
Sonakshi Raju
Medical Student
Pronouns: She/ Her/ Hers
Email:
Week 1: Observations in Urology Heading link
This week was our team’s first week shadowing in the urology department. During this time we observed patient care in a variety of settings including inpatient surgery, outpatient surgery, and in-office procedures. Along with this wide range of procedures, we saw many different workflows and tools being used. It was particularly interesting to observe the process of setting up a surgical OR prior to the patient entering the room. All the supplies are carefully tracked and arranged with a specific purpose.
Below are examples of good and bad design that I observed this week:
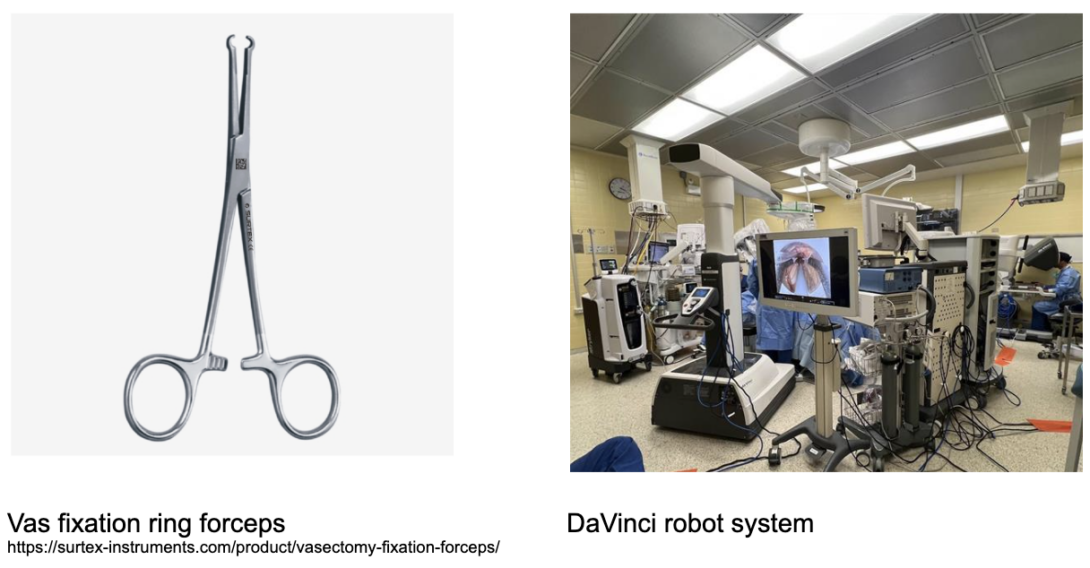
Good design: Vas fixation ring forceps
Activities: Vas fixation ring forceps are used during a vasectomy procedure.
Environment: I observed this procedure being done in the outpatient clinic.
Interactions: The major interaction between the user and the forceps is when the user grasps and clamps them around the vas deferens. A key step in the procedure is locating and then isolating a portion of each vas deferens using these forceps.
Objects: The vas fixation ring forceps are used during the vasectomy procedure, along with other types of forceps, scissors, a cautery, a syringe of local anesthetic, and suturing materials.
Users: The tool is used by the resident and attending who were performing the procedure together.
The vas fixation ring forceps are a tool specifically designed to allow the user to grasp and pull the vas deferens upwards without crushing its tubular structure. I thought the ring-like tip was very well designed because it completely encircled the vas deferens and was the correct diameter to do so without compressing the tube. The forceps appear to be equally usable with both the left and right hand. The simplicity of the tool contributes to why I think this is a good design. A vasectomy is a fairly quick procedure that is done with local anesthetic while the patient is awake, so tools that are low profile and get the job done quickly have great value here.
Bad design: Wheels on the robotic arm component of the single-port DaVinci robot
Activities: We observed a DaVinci robot being used for single-port robotic surgery.
Environment: We observed this device being used in the inpatient OR, but it can be used in an outpatient OR setting as well.
Interactions: A surgeon (attending or resident) interacts with the console, which stays in place, a resident interacts with the robotic arm by changing out the instruments that are attached to it, a tech places a sterile sleeve around the robotic arm, and a nurse physically positions the robotic arm prior to surgery starting.
Objects: The entire DaVinci system has three physically separate components- a robotic arm, a console from where the surgeon controls the device, and a monitor. The robotic arm has 3 instruments, which can be changed out, and an endoscope.
Users: The person responsible for positioning the robotic arm above the patient’s bed was a nurse.
