
Nora Qatanani
Student Participant
Week 1: Good Designs Vs. Bad Designs
Being the first week of the Clinical Immersion Program, it was challenging not only to remain as a ‘fly on the wall’ but also to fully understand the observations that were being made from a third party standpoint. To accomplish this, I asked many questions to my group mates and Dr. Mehta, who is our clinical mentor in the Neurosurgery department. This also was the first time I had stepped into an operating room, and given the opportunity to observe. It was definitely a memorable experience, watching all the doctors and nurses work together smoothly, almost as if they were gears of the same machine.
My team and I shadowed Dr. Mehta throughout the week, which included observing both the operating room and his clinic. We were able to observe multiple surgeries, some of which were a craniotomy, posterior decompression of the spine, and a bullet removal. Not to mention being able to observe his clinic as well, which includes post-surgical and incoming patients. His clinic had approximately thirty patients that were seen by Dr. Mehta or the other available doctor. That being said, all this allowed the opportunity to observe both good and bad designs being utilized throughout the week.
- Good Design: One good design that I had the pleasure of observing was the Stealth Station of Surgical Navigation. I was able to observe this machine being utilized in a brain surgery that involved a tumor being removed. This machine would allow for the surgeons to use the probe and be able to match the probe’s placement with the previously taken scans. The probe was used to map out the patient’s face, then after the mapping process was completed the probe was able to depict the location of the scans on the monitor. This from what I could tell majorly assisted in surgeons being able to not only locate the brain tumor but also avoid damaging other tissue in the brain. The probe was easy for the surgeon to use and was hand held, making it easy for the one surgeon to use to navigate the brain, while the other removed the tumor.
- Bad Design: One bad design, or rather a design that could be improved, is the chairs in the clinic. Through my observations it was clear that most of the clinic patients I had encountered sat in seats in the room opposed to the examination chair. Some of these patients had come to the clinic seeking consultations, mostly regarding spinal issues or back pain. I noticed many of the patients struggled in sitting up or following the doctor’s directions during the strengths tests during their examinations. Due to the chair being a standard waiting room chair, it does not offer the support/accommodations needed for a patient who is experiencing extreme back pain. Another design that could be improved, my team and I observed the placement of the light switch outside of the operating room. So when one of the anesthesiologists requested for the lights to be dimmed, she had to physically exit the room to accomplish this. The lack of patient comfort/accommodation and the requirement of leaving the operative room to change the level of lighting make these two prime examples of designs that could be improved.
Overall, being able to observe medical devices being used in a clinical setting definitely changed my view of medical devices as a whole. Most specifically, the intuitiveness and the simplicity of use that accompanies medical devices as they are utilized in these clinical settings. Not to mention all the designs that are encompassed in clinical settings that are used to ensure smooth daily operations in hospitals.
Week 2: One Upon a Mayfield, a Storyboard
The second week of the program proved to be challenging again but in ways different than Week One. This week we were given vague instructions on the structure of the week, this led to us spending more time in the Neuro ICU than in the operating room. We spent two days in the Neuro ICU which involved 6 am Surgical Rounds, 8 am Resident Rounds, and observing the inner workings of the ICU. It was interesting to see how different the Surgical Rounds were compared to the Resident Rounds.
The Surgical Rounds mainly involve pre-operative patients or postoperative patients, where the doctors would discuss the updates on the patients first in a conference room, then go on to visit each patient. Which included performing different exams which ranged from asking what year it is or who is the current president, to strength tests such as asking the patient to lift their arms or wiggle their toes. During Resident Rounds the patients were mostly asleep, and the Resident would present on each patient’s progress while being asked questions to justify their medical decisions. The nurse on duty that was monitoring the patient being presented on would also be requested to join for the patient’s presentation by the Resident. Through the Resident Rounds I noticed how much of the information is actually documented on sheets of paper and then the information is relayed through these presentations. This when asked about is in order to avoid over documentation on the patients charts.
