
Ikram Isa
2023 students
Biomedical Engineering Student
Department of Anesthesiology
Email:
Week I: The Storm Before The Calm

It all hit me as I stepped into the main operating room floor. There were nurses, students, representatives, and surgeons going in every direction. I stood by the OR front desk and absorbed the energy in the room. It was 8 am and most surgeries were just about to start, and contrary to the saying “the calm before the storm”, this was the storm before the calm because once the surgery started, everyone had taken their places and entered focus mode.
The first surgery we observed was a gastric bypass revision (also known as a “sleeve”) performed laparoscopically using the magnificent Da Vinci Xi machine. Our group got the chance to observe the entire surgery, however, the position that we stood in when the surgery began greatly limited our access to the anesthesiologist’s station, and by the time we had realized that there was barely any room for us to reposition ourselves due to the various machines in the room. We knew that next time we would need to get a good spot early on. Through interactions and conversations, we were able to have with the anesthesia residents and attendings during the next few surgeries, we quickly came to understand the incredible diligence and adaptability that anesthesia requires.
Through our observations for the next three days, there were a couple of good and bad engineering designs that we saw present in the anesthesiology equipment used in the main OR as well as the outpatient care center.
Good Design
A major part of anesthesia includes providing a source of oxygen to patients while they are unconscious. This is achieved through the use of a breathing tube that is fed down the trachea usually through the month, but occasionally through the nasal cavity. To gain appropriate access to this structure, a device called a laryngoscope is used to open up the pathway and provide a guide for the breathing tube. A good design I observed in this device was that certain laryngoscopes could be attached to a camera, which displays live footage on a screen, to allow for better visualization of the field. This visualization improvement enables anesthesia physicians or nurses to perform intubation with fewer jaw and neck realignments. However, the camera-imbedded laryngoscopes were not utilized universally throughout the hospital; we only observed them in the outpatient care center setting. I noticed that in these settings, attendings and nurse practitioners were the ones performing intubations using the camera-imbedded laryngoscope.
Activity: Intubation is the process of placing a tube down a patient’s trachea for respiratory (and other) purposes. A laryngoscope with a camera is used to open and provide visualization of the throat area and provide a passageway for the tube.
Interaction: the laryngoscope handle is held in one hand as the user guides the blade down the airway, using their unoccupied hand to open the mouth. Once the laryngoscope is in position and the vocal cords are visualized on the laryngoscope camera, the endotracheal tube will be fed down the created pathway and into the larynx. Once the tube is in position, the laryngoscope is extracted.
Environment: Camera-imbedded laryngoscopes are used in a variety of hospital settings, including emergency departments, intensive care units, and operating rooms. Patients should preferably be placed on a bed or flat surface in a horizontal position.
Object: The camera-imbedded laryngoscope is composed of two parts a detachable curved blade(head) and a handle. The blade contains a light source that runs on batteries. The camera is attached to the back of the blade from a machine that contains the screen display.
Users: Laryngoscopes are used by trained health professionals, such as anesthesiologists and CRNAs.
Bad Design
In contrast, a bad design that we observed was the inability of the oxygen masks to provide a proper seal with the patient’s face during the intubation process. Providing a tight seal between the patient and the mask is especially important because you want the patient to exclusively receive 100% oxygen coming from the machine. However, due to the design of the oxygen mask, the anesthesiology team often needed to tightly grasp the patient’s jaw towards the mask to achieve the desirable seal.
Activity: Patients receive 100% oxygen from a machine during intubation preparations. This peroxidation procedure helps reduce the risk of hypoxemia, low oxygen levels, during intubation.
Interaction: The user places the oxygen mask over the patient’s mouth and noise. To create the desired tight seal, the user would place their two thumbs on either side of the oxygen mask and grab the jaw of the patient with their remaining fingers.
Environment: This technique is done in a variety of hospital settings, including emergency departments, intensive care units, and operating rooms before intubation.
Object: oxygen masks are made of rubber materials such as PV. They have an opening at the top that connects to the oxygen machine and have a general shape that is supposed to complement the structure of the human face (noise area to chin).
