
Laura Navarro
2023 students
IMED, M2
Department of Neurosurgery
Pronouns: She/Her/Hers
Email:
Week 1: Design Observations in the OR and Clinic

As a novice to the operating room, spending the first week observing neurosurgery cases was a steep learning curve. Although the week was full of adjustment, being unfamiliar with environments offers the advantage of a fresh perspective. This past week, I observed two transforaminal lumbar interbody fusion (TLIF) cases, an anterior lumbar interbody fusion (ALIF) case, and shadowed in clinic alongside my team. These surgeries involve the fusion of vertebrae by the insertion of screws between pedicles and an interbody cage with bone autograft between the vertebrae. The TLIF is a posterior approach, while the ALIF is an anterior approach. Among the innumerable pearls I drew from this week of clinical immersion, particular designs stood out to me as either assets or drawbacks in the delivery of quality patient care.
Good design: Bone milling and bone autografts
A feared outcome of any allograft is rejection, and a common limitation is supply. In TILF procedures, bone autografts are inserted into the interbody cage. This complex of bone graft, cage, and screws between vertebrae facilitate fusion to alleviate nerve compression and pain. During the process of bone grafting, a machine was used to recycle the bone removed from the patient’s vertebrae in the procedure. This machine separates bone from tissue and grinds the bone into fine pieces. This design eliminates the risk of rejection being that it is the patient’s own tissue, and it also resolves the supply limitation. The graft was prepared during the procedure by the pictured bone mill. The plastic attachment at the top is disposable to maintain sterility, and the device makes little noise and operates smoothly. The bone size can be customized, is protected from heat, and the set-up of the device is quick and involved connecting two parts together. Overall, this device is an excellent alternative to manual bone milling and allows for more effective separation of bone from tissue to ensure enough autograft is available for the procedure.
Bad design: Epidural
On Friday we had the opportunity to shadow in the clinic. I noticed some flaws and difficulties while observing the OR, but the clinic visits exposed problems in delivery of care that could not possibly be gathered without patient feedback. Majority of the patients dealt with chronic pain, had tried various interventions for relief, and were referred to neurosurgery as an advanced step. One patient presented to clinic with severe back pain, left arm pain, and left arm numbness associated with disc degeneration. The patient underwent 3 epidurals, none of which provided any relief. She expressed hesitancy about surgical interventions, and a fourth epidural was recommended to the patient. This sparked the question: how can a patient have three failed epidurals with the possibility of success on the fourth? I learned that epidurals are safe procedures with low incidences of hematomas and nerve damage, and therefore it is safe to order multiple lifetime epidurals for a patient. However, there are many technicalities when delivering medication to the effected nerve roots, resulting in sub-optimal success rates. The cause of this patient’s history of failed epidurals was that the target area was not reached by the medication, and therefore a fourth epidural may be effective. Extensive training in the procedure and recognition of fluoroscopic imaging patterns is required to perform an epidural, which leaves room for error. While the concept of a transforaminal steroid injection is a good design, the procedure and delivery has room for improvement to increase success rates and patient outcomes.
Week 2: Chronic back pain storyboard
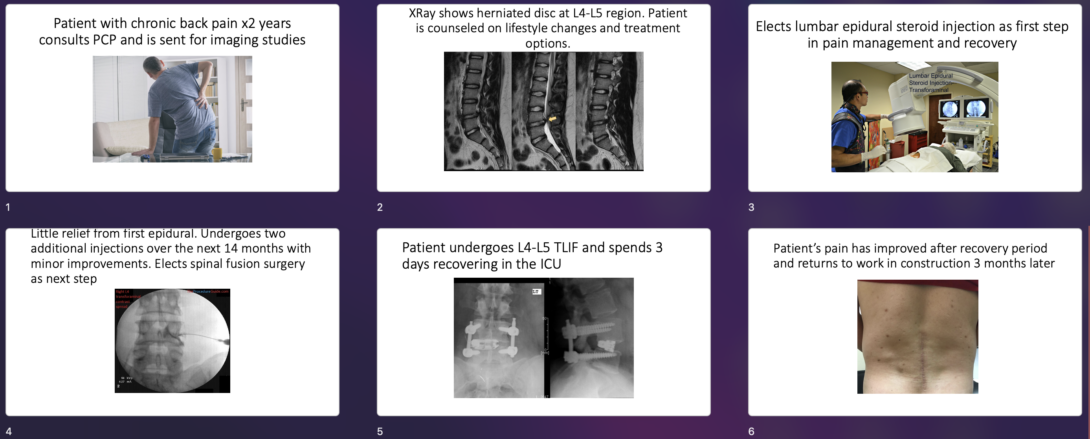
Visualizing a process through a storyboard simplifies events to highlight the “pain points” and exposes opportunities for improvement in flow. In this storyboard, I depict a patient’s experience seeking care for chronic back pain. The patient is a 50-year-old male who has had back pain for 2 years that has been worsening lately. He has been unable to work in his construction job and the daily pain is a constant stressor for him.
We can assess the storyboard for shortcomings in the healthcare system that add difficulties, also known as the pain points.