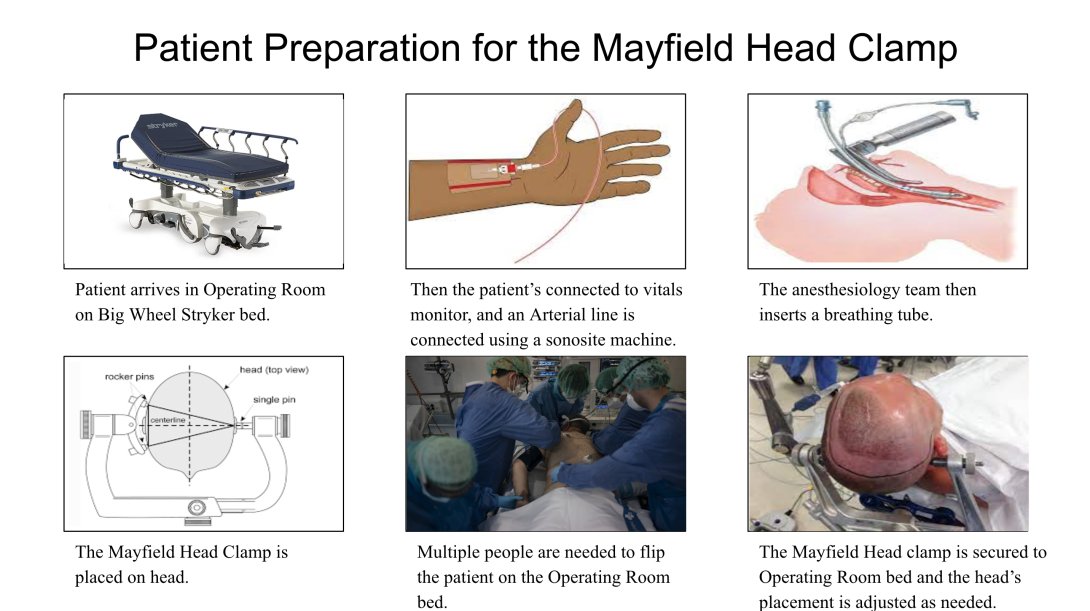
Then the last day of our shortened week was a day in the operating room. During this procedure the Mayfield Head Clamp was utilized in order to secure the patient’s head in a desirable position for their surgery. The Storyboard will be depicting a posterior cervical spinal fusion. As can be seen in the Storyboard there are multiple steps and pain points involved in preparing the patient before placing the head clamp, and then securing the head clamp on the surgical bed.
- The first step is for the patient to arrive in the operating room on the Stryker Big Wheel bed.
- Pain point: This could be complicated by the patient arriving late due to any number of reasons, which would of course delay the surgery’s start time.
- Then the next step is to monitor the patient’s vital signs by hooking them up to a vitals monitor and securing the A-line or the arterial line. In this step a sonosite ultrasound machine was utilized in order to secure the needle in the middle of the blood vessel.
- Pain point: This proved to be complex due to the difficulty in penetrating the vessel as well as securing the middle position, and this can be further complicated if a patient is a smoker.
- Then the next step was to insert the breathing tube by the Anesthesiology team.
- Pain point: This was done as an awake intubation, meaning the patient was conscious and had to endure their gag reflex being trigger as the tube was being inserted. When asked why an awake intubation was preformed, the answer was that this was done in order to ensure the positing of the patient is not compromised before surgery.
- Finally the Mayfield head clamp is placed on the patient’s head by a neurosurgeon.
- Pain point: This needs to be perfectly aligned in order to avoid injuries, and may also require to be placed multiple times. The lead surgeon verifies that it is placed ideally before continuing in patient prep.
- Then once everything is in place multiple surgeons and OR staff are needed to flip the patient from the Stryker bed to the operating table.
- Pain point: This requires more or less staff depending on the size of the patient. Also during this flipping process someone must keep their hand on the Mayfield head clamp in order to avoid it moving or tilting the patient’s head.
- Then finally the clamp is secured to the operating bed in the optimal position for the given surgery, which involves adjusting the bed to accommodate the positioning for the surgery and the clamp itself.
