
Ryan Park
Second Year Medical Student (M2)
Ophthalmology
Email:
Week 1: Good and Bad Des-EYE-gns
During the first week of Clinical Immersion, our group observed several ophthalmologists across several subspecialties at the clinic and OR. The goal was to observe current workflows, procedures, and devices to determine any unmet needs or areas requiring improvement. Given my undergraduate education in biomedical engineering, it was difficult for me to make observations without immediately jumping to possible technical solutions. After all, our goal was not to produce solutions, but to identify needs. Given the wide variety of subspecialties, ophthalmology implements a wide variety of procedures and devices, making it a field with lots of potential for both good and bad designs. Below I describe two of the most notable designs that we observed, one good and one bad.
Good Design: Tono-Pen
In the ophthalmology clinic, the Tono-Pen is a pen-shaped implement that allows for intraocular pressure measurement by lightly touching the tip of the device to the surface of the patient’s eye multiple times. The device estimates intraocular pressure by sensing the pressure of the eye pushing back on the tip of the device.
Activities: Clinicians measured the patients’ intraocular pressure (IOP) with the Tono-Pen. The Clinicians first applied a single drop of Properocain numbing agent to each of the patient’s eyes. The clinicians prepared the Tono-Pen by inserting a disposable tip and pressing a button to activate the device. They then asked the patient to stare straight ahead and keep their eye open. The clinicians then lightly tapped the tip of the Tono-Pen onto the patient’s cornea 6-10 times until a loud beep was emitted from the device, indicating a complete measurement. This was repeated on the patient’s other eye.
Environment: The Tono-Pen was used in the general eye clinic, as well as the other subspecialty clinics, in the outpatient care rooms. Given that it is easily transportable and storable, the Tono-Pen is ideal for carrying around outpatient clinics.
Interactions: Clinicians (residents, attending physicians) and technicians interacted with the Tono-Pen by holding it in a pen grip, between the index finger and thumb. They applied the Tono-Pen to the patient’s eye by first resting the base of the hand holding the Tono-Pen against the patient’s cheek for stability, then lightly pressing the Tono-Pen tip towards the patient’s cornea. Clinicians interacted with patients before Tono-Pen use by applying Properocain to the patient’s eyes to minimize discomfort with the Tono-Pen contacting the eyes. Clinicians would give patients simple instructions to stay still and keep their eyes open during Tono-Pen use, which the patients could easily comply with thanks to the Properocain. During Tono-Pen measurement, the Tono-Pen would give live audio feedback about when IOP measurements were complete.
Objects: The equipment used for Tono-Pen IOP measurement include the Tono-Pen itself, disposable Tono-Pen tips, and a bottle of Properocain numbing agent.
Users: The users of the Tono-Pen include residents, attending physicians, and technicians in the clinic. All of them use the Tono-Pen for the purpose of initial screening for diseases associated with high eye pressure, such as glaucoma.
This is an example of good design because the Tono-Pen is meant for initial screening for glaucoma and other diseases related to high eye pressure. Compared to other eye pressure measurement methods, which require the patient to sit still at a chinrest, the Tono-Pen allows clinicians to more easily check eye pressure without having to secure the patient. Very little preparation is required (just apply numbing drops), and measurements are obtained relatively quickly (6-10 taps to obtain an average pressure reading). Patients did not seem uncomfortable with the Tono-Pen thanks to the numbing drops. Although clinicians have said that the Tono-Pen is less accurate than other methods, its ease of use, low cost, high transportability, and fast measurements make it ideal for its intended purpose of initial screening.
Bad Design: Alcon Constellation Vision System
The Alcon Constellation Vision System allows for control of intraocular pressure (IOP) during vitrectomy (removal of the vitreous humor of the eye) via controlled infusion. More specifically, in a vitrectomy, the surgeon uses a tool called a vitrector, which is essentially a vacuum that cuts and extracts the vitreous humor, which is the jelly-like substance in the large chamber of the eye. Vitrectomies are useful for retinal surgeries since removal of the vitreous humor gives better access to the retina. As the vitreous humor is removed, the empty space left behind needs to be replaced with a controlled amount of gas or saline to maintain IOP; otherwise, the eye would lose pressure and could incur injuries like retinal hemorrhaging. Systems like the Alcon Constellation Vision System combine vitrector functionality with controlled intraocular infusion, meaning that the device can maintain the IOP during vitrectomy.
Activities: The surgeon used the Alcon system to perform a Pars Plana vitrectomy. They first inserted three ports into the Pars Plana region of the eye (a relatively bloodless area) to allow for direct access to the vitreous humor and retina. One port was for inserting a light, one was for inserting the vitrector probe and any other tools (forceps, lasers, etc.), and the third was for inserting a saline infusion tube connected to the Alcon system to control IOP. The surgeon controlled the vitrector probe via a foot pedal, with the suction strength controlled by how far the pedal was depressed. A scrub nurse continuously monitored the IOP by looking at the touch screen on the Alcon system and would change the IOP at the surgeon’s request by pressing touch screen buttons.
