
Lana Khadra
Student Participant
Good and Bad Designs

My first week with the gastroenterology department was an eye-opening experience. Observing the inner workings of the GI lab allowed me to expand my knowledge beyond what I already knew: the basics of colonoscopies and endoscopies. On a daily basis, procedures ranged from simple routine colonoscopy screenings to more complex endoscopies such as EGDs, EUSs, ERCPs, and the placement of AXIOS stents. Each procedure utilized either an endoscope passing through the mouth or a colonoscope passing through the rectum, however, different courses of action are taken by the doctor based on the patient and the symptoms they presented. Employing these scopes enables doctors to provide patients with a minimally invasive outpatient procedure.
On my first day, I observed Dr. Naga perform four back-to-back routine colonoscopy screenings in the same procedure room. A polyp was found in the colon during one of the procedures and removed using a cold snare, the tissue was then sent to be biopsied. Watching the same procedure several times in the same environment allowed me to gain a better understanding of how a colonoscope is used, how doctors and nurses interact, and how the procedure room is optimized.
For the next couple of days, I followed Dr. Boulay around and observed more complex endoscopies performed in a larger procedure room as more equipment was required. Ultrasound, x-ray, and endoscope cameras were consistently used for EUSs and ERCPs. Pulmonary tech, Kevin Johnson, assisted on most of the procedures and allowed my team and I to interview him to gain a deeper understanding of the basics of an endoscope and a colonoscope. He explained the difference between the two scopes, the various options of camera angles, and walked us through the sterilization process.
Observing the clinical environment while taking notes using an AEIO framework (activities, environment, interactions, and observations) assisted us in identifying good and bad designs within the lab.
Good Designs:
The GI lab consisted of five procedure rooms each having a distinctive layout that catered to the needs of different procedures. The smaller rooms were equipped with the essentials needed for basic endoscopies and colonoscopies. While the larger room had an additional MRI machine for more complex procedures. The lab itself was designed in a circular pathway to accommodate the constant movement of hospital beds from the pre-procedure rooms to the recovery rooms without bumping into other patients.
After procedures, doctors documented their findings and wrote up their reports on healthcare software: ProVation. Electronic healthcare records allow doctors to easily access patients’ information to record and organize data. The templates provided and the immediately imported exam images are features that helped reduce the time doctors spent at their desks. This allowed for more time to focus on patients while also decreasing their wait time in pre-procedure rooms. Dr. Naga was able to perform his procedures and then quickly and efficiently document his findings in under 5 minutes before moving on to his next patient.
Bad Designs:
After only observing several procedures it became evident that the size of the procedure rooms posed a problem for nurses and doctors. Being able to efficiently move around and garb additional equipment was compromised by not only the size of the room but also wires all over the floor. During the colonoscopies, nurses had to constantly duck under screens mounted onto the walls to reach the vital signs monitor on the other side of the room. Moving around the procedure room was a struggle for nurses and doctors as they are consistently having to watch where they are going.
Gastroenterologists spend almost half their time performing procedures and up on their feet. While speaking with Dr. Trivedi she informed us that gastroenterologists are more prone to long-term disability as they are at increased risk for musculoskeletal disorders. The weight of the endoscope control along with the constant movement of the knobs leads to issues such as carpal tunnel. Standing during procedures and having poor body posture throughout also leads to back and neck pain.
Storyboard

With every procedure I watched, the more in-depth my questions and observations became. A lot of the procedures I watched were colonoscopies performed by the many physicians in the GI department. I became more interested in the process and the various equipment utilized during colonoscopies to ensure optimal comfort for patients. One of the topics Dr. Naylor discussed with me that really stood out was the use of CO2 instead of air for colonic expansion. With CO2 having a faster absorption rate, patients felt less pain and bloating during and after the procedure. However, its fast absorption affects its effectiveness in colonic expansion. I began to research this topic to gain a better understanding of how different gasses can have different effects on pain and colonic expansion.