- Pain point: This requires two or more people while one surgeon is holding the head of the patient with the head clamp, the other is securing the clamp to the arm on the operating table.
Through further research on the Mayfield Head Clamp I found a review article, “The Mayfield Skull Clamp: A Literature Review of Its Complications and Technical Nuances for Application.” This article details all the complications that arise from the use of these head clamps, for example some of the discussed complications included skull fractures and epidural hematomas. The article discussed how there are many patient facts that are involved in these complications such as the patient’s age, skull thickness, and weak points in their cranium. Children have thinner skulls and due to the force form the Mayfield clamp this leads to skull fractures, and this also holds true for people with thinner skulls making them more susceptible to injuries from this medical device. However despite this the article concludes that the Mayfield clamp is a very popular skull stabilization device, and there seem to be very few complications that are lethal that arise from these devices. Also it is imperative that the device is properly handled in order to avoid injuries to their patients; however, the same could be said about all medical equipment.
Citations:
Dieter, T., & Menovsky, T. (2021). The Mayfield Skull Clamp: A Literature Review of Its Complications and Technical Nuances for Application. Shibboleth authentication request. World Neurosurgery, Volume 151, 2021, Pages 102-109, ISSN 1878-8750. Retrieved July 10, 2022, from https://doi-org.proxy.cc.uic.edu/10.1016/j.wneu.2021.04.081
Endotracheal tube or breathing tube. Intensive Care Hotline. (2020, May 6). Retrieved July 10, 2022, from https://intensivecarehotline.com/breathing-tube-or-endotracheal-tube/
Google. (n.d.). Google image result for https://upload.wikimedia.org/wikipedia/commons/thumb/b/bb/arterial-line-shaded.png/1200px-arterial-line-shaded.png. Retrieved July 10, 2022, from https://www.google.com/imgres?imgurl=https%3A%2F%2Fupload.wikimedia.org%2Fwikipedia%2Fcommons%2Fthumb%2Fb%2Fbb%2FArterial-line-shaded.png%2F1200px-Arterial-line-shaded.png&imgrefurl=https%3A%2F%2Fen.wikipedia.org%2Fwiki%2FArterial_line&tbnid=MG5A1r5M_c0yOM&vet=12ahUKEwi3kqO69-74AhUIRc0KHY-0AXoQMygBegUIARDHAQ..i&docid=GbkX_wzPENATWM&w=1200&h=900&q=arterial+line+in+hand&ved=2ahUKEwi3kqO69-74AhUIRc0KHY-0AXoQMygBegUIARDHAQ
Prime series. Stryker. (n.d.). Retrieved July 10, 2022, from https://www.stryker.com/us/en/acute-care/products/prime-series.html
Sales, J. (n.d.). Mayfield Skull Clamp. mayfield_skull_clamp [Operative Neurosurgery]. Retrieved July 10, 2022, from https://operativeneurosurgery.com/doku.php?id=mayfield_skull_clamp
Skull clamp placement | The Neurosurgical Atlas. (n.d.). Retrieved July 11, 2022, from https://www.neurosurgicalatlas.com/volumes/principles-of-cranial-surgery/skull-clamp-placement
Stobbe, M. (2020, April 8). Some doctors moving away from ventilators for virus patients. AP NEWS. Retrieved July 10, 2022, from https://apnews.com/8ccd325c2be9bf454c2128dcb7bd616d
Week 3: Neuro's Needs
The goal for this week was to create a need statement through first and secondary research. However in Neurosurgery since at first glance everything appears to be a well defined system that is fine tuned to perform a well choreographed routine, this makes it difficult to find areas of improvement. Luckily in the third week we had the opportunity to observe more surgeries including spinal fusions of cervical and lumbar vertebrae. This was an interesting opportunity since we previously had only seen cervical fusions.
