Abdul Zakkar
Abdul Zakkar
Basic Information about Student (Small Background introduction)
Year:
Area of Research:
Contact Information:
Blog
First exposure to Dry Eye Disease
This week, we first visited the ophthalmology clinic as well as the clinical trial center for Dry Eye Disease (DED). We observed many patients with DED, and learned that these patients often have a history of bone marrow transplant, and the DED is one of the manifestations of their graft-vs-host disease that results from the bone marrow transplant. Other causes of DED include aging as well as autoimmune disorders; commonly Sjogren’s and rheumatoid arthritis.
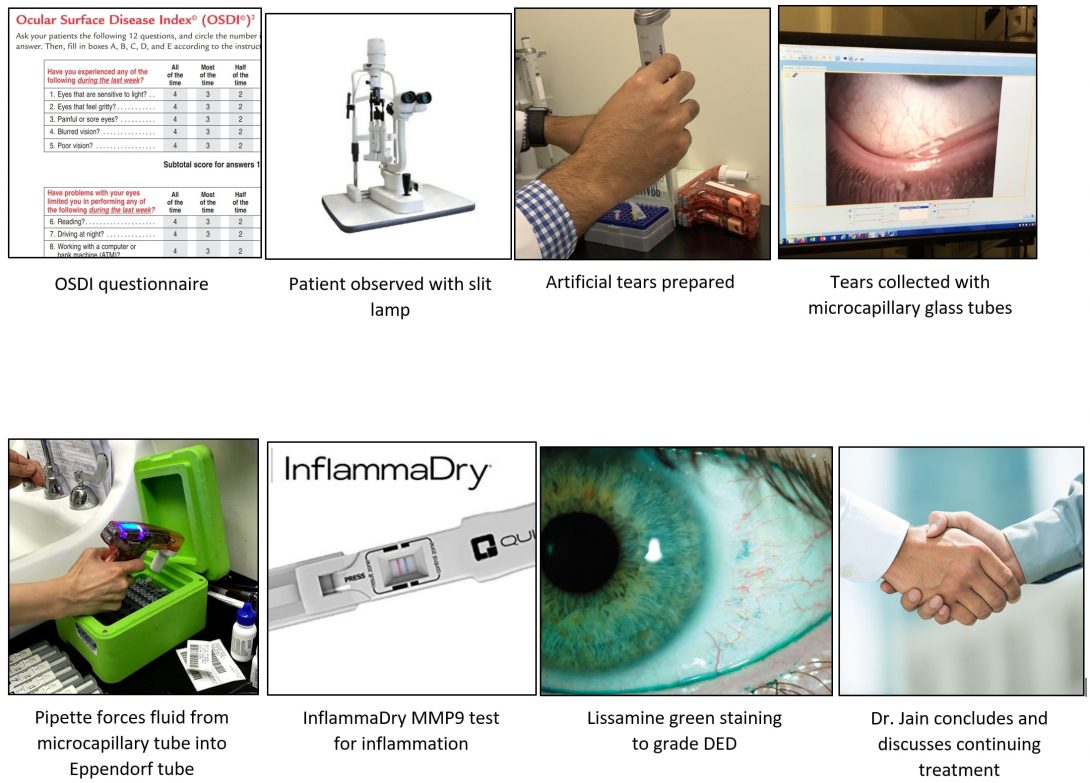
For most patients, Dr. Jain follows a similar procedure. He first collects a short relevant history from the patient, then observes their eye using a slit lamp to look closely. Next, he begins a tear collection process. He first adds artificial tears to the patient’s eye, then collects those tears using micro-capillary tubes. Next, he adds a special dye to the patient’s eye to observe damage done by DED and grade it. Then, they dye is washed out, and Dr. Jain discusses his findings with the patient, and their treatment plan moving forward. This process may seem short, but we found many instances of both good and bad design within it
Good and Bad Design
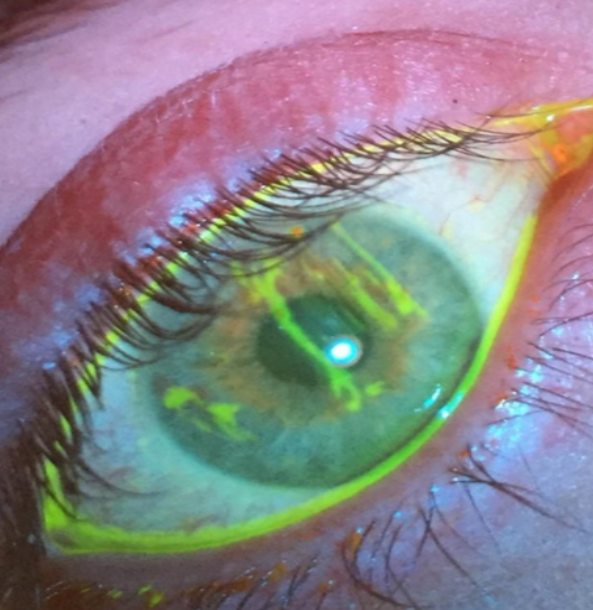
I will focus on the process of adding dye to the patient’s eye (staining) to illustrate both good and bad design. The procedure that Dr. Jain and his team follow when staining the patient’s eye is very efficient and smooth. First, one of Dr. Jain’s assistants prepares a pipette with the exact amount of dye needed for staining, and presents it to Dr. Jain the moment he needs it. After Dr. Jain has observed the stained eye, the assistant begins washing the eye out while Dr. Jain records his findings to begin discussion with the patient.
