
Klea Hondro
Student Participant
Division of Cardiology | Department of Medicine | Heart Center University of Illinois
Email:
Week 1: Good Designs vs. Improvements
The first week of the clinical immersion program was packed full of running after doctors for inpatient cardiology appointments, being part of different labs and echo procedures. The start of this program can sometime feel like taking a sip of water from a fire hydrant because there is an entirely new terminology and environment you are being exposed to, yet it feels like a humbling and exciting experience.
After our first meeting with Dr. Erik Wissner, Director of Cardiac Electrophysiology, he introduced us with a tour of the cardiology department. From there we headed to the outpatient clinic care center where we followed him to different appointments that he had scheduled throughout the first day. The second day we observed different procedures that were taking place in the eco lab and the last couple of days we were introduced to different methods in the EP and Cath Lab where we saw procedures such as ablations, thrombectomies, and transesophageal echocardiogram (TEE). While trying not to get in the way of the staff, we kept asking questions, taking notes, and documenting moments while trying to prioritize user needs and identify some of the potential problems in the cardiology department.
Good design: Inari FlowTriever
Among the other procedures that we experienced, the FlowTriever was designed to extract large volumes of blood clots while limiting blood loss. A guidewire was advanced past the target clot in the pulmonary artery and this trackable large lumen catheter called ‘The FlowTriever’ was inserted over the wire until it reached a large clot burden from the big vessels of the heart. The most fascinating part of the procedure was that in order to reduce blood loss, this system filtered the blood for reinfusion back to the patient, thus enabling bloodless thrombectomy for pulmonary embolism (PE) procedures. At the end of the procedure this accessible filtration design also allows clot examination and reservoir cleaning for more filtrations.
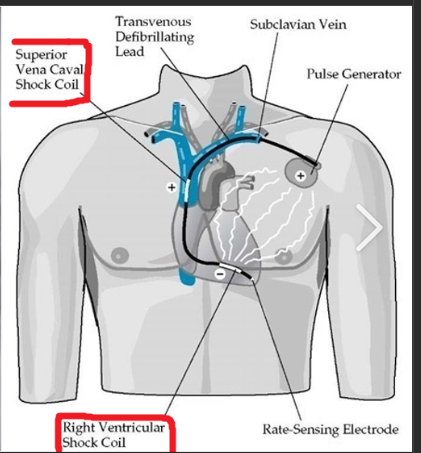
Improvements: Implantable Cardioverter Defibrillator (ICD)
This is a small device that is placed in the chest and detects any life-threatening, rapid heartbeat. If this occurs, the ICD sends an electrical shock to the heart bringing the rhythm back to normal. While Dr. Wissner was explaining to the patient the effectiveness of this device, he also mentioned that in a certain amount of time the battery of the device runs out. Thus, in the future the patient will certainly need a replacement surgery which may lead to complications such as vein damage, swelling, bleeding, blood leaking through the valve, movement of the ICD generator out of its proper position, which can cause pain or skin erosion.
Week 2: Storyboard
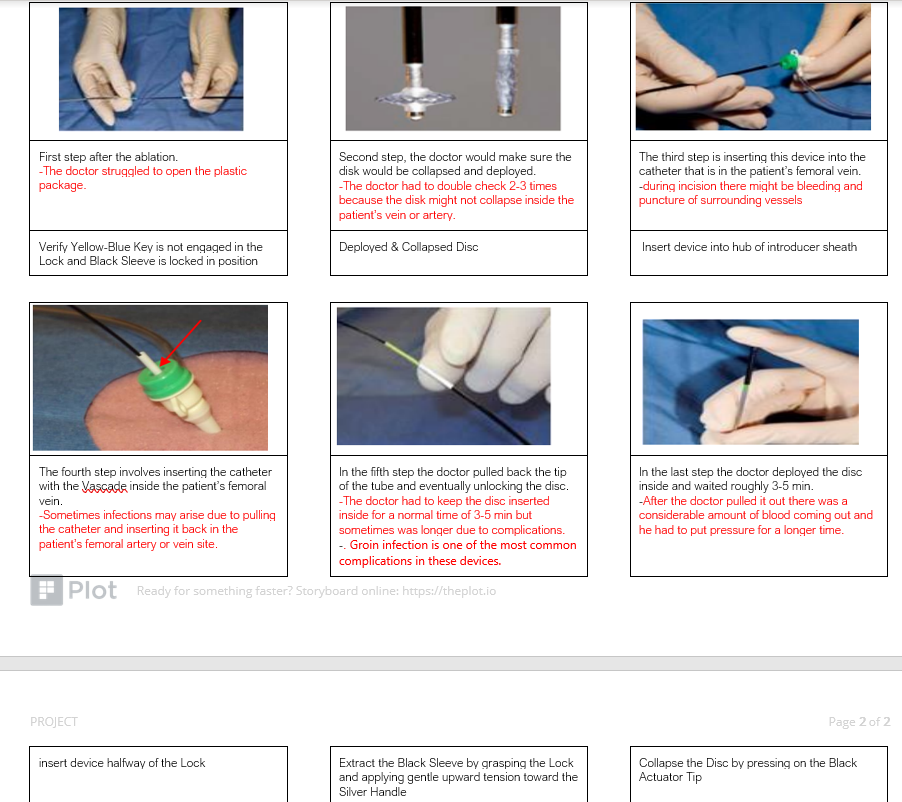
The second week of CIP was different from the first one. We got to experience things much more because we knew the staff, the people who we were working with, the divisions and the general idea of the procedures. Of course, there are always new things to learn about especially in a hospital where you get different cases every now and then. Specifically, this week we got introduced to this amazing tool that Dr. Wissner used after the ablation which is called the VASCADE VCS and its intended is to seal the femoral arterial or femoral venous access site at the completion of an endovascular procedure.