In the cervical fusions we had observed the head of the patient was stabilized utilizing a Mayfield head clamp, this however was not the case during the lumbar fusion. The reason why Mayfield head clamp is utilized in cervical opposed to lumbar, upon asking the Operating Room Staff, is due to the distance from the incision. The cervical vertebrae are much closer to the skull than the lumbar vertebrae. So the stabilization and movement restriction of the skull is instrumental in a successful surgery. While the Mayfield head clamp does in fact inhibit movement of the patient it also includes possible complications such as hematomas and skull fractures, and they pose a higher risk for people with thinner skulls. [1] Which is where I chose to formulate my needs statement for this week. The first iteration can be seen directly below which was:
- 1. Patients undergoing spinal fusion surgery require better stabilization of the skull to reduce the possibility of patient injury.
The population being patients who are undergoing spinal fusion surgery. The opportunity is to better stabilize the skull, and then the outcome is to reduce the possibility of patient injury. This was the first version of my needs statement which I chose to adjust to from spinal fusion surgery to specifically spinal fusion of the cervical vertebrae. This was made because of the closer proximity to the skull. Not to mention thoracic and lumbar vertebrae have different requirements and the stability of the skull. By limiting the population to cervical vertebrae being fused this allows for the focus to be on to the close proximity to the skull. Currently one of the common medical devices to hold the skull in place is the Mayfield head clamp which presents a number of issues including Skull fractures, and which were being reported from 1997 to 2018. [1]
- 2. Surgeons performing spinal fusion of the cervical vertebrae require better stabilization of the skull to reduce the possibility of patient injury or movement during surgery.
In the second version of my needs statement I changed the population from the patients requiring the surgery to the surgeons performing the surgery. I did this because the one utilizing the device would be the surgeons placing the head clamp. However the current design is very convenient for surgeons, since it does well to constrict patient movements while keeping the skull stabilized. [1] The real target population is patients due to the number of complications that may arise from the tension from the clamp. A new design would mainly impact the patients opposed to the surgeons which is why I adjusted the population back. I also added the movement during surgery to the outcome portion of the needs statement; this is due to secondary research that I conducted and found that there are reports of the Mayfield head clamp breaking or slipping off in the middle of the surgery. [2-3]
- 3. Patients undergoing spinal fusion of the cervical vertebrae require better stabilization of the skull to reduce the possibility of patient injury or movement during surgery.
