Agata Bogdanowicz
Agata Bogdanowicz

Basic Information about Student (Small Background introduction)
I am thrilled to be part of the Clinical Immersion Program this summer and see first-hand the valuable dynamic between clinical observation and engineering. Having a particular interest in medical devices, I feel that there is no better way to learn about their design and development stages, as well as how they can be improved, than to observe the interactions that healthcare professionals have with them, specifically in the GI/Liver Department. Not only that, but by being a ‘fly on the wall’ and observing clinical operations and workflow, my team will have the opportunity to hopefully improve the efficiency of the overall work environment and therefore the quality of patient care.
I am currently in my final year as an undergraduate student looking to pursue a career in the medical device industry upon graduation. Being interested in the technical aspects of medical instruments and hardware, I have also picked up a minor in Electrical Engineering that I am hoping I can put to good use during this program. During my free time I am heavily involved with Biomedical Engineering Society as its current President and work as a Pharmacy Technician, not to mention enjoy hanging out with friends and family, going to concerts, and spending time exploring Chicago and its many coffee shops.
Year: Senior Undergraduate Bioengineering Student
Area of Research: Medical Devices & Bioinstrumentation
Department: Gastroenterology & Hepatology
Contact Information: abogda7@uic.edu
Blog
A Lot to Digest
This first week of clinical shadowing proved to me that I have a lot to see and even more to learn. With each day bringing new procedures, new patient interactions and new engineering problems to dwell on, my first days were a culmination of confusion and amazement. I have quickly come to see that GI/Hepatology are much more complex branches of medicine than previously thought that examine the intricate symphony between various organs and what repercussions follow if these systems encounter disease or complications. More specifically, I have realized the immense value of this specialty after seeing routine colonoscopy screenings turn into urgent polypectomies, the importance of endoscopic procedures like EGDs and ERCPs and their role in the diagnosis of conditions such as ulcerative colitis and Crohn’s Disease, as well as the imperative interplay between medical instruments like scopes and the sophisticated techniques employed when using them to get optimal results. Being present in the clinic and viewing procedures has also opened my eyes to the significance of patient-physician communication, patient education, and how even the communication between physicians from various departments can impact patient outcomes. Despite a hefty load of medical jargon to digest, I am grateful that our assigned team of doctors has taken the time to expose us to various procedures like esophageal dilation, EVL, pouchoscopies, as well as the repositioning of colonic stents and has played an active role in teaching us about what is happening as we observe.
Although only a few days into the program, so far my time in the clinic and scoping lab has been nothing but thought-provoking and has led me to identify a number of potential issues and areas for improvement, some more straightforward to fix than others. From an engineering perspective, my group has utilized the AEIOU concept which involves evaluation of activities, environment, interactions, objects and users to begin organizing and framing our observations. This structure will lead us to successfully integrate user-centered design principles to develop solutions to such problems. Preliminary assessments in our experience have revealed good and bad designs all throughout the AEIOU framework.
Bad Design Characteristics: After a discussion with one physician, it was mentioned that Gastroenterologists are especially prone to developing conditions like carpel tunnel and tendonitis in their hands due to extensive and repetitive turning and twisting of dials and knobs. This issue indicates poor ergonomics and designs of common scopes which can be improved by simply paying closer attention to how they are held and modifying their features. We also noticed that inefficient scope designs can easily lead to obstructions consequently limiting the field of vision of the user. Another problem we encountered time and time again was the cable-tangling fiasco. Not only were wires exposed on the ground, a potential tripping hazard in a small space, but were also tangled on patients. This was especially noticeable after a patient was being repositioned and proceeded to say “something just got unplugged from my arm”. Although this may be a complicated issue to fix it is still problematic and can cause major issues for hospital staff during patient transport, procedure organization and even staff safety. Furthermore, we also noticed that procedure rooms are relatively small for the amount of equipment, supplies and individuals that are inside at a time. During a procedure, it took the nurse almost two minutes to walk over, locate and prepare an instrument simply because she had limited space to do so.
