Daniela Merlos
Daniela Merlos

Basic Information about Student (Small Background introduction)
Year: 4th, Senior
Area of Research:
Contact Information: dmerlo3@uic.edu
Blog
Merely Observing...

This first week under Dr. Ramanathan’s supervision, my team was able to observe several procedures in a variety of settings including the clinic, OR and procedure rooms. My team was heavily focused on observing and recording all items considered relevant to the AEIOU framework, while still seeking for good and bad designs.
On the second and third day of the Clinical Immersion, my team was alternating in pairs to sit in on clinical visits. Dr. Ramanathan was able to provide medical attention to her patients but also educate us on steps done in procedures like IUD insertions and pap smears
On the fourth day, my team was able to sit in on a total of three, OB/GYN-related, surgical procedures. That day provided insight into the workings of the OR and ICU, where most operations were observed from start to finish. The tools and interactions made by the surgical staff provided a better understanding of roles and responsibilities -lending to a better assessment for areas of improvement.
On the fifth day, Dr. Ramanathan had my team shadow her colleagues in their procedure rooms. The procedures done on this day helped to provide further observation of tools and equipment used for, do I dare to say, “less invasive” procedures.
The designs that my team evaluated ranged from room color scheme to surgical tool handling. Here is a list of just a few.
Good designs:
- Clinic: calm, light color schemes
- Clinic: Medical Assistant & Physician teamwork in procedures to maintain sterility
- Clinic: 7 rooms and 7 sonographers for ultrasound
- ICU: spacious and accessible layout
Bad Designs:
- OR: cable/outlets pose tripping hazard
- OR: surgical drapes must be altered to fit incision
- Clinic: bed/chair no support for patients to lift themselves
- Clinic: cluttered consultation rooms
- Procedure Room: tools and devices uncomfortable for doctors’ use
- OR: collecting and assessing blood loss
Storyboard: Vaginal Wet Mount
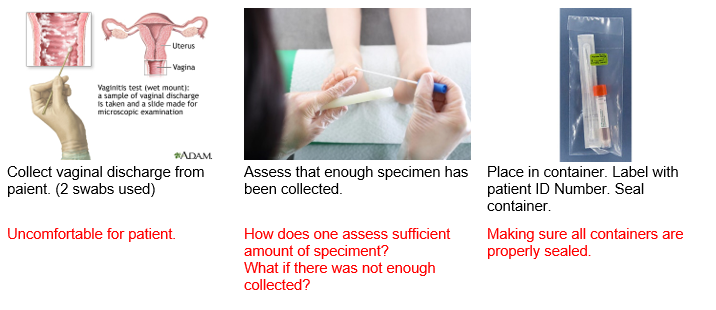
Steps 1-3
Row 2
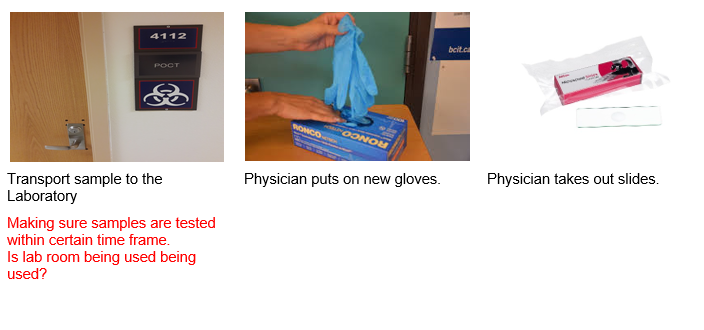
Steps 4-6
row 3
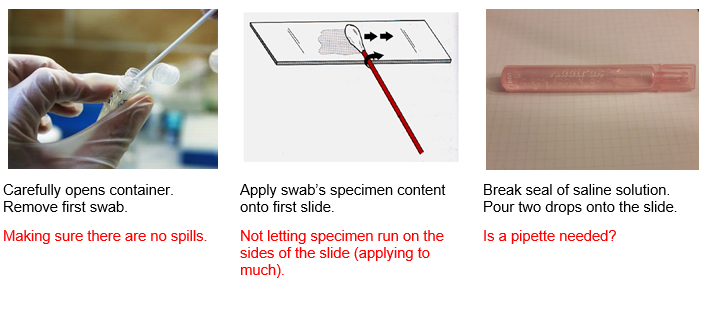
Steps 7-9
row 4
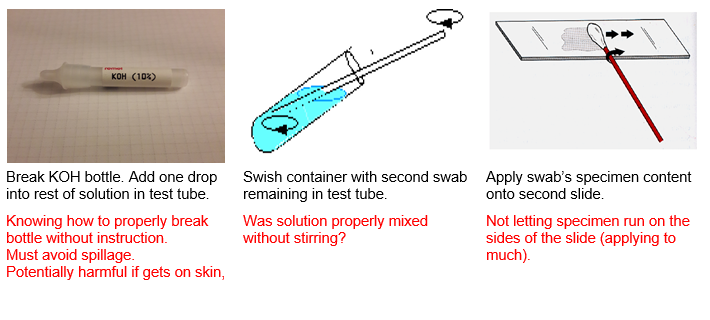
Steps 10-12
row 5
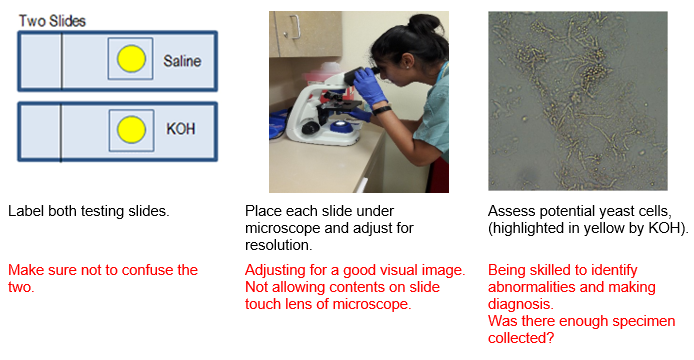
Steps 13-15
Creating the Needs Statement

