Jailene Silveri
Jailene Silveri

Biography:
Jailene is native Illinoian born in Chicago but raised in small town Channahon. She is a 4th year UIC undergraduate student pursuing a Bachelor of Science in Bioengineering with a concentration in Neural Engineering, all in preparation to receive a Master’s in Bioinformatics at UIC in the near future. Jailene enjoys drawing realism, hiking, rock climbing, weightlifting, and eating good food.
As of now, Jailene conducts research with Dr. Hetling, UIC Associate Professor & Director of Bioengineering Undergraduate Studies, at the Neural Engineering Vision Laboratory (NEVL), assessing the application of therapeutic hypothermia to reduce retinal ischemia following traumatic injury to the eyes.
During the extent of the Clinical Immersion Program, Jailene will be participating in the Pulmonary Critical Care Unit.
Year: 2021
Area of Research: Neural Engineering and Bioinformatics
Contact Information:
jsilve2@uic.edu (Email)
Jailene Silveri LinkedIn (Professional Profile)
Blog
Embarking on a New Journey
Over the course of this first week, I encountered another world hidden behind concrete walls, overwhelmed with chatter, buzzes and bings, and clanking footsteps. Fortunately, I had only visited the hospital a few times in the past for personal appointments or to see a beloved; however, I had never wandered past the wide, clear doors embellished with the words “Restricted Access.”
On Tuesday, Dr. Dudek, Chief of the Pulmonary Critical Care Department, introduced himself and provided a brief (roughly 2-hour-long) discussion pertaining to the complications he had encountered within the hospital. It was a bit funny to all of us at first, considering that Dr. Felder explicitly told us that the doctors had been informed to guide the students instead of spoon feed them solutions, but the conversation delivered an insightful perspective as to what we would be dealing with during these 6 weeks. After the meeting, we were left to venture on our own to meet the attending physicians, fellows, and nurses buzzing around the MICU (Medical Intensive Care Unit). Within the entire week, we had tentatively made our way into the MICU, Outpatient Care Clinic, Sleep Center Clinic, and Pulmonary Function Testing (PFT) Lab.
Good Design: In the Outpatient Care Center, most of the patients admitted have some variation of Chronic Obstructive Pulmonary Disease (COPD) or asthma. Essentially, patients struggle to either exhale or inhale the air within their lungs, respectively. As you walk through the hallways, you will see a variety of posters pinned up for the patients to learn about what respiratory treatments may work well for them. The posters are formatted to preview the most common and popular medications, noting the brand and type of delivery system for each, in color categorization. Likewise, large diagrams demonstrating the general strategy utilized to properly operate these delivery systems were scattered along the walls as well.
Bad Design: In the MICU, residents lug around this large, cumbersome work station on wheels (WOW). The primary function of these mobile units is to electronically access patient medical records and display pertinent exams or charts for the attending physician to review. Honestly, the implementation of this cart is pretty impressive. However, it’s clunky and, at times, obsolete, considering that the operator of the machine must swivel the station around for the rest of the team to see the displays. Moreover, nothing regulates the foot traffic that crowds the MICU, so maneuvering large devices and machineries will only further the present overcrowding.
In short, this summary presents only a fragment of good and bad designs implemented within the clinical setting. But for now, we’ll see what I can observe and absorb within week 2!
Tales of a Little Spirometry Test
Spirometry Test: This procedure measures the amount (volume) of air and speed in which you can move air into (inspiration) and out (expiration) of your lungs. While the measurements are taken, a graph visually displays the results. From this graph, doctor may diagnose pulmonary diseases depending on certain abnormal patterns.
During the first and second weeks of observing the Outpatient Care (OC) Clinic and Pulmonary Function Testing (PFT) Lab, all of us were fortunate enough to witness spirometry tests. At the OC, the spirometry tests were given through a small hand held device versus at the PFT Lab, the spirometry test performed consisted of larger equipment with more advanced capabilities to measure lung capacity.
