
Jeremy Yuan
Student Participant
Gastrointestinal Department
Good Design and Bad Design Within the GI Department
Good Design
A 2017 study focused on patients aged 50 and older who were treated at Veterans Affair facilities between 1997 and 2010 found that a colonoscopy reduced the risk of death from right-sided colorectal cancer by 46 percent and reduced the left-sided colorectal cancer by 72 percent, which results in a combined reduction of 61 percent. This result puts the colonoscopy screening procedure on the same level of screening benefit as the pap smear and the mammogram, two screening procedures long known to detect and prevent cervical and breast cancer at high rate.
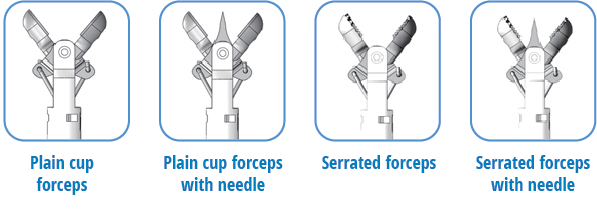
Despite how widespread and important the colonoscopy is to human society today, the procedure is only made possible by the advanced technology it uses. While I was shadowing the endoscopy lab, I witnessed many devices and procedures that were of great design, but one design that stood out to me was the cold biopsy forceps that are used in many scoping procedures. There are four designs of the forcep “jaws”: the plain cup, the plain cup with needle, the serrated cup, and the serrated cup with needle. The design I found particularly remarkable was the serrated cups with needle design, as it fits the need to take a large biopsy sample from an elastic and tough organ, as the colon is. An image of the designs can be found attached.
Activities
The forceps are usually operated by a technician or a endoscopy nurse who is well-trained in scoping procedures. The technician inserts the forceps through a chamber in the endoscope which allows it to stretch all the way to the scope camera. Once visible in the scope camera view, the technician will open the forcep jaws and then close it, which essentially takes a “bite” of the colon tissue. This entire process takes less than 20 seconds to complete.
In terms of biopsies, the pathology department enjoys having a larger amount of tissue, so two “bites” are taken of the tissue in quick succession. The needle and the serrated jaws allow the tissue from the first biopsy to remain trapped on the claw while the second “bite” is being taken. This design allows a large amount of tissue to be taken from two separate biopsy locations without losing any of the first “bite’s” tissue.
Environment
The specific and relevant environment that the forcep design is being used is within the GI tract. This includes the esophagus, the duodenum, the ileum, cecum, the rectum, and all four parts of the colon. All of these tissues are very elastic and tough, which means the serrated cups of the forceps are required to be able to grab and cut a significant portion of the tissue. The needle is effective in being able to spear or skewer the tissue piece and hold it in place while the second biopsy “bite” is taking place.
Interactions
An important point to note about the interaction surrounding the forcep usage is that the forcep is controlled by the technician, but the aiming of the claw to hit the correct location is the responsibility of the doctor. Once the forcep appears in the scope camera view, the doctor will navigate the scope such that the technician only needs to open and close the forcep to grab the sample.
Objects
As stated previously the specific objects that contribute to the good design of the serrated cup with needle forceps are the serrated cups and the needle. The serrated cups are needed to grab and cut the tough tissue, and the needle is needed to skewer the first sample while the second one is being taken.
Users
The users in this setting are the doctor, the technician, and the patient. The doctor needs to be able to take a biopsy of the desired location without using either of his hands, as those need to stay put in order to make sure the scope remains aimed at the correct location. The technician needs a way to take a biopsy of the location without disturbing the scope location and orientation. The patient needs a way for a biopsy of tough, elastic, and possibly diseased tissue to be taken.
The forceps are able to validate all three of the needs of the three users. The doctor is able to utilize both of his hands to aim and drive the scope, while the technician is able to just slide the forceps through the scope chamber and take the physical biopsy. This allows the patient to receive his diagnosis of the special tissue.
Bad Design
In such a high-stakes environment like the hospital, there is no single thing that is a truly bad or horrible design. However, there are quite a few designs that can be considered as “sub-optimal” or designs that ends up being not very effective.
