
Kelly McConnell
2023 student
Pronouns: She/Her/Hers
Email:
Week 1 Heading link
This was my first week of the Clinical Immersion Program as part of the team partnering with the Pediatric Surgery Department. Our overall goal is to identify user needs through observation of the clinical environment, and then validate those needs. The majority of my time this week was spent in the operating room watching surgeries.
I thought the design of the hospital scrubs was a good design to fulfill the need of the hospital to be able to provide a standard and clean uniform for a large volume of employees. The operating room and the surrounding unit needs to be a controlled environment, which includes the garments people are wearing. The users include the physicians, nurses, technicians, students, and anyone else entering and working in the operating room area of the hospital. The hospital and the laundry services are also important users. Two features of the design that stand out to me are that the scrubs are reversible and color-coded. The reversibility removes a step for either the wearer or washer as they do not have to turn it right side out, as garments often become inside-out when taken off. The scrub size is indicated by the color on the collar and waist-tie.The color-coding helps the people washing and restocking the scrubs to more quickly identify the size to match the top and bottom and restock the scrub machine.
Figure 1: Example of color-coded reversible scrubs [1]
Another need in the operating room is to minimize exposure to the hazardous smoke created by the Bovie cautery devices, which are used to minimize bleeding during surgery. This affects the surgeons, nurses, patient, anesthesiologists, and anyone else in the operating room when the device is running. Figure 2 shows a Bovie cautery pen with a smoke evacuator. This design has several shortcomings. First, while the evacuation device presumably does reduce the amount of smoke released into the operating room, it appears that a lot of the smoke does still remain. Next, the placement of the open end of the tube near the electrode can cause obstructions, either getting in the way of the surgeon’s view or obstructing the use of the device on the tissue. Third, the evacuation tube needs to be connected to the machine to provide the suction. This causes extra force on the back of the cautery pen, both from the extra weight and the stiffness of the tube. I noticed this especially when the surgeon was trying to change their angle, and would have to wrangle the tubing so it did not interfere with their movement. The tube was also a problem when the surgeon was trying to put the instrument down, as it would often shift or move and someone else had to grab it. This problem of minimizing smoke exposure without impeding the ability of the clinical team to perform surgery is a difficult one, and could be an interesting design challenge.
Figure 2: Bovie® Orca™ Smoke Evacuation Pencil [2]
References
- Hospital Scrubs. Direct Textile Store LLC; 2023. Accessed July 9, 2023. https://directtextilestore.com/T180-Reversible-Scrubs-Ceil-Blue?sku=SPNTT180CBXL&gclid=Cj0KCQjwtamlBhD3ARIsAARoaEwqMCM7c1xLfVaMoADviblu8ZAsGzlkD2JmFUMgPXx6mTE2hX7dL_UaArO7EALw_wcB.
- Bovie® Orca™ Smoke Evacuation Pencil. Symmetry Surgical Inc.; 2023. Accessed July 9, 2023. https://symmetrysurgical.com/products/portfolios/electrosurgery/electrosurgical-accessories
Week 2 Heading link

I spent week two of CIP observing pediatric surgery primarily in the operating room, with one morning in the clinic. One of the frequent processes that I noticed was preparing the patient for surgery, as detailed in the attached figure. The process started with bringing the patient into the room on the transport bed, and then the patient moving to the surgical bed. Then devices and monitors were attached to the patient, like pulse ox sensor, leg compression wraps, a blood pressure cuff, and an IV line if needed. The patient is then put to sleep and while unconscious, intubated. The patient is then positioned for surgery, with various gel pads, pillows, and blankets, and strapped down to the table. The surgical site is shaved if necessary, then prepped with antiseptic solution. Then the surgeons scrub in, and set up the sterile drapes and towels around the site.
One of the pain points of this process was positioning the patient on the bed, especially when the patient had a lot of hair, or needed to be in an alternative position than lying on their back (supine). When the patient has a lot of hair, the hair interfered with the positioning of the head. For surgeries concerning the back or sides of the patient, the patient is positioned on their side, in a prone position, or some intermediate of the two. The anesthesiologist and/or surgeon has some gel pads and pillows to work with, but often need to improvise with rolled up sheets and blankets. This is an important step in the perioperative procedure, as improper positioning can lead to a variety of complications. Zillioux and Krupski identified examples of position injuries following minimally invasive surgery, both laparoscopic and robotic, including vision loss, neuropathy, compartment syndrome, and rhabdomyolysis. They described several mechanisms underlying these injuries: nerve stretching, pressure, and interruption of blood flow. Several factors increased risk of complications, such as increased procedure time, low or high patient BMI, and low functional status. Zillioux and Krupski detailed preventative measures that surgical teams can take: increase institutional awareness, careful choice of positioning to reduce slipping and pressure, and minimizing use of intraoperative drugs and positions that increase risk. They also mention several strategies identified in their literature review including a second timeout for long procedures (4+ hours) and the use of Doppler to assess blood flow. Overall, the process of preparing the patient is a critical part of the perioperative procedure to insure successful outcomes after surgery.
