
Rixzie Jimenez
4th Year Biomedical Engineering Student
OB/GYN Department
Email:
Week 1 - Good and Bad Designs
Good Design – Samsung Hera W10 Ultrasound Machine. During observation, the machine was highly advanced. It had a lot of features and controls that was easily maneuvered by the ultrasound tech.
Activity: An ultrasound tech conducted an anatomic scan of a fetus of a pregnant patient. Tech had applied gel and used the probe to apply the gel all over the belly. There were various controls and buttons that allowed the tech to change the parameters of the scan. Images and videos were taken from the examination. The tech was also able to label certain captured images, along with measuring certain body parts. Real time feedback was seen through the screen. A TV, in addition, was positioned behind the tech so that the patient was able to observe the scan as well.
Environment: Small clinic room with minimal light. Curtain was used for added privacy.
Interactions: Communication between the tech and the patient was conducted to ensure medical information was accurate. Communication between the tech and the doctors were also observed once all images were taken.
Objects: Ultrasound machine. Examination chair. Mounted TV.
Users: Ultrasound tech had control of the entire machine. Patient was laying on the chair. Patient’s family member was also present in the room.
Bad Design – Cardiotocography Machine. Main concern regarding this machine revolves around the printing and sound output. The data printed out just hangs from the machine. Multiple patient testing could lead to over stimulation with the different heart beats playing out loud. It could cause some discomfort for individuals in the room.
Activity: Nurse conducted antenatal testings, which includes a non-stress test and amniotic fluid index. Nurse connected leads to the patient’s belly for examination. The cardiotocography machine was used to monitor the fetal heartbeat and contractions. Paper printed out of the machine with the cardiac activity and contraction. Nurse was also able to monitor the readings on the computer.
Environment: Clinic room with three beds. Nurse would take in two patients at a time. It was a dim room to create a more calming environment. Heart beat from each machine would play out loud.
Interactions: Nurse was in charge of setting up and using the CTG machine. Communication present between nurse and patients.
Objects: CTG Machines. Clinic Beds. Curtains for privacy. Nurse’s desk and computer.
Users: Nurse had control of the CTG machine. Patients were laying on the beds.
Week 2 - Secondary Research and Commercial Products
In the Center for Women’s Health, a numerous number of patients often come in for a fetal ultrasound (US). It is an important evaluation that healthcare providers rely on to assess patient and fetal conditions. Depending on the gestational period and patient conditions, the type of US does vary. The two main types include transvaginal and abdominal US. Transvaginal focuses on the pelvic cavity, cervix, uterus, fallopian tubes, and ovaries. Abdominal US, on the other hand, allows clinicians to record images across the belly. Dating, nuchal translucency, noninvasive prenatal testing (NIPT), and anatomy scans can be conducted. Although the same technology can be used to perform these scans, the kind of transducer used does vary between transvaginal and abdominal. Ultrasonographers and clinicians are trained to record different anatomies.
Secondary Paper – “Sonography Fetal Assessment, Protocols, and Interpretation”
To understand the intricacies at play during different evaluation processes, “Sonography Fetal Assessment, Protocols, and Interpretation” provides a detailed review of the indications and protocol of fetal US. Screening and assessment does vary based on certain indications, which is impacted by the trimester. There are different levels that a scan may be categorized in depending on how detailed or specific the exam is. Additional exams include fetal echocardiogram, fetal doppler US, cervical length measurement and biophysical profile. Gestational age and clinical scenarios are considered for different approaches, assessment, timing and test frequencies. There are different indications for each trimester US examinations: standard first trimester US, detailed first trimester anatomy US, standard second trimester anatomy US, detailed second trimester anatomy US, and specialized third trimester US. Ultrasounds are commonly used, but patient refusal is possible. Moreover, the technology used to conduct these examinations are gray-scale real-time scanners and varying transducers. Abdominal curvilinear transducers (3 to 5 MHz) are used for abdominal exams. However, transvaginal exams are conducted using high frequency probes (9 to 12 MHz). License ultrasonographers conduct the screening and a physician is medically trained to interpret the US scans. The visibility of the scans are affected by bladder content. Full bladder is ideal for higher resolution image for abdominal US. Meanwhile, empty bladder is recommended for a transvaginal exam. These scans can examine fetal biometry, fetal head, face and profile, neck, thorax and heart, abdomen and pelvis, spine and extremities, and the placenta, uterus and adnexa. Each anatomical structure is associated with specific techniques and parameters to be images and/or measured. These clinical examinations are highly significant. Morbid obesity, hypertension and gestational diabetes can set patients in the high risk populations, which have an increased potential for adverse fetal events. US scans can raise awareness for any abnormal or suspicious structural scans and measurements. Future actions and monitoring are affected by the findings. The goal is to optimize clinical outcomes for both the mother and fetus.