This final statement includes the specification of the cervical vertebrae, and both outcomes to reduce the possibility of patient injury and movement during surgery. This encompassed both what a surgeon and patient’s needs from this device, despite it being mainly geared toward the patient in order to reduce harm and increase comfort. These need statements are still open for improvement and will continue to be adjusted based on the direction my team and I decide to explore more in depth.
Citations:
[1] Dieter, T., & Menovsky, T. (2021). The Mayfield Skull Clamp: A Literature Review of Its Complications and Technical Nuances for Application. Shibboleth authentication request. World Neurosurgery, Volume 151, 2021, Pages 102-109, ISSN 1878-8750. Retrieved July 10, 2022, from https://doi-org.proxy.cc.uic.edu/10.1016/j.wneu.2021.04.081
[2] Lee, T. H., Kim, S. J., & Cho, D. S. (2009). Broken mayfield head clamp. Journal of Korean Neurosurgical Society, 45(5), 306. https://doi.org/10.3340/jkns.2009.45.5.306
[3] Sakakura K, Fujimoto A, Ichikawa N, Ishikawa E, Matsumura A, Enoki H, Okanishi T. Estimation of Risk Factors for Head Slippage Using a Head Clamp System. A Retrospective Study. Ther Clin Risk Manag. 2020;16:189-194 https://doi.org/10.2147/TCRM.S247402
Week 4: Better Headspace, Patents
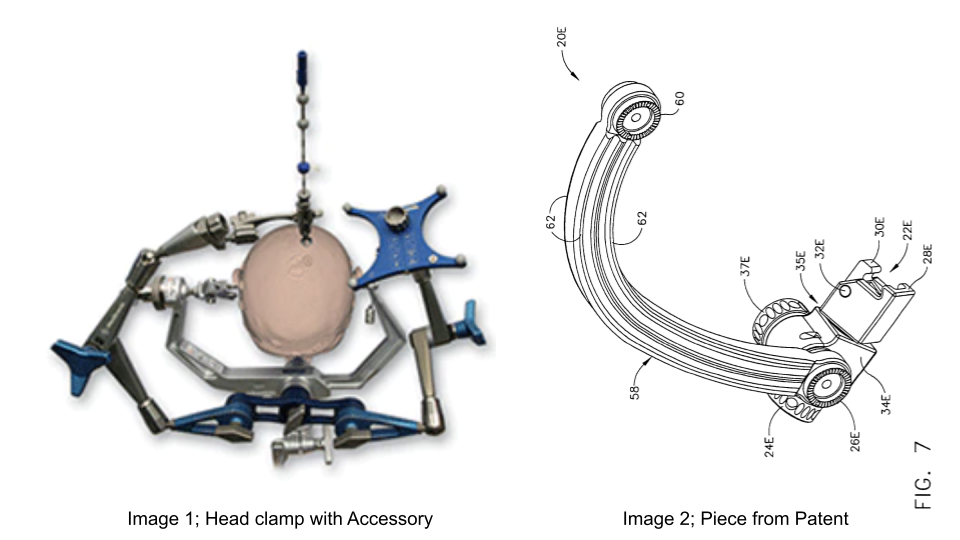
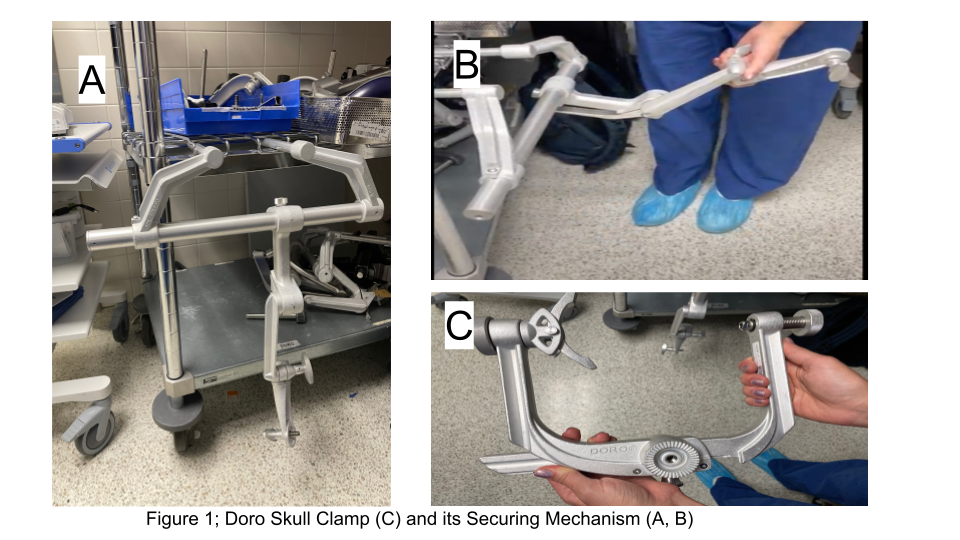
The more we visited the Operative Room, the more innovations that I hadn’t noticed before became apparent. This week we frequented the OR and had the opportunity to view more craniotomies, this included the use of a skull head clamp. The skull head clamp has been a point of interest to my group and myself, which led to me focusing on the placement and removal of the clamp. When the clamp was placed and secured to the bed I noticed that it was Doro head clamp from Black Forest Medical. This clamp’s securing mechanism to the bed had an additional piece that allowed for attachments. In one surgery involving the StealthStation, the additional piece was utilized in attaching to one of the StealthStations calibration pieces for targeting the intended area in the brain. This can be seen in Figure 1to the left where the component is attached. [1]
This was a much better alternative opposed to securing the attachment directly to the operating table which already had a lot of tubes and wires already on it. This was an interesting solution to one of the first things I noticed in the operating room, that there are so many attachments on the operating table and the patient, making it a hectic environment to an outsider. However when my group and I questioned this, we were told that it may appear like a lot, however with a good surgical team then the amount of wires and attachments is typically not an issue. Despite this being able to minimize the number of attachments to the bed, and having one less thing in the surgeon’s way is something to be desired which is why the attachment’s ability caught my eye this week.