Users: Oxygen masks are used for patients that are about to undergo intubation by the anesthesiology team, which includes the anesthesia attending, resident, and CRNA.
With the first week of immersion under our belts, we have begun to understand the flow control of the operating room, and more specifically the flow of inducing a patient, maintaining anesthesia, and safely emerging them. I am looking forward to asking more questions regarding the techniques we have observed, comparing different anesthesia approaches, and identifying gaps that can be reduced or eradicated altogether.
Week II: Flushed Away - Storyboard Edition
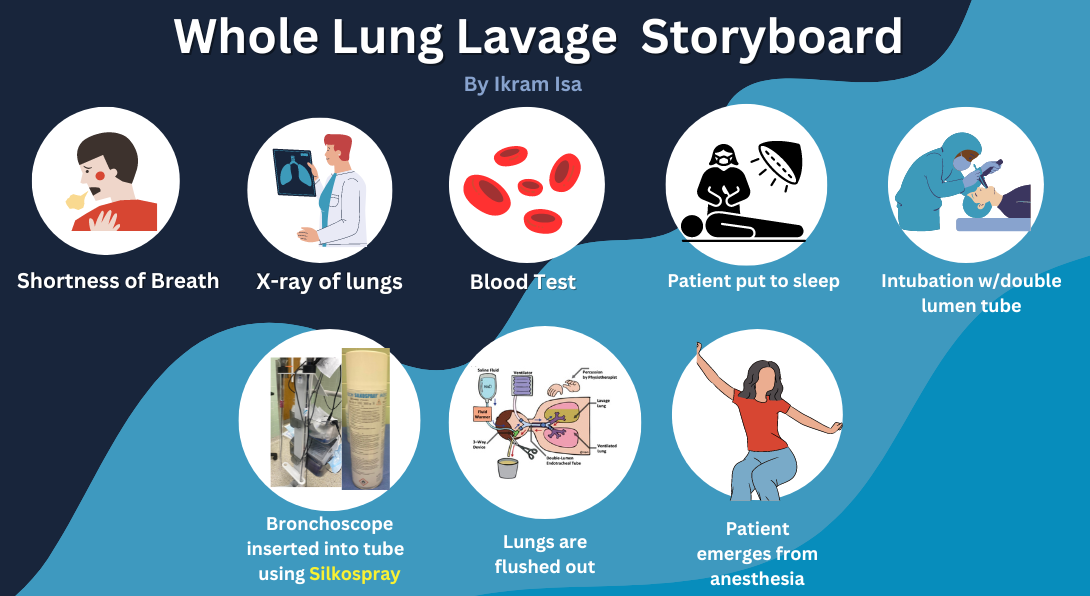
Over the past week, our team had the opportunity to observe a diverse pool of surgeries that involved different anesthesia techniques. One of the cases we sat in on involved a rare disease affecting the lungs. Using the peer-reviewed article, “Pulmonary Alveolar Proteinosis: a case report and world literature review” by Armando J. Huaringa and Wassem H. Francis, I took a deeper look at what this disease entailed. Pulmonary alveolar proteinosis (PAP) is a lung disease characterized by the accumulation of insoluble proteins in the alveolar space negatively impacting respiratory exchange. With an incident rate of about 1 in 1,000,000, PAP has been understood to be idiopathic, however, accumulating evidence suggests that PAP can be triggered by exposure to toxins, such as silica, as was the case explored in this particular article. Whole lung lavage, the irrigation of the lungs using saline, is the typical treatment given to PAP patients. This was the procedure that our team got the opportunity to observe last week. It was very interesting as we could clearly see the proteins being flushed out as a whitish liquid into the clear canisters.
As we observed this case, there were different stages involved from the onset of the symptoms up to the surgery itself. There were different pain points we were able to identify, which I depict here using a storyboard model.
1. Shortness of breath
Build up of proteins in the alveolar space will cause the patient to experience respiratory distress due to the decreased gas exchange capabilities of the lungs. This can result in labored breathing and oxygen deficiency, which can impact quality of life.