Environment: The device is meant to be used in the OR for the purpose of vitrectomy and retinal surgery. The OR environment includes sterile instruments, tables, stools, and large machines including surgical microscopes, anesthesia stations, and the Alcon system.
Interactions: The chief surgeon had to constantly ask scrub nurse what the IOP reading was on the Alcon and also had to ask scrub nurse to change the IOP setting. Note that during our observation, one nurse had a miscommunication with the surgeon and did not apply enough IOP, leading to slight retinal hemorrhage.
Objects: The Alcon Constellation Vision System is a large machine with a touch screen and several attachments, including a vitrector attachment, an infusion pump, and a laser (for retinal detachment surgery).
Users: The scrub nurse directly controlled the Alcon system, while the chief surgeon relied on the system to provide infusion to maintain pressure in the eye during vitrectomy.
This is an example of bad design because the system is a separate device that the surgeons can neither directly control nor directly monitor, which leaves room for errors in IOP due to miscommunication between the surgeon and the scrub nurse controlling the device. When we observed a vitrectomy, a nurse in training did not adjust the IOP when the chief surgeon asked, leading to slight retinal hemorrhaging because the IOP became too low. The surgeon herself expressed her frustration with the nurse when we interviewed her after the procedure. It is clearly critical for the surgeon to be able to closely control IOP during the procedure due to the surgeon’s expertise on appropriate IOP maintenance.
Week 2: Ins-EYE-ghtful Secondary Research
This week, I continued to make observations and perform interviews in the clinic and OR to continue investigating their devices and procedure. To augment that primary research, I also began to conduct secondary research on some of the devices I observed. The devices that captured my attention the most were the tonometers: devices that measure intraocular pressure (IOP). The UIC general eye clinic employs two methods of IOP measurement: the Tono-Pen and Goldmann applanation tonometry. To find out more about these methods, I identified a relevant research article and patent.
Study: Accuracy of Dynamic Contour Tonometry, Goldmann Applanation Tonometry, and Tono-Pen XL in Edematous Corneas [1].
This article is an in vitro study on the accuracy of three different methods of tonometry (intraocular pressure measurement): dynamic contour tonometry, Goldmann applanation tonometry, and the Tono-Pen XL. They were specifically tested in the case of edematous corneas. This study is relevant to my observations because I have observed the use of applanation tonometry and the Tono-Pen in the general eye clinic at UIC in the case of edematous corneas due to inflammation or glaucoma. The clinicians claim that the Tonopen is less accurate compared to the applanation tonometer.
This study used 20 porcine eyes that were modified to have hydrostatically adjusted intraocular pressures of 17, 33, and 50 mmHg. The intraocular pressures of each of the eyes was then measured using dynamic contour tonometry, Goldmann applanation tonometry, and the Tono-Pen. Dynamic contour tonometry is a method independent of corneal thickness and curvature where the probe applied to the eye surface matches the contour of the cornea, which indicates that the pressure on the probe is indicative of true IOP. Goldmann applanation tonometry is considered the current gold standard, and it uses the pressure to flatten a specified area of the cornea as an indicator of IOP. The Tono-Pen is an automated handheld tool acting on a principle similar to that of the Goldman tonometer, where pressing the Tono-Pen tip lightly against the cornea flattens a specific area, causing a force transducer to sense the pressure applied to flatten the surface.
The study found that, at 17 and 33 mmHg, both Goldmann applanation and dynamic contour tonometry significantly underestimated the true intraocular pressure. However, the Tono-Pen only slightly underestimated the true pressure at these pressure values, and the difference from control was not statistically significant. At 50 mmHg, however, all three methods significantly underestimated true intraocular pressure. This suggests that Goldman applanation tonometry is the most affected by corneal edema and leads to significant underestimation, while the Tono-Pen is more accurate in corneal edema, although there was still some level of underestimation.
This in vitro study is somewhat contradictory to what we have heard from clinicians; although Goldmann applanation is the gold standard for most cases, it is calibrated based on average population values of corneal thickness, shape, and rigidity, which do not match the characteristics of corneal edema.
