
Rohith Erukulla
Second Year Medical Student (M2)
Ophthalmology
Email:
Final Need
While rotating in various specialties of the ophthalmology department, I determined many clinical needs, some of which I have discussed in previous posts. However, the largest problem I found has to do with the limitations of imaging methods when a patient’s eye has media changes (corneal, lens, or vitreous changes like cataracts or vitreous hemorrhage that block visualization of the retina). About 10% of retinal patients have some kind of medial opacity complicating retinal view. In such circumstances, ophthalmologists face challenges in viewing the retina clearly. Sometimes, cataract removal or vitrectomy may be performed just to get a clear view of the retina. Additionally, endoscopic vitreoretinal surgery may have to be performed if retinal view cannot be acquired, and this procedure carries more risks. This necessitates an alternative examination method to increase the frequency and certainty of in-clinic diagnosis. I discuss my research about this problem and the formulation of a needs statement below.
Needs Statement: Ophthalmologists require a method to provide clear, high-resolution imaging of the retina that is not hindered by media opacities (e.g., dense cataracts, vitreous hemorrhage).
Current Imaging Modalities:
Slit Lamp:
- Advantages: High-resolution imaging of anterior and posterior segments, accessible in clinics.
- Limitations: Limited view of the peripheral retina, obstructed by dense cataracts, vitreous hemorrhage.
Indirect Ophthalmoscope:
- Advantages: Provides a wide-field view, useful for detecting peripheral lesions.
- Limitations: Requires skill and clear visual pathways, obstructed by opacities.
Optical Coherence Tomography (OCT):
- Advantages: High-resolution cross-sectional images, useful for macular pathologies.
- Limitations: Ineffective with dense media opacities.
B-Scan Ultrasound:
- Advantages: Visualizes the posterior segment when direct visualization isn’t possible, useful for detecting pathologies like retinal detachments.
- Limitations: Lower resolution, does not provide sufficient information for clinical action in about 80% of cases with medial opacities.
Total Addressable Market (TAM)
The TAM for retinal imaging solutions addressing obstructions is based on the prevalence of relevant conditions and the cost of exams per patient.
Population and Prevalence:
- US Population: 333.3 million
- Retinal Pathology Prevalence: 0.13% per year
- Retinal Blockage Prevalence: 1.15% per year
- Combined Prevalence: (0.13% * 1.15%) * 333.3 million = 438,180 patients per year
Cost of Exams per Patient (Amount per year varies by individual and condition but is estimated here):
- Retinal Exams: $270 each, 4 per year
- B-Scan Ultrasound: $375 each, 2 per year
- OCT: $41.81 each, 2 per year
- Total Cost per Patient: ($270 * 4) + ($375 * 2) + ($41.81 * 2) = $1913.62
TAM Calculation:
- TAM: 438,180 patients per year * $1913.62 per patient = $841 million
ICD and CPT Codes
CPT Codes:
- 92002: Intermediate-level ophthalmological evaluation of a new patient, facility price $44.61
- 92012: Intermediate-level eye exam of an established patient, facility price $49.27
ICD-10 Codes:
- H33, H34, H35, H36: Retinal detachments, retinal vascular occlusions, other retinal disorders
- H17: Corneal scars and opacities
- H43: Vitreous body disorders
- H25, H26: Cataracts
Summary
Patients with media changes such as dense cataracts or vitreous hemorrhage require alternative imaging methods for effective retinal visualization. Current solutions like slit lamps, indirect ophthalmoscopes, OCT utilize visible light or infrared, which is easily blocked, reflected, or scattered. B-scan ultrasound is low resolution and can display too much noise. The need for a reliable, high-resolution imaging method that can penetrate media opacities is clear. The estimated TAM for such a solution in the US is $841 million, emphasizing a market potential for innovative diagnostic tools.
