
Shreenithi Palamuthy
2024 students
Biomedical Engineering, Ophthalmology
Pronouns: She/Her
Email:
Week 1: Good and Bad Designs
My first week shadowing in ophthalmology was a very interesting experience. One of the challenges that I experienced during the first week was assessing how pressing of a concern certain needs were. My main goal while observing was to pay extra attention to any problems faced during procedures and to assess whether those issues could be addressed by modifying the medical tools or devices in any way. While shadowing in the clinic and operating room, I saw several good and bad designs that I have described below.
Good Design: Ophthalmic Eye Occluder
Activities: The patient holds the eye occluder up to their face and looks into the open eye slot while their other eye is covered by the occluder. The occluder flipper with pinholes allow the patient to be able to see clearer through the device when looking at the screen.
Environment: Used in the general eye clinic
Interactions: The patient interacts with the occluder by holding it up against their eyes.
Objects: The eye occluder is an ophthalmic tool with a closed side and a larger hole on the other side. The side of the occluder with the larger hole contained an occluder flipper filled with a group of smaller pinholes.
Users: The patient uses the occluder for eye examinations.
Based on my observations in the clinic, I could see that the eye occluder was not only easy to use, but also served its purpose of facilitating eye examinations. The design was simple and appeared to be cost effective without too many parts.
Bad Design: Patient Headrest
Activities: Prior to the procedure, the patient was asked to place their head on the headrest.
The patient was then told to adjust their head position by moving up or down until it was centered at the appropriate position for surgery. The patient was also instructed to not move during the procedure. As I was observing, I noticed that the headrest did not have any mechanism to prevent patient head movement.
Environment: Used in the operating room; attached to a wrist rest for the surgeon
Interactions: The physician placed the headrest under the patient. The patient was then instructed to place their head on the headrest.
Objects: The headrest was slightly contoured to hold the patient’s head during the procedure.
Users: The patient is the main user of the headrest because their head is positioned on it. The physician also uses the headrest to support the patient.
As I was observing in the OR, I noticed that the surgeon had to repeatedly tell the patient to stop moving in the middle of the cataract surgery despite already having instructed the patient to remain in one position prior to the start of the procedure. This appeared to be a potential issue because head movement can be risky during surgery. The headrest’s lack of a mechanism to hold down the patient’s head in place during the procedure seemed to be a bad design for two main reasons. The design was too reliant on the physician’s skill and their ability to immediately stop operating if the patient makes any sudden movements during the procedure. Additionally, the current setup places too much trust in the patient’s ability to follow instructions and remain motionless during the procedure. Based on a few interviews I conducted with ophthalmologists at the OR, I found out that physicians occasionally utilize a head tape during procedures to hold down the patient’s head. I hope to be able to observe future procedures that use this tape and assess the ergonomics of the design.
Week 2: Secondary Research
Week 2 in ophthalmology has allowed me to further explore some of the designs that I had been observing last week. This week, one of the major topics that I continued to investigate was patient movement during surgical ophthalmic procedures in the operating room. I had previously observed that the patient headrest did not contain any mechanism to hold the patient’s head in place during procedures. I was also informed about the use of head tape during ophthalmic surgeries and was able to see it be used during two vitrectomies in the OR this week.
At the beginning of the procedure, the surgeon strapped the patient’s forehead to the headrest using stability tape. I noticed that despite the inclusion of stability tape, the surgeon needed to repeatedly tell the patient to not move over the course of the procedure. Following the surgery, I spoke with Dr. Lim who confirmed that small head movements can occur despite the use of stability tape. Even small movements have the potential to affect surgical precision at a larger scale.
Research Articles
I looked into some secondary research in order to further understand the advantages and disadvantages of using stability tape during ophthalmic surgeries. In a study by Brogan et.al., one hundred cataract surgery patients were asked to complete a questionnaire prior to their procedure [1]. The questionnaire assessed patient views on physicians using stability tape to keep the head in place during cataract surgeries. The majority of participants surveyed consented to its use and believed that all patients should be offered stability tape during procedures. The article also highlighted the discomfort that patients may experience during the removal of the stability tape. However, based on my observations in the OR, this did not seem to present a major issue because the tape removal was quick and effortless. It also did not appear to cause any noticeable discomfort to the patient.