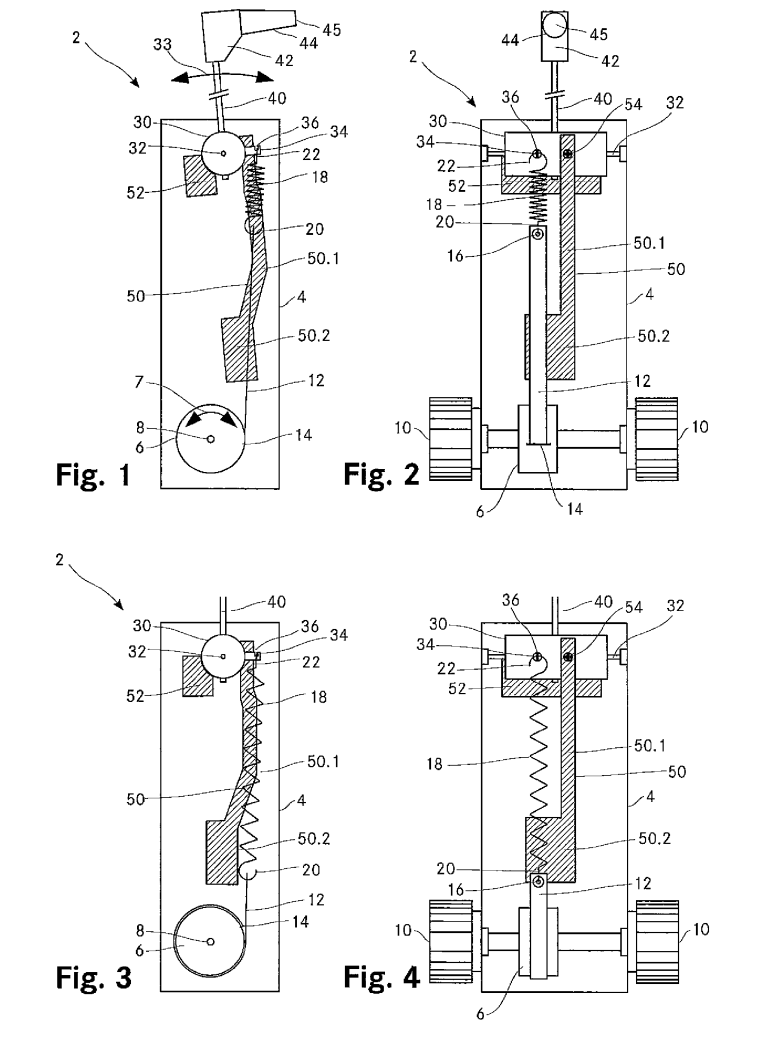
Patent: Haag-Streit Diagnostics Applanation Tonometer (8,303,501)
Since we observed a slit-lamp mounted Goldmann applanation tonometer in the general eye clinic, I researched any patents on such a device. The specific tonometer used in the clinic is made by Haag-Streit Diagnostics. Their applanation tonometer was patented on Nov. 7, 2008. The patent cites Goldmann’s original tonometer, as well as several other tonometers, as prior art. The patent distinguishes its invention from prior tonometers by claiming that it is simpler and more cost-effective while still being precise and accurate. In general, applanation tonometers work on the principle that the intraocular pressure is equivalent to the force applied to the eye divided by the area applied to it. A probe is applied to flatten the eye in a specific area, and the pressure required to flatten the eye is equivalent to the intraocular pressure upon flattening. See the figure above for reference.
This patent has two independent claims, one claiming the apparatus and one claiming the method for intraocular pressure measurement. The apparatus claim claims a tonometer that uses a measurement body (a probe), attached to a measurement arm, with a rotary knob coupled to the measurement arm by a spring, with at least one balancing weight to account for changes in torque on the measurement arm due to changes in spacing between the eye and the measurement body. Independent claims either directly or indirectly referring to the apparatus claim add specific modifications to the basic apparatus, including the material type of the tension material (helical spring, steel band, flexible/inductile material), a display device to display the rotation angle of the rotary knob (showing the applanation force), and a microprocessor attached to the rotary knob shaft to digitally measure the applanation force. The method claim claims an intraocular pressure measurement method where the applanation force required for flattening the eye is transmitted from the aforementioned rotary knob to the measurement arm and measurement body via a tension coupling (spring, elastics, etc.); in other words, it claims the applanation tonometry method dictated by the apparatus described in the first independent claim.
Although there is a wide variety of prior art in terms of Goldmann applanation tonometers, this patent makes it clear that the applanation tonometer used in the UIC general eye clinic is simpler while still applying the same tonometry principles.
Week 3: EYE-dentification and Iteration of a Need
Based on our observations and research thus far, I identified a specific need in the OR relating to the intraocular pressure (IOP) control system used during vitreoretinal surgery.
1st Iteration:
Needs statement: Ophthalmic surgeons are restricted to indirect monitoring and control of IOP, requiring communication with a scrub nurse, and they need to reduce occurrences of mismanagement of IOP.
- Population: Ophthalmic surgeons
- Ophthalmic surgeons are the ones performing eye surgeries that require control of IOP. Since IOP control is not specific to any ophthalmic specialty (retina, cornea, glaucoma), this is properly broad
- Opportunity: Restricted to indirect monitoring and control of IOP, requiring scrub nurse communication
- Based on my observations, the chief surgeon performing the operation did not have direct control over IOP, relying on communication with a scrub nurse to control the IOP.
