
Stuti Patel
Student Participant
Week 1: Not for a "Faint" of Heart Heading link
During the first week of the Clinical Immersion Program, my group and I spent most of our time in the OR observing surgeries. Each day was a new experience and as our knowledge and comfort in the OR grew, the more we were able to learn. Personally, I struggled hard on the comfort aspect of this experience. While I knew I was going to be immersed into a hospital experience, I did not fully understand that we were going to be watching some very intense procedures, which were, as my group member said, not for the “faint of heart.” I did feel as though some parts of surgeries were too difficult for me and I would feel too lightheaded and woozy, but as time went on, and I was able to sit through more procedures, I began to feel much more comfortable.
Our main focuses this week were to observe and ask questions. For that reason, one of my favorite things that we observed was the full experience of a patient, pre-op to post-op, which allowed me to have some of my previous questions answered through observation. Our best resources were the OR staff: surgical nurses, registered nurses, techs, and most importantly the anesthesiology residents. We were very lucky to have such kind people that were always asking us if we had any questions or were readily available to explain any process to us as we were observing.
Good Design: Throughout the hospital, I saw so many devices that were completely new to me. The most practical and almost “duh” design was the X-Ray machine placed into an OR for real-time X-Ray results of a heart. The surgeon was performing a bypass using an arterial graft on a patient but there were so many wires and stents needed to be placed within the heart which required extreme precision. For this invasive and detailed surgery, using an X-Ray machine that can be placed within the patient and for it to deliver real-time information for the most accuracy is so important and valuable for time and patient experience. To specify, a tech or nurse having to run back and forth for X-Ray results would be huge waste of time as well as would deter accuracy for the surgeon.
Bad Design: One of the most apparent issues in the OR are the wires that are laying everywhere, especially near the anesthesiologist as they have multiple wires for drug delivery. While these anesthesiologists have so much practice dealing with their own organization, it really does change from person to person so there is no order for the wires and bags of the drugs. It seems that there is just a mess of wires that get messed up/ confused. I have attached pictures of an example of just wires. Other times, there were plugs for important pieces of equipment, like the vitals monitor, plugged into a socket that could be kicked by any body which also seemed like a huge hazard.
What a great week!
Week 2: Narrowing the Scope Heading link
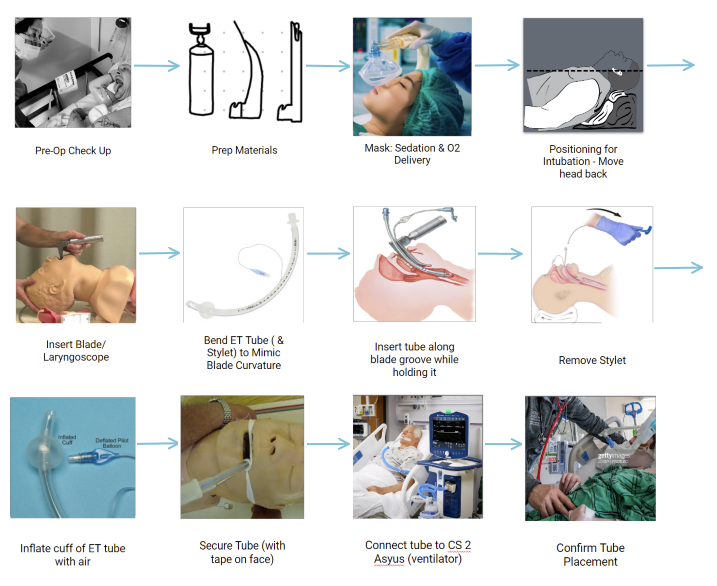
This week, my group and I returned to the OR with a narrower focus to observe the ideal intubation process. During the first week, we were immersed in the OR and trying to find the way of the land. Personally, I felt that having this experience in the first week really allowed us to narrow down into a specific process because we weren’t worried about having to find our way through the hospital. Most of my time was spent asking medical students and/or residents, who were conducting the intubation, questions about the process after they were done. We were so grateful that they were able to explain step-by-step because they learned that process from professionals and were able to break it down for us. In addition, because the medical students and residents are relatively new at the procedure, they were able to identify pain points in the process that would not be recognizable from a spectator. Observing the process also allowed us to see how important it is for the person intubating to be well trained for emergencies and a variety of different circumstances.
Clearing the airway is one of the most important procedures in a surgical or emergent process and can be done through intubation. However, the process itself is not the most perfect and there are many “pain points” that can be identified. As a group, we chose to focus on the most ideal intubation situation, which would be under most surgical situations where there is immediate access to anesthetics as well as all of the tools that would be necessary in case of an emergency. In that way, the oral intubation is the most common which is later followed by the nasal and tracheal. To be able to highlight a most ideal situation, a lot of the “what ifs” must be eliminated from the process, such as if there is swelling that might block the airway or any contamination such as blood and vomit.
