
Lina Kiswani
4th year Biomedical Engineering Student
Obstetrics and Gynecology (OB/GYN)
Email:
Week 1: Good and Bad Designs in Clinical

Good Design: Samsung Hera W-10 Ultrasound Machine
This machine is an ultrasound machine with many advanced technologies paired with it. It has 2 monitors: ultrasound imaging and a screen with prompts for labeling or better-quality viewing of images. A series of buttons allow for the movement of images, saving the image, printing images, expansion of images, changing image colors, etc. There are 4 big outlets on the bottom for the probes used in the machine allowing them to way from the floor. It can also measure the baby’s heart rate, as well as, weight. This can help sonographers and doctors know if the baby’s measurements correspond with the trimester it is in. Even though this machine is a little big and difficult to move around, it can still be crucial to receiving the best ultrasound imaging for the patient.
Activity: Sonographers capture ultrasound images using the ultrasound machine. The patient can watch the images live on a separate monitor that is placed higher for patient comfort. The sonographer manages the images by measuring, labeling, saving, and printing the images. At the end of the visit, the sonographer tells the patient what the heart rate and baby’s weight is.
Environment: It is in an ultrasound room that is found in the clinic with very dim lighting. There is a curtain that is provided for extra privacy for the patient.
Interactions: Sonographers use the ultrasound machine with about 2.5 years of training to properly use and accurately read the images they take while the patient is lying flat on the hospital bed. Doctors can review the images taken for a diagnosis of the baby’s health.
Objects: The ultrasound machine, the hospital bed, the extra monitor
Users: Sonographers, Doctors, and patients
Bad Design: Masimo Cardiotocography Machine
This machine was something that I did not know about previously, so it was very interesting to learn more about. It is a machine that measures the fetal heart rate in response to contractions the mother may face. It is usually in use by patients who are 36 weeks and facing a specific health condition, that requires the baby to be monitored weekly until birth. It allows you to see the baby’s baseline heart rate and how it accelerates over that baseline. The protocol is to look for 2 accelerations (15 beats for 15 seconds) over 20-40 minutes to suggest the baby is reactive. I said this is a bad design because the machine can be loud. When the mother is strapped, you begin to hear the motion and heartbeat of a baby. With 2 patients at a time, it can get uncomfortable to have to hear the motions with the static that comes with it.
Activity: Nurses and other qualified techs strap patients onto a bed to conduct non-stress testing to make sure the baby’s heart rate is normal and reactive. They monitor the patient for 20-40 minute intervals. During this procedure, the nurses take the patient’s blood pressure to make sure it is within range.
Environment: A clinic room that has 3 beds with a curtain for privacy and an extra room on the side to analyze the patient amniotic fluid index using an ultrasound.
Interactions: The nurse straps the patient with the monitors being placed against the baby’s back. They record and analyze the data to make sure the patient is getting the necessary care.
Objects: The CTG machine, the hospital beds, the nurse’s monitor
Users: Nurses, Patients, Doctors, any qualified tech
Week 2: Secondary Research
Non-stress testing (NST) is one part of antenatal testing. It detects fetal movement when the mother is experiencing a high-risk pregnancy. There are specific indications and guidelines as to when a mother begins doing antenatal testing. According to a sheet in the NST room, many conditions start at 32 weeks and continue weekly until they have the baby, but it can range from 28 weeks to 36 weeks. NST is aiming to find 2 accelerations (15 beats for 15 seconds) within a 20-40 minute range.
Peer Review Paper: Prenatal Nonstress Test
In the article, Non-stress testing is explained as a type of antepartum surveillance that monitors the fetal well-being and fetal heart rate. “It is a non-invasive test used for the surveillance of high-risk pregnancies when the fetus is judged clinically to be at risk for hypoxemia or increased risk of death.” [1]. It can be completed by trained personnel like nurses, physicians, and midwives. It is more accurate and reactive for fetuses that reach 32 weeks, which means the fetus can have 2 accelerations of 15 beats for 15 seconds over the baseline fetal heart rate. For pre-term fetuses, from 24 weeks to 32 weeks, the acceleration counts as 10 beats for 10 seconds because of the immaturity of the fetal heart. If the baby is not reactive, the patient is kept for a little longer to differentiate between the fetus’s sleep cycle and if the fetus is experiencing hypoxemia or asphyxiation. Trained personnel can use vibroacoustic simulation (VAS) to get the baby more active if they are in their sleep to get a quicker reaction. Then, if still unreactive, a full biophysical profile needs to be completed.