- Outcome: Reduce occurrences of IOP mismanagement
- By addressing the opportunity of indirect IOP control, IOP mismanagement can be curtailed.
This needs statement was based on primary observations and secondary technical and business research described below.
Primary Data:
In the OR, the surgeon was performing a vitrectomy and used the Alcon Constellation Vision System to monitor and maintain IOP. The surgeon had to constantly ask the scrub nurse what the IOP setting was on the machine and had to tell the scrub nurse to change the IOP setting to a specific number, after which the scrub nurse would press a button on the touch screen to change it. A miscommunication occurred where the scrub nurse did not increase the pressure when asked, leading to too low of an IOP and causing slight retinal hemorrhage.
During another vitrectomy, the IOP suddenly dropped to zero on the machine without any explanation, and the surgeon was not aware of it until the scrub nurse noticed and frantically increased the pressure.
Based on these observations, we identified the indirect control of IOP by the surgeon as an opportunity for our needs statement, with the scrub nurse miscommunication being a key point of error.
Technical Secondary Research:
To supplement the primary observations, I identified several patents relating to the Alcon IOP control system used in the UIHealth OR and several journal articles describing the consequences of improper IOP.
Patent: Intraocular Pressure Control (7,326,813): This patent claims a method of controlling intraocular pressure with a microsurgical system that controls the infusion of an irrigating fluid from two infusion chambers during a microsurgery. A flow rate sensor is used to predict the intraocular pressure within the eye due to the infusion, and a second signal from the computer is used to maintain the predicted IOP inside the eye.
Patent: Intraocular Pressure Control (8,430,840): This patent claims a method of controlling intraocular pressure via computer-controlled infusion that maintains a set IOP. The IOP is set to a desired level via a user input (touch screen, etc.) that triggers infusion of saline into the eye at a flowrate sufficient to achieve the desired IOP.
Patent: System and Method for a Procedure Based Graphical Interface (9,320,646): This patent claims a method of performing surgical procedures through a graphical user interface on a machine, where the user can provide inputs to several devices and functionalities (one of them being IOP control). The patent illustrates the use of a touch screen attached to the body of the surgical machine as an example of user input.
Literature Reviews: When IOP is too low, several pathologic events can occur in the eye. The choroid (the vascular middle tissue layer of the eye) can detach, and choroidal vessels can rupture to produce hemorrhaging of the choroid. Ocular decompression retinopathy can also occur, leading to intraretinal hemorrhage and loss of vision [1]. Furthermore, sudden decreases in IOP can cause sudden microbubbles to form from dissolved gas, leading to gas emboli and ischemic tissue damage [2]. When IOP is too high, on the other hand, there is excessive mechanical stress on the retinal nerve layer, potentially producing retinal ischemia and necrosis [2]. These secondary sources highlight the importance of maintaining a proper IOP especially during surgical operations requiring removal of the vitreous humor in the middle of the eye (vitrectomy).
This secondary research informed the needs statement by highlighting how it is important to avoid mismanagement of IOP (the outcome) and by showing how the IOP control system is designed to be controlled via a separate touch screen, although the patents did not necessitate that user input method.
Business Secondary Research:
One key competitor in the IOP control system market is Alcon Inc. They are a public company based in Switzerland with a global market presence that produces equipment used in cataract, retinal, and refractive surgeries, including vitrectomy machines for IOP control. Their main focus is surgical device production. UIHealth uses the Alcon Constellation Vision System during vitrectomies or other eye surgeries requiring IOP control.
Another key competitor is Carl Zeiss AG, a private company based in Germany. They have a global market presence and are focused on semiconductor production, industrial quality and research, and medical technology production, including vitrectomy machines for IOP control. Their main focus is semiconductor manufacturing, with only a moderate focus on medical technologies.
To get a sense of the potential for solutions in the IOP control system market, I calculated the total addressable market (TAM) for IOP control systems. TAM is equal to the number of units/uses per year of the product multiplied by the estimated unit cost per product.
IOP needs to be controlled in anterior (cataract) and posterior (vitrectomy, glaucoma) surgeries that penetrate the eye, so to determine the number of units used per year, I collected the numbers of vitrectomies, cataract surgeries, and glaucoma surgeries performed per year in the US. In the US, 225,000 vitrectomies per year are performed [3]. For cataract surgeries, 3.7 million are performed per year [4]. For Glaucoma surgeries, 175,000 are performed per year [5]. Therefore, the total uses per year is 225,000 + 3.7 million + 175,000 = 4,100,000 per year in the US.
