
Quetzalli Rodriguez
2023 students
Biomedical Engineering
Pronouns: She/Her/Hers
Email:
Week 1 - Pediatric Surgery: Good and Bad Designs in the OR
Summary of the week:
Our first week following the pediatric surgery team was both exciting and eye-opening. As there were only a handful of surgical pediatric cases, our team was given the opportunity to observe procedures outside of the pediatric field.
Our first day started early in the operating room (OR) with a pediatric patient undergoing a Superficial Parotidectomy. Here a premalignant portion of the parotid gland was removed to prevent further malignant development. Only what was necessary of the parotid gland was removed so as not to disturb the nearby facial nerve. Later that day, we observed a gastric bypass with robot assisted laparoscopy using the Da Vinci surgical system. During the preparation of this procedure, we were introduced to the Sequential Compression Device (SCD) that worked to prevent blood clot formation by squeezing the legs of the patient and promoting blood flow. During the gastric bypass, the attending surgeon cautioned against the danger of mixing up the different needles that were laparoscopically transported into the abdominal cavity. They advised removing needles that have already been used to prevent confusion.
Among the other pediatric procedures we were able to shadow during the week was a probing lacrimal canaliculus due to a nasolacrimal duct obstruction. The procedure went smoothly and I admired how well the surgeon wired the stent from the lacrimal canaliculus to the nasolacrimal duct or the tear duct. During a procedure addressing Hypohidrotic Ectodermal Dysplasia syndrome, we observed that the layout of the OR could have been improved especially considering how the anesthesiologist did not have a constant visual of the patient between facing the monitors and then the patient. Finally, we shadowed the pediatric surgeons as they performed a repair of an umbilical hernia. The overall procedure went well, but it did seem to take longer for the child to warm up upon waking in comparison to other patients we had seen.
Good design:
When observing the probing lacrimal canaliculus due to a nasolacrimal duct obstruction, we observed how well the surgeon applied the stent used to connect the lacrimal canaliculus to the nasolacrimal duct.
Activity: Inserting a stent into the lacrimal canaliculus to repair the nasolacrimal duct obstruction
Environment: Operating room that was fairly free of clutter. The operating table still had to be rotated after intubation so the surgeon could have access to the patient’s eye without interfering with the monitors used by the anesthesiologists.
Interactions: Surgeon was using forceps with finer tips to maneuver the pediatric patient’s eyelids and locate the lacrimal canaliculus. Later he used a stent to guide the silicon tubing into the patient’s lacrimal canaliculus and through to the nasal passageway.
Objects: The stent used by the surgeon allowed smooth installment of the silicon tube by establishing a path for the tube to follow through without resistance.
Users: The surgeon worked on the patient and directly applied the stent while the scrub nurse assisted in the surgery.
Bad design:
Dermabond
- Sealant used to cover skin incisions after sutures were applied
- Multiple medical personnel struggled when applying it
- One resident stated he had been stabbed by a piece of glass when attempting to extract the sealant from the Dermabond container
Activity: Closing the incision made to establish laparoscopic ports nearing the end of the gastric bypass surgery.
Environment: Operating room that contained the Da Vinci surgical system
Interactions: Surgeon was applying the skin adhesive to the patient’s incision after having applied sutures.
Objects: In order to apply Dermabond, the glass ampule must be crushed to allow the adhesive to begin polymerization and form a smooth layer. However, excessive crushing of the Dermabond container may lead to inadvertent skin punctures.
Users: Surgeon, residents in training, medical students, and anyone who was assisting with closing the incisions.
Week 2 - Pediatric Surgery: Surgical Process Involving a Neonatal Patient Storyboard
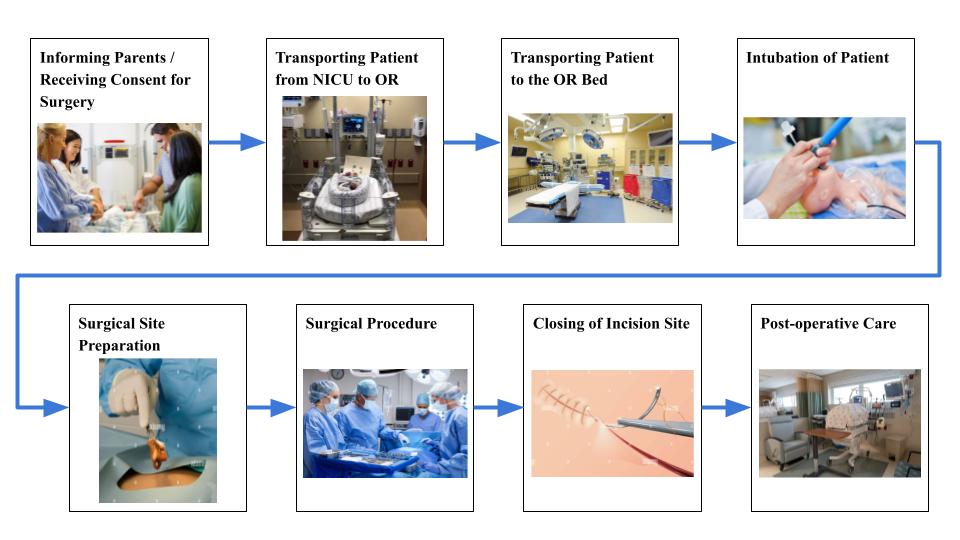
Informing Parents / Receiving Consent for Surgery
- Receiving consent for the surgical procedure may take varying amounts of time as parents require time to both understand the procedure itself and its necessity for the health of their child.