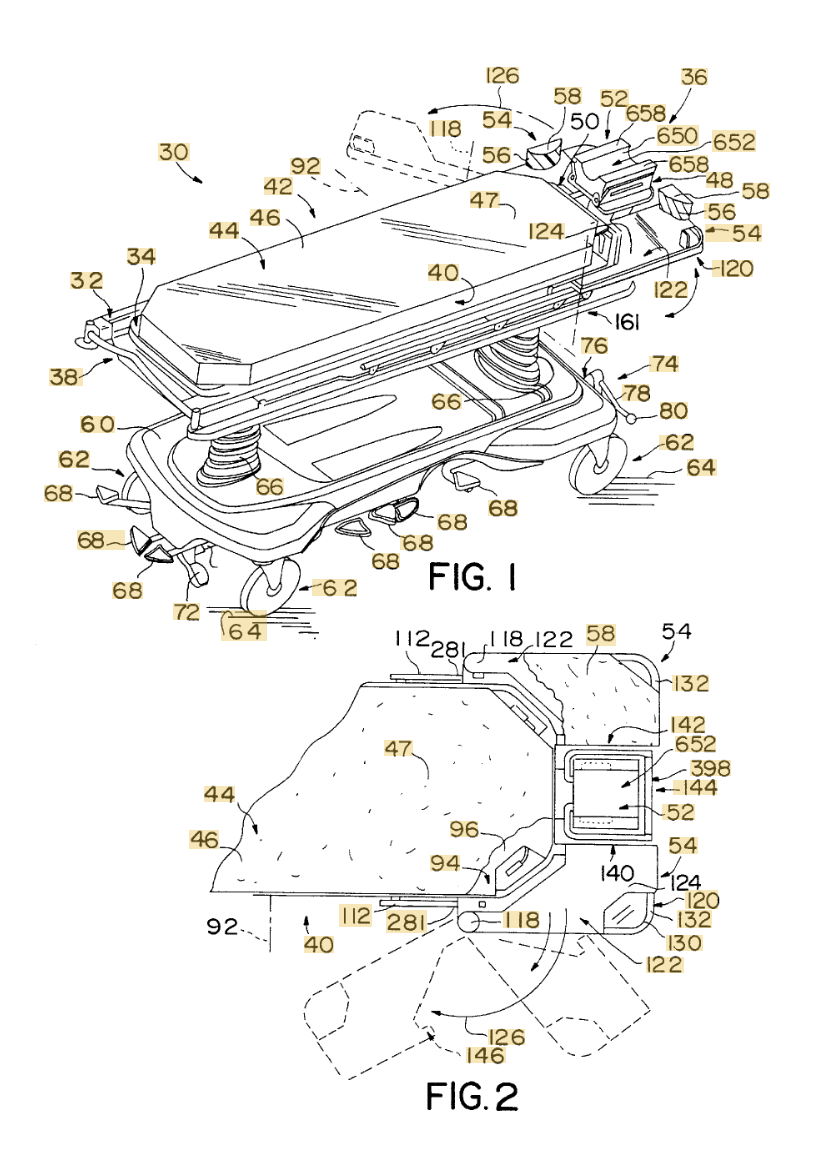
Patents
I was also able to find a patent on a patient headrest similar to what was provided to patients in the OR. Patent US6108840A describes a headrest for patient support and lists the key features of the design. The head rest has sides that are transversely spaced apart and extend longitudinally. This design allows the patient to comfortably place their head within the head rest during surgical procedures. However, as I have discussed in last week’s post, the patient headrest lacks a mechanism to hold down a patient’s head during procedures.
Overall, it appears that despite the advantages of using stability tape, there are a few key considerations that need to be made before its use in surgeries. Patient movement appears to remain an issue during eye surgeries, and I would like to continue to investigate this theme in the coming weeks.