2. X-ray of Lungs
The initial diagnostic procedure that PAP patients will undergo is the x-ray of their lungs. This procedure requires patients to stay very still as the image is taken; in fact, patients might be asked to hold their breath. Additionally, fiberoptic bronchoscopy can be done to biopsy the lungs if alveolar infiltrates are observed on the x-ray in order to confirm protein buildup. The presents of materials like alveoli filled with periodic acid of Schiff (PAS)‐positive lipoproteins can confirm the diagnosis.
3. Blood Test
A blood draw and physical examinations are done to assess the different vitals of the patient. This is done to rule out any other underlying diseases that might be responsible for respiratory distress. Depending on the patient’s tolerance, this might be a pain point in the process, as it involves puncturing the skin using a needle.
4. Anesthesia Induced
Once pulmonary alveolar proteinosis has been confirmed, a whole lung lavage(wash) can be performed to remove the protein buildup. This can be an anxious time for the patient, especially during the period immediately leading up to the surgery. In fact, during our observation, the patient requested some music to be played in the operating room before anesthesia was induced in order to help with relaxation.
5. Patient Intubation with Double Lumen Tube
Once the patient was induced, the anesthesiologist used a laryngoscope to guide a left double-lumen tube into the bronchi. Guiding a tube down the trachea can pose a bit of difficulty, especially if performed by a less experienced individual, such as a resident, due to anatomical or visualization issues.
6. Visualization of Lungs Using Bronchoscope
For this procedure, it is very important to ensure the correct placement of the double-lumen tube, as one bronchus will be flushed with saline (the right bronchi) while the other is left to carry out respiration. A bronchoscope is inserted into the lumen tube to visualize and confirm the placement. However, due to the fact that a 37Fr tube was used for our patient (for appropriate sizing reasons), it becomes quite difficult to smoothly fit the bronchoscope through the lumen. The silicone spray, Silkospray, was rubbed on the bronchoscope in order to reduce friction between the scope and tube; however, there still appeared to be some resistance that the anesthesiology team had to overcome by pushing the bronchoscope down the tube with greater effort.
7. Lungs Flushed Out
After the tube is confirmed to be in the right space, the cuffs are inflated internally and the appropriate attachments are applied externally. Saline is then flushed into the right lung from one side of the “Y” connector attached to the right lumen and flushed out of the right lung from the other side. This was repeated several times, until the fluid being flushed out became relatively clear. We observed some leakage at the “Y” connection, most likely due to the high fluid pressure applied in that area.
8. Emergence
Upon completion of the procedure, the anesthesiology team turned off the delivery of anesthetic drugs to the patient, allowing them to regain consciousness. Unfortunately, the patient woke up confused and quite agitated, repeatedly trying to remove the breathing mask that was put over their mouth and nose. The anesthesiology team made efforts to communicate with the patient regarding where they were and why it was important that they try to calm down and leave the oxygen mask on their face. While this response to emergence is quite common among younger patients, it did make carrying out the responsibilities of the anesthesiology team more difficult.
Reference: Huaringa, A. J., & Francis, W. H. (2016). Pulmonary alveolar proteinosis: a case report and world literature review. Respirology case reports, 4(6), e00201. https://doi.org/10.1002/rcr2.201
Week III: Blood Vials and Veins - Developing Needs Statements
Week three of the program continued to immerse us in the fast-paced life of the OR. However, due to our increased familiarity with the environment, we were able to pick up on more activities, interactions, and organization that the OR housed.