In the review article, Memon et al. reviewed studies that analyzed the effects of using air and CO2 for colonic expansion. Inflation of the colon allows doctors to gain a better view when ascending into the colon during a colonoscopy procedure. The dissimilarities between the two stem from the idea that CO2 is absorbed faster than air. Trapped unabsorbed air can negatively affect bowel distention while lengthening discomfort time. Adverse effects reported by patients during and after a colonoscopy were abdominal pain and nausea.
The study measured seven outcomes: pain during the procedure and 15 min after completion, early pain (between 30 and 120 min after the procedure), intermediate pain (360 min after the procedure), late pain (720 to 1140 min after the procedure), cecal intubation rate, cecal intubation time, and total procedure time. The Jaded scoring system was used to assess each study, ranging from 0 (lowest quality) to 5 (highest quality).
Twenty-four randomized clinical trials with 3996 patients, 2017 using CO2 and 1979 using air, were examined. Out of the 7 outcomes, 4 proved to favor the use of carbon dioxide for colonic distention. There was a drastic reduction in abdominal pain throughout the procedure, between 30 and 120 minutes after, 360 minutes after, and between 720 and 1140 minutes after completion when carbon dioxide was used. However, there was no difference between cecal intubation rate and time as well as total colonoscopy time. Overall, it was shown that carbon dioxide does in fact reduce abdominal pain up to 24 hours after the procedure. Unlike air, carbon dioxide is absorbed faster by the body leaving no trapped air, which was shown to be the leading cause of greater abdominal pain.
Needs Statement
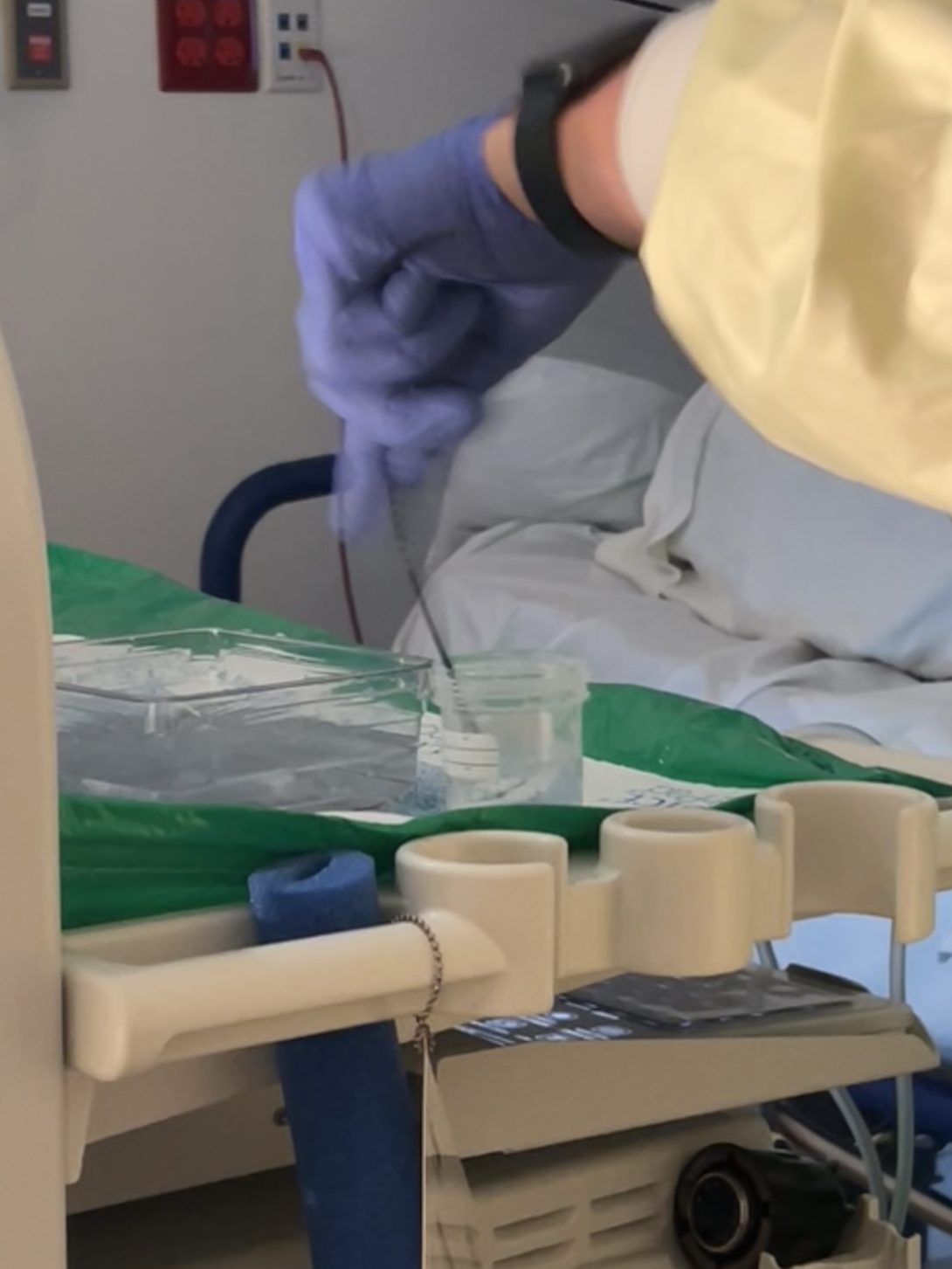
My first week in the GI lab was filled with new experiences, however, by the end of my third week, I began to feel more familiar with the clinical environment and procedures. For the past two weeks, I have observed the scope in action as well as explored its limitations. However, this past week I challenged myself to search beyond the scope. This was what led me to dig deeper into biopsy forceps and cold snares utilized in