
Nisarg Patel
2023 students
UIC BME Undergraduate
Department of Anesthesiology
Pronouns: He/Him/His
Email:
Weekly Blog: Week 1 Heading link
During this past week our team was distributed into two groups and we had the opportunity to observe various procedures within the operating room, under the guidance of Dr.Deburghgraeve and Dr. Spina. The main assignment for this week was to observe as much as we can and start to identify potential clinical needs that we could address in the following weeks. This appears to be a simple task, however it proved to be more challenging for a variety of reasons. One major obstacle was understanding medical terminology as I have just finished my junior year of my undergraduate studies and do not have much medical knowledge. Another obstacle was getting acclimated to the environment within and around operating rooms, as this is my first time in such a setting. Although the learning curve is steep, during this past week I have made a few observations and hope to learn more within the following weeks.
Good Design: Anesthesiology Cart / Main cart with vital screens
Activities: The main function of this cart is for the anesthesiologist or the CRNA to monitor and control the amount of anesthesia given to the patient.
Environment: This cart is off to the side of the patient and often the tubes on the cart are connected to the patient orally or through the nasal passage way.
Interactions: The CRNA or the anesthesiologist are the people who interact with this cart and the machines within the cart to deliver anesthesia and monitor patient vitals.
Objects: This cart has two monitors that display the patient vitals in a very efficient and simple manner, furthermore this cart also has dials and buttons through which the amount of anesthesia can be controlled.
Users: Primarily the anesthesiologists and CRNAs who monitor patient vitals and administer the anesthesia
Bad Design: Arterial Catheter (A-line Catheter)
Assuming not particularly designed to work with left handed people. Upon talking to Dr. Spina, primarily left-handed, mentioned that sometimes when he was using the a-line catheter he would find it awkward to use sometimes as his arms would cross over.
Activities: A thin, hollow tube that is placed into an artery to measure blood pressure more accurately than is possible with a blood pressure cuff.
Environment: Primarily used in an surgical setting when arterial pressure requires continuous monitoring
Interactions: the anesthesiologist or the CRNA is usually the one to insert the A-line catheter into the patient
Objects: the overall design of the catheter
Users: The anesthesiologist or the CRNA inserting the A-line catheter
Week 2: Storyboarding Heading link
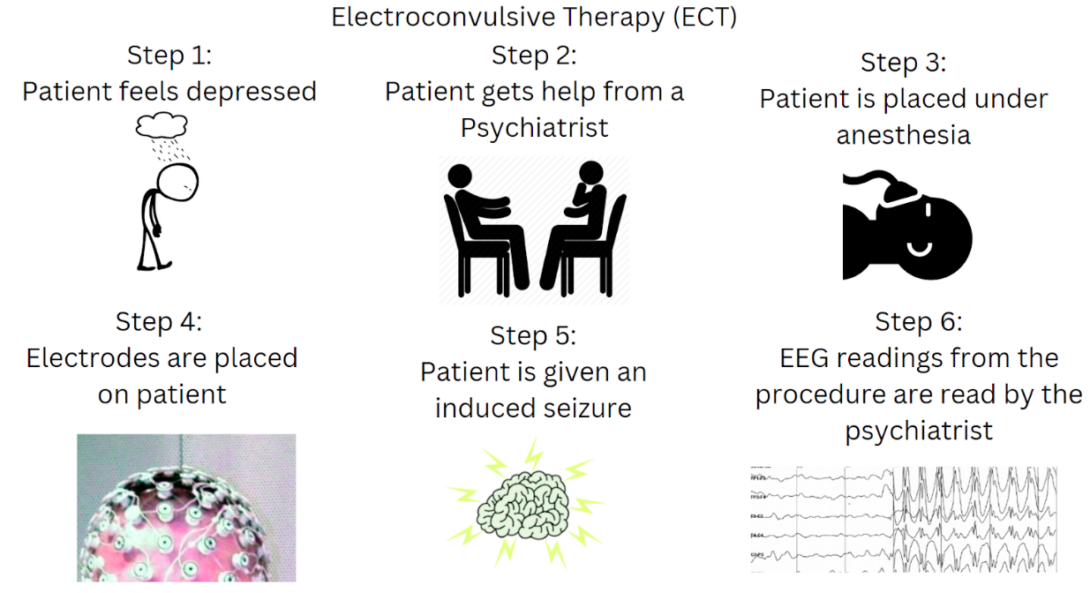
Possible Pain Points:
Step 1: Patient notices a decrease in their quality of life due to their depression. This can be considered a psychological pain point rather than a physical pain point.
