
Somaya Motan
4th Year Biomedical Engineering Student
Email:
Week 1: Clinic & OR Instrument Designs {Getting Started!}

Good Design: Cystoscope Used in Cystourethroscopy
- Activity: The cystoscope facilitates precise visualization during cystourethroscopy procedures, allowing surgeons to accurately diagnose and treat conditions in the urinary tract. The cystoscope is equipped with ports/openings that allow for the insertion of additional instruments, enabling access to the kidneys, ureters, and bladder during surgical procedures.
- Environment: It is designed for use in sterile surgical environments, with a compact and ergonomic design that supports ease of handling and maneuverability.
- Interactions: Controls on the cystoscope are intuitive, enabling surgeons to adjust settings like focus and light intensity seamlessly during procedures.
- Objects: The high-resolution camera integrated into the cystoscope provides clear and detailed images, enhancing diagnostic accuracy and surgical outcomes.
- Users: Surgeons find the cystoscope easy to operate, enhancing their ability to perform procedures efficiently and effectively.
Bad Design: Electronic Health Record System for Patient Information
- Activity: The charting system is designed for documenting patient encounters and managing medical records but lacks efficiency in retrieving specific patient information quickly.
- Environment: It operates within the clinical setting but may not integrate seamlessly with other hospital systems, leading to fragmented data management.
- Interactions: Navigating the system interface to find specific patient data can be cumbersome and time-consuming for healthcare providers.
- Objects: While the system stores comprehensive patient records, its search functionality for specific information like test results or past procedures may not be optimized.
- Users: Healthcare providers require a more streamlined and intuitive interface for accessing critical patient data promptly during clinical decision-making.
Week 2: Breaking Stones: Laser Lithotripsy through Secondary Research
This week, I continued to make observations and perform interviews in the clinic and OR to investigate the devices and procedures in urology. During my observations, I noticed the challenge of collecting stone fragments generated during the lithotripsy procedure. To augment my primary research, I conducted secondary research on the laser lithotripsy device and related technologies. I identified a relevant peer-reviewed paper and a commercial solution/patent that align with my observations.
Secondary Research:
The study titled “The thermal effect of lasers in urology: a review article” provides a detailed analysis of the performance of the laser lithotripter. This paper is relevant to my observations as it investigates the efficiency of laser lithotripsy in breaking down kidney stones into smaller fragments, which is a crucial aspect of the procedure I observed.
The study aimed to evaluate the effectiveness of the Ho:YAG laser lithotripter in fragmenting different types of urinary stones. The researchers used an in vitro setup with synthetic and natural urinary stones. The stones were subjected to laser lithotripsy using the Ho:YAG laser, and the fragmentation process was analyzed.
The data were collected by measuring the size of stone fragments before and after the lithotripsy procedure. Statistical analysis was performed to assess the fragmentation efficiency. The study found that the Ho:YAG laser lithotripter was highly effective in fragmenting both synthetic and natural stones. The size of the fragments was significantly reduced, facilitating easier removal or passage.nThe Ho:YAG laser lithotripter demonstrates excellent efficacy in stone fragmentation, making it a valuable tool in urological procedures. However, the study also highlighted the need for effective methods to collect the resulting fragments.
