Jacob Gasienica
Jacob Gasienica

Year: Senior (BioE)
Area of Research: Urology
Contact Information:
jgasie3@uic.edu; jgasienica17@gmail.com
Blog
First Day on the Job
Today was the first day on site. We tested…………
picture
picture

blog
And the story continues as such…
Testing Day
As we continued out research on…..
First week in Urology:

In my first week in the Urology Department, I was pleasantly surprised by how much I enjoyed observing in this field. I was also surprised by how much bioengineering innovation is utilized within the clinic and in the operating room. This department is highly adaptive to advances in bioengineering and technology and provides cutting-edge patient care.
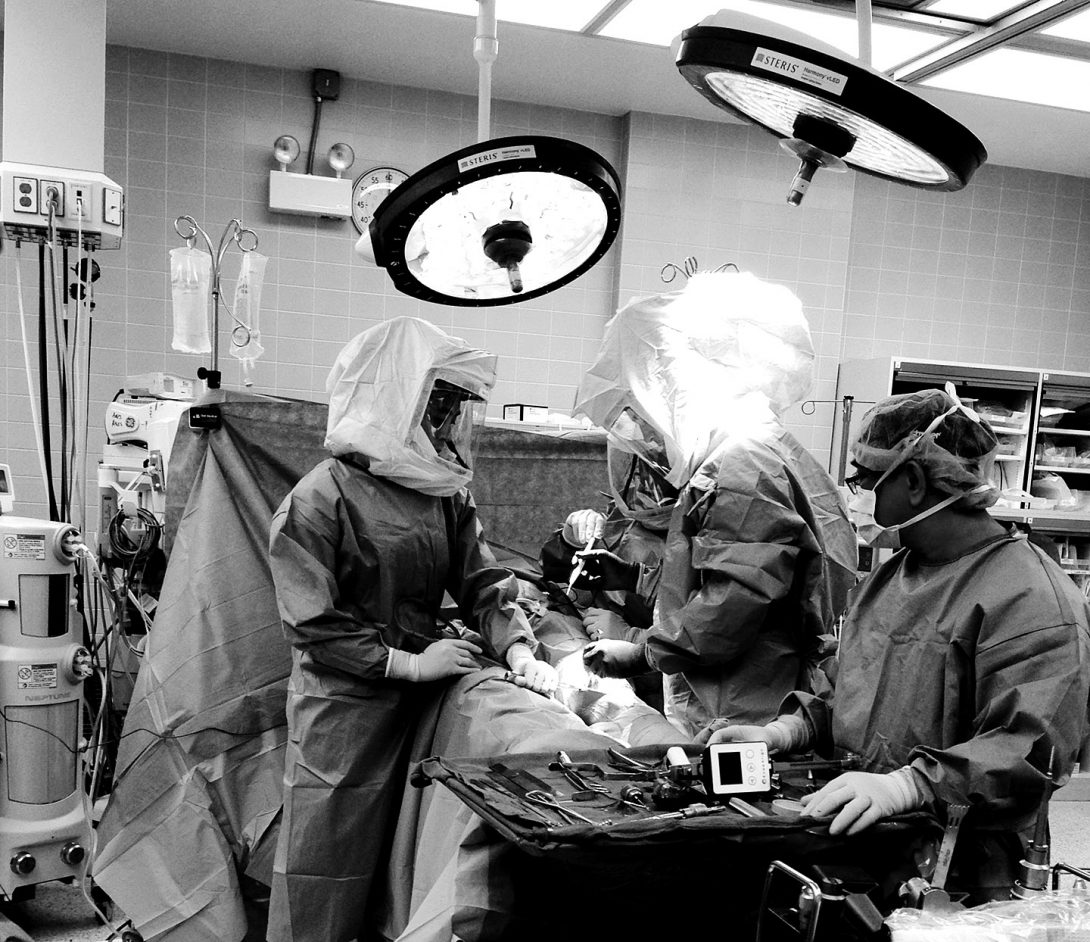
With regards to good engineering I observed during my rotations this week, a notable example would be the single port da Vinci robotic surgical system for performing a nephrectomy. The device requires a single incision through which a camera and three rotatable, exchangeable arms can enter the body to perform the operation. From a remote operating station (see the above image), the surgeon can control the robot to precisely make the incisions to detach the kidney. By exchanging the detachable arms of the robot, the robot can then also be used to bag the kidney; pulling the robot out of the incision, the surgeon could then grab the bag and pull the kidney through the same incision. This system allows for this complex operation to be performed without the need for an open surgery. In the hands of a trained surgeon, this system can be used to navigate around the body and make minimally-invasive precise changes. Drawbacks to this system include its price and the extensive training required to utilize it effectively. In all, this system is a bioengineering feat which greatly advances our surgical capabilities, specifically in urology.
