
Nolan Ryan
Student Participant
Week of 7/10
Three iterations of a needs statement.
TEE probes are very expensive (~20K) and delicate. Damage occurs between uses that is costly and delays care since a replacement is not always available.
Iteration #1
Process standards for cleaning TEE probes without damage.
Population: Processing Techs
Opportunity: Rough handling
Outcome: Not damaging TEE Probe.
After following probes around the OR it was apparent that they are moved in a bag without protection and that the actual cleaning is quite standard and gentile. Transporting of the probes after use is also a potential for damage.
Iteration #2
Solution for handling and moving probes between uses to prevent damage.
Population: Processing and Anesthesia Techs
Opportunity: Handling and transporting probes.
Outcome: Prevent damage to TEE Probe.
After interviewing the techs, it sounds like the probe is bagged by the anesthesiologist immediately after being pulled from the patient. They then place the bag on the floor or the machine. From there anesthesia techs walk it to the dirty room and wipe it down with pre-cleaner. HOWEVER. Sometimes during room turnover when the staff is busy, the bag may be moved to the hallway and thats where they find it after use.
Iteration #3
A solution to prevent TEE damage from mishandling or accidental damage between uses.
Population: OR Staff
Opportunity: Handling, Transporting, Storage, and Processing probes
Outcome: Prevent expensive repairs and downtime to/of TEE Probe.
This iteration broadens the scope to include all staff that handle the probe. Both the staff that are supposed to be handling it as well as the infrequent staff that may be handling it not knowing what it is. Any solution should take into account the potential for anyone to handle the probe between placement and removal from the patient.
Week if 7/17
Previous needs statement relating to downtime and expense of TEE probes breaking between use.
An OR wide solution to prevent TEE probe damage between uses.
Patent found:
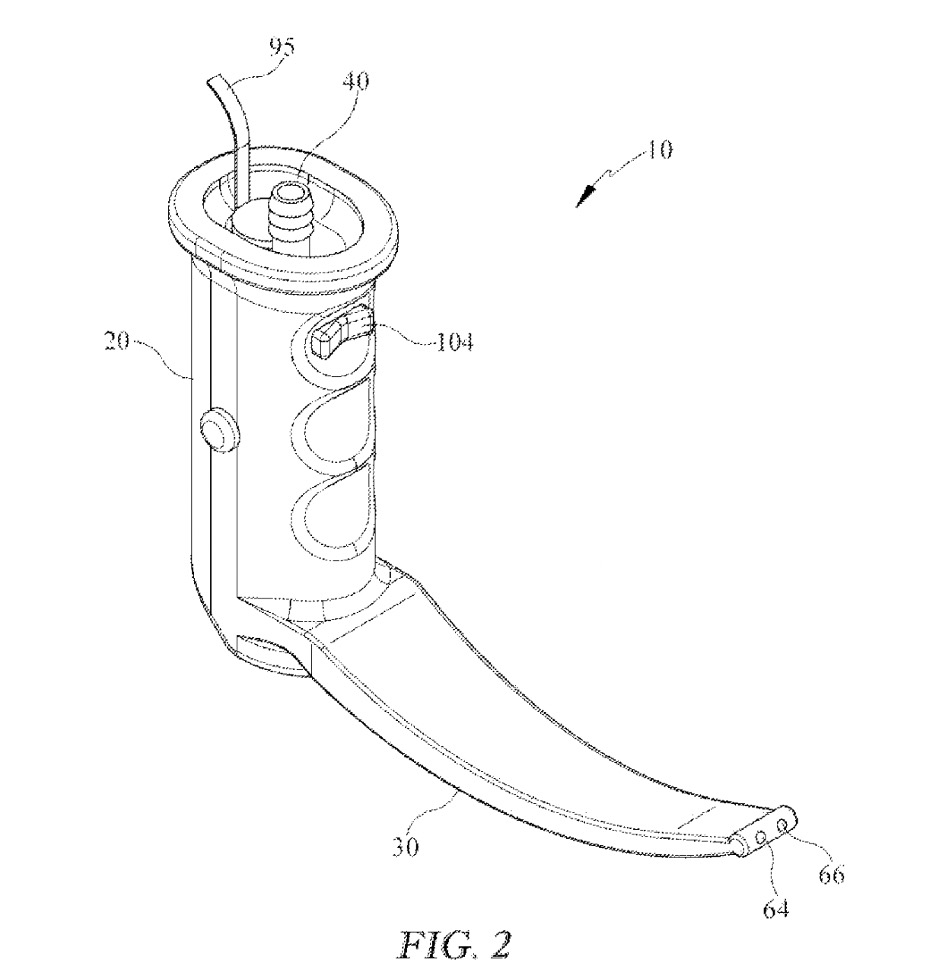
Multifunctional enclosure system for medical probes and method of use
WO2015047455A2
Week of 7/24
NS: “Medical professionals who intubate patients in an emergent setting experience difficulty visualizing the airway due to contamination and need to increase first-time intubation success rate.”
One of the very interesting approaches to dealing with airway contamination integrates suction into the laryngoscope blade. Many of the clinicians we interviewed have let us know that one way to deal with camera contamination is to suction before inserting the blade. Leading the camera down behind the suction making a clear path. This device does just that without the need for a second had operating the suction. Some notable drawbacks are the lack of detectability of the suction, you must either aim your blade to intubate or to suction. We observed many intubations of patients who had been NPO and there rarely enough secretions to obscure the camera. We did see however that the cords from a VL device sometimes got tangled or other wise needed to be delt with by the operator and this would add another connection to the device that could become entangled. We also had a lot of feedback from emergent intubators (flight teams, EM residents) that traditional suction devices are too small bore for thick vomit in patients who haven’t been NPO. As you can see in the image the suction openings at the tip are quite small also, most capable of salivary secretions. One of the providers we discussed this design with was also concerned for the possibility of “sucking” contamination toward the camera lens. This device was brought to marked as InScope, but based on their website no longer being in existence and the lack of a supplier we don’t think it was a market success.
Ref:
US10709322B2
Week of 8/31
NS: A solution to prevent TEE damage from mishandling or accidental damage between uses.
Based on a 10 year analysis of Echo in the US there has been consistent growth in the number of exams by more than 3% annually. There were 816,000 patients who received exams in 2010. According to their background data collected from Medicare service records they estimate trans thoracic echo (TEE) outnumbers trans esophageal echo 100:1.1
Assuming a continued growth of 3% annually over the last 11 years we can assume just over 1.1 million echo’s last year. This means around 11,000 TEE. If a single use solution valued at $30 was utilized that would mean around $300,000 in sales.
This number is quite small in comparison than the more than 15 million colonoscopies performed annually2. Any single use endoscope protector would be at minimum applicable to TEE probes as well as colonoscopes and bronchoscope. If you assume more than 15 million uses at $30 each it’s possibly a half billion dollars of total addressable market.
1Papolos, A., Narula, J., Bavishi, C., Chaudhry, F. A., & Sengupta, P. P. (2016). US hospital use of echocardiography: insights from the nationwide inpatient sample. Journal of the American College of Cardiology, 67(5), 502-511.
2https://www.pennmedicine.org/cancer/about/focus-on-cancer/2019/december/lets-get-screened-colonoscopy#:~:text=More%20than%2015%20million%20colonoscopies,remove%20them%20during%20the%20procedure.