[1] Brogan K, Young D, Ramaesh K, Lockington D. Patients’ attitudes towards the potential use of stability tape to minimize head movements during cataract surgery. Seminars in Ophthalmology. Published online February 27, 2021:1-5. doi:https://doi.org/10.1080/08820538.2021.1890783
Week 3: Needs Statements
Needs Identification
For this week, I focused on identifying a specific need at either the ophthalmology clinic or operating room. One of the problems that I observed was that ophthalmologists often spent extended amounts of time in positions that negatively affected their posture. Over time, poor posture could lead to musculoskeletal injuries.
Needs Statement 1st iteration:
Population: Ophthalmologists
Ophthalmologists are the population that is at risk of musculoskeletal injuries due to ergonomic concerns. This population encompasses all ophthalmologists who perform a wide variety of ophthalmic surgeries including retina and cataract surgeries.
Opportunity: Neck and back strain while using surgical microscopes in the operating room
The surgeons in the operating room appeared to be seated in positions that would place strain on their neck and spine.
Outcome: Reduce musculoskeletal injuries
Over time, repeated strain on the neck and back could lead to musculoskeletal injuries.
Primary Research:
In the operating room, we observed several eye procedures in which the surgeon was seated in positions that would strain their neck and back. The surgeon was typically seated at the edge of their seat while leaning forward, their back was slouched, and their neck was tilted slightly upward to look into the microscope lens. The Zeiss Artevo digital microscope was used for the surgeries that we observed. The surgeons adjusted the height of their Stryker chairs prior to operating, however still exhibited posture issues during the procedures. The ophthalmologist also used a foot pedal to control different devices during the surgeries.
Despite the position adjustability of the surgical microscope, the surgeon’s posture appeared to remain an issue during eye surgeries. Therefore, ergonomics in the operating room during ophthalmic surgeries seemed to be an area of need.
Secondary Research:
Patent: Surgical microscope (US20170065172A1): The surgical microscope patent claims a front optical unit, an illumination device that uses radiation to illuminate the retina, and an adjustable camera optical unit.
Study: This literature review conducted by Betsch et. al., discusses the different factors that can impact ergonomics in ophthalmic surgeries including microscope placement, the surgeon’s chair, foot pedals, and surgical bed height [1]. From a mechanical standpoint, this article outlined forceful gripping, non-neutral positions, repetitive movements, and static loading as likely sources of musculoskeletal complications due to ergonomics [1]. Additionally, patient head movement during eye procedures was described as a factor that could affect the surgeon’s posture since the surgeon will need to adjust their position depending on the position of the patient’s head [1].
Business Research:
Major surgical microscope companies include Leica Microsystems, Carl Zeiss Meditec AG, Alcon, and Olympus Corporation. An example of a surgical microscope used during ophthalmic procedures is the Zeiss Artevo 800 model. This model includes features such as a 3D overhead monitor display and intraoperative OCT.
In the domain of surgical chairs, key companies include Stryker and Hill-Rom. The Stryker 830 Surgistool II is an example model on the market. This includes features such as an adjustable back and armrests, a 3-spindle base for unobstructed foot pedal access, and hydraulic height adjustment. The height on this model can be adjusted from 53cm to 72 cm and can support a maximum weight of 136 kg.
Total addressable market (TAM):
In order to calculate the total addressable market for ergonomics in the operating room for eye surgeries, I multiplied the cost per unit by the total number of uses per year.
Based on inpatient data from 2021, I found that approximately 438,180 vitreoretinal procedures, 106,830 cataract surgeries, 366,005 glaucoma procedures, and 73,865 oculofacial plastic procedures were performed [2]. Therefore, total uses = 438,180 + 106,830 + 366,005 + 73,865 = 984,880.
Additionally, I found the costs of the devices used during the procedures. In particular, I focused on the devices contributing to ergonomic injuries in the operating room. Based on primary and secondary research, I decided to find the costs for the surgical microscope, surgical seat, and foot pedal used in the OR. The Zeiss surgical microscope costs roughly $22,000 [3], the Stryker surgical seat costs $2,426 [4], and the Alcon Centurion Vision system with foot pedals costs $27,777 [5]. Therefore, total cost of devices = $22,000 + $2,426 + $27,777 = $52,203
I approximated the TAM as (984,880 total uses)($52,203) = $51,414 billion.