Andelija S, Tafti D. “Sonography Fetal Assessment, Protocols, and Interpretation.” [Updated 22 May 2023]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK576427/. Accessed 6 July 2024.
Commercial Product – Philips Ultrasound Compact 5000 Series
The Philips Ultrasound Compact 5000 Series for Ob/Gyn is a commercial product used by many healthcare sites. There are various features and claims made by the manufacturer. “Superb image quality, flexibility, and standardized workflow” is promised. The familiar touchscreen, user interface and high performance transducers are designed to aide technicians during screening. To enhance cleanability, the control panel is sealed. Moreover, easy connectivity using WiFi to share images and reports is possible. This would allow real time collaboration with colleagues. This also makes it easier for clinicians to access the scans for assessment. The US system is intended to have a long battery life (2.5 hour battery life). The main feature advertised is the system’s award winning compact design. It is meant for easy mobility so that it can fit in tight spaces in order to make bedside scanning easier. This mobility is ideal for multi-site support. It comes with a convenient travel case to make transporting the system and tools more convenient. The Ob/Gyn specific features include 3D/4D capabilities, aBiometry Assist, and FlexVue with Orthogonal View. aBiometry Assist reduces the need for conventional biometric measurement steps by assessing age and growth trends systematically. FlexVue simplifies the 3D volume evaluations (especially in the often difficult to acquire coronal plane). The Philips Ultrasound Compact 5000 Series is a great example of an US system that many technicians operate.
Philips. “5000 Series HC795140 Premium Compact Ultrasound System.” Philips, www.usa.philips.com/healthcare/product/HC795140/5000-series-hc795140-premium-compact-ultrasound-system. Accessed 6 July 2024.
Week 3 - Need Statements

Primary Observation:
Ultrasound techs conduct various ultrasounds each day. While holding the transducer with one hand, the other hand has to simultaneously control the ultrasound machine. Repetition of the same moves are observed. Techs often have to reach over the patient’s belly for a better view of the fetus or reach the opposite direction to press and adjust the controls of the machine to obtain the image. In addition, techs often apply pressure to the patient’s belly to stimulate movement of the baby.
Secondary Technical Observation:
There have been many studies that focus on work related musculoskeletal disorders (WRMSDs) in the sonography field and many improvements throughout the years. Although this is the case, numerous sonographers are still affected. A study indicates that 90% of clinical sonographers experienced symptoms of WRMSDs [1]. The physical risks for sonographers include force, repetition, awkward postures and contact pressure. For force, the tech must apply downward pressure with the transducer to get an image and drop force to hold the transducer. Repetition influences the use of similar muscle activity throughout the day to perform the same type(s) of exams. Awkward positioning is frequently exhibited by sonographers during scanning in order to access regions of interest or due to insufficient adjustability of equipment. Contact pressure is also prevalent in sonographers, which is described as the sustained contact between a body part and an external object. This could include resting one’s hip against the exam table. WRMSDs have a huge impact on sonographers physically, and eventually financially. The most common injuries include carpal and cubital tunnel syndrome, epicondylitis of the elbow, shoulder capsulitis and tendonitis, and neck and back strains [2]. It’s been reported that employers are paying over $120 billion dollars yearly in direct and indirect costs to accommodate for WRMSDs related [1].