During our observation this week, we sat in on a parathyroidectomy surgery, where an overactive parathyroid was removed in order to reduce the amount of parathyroid hormone released to the body. To confirm the success of the surgery, three separate blood draws needed to be tested at different time points (before the first skin incision, right before clamping the malfunctioning parathyroid blood supply, and after removing the gland), in order to ensure that the malfunctioning parathyroid was retracted (and not the healthy ones) [1]. Due to the way the patient was prepared for the surgery (with their hands wrapped by their sides), the anesthesiology team was tasked with collecting blood via the veins in the leg. As we spoke to the anesthesiology resident, they explained how putting in an arterial line (a-line) would have been a smoother option as it would allow them to easily collect blood multiple times. Unfortunately, a discussion on what the procedure would entail was not thoroughly discussed between the surgical and anesthesiology team beforehand, therefore blood draws through the leg quickly became the only option. It was not easy though. The patient’s leg veins were quite difficult for the anesthesiologist resident to access, requiring the help of the attending anesthesiologist. Due to the time sensitivity of the blood draws, delays in accessing the vein heightened the tension in the room.
Using the P(opulation), O(pportunity), and O(utcome) style, I developed three iterations of a need statement addressing the problem I observed during the parathyroidectomy.
Iteration 1: Anesthesiologists finding it difficult to identify veins for drawing blood need a quicker way to locate veins in order to make the blood drawing process more efficient.
Population: Anesthesiologist
Opportunity: Difficulty finding veins
Outcome: More efficient blood drawing process
This iteration of the needs statement identifies a general population of anesthesiologists that experience hardship while trying to find veins to draw blood from, which slows down the process. This iteration, however, fails to address whether the experience level of the population or the location of the vein plays a role in the rise of this need.
Iteration 2: Anesthesiologist residents experiencing difficulties identifying veins in the leg for drawing blood during surgery need a quicker way to locate veins in order to make the blood drawing process more efficient.
Population: Anesthesiologist residents
Opportunity: Difficulty finding veins in the leg during surgery
Outcome: More efficient blood drawing process
The second iteration here, narrows in on a population of anesthesiologists with less experience, refining the targeted audience. This refinement is supplemented by the focus on veins specifically found in the leg under the conditions of surgery. Nonetheless, the outcome of addressing this need still remains superficial as it does not go a step further to include the result of increasing efficiency in blood draws.