After three weeks of intense observation and recording following the AEIOU Framework, our team was finally selecting an area of focus. This part was perhaps the most difficult part. However, we saw that in the surgical rooms there was a need for the sizing and application of the drapes. Please refer to the following needs statements:
Iteration 1:
A way to address draping in patients during surgery that provides ideal surgical area.
The problem with this need statement is that most key terms to describe population and problem are very broad. In fact, there is no clear outcome expressed in the statement as well. Population is merely defined as patients. The problem is merely defined as providing ideal surgery. What is d
Iteration 2:
A way to address the need to cut surgical drapes to better expose incision area for patients in surgery that does not minimize the adhesive property of the drape against the patient’s skin in cutting the drape.
The problem with this need statement is that the outcome is clearly stated and is very specific.
Iteration 3:
A way to minimize the loss of time and adhesive properties that result from the cutting of standard-sized surgical drapes to fit an incision area in patients of different stature during various gynecological surgical procedures.
Concept
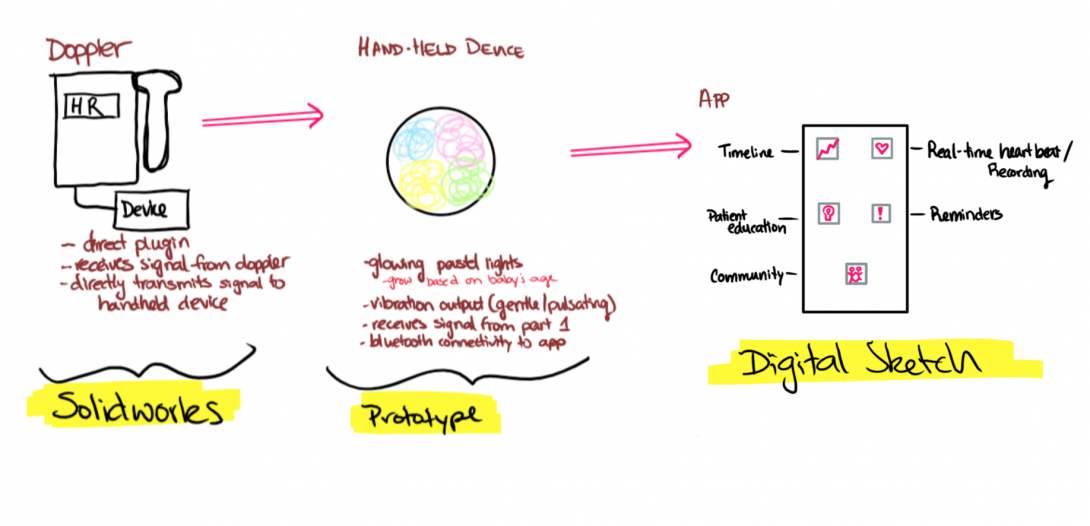
Background: The idea originated in the OB/GYN Clinic where we saw the lack on interaction experienced by a deaf pregnant patient who came in for a regular clinical visit. She is unable to hear her baby’s heart tones, so the nonideal alternative would be to have her place her hand on the end of the Doppler Sonoline to feel the pulsing. However, she was unable to detect the pulsing emitted through the handle. We spoke with the patient and even allowed her to test out an app that simulated fetal heartbeat. The limitation on the interaction of this experience presented itself as an area of interest for my team. Afterwards, we continued research and interviews to facilitate the design criteria and specifications of the prototype.
Problem: method to improve interaction
Population: deaf pregnant mothers and their fetuses
Outcome: increasing of maternal involvement in prenatal care
Key Components:
- Component 1: Attachment to doppler and transmits sound.
- Component 2: Device that has friendly appearance and has interactive output: vibrational motor and LEDs. It display fetal heartbeat in real-time
- Mobile App: a hub that has many neat features related to prenatal care.
Design Criteria
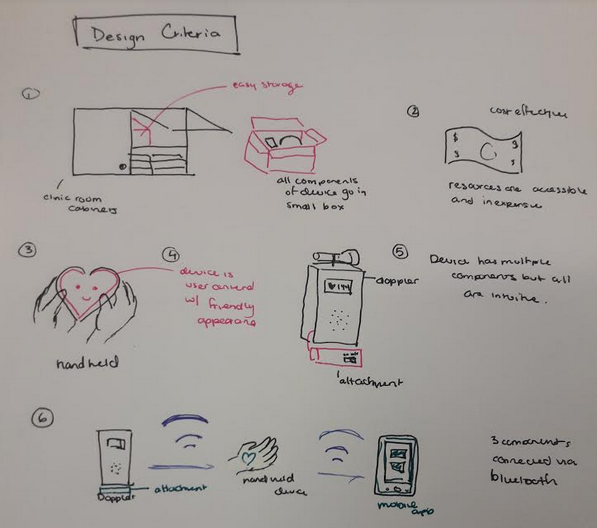
It has been a truly incredible experience, thus far. We have learned so much under the supervision of Dr. Ramanathan and her colleagues. At this point, my team and I had finalized the need statement and began the initiation of designing potential solutions that would cover the need statement. After the idea to explore the enhancement of maternal experience in prenatal care for deaf pregnant women became our focus, we consolidated and refined the designs for our prototype. We came up with the following criteria as critical factors to remain in all revisions of any design.