scoping procedures. I began with the cold snare, the most commonly used technique for polypectomies. The snare is inserted into the instrument channel of the scope and the diamond-shaped wire on the end is opened up to remove the polyp. A polyp trap is then placed to capture the tissue sample upon suctioning it out of the colon. This method was highly effective for small polyps commonly found in patients. Next, I moved on to observing biopsy forceps used for collecting tissue samples. The forceps are inserted through the instrument channel of the scope and their sharp blades are used to safely retrieve a tissue sample. Upon watching the technicians and nurses operate the forceps I began to notice a consistent obstacle they faced when transferring the biopsy from the forceps into the specimen cup. Every excised tissue must be aggressively shaken off by the technician or nurse in order for it to fall off the spike and into the specimen cup. I discussed my thoughts and observations with the technician who explained that the constant need to shake the sample off can be tiresome and can lead to tendonitis over time.
This problem became my focus when composing my need statements. As discussed in our workshop class, a need statement consists of a population, opportunity, and outcome.
Population: GI nurses
Opportunity: difficulty placing biopsies into specimen cups
Outcome: effortless tissue sample transfer
1st iteration:
Nurses have difficulty placing biopsies into specimen cups and need a more efficient way to release the samples
2nd iteration:
Gastroenterology nurses assisting with scoping have difficulty placing biopsies into specimen cups and need a more efficient way to release the samples
This need statement now specifies that the nurses and technicians are part of the gastroenterology department and aid with scoping. These additions help narrow down the scope of our population.
3rd iteration:
Gastroenterology nurses need an effortless method to place biopsies into specimen cups in order to reduce musculoskeletal pain.
This need statement is arranged differently and focuses on methods that specifically reduce musculoskeletal pain rather than just easily transferring the tissue samples.