Week 1: An Analysis of Ophthalmic Medical Devices
I shadowed ophthalmologists in various subspecialties during the first week of the Innovation Medicine Clinical Immersion Program. In particular, I shadowed ophthalmologists specializing in the retina, cornea, uveitis, and dry eye related to autoimmune conditions. I focused on analyzing the usability, efficiency, and patient comfort of the various machines that are used to diagnose and treat eye conditions. One bad design and one good design that I have chosen to highlight are discussed below:
Bad Design: iTrace Aberrometer or Topographer
Activities: The iTrace machine combines wavefront aberrometry and corneal topography to provide detailed analysis of the eye’s optical system. A technician performing an eye exam can use the iTrace machine in order to collect vision data, including refractive error, astigmatism, and other corneal curvature measurements.
Environment: Used in eye clinics. Observed in the Dry Eye and Graft vs. Host Disease Clinic at the Illinois Eye and Ear Infirmary.
Interactions: The technician asks the patient to place their head in the rest and takes measurements for each eye. The technician mentioned that the patient’s nose often hits the machine, so they have to awkwardly tilt their head.
Objects: iTrace Aberrometer and Topographer with integrated software for capturing and analyzing eye measurements
Users: The technician directly controlled the iTrace system, while the ophthalmologist relied on the data provided by the system for diagnostic and treatment planning.
Good Design: LipiView II Ocular Surface Interferometer
Activities: The LipiView is used to assess the lipid layer of tears and the morphology of meibomian glands to diagnose dry eye conditions.
Environment: Typically used in ophthalmology clinics specializing in dry eye management. Observed in the Dry Eye and Graft vs. Host Disease Clinic at the Illinois Eye and Ear Infirmary.
Interactions: The technician instructs the patient to place their chin on the chin rest, aligns the device, and captures images of the tear film.
Objects: LipiView device with integrated software for imaging the tear film and meibomian glands.
Users: The technician operates the LipiView system, capturing images for analysis. Ophthalmologists rely on these images to diagnose and plan treatments for dry eye conditions related to lipid deficiency.
Week 2: Handheld Ophthalmoscopes

This week, I rotated through the Dry Eye Clinic, pediatric retina, oculoplastics, and neuro-ophthalmology. A key theme I have noticed in the last two weeks is that many of the ophthalmoscopy techniques require great hand stability, which can make it difficult to look at the retinas of patients who do not hold still or who have small pupils. This can result in blurry images, making it difficult for the ophthalmologist to properly diagnose, monitor, and treat the patient’s condition. Additionally, aspiring ophthalmologists have a hard time gaining proficiency with handheld devices and the slit lamp due to the practice required to gain adequate hand stability.
I perused existing literature regarding different ophthalmoscopic methods, and I found a very good review article that discusses the different existing ophthalmoscopic devices [1]. Screening for retinal conditions requires expensive equipment and trained personnel, which can especially provide a challenge in low-resource settings. However, many smartphone-based fundus photography devices have been developed with consideration of image quality, diagnostic accuracy, and ease of use. When combined with artificial intelligence algorithms, these devices can even be used by untrained individuals to detect retinal disease with high sensitivity and specificity. Additionally, these devices are cost-effective and portable. Many of these devices are designed to be propped up on the patient’s head, so great stability and training is no longer needed for operation (See image from [1]). Additionally, they utilize smartphones, which are readily accessible in many environments. Yet, these devices are limited due to decreased and variable image quality.
After looking at existing ophthalmoscopes, I chose to further research the Remidio FOP NM-10. The Remidio FOP NM-10 is designed to visualize non-dilated eyes, making fundus examination more comfortable, convenient, and accessible. The device is also very portable and can be attached to a smartphone, making it easy to transport and use in various settings, from clinics to community health camps. However, the Remidio FOP NM-10 also has some drawbacks. The quality may not always match traditional fundus cameras, which could affect diagnostic accuracy. Additionally, the non-mydriatic nature of the device may not be as amenable for patients with smaller pupils or specific retinal conditions that require more detailed imaging. Yet, this device still may be easier to use for untrained individuals and can be utilized for many patients. The Remidio FOP NM-10 is protected by several patents, including US Patent No. 10,918,489, which covers the device’s method and apparatus for non-mydriatic retinal imaging, and US Patent No. 10,168,924, which details the system and method for capturing retinal images using a smartphone.