A bad engineering example includes the biopsy gun utilized for transrectal ultrasound-guided prostate biopsy. This technique is used to screen for prostate cancer. Using the ultrasound probe, the prostate can be located and locally anesthetized. Through the probe, a biopsy gun can be inserted and is used to collected 12 samples. Thus far, this may seem like a well configured process; however, the issue presents itself in the noise produced by the biopsy gun. When a sample is collected, the spring-powered biopsy gun lets out a loud snap which a majority of time causes the patient to be startled. Even though they are anesthetized, the noise alone can cause significant distress for the patient. This has been known to lower patient satisfaction, and I noticed that their movement requires that the physician reposition the probe after each collection, taking additional time. The overall experience for both the physicians and the patients would be significantly improved by developing a quieter biopsy gun.
Storyboard for transrectal ultrasound-guided prostate biopsy
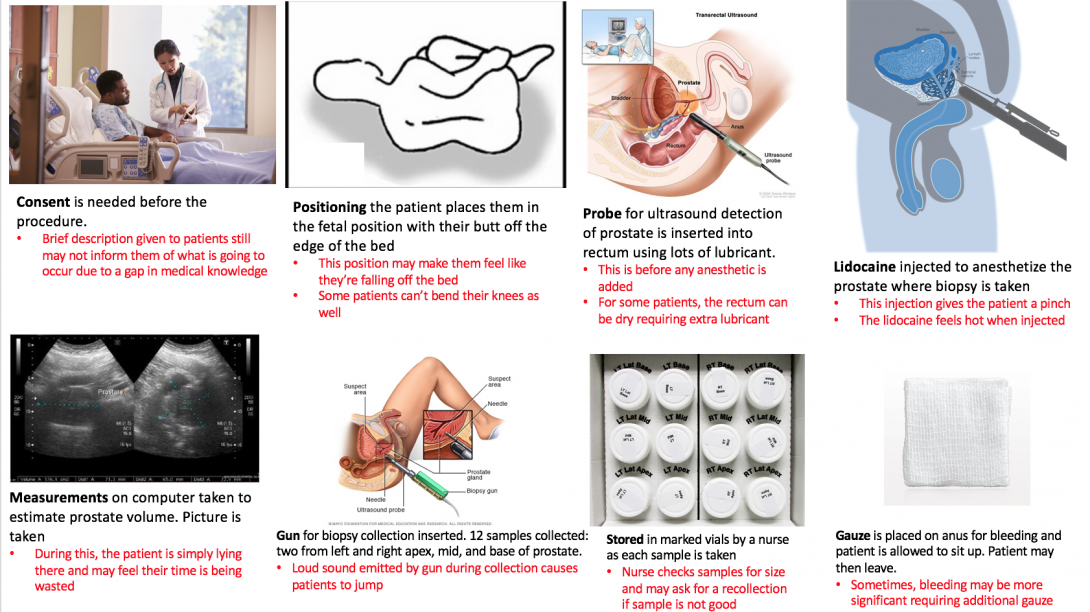
A transcrectal ultrasound-guided prostate biopsy is a procedure performed for random screening of the prostate for cancer. It is random as the samples are collected from 6 generalized locations on the prostate: left apex, left mid, left base, right apex, right mid, right base. In most cases, patients undergoing a prostate biopsy have already underwent a protein specific antigen test (PSA), a highly sensitive yet none-specific test which tells the physician something might be going on with the patient’s prostate. The three most common causes for a heightened PSA is 1) an enlarged prostate due to aging 2) a prostate infection or 3) prostate cancer. In order to eliminate prostate cancer as the cause of the high PSA, this random prostate biopsy is performed. The samples collected are sent to the lab where they are analyzed specifically for the presence of cancer.