- The patient’s herniated disc remained undiagnosed for 2 years. If a herniated disc is detected early on, steroid injections can facilitate healing of the disc and long-term symptom relief. In this case, surgical interventions are not needed if lifestyle modifications are implemented as well. The pain point here is delayed diagnosis.
- The patient is presented with his diagnosis and treatment options. Shared decision making is practiced with emphasis on epidurals as a first step. This experience is new to the patient and they although this is shared decision making, the patient likely relies mostly on insight and education provided by the surgeon. The pain point here is access to education.
- Various pain points can be identified in an epidural procedure. From the perspective of the patient, a pain point is the physical discomfort of local anesthetic around the spine prior to the steroid injections.
- The patient underwent several epidurals that were not effective. There was no indication of the chance of effectiveness prior to electing these procedures, and the patient then moved to surgical interventions. The pain point here is variability in effectiveness.
- The TLIF procedure requires anesthesia, about 4 hours in the OR, and 3 days in the ICU. The pain point here is recovery time.
- Although the patient recovered with the desired outcome, the patient has been out of work for 3 months which could pose a financial and professional burden. The pain point here is lifestyle changes.
Assessment of these pain points help us identify where interventions for chronic back pain can be improved to prevent surgical intervention or to make the outcomes more manageable for patients.
Image sources:
1. Minnesota Valley Surgery Center. (2023, June 14). Treatment for chronic back pain: Pain management vs surgical options. Minnesota Valley Surgery Center. https://minnesotavalleysurgerycenter.com/orthopedic-surgery/treatment-for-chronic-back-pain-pain-management-vs-surgical-options-2/
2. Moussa MK, Alkefrawi P, Elkhalil JK. Large central disc herniation causing cauda equina syndrome in an adolescent. A case report. Int J Surg Case Rep. 2021;79:119-122. doi:10.1016/j.ijscr.2020.12.066
3. Lumbar epidural steroid injections – transforaminal. Virginia Interventional Pain & Spine Centers. (n.d.). https://www.vapainsc.com/treatments-and-procedures/lumbar-epidural-steroid-injections%E2%80%93-transforaminal.html
4. Fluoroscopic guided thoracic/lumbar transforaminal epidural steroid injection – technique and Overview. The Procedure Guide. (2021, December 22). https://theprocedureguide.com/fluoroscopic-guided-thoracic-lumbar-transforaminal-epidural-steroid-injection/
5. Transforaminal lumbar interbody fusion (TLIF) in New Jersey. Comprehensive Spine Care. (2023, February 13). https://compspinecare.com/treatments/transforaminal-lumbar-interbody-fusion/
6. Anterior versus posterior lumbar fusion. Rocky Mountain Brain and Spine Institute. (2019, March 13). https://rockymountainbrainandspineinstitute.com/anterior-versus-posterior-lumbar-fusion/
Week 3: Assessing Needs
After three weeks of observing in the OR, clinic, and ICU, additional shortcomings in healthcare delivery have surfaced. A particular procedure that caught my attention as an opportunity for innovation was the endoscopic TLIF, which is a minimally invasive approach to the open TLIF. This approach allows for shorter recovery time (24 hours versus 3 days). Currently, few surgeons in the US are trained in the operation because it is significantly more difficult than an open surgery for the following reasons: the visibility is significantly limited, bleeding obstructs the camera, the origin of bleeding is harder to identify, and tissue removal for decompression of the nerves is meticulous. After interviewing our neurosurgery mentor, it was communicated that the largest barrier to endoscopic TLIFs is identifying and controlling bleeding, and tissue removal.
This inspired the following need statement:
Neurosurgeons performing endoscopic (minimally invasive) spinal surgery require a method to quickly identify bleeding points to maintain visualization and decrease procedure time.
Several iterations of the needs statement with alterations in the population, opportunity, or outcome are listed to encompass any additional elements of this problem.
Iteration 1:
Neurosurgeons performing endoscopic (minimally invasive) spinal surgery require a method to quickly identify bleeding points to decrease patient risk.
Population: Neurosurgeons
Opportunity: Endoscopic (minimally invasive) spinal surgery
Outcome: Decrease patient risk.
Iteration 2:
Neurosurgeons performing endoscopic (minimally invasive) spinal surgery require robust training techniques to maintain visualization and decrease procedure time.
Population: Neurosurgeons
Opportunity: Robust training techniques
Outcome: Maintain visualization and decrease procedure time.
Iteration 3:
Neurosurgeons performing endoscopic (minimally invasive) spinal surgery require a method to quickly identify bleeding points to maintain visualization and decrease procedure time.
Population: Neurosurgeons
Opportunity: Endoscopic imaging technology that allows visualization despite bleeding
Outcome: Maintain visualization and decrease procedure time.
