning process. This storyboard allowed me to visually map out the key elements of the needs statement. Breaking it down into visual segments helped me organize my thoughts and see the bigger picture. This approach not only deepened my understanding of what the project truly needs but also gave me a handy tool to share with my team.
About
Incoming senior majoring in Biomedical Engineering with a concentration in Bioinformatics and minor in Computer Science.