
Klaudio Haxhillari
Student Participant
Week 1: A Good Design and a Bad Design Heading link
During week one, I had the opportunity to observe the operations in the endoscopy lab. Some of the most common procedures in the lab include colonoscopies and upper endoscopies. The lab is set-up so that when patients arrive they are placed in a pre-operation room in which they are seen by the nurse who ensures accurate chart information. Then they are seen by the doctor who assesses patient risk and then obtains informed consent from the patient. The patient is then brought to the procedure room, sedated, and the procedure is performed. When the procedure is complete, the patients are transferred to a post-operative recovery room in the lab for the sedation to wear off and are provided with preliminary findings.
A GOOD DESIGN
A design that I believe worked well was the informed consent tablet. Previously, the gastroenterologists were required to take part in a process that involved several extra steps that absorbed crucial time and effort. The informed consent tablet brought into the lab this week as a solution helps mitigate some of the prior issues. The tablet allows a physician to scan a QR code on the patient’s chart, confirm the DOB and then – after having an informed discussion about the procedure – have the patient sign so that it is submitted and added directly to the chart. Such faster and more efficient solutions are needed in medicine and this tablet does a great job of doing so.
Looking at this design through the AEIOU lens we have:
Activities: Gastroenterologists are discussing the procedure with the patient including benefits and risks and then obtaining an informed consent which includes a signed form.
Environment: The patient is in the pre-procedure room with the doctor. The doctor has the patient’s chart on the computer and the consent form on the tablet.
Interactions: The doctor explains the procedure to the patient with risks and benefits. The doctor scans a barcode on the patient’s chart with the tablet and the form opens after patient date of birth confirmation. Patient asks any questions and then signs the form on the tablet.
Objects: The tablet is used to display the form and automatically upload to the patient’s chart.
Users: The gastroenterologist uses the tablet to obtain proper consent documentation in a few steps. The patient signs the form.
A DESIGN THAT NEEDS IMPROVEMENT
A design I believe to have been underdeveloped was the separation of the vitals screen and the scope screen. The vitals are presented on a different monitor which is in a different location than the scope screen. This means a doctor has to switch their gaze from the scope screen to the vitals screen when they want to check the status of a patient. Based on my observations, this issue was exacerbated further when the machine that usually gives off an alarm to notify the doctor of vitals falling out of normal range was broken. Vitals are crucial to ascertaining the patient is tolerating the procedure and helps guide the appropriate amount of sedation. Unfortunately, underdeveloped designs such as this one are inconvenient and waste time. Thus, room exists for the creation of more user centered designs in medicine.
Looking at this design through the AEIOU lens we have:
Activities: Gastroenterologists are performing a procedure while using a scope and viewing the scope screen to navigate the location of the scope in the GI system at any given time.
Environment: The procedure room is set up with a patient lying on a bed with the scope monitor above them. The vitals monitor is at a lower height than the scope monitor and off to the side.
Interactions: The doctor is examining the GI system for abnormalities and attention is important to reduce the chances of missing abnormalities such as smaller polyps. They occasionally divert their gaze in order to check the status of the patient by viewing the vitals on a distant screen.
Objects: Several separate monitors are present including one for the scope view and one for the vitals in different places.
Users: The gastroenterologist, nurse, and technician all use the vitals to monitor the status of the patient. The gastroenterologist also makes the decision on how much sedation the patient should receive based on vitals.
Week 2: Preparation and Pre-procedure Process for Colonoscopies Heading link
Preparation and Pre-procedure Process for Colonoscopies
Colorectal cancer is one of the most common cancers in the United States and colonoscopies are a common procedure in the GI lab (CDC). In this story board, I represent the process and preparation that occurs prior to the start of the procedure. I conclude with a related review paper that focuses on bowel preparation prior to colonoscopies.
1. Patient is recommended to undergo colonoscopy for further evaluation of their GI problem (Image Source: Self).
Pain point: Patient may be worried about undergoing a procedure.
2. Patient schedules an appointment for the procedure (Image Source : Microsoft Stock Images).
Pain Point: Patient may not have the time for the procedure and may need to miss a day of work.
3. Patient is verbally told of instructions and provided with an instruction packet on bowel preparation (Image Source : Microsoft Stock Images).
Pain Point: Patient may be anxious to clarify instructions at the time or may not have any questions until later.
4. Patient purchases bowel preparation items (Image Source: Self).
Pain Point: There may be out of pocket costs to purchase items.