The method that doctors would usually use after procedures is manual compression which is the most common method to achieve hemostasis after different procedures. In most hospitals and by a lot of doctors this method is considered to be time consuming, requires prolonged bedrest, and is uncomfortable for patients and clinicians. The venous vascular closure system has showed to be an efficient and safe way for vascular closures. This method suggests shorter time of compression, faster recovery and its more convenient for patients and clinicals.
The system is designed to deliver a resorbable Collagen Patch, extra-vascularly, to help in achieving hemostasis. The system consists of a sterile disposable Vascular Closure Catheter which houses a resorbable Collagen Patch, and the VASCADE Clip. After completion of the ablation procedure, the VASCADE Catheter is inserted through a catheter in the femoral vein or artery. The VASCADE Disc is then deployed within the vessel and the introducer sheath is removed over the catheter. Then, the Black Sleeve is unlocked and is ready to deploy the collagen patch inside the patient’s body. The system is left in place for 3-5 min period to allow the patch to swell, after which the VASCADE Disc is collapsed. The VASCADE Catheter is then removed from the artery or vein leaving the collagen Patch at the artery or vein site. The patch expands as a result of rehydration in the presence of blood in the tissue tract to provide an extravascular seal. This provides vessel hemostasis and faster recovery for the patient. However, this procedure comes with some complications as acute femoral artery occlusion or groin infection as explained in the storyboard.
This procedure is explained in detail in the research paper attached to this blog along with data for the efficiency and safety of using it.
Week 3: Needs Statement
Our third week of clinical immersion program was intense yet exciting and interesting. We were able to observe different procedures and techniques which offered us more ideas on creating a more detailed needs statement as our goal of the week. While observing procedures we kept asking questions and taking notes about general cardiology but also narrowing it down to the problems that might consist during each of them. We had the opportunity to interview attendings and fellows of the field which certainly helped us with narrowing the scope of our statements furthermore.
One thing that caught my attention and wanted to share here, which made me feel nervous and anxious this week, was a procedure where they implanted a pacemaker. Since we saw this procedure last week as well, we had an idea of what was actually going on in the lab and how this would take place. However, things didn’t go as well as they were planned. The patient was previously diagnosed with COPD which makes it hard for things to go smoothly, especially in the amount of sedation that the anesthesiologist should give the patient. The procedure lasted longer and everyone in the lab put all their efforts in and turned the patient’s vitals normal. At the end of the procedure everything fell into place, and the paste maker was implanted successfully.
An implantable cardioverter defibrillator (ICD) looks similar to a pacemaker, though slightly larger. One of the big concerns of the medical field for inserting an ICD are the inappropriate ICD shocks due to internal electromagnetic interference generated by broken wires throughout years. The wire leads that connect the defibrillator to the heart are threaded through the blood vessels. Research from Journal of the American Heart Association shows the silicone-insulated leads being replaced with polyurethane ones in and its effects on newer ICD devices. The hope was that the newer leads would have fewer problems. Despite the benefits that this therapy can offer to a patient, inappropriate shocks from the devices are “common”. These inappropriate shocks can lead to fever, increased pain, redness, swelling, chest pain and sometimes place patients at a greater mortality risk.
Needs statement 1
Inappropriate ICD shocks generated by damaged wires.
This is just a statement that consists of only the problem without involving the population or the outcome. The next statement will be more detailed and will include the outcome of the problem.
Needs statement 2
Cardiologist are looking for a way to reduce the inappropriate ICD shocks that lead to serious complications.
The second statement includes the population and the outcome but still is vague and broad. You can’t precisely tell what complications may arise with the problem and the cardiologist have different specialties.
Need statement 3
Electrophysiologists are looking for a way to reduce inappropriate shocks generated by damaged wires in patients with ICD implants, in order to reduce chest pain, swelling and mortality risk.