Good Design Characteristics: Observations have also confirmed that the overall workflow of UI Health is both sophisticated, thorough, and incredibly efficient. Prior to each procedure the team takes a “time out” to confirm each patient and fills them in on what exactly is going to happen. The software that the department employs to organize patients is also very explicit in detailing what room the procedure is in, the operating physician, what procedure is taking place and whether it has started, where the patient is currently located, as well as implementing color coding to specify if the patient is entirely ready. In addition, scope sanitation procedures are also very meticulous and extensive to ensure risk of contamination and infection are minimized.
Endoscopic Ultrasound (EUS)
Fiducial Marker Placement Procedure
Procedure Background: Endoscopic Ultrasounds are minimally invasive advanced procedures that combine detailed imaging techniques of endoscopies with ultrasound capabilities. Using this method, a delivery system similar to a biopsy needle places small inert metallic markers termed ‘fiducials’ locally or inside a tumor via a scope’s instrument channel port. Successful placement of the fiducials allows for improved accuracy of tumor location during imaging as well as more focused and precise introduction of drug therapies to the targeted tumor.
1. Ultrasound + Endoscope Setup

AEIOU Summary: Clinical staff connects ultrasound to endoscope and sets up physician user’s operation preferences such as water pressure and carbon dioxide.
Pain Points: Potential implications of monitor or system failure or malfunction, insufficient knowledge of hardware operations as well as confusing button labels and overall layout.
2. Initial EGD + Secondary Ultrasound
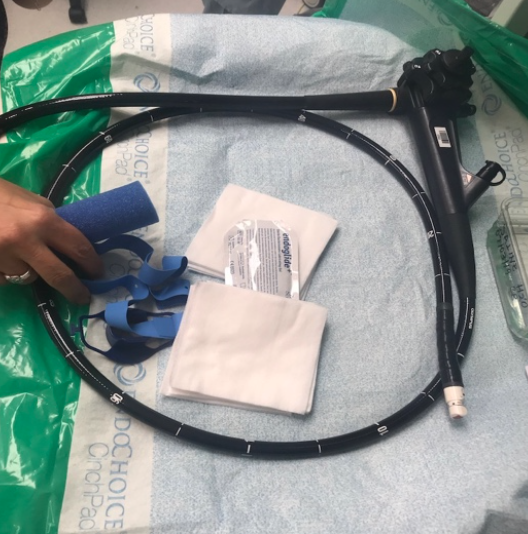
AEIOU Summary: Initially, the endoscope is inserted into the mouth and is inserted until the desired location is reached (EGD -esophagus, stomach, duodenum). This allows for visualization of the area and location of the mass. Once found, the scope is exchanged for one with an ultrasound probe on its tip.
Pain Points: Due to minimal guidelines outlining sedation protocols for patients undergoing such procedures, patients may wake up during the procedure or have little to no response to the given anesthesia. Also, once the mass is located with the endoscope, finding it again with an ultrasound probed scope is not guaranteed and may be difficult.
3. Locating of Tumor

AEIOU Summary: Attending Physician/ Fellow locates tumor using ultrasound and determines its size while echogenic properties reveal degree to which mass has invaded surrounding tissue.
Pain Points: Readings and images are unstable on ultrasound monitor due to incurring movements, patient positioning, or location of particular mass.