The equipment that is used is a cardiotocogram, which is an electric fetal monitor. “The modern equipment records fetal heart rate pattern, contractions, fetal cardiac activity, maternal blood pressure and heart rate on a graph.” [1]. Two transducers are used: a Doppler transducer, for fetal heart monitoring; and a pressure transducer, for uterine contraction monitoring. They are placed on the abdomen with straps to keep transducers in place.
References:
[1]O. D. Umana and M. A. Siccardi, “Prenatal Non-stress Test,” PubMed, 2020. https://www.ncbi.nlm.nih.gov/books/NBK537123/
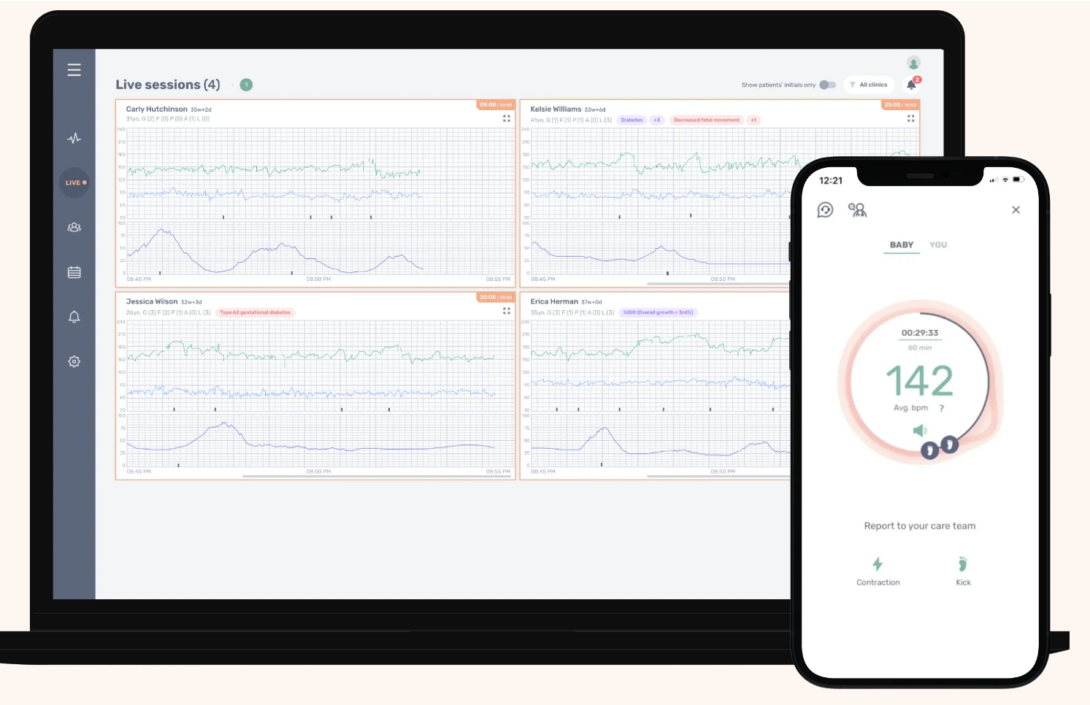
Commercial Solutions: INVU by Nuvo-Group LTD
INVU is a Non-stress test that can be done at the comfort of the home with a prescription from a physician. It monitors fetal heart rate, as well as, maternal heart rate. Nuvo-Group LTD. emphasizes on the convenience of INVU because it allows mothers to complete any necessary fetal monitoring at home without frequent trips to clinics or hospitals. It highlights the benefits it has in remote areas to improve health outcomes. According to testimony on the NUVO website, it is easy to use and produces accurate results [1]. Since it is FDA approved, it is shown that their key features are: wearable sensors that incorporates electrocardiogram (ECG) and phonocardiogram (PCG) sensors, and a mobile application that allows for real-time tracking and delivery of the information to healthcare personnel. [2] Similarly to any NST, it is done at around 32 weeks of preganancy. This technology found great satisfaction from patients because they are not troubled with the extra stress of going to the clinic to get the procedure done weekly, or even twice a week.