Upon further investigation of this interesting fact, I found that Blank Forest Medical Company holds a patent, US7836532B2, regarding how tools are to be attached to their device. The patent is titled, “Method and apparatus for attaching accessories to a surgical fixture.” [2] This patent details how a skull clamp and a surgical fixture are utilized allowing additional attachments through the body portion of the fixture which allows for accessories. Similar to other patents the wording is specific yet vague. One claim that is in this patent is, “an accessory attachment portion moveably coupled with the intermediate portion, wherein the accessory attachment portion comprises a first feature configured to selectively fix the accessory attachment portion to the intermediate portion.” [2] Then through multiple sub claims they proceed to name multiple different ways the attachment assembly may be utilized or altered. The piece to which they are describing in this section can be seen in Figure 2 on the left. In The image to the left this is where an accessory can be attached to 26E and 37E.
This relates to my previous needs statement from the week which was “Patients undergoing spinal fusion of the cervical vertebrae require better stabilization of the skull to reduce the possibility of patient injury or movement during surgery.” However, since the previous week I decided to adjust it in two ways, the first being the population being changed from the patients to the surgeons performing the surgery. This was decided through discussion with my group and Dr. Browne, since it is the surgeons utilizing the device they should be the target population. The next change involves the outcome which was adjusted to “to reduce the possibility of patient injury or movement during surgery without decreasing the surgeon’s ability to navigate around the patient.” This stemmed from my observations and research this week.
The current needs statement reads as such, “Surgeons performing spinal fusion of the cervical vertebrae require better stabilization of the skull to reduce the possibility of patient injury or movement during surgery without decreasing the surgeon’s ability to navigate around the patient.” This of course will continue to be adjusted as the program moves forward.
Citations
[1] Medtronic. (n.d.). Stealthstation Surgical Navigation – Navigation. Medtronic. Retrieved July 24, 2022, from https://www.medtronic.com/us-en/healthcare-professionals/products/neurological/surgical-navigation-systems/stealthstation/cranial-neurosurgery-navigation.html
[2] Schüle , E. F. (2006, November 23). Method and apparatus for attaching accessories to a surgical fixture. https://patents.google.com/patent/US7836532B2/en?oq=US7836532B2
Week 5; Viability
Entering the last two weeks of this program, we’re now focusing on the viability of the needs we have previously addressed as a group. The previous need which is explained in my previous blog posts has been adjusted once again.The most current version being: Surgeons preparing for cranial and cervical spine procedures face challenges in positioning and stabilizing the head and require an ergonomic and secure way to reduce patient complications and increase ease of surgeon usability.
This was adjusted with my group as we have decided to move forward with the opportunity of better stabilization of the skull, but now includes the positioning of the head as well. Through interviews we have found that a major benefit to the current method of utilizing skull clamps is being able to have multiple positioning capabilities within the same device. Not to mention the other ideas my group and I were researching involved ergonomics in the operating room which we have adapted into this need statement with the outcoming now including “require an ergonomic and secure way to reduce patient complications and increase ease of surgeon usability.” The population remained the same, however through changing the outcome we are adjusting the focus of the kind of innovation which is required from this need statement. The intended solution should not only remain safe for the patients but also decrease the possibility of surgeon discomfort or difficulty which is currently seen through the utilization of the skull clamp.
In Figure 1, it can be seen that there are multiple pieces that require to be positioned and stabilized including the clamp and securing mechanism. This was a stress point that came up during our interviews this week and we have seen in previous surgeries, and while there are points to secure to accommodate multiple positions. This takes time and requires, from what we have seen, two surgeons to safely secure the skull clamp and securing mechanism together.