- A – Dr. Jain and assistants are adding dye to the patient’s eye, Dr. Jain observing, assistants washing.
- E – The clinic/clinical trial center.
- I – Dr. Jain is engaged with the patient and the assistants.
- O – The pipette, the dye, the patient’s chair.
- U – Dr. Jain, the assistants, and the patient.
In terms of bad design, I learned about the way Dr. Jain records his findings after staining. The lissamine green stain that Dr. Jain uses stains the parts of the eye with epithelial damage caused by DED. This appears as small specks of staining scattered across the surface of the eye. Dr. Jain then decides based on the number of specks, and their size, what the clinical grade should be. I feel this is bad design because of the scale’s subjectivity. Other ophthalmologists may come to different a grading when looking at the same eye.
- A – doctor is grading the severity of eye disease
- E – in the clinic
- I – after looking at the eye on the slit lamp, the doctor is writing the numbers to grade the dots on the paper
- O – slit lamp, paper on which the eye is graded
- U – patient, doctor/healthcare provider
week of 7/1
This week, we got the chance to talk to some patients, as well as some research assistants about how they feel about the current process that every DED patient undergoes. We mostly focused on the tear collection process, since that seems to be a pain point for the assistants and the physician. However, we found that patients did not seem to mind the tear collection very much and some found it to be efficient and well-performed and thought out. Only first-time patients reported being apprehensive at first, but trusted Dr. Jain once the tear collection began. Nevertheless, the tear collection process seems to be the largest concern for Dr. Jain and his lab, since it can require up to two assistants to perform effectively. I asked the assistants about their use of time and how much the tear collection can take away from that and found that there is plenty more they can be spending their time on to push the agenda of the lab forward.
I will story board the entire general process that a returning DED patient undergoes when they see Dr. Jain, starting with the history and ending with a prescription or other recommendations.
Storyboard
First, Dr. Jain asks the patient how they have been doing in general, then asks focused questions based on the Ocular Surface Disease Index (OSDI) to record responses consistently over time.
Next, Dr. Jain examines the patient’s eye using the slit lamp, looking for signs of worsening or improving DED.
Then, Dr. Jain initiates the tear collection process. The first assistant hands Dr. Jain a loaded pipette with artificial tears for Dr. Jain to drop into the patient’s eye. A timer is started. He asks the patient to look in various directions to distribute the artificial tears evenly.