To estimate the unit cost per use of the IOP control system, healthcare cost databases were not specific enough; they only identified the cost per entire surgery rather than the cost of specifically using the device. Instead, I estimated the unit cost by identifying the cost of the machine used at UIHealth and dividing that cost by the lifetime of the product, which would distribute the value of the machine evenly over the duration of its use. The cost of the Alcon Constellation Vision System is $13,990 [6], and Alcon typically supports a system for 5-10 years until it no longer provides replacement parts/units [7]. Assuming the device lasts for the maximum time Alcon supports the system, I calculated the cost per year of the device: $13,990/10 = $1,399 per year cost.
Therefore, the TAM is:
TAM = (4,100,000 uses per year)*($1,399 per year cost) = $5.7359 billion
Clearly there is a substantial market for IOP control devices during eye surgeries, justifying the needs statement.
2nd Iteration:
Based on careful reconsideration of my research and data, I rewrote the needs statement to better reflect the need and the desired outcome.
Needs statement: Ophthalmic surgeons are restricted to indirect monitoring and control of IOP, and they need to reduce occurrences of vision-threatening outcomes secondary to IOP mismanagement.
- Population: Ophthalmic surgeons.
- Ophthalmic surgeons are the ones performing eye surgeries that require control of IOP. Since IOP control is not specific to any ophthalmic specialty (retina, cornea, glaucoma), this is properly broad.
- Opportunity: Restricted to indirect monitoring and control of IOP
- Based on my observations, the chief surgeon performing the operation did not have direct control over IOP, relying on someone else to provide user input
- Outcome: Reduction of vision-threatening outcomes secondary to IOP mismanagement.
- The main problem caused by indirect IOP control is the damage to the eye due to excessive or insufficient IOP.
The opportunity was changed to exclude the specification of scrub nurse miscommunication because, although such miscommunication was observed at UIHealth, we cannot assume that every hospital uses scrub nurses to operate IOP control systems in this way.
The outcome was changed to be a reduction of vision-threatening outcomes secondary to IOP mismanagement. The original statement was focused on IOP mismanagement events themselves, but the actual clinical outcome of interest is what happens to the patient due to IOP mismanagement. As previously specified in my secondary technical research, vision-threatening outcomes due to IOP mismanagement include retinal/choroidal hemorrhaging and retinal ischemia. These are complications of eye surgery that can be more easily monitored than IOP mismanagement.
Works Cited:
[1] Okonkwo ON, Tripathy K. Ocular Hypotony. [Updated 2023 Aug 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK582144/
[2] Machiele R, Motlagh M, Zeppieri M, et al. Intraocular Pressure. [Updated 2024 Feb 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532237/
[3] Reddy RK, Lalezary M, Kim SJ, et al. Prospective Retinal and Optic Nerve Vitrectomy Evaluation (PROVE) study: findings at 3 months. Clin Ophthalmol. 2013;7:1761-1769. doi:10.2147/OPTH.S49375
[4] Rossi T, Romano MR, Iannetta D, et al. Cataract surgery practice patterns worldwide: a survey. BMJ Open Ophthalmol. 2021;6(1):e000464. Published 2021 Jan 13. doi:10.1136/bmjophth-2020-000464
[5] Ma AK, Lee JH, Warren JL, Teng CC. GlaucoMap – Distribution of Glaucoma Surgical Procedures in the United States. Clin Ophthalmol. 2020;14:2551-2560. Published 2020 Aug 28. doi:10.2147/OPTH.S257361
[6] Shape Ophthalmics. shapeophthalmics.com. Accessed July 8, 2024. https://shapeophthalmics.com/product/alcon-constellation/
[7] Still Servicing Alcon Accurus, No Need to Retire. medisurg.com. Published September 8, 2017. Accessed July 8, 2024. https://medisurg.com/2017/09/08/still-servicing-alcon-accurus-no-need-retire/
Week 4: Rev-EYE-sing my Needs Statement
Needs Statement Revision:
My needs statement from last week was as follows:
Ophthalmic surgeons are restricted to indirect monitoring and control of IOP, and they need to reduce occurrences of vision-threatening outcomes secondary to IOP mismanagement.
- Population: Ophthalmic surgeons
- Opportunity: Restricted to indirect monitoring and control of IOP
- Outcome: Reduction of vision-threatening outcomes secondary to IOP mismanagement
Although technically the components are acceptable, I recently realized that the scope of this needs statement is a bit artificial. It focuses primarily on IOP control during vitrectomy; however, the machine used to control IOP also has multiple other functions that are crucial to vitrectomy. The scrub nurse operating the machine on behalf of the surgeon not only has to adjust IOP, but they also have to activate the proportional vacuum (when sucking out the vitreous humor), fill in gas syringes (for gas bubble insertions into the eye), and control the wattage and pulse pattern of the endolaser (for retinal detachment). I came to this realization because I noticed that IOP mismanagement was only a small part of all the observations we saw. The majority of observations included inefficiencies caused by the scrub nurse needing constant back and forth communication with the chief surgeon to operate the all-in-one vitrectomy machine (Alcon Constellation Vision System).