References:
[1]“Nuvo – Solutions,” www.nuvocares.com. https://www.nuvocares.com/solutions
[2]J. Dear and Hogan, 2021. Accessed: Jul. 11, 2024. [Online]. Available: https://www.accessdata.fda.gov/cdrh_docs/pdf21/K210025.pdf
Week 3: Need Statement with Iterations
Primary Observation
A: Patient is in a temporary room waiting for the indications of labor, so that they can give birth. The doctor enters the room and puts on sterile gloves and adds a gel to their hand. They insert their hand into the cervix to and manually measure how dilated the patient’s cervix is. E: A triage room, which is a temporary room used for assessment of patient. I: The doctor is measuring the cervix by hand. O: The doctor’s hand, gel, gloves. U: Doctors, pregnant mothers.
Secondary Research
Although cervical dilation is not a reliable indication of beginning the labor process, it can be a crucial step to check on the progression of a patient in labor. [1],[2]. Digital vaginal examination (DVE) is a cervical measurement exam that requires doctors to manually check the size of the cervix with their hands. This is the most common method of measuring cervical dilation, but it may not be the most accurate estimation. This is because it is a subjective exam based on the doctor’s experience and can be painful for the patient. It has been shown that only 50% of exams are accurate. [2]
Business Research
Since the most common practice of the exam is using the hand, we can take a look at the salary of an attending doctor and resident doctor in comparison with the number of deliveries done in the USA per year.
OBGYN Attending = $334,870 / year [3]
OBGYN Resident = $70,958 / year [4]
# of labors in USA = 3.67 million / year [5]
TAM / attending = $334,870 * 3.67 million = $1.2 trillion
TAM / resident = $70,958 * 3.67 million = $ 260 billion
Another method to check the cervical dilation is to use a transvaginal ultrasound machine. While this may cause the patient to feel pressure from the exam, it can give more standard results on the dilation of the cervix.
- GE Healthcare Versana Family Ultrasound for Primary Care: It is said to create powerful 3D and 4D imaging. It has a variety of probes to choose from for the necessary examination.
- Phillip’s Affiniti 70 Ultrasound System: It has adaptable imaging technology to help with accurate dilation measurements. It shows the blood flow and can allow for live collaboration.
The total addressable market for the ultrasound is going to focus on the price of the ultrasound in coordination with the number of hospitals in the US, if there is a need for only one ultrasound in the Labor and Delivery Unit.
Price of Ultrasound = $ 27,000 [6]
Number of Hospitals = 6,120 Hospitals [7]
TAM = $27,000 * 6120 = $ 165 Million
Need Statements
Iteration 1: OBGYN clinicians (population) are measuring the patient’s cervix by hand (opportunity) which needs a more accurate tool for detecting the size of the cervix (outcome).
Iteration 2: OBGYN clinicians (population) are measuring the patient’s cervix by hand, which can be subjective to the clinician’s training (opportunity), and needs a more accurate tool for detecting the size of the cervix (outcome).
- In the second iteration, the opportunity expanded the information as to why the outcome was needed. This can increase the desirability of changing the current methods of measuring the dilated cervix.
References:
[1] “What Happens When You Arrive at the Hospital in Labor,” Lamaze International. https://www.lamaze.org/Giving-Birth-with-Confidence/GBWC-Post/what-happens-when-you-arrive-at-the-hospital-in-labor-1
[2] Z. Mohaghegh, S. Jahanfar, P. Abedi, and M. A. A. El Aziz, “Reliability of ultrasound versus digital vaginal examination in detecting cervical dilatation during labor: a diagnostic test accuracy systematic review,” The Ultrasound Journal, vol. 13, no. 1, Aug. 2021, doi: https://doi.org/10.1186/s13089-021-00239-1.
[3] N. M. MD, “What Is the Average Obstetrics and Gynecology (OBGYN) Physician Salary in 2024?,” physiciansidegigs, May 10, 2024. https://www.physiciansidegigs.com/average-obgyn-salary
[4]“OBGYN Residency Stipends & Benefits | Summa Health,” www.summahealth.org. https://www.summahealth.org/medicaleducation/residency-programs/obstetrics-gynecology/stipends-and-benefits (accessed Jul. 22, 2024).