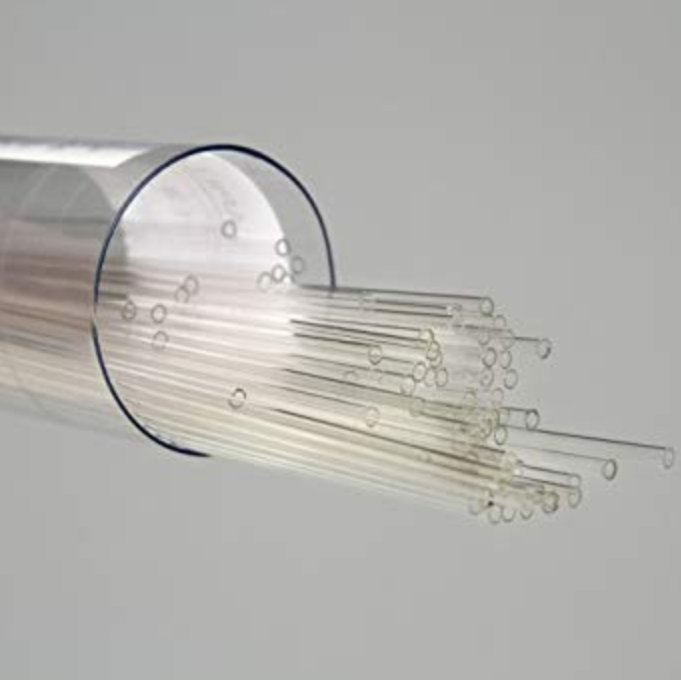
After 40 seconds, Dr. Jain is handed the first microcapillary glass tube and draws some of the fluid from the patient’s eye, with the help of the slit lamp. He then returns the microcapillary to the assistant, who hands it over to the next assistant who forces the tube fluid out into an Eppendorf tube using another pipette. This process repeats until all the fluid has been removed from the patient’s eye.
The last portion of the patient’s tears is used to conduct an MMP9 test, which involves dropping some of the tear fluid onto a small device that will detect the presence of MMP9, which is a general sign of active inflammation.
Next, the patient is handed a tissue to dry their eye with, in preparation for the staining.
The assistant hands Dr. Jain a pipette loaded with lissamine green dye, which Dr. Jain then drops into the patient’s eye. He asks the patient to look in various directions to distribute the dye evenly.
Dr. Jain then uses the slit lamp to observe the staining of the eye, recording his findings using the NEI metric for DED. He may take photographs if the option is available (i.e. in the clinical trial center).
Finally, the assistant cleans the dye out of the patient’s eye with saline while Dr. Jain records his findings.
Dr. Jain gives his conclusions on the visit and makes recommendations about continued treatment for the patient’s DED. The patient may head to the waiting room to make the next appointment.
week of 7/8
This week, my team and I had the chance to conduct an interview with the researcher in Dr. Jain’s lab who conducts tests to analyze tears after Dr. Jain collects them. We learned that tears are assessed for various bio-markers such as extracellular DNA, cytokines, immunoglobulins, ACPA antibodies, and others in order to identify the causative agent of a patient’s dry eye disease. The researcher discussed the process of tear collection in detail and noted that the process is not sterile. The researchers do not use gloves, which are generally not used with ophthalmology clinic patients because they make the patients “skeptical.” Dr. Jain will still sanitize his hands though, and the team still takes appropriate measures for sanitation. However, it is nearly impossible to keep the tear sample completely untouched throughout the process.
For this week, we were tasked with creating a needs statement that describes a problem that Dr. Jain and his team face. The following are a few iterations of this needs statement.
Needs statement 1

Make tear collection accessible for more healthcare workers and safe for patients.
The main point that we would like to get across is that tear collection is currently restricted to highly trained ophthalmologists who have access to a slit lamp and other devices in order to perform the collection safely. We would like to remove this restriction and make tear collection feasible for most healthcare workers in any setting.
Needs statement 2

Modify the tear collection process to make it user friendly for more healthcare workers to use safely on patients.
Here we are specifying what we mean by accessible in particular. We went from broad accessibility which includes cost as well as training, and the more specific user-friendly, which indicates ease of use as our primary goal.
Needs statement 3
To create a more user-friendly tear collection process that allows any healthcare professional with minimal training to collect patients’ tears safely
Here were are specifying the user to a more defined set of people. We are targetting healthcare workers who have not been trained like the ophthalmologist Dr. Jain, and we would like them to still be able to use our process/device easily.
week of 7/15
This week, my team and I came up with design criteria that we would like to implement in improving the current tear collection process carried out by Dr. Jain and his assistants. We also tried to come up with solutions and ideas to get ourselves started. Some of these ideas involved modifying the current glass capillary tube that Dr. Jain uses to something that can hold a larger volume, and be less abrasive to the patient’s eye. Some ideas involved suction in addition to the tried and true capillary action. This suction may be motorized or mechanized. Some ideas involved a pen-like device, while others involved a device that rests on a table in between the patient and the healthcare provider. All these designs were thought of in order to meet at least one of our design criteria, which are listed below.