Puliyath, N., Venugopalan, A.V., Das KV, S. et al. The thermal effect of lasers in urology: a review article. Lasers Med Sci 39, 6 (2024). https://doi.org/10.1007/s10103-023-03948-2
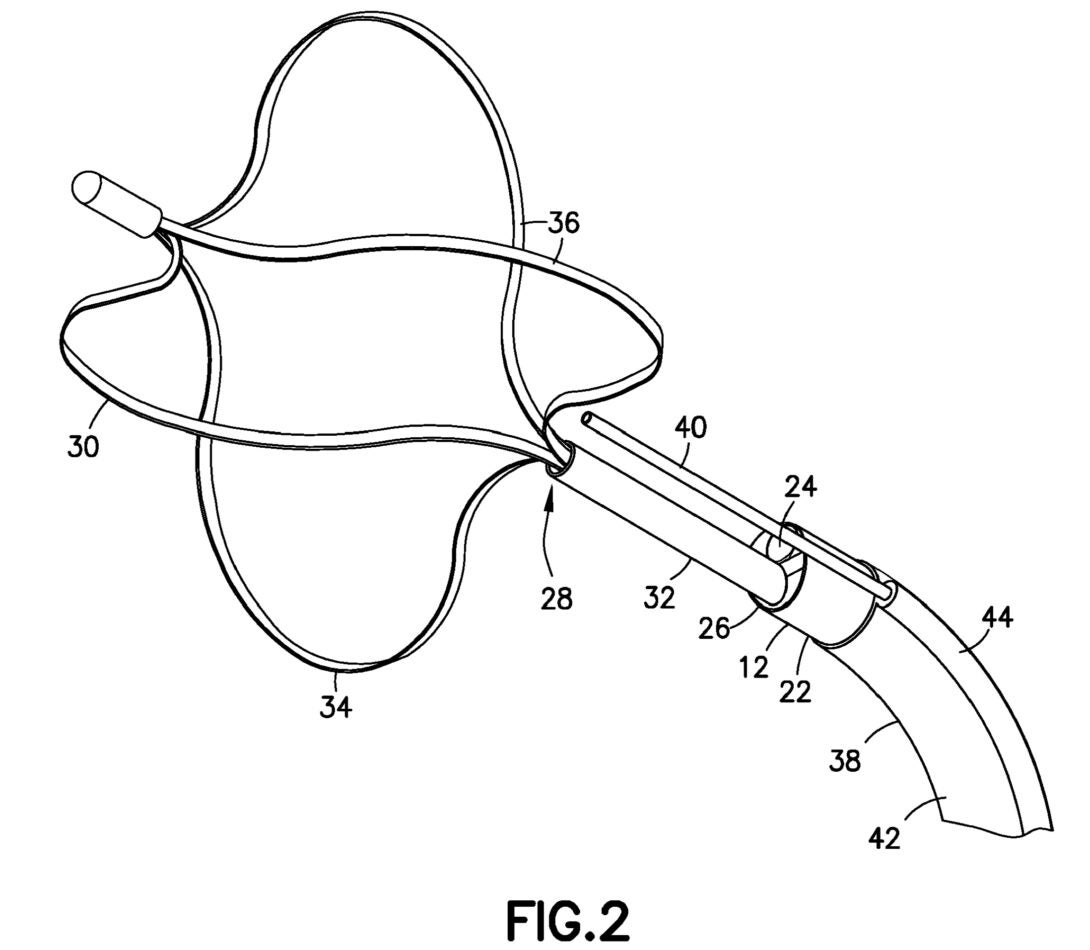
Patent: Laser Lithotripsy Device with Stone Fragment Collection System (US Patent 8,303,501)
To address the challenge of collecting stone fragments during laser lithotripsy, I identified a relevant patent titled “Laser Lithotripsy Device with Stone Fragment Collection System.”
This patent describes a laser lithotripsy device equipped with a system for collecting stone fragments. The device utilizes a specialized collection mechanism integrated with the laser probe to capture fragments as they are generated.
Key Features:
– Collection Mechanism: The patent claims a novel collection system that includes a suction device and a filter to gather and retain stone fragments.
– Design Enhancements: The system is designed to be minimally invasive and operates concurrently with the laser lithotripsy procedure, ensuring efficient fragment collection without interrupting the procedure.
– Material Specifications: The apparatus is made from biocompatible materials to ensure safety during the procedure.
The integration of a stone fragment collection system with the laser lithotripsy device addresses a critical need observed during my primary research. This innovation enhances the overall efficiency of the lithotripsy procedure by minimizing the challenges associated with fragment removal.
EUROPEAN PATENT APPLICATION. (n.d.). https://patents.google.com/patent/EP3632359A1/en
Conclusion
The secondary research on the Ho:YAG laser lithotripter and the commercial solution for stone fragment collection provides valuable insights into improving laser lithotripsy procedures. The peer-reviewed study confirmed the effectiveness of the Ho:YAG laser in fragmenting stones, while the patent offered a practical solution for collecting the resulting fragments. Together, these findings can inform future improvements in clinical practice, potentially leading to better patient outcomes in urological procedures.