4. Fiducial Delivery Device Prep
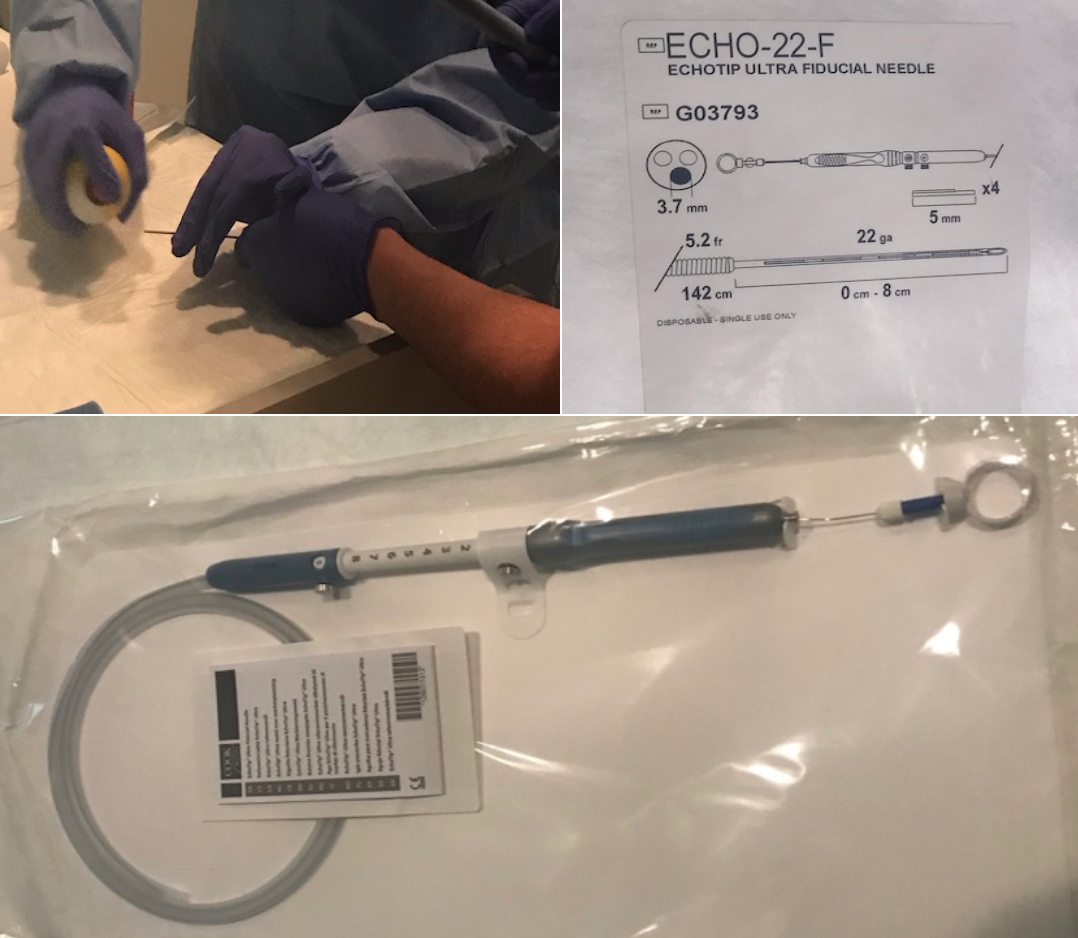
AEIOU Summary: Fiducial delivery system prepared by nurse at instrument holding table, additional lubrication is needed and then needle is fed through scope’s channel port to targeted tumor site.
Pain Points: For improved deployment of markers needle is lubricated with PAM cooking spray.
5. Deployment of Fiducial Marker

AEIOU Summary: Deployment of fiducial markers locally or directly into tumor using needle fed through scope’s port. Successful implantation is confirmed via ultrasound scope.
Pain Points: Possibility of surrounding blood vessel puncture or hitting of already present stent.