The robotic arm has to be positioned above the patient after they are on the surgical table, making it the last instrument moved into place before the surgery starts. I noticed that the process of moving the robotic arm from the side of the room to above the patient took a lot of maneuvering. The wheels on the device only allow the device to move forward and back, so this, along with the device’s large size, large arm with a sterile cover on it, and lack of space in the OR, made it so that the robot had to be pushed back and forth with small movements many times to allow it to turn and reach its final position. This process was time consuming.
Week 2: Storyboarding a Urologic Procedure Heading link
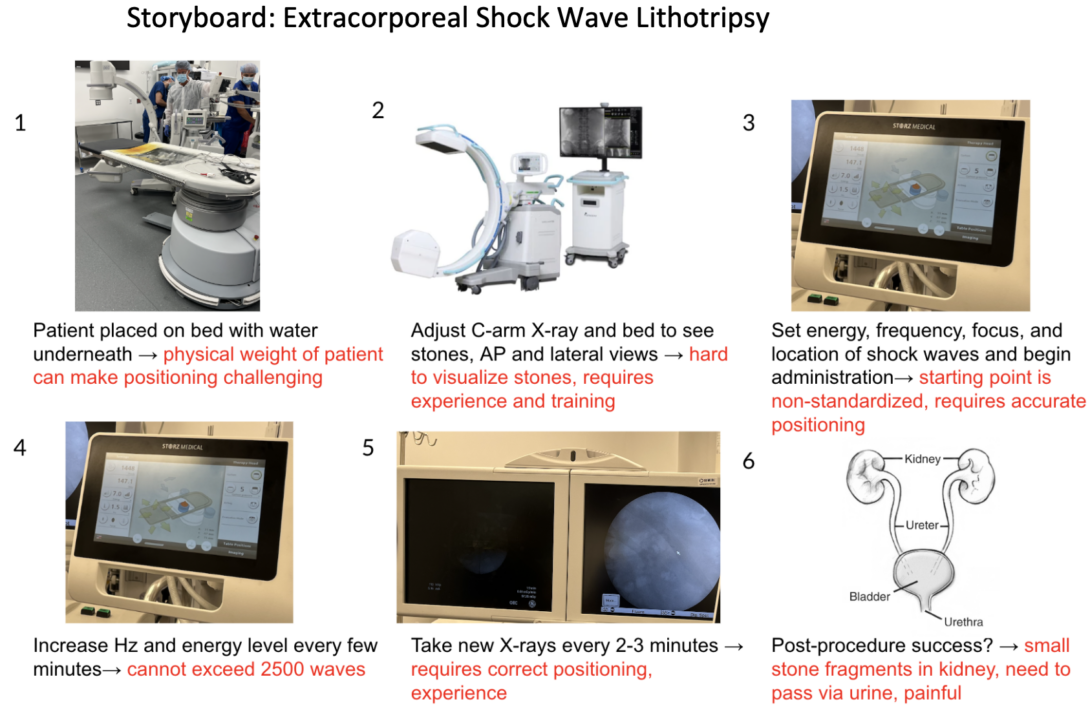
My storyboard is on the extracorporeal shock wave lithotripsy (ESWL) procedure, an outpatient surgical procedure that we observed this week. The purpose of the procedure is to break up kidney stones via high energy shock waves. The shockwaves break the stones down into small pieces that can be safely passed in the urine. The pain points with each step in this procedure are in red text in the above image.
I found a review paper that compared the outcomes of ESWL to outcomes with ureteroscopic lithotripsy (URSL) in the treatment of ureteral stones. The authors analyzed ten studies which included 1509 patients in total and looked at various outcome markers for each treatment method including failure rate, stone clearance, and complications. Their analysis found that overall, a stone-free outcome was more common with URSL. They also found that the perforation rate was higher with URSL as compared to ESWL.
Sokouti M, Sokouti M, Sokouti B. A systematic review and meta-analysis on the outcomes of extracorporeal shock wave compared to ureteroscopic lithotripsy for the treatment of ureteral stones. J Taibah Univ Med Sci. 2023;18(6):1459-1471. Published 2023 Jun 14. doi:10.1016/j.jtumed.2023.06.001
Storyboard image citations:
2- https://store.mavenimaging.com/products/c-arm-x-ray-system-genoray-oscar-15
Week 3: Crafting a Needs Statement Heading link
This week we observed more urologic procedures in both the operating room and the clinic. We were tasked to develop a needs statement based on our observations and research, and my needs statements center around the problem of exposure to surgical smoke in the operating room.
Iteration #1:
Medical professionals in a urologic operating room where cautery tools are being used need a decrease in exposure to surgical smoke.