Websites from which images originate
Sources for images from left to right:
- https://formfast.com/top-6-reasons-healthcare-organizations-should-automate-the-informed-consent-process/
- https://www.researchgate.net/figure/Patient-positioning-1-Left-lateral-position-patient-on-his-left-side-with-legs-flexed_fig3_244989280
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/endorectal-ultrasound
- http://www.procure.ca/en/2018/06/28/scared-stiff-prostate-biopsy/
- https://www.researchgate.net/figure/Dimensions-used-to-measure-prostate-volume-by-trans-abdominal-ultrasound_fig8_291748115
- https://www.mayoclinic.org/tests-procedures/prostate-biopsy/about/pac-20384734
- https://www.dpmginc.com/supply-orders/
- https://www.qosmedix.com/intrinsics-4-ply-gauze-pad-93301
Forming a need statement
This week, the major focus was writing tentative needs statements from which the scope of our observation in clinic could be focused. Below are three iterations of a need statement relating to the transrectal ultrasound-guided prostate biopsy procedure performed with patients suspected to have bladder cancer. With all changes made through this iterative process, the rationale for the changes made are provided.
1. A device to obtain a prostate biopsy sample in patients suspected to have prostate cancer that increases patient satisfaction with the procedure.
2. A method to obtain a prostate biopsy sample in patients suspected to have prostate cancer that increases patient satisfaction and compliance with the prostate biopsy collection process.
• “Device” was changed to “method” to be more all-encompassing. Rather than changing the device for the sample collection, perhaps a change is required for the more general process of prostate biopsy. Also “compliance” was added as it is an important outcome that patients come in for their biopsy in order to screen for prostate cancer.
3. A method to obtain prostate biopsy samples in patients whose PSA test result is greater than 4 that increases patient satisfaction and compliance with the prostate biopsy collection process.
• “Sample” was changed to “samples” to allow for the possible case in which multiple biopsy samples are acquired simultaneously. Also “patients suspected of prostate cancer” was changed to “patients whose PSA test result is greater than 4” to narrow the population of interest.
Analyzing the need
This week, we were majorly tasked with analyzed our selected need, the transrectal prostate biopsy gun, and develop criteria for a solution concept to fulfill. This criteria took the form of product requirement definitions (PRDs) which we wrote as quantitative metrics by which our device can be constrained. We then used these criteria to refine some brainstorming. The PRDs provide a filter through which ideas which were generated during brainstorming can be refined. Below are the PRDs which were written for this need:
- The device shall be used for prostate biopsy.
- The device shall be used in clinic on patients who have a PSA over 4.
- The device shall collect biopsy cores one at a time.
- Each region collection (RA, RM, etc.) shall take at most one minute.
- The device shall be operable by one physician.
- The device shall fit within a 5000 cm^3 volume, excluding the length of any needles.
- The device shall be spring-loaded but also contain an electrical power source in the form of a battery.
- Any electrical source (ie. battery) shall last at least 2 hours.
- The device body shall be plastic and any needles shall be metal.
- The device shall be no louder than 50 dB.
- The device shall cause patient to lose no more than 5 cc blood.
- The device shall weigh no more than 1000 g.
- The device should allow concurrent use of a transrectal ultrasound transducer.
Utilizing these criteria as a filter, our initial ideas from brainstorming were refined down to an enhanced biopsy gun used concurrently with ultrasound. The actual mechanism and specifics by which the gun operates were a major point of brainstorming. We considered spring-powering, electrically powering, or magnetically powering the biopsy mechanism. We also have considered methods of loading vials directly into the gun itself so that a core can be stored immediately following its collection, requiring less personnel to perform this collection. We thought of the use of padding or some form of gel to prevent the sound from going over 50 dB for each core collection. We also considered several mechanisms for allowing the physician to cock the biopsy gun with one hand which allows him or her to maintain the other hand on the ultrasound probe. This could be a sort of hammer mechanism which the physician could reach with a thumb. Altogether, the PRDs we developed led us to think that the best concept would be a reiteration on the current biopsy gun procedure used, improving the major flaws we found with the current standard.
Conceptualizing a better prostate biopsy
Last week, our team had mulled over the many needs we found during our time observing in the Urology clinic and OR at UI Hospital. Ultimately, we decided that the most impactful and tractable need was the transrectal ultrasound-guided prostate biopsy procedure.
While developing the criteria and specifications for our improved concept, three major areas in need of improvement became clear: the sound of the device, the ergonomics/ease of physician use, and the speed with which the device can complete the procedure.