6. Holding of Patient's Jaw
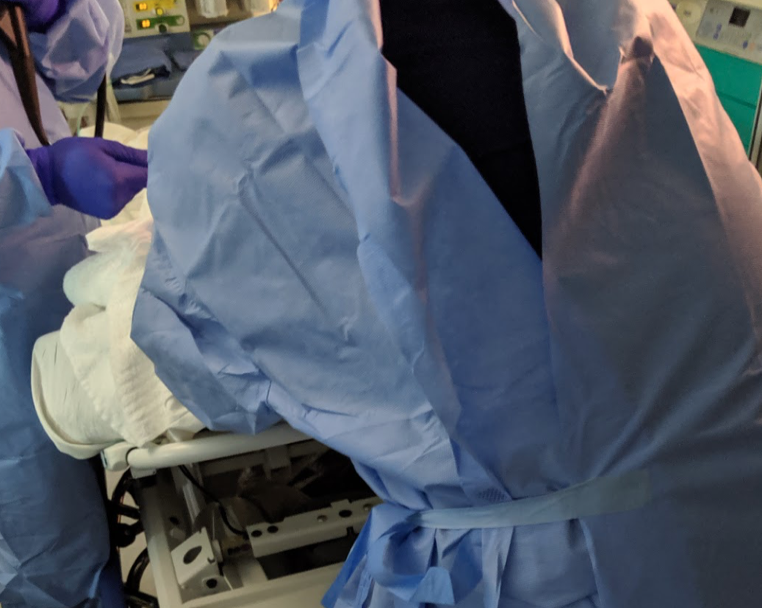
AEIOU Summary: Staff nurse standing behind bed holding patient’s jaw forward for approximately 15 minutes to avoid airway obstruction which may lead to potential intubation. This was done throughout the entirety of the procedure.
Pain Points:This action results in a more crowded environment inside an already small lab room. During this EUS procedure, two different staff nurses had to be involved in this activity after the first one became fatigued from holding the jaw for a prolonged period of time.
Nurses Have A Lot of Upper Body Strength
Close observation in the clinic these past three weeks has led to me to notice a very apparent trend in the way that hospital staff, especially nurses, interact with patients undergoing upper endoscopic procedures. That being said, these procedures may pose a risk to patients, namely those with underlying pulmonary conditions like asthma or COPD, leading to compromised airways and then causing them to go into severe respiratory depression. This abrupt change in their breathing pattern may ultimately cause them to need intubation and full anesthetic sedation, something that is not ideal for the patient and overall procedure. On several occasions where patients were beginning to have trouble breathing during their procedure due to their position, a nurse was instructed leave her designated location and other responsibilities to stand at the head of the patients bed to push the patient’s jaw forward with full force in in order to mitigate the airway obstruction and improve respiration. In certain cases the nurse did this for over 15 minutes, until she became exhausted and her arms were so fatigued that they were shaking at which point the anesthesia team was called in to intubate and fully sedate leading me to conclude that: nurses do in fact have a lot of upper body strength. It should be noted that in certain situations before deciding to intubate the patient, if the first nurse got so tired she could no longer hold the patient’s jaw with full force, another nurse was called in to do the same.
These observations lead me to beg the question if this process can be circumvented and if there can not only be a decreased dependence on staff for sustaining manual manipulation of patients during procedures, but also a decrease in the physical burden placed on this staff. Moreover, if addressing these issues would eliminate the need for an extra individual in an already crowded environment pigeonholed into doing one task.
Engineering Process Application:
As discussed in this week’s workshop, a successful and effective needs statement should be framed in an appropriate context within a particular design stage and is comprised of three components; a problem, population, and outcome. As more data is collected and information is gathered, new iterations of this statement should be created to narrow the scope and specificity of the needs being addressed.
Problem: airway obstructions
Population: patients with underlying obstructive airway conditions
Outcome: decreased dependence of sustained manual manipulation of patients during procedures
Iteration #1:
A way to eliminate airway obstructions in patients with underlying obstruction inducing pulmonary conditions that decreases dependence of staff sustained manual manipulation of patients during procedures.
Iteration #2:
A way to minimize airway obstructions and need for intubation in patients with underlying obstruction inducing pulmonary conditions that decreases dependence of staff sustained manual manipulation of patients during upper endoscopic procedures.