5. Patient follows bowel preparation instructions (Image Source : Microsoft Stock Images).
Pain Point: Instructions may be difficult to follow depending on medical literacy or language barriers. Bowel preparation can be difficult to tolerate.
6. Patient shows up to the GI lab and checks in on the day of the procedure (Image Source : Microsoft Stock Images).
Pain Point: It may be difficult to find the GI lab at a large hospital.
7. Patient waits in the waiting room to be called (Image Source : Microsoft Stock Images).
Pain Point: Long wait times decrease patient satisfaction.
8. Patient is brought into a pre-procedure room where their history and chart information is confirmed for accuracy by staff (Image Source : Microsoft Stock Photos).
Pain Point: Patient may be exhausted from repeating information several times.
9. Gastroenterologist recaps basic chart information and ensures that the patient took the bowel prep correctly (Image Source : Microsoft Stock Images).
Pain Point: Patient may believe that they took the bowel preparation correctly even if they did not. Or patient may be afraid to admit that they did not take the full prep if they did not do so.
10. Gastroenterologist confirms appropriate conditions such as sedation or anesthesia that will be needed for the patient (Image Source : Microsoft Stock Images).
Pain Point: If a patient was scheduled through another provider and was selected to have the procedure done with sedation, but it was then determined by the expert that they will actually require anesthesia it will take up time as anesthesia needs to be arranged with the anesthesiology team.
11. Gastroenterologist obtains informed consent from the patient about the procedure (Image Source : Microsoft Stock Images).
Pain Point: Adds more tasks that take up time in the procedure day.
12. Patient signs the consent packet on the tablet which gets automatically updated to the chart (Image Source : Microsoft Stock Images).
Pain Point: If the technology fails to upload there would be no proof of consent which may pose a legal problem.
Review Paper: Bowel Preparation for Colonoscopy in 2020: A Look at the Past, Present, and Future
This review focused on bowel preparation including types of products used for preparation and barriers to achieving adequate preparation. The authors found that when technology was added into patient education about bowel preparation there was improved adequate bowel preparation rates. When videos and multimedia were used patients also had less anxiety about the procedure. The review also looked at toleration to the various bowel preparation products out on the market. It found that the volume needed to ingest, taste of the products, and cost were important factors for compliance and tolerance to the preparation.
Source: Millien, V. O., & Mansour, N. M. (2020). Bowel preparation for colonoscopy in 2020: a look at the past, present, and future. Current Gastroenterology Reports, 22(6), 1-9.
Week 3: Needs Statements Heading link

This week, I focused on the endoscope in particular as it is one of the most common and important tools used in GI. While the scope has improved over the last few years it is not perfect and can be further improved on. Repetitive use and torquing of the endoscope, turning the control wheels, and unnatural body positioning puts GI physicians at high risk of work related injuries, many of which are musculoskeletal in nature (Harvin, 2014).
Needs statements are developed to identify and summarize the purpose of a project. I will be using the components Population, Opportunity, and Outcome to create 3 iterations of a needs statement regarding the ergonomics of GI procedures.
Needs Statement #1: Gastroenterologists work in a non-ergonomic workspace and need a way to reduce musculoskeletal injuries.
Population: Gastroenterologists
Opportunity: Non-ergonomic workplace
Outcome: Reducing musculoskeletal injuries
Rationale: Gastroenterologists are the doctors I have been observing performing procedures therefore I selected them as my population. An opportunity for improvement is the workplace design as many aspects of the design are lacking in terms of ergonomics. For instance, the many monitors that are utilized lead to neck strain and the several maneuvers required with the current endoscope lead to musculoskeletal injuries. The outcome that would be assessed is reducing musculoskeletal injuries as currently research shows a high rate of these injuries among gastroenterologists (Harvin, 2014).
Needs Statement #2: Gastroenterologists utilize a non-ergonomic endoscope and need a way to reduce musculoskeletal injuries.
Population: Gastroenterologists
Opportunity: Utilization of a non-ergonomic endoscope
Outcome: Reducing musculoskeletal injuries
Rationale: Gastroenterologists are the population as they are the main handlers of the scope. I changed the opportunity for improvement to be the non-ergonomic endoscope to focus on a more specific issue that has opportunity for improvement. The outcome would remain the same as the goal is to reduce musculoskeletal injuries.
Needs Statement #3: Gastroenterologists utilize a non-ergonomic endoscope and need a way to reduce upper extremity musculoskeletal injuries.