Secondary Business Observation:
To address these concerns, industry standards were set to prevent WRMSDs [3]. There are many companies and products that aim to fulfill these standards.
Brandt Sonography Chair (~$2,200) [4] is meant to optimize posture to avoid neck and back injuries. It allows techs to sit comfortably, while providing support at any angle. The ergonomic design supports arms to avoid shoulder injury. Adjustments of seat height, seat depth, back height, and backwards tilt tension with integrated seat slider. Foot support for additional bracing and positioning is also important. The chair allows variation of position, movement and posture.
Clinton Model 80069 Power Multi-Use Ultrasound Trendelenburg Table with Stirrups (~$4,500 + accessories) [5] offers support for patients obtaining ultrasound procedures with pneumatically adjustable backrest and footrest. It is made up of a 3 piece top with pneumatic adjustable backrest, manual footrest and stirrups. This design allows for precise patient positioning. The table is powered to allow sonographers to raise and lower patients. Offers tilting adjustment into trendelenburg and reverse trendelenburg. The table is aimed to offer a rigid and stable lift.
Samsung WS80A with Elite (~$25,000) [6] has many features that aid sonographers with the imaging process and results. Imaging system features include CrystalLive, BiometryAssist, ClearVision, 5D Ultrasound Advancement, Realistic 3D Imaging (RealisticVue and CrystalVue), etc. The machine design is well thought out with goal to make it convenient for sonographers. The S-Vue transducers compatible with this machine enables better penetration and higher quality resolution. It is ergonomically designed to fit well in user’s hand and it’s easy to handle. It is claimed that the LED monitor delivers excellent contract resolution, image clarity and vibrant color. The touchscreen is designed to be highly sensitive to minimize user stress from repetitively pressing buttons. The control panel is adjustable, while allowing for smooth up and down lift to preferred height without straining. The transducer sable hangers accounts for users arranging cables neatly. Built in gel warmer is meant to keep ultrasound gel at a comfortable temperature for patients.
Total Addressable Market:
Population- Percentage of Sonographers with WRMSDs
Cost- Direct and Indirect Costs due to WRMSDs
TAM- $120 Billion [1]
Need Statements:
#1: Ultrasound technicians (population) require ergonomic equipment solutions (opportunity) to reduce work-related musculoskeletal disorders (outcome).
#2: Ultrasound technicians require ergonomic equipment solutions (population) to reduce work-related musculoskeletal disorders (opportunity), in order to reduce cost for treatment (outcome).
- The second NS is the revised version for which includes an outcome that can be measured.
[1] Murphey, Susan. “Work Related Musculoskeletal Disorders in Sonography.” Society of Diagnostic Medical Sonography, 2021, www.sdms.org/docs/default-source/Resources/work-related-musculoskeletal-disorders-in-sonography-white-paper.pdf.
[2] Harrison, Gill, and Allison Harris. “Work-Related Musculoskeletal Disorders in Ultrasound: Can You Reduce Risk?” Ultrasound (Leeds, England), U.S. National Library of Medicine, Nov. 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4760593/.
[3] Murphey, Susan. “Industry-Standards-for-the-Prevention-of-Work-Related- …” Society of Diagnostic Medical Sonography, 2016, www.sdms.org/docs/default-source/Resources/industry-standards-for-the-prevention-of-work-related-musculoskeletal-disorders-in-sonography.pdf.
[4] “Sonography Chair.” AliMed, www.alimed.com/sonography-chair.html.
[5] “Clinton Model 80069 Power Multi-Use Ultrasound Trendelenburg Table with Stirrups – 27” Width.” Universal Medical, https://www.universalmedicalinc.com/clinton-multi-use-ultrasound-power-table-with-stirrups-27-width.html.
[6] “WS80A with Elite.” Samsung, https://www.samsunghealthcare.com/en/products/UltrasoundSystem/WS80A%20with%20Elite/Womens%20Health/benefit.
Week 4 - Revised and New Need Statements
Revised Need Statement:
Ultrasound technicians require ergonomic equipment solutions (population) to reduce work-related musculoskeletal disorders (opportunity), in order to improve their health and productivity (outcome).