Solutions and Patents
This week I took a deeper dive into the steps nurses take to excise tissue samples using biopsy forceps. After my initial observations regarding the struggle faced with releasing tissue samples off the spike and into specimen cups, I began asking questions to gain a better understanding of the process. One nurse informed me that in order to remove the tissue sample off of the spike, they are given toothpicks to drag the biopsies off. However, the constant need to open the drawer, grab the cup of toothpicks, take one out, use it and then dispose of it is a time-consuming process. The workaround nurses have come up with is to shake the tissue sample off of the forceps and into the cup, a much faster process. Despite the fact that it works, over time this get-around solution is affecting nurses. The constant motion exerted on their hands leads to musculoskeletal injuries and often times the tissue does not fall into the cup and the forceps are inserted back into the scope for more biopsies with the sample remaining on the spike.
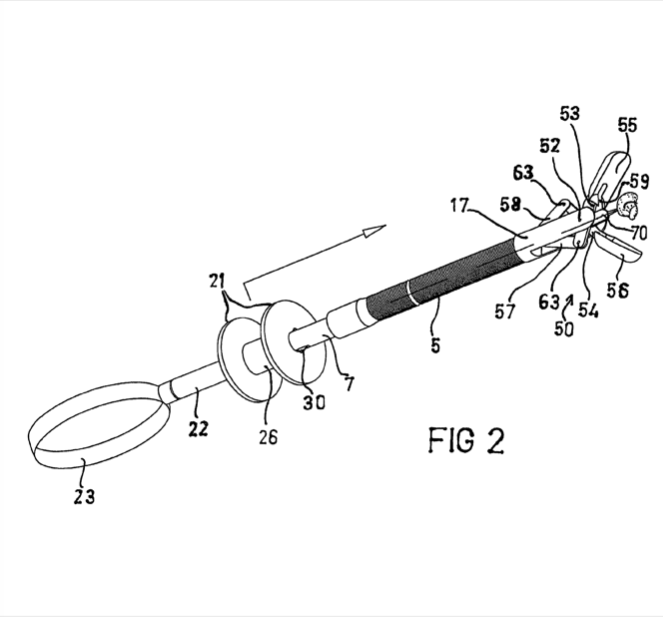
Although I observed this process to have flaws, I began my research to explore if others felt this inconvenience as well and what solutions have been created to reduce or completely overcome the issue. I came across a patent for a device called Needle Biopsy Forceps with Integral Sample Ejector that catered to the needs of my identified limitation. This device has a sample contacting surface located near the center of the needle which moves back and forth between the surface and needle in order to push the sample off of the spike when the cups are open. The control for this surface is located at the end of the forceps, near the handle.
The relevant claims of this patent state that the device shall have a hallow cable with two cups at the distal end. The cups shall have the ability to open and close, allowing for at least one sample extraction. Between the moveable cups, a needle will be connected that can extend no more than the cups. However, the movement of the needle is separate from the movement of the cups. The tissue sample pushing surface is located at the proximal end of the needle and interacts with the excised sample. Upon retraction of the needle, the tissue sample will be removed from the needle. A needle lock and advance stop mechanism will allow the needle to lock and be prevented from advancing past the cups when in an open and closed position. Then the device shall eject the tissue sample off the needle.
The abilities of this device meet the needs of my observations; the struggle nurses face to release tissue samples off of the needle in biopsy forceps. The biopsy needle forceps essentially remain the same as the biopsy forceps currently used in the GI lab, allowing a familiar way of use. However, the addition of the ejector is a new feature that will help successfully release tissue samples. This device also allows for multiple tissue samples, which is needed when taking biopsies. Through my primary and secondary research, this instrument showed to be equipped with an additional property that meets the needs rooted in my observation.
Total Addressable Market

For the past five weeks, I have been actively observing the clinical environment and identifying user needs. A colonoscopy screening was the first procedure I observed in the GI lab and my first encounter with biopsy forceps. However, as the weeks went by I sat in on numerous procedures with patients who required biopsy samples to be taken. I soon became very familiar with how biopsy forceps are used, allowing me to better find the limitations. It became evident that GI nurses assisting with scoping procedures had difficulty emptying excised biopsy samples into specimen cups. A less tiresome and more efficient way was needed to be able to successfully remove tissue samples.