Needs Statement 2nd iteration:
Population: Ophthalmologists
Ophthalmologists are the population that is at risk of musculoskeletal injuries due to ergonomic concerns. This population encompasses all ophthalmologists who perform a wide variety of ophthalmic surgeries including vitreoretinal, cataract, and oculoplastic surgeries.
Opportunity: Neck and back strain while using surgical microscopes, foot pedals, and surgical seating in the operating room.
The surgeons in the operating room appeared to be seated in positions that would place strain on their neck and spine.
Outcome: Reduce musculoskeletal injuries
Repeated strain on the neck and back could eventually lead to musculoskeletal injuries that prompt the early retirement of ophthalmologists.
After additional research, I have decided to revise my initial outcome. Instead of only considering the impact of the surgical microscope on surgeon posture, I am focusing on the different components that play a role in surgeon posture. In my revised outcome, I will examine how surgical microscopes, seating, and foot pedal position all affect posture. Based on secondary literature that I have reviewed, it appears that the surgeon’s posture is affected by the interplay of multiple factors as opposed to the positioning of a singular device. For example, if the position of the surgical microscope is adjusted, the height of the chair must also be adjusted accordingly in order for the surgeon to maintain a neutral position. Therefore, it appears that all components should be simultaneously adjusted in order to maintain proper posture.
[1] Betsch D, Gjerde H, Lewis D, Tresidder R, R. Rishi Gupta. Ergonomics in the operating room: it doesn’t hurt to think about it, but it may hurt not to! Canadian Journal of Ophthalmology. 2020;55(3):17-21. doi:https://doi.org/10.1016/j.jcjo.2020.04.004
[2] HCUPnet Data Tools – Healthcare Cost and Utilization Project (HCUPnet). https://datatools.ahrq.gov/hcupnet/
[3] Milano S. Zeiss OPMI LUMERA 700 Surgical Microscope | Ophthalmicmart. Ophthalmicmart. Published 2022. Accessed July 10, 2024. https://www.ophthalmicmart.com/product/opmi-lumera-700/
[4] Stryker 830 Surgistool II Stool. MFI Medical. Published 2024. Accessed July 10, 2024. https://mfimedical.com/products/stryker-830-surgistool-ii-stool
[5] Alcon Centurion Phaco Vision System | Saturn Optical. Saturn Optical. Published 2022. Accessed July 10, 2024. https://saturnoptical.com/product/alcon-centurion/
Week 4: New Needs Statement
We observed a right lateral orbital wall decompression surgery in oculoplastics. During this procedure, the operating surgeons used surgical headlights that were attached to their foreheads. The Ronin X6 surgical headlight model was used in the operating room. The headlights were used to guide the surgeons and provide illumination that would help them visualize different anatomical structures while operating.
The surgeons positioned the headlights on their heads prior to beginning the procedure. However, they were unable to make adjustments to the headlight position once they began operating. In particular, we observed a situation where an ophthalmology fellow needed to adjust their surgical headlight midway through the procedure. The fellow needed to ask people nearby to position their headlight for them. The headlight design did not have any mechanism for the user to adjust their own headlight without requiring someone to manually position it using their hands. This appeared to be an issue because this design could stall or delay the procedure. If the surgeon is unable to adjust their own headlight, they will need to rely on the medical assistant or nurses to assist them.
New Needs Statement:
Oculoplastic surgeons require a surgical headlight that can be adjusted without direct contact, reducing the need for external assistance with headlight adjustment during surgical procedures.