Population: medical professionals in a urologic operating room
Opportunity: cautery tools are being used
Outcome: decreased exposure to surgical smoke
I identified this need based on operations that we observed, where cautery and laser tools were used, both of which generate a lot of surgical smoke. Upon review of the literature I found that surgical smoke is not only harmful and contains carcinogens, but that current smoke evacuation devices leave a lot of smoke behind in the room, with one study finding that use of wall suction causes only a 48-65% decrease in fine particle inhalation (Wang et al., 2015).
Iteration #2:
A solution to decrease inhalation of surgical smoke among medical professionals in a urologic operating room is needed when cautery tools are being used in surgery.
Population: medical professionals in a urologic operating room
Opportunity: cautery tools are being used in surgery
Outcome: decreased inhalation of surgical smoke
I altered the outcome of my needs statement to focus more on the need for a solution to specifically decrease inhalation of surgical smoke as opposed to decreasing exposure to it. I chose to use the term inhalation because based on my literature review, the negative impact from surgical smoke comes specifically from inhalation rather than exposure alone.
Iteration #3:
A solution to decrease inhalation of surgical smoke among medical professionals in operating rooms is needed when electrosurgical tools are being used in surgery.
Population: medical professionals in operating rooms
Opportunity: electrosurgical tools are being used in surgery
Outcome: decreased inhalation of surgical smoke
In my final iteration of my needs statement I widened my population to medical professionals in operating rooms instead of the more limited population of those in urologic operating rooms, because surgical smoke is an issue not limited to urology only. I also widened my opportunity from cautery tools to electrosurgical tools because cautery tools are not the only devices that create surgical smoke, devices like lasers do as well and this term more appropriately describes this.
Wang, HK., Mo, F., Ma, CG. et al. Evaluation of fine particles in surgical smoke from an urologist’s operating room by time and by distance. Int Urol Nephrol 47, 1671–1678 (2015). https://doi.org/10.1007/s11255-015-1080-3
Week 4: Assessing Existing Patents Heading link
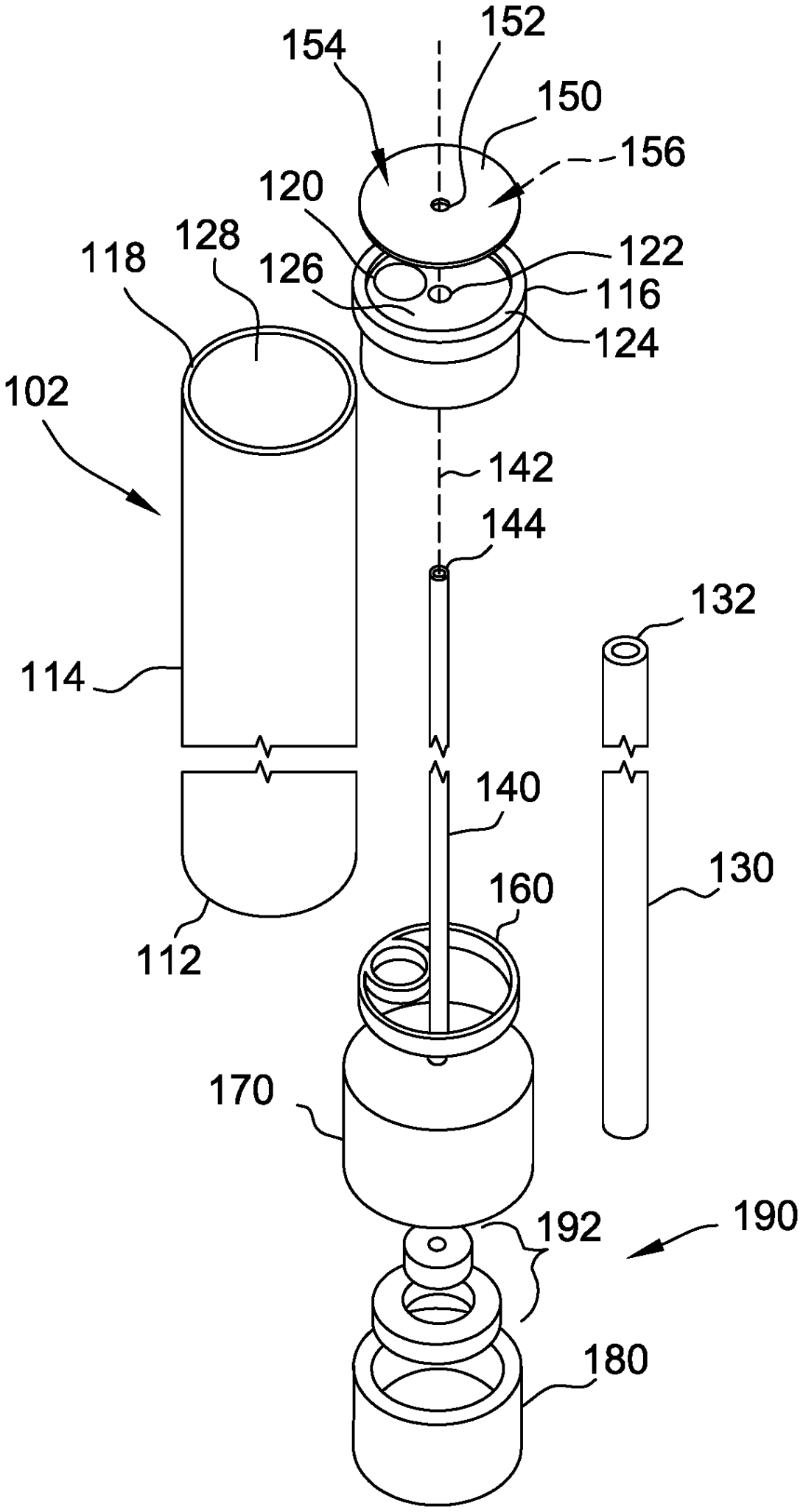
This week we started exploring patents that may address the needs statements that we have been developing. I developed a needs statement regarding endoscopes and found a relevant patent.