Our subsequent conceptualization focuses on these three areas, and we developed crude concepts to address each. Firstly, upon further investigation of a biopsy gun that is currently used in the hospital, we discovered that the loud sound was a product of two plastic components coming into contact when the gun was fired. Therefore, the simplest concept was to place some sort of shock-absorbing material between these components to mitigate the sound. Secondly, using the insights of several urologists, we determined that the rotating mechanism used to currently ready the gun for firing was ill-suited to a physician wearing latex gloves covered in lubricant. Thus, we propose a pull or cocking mechanism which should allow the physician to more easily and swiftly ready the biopsy gun. Lastly, I had noticed that with each biopsy core collected, the gun had to be removed from the patient so that the core could be stored in a vial. This procedure necessitates the collection of 12 cores; therefore, it is easy to see how this constant removal and replacement delays the end of the procedure. We conceptualized a method to quickly extract the core sample once it is acquired such that the biopsy gun can be left inside the patient and more quickly collect all samples.
We then scheduled a meeting with a urologist mentor, to present our concepts and receive feedback. He advised us to focus on prototyping one of the aforementioned concepts due to the limited time frame of this program. He went on to say that the issue of sound was the most inviting area for us to prototype. Taking his advice, we did just that. We had two biopsy guns with which to conduct simple experiments to prove our concept. One biopsy gun was left intact and served as our control. Using a decibel-measuring application, over several trials, we determined the original biopsy gun to emit sound at an average of 106 dB. Using a soldering iron, we were able to melt and remove a panel on our test biopsy gun to reveal the two plastic components which were making contact and emitting the sound. In the sparse materials we had available to us, we found some foam, which we preceded to place between the two plastic components. We then ran several more trials and determined the padded gun to emit sound at an average of 96 dB. Thus, with just the miscellaneous materials we could acquire, we were able to reduce the sound emitted by an order of magnitude. Reiterations of this design utilizing viscoelastic materials in the place of the foam should be even better able to mitigate the sound.
