
Amirali Monshizadeh
2023 students
Biomedical Engineering
Email:
Week 1: Planned chaos
A real life OR, was nothing like Gray’s Anatomy. Even though there was much less drama, the stake’s seemed to be on a whole new level. I guess at its core, it was apparent that somebody’s life was at risk, and it felt tangible. The OR staff were chatting and talking like colleagues do in any work environment, but there was a calm seriousness to their conduct. More than any other jobs that I have seen, they seemed truly awake.
The first time seeing a patient lying face down on the OR table was shocking. She was covered with drapes and covers but the inevitably part of her back, where the surgery was to be had, was exposed, and served as a reminder that a human being is there. Alive, and with a family.
Talking to one of my friends, it seemed like the realization of human mortality was not universal amongst our group. He seemed much more successful in distancing himself away from the person who was lying there.
When the attending surgeon confirmed “incision”, the surgery was on its way. As much as I thought the cutting would trouble my stomach, it wasn’t the case at all. Perhaps it was the precise meticulous movement of the scalpel, or the thought that this was all for the betterhood of the patient. Either way, there was no going back now.
Looking back, it was the smell of burning bone, thanks to the cauterizer, that snapped me out of reconsidering millions of years of human evolution which led us to cutting one another and hammering each other’s spine. It made me realize that I was there for something more important: to identify problems with an engineering mindset.
And they were as follows:
Good design identified.
A – Level of patient consciousness is continuously monitored by the anesthesia team in the form of the BIS number. This number indicates consciousness of a patient. The lower the number, the less awake.
E – This information is displayed alongside all the patient vitals on the anaesthesia monitor
I – If the score fluctuates, the anaesthesiologists seeks the verification of the intraoperative neuromonitoring team before adjusting drug
O – if the patient becomes “light” i.e. starts waking up, the BIS number goes up and the monitor beeps
U – The main user is the anaesthesiology nurse who continuously monitors the bis number and is in constant communication with the rest of the team
Bad design identified:
A – During the surgery, the surgeon consults company representatives on the proper use of their specific novel tool
E – The reps are usually in the OR, and consult the nurse on the proper assembly of the tools before handing it to the surgeon
I – Surgical techs are experts on their respective tools. However, they often attempt to verbally communicate the procedure as opposed to explain with a physical model
O – Each novel tool has its town surgical tech which leads to somewhat overcrowding in the OR. Further, the techs have not shown the proper procedure to the surgeon prior to surgery
U – The surgeon and the techs verbally communicate with each other. The tech’s expertise sometimes leads to confusion by the surgeon who is unfamiliar with the device.
Week 2: Details matter
Week 2: details matter
Any process where a human is responsible for making decisions involves errors and inefficiencies. For every cut the surgeon makes, there is an error bound of possible mistake. Unlike most other work environments, however, these mistakes are not very reversible – you cannot uncut someone. That is why it is so important to create failsafes for the entire process to make sure that mistakes are caught at the brink of when they happen.
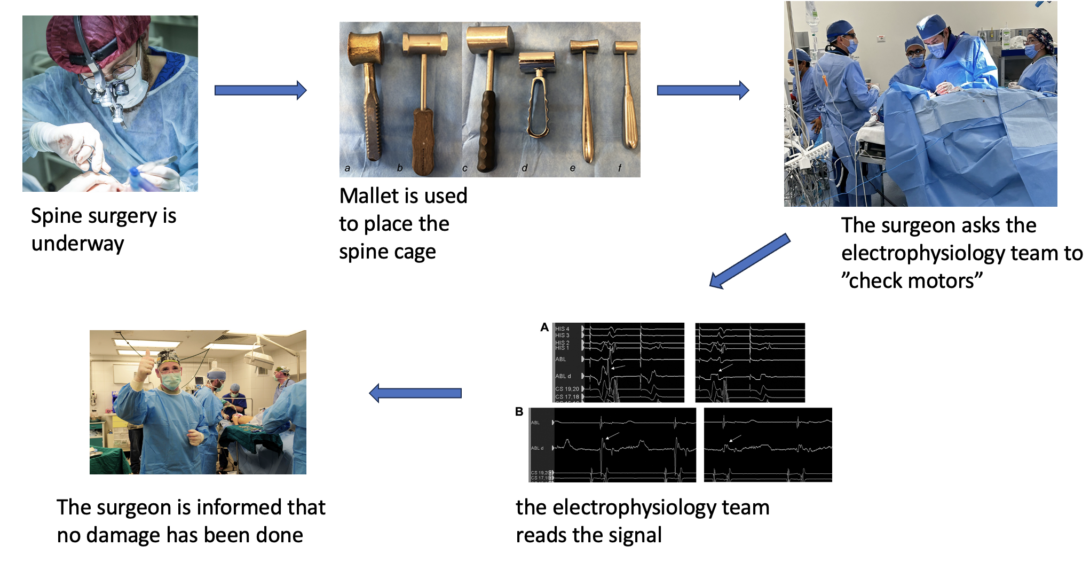
Every once in a while, in the OR, the surgeon looks up, glances around the room, systematically searching for the electrophysiologist and asks her to “check the motors”. What this essentially means is the surgeon asks for an electric shock to be delivered to the patient and for their response to be measured. If the patient suddenly jerks, then the surgeon knows that all the nerves are still intact, and the patient will be able to walk again.