*Here we narrow the scope of our population emphasizing that these individuals will eventually require intubation if the obstructed airway is not cleared and respiratory depression persists. Moreover, this needs statement clarifies that the problem is specifically correlated to upper endoscopic procedures.
Iteration #3:
A way to minimize airway obstructions and need for intubation in patients with underlying obstruction inducing pulmonary conditions that decreases physical burden on staff during sustained manual manipulation of patients as well as number of people in procedure room at a given time during upper endoscopic procedures.
*Here we further specify the outcome of the needs statement indicating that not only is the dependence on staff minimized but also the physical burden of applying their full strength for prolonged periods of time as well as the number of people in an already crowded procedure room.
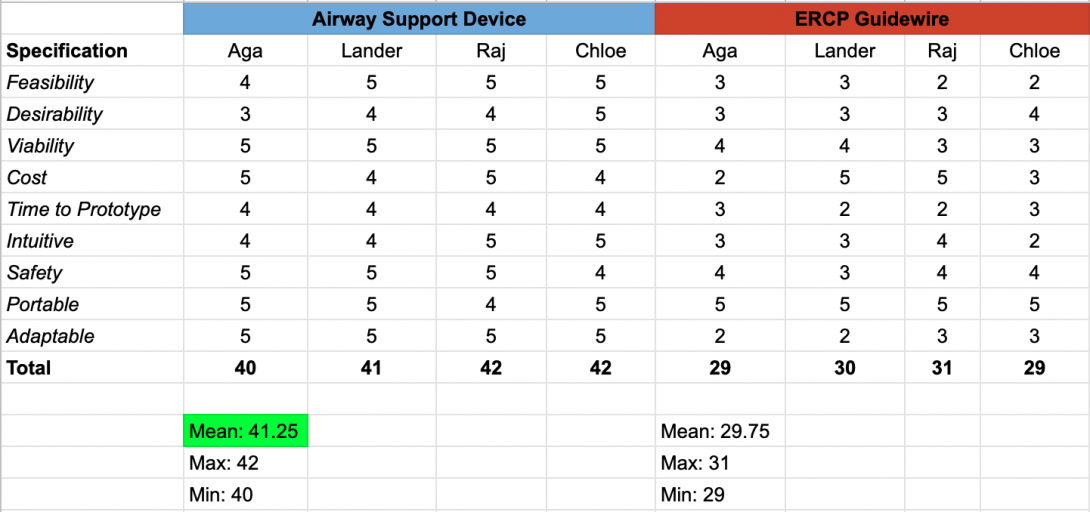
Narrowing the Scope of Our Ideas and Getting a Taste of Some Real Engineering
I can undoubtedly say that this week was a major turning point in our Clinical Immersion experience, both in and outside the clinical environment. Interestingly enough, our focus shifted from procedure observation, which was mildly placed on the back burner, to analysis, in which we were hit with a mega dose of engineering and brainstorming. In that regard, I can say, in confidence, that our brains were flooded with ideas, decisions, and outside feedback. Most importantly, this week presented us with new challenges and gave my team a valuable glimpse of what real-world applications of engineering and product development look like. In terms of narrowing the scope of our ideas and choosing a final direction, what started off with two strong competing ideas, an airway support device or a revamped ERCP guide-wire with improved control, ended in victory for the airway support apparatus. Although not a simple decision to make, my team employed a specification matrix and individual ranking system to aid us in making a final decision with which need we wanted to pursue.