While this was simply a proof-of-concept, a final prototype would need to be changed further to maintain the mechanics of the biopsy gun itself. As we are effectively shortening the firing chamber with our padding material, a final prototype would either require this chamber to be lengthened or the needle itself to be lengthened. The amount of length required would be equivalent to the width of the padding placed in the device.
Below are images showing our initial concept images. The second set of images depict the inner mechanics of the prostate biopsy gun, as well as the altered gun.
Image: Concept Card Quieter
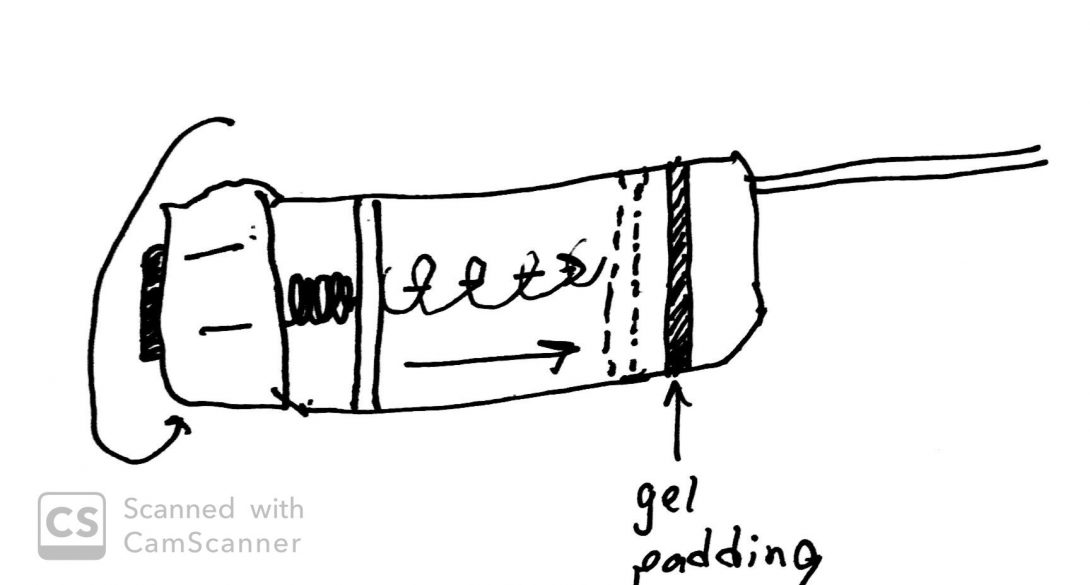
Concept for improving sound characteristics of the biopsy gun
Concept Card Ergonomics
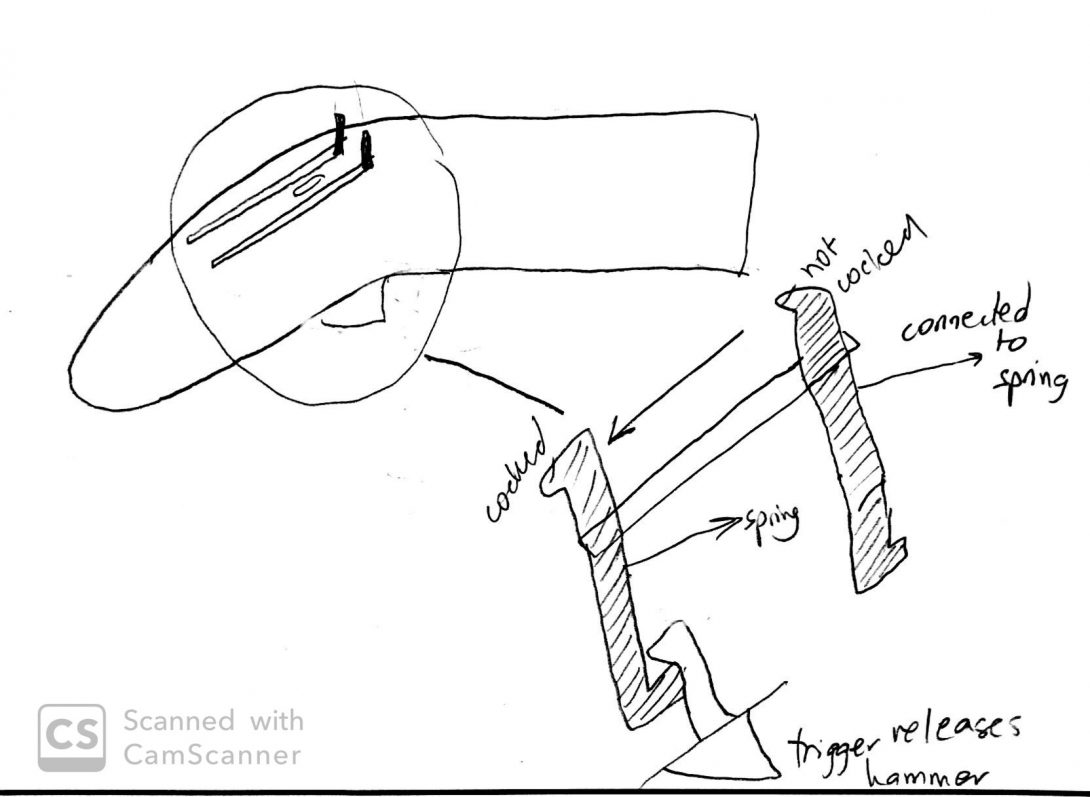
Concept for improving physician’s ease of use of the biopsy gun
Concept Cards: Speed
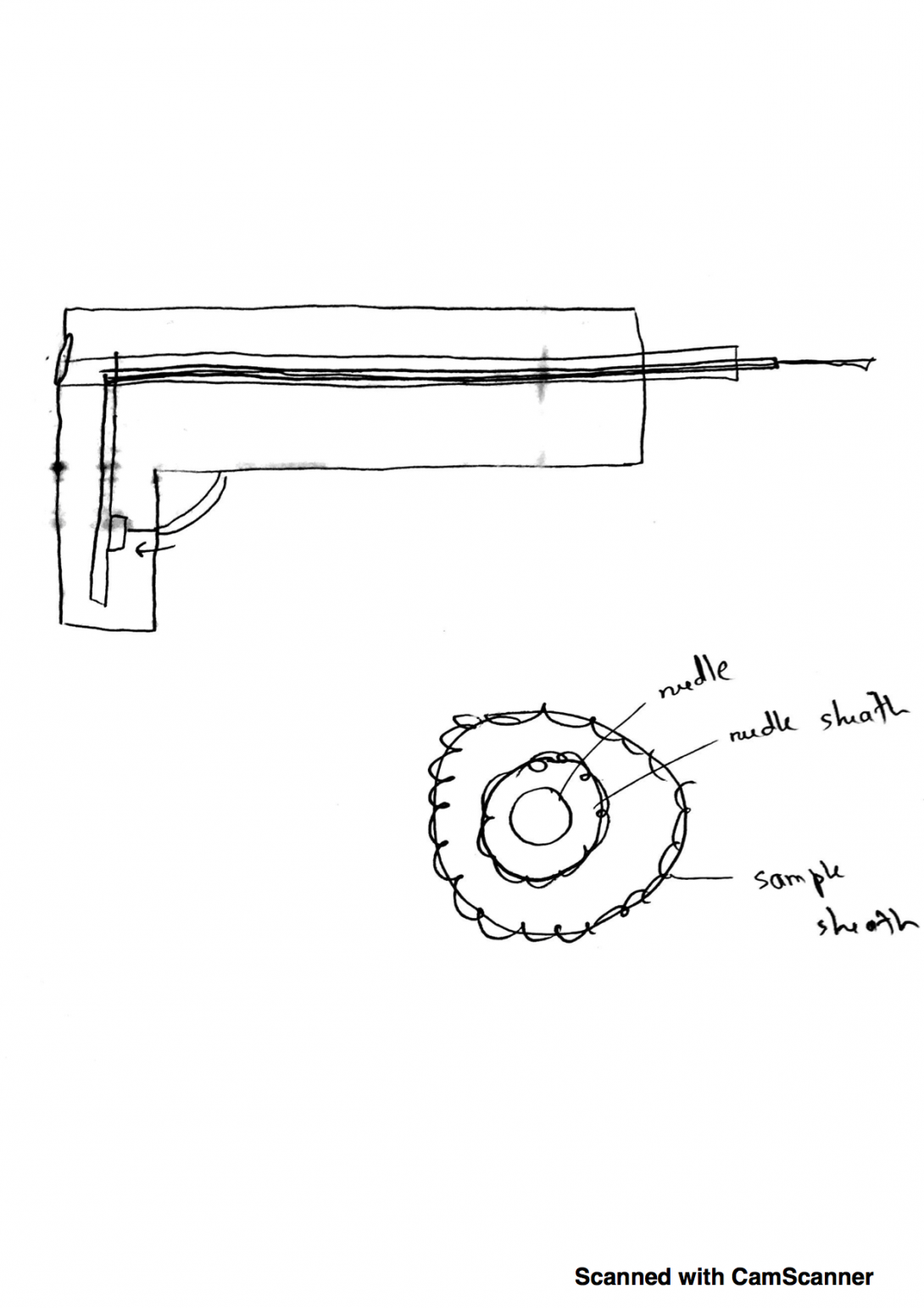
Concept for improving the speed with which the biopsy gun can acquire samples
opened gun
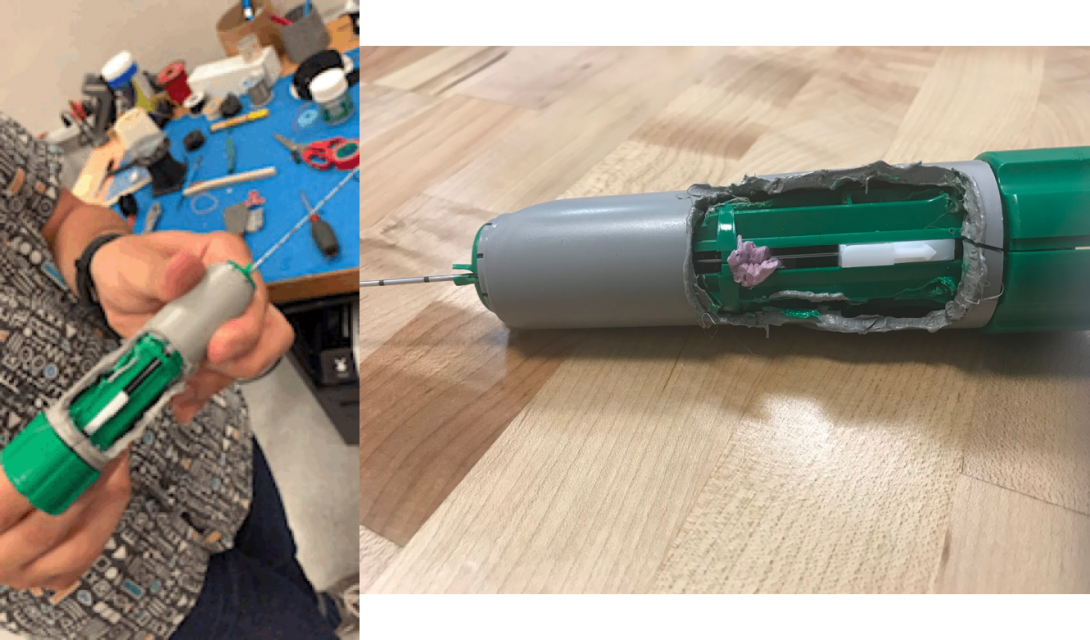
The inner mechanics of the biopsy gun revealed (left) and the addition of foam to mitigate escape of sound