- With the revised need statement, the outcome is focused on the ultrasound technicians. The previous version of this NS included an outcome that was focused on healthcare providers, rather than the ultrasound technicians themselves. With this revision, the focus is now geared towards direct benefits to the technicians in their workplace environment. Improvement in health and productivity can lead to better job satisfaction. This can be measured with surveys.
IDEO:
- Desirability: Ultrasound technicians spend long hours repeating various tasks, which leaves them susceptible to work-related musculoskeletal disorders. The need for ergonomic equipment is critical to alleviate these risks and enhance their overall health and productivity. It is essential to maintain comfort and ensure safety on the job. By addressing the needs, healthcare providers are able to enhance job satisfaction and the well-being of the technicians. Workplace health and safety standards are a priority, especially in the healthcare industry. Investment in ergonomic equipment for ultrasound technicians has immediate and long-term benefits for both technicians and their healthcare providers.
- Feasibility: The development of ergonomic equipment solutions for ultrasound technicians is highly feasible. There are numerous current advancements in ergonomic design and technology. Many ergonomic features are already available in the industry: powered examination tables, height-adjustable ultrasound machines, and ergonomic chairs. These are tailored to meet the specific needs of ultrasound technicians.
- Viability: Investing in ergonomic equipment solutions for ultrasound technicians is highly viable. There are substantial long-term benefits: reduced number of work-related musculoskeletal disorders, diminished cost of treatment paid by healthcare providers and improved health and productivity of the technicians. These would lead to a more stable and engaged workforce, which in turn enhances overall patient care. Long-term savings from reduced healthcare expenses are significant. The market potential for ergonomic solutions is substantial and growing, driven by the increasing emphasis on employee wellness.
Ultrasound technicians frequently face challenges in obtaining clear images of the fetus due to its position in the womb. When the fetus is in a difficult position, technicians often instruct pregnant patients to roll onto their side or adjust their posture to improve the view. This process, however, can be uncomfortable and inconvenient for patients, particularly as pregnancy progresses and mobility becomes more restricted. Additionally, requiring patients to change positions may not always resolve the issue, leading to prolonged scan times and potential incomplete or less accurate diagnostic results. This situation highlights the need for solutions that can either minimize or eliminate the need for patients to adjust their positions while still allowing technicians to obtain high-quality images for accurate assessments. Improved equipment or methods that address these challenges can enhance both the efficiency of scans and the overall patient experience.