-
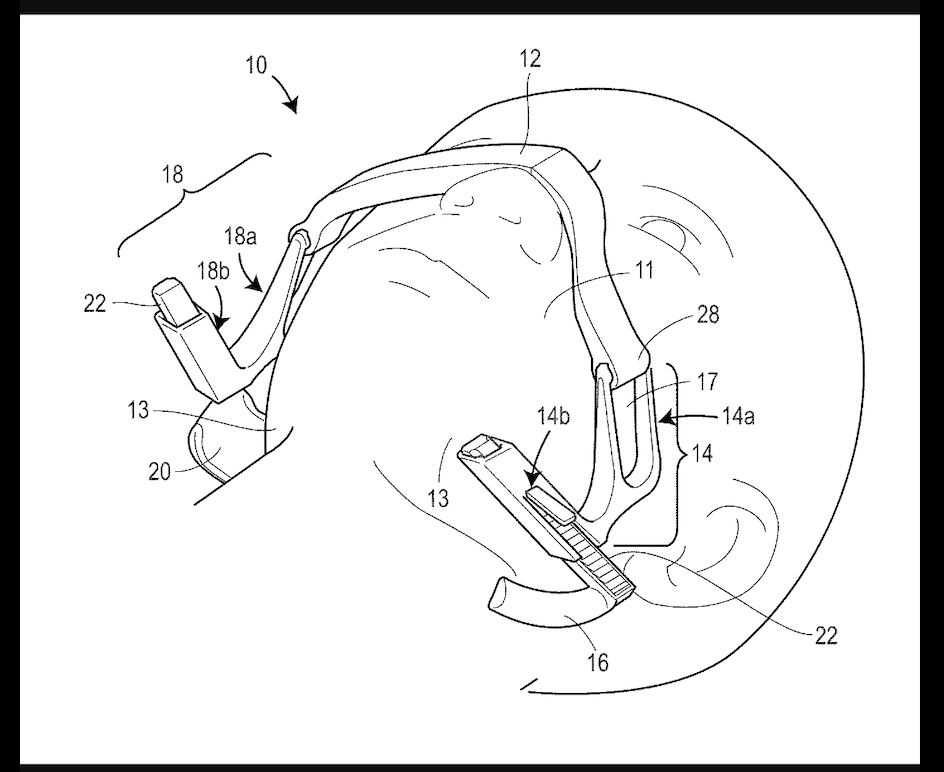
Once finalized, we went straight to the drawing board and purged all possible ideas, good and bad, as far as how a jaw thrust could be replicated in patients without the need for an individual to perform one. This process eventually plateaued as we had limited knowledge of already existing technologies, anatomical characteristics and barriers, as well as how a device, if implemented in the particular circumstance, would impact an upper endoscopic procedure. These shortcomings became the impetus to secondary research and a motivation to conduct interviews with physicians, nurses, and medical assistants to understand their first hand experiences with airway obstructions and manual jaw thrusting. After compiling all of our findings, we were able to all agree that a now abandoned patent for an airway support device initially designed by Keven Ward et al. from the University of Michigan would be the source of our preliminary concept. Although not exactly what my team and I envision for our final solution, this is an approach that we will certainly consider as we continue to develop a prototype.