- Parental anxiety throughout the duration of the surgery including pre- and post-operative care.
- The attending performing the surgery did ask the circulating nurse to regularly update the mother regarding the progress of the surgery. He also immediately called the parents upon completing the surgery to answer any questions and provide reassurance.
- Citation for image:
MountainView Hospital Opens Level III NICU. (n.d.). MountainView Hospital. https://mountainview-hospital.com/about/newsroom/mountainview-hospital-opens-level-iii-nicu
Transporting Patient from NICU to OR
- The patient may experience some discomfort if jolted during the journey through hospital hallways and an elevator ride.
- The patient was also not transported in an incubator.
Since the bed/crib used to transport the baby wasn’t enclosed, the patient may have increased exposure to airborne pathogens. - Citation for image:
Neonatal Intensive Care Unit (NICU) | Kaiser Permanente Family Birth Center. (n.d.). Kpfamilybirthcenter.org. https://kpfamilybirthcenter.org/nicu
Transporting Patient to the OR Bed
- Transportation from the crib to the operating bed took 2-3 people due to attached wires with 1 person actually carrying the baby.
The additional personnel assisted in navigating around the IV stand that accompanied the patient from the NICU. - The operating bed is a standard size and not specifically made for neonatal patients.
There appeared to be no specific way to keep the patient stable on the bed.
A few medical personnel would stay on either side of the bed to eliminate the risk of the patient rolling to the edges. - Citation for image:
Improving operating room cleaning efficiency. (n.d.). Www.hfmmagazine.com. https://www.hfmmagazine.com/articles/2090-improving-operating-room-cleaning-efficiency
Intubation of Patient
- There was some delay in the intubation as the baby kept resisting and twisting their head to avoid the oxygen mask.
- The patient’s hands had to be held to avoid further disruption of the intubation process.
- Citation for image:
In the NICU, High-Flow Oxygen Boosts Intubation Success on First Attempt. (2022, April 27). Www.medpagetoday.com. https://www.medpagetoday.com/criticalcare/intensivists/98435
Surgical Site Preparation
- Catheter was placed due to a longer surgical procedure.
- Surgical site was prepared with betadine solution.
While betadine was drying, the sterile site got contaminated when medical personnel were checking on the intubation tube.
Sterile drapes surrounding the sterile site were accidentally flipped onto the drying betadine.
Due to the size of the patient, there was less distance between the intubation tube and the sterilized site. - Betadine prep had to be redone and sterile towels were tapped down to avoid accidental contamination.
- Citation for image:
Limited, A. (n.d.). Preparing skin with betadine solution an antiseptic during surgery Stock Photo – Alamy. Www.alamy.com. https://www.alamy.com/preparing-skin-with-betadine-solution-an-antseptic-during-surgery-image3788798.html
Surgical Procedure
- The surgery itself lasted approximately three hours.
- Since the surgeons were operating on a neonatal patient, the surgical site was small.
Surgeons and assisting medical students were slightly cramped throughout the procedure. - Citation for image:
Medicine – Surgery. (n.d.). Encyclopedia Britannica. https://www.britannica.com/science/medicine/Surgery
Closing of Incision Site
- Drain was placed at the incision site to prevent fluid buildup and infection.
- Incision site was covered with gauze and secured with paper tape.
Rather than using regular cloth tape, the attending specifically requested paper tape be used as paper tape is better suited for delicate skin and avoids harsh pulling of the skin during removal.
There was a delay in retrieving the paper tape as it was not stored in the same OR. - Citation for image:
Limited, A. (n.d.). vector illustration of sewing up the wound with surgical needle Stock Vector Image & Art – Alamy. Www.alamy.com. https://www.alamy.com/vector-illustration-of-sewing-up-the-wound-with-surgical-needle-image229346712.html
Post-operative Care
- Patient was placed in a more private section of the NICU for recovery. Receives constant monitoring and care from nurses.
- Concern for infection at the drainage site.
- Patient is exposed to constant noise (beeping from monitors, other babies crying) in the NICU recovery.