Therefore, I created a new needs statement to reflect this new scope:
Ophthalmic surgeons are restricted to indirect monitoring and control of vitreoretinal surgery device settings (IOP, endolaser controls, vacuum controls, etc.), and they need to reduce occurrences of vision-threatening outcomes secondary to vitreoretinal device mismanagement.
- Population: Ophthalmic surgeons
- Opportunity: Restricted to indirect monitoring and control of vitreoretinal surgery device settings
- Outcome: Reduction of vision-threatening outcomes secondary to vitreoretinal device mismanagement.
This needs statement was also heavily influenced by key changes in the three components of the IDEO model (Desirability, Feasibility, Viability) based on recent observations and findings.
Desirability (Primary and Secondary Data):
Although last week I had listed observations about IOP mismanagement due to miscommunication between the scrub nurse and chief surgeon, there were many other observations involving indirect control of the vitreoretinal surgery device by the surgeon.
When operating the vitrector (which cuts and sucks out the vitreous), the chief surgeon would have to tell the scrub nurse to activate the proportional vacuum on the device. When the surgeon needed gas to perform a gas bubble insertion into the eye, the chief surgeon would have to tell the scrub nurse to prepare the gas, and the nurse would have to insert a syringe into a port on the machine and activate the machine to fill the syringe with sulfur hexafluoride gas before handing it off to the surgeon. Similarly, when using the endolaser, the scrub nurse would have to plug in the laser probe into the machine and then input specific settings to control the laser (wattage, pulse pattern) in accordance with the surgeon’s verbal demands. We observed a miscommunication with the laser where the laser had been set to a continuous pattern rather than a pulsatile one, similar to how a miscommunication led to errors in the IOP setting. Furthermore, as we observed last week, the surgeon had to constantly ask the scrub nurse what the current IOP setting was and had to constantly ask the scrub nurse to change it on her behalf. In total, we observed three instances of IOP mismanagement due to this indirect control scheme. The first one involved the scrub nurse not setting the IOP high enough when the surgeon asked, resulting in slight retinal hemorrhage in the patient and prompting the surgeon to use the endolaser to stop the bleeding. The second one involved a strange case where the machine’s IOP setting suddenly went to zero, and it took 2 to 3 seconds for the scrub nurse to realize the malfunction and correct it. The third one involved another miscommunication where the surgeon had to yell three times to change the IOP before the scrub nurse became aware and changed it. Our interview with Dr. Lim, the retinal surgeon we observed, confirmed her frustration with having to communicate with the scrub nurse, made worse by the fact that the nurse was a trainee.
These primary observations show that IOP control is not the only issue that should be addressed in the OR. There is clearly a problem with the indirect control of the vitreoretinal surgery devices in general, which is why my needs statement was changed to reflect this newly-scoped desirability.
Feasibility (IP and Commercial Solutions):
Last week I focused on IP and commercial solutions for IOP management specifically, but since the problem extends beyond IOP, I found several patents and commercial products that relate to control of vitreoretinal surgery in general.
A patent from Alcon (8,272,387) describes the graphical user interface for controlling the Alcon Constellation Vision System (the all-in-one vitreoretinal surgery device). It claims a touch screen where an operator can drag and drop specific surgical operations onto a touch screen to control the steps to be performed during the surgery. This gives further insight into how most, if not all, functionalities required in vitreoretinal surgeries require indirect control by an individual other than the surgeon via an external input method like a touch screen.
As for other commercial solutions, I identified several devices that function as “all-in-one” vitreoretinal surgery devices.
The Alcon Constellation Vision System is a device equipped with IOP control, endolaser, gas bubble insertion, and a 3D visualization system (NGENUITY), and it is operated via a touch screen (as previously described) as well as foot pedals to give the chief surgeon some control over certain tools like the laser or vitrector.
The EVA Phaco-Vitrectomy system (by Dutch Ophthalmic) is another system that provides precise IOP control via “flow” and “vacuum” modes, and it is fully programmable to fit the surgeon’s preferences. It also comes with a touch screen and a foot pedal to operate it.
The Stellaris PC (by Bausch + Lomb) is a combined surgical system that allows for both cataract and retinal surgery, providing functions like phacoemulsion, vitrectomy control (IOP, vacuum), and more. It also comes with a touch screen and foot pedals.
Overall, the major vitreoretinal surgery devices that are commercially available are extremely similar in that they support multiple vitreoretinal devices/functions and offer the same peripheral controls (touch screen, foot pedal).