Now that we had a need established we moved on to researching the market, about this product. We found that the specific market segment for the utilization of a skull clamp or any method to stabilize the head during a cranial and cervical spine surgery to be 240 thousand patients annually. This number was obtained through research on https://datatools.ahrq.gov/hcupnet-dua, these numbers include craniotomies and cervical spine fusion surgery from 2000 to 2007. We used the data from 2007, to complete this because this was the most recent year in that data set. Then through the assumption that every use of the skull clamp costs the hospital approximately 50$ per use, this assumption was made through UIHealth’s MyChart website to assess costs for a cervical fusion surgery. Then through these two were able to conclude that the Total Addressable Market (TAM) is approximately 12 Million dollars. This number may be underestimated due to multiple factors such as we were only able to access data up until 2007, not to mention the 50$ per use is an estimation since it is difficult to pinpoint direct costs in surgical expenses. However this remains a valuable space for innovation due to the multiple benefits that could be obtained from the patient, physician, and hospital aspects. An innovative solution can decrease the possibility of patient injury, simplify the process for physicians, and may even decrease the total time in the operating room. My team and I will continue to research and adjust our need statement as we head into the final week of the program!
Week 6; And That's a Wrap!

You never realize how fast time passes until you’re at the finish line. This was truly a once in a lifetime experience. Never again will I be approaching my final year in pursuit of my Biomedical Engineering degree, using my own primary research to identify needs in the Neurosurgical department.
This was such an amazing experience being able to observe in the operating room. As an engineering student my view of medical devices was limited to the creation of the device, but now I see that you really cannot build a device without observing and consulting the target population. Which is where CIP comes in not only allowing for first hand experience in identifying needs in a clinical setting, but also allowing us the opportunity to discuss and interview our clinical mentors in regards to our observations.
This past week we presented our final presentation which was “Reimaging Surgical Head Clamps in the OR” which discusses everything this blog has previously published with some minor changes of course. For example our Total Addressable Market Value changed from the previous week’s calculations because we hadn’t incorporated the cost of the three disposable pins per patient utilizing the clamp, not to mention the indirect cost of Anesthesia or Operating Room cost that increase if there is a delay in the surgery. This all caused a major increase in our TAM. Overall it was a successful presentation and collaboration between both medical and engineering students and our clinical mentor, Dr. Mehta.
Advice to Future CIP Scholars:
- Don’t limit yourself to one thing! While my blog may appear to have a straight shot of Surgical Head Clamps, my group and I noticed and studied many different aspects of neurosurgical instrumentation that we observed during clinic. If you focus too closely on one aspect you might miss other really interesting opportunities to research and study!
- I would also caution against the Bob the Builder, “can we fix it?” mindset. Remember you’re there to identify the need not creating the solution. Which was difficult, of course, being an engineering student and not following the million quick fixes. However if you think this way you may miss a different innovate approach to what you’re observing.
- Also don’t be afraid to ask questions, most people in the OR or department you’re in are more than willing to answer your questions. That being said, make sure you’re also prepared so you can ask more than “so what is this?” questions. A tip is we would ask our mentor what kind of surgeries he had planned for the week then we would research the surgeries. In doing this we would know what the surgery was medically, so then we could focus more on the process and devices being utilized within that surgery.
Acknowledgements:
Now for some acknowledgements! Thank you to Drs. Browne, Felder, and Kotche, for facilitating this program and offering weekly guidance and assistance in order to aid in our successful completion of the program. Thank you to the UI Health Neurosurgery Department, specifically our mentor, Dr. Ankit Mehta for his time, guidance, and welcoming us into his OR. Also to all the resident doctors, OR nurses, and the UI Health Neurosurgical ICU (NSICU) staff all for allowing us to shadow and interview during this program. Also the final thank you to my team, Dionna Bidny, Vivian Nguyen, and Sam Winters, for creating a welcoming and collaborative environment that made this program so much more enjoyable! Goodluck to all future CIP students!
About
Year: Senior in standing in Biomedical Engineering with a Neural concentration
Department of Study: Neurosurgery
Contact Information: Nqatan2@uic.edu