May result in poor sleep and general well-being disturbance. - Parents can only provide limited physical affection and cannot cradle their baby due to attached wires, monitors, and fear of disrupting the healing incision site.
- Citation for image:
Austin American-Statesman: Austin, TX News, Politics & Sports. (n.d.). Austin American-Statesman. https://www.statesman.com/?return=https%3A%2F%2Fwww.statesman.com%2Fstory%2Fnews%2Fhealthcare%2F2023%2F07%2F10%2Fst-davids-north-austin-expands-nicu-at-womens-center-at-parmer-lane%2F70392716007%2F
Related peer-reviewed papers:
Santapuram, P., Stone, A. L., Walden, R. L., & Alexander, L. (2021). Interventions for Parental Anxiety in Preparation for Pediatric Surgery: A Narrative Review. Children (Basel, Switzerland), 8(11), 1069. https://doi.org/10.3390/children8111069
The prospect of surgery has been shown to heighten levels of anxiety experienced by both parents and pediatric patients. Moreover, parental anxiety has negative effects on the child facing surgical interventions, especially their emotional response during the preoperative stage, postoperative pain, and behavioral patterns after hospital discharge. This review article covers multiple methods of reducing parental anxiety, including preoperative education and music therapy, which in turn benefits the family as a whole.
Week 3 - Needs Statement
This week, my team had the opportunity to shadow more neonatal surgery cases. We noticed how the surgical draping of the neonatal patients has some room for improvement and this needs statement goes more into detail about this observation.
Iteration 1:
Neonatal patients undergoing surgery experience lower body temperatures due to fluid leakage through the surgical draping and need a way to improve postoperative recovery time.
- Population: Neonatal patients undergoing surgery
- Opportunity: lower body temperatures due to fluid leakage through the surgical draping
- Outcome: improve postoperative recovery time
Discussion:
The population encompasses neonatal patients who are premature by varying amounts of time and typically arrive at the OR from the NICU. The time that neonatal patients spend in surgery naturally depends on the surgical procedure. The cases our team observed lasted about three to four hours. In regard to the opportunity, our team noticed how fluids used during preparation (betadine) and during the procedure (saline) spread from the incision site and around the patient’s abdomen or soaked through the sterile towels covering the patient. The patient’s body temperature, which is already poorly regulated, lowers when it comes in contact with these cold fluids. Finally, the desired outcome is to improve the postoperative recovery time which takes longer when the patient’s body temperature is not at a stable and healthy number.
Dixon, K. , Carter, B. , Harriman, T. , Doles, B. , Sitton, B. & Thompson, J. (2021). Neonatal Thermoregulation. Advances in Neonatal Care, 21 (4), 280-288. doi: 10.1097/ANC.0000000000000799.
Iteration 2:
Young pediatric patients undergoing surgery experience lower body temperatures due to fluid leakage through the surgical draping and need a way to improve postoperative recovery time.
- Population: young pediatric patients undergoing surgery
- Opportunity: lower body temperatures due to fluid leakage through the surgical draping
- Outcome: improve postoperative recovery time
Discussion:
For the second iteration, the population has been altered to include younger pediatric patients. This change was done to include the other pediatric cases our team observed in which patients struggled with temperature changes upon being awakened during the postoperative period. In these cases, the medical team used warm blankets to help the patient bring up their temperature. Studies have also shown that children are also at a risk of mild hypothermia due to their smaller size.
Singer D. (2021). Pediatric Hypothermia: An Ambiguous Issue. International journal of environmental research and public health, 18(21), 11484. https://doi.org/10.3390/ijerph182111484
Iteration 3:
Young pediatric patients undergoing surgery experience lower body temperatures due to fluid leakage through the surgical draping and need a way to maintain a comfortable body temperature during surgery.
- Population: young pediatric patients undergoing surgery
- Opportunity: lower body temperatures due to fluid leakage through the surgical draping
- Outcome: a way to maintain a comfortable body temperature during surgery.
Discussion:
The outcome was altered to focus more on the root of the problem: lower body temperature may lead to mild hypothermia during surgery. This lower body temperature is what leads to a longer recovery time as the medical team works longer to improve the patient’s condition. This change also specifies the desired outcome because recovery time may be influenced by other factors outside of the patient’s body temperature.