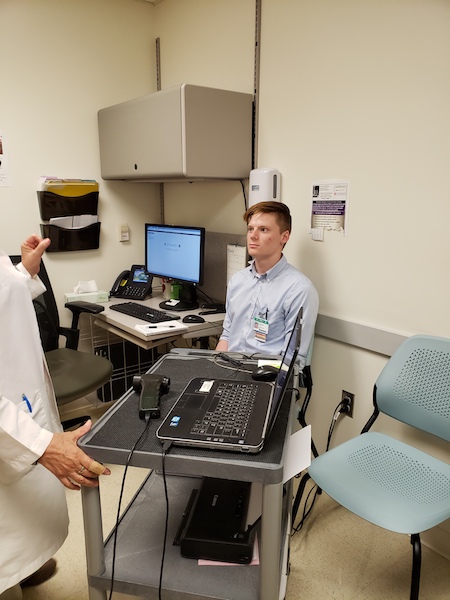
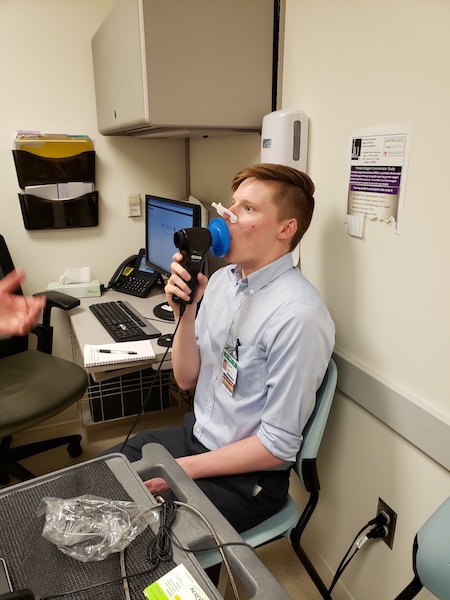
The following storyboard provides an account of our very own student (Colin, BIOE) performing a spirometry test.
Step 1: Greeting the Patient and Procedure Briefing
Step 1
Step 2: Prepping the patient
Step 2

Step 3: Normal Breathing
Step 4
Step 4: Quick Inspiration, Rapid Expiration
none
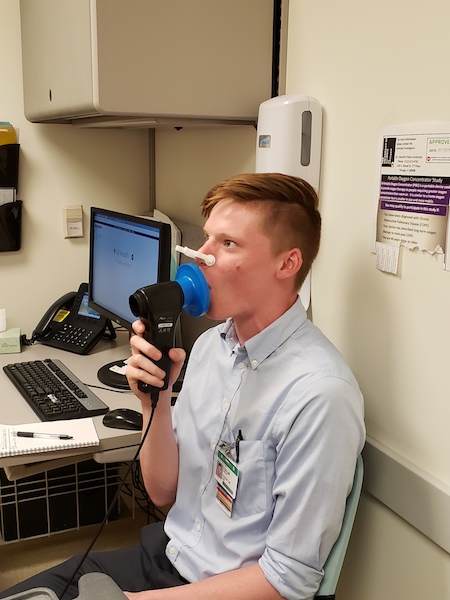
Step 5: Maximum Expulsion of Air
none
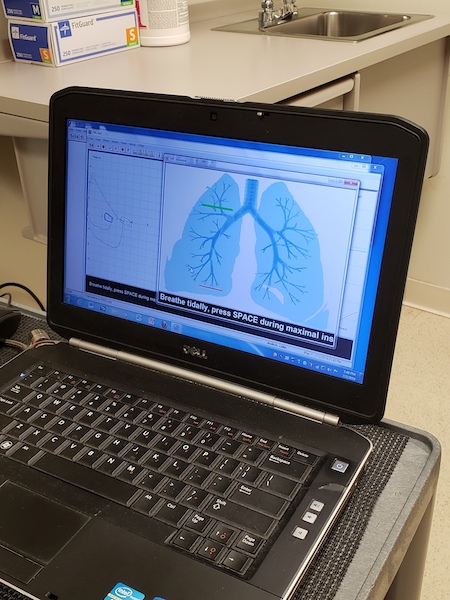
Step 6: Immediate Results
none
Diagnosis utilizing following flow curves:
none
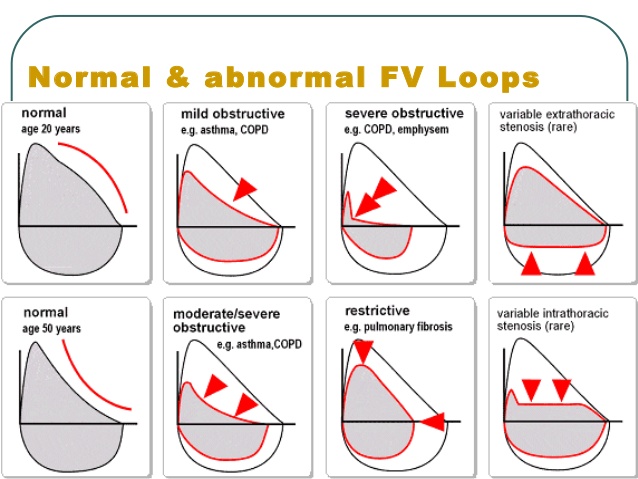
Take home: Although this procedure is non-invasive, many of the patients, especially those suffering from Chronic Obstructive Pulmonary Disease (COPD) or asthma, may feel exhaustion accompanied with lightheadedness. In the past, some patients have passed out from their efforts. Consequentially, the nurse/technician would have to administer “smelling salts.” Thus, this method may prohibit the effectiveness of the test and attaining adequate measurements.