This updated feasibility assessment shows that most vitreoretinal surgery devices do require some form of indirect control, reflecting my updated needs statement. Although there is some form of direct control via a foot pedal, another person must be present to operate the touch screen, which is arguably more important because the touch screen is where settings are changed, and different functionalities are selected.
Viability:
Last week, my viability assessment included a general market assessment and a calculation of the total addressable market (TAM). However, the TAM was inaccurate because it did not properly account for the cost of consumables, maintenance costs, and the cost of the machine itself. When using the vitrectomy device, there are several consumables packaged in “vitrectomy packs”: disposable laser probes, forceps, scissors, tubing for infusion (IOP control), and more. According to a study, the average material cost per eye surgery is $979.60 [1]. There are a total of 4,100,000 surgeries per year in the US requiring the use of devices like the Alcon Constellation Vision System: 225,000 vitrectomies + 3.7 million cataract surgeries + 175,000 glaucoma surgeries [2,3,4]. This means that the total cost of consumables per year is: 4,100,000 * $979.60 = $4.02 billion per year.
The cost of the Alcon Constellation Vision System itself is $150,000, and there are roughly 1,409 eye surgery facilities in the US, most of which likely use systems similar to the Constellation system [5]. Therefore, the total cost to all eye surgery facilities is $150,000 * 1,409 = $211,350,000. Alcon typically supports devices for 5-10 years [6]. Therefore, the average cost of all the vitreoretinal surgery devices in the US over their maximum lifetimes is $211,350,000 / 10 years = $21,135,000 per year.
I called Alcon technical support themselves and was able to find out that the bi-annual preventive maintenance cost for the Alcon Constellation Vision System is $3,895. This means that the per-year average maintenance cost is $1947.50.
To calculate the TAM, I added these per-year costs together:
$4.02 billion + $211,350,000 + $1947.5 = $4.23 billion.
This new TAM seems much more reasonable as it reflects the market for vitreoretinal surgery devices accounting for multiple sources of cost.
New Needs Statement:
Besides revising last week’s needs statement, I made several new observations that led to the creation of a new needs statement.
In the retina clinic, I observed a retina specialist using the indirect ophthalmoscope:
- Activities: Retina specialist wearing the indirect ophthalmoscope on head and looking into patient’s eye using the ophthalmoscope and a handheld lens from different angles.
- Environment: Retina clinic room
- Interactions: Retinal specialist told the patient, lying down on reclined chair, to look in different directions while the specialist looked into the pupil with the ophthalmoscope and a handheld lens placed in front. Retinal specialist had to tilt their own head in different directions.
- Objects: Head-mounted indirect ophthalmoscope, handheld 20D lens, ophthalmoscope charging station mounted to the wall
- Users: Retinal specialists, residents.
The key insight in this observation is that the retinal specialist had to contort their neck into uncomfortable positions while wearing the indirect ophthalmoscope in order to be able to see into the eye and visualize the peripheral retina. Interviews with the specialist confirmed this: the retina specialist told us that ophthalmologists in general often struggle with neck strain and neck problems due to long-term use of eye-visualizing devices, with the indirect ophthalmoscope being the biggest culprit due to it relying on neck-straining head positions. Another retina specialist and an oculoplastics specialist also confirmed these findings, saying that many devices in ophthalmology can put stress on the neck and back of ophthalmologists.
Therefore, my new needs statement is:
Ophthalmologists experience high neck strain during indirect ophthalmoscope usage, and they need to reduce occurrence of chronic neck problems.
- Population: Ophthalmologists
- Opportunity: High neck strain during indirect ophthalmoscope usage
- Outcome: Reduce occurrence of chronic neck problems.
Works Cited:
[1] Pan WW, Portney DS, Mian SI, Rao RC. The Cost of Standard and Complex Pars Plana Vitrectomy for Retinal Detachment Repair Exceeds Its Reimbursement. Ophthalmol Retina. 2023;7(11):948-953. doi:10.1016/j.oret.2023.06.021
[2] Reddy RK, Lalezary M, Kim SJ, et al. Prospective Retinal and Optic Nerve Vitrectomy Evaluation (PROVE) study: findings at 3 months. Clin Ophthalmol. 2013;7:1761-1769. doi:10.2147/OPTH.S49375
[3] Rossi T, Romano MR, Iannetta D, et al. Cataract surgery practice patterns worldwide: a survey. BMJ Open Ophthalmol. 2021;6(1):e000464. Published 2021 Jan 13. doi:10.1136/bmjophth-2020-000464
[4] Ma AK, Lee JH, Warren JL, Teng CC. GlaucoMap – Distribution of Glaucoma Surgical Procedures in the United States. Clin Ophthalmol. 2020;14:2551-2560. Published 2020 Aug 28. doi:10.2147/OPTH.S257361
[5] Eye Surgery Clinics in the US – Number of Businesses. ibisword.com. Published May 18, 2024. Accessed July 15, 2024. https://www.ibisworld.com/industry-statistics/number-of-businesses/eye-surgery-clinics-united-states
[6] Still Servicing Alcon Accurus, No Need to Retire. medisurg.com. Published September 8, 2017. Accessed July 8, 2024. https://medisurg.com/2017/09/08/still-servicing-alcon-accurus-no-need-retire/
Week 5: Recogn-EYE-zing Processes and Pain Points in a Storyboard
This week, I developed a storyboard to track the need I had identified last week:
Ophthalmologists experience high neck strain during indirect ophthalmoscope usage, and they need to reduce occurrence of chronic neck problems.