Week 5: Storyboard
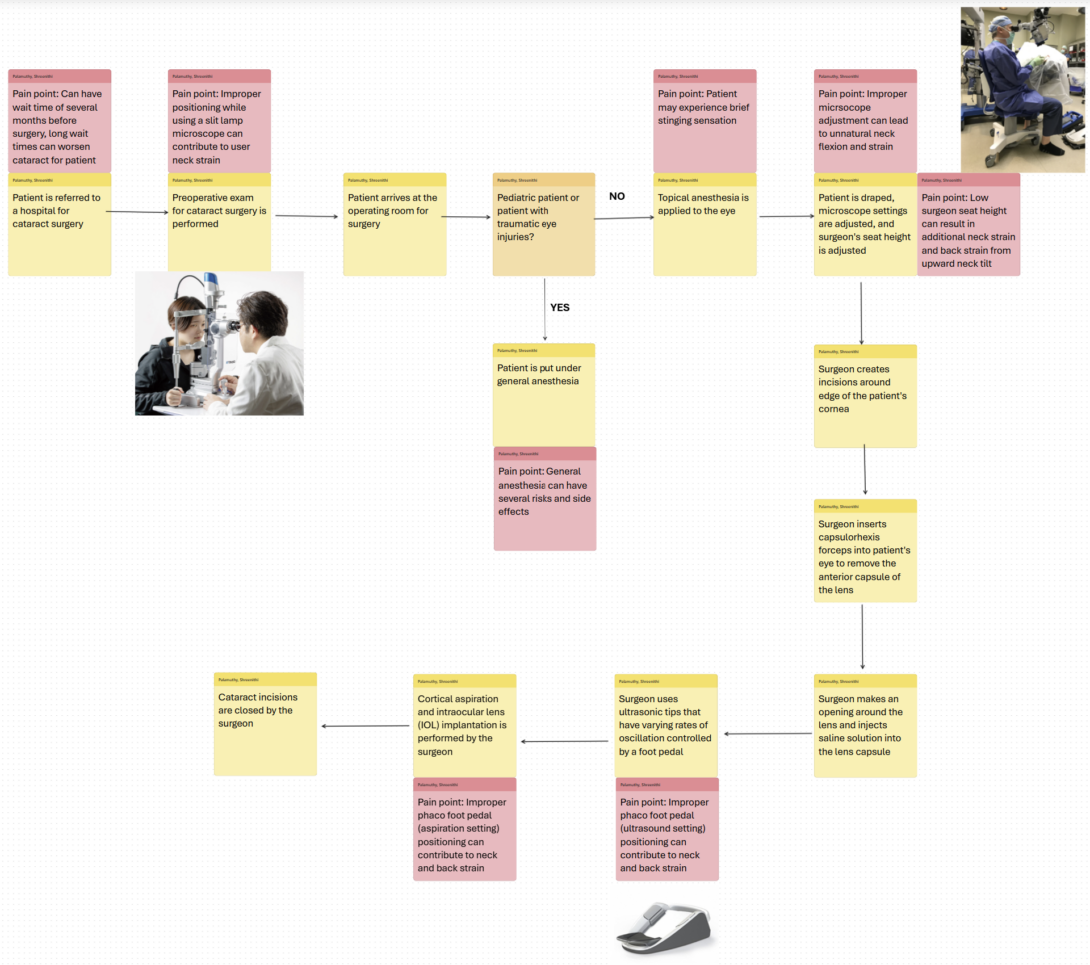
Needs Statement: Ophthalmologists face neck and back strain while using surgical microscopes, foot pedals, and surgical stools in the operating room and need to reduce the risk of musculoskeletal injuries.
I created a storyboard for the need listed above, which I had previously identified. Creating a storyboard allowed me to better visualize how users might be affected at each individual step of a process. In my storyboard, I walk through the procedure for a phacoemulsification cataract surgery beginning with patient hospital referral and ending with the completion of the surgery. I listed out pain points for several steps in the storyboard to highlight problems associated with different steps. In particular, I chose to focus on pain points related to ergonomics in the operating room to support my needs statement.
Overall, I was able to see how the ophthalmologist’s (user) interactions with different pieces of equipment during the ophthalmic surgery could contribute to neck and back strain. Additionally, the storyboard allowed me to see how the patient is also affected at several steps in the process.
Week 6: Final Post
Observing in the ophthalmology department as part of the clinical immersion program for the past several weeks has been an incredibly rewarding experience. I have gotten the opportunity to shadow several subspecialties within ophthalmology including uveitis, oculoplastics, cornea, and retina. This has allowed me to see a variety of different commonly used devices and technology in ophthalmology. A challenge that I faced over the course of this program was identifying needs that were worth pursuing.
For future CIP participants, I would recommend paying close attention to each step and smaller details while observing different encounters and procedures. Even while viewing procedures that I had seen multiple times before, I was able to gain new insights each time because of the different patients being seen and minor changes in the way that physicians operated in each situation.