Step 2: The patient may feel uncomfortable talking to the psychiatrist about their problem.
Step 3: The patient is told about the procedure before undergoing anesthesia which could potentially make the patient anxious about the whole procedure.
Step 5: A controlled seizure is induced onto the patient, complications could arise if the patient’s body does not react in a normal manner.
Electroconvulsive therapy (ECT) is one of the most effective treatment options for severe major depression. However due to the nature of the treatment and public stigma, the treatment option is often limited. The paper that I took a look at below was a clinical trial that examined ECT treatment response in bipolar depression (BPD) and major depressive disorders (MDD) to validate that ECT had faster treatment response time in BPD compared to MDD. The trial concluded that in an academic hospital setting ECT treatments displayed a clinically faster speed of response to BPD.
Images taken from: https://en.wikipedia.org/wiki/Electroencephalography and https://clipart-library.com/
Scheepstra, K. W. F., et al. “Rapid Speed of Response to ECT in Bipolar Depression: A Chart Review.” Journal of Psychiatric Research, vol. 147, 2022, pp. 34–38, https://doi.org/10.1016/j.jpsychires.2022.01.008.
Week 3: Needs Statement Heading link
During this third week of CIP, the assignment was to create a need statement with various iterations. The need statement below is based on observations made in the clinical setting where I assume improvements can be made. The area of improvement focused on below is regarding OR turnover times, which can be affected by various factors and not just the factors listed below.
Need Statement iteration 1: Staff needs increased communication to decrease turnover times.
Population: staff
Opportunity: increased communication
Outcome: decrease turnover time
In this first iteration of the need statement, everything is too broad and not specific enough. As the statement hints at what the problem is but does not narrow down on specifics.
Need Statement iteration 2: Operating room staff need increased communication to reduce any delays and decrease turnover times
Population: Operating room staff
Opportunity: increase communication
Outcome: reduce delays and decrease turnover times.
In this second iteration, I have narrowed in on the population, however the opportunity and the outcome still seem too vague.
Need Statement iteration 3: Operating Room staff need to have better communication regarding timing updates to reduce delays and decrease turnover times.
Population: Operating room staff
Opportunity: better communication regarding timing updates
Outcome: reduce delays and decrease turnover times
In the final iteration I have specified my opportunity and outcome further however I believe this need statement can be further refined. For instance the outcome could be narrowed down to one and therefore making the opportunity more specific.
Upon further review and discussion the need statements above do not have enough background information about the problem to properly construct a needs statement. Therefore more information is required about the situation and how it is currently being addressed within the clinical setting.
Week 4: Patent Research Heading link
For this week’s blog we were assigned to find a patent and review the patent’s approach and summarize relevant claims based on a needs statement. While continuing to observe the anesthesiology department within the OR, I noticed that all the tubes and wires from all the devices were getting into people’s way. For example, in one case alone the surgeon tripped over the mess of wires and tubes twice while trying to switch his position. So my needs statement for this week will be: Anesthesia providers need to have better hanging wire and tubing placements to decrease potential tripping hazards for OR staff while they are performing their duties.