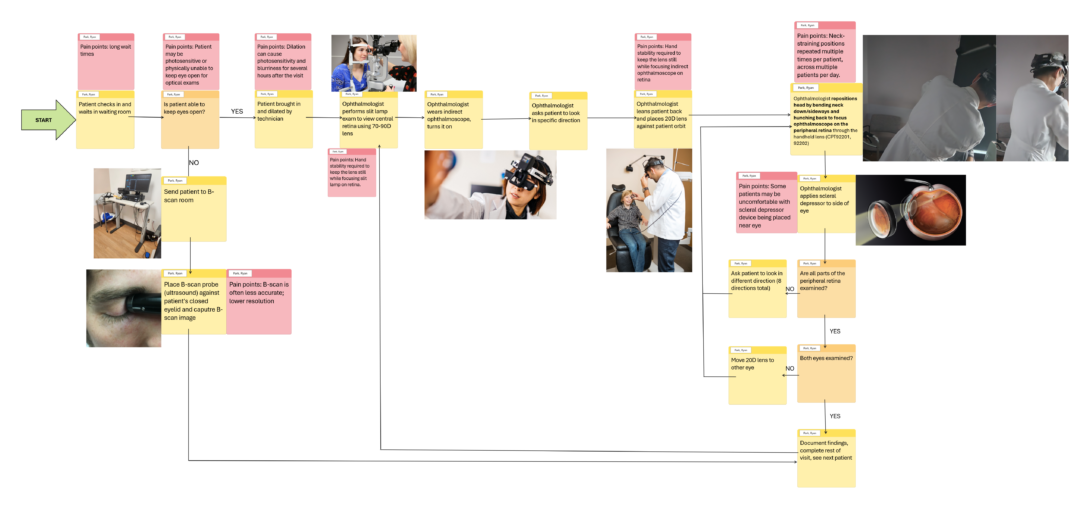
I tracked the typical events that occur at the retina/general eye clinic that require use of the indirect ophthalmoscope with an emphasis on areas of high neck strain. These events are organized in the storyboard above.
Patients are treated based on whether or not they are able to open their eyes. If not, they perform a B-scan; if they are, they undergo retinal examination via a slit lamp and the indirect ophthalmoscope. The slit lamp is for central retinal viewing, while the indirect ophthalmoscope is meant for peripheral retinal viewing.
Notice how the main area of neck strain (use of the indirect ophthalmoscope; see far right of diagram) occurs within a triple-nested cyclic region of the diagram: the innermost cycle is for each time the patient has to move their eye to a different position, the second cycle is for both eyes to be checked, and the outermost cycle is the repetition of the whole retinal exam for every patient the ophthalmologist is seeing for the day. This suggests that ophthalmologists exert high neck strain very frequently throughout the day.
Week 6: My F-EYE-nal Entry
My time observing at the ophthalmology department was an invaluable experience. I learned that, despite ophthalmology being restricted to the eye, the subspecialties within the field are very unique from one another. Observing oculoplastics specialists, cornea specialists, retina specialists, and more allowed me to appreciate the diversity of ophthalmology. From the physicians that I shadowed, I learned that ophthalmology is a device-focused specialty, relying on a plethora of diagnostic and treatment devices to treat a variety of eye conditions. Ophthalmology is a profession cluttered with machines. From the Clinical Immersion program itself, I learned that clinical reasoning and problem-solving skills are different things. While clinical reasoning can solve a patient’s problem, it does so through established evidence-based algorithms. Problem-solving skills, however, require thinking outside the box to identify problems; they require questioning the very algorithms that clinicians trust so much. A good physician can memorize current best-practice treatments, but an impactful physician can understand those best-practice treatments to the point where they can begin to question them and seek better ways through innovation and research.
For future CIP participants, I would recommend keeping an open mind for the first half of the program. You will see many obvious problems on the first weeks that you may think are worth addressing, but you may find later that the problem is not as important as you originally thought. You should not hesitate to let go of ideas and embrace new ones.
Overall, the Clinical Immersion Program gave me valuable insights into needs identification in the clinical setting, and I hope I can leverage these skills in the future to pursue my own innovation.
Goodb-EYE!