Specifically within the UIC GI Endoscopy lab, one design that I found cumbersome and ineffective was the way that power cables were oriented around the carts and through the room. Within the workspace, there were about seven or eight devices that needed to be plugged into a power source of some sort. Three of the devices were plugged into the transportation cart, which is then plugged into a power source linked to the building’s infrastructure. The frustrating part of this is that the closest plugs from the building were from a pole that hangs down from the ceiling. This resulted in many cables stemming from the workspace that hangs around above the heads of stakeholders, possibly obscuring the view and causing a distraction to those performing the procedure.
Activities
As stated earlier, the doctor, technician, and the nurses are all performing activities related to the procedure. Specifically, most of them are switching from looking down at the patient to looking up at the screen that shows the scope’s camera view. The problem with the disorganized cable management is that the hanging cables often have to be moved aside so that they do not obstruct someone’s view of the screen, especially in the case of taller individuals.
Environment
The main issue of this disorganized cable management is in the environment of the workplace. The cables complicate and act as distractions in the environment where all the individuals involved in the procedure should be focused on the procedure. The doctor should not have to move the cables as they enter the room and get situated behind the patient. The nurses should not have to move the power cables every time they step away to chart some information or get supplies from the cabinet.
Interactions
Another huge problematic interaction involving the overhanging power cables is that they have a chance of slipping out of the sockets during use. As the cables are being moved often, it is pretty likely that over time, the plug will slip from its socket. If this happens during surgery, that could mean that many devices lose power, possibly leading to adverse consequences. Klaudio and I have already discovered a few plugs that seemed like they were slipping, so we went ahead and plugged those back in more securely.
Objects
The object of most interest is the power pole that projects down from the ceiling in the room. Although the cart that houses all the devices that need this power is mobile, the pole itself is fixed in the center of the room. Often times, the procedure is occurring in the center of the room, but the transport cart housing the devices is off to the side or back of the room. As a result, the power cables must extend towards the center pole, creating the distraction. A possible solution would be to create a track of sorts on the ceiling which would allow the pole to move.
Users
The users involved in this design are once again the doctor, the technician, the nurse, and patient. However, there are also other individuals involved as well, including anybody that comes into the procedure area as well as the IT and technology workers in the hospital. All individuals entering the room have to navigate through the spiderweb of cables and IT/tech workers have to fix and reboot devices that have had their power unplugged.
Scheduling Inpatient Procedures in the Endoscopy Lab at UIHealth: Storyboard

Storyboard of a GI Inpatient
A storyboard is a visual diagram that is able to model a process. It is especially helpful for breaking down a long process into distinct steps that can be identified and analyzed. For each event, pain points that could be designed around are listed. This storyboard will follow the process of a patient that is being taken care of by the GI consult team at UIHealth.
Event 1
Source: https://www.chihealth.com/en/services/emergency-medicine.html
Patient arrives to UIHealth, generally through the emergency department. They might have been brought to the hospital by ambulance or had driven themselves. Here, they undergo defensive testing by the emergency medicine doctors and are triaged. If their condition cannot be treated in the emergency room itself, they will be admitted to the hospital.
Pain Points:
- Defensive medicine is practiced in the emergency department, so often many unnecessary tests are performed, which causes financial strain on the patient and their family.
- Many emergency departments face capacity problems, so there is not always room for the patient to be seen immediately.
- Emergency departments often have to treat more complex cases first, which means that more time is allotted to each patient, which can further increase patient wait time.
Event 2
Source: https://www.hopkinsmedicine.org/patient_care/patients-visitors/admission-discharge/hospital-room.html
Patient is admitted to the hospital as an inpatient and is moved from the emergency department to the main hospital. Here, they will have their own room and will be rounded on by an internal medicine team. Nurses will make sure they are as comfortable as possible while attaching all monitoring devices to the patient.
Pain Points:
- In the case of gastrointestinal problems, which are often related to chronic health problems, patients are in the hospital often and for long periods of time, which can cost a lot.
Event 3
Source: https://www.aarp.org/caregiving/health/info-2020/coronavirus-doctors-requirements-caregivers.html
The internal medicine team will take a complete history and make an attempt to determine what is wrong. In the case that a specialist is needed, they will contact the consult team for that department. In our case, the patient has a gastrointestinal complaint, so the internal medicine team will contact the GI consult team to see this patient. If the patient has more than one chief complain, then it is possible that multiple departments are consulted for this patient. For example, if the patient has both gastrointestinal, cardiac, and neurological complaints, then specialists in all three of those departments will be consulted and will see this patient.