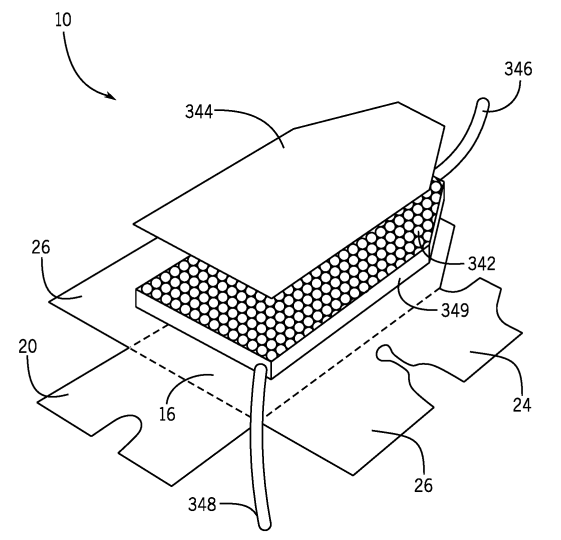
Week 4: Exploring Patents
Needs Statement:
Young pediatric patients undergoing surgery experience lower body temperatures due to fluid leakage through the surgical draping and need a way to maintain a pro-clotting body temperature during surgery.
Patent #: US-11432897-B2
The patent displayed in the image is a neonatal drape device that is formed with a heat-retaining material and is designed to wrap around a neonatal patient in a supine position. Of the numerous claims presented with this patent, only those with high relevance to the previously stated needs statement will be discussed. The drape is transparent and “provides thermoregulation” to the neonate. Additionally, the bottom of the device is described as a “bubble pack” in which water flows into the pack via a hose, makes its way through the bubble pack, and then leaves through a drain hose. The water contributes to the thermoregulation aspect since it is temperature controlled. Finally, the drape device has strategically placed holes to allow for undisrupted monitoring via wires/cables attached to the neonate that connect to some external source.
Though this drape device appears efficient in regulating body temperature of neonatal patients, it may encounter some difficulties when used during surgical procedures. The only way to have access to the neonate’s abdomen in cases of hernia repair or similar procedures is to remove the side portions of the device. This action may significantly lower the device’s effectiveness in the thermoregulation process. Moreover, the device cannot be applied to young pediatric patients in the toddler or preschool age range, who also struggle with thermoregulation during surgery. The size would have to be adjusted to accommodate larger patients, but the concept of the bubble pack may still be applicable.
Week 5: TAM Calculation
Needs Statement:
Pediatric patients undergoing surgery experience lower body temperatures due to fluid leakage through the surgical draping and need a way to maintain a pro-clotting body temperature during surgery.
- Population: Pediatric patients undergoing surgery
- Opportunity: lowered body temperatures due to fluid leakage (betadine, saline, water) through surgical draping
- Outcome: maintain a pro-clotting body temperature
Approach to # of units/year:
- # of units/year is being interpreted as the number of pediatric surgical procedures performed per year
- About 3.9 million pediatric surgeries/year according to study
- This number includes the multiple surgeries individual patients underwent.
Approach to cost of product:
- Average cost was taken from cost of common pediatric surgical drapes
- Cost of product = $10.24
Total Addressable Market (TAM) Calculation:
- TAM = # of units/year * cost of product
- TAM = 3,900,000 * $10.24
- TAM = $39,936,000
Rabbitts, J. A., & Groenewald, C. B. (2020). Epidemiology of Pediatric Surgery in the United States. Paediatric anaesthesia, 30(10), 1083–1090. https://doi.org/10.1111/pan.13993
Week 6: Reflections
Our final week in the CIP program consisted of shadowing and assembling our final presentation addressing the complications of gastrostomy tubes in the pediatric population. The past six weeks provided the amazing opportunity to both experience the daily routine of the pediatric surgery team and to work in a team with individuals of diverse backgrounds but a shared goal of identifying clinical needs.
Over the course of the program, a couple lessons I learned was to not be afraid of asking questions and to embrace your ignorance of a topic/area of study. UI Health is an established teaching hospital so the staff, including the nurses, technicians, residents, and attendings, are accustomed to students asking questions. I found that the majority of staff encourage students to pose questions. You must, of course, be sure to pose your questions when the staff member is not busy attending to a patient or carrying out other important tasks.
Regarding the latter lesson, embracing your own ignorance of a topic/area of study allows you to identify and address gaps in knowledge. Acknowledging those gaps in knowledge can provide insight into the types of questions you should be asking or the topics that require more research. Addressing your ignorance and building your knowledge on surgical equipment, procedures, or workflow contributes to your development as a learner and grants you more confidence in both your interactions with the medical staff and in identifying clinical needs. Recognizing that the competent medical personnel you are shadowing were once students like yourselves makes it easier to embrace your current lack of knowledge.
To future CIP participants, I recommend that you ask your questions, whether that be to technicians, nurses, or the doctors you are shadowing. Do not discredit the technicians or nurses; they possess a vast amount of knowledge of their field and are a valuable resource. I also highly recommend engaging with your team on a regular basis. Go over the different procedures you observed, discuss any pain points each of you identified, and be sure to listen to the different perspectives presented by your team members. Lastly, enjoy your time shadowing your chosen medical team!