-
Knowing the parameters of our needs statement, we have determined a set of criteria and restraints that we would like maintain in our prototyped model:
Criteria
- Device should be disposable
- Device should perform on a universal standard in all types of procedures where oral intervention is required
- Device should be portable
- Device should be manufactured for under $100
- Device should take less than 1 minute to set up
- Prior to use, device’s performance should be evaluated relative to individual patient criteria
- Device should be intuitive to use by anyone in the procedure room
- Device should maintain selected end-range position until relax or change is desired
- Device should be rapidly adjustable for variation in anatomical structures such as face width or desired strength of jaw thrust
Restraints
- Device should not require an external electrical power source
- Device should not induce harm, cause pain or prolonged strain to patient
- Device should not apply more than 17N of force to either jaw*
- Device should not apply more than 24N of force to mental protuberance*
*Deshpande et al, University of Illinois, “A Novel Design for a Jaw-Thrust and Head Immobilization Device and its Successful Testing Using a Human Simulator”
Conceptualization of Jaw Thrusting Apparatus
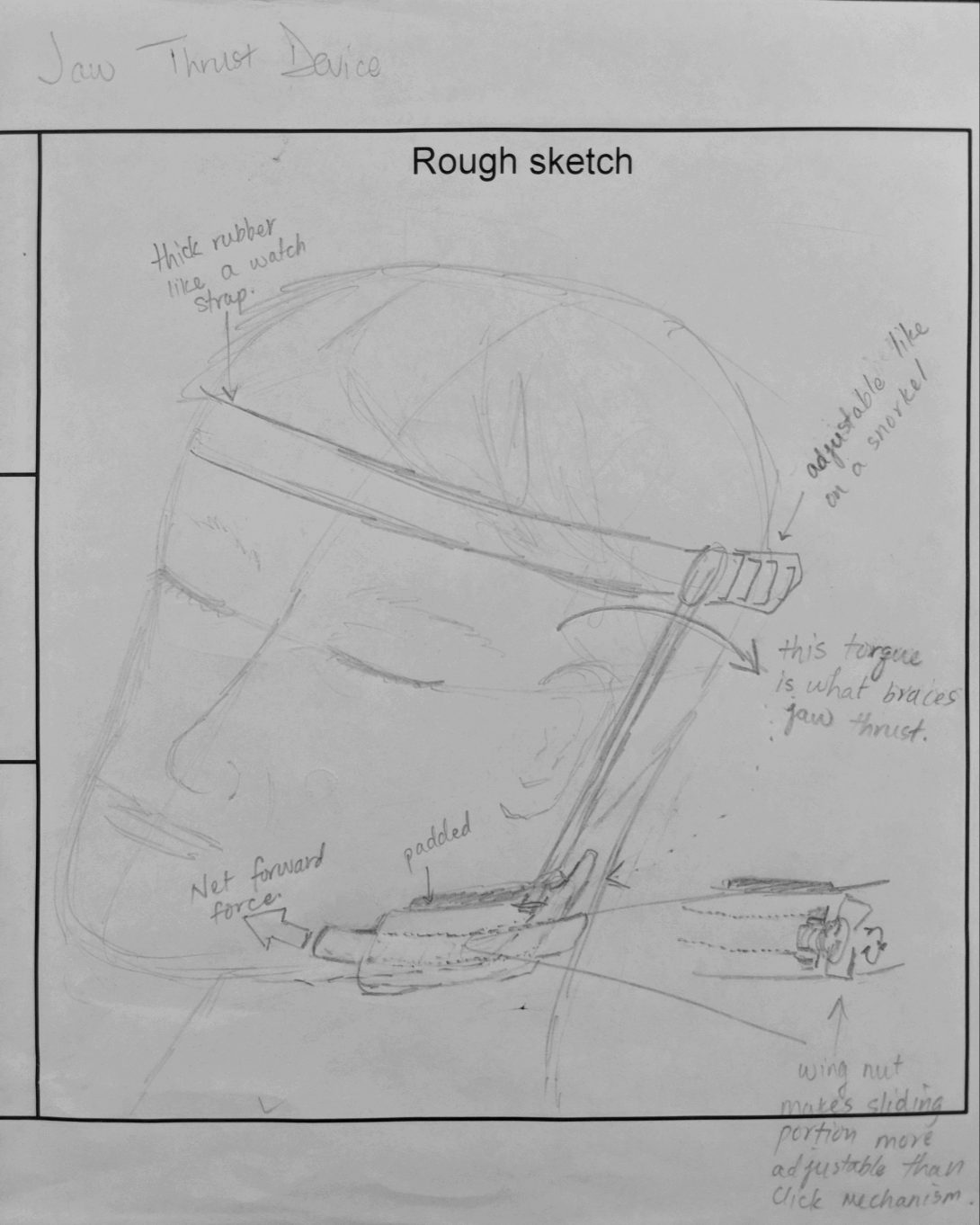
This week was geared toward finalizing the direction of our project and using the criteria and specifications we defined last week to begin the early design stages of our system. The insight and feedback we received from Dr. McGorisk, Dr. Trivedi, staff nurses who administer sedation drugs during procedures, and other hospital staff who have been involved in patient jaw thrusting situations, served as a valuable tool in helping my team and I realize what aspects would be desired in the final product. For instance, there was an emphasis on keeping the apparatus adjustable for varying anatomical facial features, fast to apply, and low-cost to make. We were even given the idea to define a metric that would determine which patients would be at risk for airway obstructions and who would most likely benefit from the device. With that said we hit the drawing board, both figuratively and literally.