The third statement includes the need and the population who is working on it. Cardiologists are being more defined and the outcome to this problem is being defined in more details.
Week 4: Potential Solutions
Differently from the third week, this week’s goal was to identify more clinical needs and to start looking for potential solutions on existing patents. This week we reobserved different procedures such as pacemaker replacement, peripheral angiography, PFO closure, Stent intervention and also got to interview attendings and fellows to give us a better understanding of the clinical needs.
Most of the procedures in the Cardiology Cath labs involve catheters and syringes to deliver fluid in the patient’s body through veins or arteries. One crucial issue that stands out with the syringes set ups in these labs are the introduction of air bubbles in the bloodstream. Air bubbles in syringes are to be cautioned against in intro-arterial injections. Even a small amount of air but remaining in venous circulation can cause obstruction of right ventricular outflow tract leading to cardiac arrest. Research emphasizes that any amount of air bubbles can lead to myocardial infection, vein or arterial blockage which can significantly cause cellular damage or a stroke to the patient.
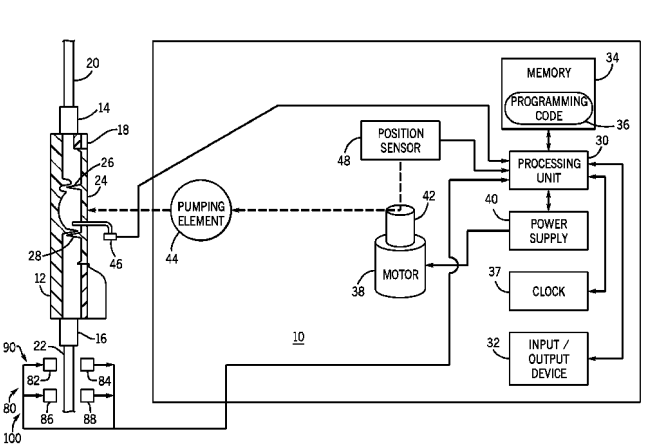
Thus, I thought of searching for a way to eliminate these bubbles so it will be easier for doctors to induce fluids and also less risky for the patient. The need statement that we came up with for this clinical need is:
Finding a way for cardiologist to avoid the formation of air bubbles during catheterization procedures in order to reduce myocardial infection, or arterial blockage which can lead to cellular damage or strokes.
While looking up potential solution from different patents online, a method and pump that accurately senses air in a fluid delivery captured my attention. The device of this invention effectively provides a mean of removing small bubbles from a relatively rapid stream of blood or other liquid by using sensors. It is programmed to activate and deactivate the air sensor, as many time as needed during surgery, and generates signals or alarms based upon a single indication of air in the line. The pump is built with multiple air sensors so that the method can use multiple signals to distinguish real moving air bubbles from air bubbles adhered to the inner wall of the fluid delivery line.
While discussing this solution with one of the attendings the only thing that concerned him was that these devices are programmed, and their cost is high for the hospital. Also, they feel safer using their hand mechanisms than these programmed devices. This is a huge concern about medicine yet to be solved by the advanced technology or who knows??? Maybe we will be able to…
Week 5: The Total Addressable Market

As we proceeded to the last week, we had a clearer idea on the procedures that were going on and started looking deeply in the problems that we had already seen. We got to narrow down the ideas from last week to a more precise conclusion by interviewing more attendings and discussing possible solutions with them. The task of this week was to calculate the total addressable market for the needs statements that we have presented in the past weeks. I introduced the statement in week 4:
Finding a way for cardiologists to avoid the formation of air bubbles during catheterization procedures in order to reduce myocardial infection, or arterial blockage which can lead to cellular damage or strokes.
Based on the statement and also based on what we have seen during the Cath and EP lab procedures we evaluated this as a problem that needs to be addressed. As I explained in week 4 post, this is one of the most important steps during these procedures to eliminate any further damaging consequences in the patient. While interviewing different attendings and fellows after these procedures they expressed that this is an important step that they have to be cautious about. They had to tap the tubbing while inserting any liquid in the patient’s veins. Although this might be easy for attendings that have practiced the process throughout years, it can be difficult for fellows that do not have much practice. From many attendings that we got to interview, they explained that there are filters in the market, that generate signals or alarms to notify the attendings or fellows upon a single indication of air in the syringe. Despite the accuracy and validity of this product, the filtering systems are expensive for the hospitals and the attendings find it easier, since they are used to it, to avoid the bubbles mechanically or by tapping.
As I mentioned in the beginning TAM can be calculated by the number of usages for each product multiplied by the cost of this product. Based on AHA journal more than 1 million cardiac catheterization occur throughout a year. A cardiac catheterization manifold could cost between $250-$300 per use. Thus, this would lead to a TAM= 1,000,000*$250/$300=$250,000,000-$300,000,000.