Population: Gastroenterologists
Opportunity: Utilization of a non-ergonomic endoscope
Outcome: Reducing upper extremity musculoskeletal injuries
Rationale: Gastroenterologists remain the population as they are the main handlers of the scope. Opportunity for improvement remains the same as I would like to focus on the non-ergonomic design of the scope. I altered the outcome as there are many different types of musculoskeletal injuries that may require different solutions so I focus on upper extremity musculoskeletal issues in this needs statement.
Source: Harvin G. Review of musculoskeletal injuries and prevention in the endoscopy practitioner. J Clin Gastroenterol. 2014 Aug;48(7):590-4.
Week 4: Patents Heading link
This week, my group surveyed gastroenterologists in the department about their view on the ergonomics of the endoscope. What we found was that people with smaller hands tend to have more issues with the current endoscope design. The main problem stems from the dials of the endoscope. The smaller dial becomes difficult to reach and maneuver for people with small hands leading to increased strain.
Going off the observations this week and the needs statement from last week, “Gastroenterologists utilize a non-ergonomic endoscope and need a way to reduce upper extremity musculoskeletal injuries”, I searched for a related existing patent.
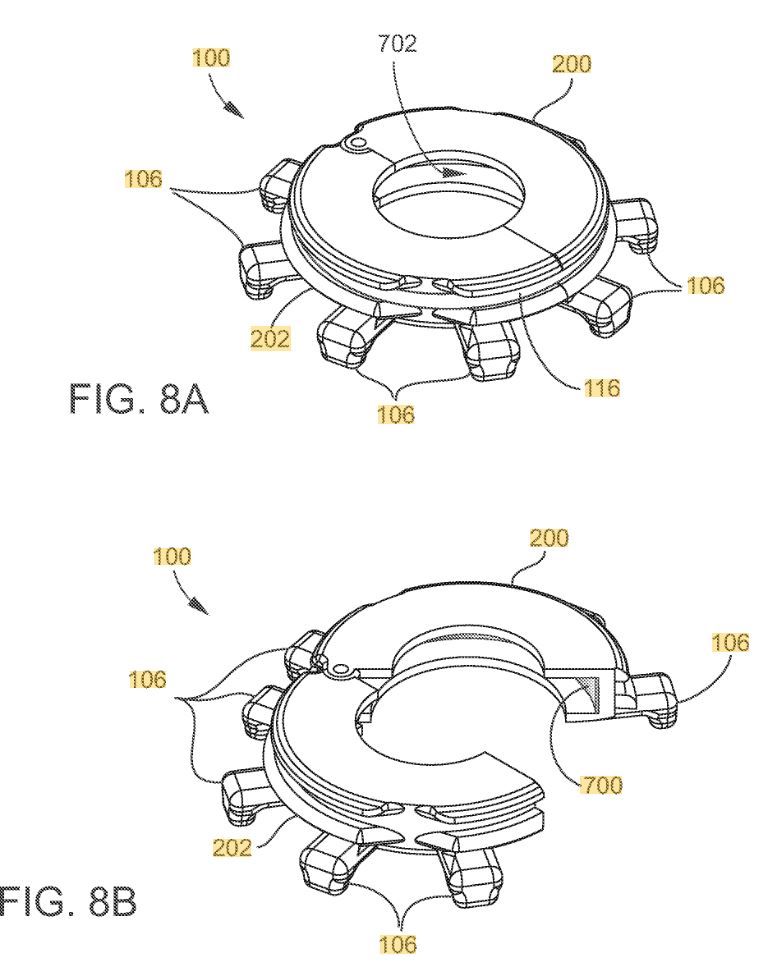
The patent is titled “Devices for assisting manipulation of input mechanisms of medical instruments.” The patent describes the device as one that assists modifications of input mechanisms relating to medical instruments. The body of the device surrounds and attaches to the input mechanism. It also includes protrusions attached to the body which extend in the direction towards the medical instrument. The body has two parts that attach together to compress against the input mechanism. Further claims describe the medical instrument as an endoscope and the input mechanism as the deflection knob of an endoscope. The body is made of either nylon, polylactic acid (PLA), acrylonitrile butadiene styrene (ABS), or high impact polystyrene (HIPS). The protrusions are between 0.3 and 0.4 inches and are made of ABS or PLA. I have included one of the images provided in the patent to show a visualization of the device.
The device does a good job at solving the problem of people with smaller hands having issues with reaching the dials. This unmet need was shown to exist based on the primary data collected by my group mentioned above and secondary literature as discussed previously. The device attempts to solve the issue as essentially a snap-on that goes onto existing endoscopes. It allows for reduced strain and greater reach of the smaller dial by increasing the radius with the clip on device.