1. Naz, H., Nijhawan, R. & Ahuja, N.J. Clinical utility of handheld fundus and smartphone-based camera for monitoring diabetic retinal diseases: a review study. Int Ophthalmol 44, 41 (2024). https://doi.org/10.1007/s10792-024-02975-4
Week 3: Indirect Ophthalmoscope
This week, I rotated more through the various ophthalmology specialties and focused on interviewing attendings, fellows, and residents in order to determine challenges they face in their practice. The most common difficulty I both heard and observed was from residents and fellows, who said that the indirect ophthalmoscope is a difficult tool to use. Based on this, I did secondary research on indirect opthalmoscopes and indirect ophthalmoscopy trainers and their efficacy. I then determined the total addressable market for this problem and crafted two iterations of clearly defined needs statements.
Primary Observation:
- I spoke to a retinal specialist said it took him over 5 years before he was skilled with the indirect ophthalmoscope. He almost said that even many attendings are not very good at using the indirect ophthalmoscope.
- I also observed residents and fellows have trouble using the device multiple times and sometimes needing to call the attending, especially for patients with smaller pupils
Technical Secondary Research:
- Simulators and trainers exist to help ophthalmologists-in-training learn to use the indirect ophthalmoscope
- The main models for indirect ophthalmoscopy training simulation include an eyeball model, a plastic canister model, and VR [1]. While there is a lack of evidence regarding the efficacy of the eyeball and plastic canister models, augmented reality (AR) trainers such as the EyeSI AR BIO simulator have been shown to result in significant improvement in indirect ophthalmoscope usage [2].
Business Secondary Research:
- Keeler Vantage Plus LED Digital Indirect Ophthalmoscope
- The Keeler Vantage Plus LED Digital Indirect Ophthalmoscope headgear costs around $4,000. This device includes LED illumination for a clearer view and digital imaging. The headgear is comfortable to wear for extended periods. However, the high cost makes it less accessible, and the digital features might introduce a steeper learning curve. Additionally, it requires regular charging and maintenance. Lenses such as the Volk 20D or 28D, commonly used with this headgear, can cost between $300 and $600 each.
- Heine Omega 500 Indirect Ophthalmoscope
- The Heine Omega 500 headgear costs approximately $3,200. It features LED illumination, a lightweight and ergonomic design, and a fully adjustable headband. Advantages include bright, uniform illumination with LED technology, excellent optical clarity, and comfortable wear for prolonged use. However, it is expensive, and there is a period of familiarization required to master its use effectively. Lenses like the Heine 20D or 30D, used with this headgear, typically cost between $400 and $600 each.
- Eyeball Model Trainer
- The Eyeball Model Trainer costs approximately $300. It simulates realistic eyeball anatomy and includes adjustable pupil sizes. Compatible with standard indirect ophthalmoscopes, it provides a straightforward and cost-effective training tool. Its advantages include offering hands-on practice for trainees and being reusable for multiple practice sessions. However, it is limited to basic anatomical simulation and does not fully replicate the dynamic nature of a live examination. Additionally, it lacks the ability to provide feedback on technique or performance.
- EyeSI AR BIO Simulator
- The EyeSI AR BIO Simulator, priced at about $50,000, utilizes augmented reality (AR) to create an immersive training experience. It provides real-time feedback and performance metrics across a variety of clinical scenarios and pathologies, with high-fidelity graphics enhancing the experience. The primary advantages include comprehensive training through realistic scenarios, immediate feedback for technique improvement, and extensive practice opportunities in a safe, controlled environment. However, its high cost significantly limits accessibility, and it requires specialized equipment and setup. Moreover, despite its advanced features, it may not fully replicate the physical feel of using an actual ophthalmoscope.
Total Addressable Market (TAM):
- Potential users: 18,000 ophthalmologists
- Estimate an institution has 1 for every 2 ophthalmologists (0.5 units per user) and that the device is replaced every 5 years (0.2 units per year)
- Cost of indirect ophthalmoscope with lens kit: $5,500
- TAM = 18,000 * 0.5 * 0.2 * 5,500 = $9,900,000
Needs Statement Iteration 1: The indirect ophthalmoscope requires a high level of physical stability and extensive practice, often taking up to 5 years for proficiency, making it a challenging tool for many ophthalmologists to master.