Comfort criteria

The device or part of the device that comes near the eye should remain there for no more than 10 seconds.
image

____________________
Efficiency Criteria
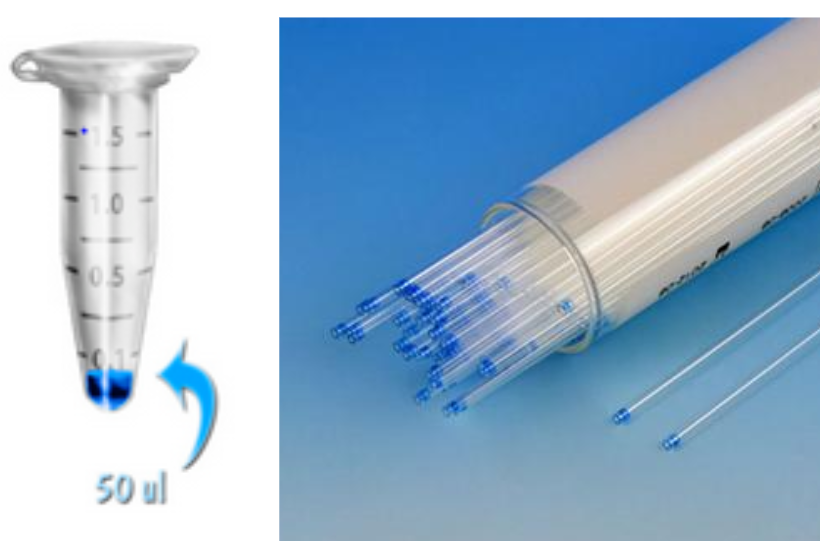
The entire process of tear collection, from start to finish, should take place in one minute or less.
The minimum amount of tear collection in a healthy individual with no DED should be at least 50 microliters, or the amount of artificial tears that was added to the eye.
Safety Criteria
The deivce or process should cause no injury to the eye during any portion of the process.
Materials that touch the eye should be sanitary.
Materials that come in contact with the tears collected should be disposable.
Image
____________________
Accessibility Criteria

Healthcare providers should be able to use the device or process after one demonstration.
The device can be used/the process can be carried out by a single person without the assistance of a slit lamp, or any additional materials.
Conceptualization

By this week, my team and I had plenty of ideas on how to make the tear collection process more efficient and accessible. We did our best to consider all of our requirements in each of our ideas; however, it was difficult to include them all. After attempting several sketches and constructing several ideas, we had a set of core features we wanted to discuss with Dr. Jain. As per Dr. Felder’s advice, splitting our ideas into core concepts when presenting to Dr. Jain reduces the risk of an entire idea being shot down as a whole even when some of its parts are viable working concepts.
So we went about creating our core features, and I felt worried that we had no clear way of developing these features into physical prototypes. We had not considered how we may take a sketch into reality. Are there parts that we can order? Do we have to 3D print custom parts? Maybe some combination of the two? I felt that going from these sketches that only convey a concept to a working prototype would not be easy. Thankfully, we had plenty of resources on our hands as UIC students to learn from others and come up with realistic ways to bring our ideas to life. This includes Innovation Center and UIC faculty in general, as well as mHUB, which is also an innovation center for product development and manufacturing. After discussing our problems with several people, including Dr. Jain, we were able to come up with a list of parts to construct our first prototype.
Discussing with Stakeholders
We brought our individual concepts to Dr. Jain in a powerpoint slide to discuss different ideas to make the tear collection process more efficient and accessible. Our expectation was that Dr. Jain would have very clear opinions on most of our concepts, and we were right. Thankfully, he did find a few concepts highly worth attempting. He told us what he felt was most important to him, and generally was open to try anything. He most valued the safety of his patients, and the ability for anyone to use the device. Dr. Jain is someone who always pushes people forward, discussing ways to push our designs to their maximum potential. On the other hand, one of Dr. Jain’s research assistants was a little bit more critical.
I found this research assistant’s hesitance and skepticism very useful as a balance against Dr. Jain’s positivity and willingness to try everything. She pointed out flaws and implausibilities which allowed us to take a step back and reassess our ideas. She brought up very good points about so and so concept that may make it unusable. Dr. Jain and his assistant provided a good Yin and Yang to the project, while UIC faculty and mHUB members helped us inch closer and closer to our first prototype, which we hope we can create in Week 6.