Reference:
Zillioux JM, Krupski TL. Patient positioning during minimally invasive surgery: what is current best practice? Robot Surg. 2017 Jul 14;4:69-76. doi: 10.2147/RSRR.S115239. PMID: 30697565; PMCID: PMC6193419.
Week 3 Heading link
One congenital malformation that has come up multiple times during our observation that usually requires surgical intervention is imperforate anus. This is when babies are born without an anal opening. In more complex cases, there can be fistulas connecting the digestive tract with the bladder, urethra, or vagina. During a case, the surgeon wanted to check for possible complications from his previous surgery to repair the patient’s imperforate anus. The surgeon used a nerve locator, which is a device that sends an electrical current through a small metal tip to stimulate nerves. The nerve is located when the innervated muscle twitches in response. The surgeon used two different nerve locators during the surgery, and was frustrated with the use of both of them, and expressed a desire for a reusable device that worked. I developed my needs statements from this moment.
Statement 1: Surgeons using intraoperative nerve locators need a reusable device.
This is a needs statement primarily based on the surgeon’s wants, and has several issues including embedding a solution. I then took a step back to reframe the needs statement.
Statement 2: Surgeons during surgery need a reliable and effective way to locate nerves.
After some review of the literature, I wanted to see how other people approached this problem, and were there other considerations that were important to this needs statement. Thallaj et al. compared a disposable and sterile nerve locator to a reusable and not completely sterile nerve locator that required communication with the anesthesiologist. Cost and availability were important factors, as well as how easy the device was to use. This informed further edits of the needs statement.
Statement 3: Surgeons during surgery need a reliable, easy to use, and cost-effective way to locate nerves.
Reference:
Thallaj A, Alotaibi WM, AlZahrani T, Abaalkhail AS, El-Sayed AAF, Al-Qattan MM. Intraoperative Nerve Stimulation During Brachial Plexus Surgery: Comparison Between a Totally Disposable Nerve Stimulator and Nerve Stimulator Normally Used for Nerve Blocks. Plast Surg (Oakv). 2017 Aug;25(3):171-174. doi: 10.1177/2292550317716120. Epub 2017 Jul 3. PMID: 29026822;
Week 4 Heading link
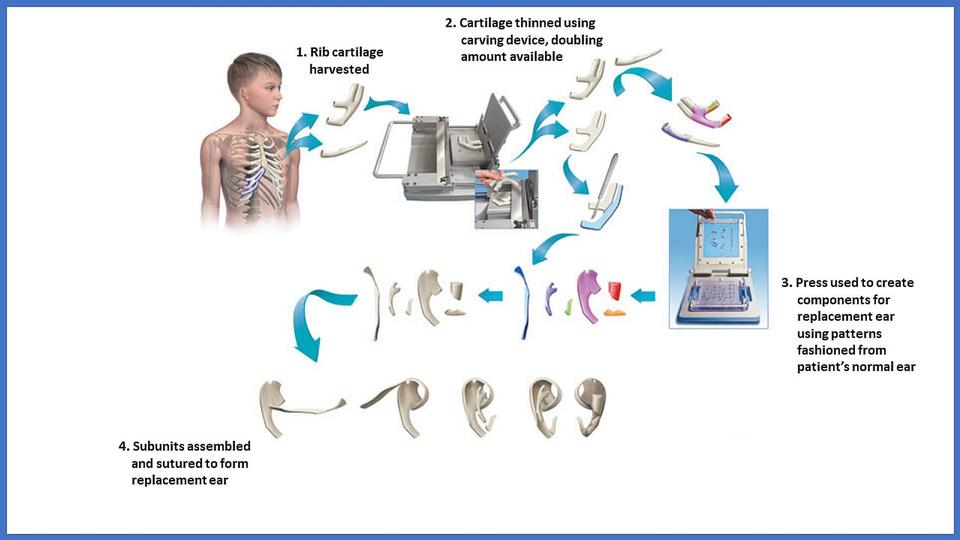
This week we observed a plastic surgery involving shaping an ear for a patient out of their own rib cartilage that was born without a left ear. After the cartilage was harvested from the patient, the surgeon used various scalpel blades, a dermatome blade, and a biopsy punch to shape the new ear. The surgeon mentioned that they used to have a set of tools more suitable for carving, but they were not approved by the hospital, and so they had to use the surgical tools available to them. The problem with this is that most of the tools are designed for straight cuts. And the only round cutting tool, the biopsy punch, has a set, very rounded contour. This makes carving out an ear, which has a lot of rounded edges and grooves, quite difficult. The surgery that we observed was a long one, lasting over 6 hours. One of the main factors contributing to the length was ensuring that the cartilage was the proper shape to match the contralateral ear. This experience lead to the development of the following needs statement:
Plastic surgeons during reconstructive surgery need a way to precisely shape autologous cartilage grafts to reduce surgical time.