Iteration 3: Anesthesiologist residents experiencing difficulties identifying veins in the leg for drawing blood during surgery need a more efficient localization method in order to be able to allocate more time to monitoring the patient under anesthesia.
Population: Anesthesiologist residents
Opportunity: Difficulty finding veins in the leg
Outcome: Anesthesiologist residents can spend more time monitoring the patient
This final iteration improves on the previous one by expanding on the impact that improving blood drawing efficiency can have on the overall care that the patient receives from the anesthesiologist resident.
[1] Khan, Z. F., & Lew, J. I. (2019). Intraoperative Parathyroid Hormone Monitoring in the Surgical Management of Sporadic Primary Hyperparathyroidism. Endocrinology and metabolism (Seoul, Korea), 34(4), 327–339. https://doi.org/10.3803/EnM.2019.34.4.327
Week IV: Patents
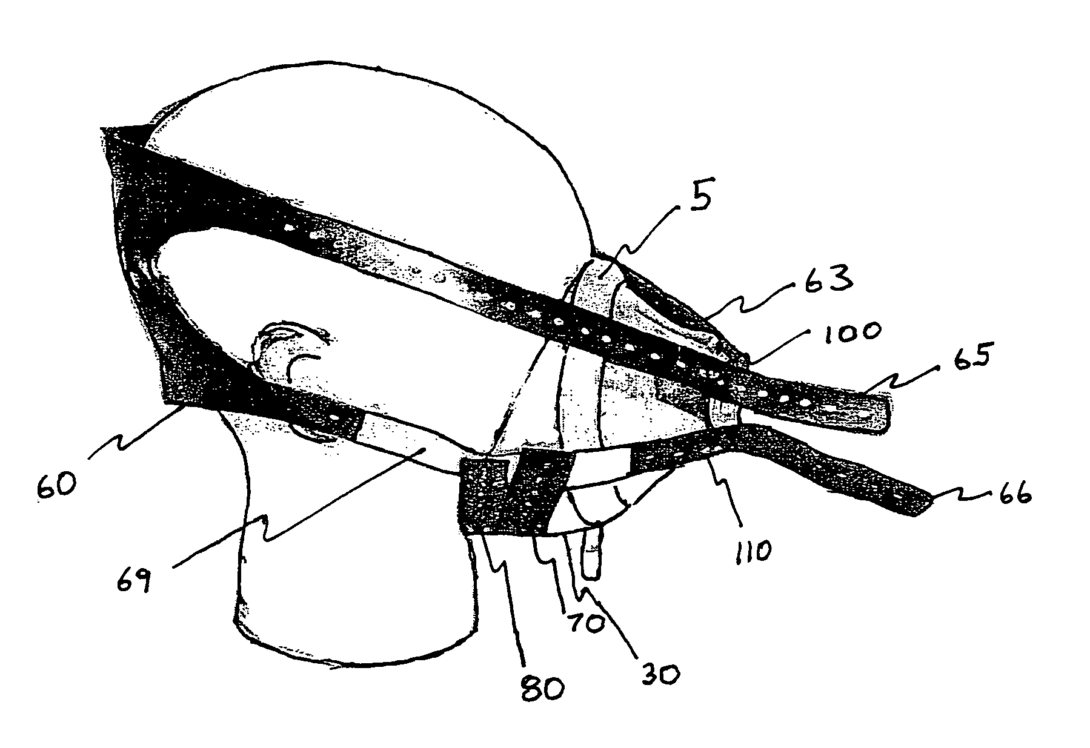
Reflecting back on our first week of the clinical immersion program, a product that we identified as needing improvement was the masks used to supply 100% oxygen gas to patients prior to being induced. As I had noted early, anesthesiology personnel (attendings, residents, or CRNAs) often had to tightly secure the patient’s face against the oxygen mask in order to create a tight seal. With the additional observations that I made in the past couple of weeks, I saw how easily occupied anesthesiology attendings and residents became in the minutes leading up to administering anesthesia. From prepping arterial lines to drawing medications, having to tightly hold onto the patient’s oxygen mask in a finger-straining manner appears to be an added inconvenience to the anesthesia provider. This led me to develop the following needs statement:
“Anesthesiology personnel need a hands-free method of attaining a tight seal between their patients’ oral-nasal space and oxygen mask in order to grant them more time to prepare for the next steps of anesthesia administration”
A current design that appears to address this need is under the patent titled “Hands-free Anesthesia Mask” (US6981503B1), which was invented by Leon Shapiro and approved in 2006. This patent describes a multi-component product: a breathing mask with four protruding indents, a strap containing a head plate and four extensions that contain complementary holes to the protrusions found on the mask, and two independent hole-containing straps similar to the ones attached to the head plate except they are smaller. The purpose of the six straps is to secure the mask around the patient’s mouth area (the four straps attached to the head plate) and jaw (the smaller two straps).