- Population: Ophthalmologists, especially those in training
- Opportunity: The indirect ophthalmoscope requires a high level of physical stability and extensive practice, often taking up to 5 years for proficiency, making it a challenging tool for many ophthalmologists to master.
- Outcome: Enhanced ease of use and proficiency in using the indirect ophthalmoscope, leading to improved diagnostic accuracy and patient care.
Needs Statement Iteration 2: Ophthalmologists-in-training face difficulty and frustration due to the indirect ophthalmoscope’s design, which requires significant hand, arm, and head stability and up to 5 years to properly learn, leading to reduced quality of care and longer appointment times for patients.
- Population: Ophthalmologists, especially those in training
- Opportunity: The current indirect ophthalmoscope design requires significant hand, arm, and head stability and a long learning curve, posing challenges and causing frustration for ophthalmologists-in-training.
- Outcome: The current design makes it very difficult for aspiring ophthalmologists to learn and use, resulting in worse quality of care and longer appointments for patients.
- Rationale for Changes: The second iteration clarifies the type of stability that is needed for indirect ophthalmoscopy. It also provides more information on the outcome, describing the frustration and difficulties associated with the learning curve and how they can lead to longer appointments for patients.
- Rai AS, Rai AS, Mavrikakis E, Lam WC. Teaching binocular indirect ophthalmoscopy to novice residents using an augmented reality simulator. Canadian Journal of Ophthalmology. 2017;52(5):430-434. doi:10.1016/j.jcjo.2017.02.015
- Ricci LH, Ferraz CA. Simulation models applied to practical learning and skill enhancement in direct and indirect ophthalmoscopy: a review. Arq Bras Oftalmol. 2014;77:334-338. doi:10.5935/0004-2749.20140084
Week 4: Indirect Ophthalmoscope Revised and Neck Strain
This week, I focused on identifying more clinical problems faced by healthcare workers in ophthalmology. I started by gathering insights from fellows and residents about their difficulties with the indirect ophthalmoscope. Based on this feedback, I revised last week’s needs statement to more accurately reflect the problem. Additionally, I wrote a needs statement addressing another issue: the significant neck strain that ophthalmologists experience throughout their careers, which can lead to musculoskeletal health problems. Many experienced ophthalmologists reported neck pain, and one fellow emphasized that during exams, it’s crucial for ophthalmologists to consider their own comfort as well as the patient’s, as they will be performing these exams for years while the patient will only be involved for a few minutes.
Indirect Ophthalmoscope
Needs Statement: Due to the technical motor and stability skills required to effectively use the indirect ophthalmoscope, ophthalmologists-in-training face need to a method to decrease indirect ophthalmoscope learning difficulty and increase ease of use.
- Population: Ophthalmologists, especially those in training
- Opportunity: The current indirect ophthalmoscope design requires significant hand, arm, and head stability and a long learning curve, posing challenges and causing frustration for ophthalmologists-in-training.
- Outcome: The current design has a large learning curve. A solution would decrease learning difficulty and increase ease of use.
- Rationale for Changes: The new version of the needs statement is much more concise. It describes the difficulties in using the indirect ophthalmoscope better and removes unnecessary words. Additionally, the outcome was changed in order to agree with the population (ophthalmologists-in-training) rather than describe effects on the patients.
Neck Strain
Needs Statement: Due to the repetitive head positions during ophthalmic examinations, ophthalmologists need a method to reduce neck strain and long-term musculoskeletal injury.
- Population: Ophthalmologists
- Opportunity: The repetitive, sustained head positions required of ophthalmologists during exams throughout their career lead to neck strain, resulting in discomfort, pain, and potential long-term musculoskeletal issues.
- Outcome: The current environment contributes to significant neck strain. A solution would ideally reduce neck strain, enhance comfort, and promote long-term musculoskeletal health for ophthalmologists.