Some pain points of the intubation process that we observed were those mentioned before such as swelling of tissue or contamination in the way, making the airway difficult to clear. After speaking with medical professionals and looking through literature, we found that there are approximately 1 million emergent cases a year. Out of those million, approximately 50% of those become adverse events which means causing more damage to the patient as more intubation attempts occur like cardiac arrest, hypoxemia, etc. For that reason, if any of the devices malfunction or intubation is failing, there would be a huge issue in terms of oxygen delivery which can cause brain and other issues.
In the article “Endotracheal Intubation Training and Skill Maintenance for Respiratory Therapists” by Andrew G. Miller, the results to a study for the skill maintenance of a respiratory therapist found that there are about three ways for one to practice an intubation: simulation training, supervised intubation, and classroom teaching. Some hospitals require mandatory 10 or fewer supervised intubations while others require written tests or classroom teaching. This type of regulated teaching keeps the skills sharp and encourages quick thinking in case of emergent airway situations.
Week 3: "Need" to Lessen the Pain Heading link
The past couple of weeks in the Clinical Immersion Program, I suspected my third week to look very similar to the others- in the OR. The doctor my group and I have been shadowing is a man who wears many hats and I was pleasantly surprised to see one of our days dedicated to listening to his meetings and seeing the kind of work he does outside of the OR. On the same day, we were able to experience one of the most “15 minutes of fame” moments at this point. The hospital is in the works of opening the new outpatient surgical building just across the street with a lot more functional space and ORs. My group and I were lucky to be able to tour some parts of the building, and also be extras in a safety video involving our doctor comforting a fake patient. It was amazing to see the different aspects of the job that are relevant to using OR, which humanized the whole experience for me. Oftentimes, I felt that the flow of the OR was a tad robotic because of the protocols and sterile procedures, but spending some time in the scenes put pieces of the puzzle together by seeing how functions make surgical procedures work smoothly.
In class, we defined our main objective for the week: observing a need and developing different need statements from the observation. Naturally, my group and I had been noticing several issues that were obvious to anyone: the mess of wires in the anesthesia area, tripping hazards from plugged-in wires, and many more. Some processes, in contrast, were very well thought out and had specific steps to follow, such as the intubation process. However, in a deeper look behind the scenes through listening in on phone calls with a resident for pre-op screening and then in the pre-op clinic, I realized that one of the main points that the doctor claims is that the intubation process can cause pain to the teeth, gums, and throat. As intubation, aware later extubation is one of the most vital parts of an emergent or surgical situation, I was confused as to why there is still not a smooth process that can prevent this kind of pain. After doing further research, I found that the sore throat from the intubation process is a prevalent issue during the anesthesia portion of a procedure and brings a bit of discomfort to the patient after extubation.
Needs Statements:
With this iteration, I was focusing on the anesthesiologists’ point of view where they can focus on how the tube is inserted can affect how the patient is scratched, ultimately causing pain. I was also trying to prevent the scratches and not only the pain as they are the leading issue in this scenario.
#1: Anesthesiologists in a surgical setting who need to clear the airway through intubation may cause the patient pain in the teeth, gums, and throat from the tube scratching the airway and need to prevent the scratch that is leading to the pain
- Population: Anesthesiologists
- Opportunity: Intubation may cause the patient pain in the teeth, gums, and throat by scratching the tube in the airway
- Outcome: Prevent scratches that are leading to pain
In this iteration, I was focusing on the patient pain experience and how the intubation can cause lingering pain through a sore throat. I found that the sore throat was one the most popular things on the list of discomfort after surgery.
#2: Patients in a surgical or emergent setting who need their airway cleared through intubation may experience pain in the teeth, gums, and throat when the tube is pushed into the airway and a sore throat after extubation, and need protection from the pain as well as less lingering pain.
- Population: Patients
- Opportunity: Intubation may cause pain in the teeth, gums, and throat by scratching the airway and a sore throat following extubation
- Outcome: Protection from the pain as well as less lingering pain
In this final iteration, I focused on changing the opportunity to make it nasal intubation that would cause pain in the soft palate as the tube is being inserted through there. As a result of nasal intubation, that rough jab can cause pain in the throat as well, leaving both of them in pain.
#3: Patients in a surgical setting who need to urgently clear the airway through nasal intubation may cause the patient pain in the soft palate and throat by roughly pushing the tube into the airway and need to lessen that pain.
- Population: Patients
- Opportunity: Nasal intubation may cause pain in the soft palate and throat
- Outcome: Lessen pain
Ultimately, the main objective of all of these iterations is to lessen the pain caused by intubation, and later the process of extubation.
Week 4: Patents Heading link
As the focus of this week was on patents, MAUDE database reports, and commercial solutions, I spent most of my time observing the brands of equipment being used. One of my main focuses was based on my needs statements from the week before: endotracheal tubes.
Needs Statement: Anesthesiologists who need to clear the airway through intubation may push the ET tube too far into the lungs and need a solution to keep the device in place as well as control the pressure of inflation of the cuff to keep a tight seal around the airway.