This innovation is actually something that we observed being used at the hospital, specifically in the intensive care unit. However, its use was not commonly observed in the operating room setting. I suspect this to be due to the brief use of oxygen masks in the OR consequently making the strapping and unstrapping process not worth the time it cost. This leads me to refine my needs statement:
“Anesthesiology personnel need a hands-free method of attaining a quick tight seal between their patients’ oral-nasal space and oxygen mask that can be quickly undone to grant them more time to prepare for the next steps of anesthesia administration”
Week V: A-lines & Money
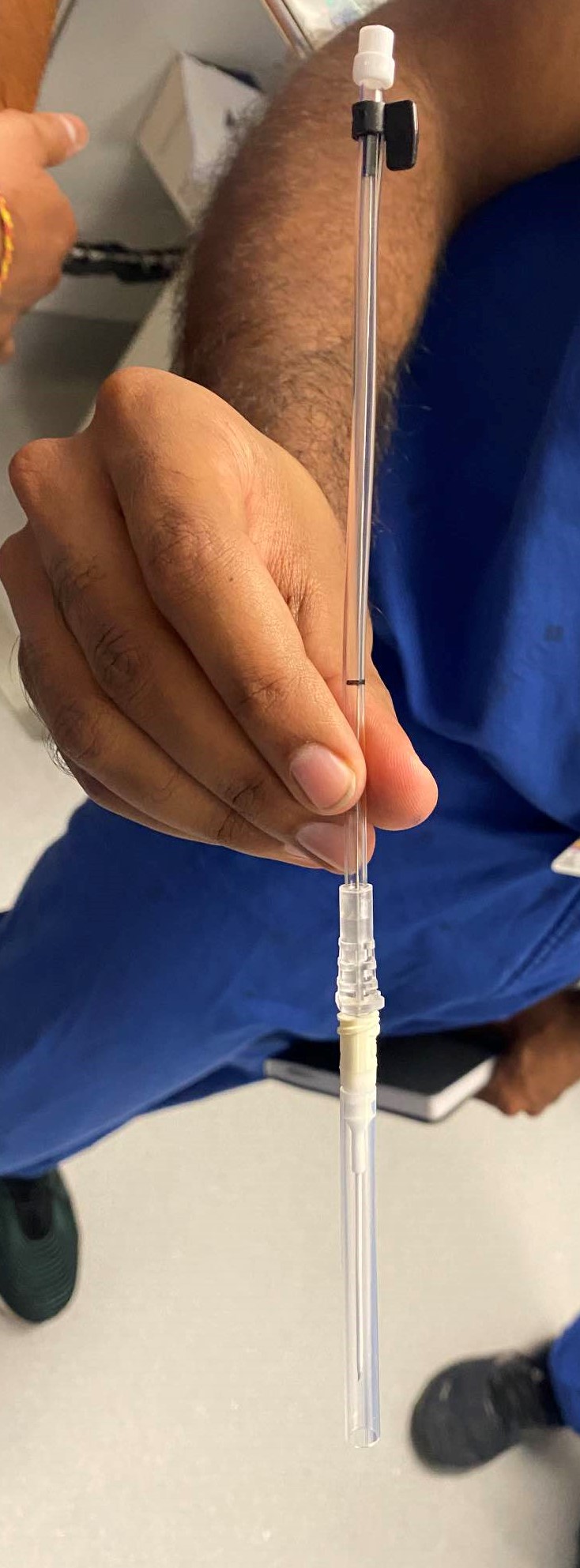
An arterial catheter serves as a medical tool employed for the measurement of arterial blood pressure or the extraction of blood samples from an artery. Using an arterial line (A-line) to measure blood pressure provides a more accurate reading as compared to the non-invasive blood pressure cuff. The arterial line catheter consists of a slender tube that is carefully placed into an artery, commonly within the arm. It is then linked to a pressure transducer, a monitoring system, and/or a syringe. The catheter is gently maneuvered through the artery until its tip reaches the intended position. Subsequently, the catheter is fastened to the skin to avert displacement and uphold the designated placement of the catheter tip.
While this form of measuring blood pressure is more accurate, it does pose risks of infection, hematoma, and or thrombosis. Consequently, not all surgeries use the A-line. As I discussed with an anesthesia fellow this week, I learned that smaller cases (less risky and typically shorter to complete) do not employ the use of an arterial line. Surgeries requiring continuous blood pressure monitoring, due to the complexity of the case, will use an A-line.
Approximately 8 million arterial lines are used in the United States each year [1]. And with an average cost of 50 USD for each catheter kit, the total addressable market for this product comes out to be approximately 400 million USD with an estimated compound annual growth rate of 5.5%, which is 1.2% less than the overall catheter market [2]. This however does not come as a surprise as the overall catheter market in the US is valued at around 12 billion USD, making arterial lines take up only 3% of the catheter market.
[1] “Arterial line kit,” Medex Supply, https://medexsupply.com/arterial-line-kit/ (accessed Aug. 10, 2023).
[2] “Catheter market size, Share & Growth Analysis Report, 2030,” Catheter Market Size, Share & Growth Analysis Report, 2030, https://www.grandviewresearch.com/industry-analysis/catheters-market-analysis (accessed Aug. 10, 2023).
About