[5]Centers for Disease Control and Prevention, “FastStats,” www.cdc.gov, Nov. 27, 2019. https://www.cdc.gov/nchs/fastats/delivery.htm
[6]“Philips Affiniti 70,” Peak Medical. https://www.peakmedsolutions.com/product-page/philips-affiniti-70?gad_source=4&gclid=CjwKCAjw4_K0BhBsEiwAfVVZ_1-wEdtuuMg2acyBtyU3Ijwz7Bs_ob0FPZKeMyce_L6Tsaz-RquwGxoCfgUQAvD_BwE (accessed Jul. 22, 2024).
[7]“Fast Facts on U.S. Hospitals, 2024 | AHA,” www.aha.org, Jan. 16, 2024. https://www.aha.org/statistics/fast-facts-us-hospitals#:~:text=There%20are%206%2C120%20hospitals%20in
Week 4: Revised Need Statement with IDEO
Revised NS: OBGYN clinicians need a method to measure cervical dilation accurately to reduce the subjectivity in the examination and ensure the safety of the mother and baby.
This revised need statement generalized the outcome. So rather than just focusing on a specific tool, which can sound closer to a solution, it focuses on wanting any new way of measuring the cervix that can solve the current issues with measuring the cervix dilation. It also adds to the patient’s well-being because the examination can be painful and a little risky for the patient.
IDEO Components
Desirability:
Physicians/clinicians can find this need desirable because measuring the dilation of the cervix is a crucial part of monitoring the progress of labor. Finding a method that can give accuracy can change the game, essentially. When I was observing the Labor and Delivery Unit, there was a dilation chart to show what the size of cervix looks like going from 1 cm to 10 cm. The residents and attending were looking at this tool and comparing their knowledge to what the tool shows. Even though they said some of it feels right, there were chart sizes that they did not agree with. This can show the subjectivity that can come with measuring the cervix. Removing that aspect can lower the stress and allow the doctors to make decisions, like mode of delivery, accurately without any bias getting in the way.
In addition, it can desired by patients as well because the cervical examination can be painful. In many of the articles I read, they had all acknowledged how uncomfortable the exam can be for the patient. Having this pain reduced can be seen as a positive step. Another aspect to look at for the patient is that when they do many cervical exams throughout the labor process, they have the ability to introduce new bacteria to the mother on the baby. Although it is a low risk because physicians make sure they have complete sterility, it is always a possibility.
Feasibility:
This need does seem to be feasible or attainable because there are many imaging sensors that can be used for this project. It becomes a matter of proper integration of the sensors to have the program work in the desired way. Since OBGYN is a strong user of ultrasounds, they already have high training with imaging technology, so integrating a tool tp use imaging sensors for the purpose of measuring the cervix can blend in seamlessly with the training they have with the current ultrasound machines.
Viability:
There is a strong demand in the market because there are a lot of labors that occur within the year, so finding an accurate method of checking progression is needed. This can help us to reduce any errors that can come with maternal and neonatal care, which can justify the cost of the production. Focusing on the accuracy of cervical measurement can cause less complications in the delivery and creating a smoother process as a whole. This can help lower the healthcare costs that are associated with labor and delivery.
–
While in the Labor and Delivery OR, I noticed that the residents and supervising doctors, that were performing the surgery, were all on footstools to help reach the height of the examination table. After discussing with the resident, why the food stools are needed, she had told me it was because the bed has a minimum height it can have and cannot go lower than that. In addition to needing a surgical stool, there is no sterile method moving the stool to either get closer to the examination table or further from the table during the surgery. Being on a higher stool, surgeons have a higher risk of facing tripping hazards, which can be detrimental in surgery. With the limited mobility, the surgeon can be highly uncomfortable and experience musculoskeletal injuries from bad posture. Overall, it is a much greater struggle to have to need a step stool, or more stacked on top of eachother, to be able to complete the surgery properly.
New Need Statement:
Surgeons that use surgical stools (population) need an ergonomic and safer method of reaching the examination table (outcome), in order to reduce the hazards and injuries that are associated with the practice (opportunity).