Pain Points:
- Because the patient is first seen by internal medicine, they might not be able to fully diagnose the problem. Instructions from internal medicine and specialists may differ, which causes increased delay on treatments.
- Instructions between specialists may differ. For example, a patient’s cardiac problem may require them to be fed through the mouth with a certain medicine, but a patient’s GI problem may require them to be NPO with another medicine.
- Treatments for different problems may have cause harmful reactions. For example, many drugs are hepatotoxic, but if the patient has liver problems that are also being treated by the hepatology consult team, then the drugs prescribed may have drug toxicity problems.
Event 4
Source: https://www.pond5.com/stock-footage/item/87114273-hospital-patient-lying-bed-his-wife-sitting-beside
One of the doctors on the GI consult team will round on this patient. Here, the doctor, fellow, and residents will take a complete gastrointestinal-related history. The GI consult team will also conduct a physical exam to further gather information. If the patient has any history of other health problems, the GI consult team will discuss with other departments to determine a care plan that takes all of the information into account. Here, the GI consult team can order further scans to further gather more information. Based on the history, the complaint, and the scans, the GI team will create a plan of care.
Usually, the plan will try to avoid procedures if possible, as every procedure comes with its risks that should not be taken if not absolutely necessary. In the case of this patient, the patient had a bowel obstruction and the large bowel was filled with gas, so a decompression tube was first used to try to take out some of the air.
Pain Points:
- Radiology services patients that have a wide variety of health problems, and they can be backed up throughout the day scanning patients. It takes a large amount of time to get a patient into the scanning room. Members of the consult team often have to wait for the patient to be scanned before doing anything else.
- Due to long wait times, patient’s hospital stays often are longer and with bowel obstructions, the more time that is taken, the greater the risk of bleeding and perforation.
Event 5
Source: https://gastroenterologen.no/2015/01/colonic-stenting-still-a-challenge/
Here, the GI team carries out the plan of care for the patient. The patient’s diet is restricted and medicines are administered. While waiting to see the results of these treatments, the patient will continue to be rounded on and monitored by the GI team as well as the medicine team responsible for their care. Further scans are ordered and taken to monitor the progress of the treatment and to determine if further interventions need to be taken. In the case of this patient, the decompression tube did not work as well as the GI team had hoped, so they decided that the patient must be scoped in order to determine the exact cause of the obstruction (small bowel or large bowel).
Pain Points:
- Because the endoscopy lab is for both inpatient and outpatient scopes, the beds in the lab are often filled. Outpatient scopes get priority first, despite the inpatient scopes being more urgent and necessary.
- If the procedure preparation beds are filled in the lab, then the inpatient will not be able to be wheeled down until a bed opens up.
- If an inpatient is moved into the preparation area but has to wait for their procedure, the flow of the outpatients will be disrupted, possibly delaying later procedures even more.
Event 6
Source: https://alexanderorthopaedics.com/preparing-for-surgery/
The patient is scheduled for a scope and moved to the endoscopy lab. The doctor will inform the patient on the procedure, what they are looking for, and possible risks of the procedure. The patient will be prepared for the procedure by the nurses in the endoscopy lab and will wait for an opening for an attending and fellow to perform the procedure.
Pain Points:
- In order for the inpatient to be scoped, they must wait for an attending doctor to sit in on the procedure. There is only one attending on service at a time, and this attending often has their own outpatients to scope as well. Therefore, the inpatient must wait until the attending is done with their outpatient scopes as well as clinic in order to finally fit their procedure in.
Event 7
Source: https://en.wikipedia.org/wiki/Colonoscopy
The patient undergoes the procedure with the attending doctor, the fellow, and procedure nurses. For our patient, a colonoscopy is performed to look for large bowel obstruction and to suction out as much air as possible. No large bowel obstruction was found in the patient, so the patient should have a full recovery after the excess air was suctioned out of the colon.
Pain Points:
- Pain points within the procedure are many, but they have been outlined in many of my colleagues blog posts. Software bugs, technology not working, as well as cluttered work areas are just some of the pain points during the procedure that are faced.
Event 8
Source: https://www.sjahs.org/how-long-do-you-stay-in-recovery-room-after-surgery/
The patient recovers from the procedure in the recovery area while the sedation wears off. The patient’s vitals are monitored by recovery nurses. Once the patient is recovered from the sedation, they are moved back to their inpatient room in the hospital to continue feeding and medicine for a few days.