New Need Statement:
Ultrasound technicians need scanning equipment designed to facilitate optimal fetal positioning during scans, reducing the need for patients to reposition and enhancing imaging quality.
Week 5 - Ultrasound Storyboard
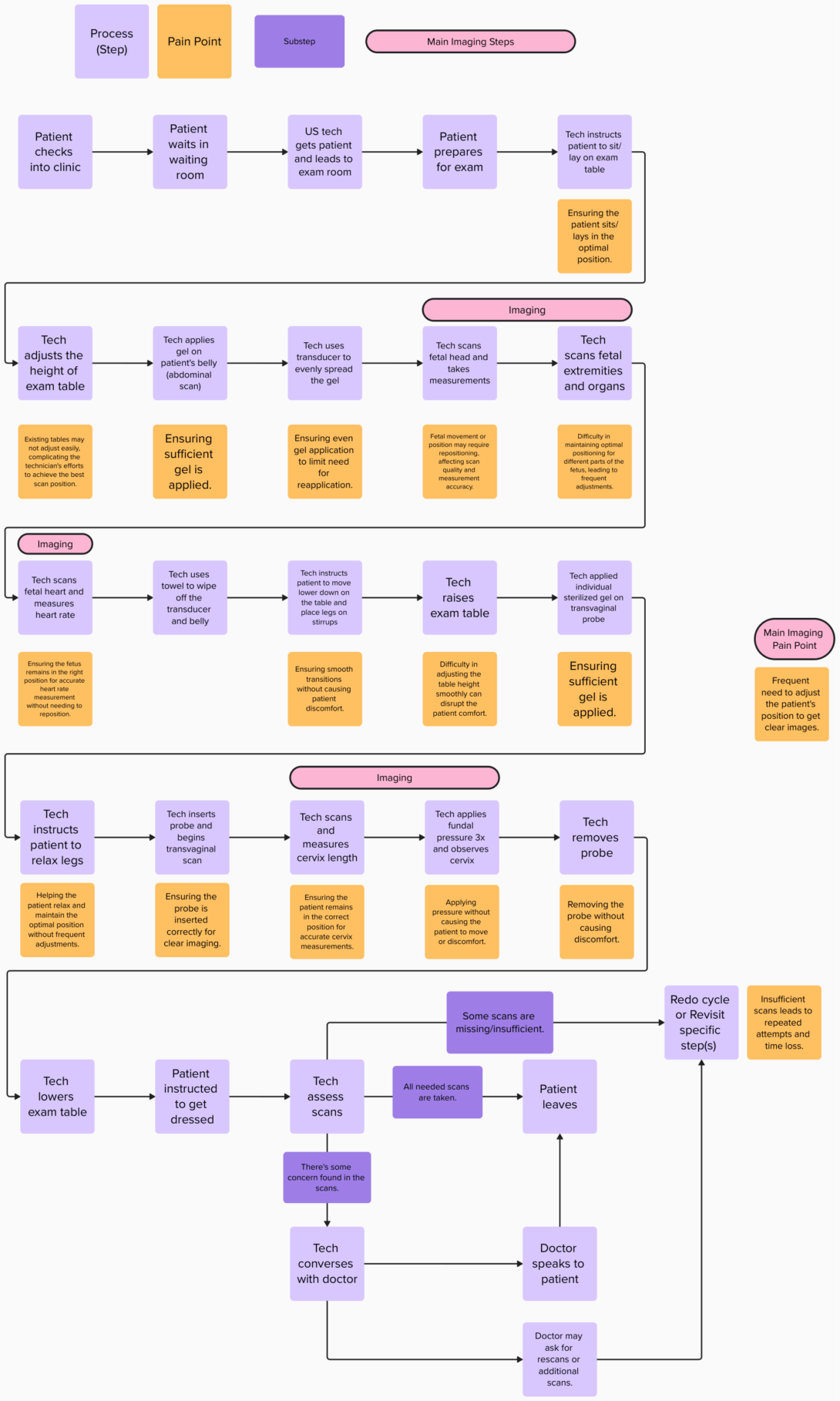
Need Statement: Ultrasound technicians need scanning equipment designed to facilitate optimal fetal positioning during scans, reducing the need for patients to reposition and enhancing imaging quality.
Week 6 - Reflection
As the program ends, it is important to reflect on the lessons I have learned the last 6 weeks.
Clinic:
It has been incredible being able to observe many clinical environments in the OB/GYN department. I spent a lot of time in the ultrasound area and was able to shadow several technicians. Technology plays a huge role in modern healthcare, thus observing the use of ultrasound machines was enlightening. My time in the High Risk clinic allowed me to observe the interactions between different staff members, along with patient interactions. Observing the clinic setting from a care provider’s perspective was fascinating. Shadowing in the Labor and Delivery Department was particularly enlightening. I gained a deeper understanding of the dynamics of a multidisciplinary healthcare team. I also learned the importance of adaptability in a clinical setting. The unpredictable nature of labor and delivery meant that plans could change quickly. I was impressed by the team’s ability to adjust quickly. This experience highlighted the value of being prepared for any scenario and the need to stay calm under pressure.
CIP Didactics:
The weekly Friday meetings taught me so much about understanding user needs, primary and secondary research, and market research. I was able to understand the difference between desirability, feasibility, and viability, which are crucial factors in the medical device industry. With the lessons covered, I feel more prepared for Senior Design.
To future CIP participants, I recommend to take every opportunity you can. This is your chance to gain firsthand knowledge about the healthcare field. This program is intended to provide insight into the complexities and interactions of clinical settings. Take notes of what you observe and form your own ideas. Then converse and ask questions from your team members and your mentors. It’s a privilege to be a part of this program, so use it to your advantage!