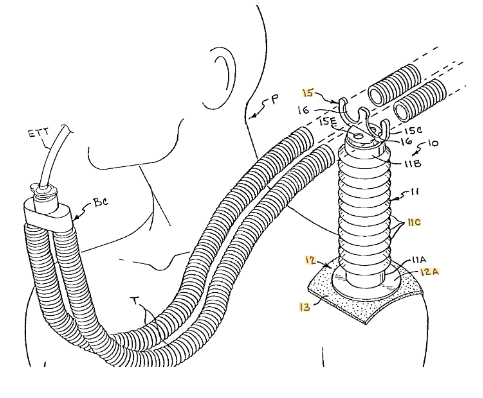
Currently within the operating room the anesthesia providers as well as the nurses work together to minimize tripping hazards in high traffic areas, often the tubes going into the anesthesia cart are left in a messy pile near the cart’s base. For breathing tubes specifically, I have noticed anesthesia personnel using tube holders that they have termed a “tube tree”. The patent that I will be reviewing is called the anesthesia breathing circuit tube support, and it functions similarly to the “tube tree”.
Patent no: US9126005B1 Inventor: Rebecca C. Blaylock
Patent Claims: The device claims to be a breathing tube support device that basically attaches to the patient or a surface in order to support/hold at least one breathing tube from a breathing tube circuit. The device consists of three distinct components: a flexible support arm, a mounting base at the bottom end of said flexible support arm, and a breathing tube holder member at the top end of said flexible support arm. The claims go into further detail of different variations of the three components.
References: https://patents.google.com/patent/US9126005B1/en
Week 5: Total Addressable Market (TAM) Heading link
This past week we have continued to shadow and observe the anesthesiology department. For this week’s blog we have been assigned to build a total addressable market (TAM) for a specific tool. The instrument that I am going to build my TAM is the laryngoscope. So far in every single procedure that I have observed, a laryngoscope has been used by the anesthesiology team to insert a breathing tube at the beginning of every procedure. According to global news wire a total of 105,814,500 surgeries were performed in the US during 2022.
According to Mordor intelligence, the laryngoscope market is comprised of the following: several different types of laryngoscopes, the different components of laryngoscopes, and the usability of laryngoscopes. Due to a lack of publicly available information on laryngoscopes, for the TAM estimate I will be assuming that all the surgeries will be performed with a basic disposable laryngoscope blade. Based on laryngoscope prices from mdmaxx, I will be using a conservative estimate of $30 per disposable laryngoscope blade. After multiplying the price per laryngoscope blade and the total number of surgeries performed in 2022, the calculated TAM estimate comes out to be $3,174,435,000. However, this TAM is just an estimate that does not include group purchasing organization preferred pricing that hospitals utilize nor does it take into consideration bulk pricing discounts. Additionally not all procedures may use a laryngoscope to insert breathing tubes, and not all procedures utilize the same laryngoscope. Therefore this TAM estimate may be grossly inaccurate. A better approach in calculating the TAM would be to take a look at the sales information for laryngoscope blades or by creating a TAM of video laryngoscopes by looking at those sale numbers, unfortunately those purchase order forms or sales order forms are not publicly available.
https://www.mordorintelligence.com/industry-reports/laryngoscope-market
Week 6: Conclusions Heading link
As this program comes to an end, looking back these past six weeks have been greatly rewarding. Over the past few weeks, I have had the opportunity to observe the operating room, the pain clinic, the ICU and the speciality care building over at UI health. Through these experiences I have gathered more insight on device innovation and how a device is brought to the market. Below are some lessons that I learned over the course of CIP.
1: Being inexperienced is sometimes a good thing as it provides a fresh perspective which could provide potential opportunities for innovation.
2: Needs are not always complex, sometimes they are simple things. Oftentimes the need will stem from minor inconveniences that can be overlooked easily.
Recommendations for future CIP participants:
- Don’t be afraid to ask questions. The staff was more than willing to answer questions when they were not busy.
- Be open minded and do not constraint yourself to a single idea.