With the existing patent in mind, although we were confident that our design would have to be secured on the front of the face, we felt that using the nose as a fulcrum for device support posed a risk for discomfort and even pain. Moreover, we wanted to minimize any other components that would disrupt the physician’s working field near the mouth so moving the support mechanism to the forehead would be most effective. We were also in agreement that the strap should be adjustable or even stretchy and that a support bar extending from behind each ear to the jaw pushing component would provide the forward thrust needed to clear an airway obstruction. Knowing that the amount of thrust should be determined on a patient-by-patient basis, we also felt that a screw-to-tighten mechanism would work best when trying to increase force on the jaw and optimize results. Furthermore, designing well- contoured jaw cups would maximize jaw surface area contact and result in a more effective and comfortable jaw thrusting maneuver. Generating these initial concept ideas gave us a platform to translate the thoughts we had on paper to a tangible design.
Prototyping (Low Fidelity > High Fidelity)
As most devices aiming for success begin with low fidelity popsicle stick and pipe cleaner models, our arts and crafts skills were put to the test over the next several days. We dedicated our time to tinkering with elastic resistance bands, wooden dowels, styrofoam, hot glue and foam padding until we gathered a clear enough idea of what our final product would look like. Following several iterations of our basic design, we began the search for CAD components that we could 3D print to ramp up our fidelity level. Eventually we 3D printed a pair of ladder-lock buckles, and designed multiple versions of our own jaw cups using CAD software. Once satisfied with the cups, we turned our attention to developing a screw-to-tighten mechanism using nuts and bolts that would be braced against a rigid bar following the lateral side of head allowing for intuitive thrust level adjustment.
Moving Forward
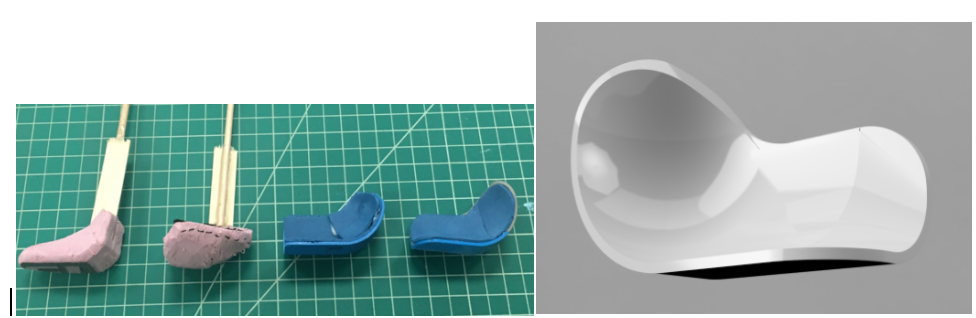
Moving forward, in the final week of the program, we hope to revisit our prototype and ensure that the support bar maintains rigidity during patient movement and during the entirety of a procedure. We also aim to define a metric to determine which patients would need the device as well as further contemplate whether or not a strap only extending across the forehead is enough to sustain full tension and thrust or if a full-circumference strap is ultimately required to achieve adequate support.
Although still far from mass manufacturing and investing in a start-up space, my team and I are optimistic that our invented apparatus could serve as a low cost, effective, innovative and impactful alternative to staff maintained manual manipulation of patients and decrease the physical burden that it has on hospital staff.