Week 5: Total Addressable Market Heading link
This week, I researched more into the viability of a potential product based on the needs statement I have focused on the past few weeks, “gastroenterologists utilize a non-ergonomic endoscope and need a way to reduce upper extremity musculoskeletal injuries.” While working through the analysis, I realized the numbers are vastly different depending on whether the device would be an attachment or a new endoscope altogether and so I decided to perform a market analysis on these segments individually. Several estimations went into the calculations and I describe them for each below.
The first analysis I performed was on the solution if the device were to be an attachment that goes on to existing endoscopes. Presumably, every gastroenterologist would need one device that is ergonomically suited for them and they can take it on and off endoscopes throughout the day. Therefore, it is important to determine how many gastroenterologists there are worldwide. This was estimated by taking the total number of physicians in the world which is known to be about 9.2 million (Crisp & Chen, 2014) multiplied by the percentage of gastroenterologists of total physicians in the United States, 1.6% (AMA, 2019). This gives a rough estimation of 147,200 gastroenterologists in the world. Therefore, there would be about 147,200 device attachments. Scopes are replaced every 5 years and so if a similar time frame is applied to our device there would be an annual demand of 29,440 attachment devices. The device attachment potential cost would be priced around $500. Thus, the Total Addressable Market= 29,440 yearly attachments demand x $500 cost = $14,720,000.
The second analysis would be based on if the device solution was a new, more ergonomic endoscope altogether. While the total amount of GI endoscopes in the world is unknown I made an estimation based on the amount of endoscopes at UIH. There are approximately 40 endoscopes at UIH and 25 gastroenterologists so there are about 1.6 endoscopes per gastroenterologist. Using the above calculation that there are about 147,200 gastroenterologists worldwide and if we multiply 1.6 gastroenterologists per endoscope we would have about 235,200 GI endoscopes worldwide. Since the endoscope replacement rate is about every 5 year dividing the number by 5 we get 47,104 annual endoscope demand. An average endoscope costs about 30,000 (Ciocirla, 2019). Using these numbers we get Total Addressable Market = $30,000 endoscope cost x 47,104 yearly cost = $1,413,120,000.
Sources:
American Medical Association. AMA Physician Masterfile (December 2019); U.S. Census Bureau, Population Division. Annual Estimates of the Resident Population by Single Year of Age and Sex for the United States and Puerto Rico: April 1, 2010, to July 1, 2019.
Ciocirlan M. Low-cost disposable endoscope: pros and cons. Endosc Int Open. 2019 Sep;7(9):E1184-E1186. doi: 10.1055/a-0959-6003. Epub 2019 Aug 29.
Crisp, N., & Chen, L. (2014). Global supply of health professionals. New England Journal of Medicine, 370(10), 950-957.
Week 6: Lessons Learned and Advice for Future Students Heading link
Lessons Learned
Spending time observing in the field of Gastroenterology was a valuable experience this summer. There were several interesting procedures and the ability to navigate through the GI system is fascinating. Due to the procedural aspect of the field, many devices are used which open the opportunity for innovation.
Throughout the weeks, I noticed that identifying issues and then focusing on ones that meet criteria where innovation would be successful was more challenging than originally expected. For example, some issues discovered were likely to require costly solutions and therefore the solution may not replace the current workarounds for that problem. Additionally, some problems in healthcare might not be best solved with a new device at all, but would rather be best addressed by quality improvements or process measures.
When issues that seemed like they could be solved through an innovative device were discovered, then many factors that assess the need came into play such as desirability, feasibility, and viability. I learned more about these components in the program, which helped me analyze needs through these factors to discover a problem worth working on.
Throughout the immersion, documenting observations in a journal was important in remembering details later on. As I progressed in the program and became more familiar with the field, it was helpful to connect points to earlier procedures I had seen in the endoscopy lab. Underlying themes developed and it was helpful to categorize opportunities into different sections for the overall process.
The endoscope is one of the most important tools used in the field of gastroenterology. Although it works well, a device so commonly used is due for innovation. My group focused and presented on the ergonomics of the endoscope and we hope for more optimization of the device down the line.
Advice for Future Students
My advice for future program participants is to be as engaged as you can. The first few weeks are crucial because there is a lot of observation to take in, but it is also a great time to ask questions. At an academic hospital, there is always faculty that are happy to speak with you and welcome involvement. Importantly, be respectful to all patients, physicians, and staff as patient care is always ongoing and remains a priority. Best of luck!