Another potential outcome could also be to reduce the amount of autologous cartilage harvested from the patient, as the grafting process leaves a permanent defect in the patient’s ribs.
The linked patent describes a system to help address this need of shaping implants for nose, ear, and eyelid reconstructive surgery. The system consists of two tools. The first tool is a slicing tool, designed to cut the implant along the transverse plane to a desired thickness. The second tool is similar to a die cutter, that can punch out specific shapes of the implant. These shapes can be combined to create the desired three dimensional structure. The system does remove much of the complexity of the surgery, and thus increases the repeatability and consistency. The inventors also claim that their system reduces the amount of cartilage needed, minimizing harm to the donor site of the patient. Another major advantage that the inventors mention is the reduction of time needed to shape the implant. One disadvantage that I see is that this system described by the patient does not seem to allow for personalization of the implant. When we observed the ear reconstruction surgery, the surgeon and his team had clearly spent a lot of time designing the shape of the new ear, in order to match the patient’s existing ear. This does not seem to be possible using the patented system. Overall, the patented system does address the need statement for intraoperatively created ear implants by improving surgical time and making the surgery more accessible, however, at the cost of personalization of the new ear shape.
Week 5 Heading link
Need Statement: Plastic surgeons during reconstructive surgery need a way to precisely shape autologous cartilage grafts to reduce surgical time.
Continuing off the needs statement from last week, the goal is now to estimate the Total Addressable Market (TAM). This is the approximate revenue opportunity assuming the product archives complete market share. For the above need statement, I will focus on microtia reconstruction surgeries in the United States. Microtia has an incidence rate of 1-10 per 10,000 live births (Bly et al.). The number of births in the US in 2021 was 3,664,292 (FastStats). This gives an estimate of 366 to 3,664 babies born with microtia per year. If we make a generous assumption that every single baby born in the US with Microtia has reconstructive surgery, and we use the most frequent incidence rate, that will give us an average of about 3,664 surgeries per year. Biopsy punches are currently used at UIC during ear reconstruction surgery. These cost about $3 per unit (Sterile Disposable, Cen Med). Assuming 3 units are used per surgery, this gives a TAM of about $33,000 USD per year.
Works Cited
Bly, Randall A et al. “Microtia Reconstruction.” Facial plastic surgery clinics of North America vol. 24,4 (2016): 577-591. doi:10.1016/j.fsc.2016.06.011
Cen Med Enterprises PMD Sterile, Disposable Biopsy Punches:Surgical Tools:Biopsy | Fisher Scientific. Fisher Scientific, https://www.fishersci.com/shop/products/pmd-sterile-disposable-biopsy-punches-6/p-7162077. Accessed 7 Aug. 2023.
FastStats – Births and Natality. CDC/National Center for Health Statistics, 2023, https://www.cdc.gov/nchs/fastats/births.htm. Accessed 7 Aug. 2023.
STERILE DISPOSABLE BIOPSY PUNCH, 5.0MM. Surgical Tools, Inc, 2023, https://www.surgicaltools.com/8111/sterile-disposable-biopsy-punch-50mm/. Accessed 7 Aug. 2023.
Week 6 Heading link
This past week wraps up the final days of the clinical immersion program. I thoroughly enjoyed the experience observing pediatric surgery and learning more about need development and validation. Here are a couple of things that I learned from this experience to pass on to future participants. One, try to always have a pair of gloves on you in the OR. You never know when you need to pick something up or hold something for someone that you don’t want to touch with your bare hands. Two, careful bending over in scrubs if you have anything in your shirt pocket. Three, what you get out of this experience very much depends on your mindset and the energy you put into it. I appreciated having the opportunity to learn so much about how the hospital and the operating room works without having clinical responsibility. I would recommend this program to any future IMED students. It was a great way to gain clinical experience, see a bunch of interesting surgeries, and figure out the systems and processes that make the hospital run.
I would also like to thank Dr. Lobe, our clinical sponsor, and the general surgery residents, for this opportunity to observe their work and their time and effort answering all of our questions.