Biopsy forceps are used during both colonoscopy and endoscopy procedures. When advancing through the digestive tract, doctors may collect biopsy samples. This may be done for several reasons. When performing scoping procedures, doctors extract biopsies to test samples for cancer or other diseases they may suspect, bleeding, inflammatory diseases, or any other abnormalities.
In order to effectively excise tissue samples, the doctor begins by informing the tech to prepare biopsy forceps and a specimen cup. The tech controls the motion of the jaws on the forceps using the handle while the doctor positions the forceps at the biopsy site using the scope. Once the doctor informs the tech to close the jaws, they apply pressure to the handle in order to close the jaws. The forceps are removed from the scopes instrument channel, and the tissue sample is emptied into the specimen cup. Once all the tissue samples have been taken, the forceps are disposed of. Biopsy forceps can take up to three samples at a time, however, most doctors prefer to take up to two samples.
Collecting tissue samples using biopsy forceps is very common in the GI lab. Almost every procedure requires some tissue excision. Overall there are around 7 million upper endoscopies and 15 million colonoscopies procedures in a year. I began to take a closer look at each category and how many procedures required biopsies. Out of the 7 million upper endoscopies, 1.2 million procedures obtained biopsies, and out of the 15 million colonoscopies, 5.3 million procedures obtained biopsies. However, finding an estimate on the number of biopsies obtained on yearly colonoscopies was difficult. A small research was conducted by Morarasu et al. in which 2109 colonoscopies were studied. Of those procedures, 748 had biopsies taken which made up 35.4% of the total. This statistic was applied to the yearly number of colonoscopies performed in order to acquire an estimate of the number of biopsies obtained. Altogether, 6.5 million biopsies are obtained every year meaning 6.5 million biopsy forceps are used each year.
With these numbers, I am able to calculate the total addressable market: the number of units per year multiplied by the cost of the product.
TAM = 6,500,000 * $530 = ~ $3,400,000,000
Morarasu, Stefan et al. “Colon biopsies: benefit or burden?.” Journal of medicine and life vol. 12,2 (2019): 156-159. doi:10.25122/jml-2019-0009
Infection rates after colonoscopy, endoscopy at US specialty centers are far higher than previously thought. Johns Hopkins Medicine Newsroom. (2018, May 31). Retrieved July 31, 2022, from https://www.hopkinsmedicine.org/news/newsroom/news-releases/infection-rates-after-colonoscopy-endoscopy-at-us-specialty-centers-are-far-higher-than-previously-thought
The End!

The past six weeks have been unbelievably amazing. Walking in at the start I was nervous about what the future held but excited to learn and expand my knowledge as well as apply what I have learnt in my classes to this program. I remember my first day at the Endoscopy Lab, I was amazed at the different technologies used throughout the procedures. Various scopes in the scope room, each targeted for a specific procedure. Various secondary equipment, each to combat a different problem. It was truly eye opening to see how the endoscopy lab worked and just how important the gastroenterology department really is. Although from an outside perspective each instrument seemed to do its job wonderfully, being immersed in the lab for over a month showed me that there is always room for improvement especially for a target audience.
A piece of advice I would offer future Clinical Immersion Program Students would be be to allow yourself to be fully immersed. Although the first couple of weeks can be a learning curve, don’t miss out on asking questions and most importantly observing all that is offered to you. Observations and primary research within the lab is critical to further your ideas and understanding.
I would like to thank the physicians, nurses, and technicians throughout the lab that made us feel welcomed and allowed us to learn and grow everyday. Thank you to Dr. Mutlu for giving my group and I the opportunity to work with the gastroenterology department and explore the GI lab. Thank you to Dr. Felder and Dr. Browne for creating this program and mentoring us each week. Lastly, thank you to my group members Jamie Rae Cuartero, Klaudio Haxhillari, Jeremy Yuan and all other participants for an incredible six weeks.
About
Year: Senior Biomedical Engineer with a concentration in Neural Engineering
Area of Research: Gastroenterology
Contact Information: lkhadr2@uic.edu