Needs Statement: A solution to reduce the time spent cleaning the endoscope mid-surgery is needed among medical staff assisting in single-port DaVinci surgery.
Patent: I searched for patents that may address this needs statement and found patent US10709321B2 entitled “Self-cleaning endoscope” that was filed in 2017 by Washington University in St Louis WUSTL. The claims describe various components of the endoscope that enable the device to be “self-cleaning”. They describe an endoscope with a lens protector that can be rotated by a motor. This motor is controlled by a button on the handle of the device. They also describe a fluid source that can expel fluid onto the lens protector. There is also a cleaning ribbon that can be pulled along the lens protector.
Assessment of ability of solution to meet need: It seems like this solution could meet our need, reducing the time spent cleaning an endoscope mid-surgery, by eliminating the step where the endoscope currently needs to be completely removed from the incision site to be cleaned. It appears that this solution would be quicker than this current process, however time will still be spent when the surgery is stopped in order for the endoscope to be cleaned. It is unclear how many cycles of cleaning this endoscope can effectively go through on its own before complete removal and cleaning may be necessary. It can only meet our need if its technology is integratable with the single-port DaVinci system, which is what our need is focused on specifically.
Leuthardt, E. C., Genin, G., Yarbrough, C., Somers, T., & Margolis, D. (2020, July 14). Self-cleaning endoscope.
Week 5: Calculating the Total Addressable Market Heading link
One of the needs statements we have been working on centers around improving efficiency and increasing patient comfort during the prostate biopsy procedure. I then worked on building out a Total Addressable Market (TAM) for this problem. Needs statement: A solution to improve ease of patient positioning during a prostate biopsy is needed among medical professionals performing and assisting in a prostate biopsy procedure in order to improve the efficiency of the procedure and increase patient comfort.
Based on my research, I found that around 1 million prostate biopsies are performed each year in the US [1]. There are various instruments that go into the prostate biopsy procedure, including a single-use prostate biopsy needle, reusable ultrasound probe, and a reusable procedure chair. The total cost of a prostate biopsy procedure at Cook County Health is $4,813. To calculate the TAM I used the formula TAM = # of units/year * cost of product = 1,000,000 * 4,813= 4.8 billion which encompasses the entire prostate biopsy space. The cost of a single procedure chair is around $14,000, however this is a reusable product so it would be more appropriate to look at the cost per use for the chair to get a better estimate at its TAM. The cost of a single-use prostate biopsy needle is around $200. Using this number the TAM for prostate biopsy needles is 1,000,000 * 200 = 200 million. Thus, if this needs statement was being addressed from the direction of the biopsy needle, the TAM for this solution is 200 million.
- Schmeusser, Benjamin et al. “Hundred years of transperineal prostate biopsy.” Therapeutic advances in urology vol. 14 17562872221100590. 21 May. 2022, doi:10.1177/17562872221100590
Week 6: Reflecting on CIP Heading link
After 6 weeks of participating in the CIP, I learned a lot. One of the biggest things I learned was how the OR is run. After observing numerous procedures and interacting with the various surgeons, nurses, and trainees in the room, I think I will feel much more confident in the OR during my clinical rotations.
My advice to future CIP participants would be to always introduce yourself to the doctors and nurses you may encounter in both the OR and clinic setting, and try asking other doctors within your department if you can shadow them if there’s ever downtime when your clinic mentor/ assigned doctor doesn’t have procedure for you to watch. I would also encourage you to interview the medical professionals you’re shadowing to understand their perspectives and experiences as you work to narrow down your needs statements.