Week 4: Patent Search
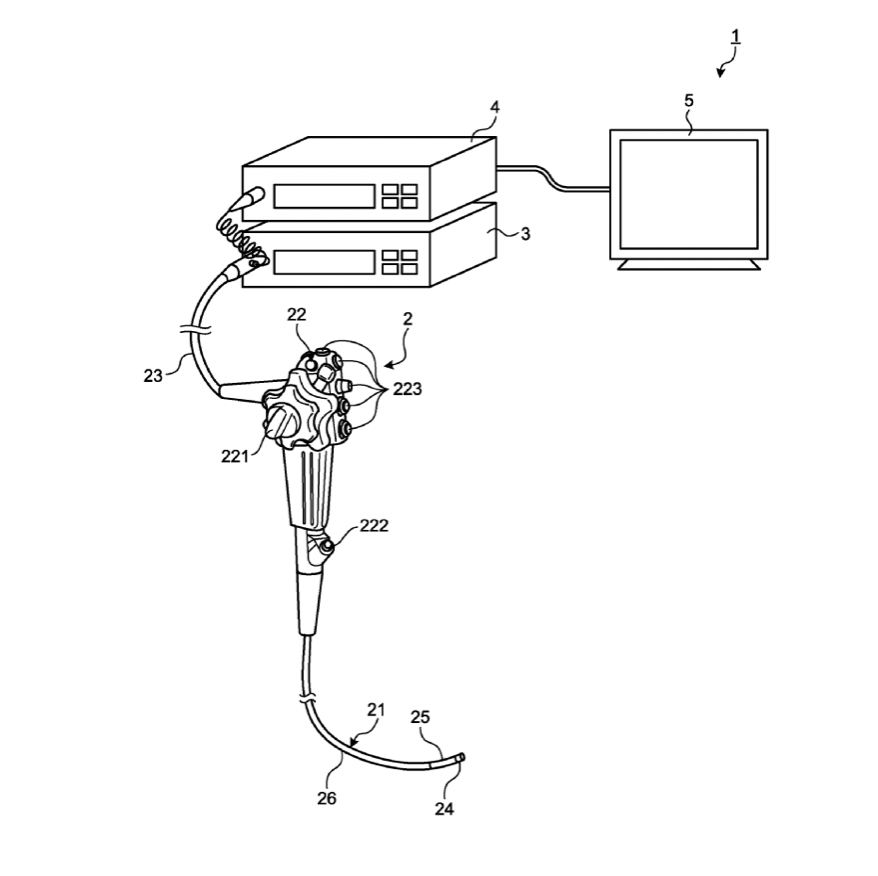
As explored during our third week in neurosurgery, identifying the source of a bleed during an endoscopic spinal procedure (TLIF, laminectomy, decompression) is imperative for decreasing overall procedure time and increasing visibility through the endoscope. A primary patent search was conducted through WIPO to explore options for bleeding identification, although designs are quite limited. Below is a patent detailing an endoscope system which emission and detection of two narrowband lights to detect hemoglobin concentration, thereby indicating the bleeding source. The region with greater optical density indicates the bleeding point.
While this solution meets the need in some regard, it relies on opacity and neglects flow and projectile motion of blood. This leaves room for error to mistake tissue or other matter in the operation site as hemoglobin, especially in the complicated setting of a disc space. Additionally, in the endoscopic spinal procedures, copious irrigation is necessary, and the surgical site is entirely fluid-filled. This causes blood to disperse in different patterns, leaving room for variability in the optical density.
Publication number: 20230000330
Type: Application
Filed: Sep 2, 2022
Publication Date: Jan 5, 2023
Applicant: OLYMPUS CORPORATION (Tokyo)
Inventor: Takaaki IGARASHI (Tokyo)
Application Number: 17/902,031
Week 5: Assessing the market
Epidurals are a commonly performed procedure in various clinical contexts. Not only is the market large, but it is gradually increasing as a pain management strategy during labor and for chronic back pain. Epidurals are a great solution for chronic back pain as they do have curative potential for herniated discs if treatment is received soon enough, and they remain a cheaper and safer alternative to surgical intervention. Additionally, they continue to relieve the intense pain of childbirth for many.
Currently, between 10-11 million epidurals are administered per year in the US. About 9 million of these are steroid injections and about 1-2 million are analgesic injections for labor and delivery. Epidural injections without imaging cost $706.00 out-of-pocket and an additional $39 for fluoroscopy imaging according to the charges posted by Cook County Health in 2023.
The main differences between epidurals for labor versus herniated discs is that epidurals for labor do not contain corticosteroids, and epidurals during labor use imaging less frequently. Because of these minor differences, nearly identical technologies are used for both procedures and so both procedures contribute to the total addressable market (TAM) for epidurals. The TAM comes out to 7.6 billion dollars at minimum under the assumption that a potential solution has the versatility to be used during labor and in the pain management clinic. Imaging was excluded for this market estimate because it is used more commonly for steroid injections than analgesic injections.
If we calculate the TAM of steroid epidurals only, we can include fluoroscopic imaging in the calculation and assume that there are at least 9 million steroid injections being administered per year, coming out to a TAM of 6.7 billion dollars. Overall, the market for epidurals is very lucrative, and these numbers are expected to be sustained or increased in the coming years because it is an efficient and practical approach for pain relief.