Pain Points:
- Inpatient scope patients are often sicker, undergo more sedation, and take longer to recover than their outpatient counterparts. As a result, they stay in the recovery bay for a longer period of time, which can further delay the flow of procedures in the endoscopy lab.
Event 9
Source: https://www.nextavenue.org/know-before-hospital-discharge/
After the patient makes a recovery, he or she is discharged from the hospital back home with instructions for home. Sometimes, a follow-up appointment is scheduled with the attending doctor in clinic to check on recovery progress.
Pain Points:
- Because most inpatient GI patients have chronic GI complications, the instructions for home are often ineffective and will most likely return to the hospital with further complications.
Large-bowel disease presenting as small-bowel obstruction is associated with a poor prognosis
Jessica L. Weaver, Rebecca E. Barnett, Danielle E. Patterson, Vikram G. Ramjee, Eric Riedinger, Jason Younga, Ernesto A. Sepulveda, Robert C. Keskey, William G. Cheadle, Large-bowel disease presenting as small-bowel obstruction is associated with a poor prognosis, The American Journal of Emergency Medicine, Volume 34, Issue 3, 2016, Pages 477-479, ISSN 0735-6757, https://doi.org/10.1016/j.ajem.2015.12.008.
Small bowel obstructions (SBOs) are more common than large bowel obstructions (LBOs), so sometimes large bowel pathology and diseases are not recognized at the time of presentation because it presents as an SBO. SBOs vs. SBOs with underlying large bowel pathology must be differentiated using imaging techniques, but these imaging techniques are not perfect. The most-relied-upon imaging technique, computer tomographic scan (CT scan) has been reported to only predict the level of intestinal obstruction in 93% of cases. The purpose of the study is to assess whether large bowel pathology presenting as an SBO has any specific risk factors or underlying causes as well as to identify differences in outcome compared with isolated SBO. Retrospective medical record review at the University of Louisville Hospital and the Robley Rex Veterans Affair Hospital in Louisville, KY where diagnosis was confirmed with CT scan was conducted. It was found that SBOs with underlying large bowel pathology had a 37% mortality rate compared to the isolated SBO population, which was 9.4%. Furthermore, 93% of the SBOs with underlying large bowel pathology patients died as a result of the obstruction, compared to 6% in the general population. In conclusion, SBOs with underlying large bowel pathology is associated with a much higher mortality rate than isolated SBO, so therefore, CT scanning is recommended for all these patients.
Needs Statement Iterations for First-Year Gastrointestinal Fellows
Since joining the GI consult service, a new class of first-year fellows have joined. GI fellows have already completed their internal medicine residency. Each of them interviewed and were accepted into our competitive program with GI knowledge, but no hands-on procedural experience yet.
First Iteration: (Based on observations only)
First-year GI fellows need a way to practice basic scoping maneuvers before scoping a real patient in order to reduce procedure time and risk of perforation.
[Population]: The population includes first-year GI fellows. I believe that this is an appropriate population scope for a few reasons. First, only GI clinicians and GI clinicians-in-training need to be trained to perform GI scoping procedures. Second, only first-year GI fellows need this basic training because these fellows will undergo more intense practice on real patients throughout their first-year. By the time they perform many procedures, they will not need this basic training anymore.
[Opportunity]: The opportunity is a way to practice basic scoping maneuvers before scoping a real patient. At UIHealth, there is currently no software or training simulation that allows a fellow to practice maneuvering a scope. The scope is not a simple instrument to use and does require skills and practice to learn and master. The first time a first-year fellow touches a scope is to scope out a real patient.
[Outcome]: Because first-year fellows are inexperienced with the scope, they spend a lot of time navigating through the colon/esophagus as well as cleaning and suctioning away debris. Often times, they spend a lot of time staring at a wall because they aren’t able to make a tough turn. Ideally for scoping procedures, you want to drive to the extent of the scope and then take time to withdraw the scope. Taking a long time to drive through to the extent would increase procedure time, which naturally also increases the risk for perforation during the procedure.
Rationale for Changes: It just seemed strange to me that a first-year GI fellow, who applied, interviewed, and was accepted into a GI program, has never touched a scope before. Furthermore, they are also a full-on internal medicine attending as well. I wanted to fill a need or an improvement for these first-year fellows to help them get acclimated faster and possibly help them impress their attendings when they finally get to real patients.