Week 3: Bladder Irritation from Ureteral Stents- A Need for Innovation
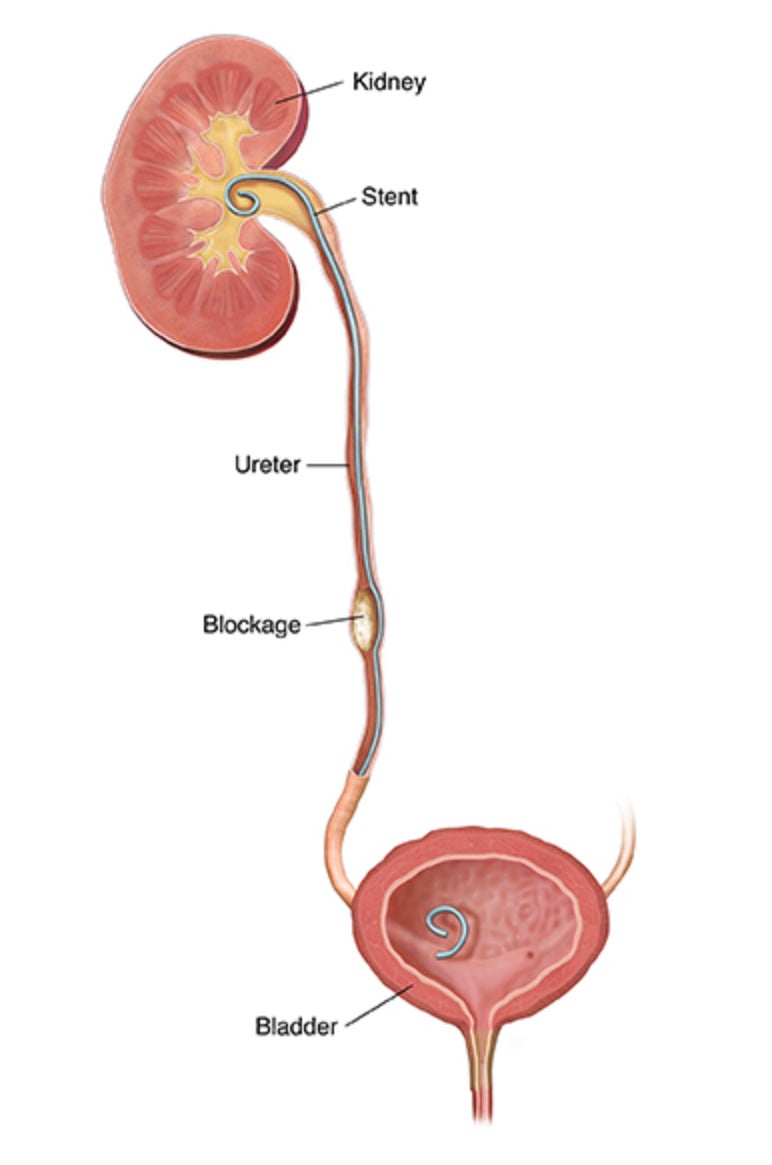
Ureteral stents are commonly used in urology to ensure the dilation of the ureters, allowing urine to flow from the kidneys to the bladder. Despite their effectiveness, many patients experience significant bladder irritation and discomfort due to the presence of these stents. There is a critical need for the development of ureteral stents that incorporate measures to reduce these adverse effects, improving patient comfort and compliance.
During ureteral stenting, a flexible tube is inserted into the ureter to prevent or relieve obstruction. However, the presence of a stent can lead to complications such as bladder irritation, which manifests as urgency, frequency, and suprapubic pain. These symptoms are often due to the irritation caused by the stent’s lower end in the bladder, leading to substantial discomfort and affecting the patient’s quality of life.
Research indicates that modifications in stent design and material can significantly impact the degree of bladder irritation experienced by patients. Innovations such as stents with smoother surfaces, biocompatible coatings, and anti-inflammatory agents are currently being explored to mitigate these symptoms . There are published studies and patents that highlight the benefits of using stents coated with hydrophilic materials, which showed a reduction in irritation and discomfort compared to conventional stents. However, from my observations, coatings on stents don’t work well as the coating tends to wear off over time.
Needs Statement Iteration 1:
Urology patients requiring ureteral stents need stents with improved measures to reduce bladder irritation, thereby minimizing the need for surgical intervention.
Population: Urology patients requiring ureteral stents
Opportunity: Need stents that reduce bladder irritation
Outcome: Enhanced comfort and compliance (with the aim of reducing surgical intervention)
Needs Statement Iteration 2:
Urology patients need ureteral stents with measures that minimize bladder irritation, improving overall patient experience and adherence to treatment.
Population: Urology patients
Opportunity: Need ureteral stents with measures that minimize bladder irritation
Outcome: Improved overall patient experience and adherence to treatment
Conclusion
There is a significant opportunity to improve the quality of life for urology patients through the development of ureteral stents that reduce bladder irritation. By focusing on innovative materials and designs, the medical community can address this prevalent issue, ensuring better patient outcomes and satisfaction.