I have decided to provide a detailed overview of the electrophysiology team, constantly ensuring that the motor and nerve functions are intact.
Week 3: Problems everywhere
There is no undo when you make a cut. Not CTRL + Z to reverse the catastrophic typo and give you unlimited attempts to get it right. As a surgeon, there is very limited room for mistakes. Every action has to be deliberate and exact. Similar to cooking the perfect steak, you can always cook it more but you can’t reverse it.
To this end, every tool at the surgeons disposal has been specifically designed to help the surgeon be more deliberate. In other words, tools help surgeons translate the specific desired outcome in his/her mind to what actually happens to the patient. For example, a surgeon may want to place a screw in a specific region of the spine. The exact placement of the screw as well as the angle is clear in the surgeon’s mind. In order for this vision to be manifested in the precise way on the patient, an intra-operative x-ray can be used to ensure the proper screw placement.
There are two types of mistakes a surgeon can make.
-
- The surgeon correctly manifested his/her personal vision on the patient but the perceived positive effect was incorrect. For example the surgeon wanted to place the screw in the coordinate x,y,z and did so accordingly. However, the screw should actually have been places in coordinates a,b,c.
- The surgeon incorrectly manifested his/her personal vision on the patient but the perceived positive effect was correct. For example the surgeon wanted to place the screw in the coordinate x,y,z but mistakenly placed it in a,b,c. Had the screw been placed in the correct position, the surgery would have been successful.
Technology can be used to minimize either type of error. The first type of error can be remedied by better diagnostics tool. If the tool was able to correctly help the surgeon determine the treatment, type 1 error would have been prevented.
The second type of error minimizes intra-operative surgeon mistake and will be the focus of my need statements.
- Neurosurgeons performing minimally-invasive endoscopic surgery need to be able to locate where bleeding is coming from
- Neurosurgeons using the StealthStation surgical navigation tool, need to be able to rely on the accuracy of the navigation map
- Neurosurgery OR staff rotating patients need to be able to flip the patient without placing their spine under stress
Week 4: A world of ideas
A patent is a powerful innovation tool and is arguably one of the very things that has made America the forefront of technological development in the modern times. The process of ideation and creation is long and arduous and at best… a coin flip. Not only do you need to identify a need, understand existing solutions and add to it, often times there is no guarantee of discovery. My favorite example from history textbooks is salvarsan 606 – the magic bullet against Syphilis. The number 606 is no accident – it took that many iterations of the drug for the scientists to find something that worked. They could have given up at any time before the 606th try and many lives would have been lost.
That is why the prospect of a patent is so important. It gives creators the chance to take ownership of their creation. Even though on paper, a patent is only a tool that enables the patent holder to litigate in court, in practice, and with historical hindsight, it has been used to give credits to major technological revolutions.
With this in mind, I set out to find the most relevant patent regarding my chosen need statement as describes in the week 3 blog. The kindest analogy I can find to describe searching for a patent is finding a needle in a haystack.
Title: Conductive optical element
International Patent Classification: A61B 1/253 (2006.01) GO2B 1/116 (2015.01)
Unfortunately, patent writers try to cast the largest net with their patents and encompass much more intellectual property than their invention actually warrants. For example the title of this patent is extremely broad and only uses 3 words. Comparing this to a typical research paper title that is often 40 words long, exemplifies my point even better.
This patent talk about a novel way of delivering energy to tissues during surgeries that are done with an endoscope. This energy is in electrical form and can be used to elucidate the shape and geometry of the surrounding area based on the specific conductance that is measured and subsequently compared to known conductances of what it should be.
By examining the patent, it seems like this idea has not been tested in vivo or even tested at all. This makes me highly skeptical of its efficacy to elucidate geometry because conductance of tissue is relatively constant and I do not see how slight variations can reveal shape. This is specially true as endoscopic surgery often uses a water filled cavity which would interfere with the inductance even more.
Week 5:
[week 5 blog]