Second Iteration: (Based on observations and interviews)
First-year GI fellows or third-year internal medicine residents without any scoping experience need a way to practice basic scoping maneuvers before scoping a real patient in order to reduce risk of perforation and procedure time.
[Population]: The population was refined to first-year GI fellows without any scoping experience and third-year internal medicine residents. After interviewing some of the fellows, they let me know that some (not all) fellows that come in already have some limited scoping experience. I have also added third-year internal medicine residents because third-year internal medicine residents who are looking to apply and be accepted into GI fellowship experiences may benefit from completing scoping courses or training before applying.
[Opportunity]: The opportunity remains the same as the previous iteration of the needs statement.
[Outcome]: The outcome also remains the same as the previous iteration of the needs statement.
Rationale for Changes: The reason for the changes was that I discovered after a few interviews that some residency and fellowship programs do have some sort of training implemented, but this training is not standardized across all healthcare institutions and some institutions (like UIHealth) don’t even have any training at all. Therefore, a modified population was called for by the needs statement. The population scope has now been narrowed down to first-year GI residents that do not have access to the training apparatuses, and third-year internal medicine residents that may be interested in applying to GI or will be matriculating into a GI program that does not have access to the training.
Third Iteration: (Based on observations, interviews, and secondary research)
First-year GI fellows or third-year internal medicine residents without any scoping experience need a way to practice basic scoping maneuvers such as driving the scope, making sharp turns, orienting the camera, spraying water and CO2, and suctioning debris in order to bridge the current gaps in endoscopy training and eventually lead to standardized endoscopy training procedures for both the faculty trainers and the trainees.
[Population]: The population remains the same as the previous iteration.
[Opportunity]: The opportunity scope has been narrowed to include a standardized set of maneuvers.
[Outcome]: The outcome has also been edited to match the new outcome goal of providing standardized endoscopy training for the trainers and the trainees. This will indirectly lead to better outcomes for patients, which was our original outcome.
Rationale for Changes: The reason for the changes was that I discovered much of the endoscopy training literature is aimed at providing a standardized training regiment for fellows and for the faculty trainers. The students (fellows and residents) would benefit from a standardized teaching approach, verbal and physical preparation for training, and training using standardized language with the avoidance of cognitive overload. The faculty trainers or attendings would benefit from this training by learning the standardized approach with the standardized language, and have better-trained fellows helping them out with their own workload and cases. The long-term effect of a standardized training regiment is generational, in that regiment-trained fellows will eventually become the attending trainers that will pass down the same training they received to new fellows.
Active Colonoscopy Training Model Patent
The needs statement being investigated for this week is, “First-year GI fellows without any scoping experience need a way to practice scoping maneuvers in order to bridge the current gaps in endoscopy training and create a standardized endoscopy training procedures for both the faculty trainers and the trainees.” This statement is an iteration of the needs statement from my blog post in the previous week.
Patent Name: Active colonoscopy training model and method
Patent Number: 9990862
Inventors: Junghun Choi
Applicant: Ohio University
Family ID: 48574790
Claims:
This device is composed of a model to simulate colonoscopies using a real endoscope. The model itself is composed of two main parts: the abdominal model and the colorectal tube. The abdominal model is composed of an outer body with a hollow interior portion that houses the colorectal tube that is configured to model the human colon. The colorectal tube is able to receive the endoscope just like the rectum does in a real patient. The physical scope is inserted through the anus unit, which is a part of the outer body of the abdominal model.
The device is able to monitor the position of the scope and the interstitial pressure inside the colorectal tube. The position of the scope is determined by load cells and photocells that are scattered throughout the colorectal tube. These cells detect the strength of the light emitted from the end of the endoscope and transmit this information to a computer which is able to calculate and record the position and path of the endoscope through the training model. The interstitial pressure inside the tube is measured using pressure transducers and this information is also sent to the computer.
Satisfying Needs:
This patent is able to partly satisfy the need described in the needs statement. Creating a standardized endoscopy training procedure is not a large overarching goal, but having a standardized simulation across all healthcare institutions would be a helpful step towards satisfying this need. If every first-year GI fellow is required to complete modules on a standardized training simulation, then instructors will also be able to reference these modules to better improve their teaching abilities.