In Need of a Need
Although working within the Pulmonary Critical Care Unit has been quite educational, our group has been scavenging the ICU hallways for potential project leads. To be honest, most of the problems we have targeted have already been solved simply by the means of money. At UIC, some of the equipment demonstrating low performance can easily be replaced by more advanced technology, yet the budget set out to acquire these new toys seemingly shrinks more and more each day, rendering innovation impossible.
So, we took a step back to re-evaluate what produced the highest hanging fruit for us to dissect and analyze. None of the procedures we observed at the ICU were up for a face-lift, but at the Sleep Center Clinic, we had one project worthy of renovation: the CPAP and BiPAP machine customizability.
1st Iteration: A method to administer adjustable non-invasive ventilation to treat individuals suffering Obstructive Sleep Apnea
- “non-invasive ventilation” is rather ambiguous, as there are many forms of ventilation prescribed for treatment
- Problem: OSA patients need breathing support–>Already an identified problem. This need can be refined
- Target population: individuals suffering from Obstructive Sleep Apnea
- Outcome: none
- This iteration needs to focus a bit more on the patients’ needs and focus on a delivery system that ensures a positive patient experience
2nd Iteration: A customizable mask designed to timely dispense gradual increments of positive airway pressure to treat individuals suffering from Obstructive Sleep Apnea and to promote patient-compliancy
- “customizable mask” pigeon-holes us into approaching this need by one method: through a mask
- Problem: in this case, a mask that can ramp up airway pressure at pre-determined times–> This idea has already been proposed and has failed many individuals
- Target population: individuals suffering from Obstructive Sleep Apnea
- Outcome: patient compliancy with method–> No consideration for comfort or quality of treatment/patient experience
3rd Iteration: A method that affords customizability for patients with Obstructive Sleep Apnea designed to gauge patient sleep patterns and auto-adjust gradual increments of positive airway pressure ventilation to promote user-comfort and compliance during sleep cycle
- Although the syntax of this statement may be altered, this iteration does not pigeon-hole us into one proposed solution
- Problem: patients need something that can be customized to accommodate differences in facial/bodily proportions and something that can take feedback from their bodies to provide sufficient treatment
- Target population: individuals suffering from Obstructive Sleep Apnea
- Outcome: patients can feel more comfortable while sleeping, promoting user-compliance with such method
Defining Our Constraints
This past week had a lot in store for us to do. We were done framing the foundation to construct our project for the upcoming weeks and quickly transitioned into the analysis phase of this six-week journey. During weeks 3 and 4, we focused on Bronchoscopies, Thoracenteses, and the compliance rates for CPAP (Constant Positive Air Pressure) machine; yet, after hours of evaluation, we decided that the CPAP machine provided the highest hanging fruit in regards to our skill level as a team and the amount of time remaining to complete the prototyping segment of this program. Thus, our new agenda consisted of brainstorming, identifying the constraints of our project, and formulating the requirements outlined for our prototype.
At first, I presumed this would be second-nature since we had already spent weeks recognizing needs in hopes to attain a purposeful solution. However, after refining our Prototype Requirement Definition (PRD), we quickly realized how oblivious we were to certain aspects pertaining to patient care and the prototype’s clinical practicality. Most of our conceived “solutions” had already been in practice or were under review. So, we either had to completely reinvent treatment for Obstructive Sleep Apnea or modify the current technology to an extent in which no other competitor within the market could offer our version of precision medicine.