Week 5: Storyboards
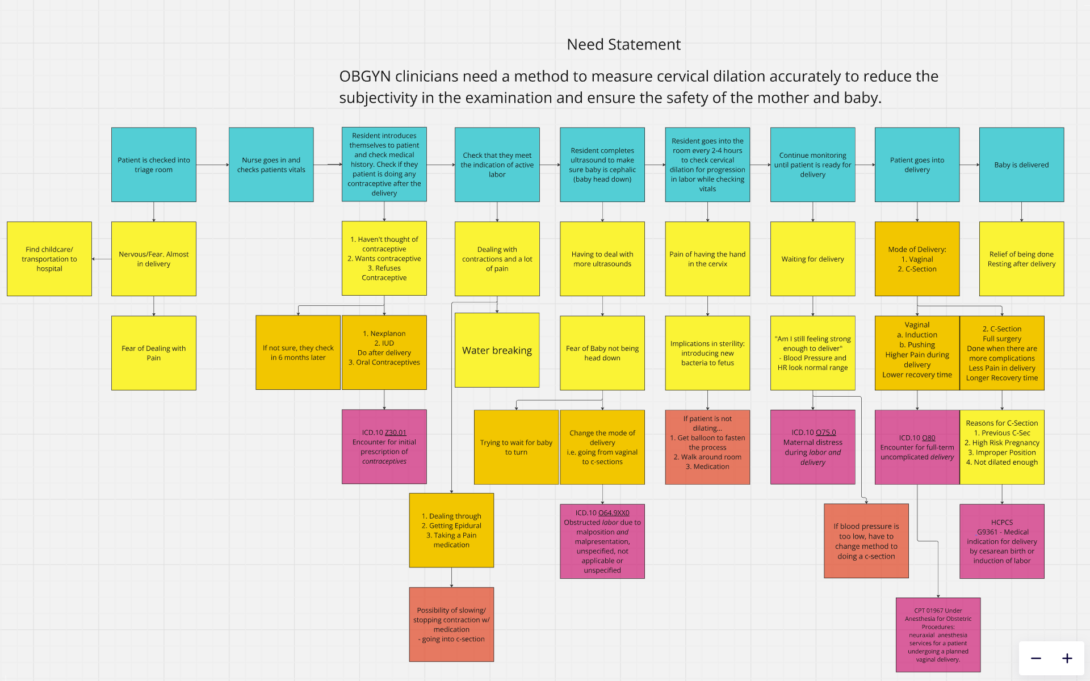
Legend:
Blue = Journey
Yellow = Pain Points
Orange = Decision points
Red = Failure
Pink = Billing Codes
Week 6: Reflections and Recommendations
OBGYN Clinic:
Coming to the end of this opportunity, I’m grateful that I got to undergo such a unique experience that allowed me to shadow physicians and authorized personnel around three distinct locations in the OBGYN Clinic. In the ultrasound department, I learned how important technology and proper training for ultrasound machines are. The high-tech nature of the ultrasound machines far exceeded my expectations. I learned about the necessary scans in the pregnancy journey and the details ultrasonographers focus on. This experience gave me a deep appreciation for the complexity of the equipment and the precision required to use it effectively. In the OB High-Risk Clinic, a significant lesson is always listening and empathizing with patients on this journey. Experiencing a high-risk pregnancy brings many challenges, so physicians must be patient with them to allow for a smoother experience for both sides. The last department in OBGYN is the Labor and Delivery Unit which is such a fascinating place to be. One of the most important lessons to learn in this area is timing. The fast-paced environment requires every step to be executed efficiently and accurately to ensure a safe and successful delivery.
Program:
A key lesson I’ve learned is to always make the most of your time. It taught me the importance of always being engaged in the didactics and being as productive as possible since one week can make such an impact on our learning. Any type of procrastination can easily set a person back.
Recommendations for Future Participants:
Take advantage of this opportunity! It is a very unique experience, especially as an engineer, since you may not always get a chance to engage in a hospital setting. I found it incredibly valuable to observe the OBGYN department’s daily functions, so make sure to always take notes of it all. Being able to experience the challenges firsthand can help ensure that your future need statement is something you are passionate about, which can influence your future work in senior design (BME students) or capstone projects (IMED students). Another thing is do not hesitate to ask questions. It may be a little intimidating, but everyone is usually happy to answer, no matter how small the question. My final piece of advice is to fully engage in this opportunity because it does go by fast.