Week 5: Neck Strain in the Day of an Ophthalmologist
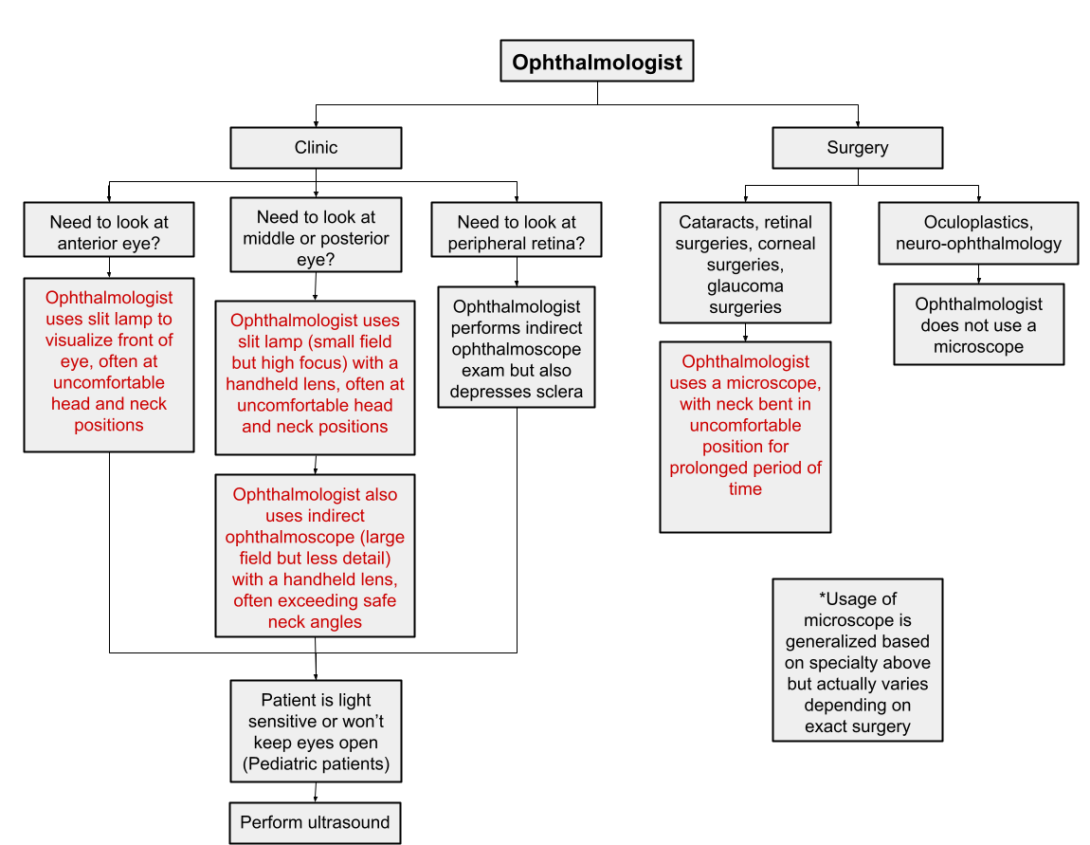
This week, I especially focused on the neck strain that ophthalmologists occur in their regular workday. I asked attendings, fellows, and residents, about neck strain, and a few noted having constant neck pain and/or discomfort. Most ophthalmologists agreed that long surgical days lead to neck discomfort due to having to look through a microscope for a prolonged period of time. Many also mentioned that the indirect ophthalmoscope and even slit lamp sometimes call for uncomfortable head, neck, and back positioning. I created a flow chart to detail my findings about the general procedures that an ophthalmologist does and when they encounter neck strain.
About
Rohith Erukulla is a dedicated MD candidate at the University of Illinois College of Medicine, where he combines his extensive background in biomedical engineering and clinical neuroscience with his passion for ophthalmology and neurology. With a B.S. in Biomedical Engineering from UIC and an MSc in Clinical and Therapeutic Neuroscience from Oxford University, he has conducted impactful research on retinal disorders, keratoconus, corneal nerve regeneration, and cognitive outcomes related to insulin resistance. Rohith's commitment to advancing medical knowledge and improving patient care is reflected in his diverse research projects and active involvement in professional organizations including the CommunityHealth free clinic, New Life Volunteering Society, and Ophthalmology Interest Group.