To start, we spent hours researching and collecting evidence needed to craft a list of our prototype’s requirements, characteristics, function, and features. The final prototype would consist of a wedge pillow with elevation capabilities and a CPAP machine capable of adjusting to real-time feedback from a third component.
Written below is the performance requirements and characteristics envisioned for our prototype system:
- The solution needs to be comfortable and should not contribute to patient irritability –> such as nasal inflammation, mouth dryness, skin irritation from abrasive surfaces
- The solution needs to work throughout the entire sleep cycle –> no systematic errors or temporary shut-downs, needs to administer continuous treatment
- The solution needs to improve sleep quality –> ensuring full progression of 90-minute sleep cycles without disruptions
- The solution needs to be customizable for each patient –> compatible with facial/bodily proportions and capable of adjusting to doctor’s prescribed settings and patient’s ideal sleeping conditions
- The solution needs to function at the patient’s home –> or where the patient currently resides
- The solution needs to be safe to use –> no tangled wires/cords/hoses, clean and smooth apparatus avoiding pinching/cutting of the skin, causing no hazardous obstacles for non-users
- The solution needs to work better than current CPAP machines –> compliance rates need to be >50%
Lastly, our features and functions for the Prototype Requirement Definition (PRD) consists of the following:
The CPAP system is intended to treat patients with Obstructive Sleep Apnea, however, incorporates a methodical approach to reducing discomfort during treatment and increasing the compliance rates of the CPAP machine. The system will include a wedge pillow that comfortably suits the trunk of each patient and slowly adjusts in elevation during the span of one’s sleep session, a wearable technology measuring a patient’s vitals to analyze stages of sleep, and a modified CPAP machine capable of modulating pressure changes based on feedback from the wearable. Under this apparatus, treatment will be tailored to each patient’s experience and preferences to effectively promote comfort during the process of falling asleep.
This system must “ramp-up” pressure settings as a patient falls asleep, detect when a patient is awake to shut off or reduce airflow, monitor heart-rate, respirations and movement, and elevate an individual to open their airway and reduce intensity of CPAP machine.
Envisioning Our Prototype
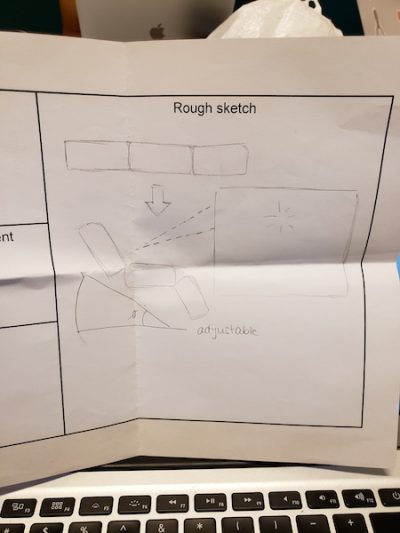
During these last few days conceptualizing and prototyping, I realized how extraordinarily beneficial concept cards have been in facilitating one’s thought process. I am an extremely visual learner who prefers audio over written descriptions to complement images and diagrams. Honestly, I spent a majority of this program watching videos that explained the anatomy and physiology of the lungs after we had finished clinical rotations because I was consumed with understanding everything that occurred beneath the skin. For my teammates, it had been easier for them to simply discuss their ideas, but I needed to draw images so that these concepts could become tangible in my mind.
After practicing these rough sketches, I began to flesh out my thoughts and create new questions that needed to be answered before I could validate a design. Yet again, we needed to revisit the clinics to confirm the specifications for our prototype. Once we were done communicating with the physicians and technologists, we briefly re-entered the concept generation phase. However, this time, we spent a few hours drawing out our ideas and delivering a so called “elevator speech” about our concepts to each other, emphasizing the needs being addressed and the project’s viability.
All in all, this projected us forward in finalizing the details of our prototype. It’s easy to simply communicate a lavish idea with words, but to take that verbatim and actually transform it into a physical object was much more difficult than we had predicted. These handheld cards could demonstrate the objective of the project, benefits, and drawbacks in an effortless, simple manner, allowing the audience to understand a summary of your thought process immediately.