Rationale for changes:
- The first needs statement points into the direction of creating a stent that ensures patient comfort.
- The aim is less irritation for the bladder which can be emphasized with affects of damage on the bladder and/or possible surgical intervention.
References:
– Deliveliotis, Charalambos et al. “Is there a role for alpha1-blockers in treating double-J stent-related symptoms?.” Urology vol. 67,1 (2006): 35-9. doi:10.1016/j.urology.2005.07.038
– “Having a Ureteral Stent.” Saint Luke’s Health System, www.saintlukeskc.org/health-library/having-ureteral-stent. Accessed 22 July 2024.
– Joshi, H B et al. “Indwelling ureteral stents: evaluation of symptoms, quality of life and utility.” The Journal of urology vol. 169,3 (2003): 1065-9; discussion 1069. doi:10.1097/01.ju.0000048980.33855.90
– Koprowski, Christopher et al. “Ureteral Stent-Associated Pain: A Review.” Journal of endourologyvol. 30,7 (2016): 744-53. doi:10.1089/end.2016.0129
Samuelsson, Patrik et al. “Toll-like receptor 4 expression and cytokine responses in the human urinary tract mucosa.” Infection and immunity vol. 72,6 (2004): 3179-86. doi:10.1128/IAI.72.6.3179-3186.2004
Week 4: Revising Needs Statements & Addressing Bladder Irritation from Ureteral Stents
Revised Need Statement:
NS Iteration: Urology patients requiring ureteral stents need stents with improved measures to reduce bladder irritation, thereby minimizing the need for surgical intervention.
Population: Urology patients requiring ureteral stents
Opportunity: Need stents that reduce bladder irritation
Outcome: Minimize the need for additional surgical interventions
New NS Iteration 2: Urology patients need innovative approaches to maintaining ureter dilation that minimize bladder irritation, improving overall patient adherence to treatment.
Population: Urology patients
Opportunity: Need innovative approaches to maintaining ureter dilation that minimize bladder irritation
Outcome: Improved overall patient adherence to treatment
Changes Based on IDEO’s Three Components:
Need Statement Iteration 1
1. Desirability:
– Old Approach: Focused on comfort, which is subjective and difficult to measure.
– New Approach: Focuses on measurable outcomes such as reducing the need for surgical interventions. This shift makes the need more tangible and actionable, aligning with patient and medical staff desires for fewer procedures.
2. Feasibility:
– Old Approach: General mention of improved measures without specifics.
– New Approach: Specifies the need for stents with upgraded design revolving around existing research and patents.
3. Viability:
– Old Approach: Lacked emphasis on long-term benefits and economic sustainability.
– New Approach: Highlights the potential to reduce surgical interventions, leading to better patient outcomes and reduced healthcare costs over time. This ensures that the solution is beneficial, sustainable, and cost-effective.
New Need Statement:
1. Desirability:
– Old Approach: Similar to the first iteration, focused on comfort.
– New Approach: Focuses on the need for innovative approaches that maintain ureter dilation and minimize bladder irritation, aiming to improve overall patient adherence to treatment. This makes the need more appealing and aligned with patient and healthcare provider goals.
2. Feasibility:
– Old Approach: General mention without exploring alternative methods.
– New Approach: Emphasizes the potential for innovative approaches that do not necessarily involve traditional stents, which is a feasible direction based on advancements in medical technology and research.
3. Viability:
– Old Approach: Lacked focus on long-term benefits.
– New Approach: Highlights the potential to improve overall patient adherence to treatment, which can lead to better health outcomes and reduced costs associated with non-compliance and additional interventions. This ensures the solution is sustainable and economically viable.
Conclusion
By revising the needs statements to focus on measurable outcomes and incorporating lessons from IDEO’s framework, we can address the critical issues related to ureteral stents more effectively. Emphasizing reducing surgical interventions, and exploring innovative approaches aligns with patient needs and ensures long-term viability and feasibility of the proposed solutions.