This patent also satisfies a quality-of-life need in the procedure room. Through my primary observations, I have noticed that the first-year fellows are not very experienced in basic maneuvers of the endoscope and often spend lots of time driving the scope into the wall, unable to progress through the colon. The attending physicians always give instructions such as “Just make a right turn and drive through there,” but first-year fellows sometimes are not able to follow these instructions because they don’t know how to make a right turn. Making a right turn with the scope requires the operator to both turn the dials and change the positioning of his/her left hand in very specific movements. Because the first-year fellows have not mastered this combination of movement to muscle memory, they are often unable to make this simple turn. As a result, both the attending physician and the fellow often get frustrated, usually with the attending asking to take over and finish the procedure. This patent is able to satisfy this quality-of-life need by giving first-year fellows a chance to practice these maneuvers on their own without an attending physician present. Therefore, they can take as much time as they need and repeat these maneuvers as many times as they need to master the fine movements. Fellows could even be able to take the training simulation home with them or practice after a day in the clinic. For example, Fellow A could finish a day in the clinic and decide to practice some scoping techniques before his procedure rotation in the following weeks. Fellow A would then use the training model to practice 20 right-hand turns, 20 left-hand turns, 20 upward-turns, and 20 downward-turns. When fellow A’s attending asks him to turn right tomorrow during a scope on a real patient, fellow A will have the necessary muscle memory to drive the scope through the colon.
Clinical Immersion Program 2022 Reflections
lessons learned from the clinic, the program, and stakeholders. Also include recommendations to future CIP participants
My experience in the Clinical Immersion Program 2022 was a unique and eye-opening experience. Now that the program has finished up and we have given our final presentation about the ergonomic pitfalls of the modern endoscope, I wanted to write a little bit about some important lessons that I learned and a few recommendations to future CIP participants.
Lesson 1: View medicine through the lens of an informed engineer rather than an aspiring doctor.
This lesson was probably the most important and first lessons that I had to learn. Medicine is a profession of perpetual learning, especially at the start of the medical education journey. Everything that is learned is new and novel and seems important: what different things mean, what different things are for, how different things are used, and many more questions. At the beginning of the program I was too enveloped in the medicine of gastroenterology, a field I could see myself pursuing in the future. I wanted to learn about all the diseases, all the diagnoses, all the signs and symptoms that helped the physicians develop their differential diagnosis. Having a chance to see sick patients urged me to do my best to help them through medicine, and that was an urge I had to suppress to maximize my time in the program.
Later, I started to take a step back and not worry so much about the patients and medicine, but to rather observe behaviors and processes involved in treating these patients. Through this perspective shift, I started to identify the needs of the clinical space as a whole instead of the specific medical needs of the patient.
This lesson leads me to my first recommendation for future CIP participants. Being an IMED student, you have an extremely unique and powerful role in the process of advancing medical technology. Because you are an aspiring physician, you have the knowledge to precisely determine the desirability of a problem space. Since you are also knowledgeable about engineering and technology, you have the knowledge to determine the feasibility and viability of a solution in this problem space. Combine all of this knowledge while participating in the clinical immersion program, this will change how you view medicine as a field in some way for sure. Furthermore, it will help you gain the skills necessary to eventually bridge the gap between physicians and engineers throughout the design process.
Lesson 2: Problems are sometimes most apparent to the youngest pair of eyes.
Medical technology has progressed drastically in the last 2o years, and many of the practicing physicians during that time may not be completely adjusted to new and improving technology as it comes out. Some might be more behind than others, and some might be less willing to learn about new technology than others as well. In my experience, one of the older attending physicians extremely disliked electronic medical records, while the majority of younger physicians and nurses believed that EMR was godsent. Sometimes, older physicians, being the most experienced in their field, might do certain things a certain way, despite you believing there could be a much more efficient way to do it. They might tell you, “This is the way it has always been done,” and tell you that they have no problem. However, younger physicians (either younger attendings or even fellows/residents) may have thought about how processes can be improved because they are able to recognize the problem.
This lesson leads me to my second and final recommendation. Whenever, conducting interviews or exploring a problem, make sure to ask not only the experienced attending physicians, but also the youngest and most inexperienced residents as well. As I explained earlier, younger physicians may have a completely different view of a problem than older attendings, and they might be too scared to voice their opinion to anybody else because they are the “lowest on the food chain”. Most people do consider age when picking potential interview candidates, but they don’t always consider that being the most experienced could occlude one’s view on the problem space.