Patent: Endotracheal tube sealing cuff system
Claims: This patent creates a system that allows control of the inflation in the cuff of an endotracheal tube. The tube works by recognizing the inhalation and exhalation of a patient. When the patient expires CO2, the diaphragm returns to a normal position which deflates the cuff to allow for at least a small amount of air to push around the endotracheal tube. Although there is a valve that is kept outside of the airway for the anesthesiologist to be able to use as a method of feeling the pressure in the cuff, this kind of cuff system allows for there to be intelligence that detects when the body moves and change the pressure accordingly. In a more direct way, the deflation of the cuff reduces irritation in the trachea as well.
As a whole, this solution truly encompasses the need well. One of my observations during the week was that there were tests that the anesthesiologists performed to ensure that the ET tube was correctly positioned into the airway and wasn’t too far deep. This is important because if the tube is too far into one lung, only one lung is inflated with air. Obviously, this shows that the proper placement of the tube is very important as well as the inhalation and exhalation of oxygen and CO2 which can be treated with a tight seal around the airway.
At this point in the process, I am finding that the airway is a huge part of anesthesia that really needs focus on. It seems that although there is a specific process when the situation is controlled, there are multiple routes you can take when something goes awry.
Week 5: Market Analysis Heading link
As the final week approaches, we spent a lot of our time focusing our efforts towards finalizing our need and putting together our components of the presentation. We wanted to make sure we incorporated the different things we learned each week into our presentation to really encompass our knowledge.
During the week, we fully put our effort into one needs statement and spent a large quantity of our time researching on that topic. For the needs statement, we decided to push towards the difficult airway route and used a lot of our resources to gain as much knowledge on the topic. For example, we went down to the Emergency Department of the hospital as there was a likelier chance that we would be able to see a difficult airway being handled as well as observe all of the resources that they use. One of the most fascinating parts of our experience was seeing the contents of an airway bag because it has everything one would need when facing a difficult airway. During our interviewing process with nurses and doctors, I found myself being a bit behind on the conversation because I was not already exposed to some methods (like the SALAD technique) or devices that the group was speaking on. Instead of being embarrassed as I was at the start of the program, I developed more confidence and chose to ask the nurses and doctors the small questions in order to keep myself involved. Even at times, I would lean back to one of my group members who have studied some of the information and just quietly ask to not disrupt the conversation. We then were set up by our group member, Nolan, to speak with two flight team members who see difficult airways very often and we learned how they like to attack situations. We found that depending on the hospital’s culture, there were differences in how they behave. Learning even those differences really helped us to look deeper into the issue and see that while there are several ways of working around the problem, but nothing is consistent in terms of methods and fixes. In the same way, it is important to sometimes go think back to the basics and just do simple things like turning the patient to the side to get the vomit out instead of inserting 10 suctions inside of the mouth. Personally, this thought really pushed me back into thinking into the basics and pushed me to not get ahead of myself to find a solution. Obviously difficult airways are a large issue, but rushing into finding solutions to solve the issue as fast as possible for the future is not going to help me.
One tool that was listed as extremely useful was the video laryngoscope for people who dealt with contamination in the airway. It allows most users to push past the contamination and visualize the glottis better. When researching the market, we found that approximately 50 million people are intubated in a year and from those numbers, approximately 10% of those are emergencies. In that sense, 50,000,000 * .1 = 5,000,000. Once you consider a single use video laryngoscope, it comes out to $18 per piece. In total, 5,000,000 * $18 = $90,000,000 TAM.
Week 6: Not Quite the End Heading link
The past 6 weeks have been absolutely incredible to say the least! I came into the program with not many expectations and my mind completely open. I had been hearing about the Clinical Immersion Program since I was a freshman, and I am very grateful that it really did not disappoint.
To future participants, I would really recommend coming in with an open mind about what each day could entail. When speaking with other interns who were in different disciplines, I realized that we had completely different experiences. I spent almost every single day in scrubs, watching surgeries or observing the ICU, while other participants had never scrubbed and were left to be very independent in what they observed. It is also important to note to be very wary of your surrounding and really know when to just stick to a wall and keep quiet or when to freely ask questions to nurses or surgeons. Contrastly, it is important to also not be shy to ask questions when the situation permits. Oftentimes, I found myself way too shy to ask questions because I did not know what to ask or who. It is important to know your place but also feel confident in your abilities because you are only there to help!
Speaking of abilities, the hardest thing when going into a medical facility is trying to fit in as an engineer and not an aspiring medical professional. People spew out medical vocabulary and it is difficult to keep up sometimes, and sometimes asking right then is not appropriate, but it is not embarrassing to not know what things are. Remember to keep your notebook and look things up after the conversation for your own knowledge! It really helped me for future conversations with others. Also remember what you have learned as an engineer when going through this process: engineering design cycles, 3D printing, circuits, product markets, MAUDE database research, etc. This will all be used during this 6 week process and grow your abilities into a full circle product analysis.
Out of all, my most important piece of advice is to wear comfortable shoes because most of the time will be spent on your feet! It was crazy days with lots of walking and standing but those days were the coolest ones where I saw the most AMAZING procedures and devices.
This program has really given me direction on what I would love to do after graduation. I’m so excited for this to continue in Senior Design in the upcoming Fall semester.