References
Koprowski, Christopher et al. “Ureteral Stent-Associated Pain: A Review.” Journal of endourologyvol. 30,7 (2016): 744-53. doi:10.1089/end.2016.0129
Miyaoka, Ricardo, and Manoj Monga. “Ureteral stent discomfort: Etiology and management.” Indian journal of urology : IJU : journal of the Urological Society of India vol. 25,4 (2009): 455-60. doi:10.4103/0970-1591.57910
doi: 10.25122/jml-2021-0352
doi: 10.1186/s12894-020-0577-y
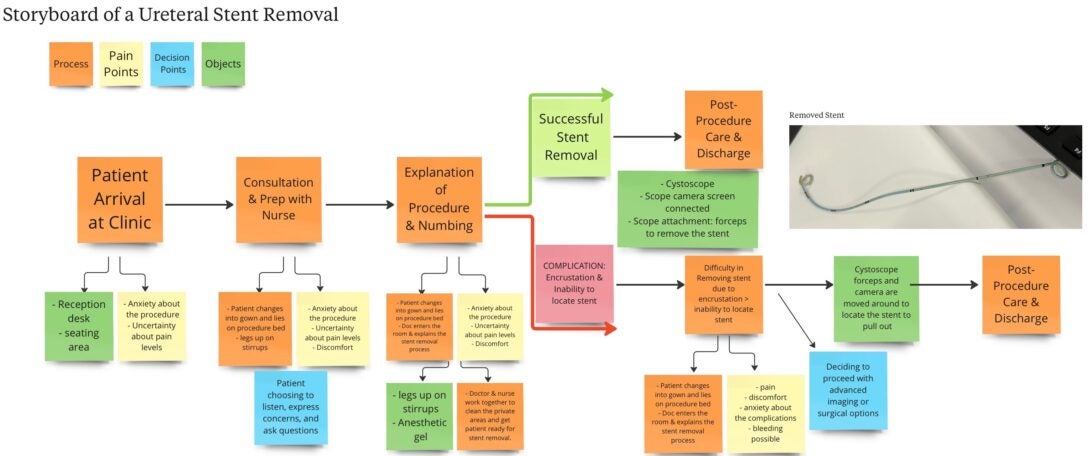
Storyboard Analysis of Ureteral Stent Removal: Identifying Key Pain Points and Areas for Improvement
Week 6: Final Reflections and Insights from the UIC Clinical Immersion Program

As we conclude Week 6 of the UIC Clinical Immersion Program, it is an opportune moment to reflect on the transformative experiences we’ve shared. Throughout the program, I had the privilege of observing within the UI Health Urology Department. With the support of our advisors and doctors, my teammates and I established meaningful connections with the dedicated doctors, nurses, and staff who welcomed us warmly. We were provided with a nurturing environment that accommodated our questions and enthusiasm for learning.
I extend my deepest gratitude to Dr. Michael Young and Dr. Daniel Garvey for their inspiring expertise and mentorship. Their guidance has been instrumental in shaping our understanding and approach. They facilitated connections with other urologists, maximizing our exposure to the specialty and helping us identify areas ripe for innovation. Special thanks to Dr. Omer Acar and the urology residents for their patience and extensive knowledge, which significantly enriched our experience. We had the opportunity to observe a wide range of surgeries in the OR and many clinical procedures, providing us with a deeper understanding of devices and various procedures. Additionally, we are grateful to Dr. Browne and Dr. Felder for their invaluable weekly guidance and support. Everyone’s collective contributions have profoundly impacted both our professional development and personal growth.
Recommendations for Future CIP Participants
1. Take Notes: Your observations in the clinic and OR are crucial for revisiting and deciding on current problems or inconveniences in your specialty. This will help you and your team compile a need to explore. Look for: what goes well/what needs improvement, what takes time/what makes things quicker, what issues staff face, and the impact of actions on patients, doctors, nurses, and other hospital staff, etc.
2. Communication: This is one of the greatest factors of success for you and your team’s experience. Almost every day, my team and I would discuss our observations together. You will learn things from their observations that you may have missed. This is crucial for building connections with your teammates and ensuring the best experience. Additionally, discuss your observations with doctors and nurses (interviews!) to gain their perspectives and feedback, which will help you identify a need within your specialty.
3. Make Connections: While in the clinic, get to know the doctors, nurses, and staff. Ask where you can observe more procedures/surgeries. You will find that everyone is very kind and accommodating! We were able to observe specific fields in urology, such as oncology, robotic surgery, and reconstruction surgery, providing us with amazing exposure and many helpful observations.
4. Stay Organized: A shared folder with your teammates becomes essential for storing pictures and notes. Our group used different colored sticky notes for various categories of observations, making it easy to locate specific information.
5. Have an Open Mind: Your group will consist of medical and biomedical engineering students. Be insightful and eager to discuss observations together and ask questions. Everyone’s experience and knowledge is beneficial!
6. Have Fun and Put in Your Best Effort: Six weeks will pass quickly. To learn the most and make the most of the program, maximize your time, connections, and resources.